Abstract
Objective To review our experience in a series of patients who underwent revision endoscopic pituitary surgery.
Methods Retrospective chart review.
Results A total of 27 patients were included in the study. Of the 21 patients who required nasoseptal flap reconstruction, a left-sided nasoseptal flap was successfully used in 13 patients. Gross total or near-total resection of tumor was achieved in 74.1%. Cavernous sinus invasion and presentation with residual disease were identified as factors limiting extent of resection (p = 0.002 and 0.009, respectively). A statistically significant difference (p = 0.027) was noted between mean largest tumor dimension in patients with gross total resection and those with near-total or subtotal resection. Complications occurred in 22% and included postoperative temporary diabetes insipidus (n = 2), postoperative hypotension (n = 2), new anterior pituitary insufficiency (n = 1), and right-sided abducens palsy (n = 1).
Conclusions Revision endoscopic pituitary surgery is advantageous but technically challenging. Cavernous sinus invasion and presentation with residual disease were significant factors limiting extent of resection. Suprasellar extension was not a factor limiting extent of resection and may prove to be an advantage over microscopic speculum-based approaches. Because of the right-sided scarring from prior surgery, a left-sided nasoseptal flap is reliable and advantageous.
Introduction
Pituitary adenomas make up ∼ 10% of primary intracranial neoplasms. Most of these lesions are benign with an indolent growth pattern. True pituitary carcinomas with documented metastasis are exceedingly rare.1 Pituitary adenomas can present as hormonally active tumors with autonomous hormone secretion or, more commonly, as nonfunctioning lesions with symptoms related to mass effect. The most common presenting symptoms include headaches, visual changes related to suprasellar extension toward the optic chiasm, and cranial nerve deficits (CN III, IV, V1, V2, VI palsies) with lateral extension into the cavernous sinus.2 3 4
Surgical management of these lesions has evolved since the first major series described by Cushing in the 1930s. Cushing published a series of ∼ 400 patients undergoing sublabial, transseptal, and transsphenoidal excision of these tumors. He eventually abandoned this technique for a transfrontal approach due to a high rate of symptomatic tumor recurrence.5 6
In the 1950s, with the advent of microscopic techniques, we saw further advancement in surgical management of these lesions.7 Finally, within the last decade, we have seen the endoscopic endonasal approach (EEA) technique gain prominence.8 This technique is now well described, along with its efficacy and safety.
Multiple large series have reported successful gross tumor resection (GTR) (∼ 80%), hormone resolution (∼ 80–85%) and improved visual symptoms along with low incidence of complications (< 2% cerebrospinal fluid [CSF] leak, 0.24% mortality).2 However, the management of recurrent or residual tumors is not as well described within the literature.
The rate of recurrence remains high and is typically thought to range from 7% to as high as 33%. This varies with the type of adenoma, with a 10% risk with growth hormone–secreting tumors, 13% with adrenocorticotropic hormone–secreting tumors, 20% for prolactinomas, and 26% with nonsecreting adenomas.9 10 11
The optimal management of these lesions is still highly contentious. Few published studies have included the cure rate of recurrent pituitary tumors after a previous microsurgical transsphenoidal approach. The cure rate of the second transsphenoidal selective surgical resection is thought to be significantly lower than that of primary surgery, with significant increased morbidity.8 11 12
Revision surgery presents with technical challenges related to scarring and an altered anatomy from the previous dissection. The second operation is usually more difficult and harbors more risks secondary to the distorted anatomy such as septal and intrasellar scarring, as well as sequelae of the previous surgery, such as postoperative mucoceles.11 13 Because of the low success rate and high morbidity, some authors have recommended not reexploring such patients, recommending radiation treatment instead, or exploring only as a last resort for highly symptomatic patients.12 14
This current study aims to assess the technical challenges to the approach in the endoscopic method for treatment of recurrent and residual pituitary tumors in patients who were previously treated with microscopic speculum-based or endoscopic approaches. We focus on efficacy, complications, and technical considerations of operating in a previously operated/irrradiated field.
