Abstract
Relatively few interventions have tested the efficacy of female condom promotion either alone or in combination with other barrier methods. We evaluated the efficacy of a two-session (enhanced) cognitive-behavioral intervention (EI) (n=147) against aone-session control (minimal) educational intervention (MI) (n=149) to promote female condom (FC) use among female students aged 18-28 at a South African university. We assessed change from baseline to 2.5 and 5 months in number of vaginal intercourse occasions unprotected by male or female condoms in EI vs. MI using generalized linear models with a log link function and GEE. Both groups reported significant reductions in number of unprotected vaginal intercourse occasions from baseline to each follow-up, with no significant difference between the two-session and single-session intervention. Introduction of a brief group-based MI FC promotion intervention with FC access holds promise for delivery in clinics and other community venues.
Keywords: Female condom, South Africa, University students, HIV, Pregnancy
Introduction
The Reproductive Health Supplies Coalition and UN Commission on Life-SavingCommodities for Women and Childrenidentified the female condom (FC) as one of several overlooked and under-used reproductive health technologies having the potential to expand choice in family planning and HIV/STI prevention programs, add value to the method mix, and respond to the needs of diverse clients[1, 2].The FC has also been cited as an essential strategy for pregnancy and HIV/STI prevention by the World Health Organization[3]. A number of studies [4-7] and one review [8]suggest that concurrent availability of female and male condomsresults in higher rates of protected sex compared with only male condom availability.The FC affords women greater control over negotiating protection of their health[9].
The FC as a tool for reducing HIV/STI and pregnancy risks has not been fully recognized, resulting in inadequate marketing [2] and underfunding of programs [10, 11]. Despite increased FC distribution globally (from 25 million units in 2007 to 50 million units in 2010[12], and in 2012, 60 million units[13]), distribution still lags behind that of the male condom [14].The average unit cost is about US $0.57 for FC compared to $0.03 for a male latex condom [2].
FC acceptability and uptake may increase, however, now that there are several new FCsusing alternate designs and materials and others on the horizon[15-17].Coupled with new product development have been intensified strategic campaigns of several international groups, including the United Nations Population Fund's Global Female Condominitiative, which provides support to at least 23 countries to scale up FC programming and the Universal Access to Female Condoms Joint Programme, through the provision of FCs and educational programs targeting men, youth and women at risk. The governments of a number of countries, including South Africa, Brazil and India,are committed to promoting the FC, reflected in their large-scale purchase of FCs for public-sector distribution[18]. Programming support is critical as it has been documented that funding for the product, without investment in effective and comprehensive programming, can lead to stock-outs, lack of access and limited availability[19].
Methods that women can use such as the female condom are an important prevention option to enable women to protect themselves, especially in regions such as sub-Saharan Africa, where heterosexual transmission is the predominant mode of HIV transmission.South Africa has a generalized HIV epidemic with an HIV prevalence of 12.2% and the largest HIV-positive population in the world (6.4 million persons) [20].HIV prevalence is 14.4% among South African women,and among women aged 20-24, 17.4% compared to 5.1% among men of the same age, peaking at 36.0% among women aged 30-34% and at 28.8% among men aged 35-39[20]. TheHIVincidence rate among female youth aged 15–24 is more than four times higher than the incidence rate found in males in this age group (2.5% vs. 0.6%) and[20], and black African females aged 20–34 years have the highest incidence of HIV at (4.5%) compared to other population groups. Unintended pregnancy rates also are high, with one study estimating 66% of young women having had an unintended pregnancy[21], despite a 65% contraceptive use prevalence[22].
South Africa has highly-supportive government policies for the FC [23] and one of the largest, best-established, government-funded, public-sector FC programs world-wide, with robust distribution in clinic and community venues [15, 17].In 2010, the South African government procured 5.1 million FC units in 2010[14], and for 2012, projected procurement more than doubled to 11 million FCs[24].This creates a receptive environment for testing interventions to promote the FC.However, a 2008 population-based household survey found that only 7.2% of sexually active women and 6.0% of men reported ever having used the FC [25]. The target group for this intervention, university students in South Africa, is an understudied population at risk for HIV/STIs, with HIV prevalence at 3.8% among sexually active students.In KwaZulu-Natal, prevalence was 6.1% in students overall and 8.7% in African Black students in a survey of 22 institutions of higher learning in 2008-2009[26]. To our knowledge, there are no studies in South Africa that have tested the efficacy of an intervention that promoted the FC.
Relatively few intervention studies have tested the efficacy of FC promotion either alone [27-35], or in combination with other barrier methods [4, 5, 36-38], and few have been conducted in sub-Saharan Africa [6, 27, 31, 35]; none have been conducted with university students.We compared the efficacy of a two-session group-delivered Enhanced Intervention (EI), which included didactic information delivered in the MI, in addition to behavioral rehearsal of FC use, partner negotiation,and opportunity to practice these skills and problem-solve in the second session,against a one-session control information-only,group-delivered (MI). We assessed whether the EIcompared to the MI resulted in (1) a greater decrease in the proportion of vaginal sex acts unprotected by condoms, (2) a greater increase in the proportion of vaginal sex acts protected by FCs, and (3) a greater number of female condoms used.
Methods
Participants and Procedures
Between March 2008 and October 2009 we recruited women on the campus of a higher education institution in KwaZulu-Natal,South Africa,using outreach atcampus sites where students congregated. Women were eligible for study participation if they met the following criteria: 18 years or older; full-time students; self-reported HIV-negative or unknown serostatus; not pregnant or wanting to become pregnant in the next nine months; reported condom-unprotected vaginal intercourse in the past two months; capacity to complete informed consent and be interviewed; willing to have assessments and interventions audio-recorded. First-year, first semester students were excluded because of high drop-out rates.
We approached students to inform them about the study and determine whether they might be interested in volunteering to participate. Following screening, eligible students completed written informed consent and were scheduled for a baseline interview.After the baseline interview, participants were invited to attend an intervention randomization meeting within the following three weeks,where they were randomly assigned,in blocks of two,to either the one-sessionMI (N=149) or two-sessionEI(N=147); they participated in their assigned intervention on the day of randomization.Those randomized to the two-session intervention attended the second session approximately three weeks after the first. All study staff, other than the intervention facilitators, were blinded to intervention condition. Follow-up assessments were conducted at 2.5 and 5 months after completion of the intervention. Participants received the ZAR equivalent of $4 for the baseline assessment, $10 for the first follow-up assessment, and $15 for the second follow-up interview. The Institutional Review Board of the New York State Psychiatric Institute-Columbia University Department of Psychiatry and Research Ethics Committees at two South African universities, including the institution where the study was conducted, approved the study.
