Abstract
Objective
To determine whether the obese population is more likely to be vitamin D deficient compared to healthy and overweight individuals.
Patients and methods
A retrospective chart review was performed for patients seen in two ambulatory clinics in South Florida over a 1-year period (n=402). Patients’ vitamin D levels drawn during annual wellness visits were analyzed. Subjects were categorized based on body mass index (BMI) as normal (BMI <24.9), overweight (BMI 25.0–29.9), and obese (BMI >30.0). Their 25-OH vitamin D status was defined as normal (>30 ng/mL), insufficient (20.0–29.9 ng/mL), and deficient (<20 ng/mL). The study included both men and women of black, white, Hispanic, and Asian races. Other variables in the study included age, history of hypertension, and diabetes. Patients with conditions leading to vitamin D malabsorption (chronic pancreatitis, celiac disease, Crohn's disease, cystic fibrosis, ileocecal resection) were excluded. Patients with prior vitamin D supplementation were also excluded.
Results
The results of the study indicated a significant association of vitamin D deficiency and obesity (p<0.05). Patients who were obese had a relative risk of 3.36 (95% CI: 1.50–7.54) for vitamin D deficiency compared to subjects with normal BMI. The study also showed a significant association between vitamin D levels and obesity when controlling for age, race, and presence of hypertension (p <0.05), with Asians and blacks more likely to be vitamin D deficient.
Conclusion
These results demonstrated that obesity was a risk factor for vitamin D deficiency in all races, especially the Asian and black populations. This suggests that physicians should screen for vitamin D deficiency in the obese populations, especially among Asian and black races.
Keywords: 25-OH vitamin D, obesity, hypertension, diabetes
Previous studies have indicated that vitamin D deficiency may be associated with obesity (1, 2). The exact mechanism by which obese individuals are vitamin D deficient has not been precisely determined. Proposed reasons include decreased bioavailability of vitamin D secondary to increased adiposity in the obese populations (1), and increased oxidative reactions occurring in adipose tissue leading to break down of vitamin D (3).
The purpose of this study was to investigate which population of individuals may be more prone to vitamin D deficiency, thereby aiding clinicians in being diligent in appropriately ordering vitamin D levels. The research will investigate if patients with higher body mass index (BMI) are more prone to lower 25-OH vitamin D levels.
Methods
Patients were categorized based on their BMI: <24.9, 25.0–29.9, and >30 representing normal, overweight, and obese individuals respectively. Corresponding 25-OH vitamin D levels were designated as normal (>30 ng/mL), insufficient (>20 to 29.9 ng/mL), and deficient (<20 ng/mL). 25-OH vitamin D levels were obtained from previous lab studies, preferably before vitamin D supplementation. Specific groups of patients that were excluded from the study included those with diseases that have been known to lead to malabsorption of vitamin D: chronic pancreatitis, Crohn's disease, cystic fibrosis, primary biliary cirrhosis, celiac disease, and ileocecal resection. The study included white, black, Hispanics, and Asians.
Measurements of BMI were taken during the initial patient visits by the medical assistant staff at the respective clinics. Patients were not specifically reweighed by the research staff for purposes of this study. Respective BMIs were calculated manually for each individual based on measurements of height and weight recorded on the patient medical record. These values were then compared to BMI values written in patient files in order to ensure accuracy of measurements.
Prevalence of vitamin D deficiency (deficient, insufficient, normal) was assessed in three different (BMI groups: 1) normal weight 18.5–24.9 BMI, 2) overweight 25–29.9 BMI, and 3) obese >30 BMI. The variables sex (male or female), race (Asian, black, Hispanic, and white), hypertensive (yes, no), diabetic (yes, no) and age were used in the modeling process. A four-step modeling procedure was used. First, descriptive statistics were calculated for all variables. Second, univariable analysis was used to test the association between study variables and the outcome vitamin D status. Third, a multinomial regression model using robust standard errors was used to evaluate the association between the study variables found significant in step two and vitamin D status. The fourth step was to examine the final model using Pearson and deviance goodness-of-fit tests. STATA (version 13.1, 2014, College Station, TX) and R (version 3.1.1, 2014, http://www.R-project.org/) were used for all data analysis. A p value was significant if equal or less than 0.05. All tests were two-tailed.