Methods
We retrospectively reviewed a database of all patients undergoing endoscopic endonasal surgery at UCLA Medical Center from August 2010 through June 2013. A total of 27 patients were identified who required revision pituitary surgery. All 27 patients included in this study had recurrent (48%) or residual (52%) pituitary adenomas. Table 1 outlines the patients' characteristics. The senior authors, neurosurgeon (M.B.), and otolaryngologists (M.W. and J.S.) were the primary surgeons in all of the cases. The patient demographics, lesion size and volume, pathology, complications, adjuvant treatment, and clinical outcomes were analyzed. Extent of resection was based on magnetic resonance imaging (MRI) obtained pre- and postoperatively. Charts were further reviewed for type of skull base reconstruction, hospital course, and development of complications.
Table 1. Patient information including type of pathology, extent of tumor invasion, and method of reconstruction.
| Age, y | Sex | Largest tumor dimension, mm | Secretory? | Cavernous extension? | Suprasellar extension? | Type of reconstruction |
|---|---|---|---|---|---|---|
| 22 | M | 13 | Yes | Yes | No | Right nasoseptal flap |
| 25 | F | 5 | Yes | No | No | Right nasoseptal flap |
| 59 | M | 33 | No | Yes | Yes | Left nasoseptal flap |
| 39 | F | 5 | Yes | Yes | No | Left nasoseptal flap |
| 46 | F | 5 | No | No | No | No reconstruction |
| 64 | M | 23 | No | Yes | Yes | Left nasoseptal flap |
| 63 | F | 14.5 | No | No | Yes | Absorbable graft clipped to dura, absorbable plate, abdominal fat, left nasoseptal flap |
| 35 | F | 23 | Yes | Yes | No | Left nasoseptal flap |
| 50 | M | 26 | No | No | No | Left nasoseptal flap |
| 22 | F | 15 | No | No | Yes | Absorbable graft clipped to dura, absorbable plate, abdominal fat, left nasoseptal flap |
| 50 | M | 20 | No | No | No | Left nasoseptal flap |
| 53 | M | 72 | Yes | Yes | Yes | Absorbable graft clipped to dura, absorbable plate, abdominal fat, left nasoseptal flap |
| 22 | M | 20 | Yes | Yes | No | Absorbable graft clipped to dura, absorbable plate, abdominal fat, left nasoseptal flap |
| 40 | F | 43 | No | Yes | Yes | Absorbable graft clipped to dura, left nasoseptal flap |
| 63 | F | 14 | No | Yes | Yes | Right nasoseptal flap |
| 54 | F | 24 | No | No | Yes | Right nasoseptal flap |
| 26 | F | 32 | Yes | Yes | No | Abdominal fat, right inferior turbinate flap |
| 46 | F | 5 | Yes | No | No | Abdominal fat, septal bone, right nasoseptal flap |
| 78 | M | 25 | No | No | Yes | Abdominal fat, absorbable plate, right nasoseptal flap |
| 33 | F | 14 | Yes | Yes | No | Right nasoseptal flap |
| 31 | F | 12 | Yes | No | No | No reconstruction |
| 52 | M | 27 | No | Yes | Yes | Dura matrix graft |
| 62 | M | 24 | No | No | Yes | Absorbable graft clipped to dura, absorbable plate, abdominal fat, right nasoseptal flap |
| 34 | F | 17 | Yes | Yes | Yes | Absorbable graft clipped to dura, absorbable plate, abdominal fat, right nasoseptal flap |
| 46 | F | 33 | No | Yes | Yes | Abdominal fat, free mucosal graft from middle turbinate |
| 66 | M | 34 | No | Yes | Yes | Abdominal fat, left nasoseptal flap |
| 40 | F | 2 | Yes | No | No | Free mucosal graft from sella |
To assess whether baseline variables resulted in reduced extent of resection, the nonparametric qualitative variables were cross-classified into contingency tables and compared using chi-square tests. The Fisher exact test was used when expected value was < 5. To assess tumor size and extent of resection, mean largest tumor dimension was compared between the GTR and near-total resection/subtotal resection (NTR/STR) groups using the Student t test. A p value ≤ 0.05 was considered significant for all statistical tests. Statistical analyses were performed in SPSS v.21 (IBM Corp., Armonk, New York, United States).