Description of Interventions
The enhanced and minimal (control) interventions, developed and refined by the US-South African Research team, including Student Health Service and Counseling Centre staff, are described below.
Minimal Intervention
The one-session, 1-1.5 hour MIfocused on HIV/STI transmission and safer sex practices;personal vulnerability to disease and pregnancy; ways to address these risks and problems encountered; importance of barrier method use and universal safer sex precautions; FC's ability to prevent both HIV/STIs and pregnancy; how to use, insert, remove and dispose of FCs; and comparison of the use-effectiveness and other features of the male and female condom.In addition, a brief review of the female reproductive system was provided, and FC insertion was demonstrated on a pelvic model, but insertion practice by participants on the model was not done. The facilitators elicited perceptions about the FC and anticipated problems with use. The intervention also sensitized women to the potential for partner abuse and provided instruction on how to assess signs of potential abuse and presented strategies to minimize the risk. Women were cautioned about possible dangers of initiating male or female condom use in the presence of these signs, and were provided with pamphlets listing referral sources.
Enhanced Intervention
The two-session, 4-5 hour EI,grounded in Social Learning Theory [39, 40], included the same information as the one-session MI, but also covered partner negotiation, FC insertion skills, and personal goal-setting to achieve HIV/pregnancy prevention. The EI specifically addressed (1) obtaining and maintaining a condom supply; (2) having condoms for use when needed; (3) negotiating condom use with partners in a way likely to succeed; (4) overcoming objections, resistance, refusal and violence that might be encountered; (5) inserting and using female and male condoms correctly;(6) using cognitive restructuring, behavioral rehearsal, and structured practice with feedback strategies;(7) increasing positive expectancies for FC use by fostering positive peer norms; and (8) providing encouragement and reinforcement through social support.
Women in both groups were given a supply of 10 FCs and 10 male condoms and had access to free male and female condoms through the Campus Health Service.All sessions were conducted in English, but isiZulu was spoken when issues needed further clarification. The interventions were facilitated by study staff with nursing or social science backgrounds trained and experienced in group facilitation. Each of the interventions was delivered by a different interventionist to avoid contamination across the arms. The quality of intervention delivery was monitored by the study intervention director and was considered to be similar.In both groups,facilitators were assisted by trained student peer educators who led many of the group exercises.
Measures
Primary and secondary outcomes
The primary study outcome was the number of vaginal intercourse occasions unprotected by either male or female condoms in the past 2.5 months across all partners.Unprotected occasions, in contrast to percent protected occasions, is an indicator of overall public health impact since the raw number of potential viral exposures is more clearly interpretable in terms of infection risk than percent condom use, which can mask different levels of risk among those reporting the same rate of use (e.g., two persons reporting 50% condom use who have 100 or 10 sex occasions would have 50 and 5 unprotected occasions, respectively). Secondary outcomes included the (1) number of FCs used; (2) proportion of FC-protected vaginal intercourse occasions across all partners; (3)proportion of vaginal intercourse occasions protected by either a female or male condom; and (4) male/female condom use at last sex occasion.
Other sexual risk-related outcomes
Perceived susceptibility to HIV and unintended pregnancy were measured by single itemsasking how greatthe participant thought her chances were of getting infected with HIV or getting pregnant unintentionally in the next six months, with responses on a four-point Likert scale ranging from no risk at all to great risk. Single items were used to assess participants’ overall attitude toward the male condom and to the FC – How do you feel about using the male condom? the female condom? Responses were on a five-point Likert scale ranging from extremely positive to extremely negative. Participants used the same metrics to evaluate their main partner's perceived attitude toward male and female condom use. Intention to use female condoms was assessed by a single item about the likelihood of using a female condom during sex. Responses were on a four-point Likert scale ranging from very unlikely to very likely.Peer norms for condom use were measured by an eight-item scale (α=0.71)developed for this study with items that assessed what participants thought the women they knew were doing regarding condom use (e.g., Women I know will say “no” to sex if a partner won't use condoms). Response categories were on a four-point Likert scale, ranging from strongly disagree to strongly agree.Condom self-efficacy,which assessed participants’ confidence in using condoms, was adapted from a measure used in Project FIO [41, 42] and included items suggested by pilot data as relevant to the South African context. It was measured by a 13-item scale (α=0.78) (e.g., How sure are you that you could insist on using a condom if a main partner threatens to leave you if he has to use a condom?). Responses ranged on a four-point Likert scale from very unsure to very sure. Gender norms for women's and men'ssexual behavior were measured with a nine-item scale tapping male dominant sex roles (α=0.65) originally developed on a sample of young South African adults[43] (e.g.,Men cannot live with just one girlfriend). Response categories were on a four-point Likert scale, ranging from strongly disagree to strongly agree. Hormonal contraceptive use was measured by whether participants used the pill, injectable, or emergency contraception, with yes, no responses. Total number of sex occasions was assessed across all partners.
Statistical Analysis
Descriptive statistics were generated overall and by group for demographic variables at baseline, as well as for sexual behavior and pertinent knowledge, normative and attitudinal factors at baseline and follow-ups. Baseline differences were evaluated using t-tests for continuous and chi-squared test for categorical variables. The a priori primary analysis, following intent-to-treat principles, compared the EIto MIin terms of the meanchange from baseline to 2.5 months post-intervention (FU1) in total number of vaginal intercourse occasions unprotected by male or female condoms. We used generalized linear models (GLM) with a log link function. The model included the group indicator for EI (vs. MI), the indicator for time (FU1 vs. baseline), and the interaction of the two indicators. The regression coefficient corresponding to the group-by-time interaction term estimates the logarithm of the ratio of the two study group population rate ratiosand thus represents the effect of the intervention on change in unprotected sex occasions.The rate ratio is defined as the mean number of vaginal intercourse occasions unprotected by either male or female condoms at 2.5 months divided by the mean number of vaginal intercourse occasions unprotected by either male or female condoms atbaseline. We employed generalized estimating equations (GEE) to account for the effect of intra-cluster correlations introduced by multiple assessments on the same participant. An over-dispersion parameter was used to account for the between-subject heterogeneity for Poisson regression analysis. Rubin's [44] multiple imputation method with 11 repeated imputations was employed to impute the missing endpoint for conducting the intent-to-treat analysis.
