Abstract
Macitentan is an orphan drug for the treatment of pulmonary arterial hypertension (PAH). Endothelin-1 (ET-1) plays a critical role of pathophysiology of PAH. Macitentan, a new dual endothelin receptor antagonist, has reportedly improved prognosis of PAH patients by delaying the progression of disease. It prevents the binding of ET-1 to both endothelin A (ETA) and endothelin B (ETB) receptors. Macitentan displays higher efficacy, lesser adverse effects and drug interactions. It has completed phase III trials in 2012 for treatment of PAH and has been tried for ischemic digital ulcers in systemic sclerosis, recurrent glioblastoma and combination with chemotherapeutic agents against various cancers. Safety data for macitentan were obtained primarily from a placebo-controlled clinical study in 742 patients with PAH. The Food and Drug Administration (FDA) approved the drug on 13 October 2013. It is an important addition to long-term treatment of PAH.
Keywords: Cancer, endothelin, macitentan, pulmonary arterial hypertension (PAH)
INTRODUCTION
Macitentan is a tissue-targeting endothelin receptor antagonist (ERA). The chemical name of macitentan is N-[5-(4-Bromophenyl)-6-[2-[(5-bromo-2-pyrimidinyl) oxy] ethoxy]-4-pyrimidinyl]-N’-propylsulfamide. Macitentan is a crystalline powder that is insoluble in water. Macitentan is very stable in the solid state and is neither hygroscopic nor light sensitive.[1,2,3]
The endothelins are a family of naturally occurring peptides that include endothelin-1 (ET-1), endothelin-2 (ET-2) and endothelin-3 (ET-3). Endothelin-1 is synthesized predominantly by the vascular endothelium and is one of the most potent and long lasting vasoconstrictor.[2,3] Elevated ET-1 levels have been found in numerous diseases, suggesting a pathophysiological role of this peptide. ETs regulate diverse biologic processes such as tissue remodeling, tissue repair, cellular differentiation, smooth muscle cell proliferation and inflammation.[3] The two subtypes of endothelin receptors have distinct ligand preference. Endothelin receptor A (ETA) has 10-times more binding affinity for ET-1 and ET-2 than for ET-3, while endothelin receptor B (ETB) has equally potent affinities to all three endogenous endothelins. ET-2 displays similar pharmacology to ET-1, whereas ET-3 is a weaker vasoconstrictor but is a more potent inhibitor of platelet aggregation. Therefore, a selective ETA receptor antagonist may theoretically offer greater beneficial effects in PAH than antagonists of both ETA and ETB receptors.[3,4,5]
Pulmonary arterial hypertension (PAH) is characterized by endothelial cell dysfunction, endothelial and pulmonary artery smooth muscle cell (PASMC) proliferation, pulmonary vasoconstriction and in situ thrombosis, which leads to sustained increases in pulmonary vascular resistance (PVR) and pulmonary arterial pressure, culminating in progressive right ventricular dysfunction and death.[6] The diagnosis of PAH is confirmed by a resting mean pulmonary arterial pressure (mPAP) of ≥25 mmHg and a normal (≤15 mmHg) pulmonary capillary wedge pressure. Circulating plasma levels of ET-1 are raised in patients with PAH. Importantly, increased circulating levels of ET-1 correlate with increased right atrial pressure, increased pulmonary vascular resistance, decreased pulmonary artery oxygen saturation and increased mortality in patients with PAH. Several specific therapeutic agents were developed for the medical management of PAH, including prostanoids (epoprostenol, trepoprostenil, iloprost), ERAs (bosentan, ambrisentan) and phosphodiesterase type 5 inhibitors (sildenafil, tadalafil).[6,7,8]
ERAs are either ETA selective, such as sitaxentan and ambrisentan, or nonselective for the ETA and ETB receptors, such as bosentan. ERAs block the activation of endothelin receptors on endothelial or smooth muscle cells, thereby inhibiting the vasoconstriction and cellular proliferation mediated by endothelin.[6] Currently, both selective and nonselective ERAs are approved and available for treating PAH. Bosentan shows 20:1 ETA/ETB selectivity, ambrisentan has 100:1 selectivity and sitaxsentan has 6500:1 selectivity.[8,9,10]
A reduced risk of edema would constitute a major advance and would allow for the application of ERAs in other diseases. Recent findings showed that darusentan provided additional reduction in blood pressure in patients in whom hypertension could not be controlled adequately with available drugs, and edema or fluid retention occurred in 27% of the patients compared with 14% in patients treated with placebo. Sitaxentan is withdrawn from the market because of unpredictable serious liver injury, which emphasizes the need for compounds with a reduced liver liability.[2,9,11,12]
Macitentan is a competitive ERA with significantly slower receptor dissociation kinetics than the currently approved ERAs.[13] Macitentan improves survival in pulmonary hypertensive patients and is also useful in other disorders associated with chronic tissue ET system activation.