Results
Twenty-seven patients were identified within our database (Table 1). The mean age was 45 years, with a range of 22 to 78 years. There were 11 men and 16 women. All patients had at least one prior surgery, ranging from 1994 to 2013. The average length of time from the previous surgery was 75.6 months. Approximately 52% (14/27) of the patients had a known residual tumor, where the lesion was deemed “unresectable” or the procedure was aborted for another reason. Six of the patients had two prior surgeries, and two of the patients had three or more prior surgeries. Twenty-three patients had previous microscopic speculum-based approaches only; one patient had a combination of surgeries, which included microscopic speculum-based approaches and endoscopic approaches; and three patients had prior endoscopic approaches only. One patient had a prior craniotomy. In addition, one had undergone prior stereotactic radiosurgery. Patients in this series all underwent EEAs for tumor removal. Image guidance was used in all cases.
A vast majority of the tumors, 81% (22/27), were macroadenomas. In addition, most of the lesions, 56% (15/27), involved the cavernous sinus. Cavernous sinus invasion was identified on preoperative MRI imaging and confirmed intraoperatively. Overall, 44% (12/27) were secretory adenomas. GTR, defined as no residual tumor on postoperative MRI, was achieved in 63% (17/27) of the patients (Fig. 1). In an additional 11% (3/27), NTR was achieved, defined as > 95% reduction in tumor volume on postoperative MRI. In the remaining 26% of patients (7/27), an STR was achieved. There was a statistically significant difference (p = 0.027) between mean largest tumor dimension for patients with GTR (16.9 mm; standard deviation [SD]: 10.8) and NTR/STR (29.4 mm; SD: 17.0). Of patients with secretory tumors (12/27), seven patients achieved GTR, one patient had a NTR, and four patients had a STR. All patients with secretory adenomas with GTR remained in remission.
Fig. 1.
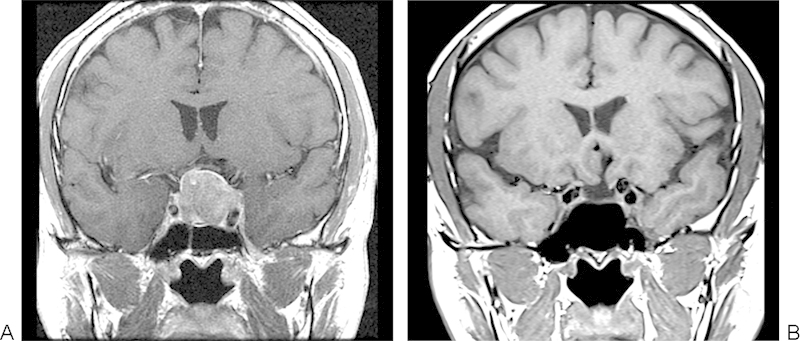
(A) Preoperative magnetic resonance imaging (MR)I demonstrating a large recurrent pituitary adenoma. (B) Postoperative MRI shows gross total removal of the adenoma.
Twelve patients in our series had undergone prior microscope speculum-based approaches presenting with residual disease. Of these 12 patients, 7 of them had both cavernous sinus and suprasellar extension, two patients had suprasellar extension only, two had cavernous sinus extension only, and one had no evidence of suprasellar or cavernous sinus invasion. Of the nine patients with cavernous sinus invasion, GTR was only achieved in one patient.
Baseline characteristics such as suprasellar extension, cavernous sinus involvement, secretory status, and presenting with residual disease after failed initial surgery were analyzed to identify factors resulting in reduced extent of resection. Presentation with residual disease after failed initial resection (chi-square: 9.430; p = 0.009) and cavernous sinus invasion (chi-square: 12.706; p = 0.002) were the only factors identified to result in reduced extent of resection. Suprasellar extension (chi-square: 2.114; p = 0.347) and secretory status (chi-square: 0.681; p = 0.712) did not result in a significant difference in extent of resection; however, a larger sample size will be needed to better assess these factors.