In secondary analyses, we evaluated longer-term intervention effects on reducing unprotected vaginal sex occasions, comparing the EIto the MIon the change from baseline to five-month follow-up (FU2). We also compared the two groups on other sexual risk-related secondary outcomes, such as condom use self-efficacy and peer norms for condom use. We used GLM with identity, logit, and log link function for continuous, dichotomous, and count variables respectively. As with the primary analysis, GEE methodology was employed to account for the correlation due to repeated measures and an over-dispersion parameter was used to account for the between subject heterogeneity when appropriate. Data were cleaned and processed in SPSS (Chicago, IL) version 20 and regression models run in SAS version 9.3 (IBM, Cary, NC).
Results
Participant flow and characteristics of the randomized sample
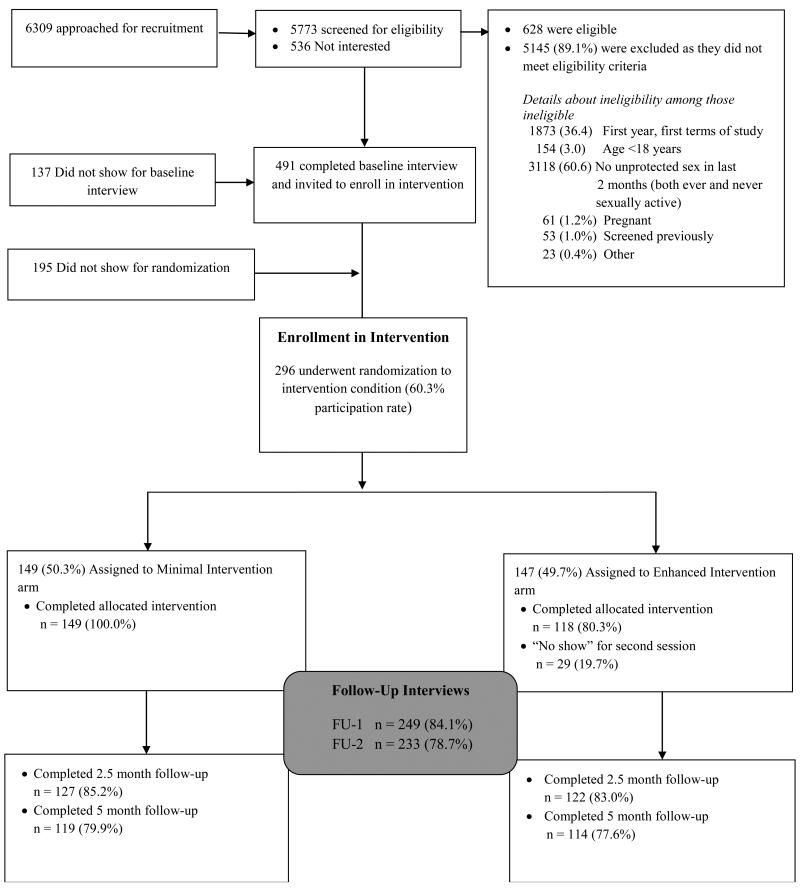
Figure 1 shows the participant flow from recruitment to five months post-intervention. Of the 5,773 women screened, 628(11.0%) were eligible for study participation, 491 (78.2% of those eligible) completed the baseline interview, and 296 (60.3% of those completing baseline) were randomized. Of the randomized participants, 147 were assigned to the EI and 149 to the MI. All women who were randomized to the MIattended the intervention since the intervention comprised one session on the same day as randomization. Of the 147 women assigned to the EI, all attended the first session and 118 (80.3%) attended both sessions.Overall, 84.1% of all participants completed the 2.5-month post-intervention interview (83.0% of EI and 85.2% of MI; p=0.60) and 78.7% completed the 5-month post-intervention interview (77.6% of EI and 79.9% of MI; p=0.63).
Figure 1.
Overview of study enrollment and flow
Participants were on average 20.1 years of age (SD=1.9). All participants were Black African. Most(95.3%) currently had a main partner, who on average was 3.5 years older than the participant (SD=2.8). Many (44.3%) believed their partner to be at risk for HIV/STI, with 8.0% reporting that their partner had an STI in the prior year. Participants had on average 2.6 partners (SD=2.3) in their lifetimes(Table 1). At baseline, only 12 women (4.7%) reported they had ever used a FC, whereas most had partners who had used male condoms (97.6%). There were no significant differences by intervention condition in any of the demographic, attitudinal, HIV/STI, pregnancy, contraception, sexual behavior, orcondom use variables.
Table 1.
Baseline characteristics of sample by minimal and enhanced intervention conditions, female university students in South Africa
| Variables | Minimal Intervention (N = 149) | Enhanced Intervention(N = 147) | Total (N = 296) | P a |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Main language Zulu, n (%) | 120 (80.5%) | 125 (85.0%) | 245 (82.8%) | 0.36 |
| HIV/STIs | ||||
| Ever diagnosed with STI, n (%) | 29 (19.9%) | 26 (17.8%) | 55 (18.8%) | 0.77 |
| Perceived chances of getting infected with HIVin next 6 months (range=1-4), mean(SD) | 2.18 (0.86) | 2.00 (0.89) | 2.09 (0.88) | 0.09 |
| Condom Use for Contraception | ||||
| Ever used male condom, n (%) | 145 (99.3%) | 136 (95.8%) | 281 (97.6%) | 0.06 |
| Ever used female condom, n (%) | 4 (2.7%) | 8 (5.6%) | 12 (4.2%) | 0.25 |
| Ever used either male or female condom, n (%) | 145 (99.3%) | 137 (96.5%) | 282 (97.9%) | 0.12 |
| Male or female condom use past 2 months, n (%) | 105 (71.9%) | 96 (68.1%) | 201 (70%) | 0.52 |
| Male or female condom use last sex, n (%) | 84 (56.8%) | 75 (51.0%) | 159 (53.9%) | 0.35 |
| Sexual Partners | ||||
| Number of sex partners lifetime (range = 1-20), mean (SD) | 2.78 (2.29) | 2.50 (2.16) | 2.4 (2.3) | 0.29 |
| Has main male sex partner, n (%) | 142 (95.3%) | 140 (95.2%) | 282 (95.3%) | 1.00 |
| Most recent main partner characteristics | ||||
| Age difference between participant and main partner, mean (SD) | 3.77 (3.12) | 3.26 (2.36) | 3.52 (2.78) | 0.13 |
| Perceive main partner to be at risk for HIV and/or STI, n (%) | 64 (45.4%) | 60 (43.2%) | 124 (44.3%) | 0.72 |
| Partner has had STI in last year, n (%) | 10 (8.5%) | 9 (7.6%) | 19 (8.0%) | 0.82 |
t-tests and Chi-squared analyses were used to assess continuous and categorical variables, respectively; for two-by-two tables we report the Fisher exact two-sided p-value, and otherwise report Pearson p-values
Trial results
Both groups reported significant reductions in the number of vaginal intercourse occasions unprotected by either male or female condoms from baseline to the 2.5- and 5-month follow-up (Table 2). Specifically, at the 2.5-months follow-up, the number of unprotected vaginal sex acts was 0.53 times lower in the MI (p=0.02) group and 0.41 times lower in the EI group (p<0.0001)relative to baseline; at the 5-month follow-up, it was 0.39 times lower in the MI group (p<0.0001) and 0.40 times lower in the EI (p<0.0001) group. (Table 2)The change in number of unprotected vaginal sex acts over time did not differsignificantly by intervention group (interaction p-value=0.44 at 2.5months and 0.97 at 5months). (Data not shown)
Table 2.