Mechanism of Action
ET-1 binds to G-protein-coupled receptors, namely ETA and ETB. Activation of ETA and ETB receptors on smooth muscle cells mediates the vasoconstrictive and mitogenic effects of ET.[6,8,9] The mitogenic effects of ET-1 are mediated by the activation of protein kinase C secondary to increases in diacylglycerol and intracellular calcium, which in turn stimulate the production of cytokines and growth factors. Elevated levels of ET-1 have been found in patients with PAH, and PAH was found to be associated with the increased expression of ET-1 in vascular endothelial cells of pulmonary arteries.[10,14] Macitentan prevents the binding of ET-1 to both ETA and ETB receptors. Macitentan has a 50-fold increased selectivity for the ETA subtype compared with the ETB subtype.[3] Macitentan displays high affinity and sustained occupancy of the ET receptors in human pulmonary arterial smooth muscle cells. Blocking of the ETA receptor subtype seems to be of higher importance in the treatment of PAH than blocking of ETB, likely because there are higher numbers of ETA receptors than ETB receptors in pulmonary arterial smooth muscle cell.[12,15,16]
Pharmacokinetics
Macitentan is a lipophilic compound. It is absorbed orally. Food has little effect on absorption. Maximum plasma concentrations of macitentan are achieved approximately 8 h after oral dosing in humans.[11] It is metabolized primarily by oxidative depropylation of the sulfamide into ACT-132577, a pharmacologically active depropylated metabolite, and the carboxylic acid metabolite ACT-373898. Macitentan and its active metabolite are highly bound to plasma proteins (>99%), primarily to albumin and to a lesser extent to to alpha-1-acid glycoprotein. The apparent volumes of distribution of macitentan and its active metabolite were about 50 L and 40 L, respectively, in healthy subjects. After multiple dosing, the pharmacokinetics are proportional over the tested dose range (1–30 mg); steady state is achieved by Day 3. The elimination half-life (t1/2) for macitentan is approximately 16 h while ACT-132577 has a t1/2 of approximately 48 h. Excretion involves both renal and fecal route.[14,17,18]
Macitentan has significantly slower receptor dissociation kinetics than the currently approved ERAs. Slow dissociation caused insurmountable antagonism in functional PASMC-based assays, and this could contribute to an enhanced pharmacological activity of macitentan in ET-1-dependent pathologies than bosentan and ambrisentan.[19]
Clinical Efficacy
The large Phase III study with an ERA in PAH to improve clinical outcome (SERAPHIN) showed that the effect on a composite clinically relevant morbidity/mortality end point was highly significant at a 10 mg/day dose with superior safety profile in relation to hepatic safety and edema/fluid retention than bosentan and ambrisentan, respectively.[24,25]
The registry to evaluate early and long-term PAH disease management (REVEAL Registry) in the United States suggests considerable improvements in survival in the past two decades, the effects of which most likely reflect a combination of changes in treatments, improved patient support strategies and possibly a PAH population at variance with other cohorts.[26]
Many tumors have been found to express ETs and ETRs. ET pathways have been shown to play important roles in tumor cell proliferation, migration and invasion and vascular differentiation. The ET axis has been reported to be of relevance in lung cancer, colon cancer, renal cancer, cervical cancer, brain tumors and ovarian cancer. Macitentan alone decreased the expression of survival pathways but was ineffective or was only marginally effective alone as an antitumor agent therefore leading to strong synergism with chemotherapy.[15,16]