Nasoseptal flap reconstruction was used in 78% (21/27) of patients. When needed, reconstruction was performed via a left-sided nasoseptal flap in 48% (13/27) of patients. When scarring did not significantly impair the vascular supply of the nasoseptal flap, a right-sided nasoseptal was used in 30% of patients. An inferior turbinate flap was used in one patient, a free mucosal graft was used in two patients, and three patients did not require mucosal coverage for reconstruction.
Postoperative complications were largely minor and occurred in 22% of patients. Two patients developed postoperative temporary diabetes insipidus (DI) requiring only a single dose of desmopressin. Both patients had subsequent resolution of their DI prior to discharge. Two patients developed postoperative hypotension requiring prolonged stay in the intensive care unit (ICU). One patient developed new anterior pituitary insufficiency requiring hydrocortisone replacement and readmission. One patient developed right-sided abducens palsy. This occurred in a patient who had previously had three transsphenoidal surgeries, a superficial temporal artery to middle cerebral artery bypass, and had been treated twice with radiosurgery presenting with the bulk of her tumor in the right cavernous sinus.
An intraoperative CSF leak was encountered in 41% and reconstructed intraoperatively with a multilayer closure. No patients required lumbar drain placement, and no patients developed CSF leaks postoperatively. Most patients (89%) were admitted directly to the surgical ward postoperatively and did not require ICU admission. Length of hospital stay was minimal with 82% of patients discharged from the hospital by postoperative day 3e with most patients leaving on postoperative day 2 (48%).
Discussion
Using an endoscopic endonasal approach, we were successful in obtaining a GTR or NTR rate in 74% of the patients with residual or recurrent pituitary tumors. Postoperative complications occurred in 22%. These outcomes are contrasted with primary EEA cases where the successful excision rate is ∼ 80% with a 2% complication rate.2
Of the seven patients where we obtained an STR, all had extensive involvement of the cavernous sinus, and the residual tumor was left within this region. Indeed, statistical analysis revealed cavernous sinus invasion as a significant factor resulting in reduced extent of resection (chi-square: 12.706; p = 0.002). Cavernous sinus involvement has been a well-recognized risk factor for failure in surgery and been cited as a frequent cause of failure in revision cases. Cappabianca et al reported a series from Italy of 12 revision cases.11 Of the six where they failed to obtain GTR, all had involvement of the cavernous sinus. Similar findings were noted by Rudnik et al in a series from Poland where they were able to achieve GTR in 40% of revision cases; however, when they examined the subgroup that did not involve the cavernous sinus, their success rate was 70%.1 Finally, Abe and Lüdecke reported a series from Japan on revision cases where they were unable to cure any patient with tumor infiltrating the cavernous sinus.13 In addition to cavernous sinus involvement, tumor size and invasiveness of the adenoma are also important predictive factors. In our series, there was a statistical difference between mean largest tumor dimension in the GTR and NTR/STR groups (p = 0.002) supporting increased size as a factor limiting complete resection. Multiple other authors have also noted the importance of tumor size.13 15 16
The benefits of the endoscopic approach were recently emphasized by Paluzzi et al in their series of 555 patients who underwent a purely EEA for pituitary adenoma resection.16 Their data supported the added advantage of the endoscopic approach in addressing adenomas with extension into the suprasellar compartment, those invading the cavernous sinus, and in recurrent adenomas. In fact, in 91 patients with residual and/or recurrent disease in their series, GTR/remission was possible in 49.5%. Due to insufficient baseline medical records, they were unable to reliably identify which patients had undergone microscopic speculum-based approaches, and thus they were not able to comment statistically on the superiority of the endoscopic approach over the microscopic approach in all cases, but the endoscopic approach was confirmed to be safe and efficacious, particularly for challenging and recurrent adenomas.