Sexual behavior variables: Regression models comparing baseline to each follow-up (2.5- & 5-months) within each intervention group (MI and EI)
| Minimal Intervention (1 Session) | Enhanced Intervention (2-Session) | ||||||
|---|---|---|---|---|---|---|---|
| Number of vaginal intercourse occasions unprotected by either male or female condomsa | |||||||
| Mean | Rate Ratio | p-value | Mean | Rate Ratio | p-value | ||
| Baseline | 12.68 | - | - | Baseline | 7.10 | - | - |
| FU1 | 6.75 | 0.53 | 0.02 | FU1 | 2.29 | 0.41 | <.0001 |
| FU2 | 5.02 | 0.39 | <.0001 | FU2 | 2.24 | 0.40 | <.0001 |
| Number of female condoms useda | |||||||
| Baseline | 0.02 | - | - | Baseline | 0.15 | - | - |
| FU1 | 2.43 | 135.64 | <.0001 | FU1 | 2.40 | 16.78 | <.001 |
| FU2 | 1.04 | 57.97 | <.0001 | FU2 | 1.78 | 12.68 | <.01 |
| Percentage of vaginal intercourse occasions protected by female condomb | |||||||
|---|---|---|---|---|---|---|---|
| Mean | Mean difference | p-value | Mean | Mean difference | p-value | ||
| Baseline | 0.00 | - | Baseline | 0.01 | - | - | |
| FU1 | 0.15 | 0.15 | <.0001 | FU1 | 0.18 | 0.17 | <.0001 |
| FU2 | 0.08 | 0.08 | <.0001 | FU2 | 0.12 | 0.11 | <.0001 |
| Percentage of vaginal intercourse occasions protected by female or male condomb | |||||||
| Baseline | 0.50 | - | - | Baseline | 0.48 | - | - |
| FU1 | 0.79 | .29 | <.0001 | FU1 | 0.85 | .37 | <.0001 |
| FU2 | 0.75 | .25 | <.0001 | FU2 | 0.82 | .34 | <.0001 |
| If used a female or male condom at the last sex occasionc | |||||||
|---|---|---|---|---|---|---|---|
| % Yes | Odds Ratio | p-value | % Yes | Odds Ratio | p-value | ||
| Baseline | 56.80 | - | - | Baseline | 51.00 | - | - |
| FU1 | 86.60 | 4.95 | <.0001 | FU1 | 82.00 | 4.35 | <.0001 |
| FU2 | 80.20 | 3.10 | <.0001 | FU2 | 86.00 | 5.93 | <.0001 |
| Total number of vaginal intercourse occasionsa | |||||||
|---|---|---|---|---|---|---|---|
| Mean | Rate Ratio | p-value | Mean | Rate Ratio | p-value | ||
| Baseline | 23.75 | - | - | Baseline | 18.20 | - | - |
| FU1 | 21.45 | 0.90 | 0.35 | FU1 | 22.19 | 1.22 | 0.11 |
| FU2 | 18.34 | 0.77 | 0.02 | FU2 | 18.78 | 1.03 | 0.83 |
| If hormonal contraceptive use at the last sex occasionc | |||||||
|---|---|---|---|---|---|---|---|
| % Yes | Odds Ratio | p-value | %Yes | Odds Ratio | p-value | ||
| Baseline | 12.50 | - | - | Baseline | 9.90 | - | - |
| FU1 | 13.40 | 1.08 | 0.75 | FU1 | 12.30 | 1.27 | 0.42 |
| FU2 | 9.40 | 0.73 | 0.29 | FU2 | 12.20 | 1.26 | 0.55 |
Poisson regression model
Linear regression model
Logistic regression model
The same pattern of results was found for secondary sexual behavior outcomes. Number of FCs used increased 135.6 times between baseline and 2.5-month follow-up among the MI group (p<0.0001) and 16.8 times in the EI group (p<0.001), although this group difference was not statistically significant (p-value for interaction between time and intervention=0.06), nor were there significant differences between groups on any of the other sexual behavior variables. The number of FCs used between baseline and 5-month follow-up increased 58.0 times in the MI group (p<0.001) and 12.7 times in the EI (p<0.01); (p=0.18 for difference in the change over time by group). Additionally, the percent of vaginal intercourse occasions protected by a FC increased in the MI group by 0.15from baseline to 2.5-months (p<0.0001) and by 0.08 from baseline to 5-month follow-up (p<0.0001)(p=0.46 for difference in the change over time by group); and in the EI group by 0.17 from baseline to 2.5months (p<0.0001) and 0.11 from baseline to 5 months (p<0.0001)(p=0.18 for difference in the change over time by group).A similar patternemerged for the percent of vaginal intercourse occasions protected by either a female or a male condom. Compared to baseline, the odds of condom use (male or female) at last sex act was5.0 times higher at 2.5-month follow-up (p<0.0001) and 3.1 times higher 5-month follow (p<0.0001) in the MI group and 4.4 times higher at 2.5months (p<0.0001)(p=0.74 for difference in the change over time by group); and 5.9 times higher at 5months (p<0.0001) in the EI group (p=0.12 for difference in the change over time by group). Use of hormonal contraceptives did not change significantly over time in either group; number of vaginal sex acts decreased significantly between baseline and 5-month follow-up in the MI but not in the EI group (Table 2). However, change in number of vaginal sex acts over time by group did not account for the finding of no differences in outcomes between the two intervention conditions (data not shown).