ET-1/ETA receptor axis appears to be critical in epithelial-to- mesenchymal transition in ovarian tumor cells in which epithelial cells depolarize, disassemble cell–cell contacts and adopt an invasive phenotype becoming a key event in ovarian cancer pathophysiology. ET-1 enhances the secretion of matrix metalloproteinase, disrupts intercellular communications and stimulates cell migration and invasion. ET-1 binding to the ETA receptor results in p125 focal adhesion kinase (FAK) and paxillin activation, which are thought to transduce signals involved in tumor cell invasion. Furthermore, ETA receptor activation triggers the antiapoptotic signaling through phosphatidyl inositol 3-kinase (PI3-K)-mediated Akt pathways indicating the existence of multiple signal transduction pathways downstream to ETA receptor activation in ET-1-stimulated ovarian cancer cells involved in tumorigenic events.[20]
ETs inhibit the Prolyl Hydroxylase Domain 2 (PHD2) to regulate angiogenesis and melanoma cell invasion and to activate hypoxia-inducible factor-1a in melanoma cells.[21]
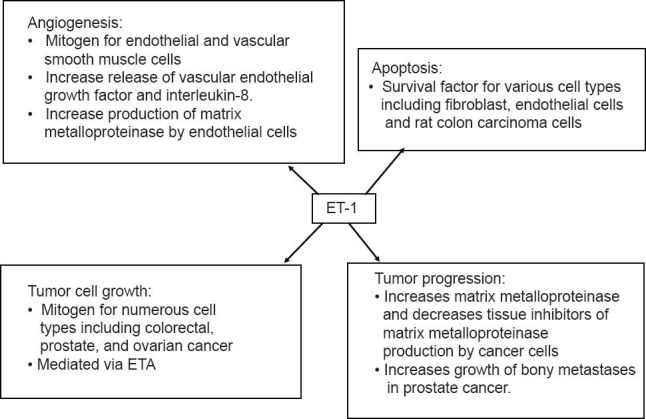
ET-1 acts as a co-mitogen with factor such as epidermal growth factor. ET-1 also stimulates colonic fibroblast cellular processes in vitro that are involved in developing tumor stroma. It upregulates genes for profibrotic growth factors and receptors, signaling molecules, actin modulators and extracellular matrix components that have a central role in the development of colorectal cancer.[22,23,24,25] Actions of endothelin-1 in cancer are depicted in Figure 1.
Figure 1.
Indications
Macitentan is available as a 10 mg film-coated tablet for once daily oral administration and is used in the following conditions:
Treatment of pulmonary arterial hypertension: It is given 10 mg once daily. It has an orphan drug status for the treatment of pulmonary arterial hypertension to delay disease progression. The drug was approved by the FDA on 13 October 2013.[26,27,28,29]
Orthotopically implanted human ovarian carcinoma: Macitentan enhances the therapeutic efficacy of paclitaxel against ovarian carcinoma by modulating the survival pathways of the tumor cells.[15,16]
Clinical development is underway for other indications including Eisenmenger syndrome, ischemic digital ulcers secondary to systemic sclerosis, idiopathic pulmonary fibrosis and glioblastoma.[9,30,31,32,33]
Adverse Effects
Most common adverse effects are anemia, nasopharyngitis/pharyngitis, bronchitis, headache, influenza and urinary tract infection. Other rare adverse effects are hepatotoxicity and liver failure, decreased spermatogenesis and edema.[4,9,14,18,32]
Contraindications and Precautions
Macitentan is contraindicated in pregnancy. Females of reproductive potential should be counseled on the use of reliable contraception and have a negative pregnancy test prior to initiating therapy and monthly thereafter.[7,11,13] Pharmacokinetic alterations of macitentan due to hepatic or renal function impairment are not considered clinically relevant and no dose adjustment is necessary in these patients.[18,28,34]
Pediatric Use
The safety and efficacy of macitentan in children has not been established.[14]
Safety in Pregnancy
Pregnancy category X. Macitentan may cause fetal harm. It has potential to cause teratogenicity as well as cardiovascular and mandibular arch fusion abnormalities in rabbits and rats at all tested doses.[11,14]
Drug Interaction