Data was gatherd from 402 individuals. Eight people were excluded because their BMI was considered underweight (<18.5 BMI). Therefore, 394 subjects were used in the statistical modeling. The average age was 57 (±14.9), 38% of subjects possessed normal vitamin D levels, 40% were white, 69% were female, and 24% had normal BMI (Table 1). Due to insufficent observations the underweight group was removed for the statistical modeling.
Table 1.
Descriptive statistics
| Freq. | Percent | Cum. (%) | |
|---|---|---|---|
| Vitamin D status | |||
| Deficient | 89 | 22.1 | 22.1 |
| Insufficient | 161 | 40.1 | 62.2 |
| Normal | 152 | 37.8 | 100.0 |
| Race | |||
| Asian | 30 | 7.5 | 7.5 |
| Black | 127 | 31.6 | 39.1 |
| Hispanic | 68 | 16.9 | 56.0 |
| White | 177 | 44.0 | 100.0 |
| Gender | |||
| Female | 276 | 68.7 | 68.7 |
| Male | 126 | 31.3 | 100.0 |
| Hypertension | |||
| No | 117 | 29.7 | 29.7 |
| Yes | 277 | 70.3 | 100.0 |
| Diabetes | |||
| No | 263 | 66.7 | 66.7 |
| Yes | 131 | 33.2 | 100.0 |
| BMI | |||
| Normal | 95 | 24.1 | 24.1 |
| Overweight | 153 | 38.8 | 62.9 |
| Obese | 146 | 37.1 | 100.0 |
Results
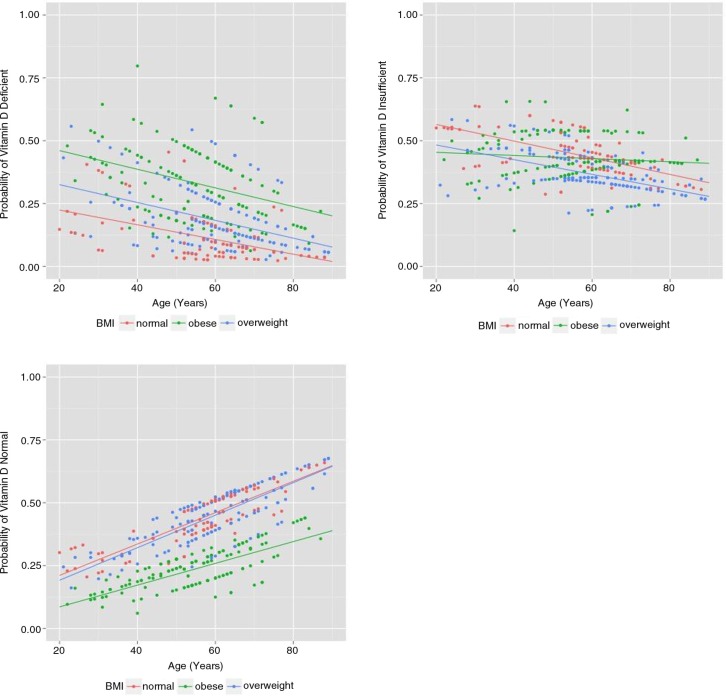
The univariable analysis revealed no significant association between a subjects'sex, diabetic status, and vitamin D levels (Table 2). The final model included the subject's age, race, hypertension, and BMI category. We found a marginal association between age and vitamin D deficiency (p<0.05). A 1-year increase in age decreases the probability of being vitamin D deficient by 22% (95% CI: 18–26%), decreases the probability of being vitamin D insufficient by 40% (95% CI: 36–46%), but increases the probability of having normal vitamin D by 37% (95% CI: 32–42%) (Fig. 1).
Table 2.