Changes in Other Secondary Outcomes over Time
As shown in Table 3,participants in both groups had a lower perception of their risk for unintended pregnancy and for HIV infection atfollow-up. The decrease in unintended pregnancy risk perception at 5-months follow-up was significantly greater in the MI group (decrease of 0.42, p<0.001) compared to the EI group (decrease of 0.16, p=0.11) (interaction p=0.04).
Table 3.
Risk Perception: Regression models comparing baseline to each follow-up (2.5- & 5-months) within each intervention group (MI and EI)
| Minimal Intervention (1 Session) | Enhanced Intervention (2-Session) | ||||||
|---|---|---|---|---|---|---|---|
| Perceived risk of having an unintended pregnancy in the next 6 monthsb | |||||||
| Mean | Mean difference | p-value | Mean | Mean difference | p-value | ||
| Baseline | 2.23 | - | - | Baseline | 2.02 | - | - |
| FU1 | 1.75 | −0.48 | <.0001 | FU1 | 1.69 | −0.33 | <.0001 |
| FU2 | 1.81 | −0.42 | <.0001 | FU2 | 1.86 | −0.16 | 0.11 * |
| Perceived risk of getting infected with HIV in the next 6 monthsb | |||||||
| Baseline | 2.18 | - | - | Baseline | 2.00 | - | - |
| FU1 | 1.90 | −0.28 | 0.01 | FU1 | 1.64 | −0.36 | <.0001 |
| FU2 | 1.97 | −0.21 | 0.01 | FU2 | 1.75 | −0.25 | <.01 |
Significant difference in change over time between the two interventions
Linear regression model
Furthermore, participants in both groups had more positive feelings about male and female condom use and believed that their partners had more positive attitudes as well at each follow-up interview compared to baseline (Table 4). Both groups reported more positive peer norms for condom use at each follow-up, with those in the EI group reporting significantly greater increases relative to the MI at the 2.5 month follow-up (interaction p=0.04). As shown in Table 5, participants in both groups reported greater intention to use FCs in the future and increased self-efficacy for condom useat follow-up, although they did not differ with respect to each other.
Table 4.
Condom use attitudes and norms: Regression models comparing baseline to each follow-up (2.5- & 5-months) within each intervention group (MI and EI)
| Minimal Intervention (1 Session) | Enhanced Intervention (2-Session) | ||||||
|---|---|---|---|---|---|---|---|
| Personal attitude about using the male condomb | |||||||
| Mean | Mean Difference | p-value | Mean | Mean Difference | p-value | ||
| Baseline | 4.22 | - | - | Baseline | 4.35 | - | - |
| FU1 | 4.43 | 0.26 | 0.01 | FU1 | 4.48 | 0.13 | 0.10 |
| FU2 | 4.45 | 0.23 | 0.01 | FU2 | 4.49 | 0.14 | 0.09 |
| Perceived partner attitude toward male condom useb | |||||||
| Baseline | 3.53 | - | - | Baseline | 3.56 | - | - |
| FU1 | 3.93 | 0.40 | <.01 | FU1 | 3.98 | 0.41 | <.001 |
| FU2 | 3.87 | 0.34 | 0.01 | FU2 | 3.79 | 0.23 | 0.10 |
| Personal attitude toward female condom useb | |||||||
| Baseline | 2.97 | - | - | Baseline | 3.11 | - | - |
| FU1 | 3.70 | 0.73 | <.0001 | FU1 | 3.96 | 0.85 | <.0001 |
| FU2 | 3.39 | 0.43 | <.001 | FU2 | 3.56 | 0.45 | <.001 |
| Perceived partner attitude toward female condom useb | |||||||
| Baseline | 2.67 | - | - | Baseline | 2.63 | - | - |
| FU1 | 2.92 | 0.25 | 0.05 | FU1 | 2.89 | 0.27 | 0.03 |
| FU2 | 2.88 | 0.21 | 0.10 | FU2 | 2.94 | 0.31 | 0.02 |
| Peer norms for condom useb | |||||||
| Baseline | 2.76 | - | - | Baseline | 2.72 | - | - |
| FU1 | 2.94 | 0.18 | <.0001 | FU1 | 3.03 | 0.31 | <.0001 * |
| FU2 | 2.93 | 0.17 | <.001 | FU2 | 3.01 | 0.28 | <.0001 * |
Significant difference in change over time between the two interventions
Linear regression model
Table 5.
Condom use intention and self-efficacy: Regression models comparing baseline to each follow-up (2.5- & 5-months) within each intervention group (MI and EI)
| Minimal Intervention (1 Session) | Enhanced Intervention (2-Session) | ||||||
|---|---|---|---|---|---|---|---|
| Intention to use female condomsc | |||||||
| Mean | Mean Difference | p-value | Mean | Mean Difference | p-value | ||
| Baseline | 2.28 | - | - | Baseline | 2.23 | - | - |
| FU1 | 2.77 | 0.49 | <.0001 | FU1 | 2.77 | 0.54 | <.0001 |
| FU2 | 2.47 | 0.18 | 0.10 | FU2 | 2.71 | 0.48 | <.0001 |
| Condom use self-efficacyb | |||||||
| Baseline | 3.16 | - | - | Baseline | 3.21 | - | - |
| FU1 | 3.56 | 0.39 | <.0001 | FU1 | 3.49 | 0.28 | <.0001 |
| FU2 | 3.46 | 0.29 | <.0001 | FU2 | 3.51 | 0.29 | <.0001 |
Linear regression model
Logistic regression model
Discussion
We conducted an RCT comparing two HIV prevention interventions designed to promote FC use among women attending a South African university using a theory-driven model. Our main and secondary hypotheses were not supported in that women in the EI did not do better than women in the MI. Our findings suggest that both the EI andMIresulted in adecrease in sexual risk behavior among women at 2.5and 5months relative to baseline.Unprotected sex due to using a male or female condom was reduced, and FC-protected sex and number of FCs used increased over this time period.