A recent large series from McLaughlin et al confirmed the value of endoscopy in removal of residual tumors after speculum-based approaches. Their series showed that endoscopic visualization led to an additional adenoma removal in over a third of patients. Residual tumor in their series was typically removed from suprasellar extension and folds of collapsed diaphragma sellae or along or within in the medial cavernous sinus.17 In 7 of 12 patients presenting with residual disease after failed microscopic approaches in our series, a GTR/NTR resection was possible.
Our data suggest that suprasellar extension may be better addressed with endoscopy because suprasellar extension was not a significant factor for extent of resection (chi-square: 2.114; p = 0.347). In fact, all five patients presenting with suprasellar extension only had full GTR. However, of the nine patients presenting with residual disease in the cavernous sinus after failed microscopic approaches, only one patient had GTR. It is technically difficult to clear extensive tumor from the cavernous sinus due to bleeding and concern for injuring the carotid and cranial nerves. Our technique involves complete exposure of the medial aspect of the cavernous sinus from the superior intercavernous sinus to the inferior intercavernous sinus. This allows exploration of the sinus and removal of tumor along the medial wall. However, the risk of exploration more laterally must be balanced against the increased risk involved, particularly in surgery for a benign tumor. Therefore, in this study suprasellar extension was better addressed by the endoscopic approach; however, the same could not be said regarding cavernous sinus invasion. A larger sample size is needed to confirm these findings.
Our series did not have any postoperative CSF leaks. CSF leaks are reported to be the most common minor complication associated with EEAs, with a rate of 2 to 27%.2 In our series, if the patient was noted to have an intraoperative leak at the time of resection, seen in 41% of the cases, the surgical site was closed in layers. We used an abdominal fat graft, bone, or absorbable plate, followed by a nasoseptal flap. No patient required placement of a lumbar drain. Using this method, our postoperative CSF leak rate was lower than that of many series of primary EEA pituitary surgeries.
An additional explanation for the lower rate of CSF leaks may be a modification of our technique. We generally use a right-sided nasoseptal flap for sellar reconstruction. There is an advantage to using a right-sided flap because the drill is usually passed through the left nostril and may inadvertently catch and damage a left-sided flap. However, it was noted in the experience of the senior authors that the right-sided nasoseptal flap was difficult to raise secondary to prior scarring, and the vascular pedicle was subsequently tentative. Speculum-based approaches are nearly always done through the right nostril, and the bone inferior to the sphenoid ostium is taken down to provide better access to the sella. As a result, there is increased scarring and compromise of the vascular supply from the posterior septal branch of the sphenopalatine artery, which supplies the right-sided nasoseptal flap (Fig. 2). In one instance, a right-sided nasoseptal flap was attempted and abandoned because the mucosal bridge between the sphenoid ostium and the choana was so tenuous that it was transected. In this patient, a left-sided nasoseptal flap was successfully utilized.
Fig. 2.