Vitamin D status by demographic variables
| Deficient | Insufficient | Normal | Chi-square | Φc | |
|---|---|---|---|---|---|
| BMI | |||||
| Normal | 11 (11.6%) | 42 (44.2%) | 42 (44.2%) | X 2=25.29 | 0.179 |
| Overweight | 48 (32.9%) | 63 (43.2%) | 35 (24.0%) | p=0.001 | |
| Obese | 28 (18.3%) | 56 (36.6%) | 69 (45.1%) | ||
| Race | |||||
| Asian | 14 (46.6%) | 8 (26.7%) | 8 (26.7%) | X 2=23.99 | 0.175 |
| Black | 38 (29.9%) | 50 (39.4%) | 39 (30.7%) | p=0.002 | |
| Hispanic | 8 (11.8%) | 35 (51.5%) | 25 (36.7%) | ||
| White | 29 (16.4%) | 68 (38.4%) | 80 (45.2%) | ||
| Gender | |||||
| Male | 32 (20.7%) | 48 (40.9%) | 46 (38.4%) | X 2=1.35 | 0.056 |
| Female | 57 (25.4%) | 113 (38.1%) | 106 (36.5%) | p=0.508 | |
| Hypertension | |||||
| No | 17 (14.6%) | 58 (49.5%) | 42 (35.9%) | X 2=17.44 | 0.137 |
| Yes | 70 (25.3%) | 103 (37.2%) | 104 (37.5%) | p=0.024 | |
| Diabetes | |||||
| No | 54 (20.5%) | 107 (40.7%) | 102 (38.8%) | X 2=1.50 | 0.061 |
| Yes | 33 (25.2%) | 54 (41.2%) | 44 (33.6%) | p=0.473 | |
Fig. 1.
Predicted probability of vitamin D deficiency by age and BMI.
Results show a significant association between vitamin D levels and BMI controlling for age, race, and hypertension (p<0.05). The relative risk of being vitamin D deficient is 1.65 (95% CI: 1.25–2.51) times greater for obese versus normal subjects, and 1.04 (95% CI: 1.03–1.86) times greater for obese than overweight subjects. Hypertension subjects are also 2.28 (95% CI: 1.07–4.86) times more likely to be vitamin D deficient than non-hypertensive subjects.
Results reveal a significant association between vitamin D levels and race (p<0.05). Specifically, Asians and blacks are more likely to be vitamin D deficient. Results are as follows (Table 3):
The relative risk of being vitamin D deficient is 2.06 times greater for Asians than Hispanics (95% CI: 1.16–3.23).
The relative risk of being vitamin D deficient is 1.71 times greater for Asians than whites (95% CI: 1.44–2.73).
The relative risk of being vitamin D deficient is 1.11 times greater for blacks than Hispanics (95% CI: 1.09–2.03).
The relative risk of being vitamin D deficient is 1.06 times greater for blacks than whites (95% CI: 1.01–1.45).
Table 3.
Predicted probabilities of vitamin D deficiency
| No hypertension | hypertension | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Race | Normal (%) | Obese (%) | OW (%) | Normal (%) | Obese (%) | OW (%) | ||
| Asian | Mean | 36.2 | 0.0 | 33.2 | 34.4 | 64.0 | 43.2 | |
| SD | 3.7 | 0.0 | 0.0 | 10.1 | 7.9 | 6.7 | ||
| Black | Mean | 13.9 | 37.5 | 19.4 | 16.1 | 42.9 | 27.4 | |
| Deficient | SD | 6.5 | 7.8 | 5.3 | 3.9 | 7.9 | 10.0 | |
| Hispanic | Mean | 3.8 | 11.5 | 7.6 | 4.8 | 21.3 | 11.0 | |
| SD | 1.3 | 3.8 | 3.3 | 1.8 | 7.4 | 5.2 | ||
| White | Mean | 5.7 | 20.2 | 8.0 | 7.5 | 30.4 | 12.8 | |
| SD | 3.8 | 5.3 | 2.1 | 3.3 | 10.9 | 6.6 | ||
| Asian | Mean | 40.3 | 0.0 | 34.0 | 30.2 | 21.6 | 23.2 | |
| SD | 1.1 | 0.0 | 0.0 | 1.1 | 3.6 | 1.0 | ||
| Black | Mean | 53.6 | 48.1 | 46.5 | 42.2 | 37.5 | 34.4 | |
| Insufficient | SD | 2.5 | 3.7 | 0.9 | 2.0 | 3.1 | 1.6 | |
| Hispanic | Mean | 58.3 | 64.7 | 54.0 | 45.6 | 52.8 | 42.7 | |
| SD | 3.0 | 1.7 | 4.0 | 4.9 | 1.6 | 3.1 | ||
| White | Mean | 46.6 | 53.6 | 41.5 | 36.5 | 40.1 | 31.5 | |
| SD | 4.5 | 1.1 | 2.3 | 3.2 | 2.4 | 2.5 | ||
| Asian | Mean | 23.5 | 0.0 | 32.8 | 35.4 | 14.4 | 33.6 | |
| SD | 2.6 | 0.0 | 0.0 | 9.1 | 4.3 | 5.7 | ||
| Black | Mean | 32.5 | 14.4 | 34.1 | 41.7 | 19.6 | 38.2 | |
| Normal | SD | 8.8 | 4.1 | 6.0 | 5.8 | 5.0 | 9.2 | |
| Hispanic | Mean | 38.0 | 23.7 | 38.4 | 49.6 | 26.0 | 46.3 | |
| SD | 4.3 | 5.4 | 7.2 | 6.7 | 6.4 | 8.0 | ||
| White | Mean | 47.6 | 26.2 | 50.5 | 55.9 | 29.4 | 55.7 | |
| SD | 8.3 | 4.5 | 4.5 | 6.3 | 9.0 | 8.6 | ||
Discussion