Strong inducers of CYP3A4 such as rifampin significantly reduce macitentan exposure. Use of strong CYP3A4 inhibitors like ketoconazole and ritonavir approximately double the macitentan exposure. Avoid concomitant use of macitentan with strong CYP3A4 inducers and CYP3A4 inhibitors. It is markedly less prone to drug–drug interactions than bosentan and other ET antagonists.[8,29,35,36,37,38]
CONCLUSION
Macitentan is an orally active, novel, highly potent, tissue-targeting ERA. It displays antihypertensive and anticancer activity. It is an important addition to the therapeutic armamentarium in the long-term treatment of PAH based on its high safety profile with less drug interaction than the currently available treatment option for PAH.[39,40] It also has a synergistic effect with chemotherapy in the treatment of ovarian cancer, colon cancer, melanoma, etc., Its potential use in other disorders is under investigation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bruderer S, Hopfgartner G, Seiberling M, Wank J, Sidharta PN, Treiber A, et al. Absorption, distribution, metabolism, and excretion of macitentan, a dual endothelin receptor antagonist, in humans. Xenobiotica. 2012;42:901–10. doi: 10.3109/00498254.2012.664665. [DOI] [PubMed] [Google Scholar]
- 2.Lepist EI, Gillies H, Smith W, Hao J, Hubert C, St Claire RL, et al. Evaluation of the endothelin receptor antagonists ambrisentan, bosentan, macitentan, and sitaxsentan as hepatobiliary transporter inhibitors and substrates in sandwich-cultured human hepatocytes. PLoS One. 2014;9:e87548. doi: 10.1371/journal.pone.0087548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Iglarz M, Binkert C, Morrison K, Fischli W, Gatfield J, Treiber A, et al. Pharmacology of macitentan, an orally active tissue-targeting dual endothelin receptor antagonist. J Pharmacol Exp Ther. 2008;327:736–45. doi: 10.1124/jpet.108.142976. [DOI] [PubMed] [Google Scholar]
- 4.Sitbon O, Morrell N. Pathways in pulmonary arterial hypertension: The future is here. Eur Respir Rev. 2012;21:321–7. doi: 10.1183/09059180.00004812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seferian A, Simonneau G. Therapies for pulmonary arterial hypertension: Where are we today, where do we go tomorrow? Eur Respir Rev. 2013;22:217–26. doi: 10.1183/09059180.00001713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parida A, Nayak V. Endothelins: Their current status and future prospects. Int J Pharm Sci Rev Res. 2013;23:94–7. [Google Scholar]
- 7.Sidharta PN, van Giersbergen PL, Halabi A, Dingemanse J. Macitentan: Entry-into-humans study with a new endothelin receptor antagonist. Eur J Clin Pharmacol. 2011;67:977–84. doi: 10.1007/s00228-011-1043-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Y, O’Callaghan DS, Humbert M. An update on medical therapy for pulmonary arterial hypertension. Curr Hypertens Rep. 2013;15:614–22. doi: 10.1007/s11906-013-0394-8. [DOI] [PubMed] [Google Scholar]
- 9.Yao A. Recent advances and future perspectives in therapeutic strategies for pulmonary arterial hypertension. J Cardiol. 2012;60:344–9. doi: 10.1016/j.jjcc.2012.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Pulido T, Rubin LJ, Simonneau G. Macitentan and pulmonary arterial hypertension. N Engl J Med. 2014;370:82–3. doi: 10.1056/NEJMc1313112. [DOI] [PubMed] [Google Scholar]
- 11.Galiè N, Ghofrani AH. New horizons in pulmonary arterial hypertension therapies. Eur Respir Rev. 2013;22:503–14. doi: 10.1183/09059180.00006613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruderer S, Marjason J, Sidharta PN, Dingemanse J. Pharmacokinetics of macitentan in caucasian and Japanese subjects: The influence of ethnicity and sex. Pharmacology. 2013;91:331–8. doi: 10.1159/000351704. [DOI] [PubMed] [Google Scholar]