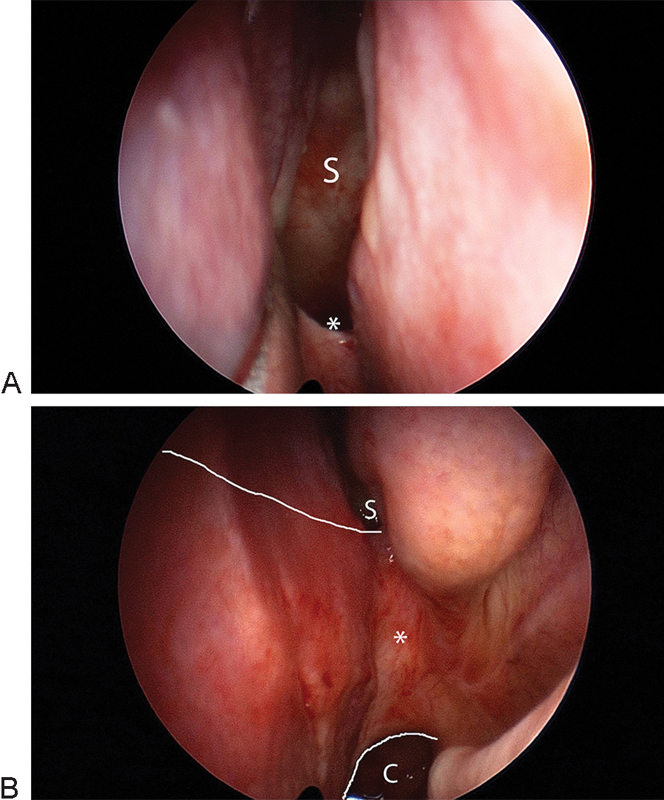
Appearance of the posterior nasal cavity in a revision pituitary case. (A) There is scarring of the right posterior nasal cavity, where the anterior sphenoid has been widely opened (S). The vascular pedicle for a nasal septal flap would be compromised (asterisk) due to the inferior widening of the right sphenoid ostium. (B) In contrast, the left posterior nasal cavity does not have a widely opened sphenoid ostium. The vascular pedicle for a nasal septal flap (asterisk) is well preserved between the sphenoid ostium (S) and the choana (C). White lines demonstrate the outline of the flap incisions.
Based on this early experience, it was observed that there was generally less scarring of the left posterior nasal cavity, and the mucosal bridge between sphenoid opening and choana, which contains the vascular pedicle for the nasoseptal flap, was better preserved. Therefore, prior to utilization of a right-sided nasoseptal flap, the mucosal bridge between the sphenoid opening and choana was assessed for degree of scarring and narrowness. If excessively scarred and narrowed, a left-sided nasoseptal flap was chosen for reconstruction. This improved the success of raising a flap with a cleaner dissection and a more robust vascular pedicle. There were 13 left-sided nasoseptal flaps in this series. In addition, when a nasoseptal flap was not an option due to a septal perforation, additional techniques were used including an inferior turbinate flap or a free mucosal graft. These technical modifications allowed for improved closure of the surgical defect.
Revision endoscopic pituitary surgery is more difficult and harbors more risks because the surgeon is faced with distorted anatomy and scar tissue. Image guidance was essential to identify otherwise obscured anatomic landmarks. However, our series shows that the endoscopic approach is a viable option for patients presenting with recurrent or residual disease. The importance of a dual-team approach with the otolaryngologist and neurosurgeon should also be underscored. The role of the otolaryngologist is critical in the revision case as his or her expertise in evaluating aberrant nasal anatomy is critical in evaluating optimal choice for reconstruction. Furthermore, despite a high degree of comfort by the neurosurgeon with the zero-degree endoscope, the use of an angled endoscope by an otolaryngologist can often aid in visualization of the lateral and superior aspects of the sella, which can often harbor residual or recurrent disease. Using this team approach, our overall success rate of 74% GTR or NTR is comparable with primary surgery, with similar rates of complications. Longer follow-up data will be necessary to analyze locoregional control and long-term survival data.
Notes
Presented at the Annual Meeting of the North American Skull Base Society; February 18–20, 2011; Phoenix, AZ.