Both obesity and vitamin D deficiency are common problems encountered in the primary care clinic. Estimates from the Center for Disease Control indicate that approximately one-third (~34.9%) of the US adult population are obese. The national annual medical costs associated with obesity are estimated to be a staggering $147 billion in 2008. Highest rates of obesity are seen in the black population (47.8%), followed by Hispanics (42.5%), whites (32.6%), and Asians (10.8%) (4). Meanwhile, the prevalence and cost of vitamin D deficiency has significantly affected the national health care system. A National Center for Health Statistics Data Brief published in March 2011 indicated that the proportion of males over the age of 12 at risk for vitamin D deficiency increased from 3% in 1988–1994 to nearly 7% in 2001–2002. Prevalence of vitamin D insufficiency also increased from 20% in 1988–1994 to 24% in 2001–2002. The study showed a similar increase in the prevalence of vitamin D deficiency in females older than 12, from 7% in 1988–1994 to 11% in 2001–2002. In contrast to other groups, rates of vitamin D inadequacy decreased in this population from 29% in 1988–1994 to 26% in 2001–2002. Patients at risk of vitamin D deficiency were defined as a 25-OH vitamin D level less than 12 ng/mL and vitamin D inadequacy as levels between 12 and 19 ng/mL (5, 6).
The major complications of vitamin D deficiency in the adult population include osteomalacia, osteopenia, and osteoporosis. According to the World Health Organization approximately 9% of adults older than 50 years had osteoporosis with the prevalence of osteoporosis at the femur neck and lumbar spine of 5 and 6% respectively (7). A retrospective cohort study by Vishwanathan et al. indicated that the additional health care costs incurred by patients due to osteoporotic related fractures was $10,000 each within the 6 months post-fracture period compared to patients without fractures (8). In regards to the incidence of osteopenia, it is estimated that nearly 30% of men and 49% of women older than 50 were osteopenic at the femoral neck (9).
Possible reasons that the obese population is vitamin D deficient include inadequate sun exposure. This study however did not control for the amount of time that the patients spent outside. Previous studies have shown that patients require only 5–30 min of sun exposure twice a week (10). This particular study involved patients living in South Florida, where sunlight exposure is plentiful throughout the year. Based on these factors we do not believe that it would be an accurate assessment to attribute vitamin D deficiency to decreased activity and exposure to sunlight. Other potential reasons may stem from dietary habits that lead to decreased consumption of vitamin D fortified foods such as fish, milk, yogurt, and cheese. Studies have suggested that differences in diet may be secondary to lactose intolerance among blacks and Asians (11, 12). Future studies should look at symptoms of lactose intolerance and consequent dietary habits among these different groups in relation to vitamin D levels to assess for a possible correlation. Other obvious factors that may also affect vitamin D levels in these populations is the use of sunscreen and hats, however this factor was not accounted for in this study. There are limitations to our study. We did not account for the reason why vitamin D levels were obtained. Also it is a retrospective chart review, and as such is subject to selection, treatment, and diagnosis bias. The study only included approximately 400 patients. Despite the small number of patients included in the study, we were able to achieve a significant p value of less than 0.05. We ensured that all patients included were not already on vitamin D supplementation.