- 13.Humbert M, Souza R, Galiè N, McLaughlin V, Simonneau G, Rubin L. Pulmonary arterial hypertension: Bridging the present to the future. Eur Respir Rev. 2012;21:267–70. doi: 10.1183/09059180.00005312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolli MH, Boss C, Binkert C, Buchmann S, Bur D, Hess P, et al. The discovery of N-[5-(4-bromophenyl)-6-[2-[(5-bromo-2-pyrimidinyl) oxy] ethoxy]-4-pyrimidinyl]-N’-propylsulfamide (Macitentan), an orally active, potent dual endothelin receptor antagonist. J Med Chem. 2012;55:7849–61. doi: 10.1021/jm3009103. [DOI] [PubMed] [Google Scholar]
- 15.Sidharta PN, van Giersbergen PL, Dingemanse J. Safety, tolerability, pharmacokinetics, and pharmacodynamics of macitentan, an endothelin receptor antagonist, in an ascending multiple-dose study in healthy subjects. J Clin Pharmacol. 2013;53:1131–8. doi: 10.1002/jcph.152. [DOI] [PubMed] [Google Scholar]
- 16.Kim SJ, Kim JS, Kim SW, Yun SJ, He J, Brantley E, et al. Antivascular therapy for multidrug-resistant ovarian tumors by macitentan, a dual endothelin receptor antagonist. Transl Oncol. 2012;5:39–47. doi: 10.1593/tlo.11286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim SJ, Kim JS, Kim SW, Brantley E, Yun SJ, He J, et al. Macitentan (ACT-064992), a tissue-targeting endothelin receptor antagonist, enhances therapeutic efficacy of paclitaxel by modulating survival pathways in orthotopic models of metastatic human ovarian cancer. Neoplasia. 2011;13:167–79. doi: 10.1593/neo.10806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bruderer S, Aänismaa P, Homery MC, Häusler S, Landskroner K, Sidharta PN, et al. Effect of cyclosporine and rifampin on the pharmacokinetics of macitentan, a tissue-targeting dual endothelin receptor antagonist. AAPS J. 2012;14:68–78. doi: 10.1208/s12248-011-9316-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gatfield J, Grandjean CM, Sasse T, Clozel M, Nayler O. Slow receptor dissociation kinetics differentiate macitentan from other endothelin receptor antagonists in pulmonary arterial smooth muscle cells. PLoS One. 2012;7:e47662. doi: 10.1371/journal.pone.0047662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosanò L, Spinella F, Bagnato A. The importance of endothelin axis in initiation, progression, and therapy of ovarian cancer. Am J Physiol Regul Integr Comp Physiol. 2010;299:R395–404. doi: 10.1152/ajpregu.00304.2010. [DOI] [PubMed] [Google Scholar]
- 21.Spinella F, Rosanò L, Del Duca M, Di Castro V, Nicotra MR, Natali PG, et al. Endothelin-1 inhibits prolyl hydroxylase domain 2 to activate hypoxia-inducible factor-1alpha in melanoma cells. PLoS One. 2010;5:e11241. doi: 10.1371/journal.pone.0011241. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 22.Knowles JP, Shi-Wen X, Haque SU, Bhalla A, Dashwood MR, Yang S, et al. Endothelin-1 stimulates colon cancer adjacent fibroblasts. Int J Cancer. 2012;130:1264–72. doi: 10.1002/ijc.26090. [DOI] [PubMed] [Google Scholar]
- 23.Grant K, Loizidou M, Taylor I. Endothelin-1: A multifunctional molecule in cancer. Br J Cancer. 2003;88:163–6. doi: 10.1038/sj.bjc.6700750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kummer O, Haschke M, Hammann F, Bodmer M, Bruderer S, Regnault Y, et al. Comparison of the dissolution and pharmacokinetic profiles of two galenical formulations of the endothelin receptor antagonist macitentan. Eur J Pharm Sci. 2009;38:384–8. doi: 10.1016/j.ejps.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 25.Torbicki A, Mehta S, Perchenet L, Pulido T, Sastry BK, Sitbon O, et al. Effect of macitentan on haemodynamics in patients with pulmonary arterial hypertension: Results from the long-term, randomised, placebo- controlled SERAPHIN trial. Eur Heart J. 2013;34(Suppl 1):1062. [Google Scholar]