References
- 1.Rudnik A, Zawadzki T, Gałuszka-Ignasiak B. et al. Endoscopic transsphenoidal treatment in recurrent and residual pituitary adenomas—first experience. Minim Invasive Neurosurg. 2006;49(1):10–14. doi: 10.1055/s-2006-932126. [DOI] [PubMed] [Google Scholar]
- 2.Tabaee A, Anand V K, Barrón Y. et al. Endoscopic pituitary surgery: a systematic review and meta-analysis. J Neurosurg. 2009;111(3):545–554. doi: 10.3171/2007.12.17635. [DOI] [PubMed] [Google Scholar]
- 3.Hornyak M, Couldwell W T. Multimodality treatment for invasive pituitary adenomas. Postgrad Med. 2009;121(2):168–176. doi: 10.3810/pgm.2009.03.1989. [DOI] [PubMed] [Google Scholar]
- 4.Melmed S. Update in pituitary disease. J Clin Endocrinol Metab. 2008;93(2):331–338. doi: 10.1210/jc.2007-1409. [DOI] [PubMed] [Google Scholar]
- 5.Cushing H. Intracranial tumors: notes upon a series of two-thousand verified cases with surgical-mortality percentages pertaining thereto. JAMA. 1933;100(4):284. [Google Scholar]
- 6.Cohen-Gadol A A, Laws E R, Spencer D D, De Salles A A. The evolution of Harvey Cushing's surgical approach to pituitary tumors from transsphenoidal to transfrontal. J Neurosurg. 2005;103(2):372–377. doi: 10.3171/jns.2005.103.2.0372. [DOI] [PubMed] [Google Scholar]
- 7.Hardy J, Wigser S M. Trans-sphenoidal surgery of pituitary fossa tumors with televised radiofluoroscopic control. J Neurosurg. 1965;23(6):612–619. doi: 10.3171/jns.1965.23.6.0612. [DOI] [PubMed] [Google Scholar]
- 8.Jho H D, Carrau R L. Endoscopic endonasal transsphenoidal surgery: experience with 50 patients. J Neurosurg. 1997;87(1):44–51. doi: 10.3171/jns.1997.87.1.0044. [DOI] [PubMed] [Google Scholar]
- 9.Ciccarelli E, Ghigo E, Miola C, Gandini G, Muller E E, Camanni F. Long-term follow-up of 'cured' prolactinoma patients after successful adenomectomy. Clin Endocrinol (Oxf) 1990;32(5):583–592. doi: 10.1111/j.1365-2265.1990.tb00901.x. [DOI] [PubMed] [Google Scholar]
- 10.Abosch A, Tyrrell J B, Lamborn K R, Hannegan L T, Applebury C B, Wilson C B. Transsphenoidal microsurgery for growth hormone-secreting pituitary adenomas: initial outcome and long-term results. J Clin Endocrinol Metab. 1998;83(10):3411–3418. doi: 10.1210/jcem.83.10.5111. [DOI] [PubMed] [Google Scholar]
- 11.Cappabianca P, Alfieri A, Colao A. et al. Endoscopic endonasal transsphenoidal surgery in recurrent and residual pituitary adenomas: technical note. Minim Invasive Neurosurg. 2000;43(1):38–43. doi: 10.1055/s-2000-8814. [DOI] [PubMed] [Google Scholar]
- 12.Long H, Beauregard H, Somma M, Comtois R, Serri O, Hardy J. Surgical outcome after repeated transsphenoidal surgery in acromegaly. J Neurosurg. 1996;85(2):239–247. doi: 10.3171/jns.1996.85.2.0239. [DOI] [PubMed] [Google Scholar]
- 13.Abe T Lüdecke D K Recent results of secondary transnasal surgery for residual or recurring acromegaly Neurosurgery 19984251013–1021.; discussion 1021–1022 [DOI] [PubMed] [Google Scholar]
- 14.Barkan A L. Acromegaly. Trends Endocrinol Metab. 1992;3(6):205–210. doi: 10.1016/1043-2760(92)90029-z. [DOI] [PubMed] [Google Scholar]
- 15.Giovanelli M Losa M Moritini P Acromegaly: surgical results and prognosis. In: Landolt A M Vance L Reilly P L, eds. Pituitary Adenomas. New York, NY: Churchill Livingstone; 1996333–351. [Google Scholar]
- 16.Paluzzi A Fernandez-Miranda J C Tonya Stefko S Challinor S Snyderman C H Gardner P A Endoscopic endonasal approach for pituitary adenomas: a series of 555 patients Pituitary 2013. August 2 ( Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 17.McLaughlin N, Eisenberg A A, Cohan P, Chaloner C B, Kelly D F. Value of endoscopy for maximizing tumor removal in endonasal transsphenoidal pituitary adenoma surgery. J Neurosurg. 2013;118(3):613–620. doi: 10.3171/2012.11.JNS112020. [DOI] [PubMed] [Google Scholar]