The lack of difference between the minimal and enhanced interventions could possibly be because messages delivered in the MI were more easily retained by participants in the shorter, more focused MI, thus counter balancing the effect of the enhancements in the EI.The need to attend only one session also may have been more feasible for the students to accommodate within their busy academic timetable.Assessment itself has been shown to affect sexual risk-reduction (e.g.,[45]), and the cumulative effect of MI plus assessment may have been equivalent to EI.Participants in both interventions may have reduced unprotected sex because of exposure to the intensive condom promotion that has taken place in South Africa and the greater availability of FCs in public sector clinics and in non-governmental organizations. FC distribution may have played a critical role in observed increased safer sex as well, since participants in both arms left the interventions with 10 FCs in hand. An increase in FC use in both conditions also could occur independent of the intervention if there were co-temporal increases in FC use in the general population of students on campus. However, evidence from two campus surveys we conducted at this higher education institution in 2008, at the time of the intervention, and two years later in 2010, does not support this idea.Among women who reported ever having had vaginal sex, we found a decrease from 4.7% of women who ever used the FC (21/333) in 2008 to 2.7% (11/324) who reported having used it in 2010 [46, 47].
Facilitators in the MI as well as EIwere encouraged to be champions of „their’ intervention, and thus the passionate delivery of the MI may have had a role in the equivalence of the two interventions.Perhaps a key to success in both groups lies in having female condoms on hand as a way to introduce discussion of safer sex with partners with whom they were clearly, at baseline, engaging in risky sex.
It is promising that both interventions showed significant reductions in unprotected sex and increases in the proportion of FC-protected sex at 5 months post-intervention,as well as more immediate effects, as a number of studies have found shorter-term (3 months) intervention effects [28-30, 36]. Nevertheless, further study is needed to investigate whether the intervention actually contributed to such improvement over time, given that the study did not include an assessment-only group in this comparison.
With competing non-health promotion activities on campus, that a brief one-session intervention delivered over a 60-90 minute period had the same effect as a two-session, total offour to five-hour intervention in decreasing sexual risk behavior is noteworthy because of feasibility. The shorter, less labor-intensive MIholds promise in resource-constrained settings, potentially having greater likelihood of being implemented in a non-research context.
Some limitations are noted.First, since intervention effects only were assessed over a five-month period, we are unable to determine whether they were maintained over a longer period and, therefore, we cannot rule out the possibility of differential longer-term effects between groups. Another limitation is that the study did not collect biomarkers of unprotected sex; rather, sexual behavior was self-reported via face-to-face interviews and therefore subject to social desirabilityreporting bias. This bias would likely be non-differential by intervention and would therefore reduce our ability to find a difference by intervention arm. We also did not have a non-intervention assessment-only group and therefore cannot rule out the possibility that neither intervention accounted for the observed results.
This research with university students in South Africasupports the value of a brief FC intervention. Many South African universities have health service delivery systems in place that can be mobilized to provide HIV prevention and support services, making them ideal venues for promoting female and male condoms. Even with the above noted limitations, ourfindings may also have applicability for populations other than female university students. Introduction of a single group-based FC promotion intervention holds promise in a number of service delivery points in resource-constrained settings, and could easily be delivered in clinic waiting-rooms as well as in various community venues.
Interventions that promote female and male condom use are clearly neededinSouth Africa. The South African National HIV Survey found that overall condom use at last sex at the national leveldecreased from 45.1% in 2008 to 36.2% in 2012, with a higher percentage of males (38.6%) reporting that they had used a condom thanfemales (33.6%); and among those who reported using condoms, use was inconsistent (27%) [20].This decline in condom use has been accompanied by an increase in multiple sexual partnerships among men, thus highlighting omnipresent structurally-based gender inequalities that contribute to women's increased risk of HIV infection. Many women lack control over self-protection from HIV and other STIs because of gender inequities. Male partner resistance to prevention methods that interfere with their sexual pleasures makes itdifficult for women to negotiate male condom use. Thus, promotion of methods that can be negotiated by women, such as the FC, to protect themselves from HIV infection needs to be accelerated [48, 49], highlighting the need for interventions targeted to both women and men.
Conclusion
The FC is a highly under-utilized, effective HIV prevention method that has the potential to reduceHIV incidence among women and their partners as shown by a cost-effectiveness analysis in Brazil and South Africa [50].Findings from a comprehensive national evaluation of South Africa's FC program currently underway[51] will elucidate key system, supply, partner, and user challenges to FC use, whereas the revitalization of South Africa's once thriving FC social marketing program will provide an opportunity for documenting FC demand through this distribution strategy and comparing it to public-sector demand. With greater global investment in both FC design to increase method acceptability and programming to increase product demand as well as implementation of interventions that can be easily replicated and do not drain resources, we may be able to maximize uptake and use of FCs.
Acknowledgements
This research was supported by a grant from NICHD (NICHD; R01-HD046351; Joanne E. Mantell, M.S., MS.PH, Ph.D., Principal Investigator; Jennifer A. Smit, Ph.D., South Africa Site Principal Investigator). The HIV Center for Clinical and Behavioral Studies at the New York State Psychiatric Institute and Columbia University is supported by a center grant from the National Institute of Mental Health (P30-MH43520; Principal Investigator: Robert H. Remien, Ph.D.). We are grateful to the students who participated in this study and the valuable contributions of the study's Community Advisory Board. We also acknowledge the contributions of the officials at the higher education institution study site, who supported the study. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development, the HIV Center for Clinical and Behavioral Studies at the New York State Psychiatric Institute and Columbia University, MatCH Research (Maternal and Adolescent Child Health Research), and the University of the Witwatersrand, Faculty of Health Sciences, Department of Obstetrics &Gynaecology.