- 26.Benza RL, Miller DP, Barst RJ, Badesch DB, Frost AE, McGoon MD. An evaluation of long-term survival from time of diagnosis in pulmonary arterial hypertension from the REVEAL Registry. Chest. 2012;142:448–56. doi: 10.1378/chest.11-1460. [DOI] [PubMed] [Google Scholar]
- 27.Macchia A, Mariani J, Tognoni G. Macitentan and pulmonary arterial hypertension. N Engl J Med. 2014;370:82. doi: 10.1056/NEJMc1313112. [DOI] [PubMed] [Google Scholar]
- 28.Thompson CA. Macitentan approved by FDA to delay progression of PAH. Am J Health Syst Pharm. 2013;70:2054. doi: 10.2146/news130076. [DOI] [PubMed] [Google Scholar]
- 29.Patel T, McKeage K. Macitentan: First global approval. Drugs. 2014;74:127–33. doi: 10.1007/s40265-013-0156-6. [DOI] [PubMed] [Google Scholar]
- 30.Raja SG. Macitentan, a tissue-targeting endothelin receptor antagonist for the potential oral treatment of pulmonary arterial hypertension and idiopathic pulmonary fibrosis. Curr Opin Investig Drugs. 2010;11:1066–73. [PubMed] [Google Scholar]
- 31.Tonelli AR, Dweik RA. Macitentan and pulmonary arterial hypertension. N Engl J Med. 2014;370:81–2. doi: 10.1056/NEJMc1313112. [DOI] [PubMed] [Google Scholar]
- 32.Weber MA, Black H, Bakris G, Krum H, Linas S, Weiss R, et al. A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension: A randomised, double-blind, placebo-controlled trial. Lancet. 2009;374:1423–31. doi: 10.1016/S0140-6736(09)61500-2. [DOI] [PubMed] [Google Scholar]
- 33.Raghu G, Million-Rousseau R, Morganti A, Perchenet L, Behr J MUSIC Study Group. Macitentan for the treatment of idiopathic pulmonary fibrosis: The randomised controlled MUSIC trial. Eur Respir J. 2013;42:1622–32. doi: 10.1183/09031936.00104612. [DOI] [PubMed] [Google Scholar]
- 34.Sen S, Chen S, Feng B, Iglarz M, Chakrabarti S. Renal, retinal and cardiac changes in type 2 diabetes are attenuated by macitentan, a dual endothelin receptor antagonist. Life Sci. 2012;91:658–68. doi: 10.1016/j.lfs.2012.03.032. [DOI] [PubMed] [Google Scholar]
- 35.Mule M, Scarabelli M, Capodanno D, Ussia GP, Tamburino C. Clinical pharmacotherapy and drug development for pulmonary arterial hypertension. Recent Pat Cardiovasc Drug Discov. 2011;6:180–8. doi: 10.2174/157489011797377059. [DOI] [PubMed] [Google Scholar]
- 36.Weiss J, Theile D, Rüppell MA, Speck T, Spalwisz A, Haefeli WE. Interaction profile of macitentan, a new non-selective endothelin-1 receptor antagonist, in vitro. Eur J Pharmacol. 2013;701:168–75. doi: 10.1016/j.ejphar.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 37.Kohan DE, Cleland JG, Rubin LJ, Theodorescu D, Barton M. Clinical trials with endothelin receptor antagonists: What went wrong and where can we improve? Life Sci. 2012;91:528–39. doi: 10.1016/j.lfs.2012.07.034. [DOI] [PubMed] [Google Scholar]
- 38.Aubert JD, Juillerat-Jeanneret L. Therapeutic potential of endothelin receptor modulators: Lessons from human clinical trials. Expert Opin Ther Targets. 2009;13:1069–84. doi: 10.1517/14728220903074570. [DOI] [PubMed] [Google Scholar]
- 39.Pulido T, Adzerikho I, Channick RN, Delcroix M, Galiè N, Ghofrani HA, et al. SERAPHIN Investigators. Macitentan and morbidity and mortality in pulmonary arterial hypertension. N Engl J Med. 2013;369:809–18. doi: 10.1056/NEJMoa1213917. [DOI] [PubMed] [Google Scholar]
- 40.Smith KA, Fraidenburg DR, Yuan JXJ. Targeted therapies: Endothelin receptor antagonists. In: Smith KA, Fraidenburg DR, Yuan JXJ, editors. Advances in the Management of Pulmonary Arterial Hypertension. London: Future Medicine Ltd; 2013. pp. 64–73. [Google Scholar]