The results of this study suggest that obesity can be considered a risk factor for vitamin D deficiency. This knowledge will allow physicians to effectively screen their patients. With the growing cost of health care, prudent screening procedures and preventative measures will allow physicians to proactively treat and avoid the costs of complications from vitamin D deficiency. This study also indicated that blacks and Asians are more prone to vitamin D deficiency compared to the general population. This information will delineate those at highest risk for deficient vitamin D levels and need for supplementation.
Acknowledgements
This research was approved by the Institutional Review Board at both Broward Health Medical Center and Nova Southeastern University. Permission was granted by both institutions for access to patient charts.
Conflict of interest and funding
The authors have no conflicts of interest to disclose in regards to this research study. There was no financial support that facilitated conduct of the work described in the article.
Disclaimer
The views expressed within this article are solely those of the authors.
References
- 1.Wortsman J, Matsuoka L, Chen T, Lu Z, Holick M. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–3. doi: 10.1093/ajcn/72.3.690. [DOI] [PubMed] [Google Scholar]
- 2.Buffington C, Walker B, Cowan SM, Jr, Scruggs D. Vitamin D deficiency in the morbidly obese. Obes Surg. 1993;3(4):421–4. doi: 10.1381/096089293765559142. [DOI] [PubMed] [Google Scholar]
- 3.Codoñer-Franch P, Tavárez-Alonso S, Simó-Jordá R, Laporta-Martín P, Carratalá-Calvo A, Alonso-Iglesias E. Vitamin D status is linked to biomarkers of oxidative stress, inflammation, and endothelial activation in obese children. J Pediatr. 2012;161(5):848–54. doi: 10.1016/j.jpeds.2012.04.046. [DOI] [PubMed] [Google Scholar]
- 4.Ogden C, Carroll M, Kit B, Flegal K. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;311(8):806–14. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the U.S. population: 1988–1994 compared with 2000–2004. Am J Clin Nutr. 2008;88(6):1519–27. doi: 10.3945/ajcn.2008.26182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Center for Health Statistics. National Health and Nutrition Examination Survey, 2001–2006. Available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm [cited 29 May 2014]
- 7.Looker AC, Borrud LG, Dawson-Hughes B, Shepherd JA, Wright NC. Osteoporosis or low bone mass at the femur neck or lumbar spine in older adults: United States, 2005–2008. NCHS data brief no 93. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 8.Vishwanathan HN, Curtis JR, Yu J, White J, Stolshek BS, Merinar C, et al. Direct healthcare costs of osteoporosis-related fractures in managed care patients receiving pharmacological osteoporosis therapy. Appl Health Econ Health Policy. 2012;10(3):163–73. doi: 10.2165/11598590-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Looker AC, Melton LJ, Harris TB, Borrud LG, Shepherd JA. Prevalence and trends in low femur bone density among older US adults: NHANES 2005–2006 compared with NHANES III. J Bone Miner Res. 2010;20:64–71. doi: 10.1359/jbmr.090706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.National Institutes of Health Office of Dietary Office of Dietary Supplements. Vitamin D Fact Sheet for Health Professionals. Available from: http://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/#en6 [cited 1 August 2014]
- 11.Byers KG, Savaiano DA. The myth of increased lactose intolerance in African-Americans. J Am Coll Nutr. 2005;24(6):569–73. doi: 10.1080/07315724.2005.10719505. [DOI] [PubMed] [Google Scholar]
- 12.Jackson KA, Savaiano DA. Lactose Maldigestion, calcium intake and osteoporosis in African-, Asian-, and Hispanic-Americans. J Am Coll Nutr. 2001;20(2):198–207. doi: 10.1080/07315724.2001.10719032. [DOI] [PubMed] [Google Scholar]