Footnotes
Author contributions. JEM, JAS, MB, TME, SH, ZAS designed and planned the study. JAS, ZM, and CN led study implementation and data collection. C-SL conducted the statistical analysis and JEM, JAS, TME, SH, MB, EAK were involved in interpretation of the data. JEM with input from TME, JAS, MB, SH, C-SL, EAK wrote the first draft of the manuscript. All authors contributed and reviewed all drafts of the manuscript.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Reproductive Health Supplies Coalition Caucus on new and underused reproductive health technologies. Product brief: female condom. Reproductive Health Supplies Coalition. 2012 [Google Scholar]
- 2.Ahmed K, Deperthes B, Frederick B, Ehlers S, Kapp N, Paladines C, et al. Contraceptive commodities for women's health working paper. UN Commission on Life-Saving Commodities for Women's and Children's Health; New York, NY: Mar, 2012. UN Commission on Life-Saving Commodities for Women and Children. [Google Scholar]
- 3.World Health Organization . Global HIV/AIDS response: Epidemic update and health sector progress towards universal access: Progress report 2011. World Health Organization; Geneva: 2011. [Google Scholar]
- 4.Fontanet AL, Saba J, Chandelying V, Sakondhavat C, Bhiraleus P, Rugpao S, et al. Protection against sexually transmitted diseases by granting sex workers in Thailand the choice of using the male or female condom: Results from a randomized controlled trial. AIDS. 1998;12:1851–1859. doi: 10.1097/00002030-199814000-00017. [DOI] [PubMed] [Google Scholar]
- 5.French PP, Latka M, Gollub EL, Rogers C, Hoover DR, Stein ZA. Use-effectiveness of the female versus male condom in preventing sexually transmitted disease in women. Sex Transm Dis. 2003;30:433–439. doi: 10.1097/00007435-200305000-00010. [DOI] [PubMed] [Google Scholar]
- 6.Hoke T, Feldblum P, Van Damme K, Nasution M, Grey T, Wong E, et al. Temporal trends in sexually transmitted infection prevalence and condom use following introduction of the female condom to Madagascar sex workers. Int J STD AIDS. 2007;18:461–466. doi: 10.1258/095646207781147175. [DOI] [PubMed] [Google Scholar]
- 7.Artz L, Maculuso MM, Brill I, Kelaghan J, Austin H, Fleenor M, et al. Effectiveness of an intervention promoting the female condom to patients at sexually transmitted disease clinics. American Journal of Public Health. 2000;90:237–244. doi: 10.2105/ajph.90.2.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vijayakumar G, Mabude Z, Smit J, Beksinska M, Lurie M. A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence. Int J STD AIDS. 2006;17:652–659. doi: 10.1258/095646206780071036. [DOI] [PubMed] [Google Scholar]
- 9.Gollub EL. The female condom: Tool for women's empowerment. American Journal of Public Health. 2000;90:1377–1381. doi: 10.2105/ajph.90.9.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peters A, Jansen W, Van Driel F. The female condom: The international denial of a strong potential. Reprod Health Matters. 2010;18:119–128. doi: 10.1016/S0968-8080(10)35499-1. [DOI] [PubMed] [Google Scholar]
- 11.Hoffman S, Mantell J, Exner T, Stein Z. The future of the female condom. Perspectives on Sexual and Reproductive Health. 2004;36:120–126. doi: 10.1363/psrh.36.120.04. [DOI] [PubMed] [Google Scholar]
- 12.United Nations Population Fund . HIV prevention gains momentum. UNFPA; New York, NY: 2011. 978-0-89714-933-4. [Google Scholar]
- 13.Husken S, Terlikowski J. Join the global movement for female condoms. Impatient Optimists. In http://www.impatientoptimists.org/Posts/2013/09/Join-the-Global-Movement-for-Female-Condoms 2013 September 19.
- 14.UNAIDS . Final Report. UNAIDS; Republic of South Africa. New York, NY: 2010. Country Progress Report on the Declaration of Commitment on HIV/AIDS. [Google Scholar]
- 15.Beksinska M, Smit J, Joanis C, Potter W. New female condoms in the pipeline. Reprod Health Matters. 2013;20:188–196. doi: 10.1016/S0968-8080(12)40659-0. [DOI] [PubMed] [Google Scholar]
- 16.Beksinska M, Smit J, Joanis C, Usher-Patel M, Potter W. Female condom technology: New products and regulatory issues. Contraception. 2011;83:316–321. doi: 10.1016/j.contraception.2010.07.022. [DOI] [PubMed] [Google Scholar]
- 17.Beksinska M, Smit JA, Mantell JE. Progress and challenges to male and female condom use in South Africa. Sex Health. 2012;9:51–58. doi: 10.1071/SH11011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peterson K, Herman L, Marseille E, Kahn JG. Smarter programming of the female condom: Increasing its impact on HIV prevention in the developing world. 2008 In www.fsg-impact.org/app/content/ideas/item/Female_Condom_Impact.html: FSG Social Impact Advisors.
- 19.Center for Health and Gender Equity (CHANGE) Female condoms and U.S. foreign assistance: An unfinished imperative for women's health. Center for Gender Equity and Health; Washington, DC: 2011. [Google Scholar]
- 20.Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, et al. South African National HIV Prevalence, Incidence and Behaviour Survey. HSRC Press; Cape Town, South Africa: 2014. [DOI] [PubMed] [Google Scholar]
- 21.Pettifor A, Rees H, Steffenson A, Hlongwa-Madikizela L, MacPhail C, Vermaak K, et al. HIV and sexual behaviour among young South Africans: National survey of 15-24 year olds. Reproductive Health Research Unit, University of the Witwatersrand; Johannesburg: 2004. [Google Scholar]
- 22.National Department of Health . National contraception and fertility planning policy and service delivery guidelines 2012. Department of Health; Pretoria, South Africa: 2013. [Google Scholar]
- 23.Department of Health. Republic of South Africa. National contraception and fertility planning policy and service delivery guidelines. Pretoria: Department of Health. 2012 [Google Scholar]
- 24.MatCH (Maternal Adolescent and Child Health) Developing a strategy for female condom parallel programming: Proceedings of an expert meeting; Durban, South Africa. 23-24 November 2011; MatCH; 2011. [Google Scholar]
- 25.Guerra FM, Simbayi LC. Prevalence of knowledge and use of the female condom in South Africa. AIDS and Behavior. 2014;18:146–158. doi: 10.1007/s10461-013-0580-3. [DOI] [PubMed] [Google Scholar]
- 26.Higher Education HIV/AIDS Programme (HEAIDS) HIV prevalence and related factors: Higher education sector study, South Africa, 2008-2009. Higher Education South Africa; Pretoria: 2010. [Google Scholar]
- 27.Ray S, van de Wijgert J, Mason P, Ndowa F, Maposhere C. Constraints faced by sex wokers in use of female and male condoms for safer sex in urban Zimbabwe. J Urban Health. 2001;78:581–592. doi: 10.1093/jurban/78.4.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Devanter N, Gonzales V, Merzel C, Parikh NS, Celantano D, Greenberg J. Effect of an STD/HIV behavioral intervention on women's use of the female condom. Am J Public Health. 2002;92:109–115. doi: 10.2105/ajph.92.1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Witte SS, El-Bassel N, Gilbert L, Wu E, Chang M, Hill J. Promoting female condom use to heterosexual couples: Findings from a randomized clinical trial. Perspect Sex Reprod Health. 2006;38:148–154. doi: 10.1363/psrh.38.148.06. [DOI] [PubMed] [Google Scholar]
- 30.Kalichman SC, Williams E, Nachimson D. Brief behavioural skills building intervention for female controlled methods of STD-HIV prevention: Outcomes of a randomized clinical field trial. Int J STD AIDS. 1999;10:174–181. doi: 10.1258/0956462991913844. [DOI] [PubMed] [Google Scholar]
- 31.Feldblum PJ, Kuyoh MA, Bwayo JJ, Omari M, Wong EL, Tweedy KG, et al. Female condom introduction and sexually transmitted infection prevalence: Results of a community intervention trial in Kenya. AIDS. 2001;15:1037–1044. doi: 10.1097/00002030-200105250-00012. [DOI] [PubMed] [Google Scholar]
- 32.Choi KH, Hoff C, Gregorich SE, Grinstead O, Gomez C, Hussey W. The efficacy of female condom skills training in HIV risk reduction among women: A randomized controlled trial. Am J Pub Health. 2008;98:1841–1848. doi: 10.2105/AJPH.2007.113050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Exner TM, Tesoriero JM, Battles HB, Hoffman S, Mantell JE, Correale J, et al. A randomized controlled trial to evaluate a structural intervention to promote the female condom in New York state. AIDS Behav. 2012;16:1121–1132. doi: 10.1007/s10461-012-0176-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Witte SS, El-Bassel N, Gilbert L, Wu E, Chang M, Hill J. Promoting female condom use to heterosexual couples: Findings from a randomized clinical trial. Perspectives on Sexual and Reproductive Health. 2006;38:148–154. doi: 10.1363/psrh.38.148.06. [DOI] [PubMed] [Google Scholar]
- 35.Feldblum PJ, Bwayo JJ, Kuyoh MA, Welsh MJ, Ryan KA, Chen-Mok M. The female condom and STDs: Design of a community intervention trial. Ann Epidemiol. 2000;10:339–346. doi: 10.1016/s1047-2797(00)00046-6. [DOI] [PubMed] [Google Scholar]
- 36.Malow R, Ziskind D, Jones DL. Use of female controlled microbicidal products for HIV risk reduction. AIDS Care. 2000;12:581–588. doi: 10.1080/095401200750003761. [DOI] [PubMed] [Google Scholar]
- 37.Hoffman S, Exner TM, Leu CS, Ehrhardt AA, Stein ZA. Female condom use in a gender-specific family planning clinic trial. Am J Public Health. 2003;93:1897–1903. doi: 10.2105/ajph.93.11.1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gollub EL, Cyrus-Cameron E, Armstrong K, Boney T, Chhatre S. Basic body knowledge in street-recruited, active drug-using women enrolled in a “body empowerment” intervention trial. AIDS Care. 2013;25:732–737. doi: 10.1080/09540121.2012.748167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bandura A. A social cognitve approach to the exercise of control over AIDS infection. Sage; Beverly Hills, CA: 1992. [Google Scholar]
- 40.Bandura A. Social foundations of thought and action: A social cognitive theory. Prentice-Hall; Englewood Cliffs, NJ: 1986. [Google Scholar]
- 41.Ehrhardt AA, Exner TM, Hoffman S, Silberman I, Leu CS, Miller S, et al. A gender-specific HIV/STD risk reduction intervention for women in a health care setting: Short- and long-term results of a randomized clinical trial. AIDS Care. 2002;14:147–161. doi: 10.1080/09540120220104677. [DOI] [PubMed] [Google Scholar]
- 42.Exner TM, Meyer-Bahlburg HFL, Yingling SL, Hoffman S, Ortiz-Torres B. Psychosexual and psychosocial interviews for Project FIO (The Future is Ours) Columbia University, Department of Psychiatry; New York, NY: 1994. Unpublished. [Google Scholar]
- 43.Harrison A, O'Sullivan LF, Hoffman S, Dolezal C, Morrell R. Gender role and relationship norms among young adults in South Africa: Measuring the context of masculinity and HIV risk. J Urban Health. 2006;83:709–722. doi: 10.1007/s11524-006-9077-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rubin DB. Inference and missing data. Biometrics. 1976;63:581–592. [Google Scholar]
- 45.Kamb ML, Fishbein M, Douglas JM, Jr., Rhodes F, Rogers J, Bolan G, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: A randomized controlled trial. Project RESPECT Study Group. JAMA. 1998;280:1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- 46.Mantell JE, Smit JA. Female condom use among South African students. National Institute of Child Health and Human Development. 2004-2010 R01-HD046351 unpublished data. [Google Scholar]
- 47.Mantell JE, Smit JA. HIV Prevention Efficacy Beliefs about Male Circumcision in South Africa American Foundation for AIDS Research (amfAR) 2008-2010 107200-44-RGRL unpublished data. [Google Scholar]
- 48.Mantell JE, Dworkin S, Exner TM, Hoffman S, Smit JA, Susser I. The promises and limitations of female-initiated methods of HIV/STI protection. Social Science & Medicine. 2006;63:1998–2009. doi: 10.1016/j.socscimed.2006.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mantell JE, Stein ZA, Susser I. Women in the time of AIDS: Barriers, bargains, and benefits. AIDS Educ Prev. 2008;20:91–106. doi: 10.1521/aeap.2008.20.2.91. [DOI] [PubMed] [Google Scholar]
- 50.Dowdy DW, Sweat MD, Holtgrave DR. Country-wide distribution of the nitrile female condom (FC2) in Brazil and South Africa: A cost-effectiveness analysis. AIDS. 2006;20:2091–2098. doi: 10.1097/01.aids.0000247567.57762.fb. [DOI] [PubMed] [Google Scholar]
- 51.Beksinska M, Smit JA, Mabude Z, Mantell JE. Evaluation of the national South African female condom program: Investigating factors associated with uptake and sustained Use. USAIDPEPFAR Cooperative Agreement AID-OAA-A-13-00069 [Google Scholar]