Abstract
This communication is the first of a series on South Asian fasts, festivals, and diabetes, designed to spread awareness and stimulate research on this aspect of diabetes and metabolic care. It describes the various fasts observed as part of Hindu religion and offers a classification scheme for them, labeling them as infrequent and frequent. The infrequent fasts are further sub-classified as brief and prolonged, to facilitate a scientific approach to glycemic management during these fasts. Pre-fast counseling, non-pharmacological therapy, pharmacological modification, and post-fast debriefing are discussed in detail. All available drug classes and molecules are covered in this article, which provides guidance about necessary changes in dosage and timing of administration. While in no way exhaustive, the brief review offers a basic framework which diabetes care professionals can use to counsel and manage persons in their care who wish to observe various Hindu fasts.
Keywords: Culture bound medicine, diabetes mellitus, Hinduism, India, insulin, oral hypoglycemic agents
INTRODUCTION
Religion and culture play an important part in the life of many people across the world. Religio-cultural practices are an integral component of their day- to day activities and impact their health as well. Fasting is a ubiquitous religio-cultural practice that is found, in varying forms, across the world. The month long Ramadan and Buddhist Lent fasts are example of religious observances practiced by followers of Islam, and Buddhism, respectively. These fasts are characterized by a well-documented impact on metabolic health, which can be minimized by well-known management strategies.[1,2] This communication is the first of a series on South Asian fasts, festivals, and diabetes, designed to spread awareness and stimulate research on this aspect of diabetes and metabolic care.
HINDU FASTS
Hinduism constitutes the world's third largest religion, with over 1 billion adherents.[3] Hindus comprise over 80% of the population of Nepal and India, and over 5% of the population in at least another 15 countries. Hinduism does not enjoin its followers to practice mandatory fasting. However, many day-long and week-long fasts are observed by Hindus. These include the annual Karva Chauth and Guru Purnima, undertaken by women to pray for a long life for their husbands; Hoi Ashtami observed by women for their sons’ longevity; monthly fasts (Ekadashi, Purnima, and Pradosha) and weekly fasts, as part of various vows. Longer fasts included the Navratras (9 days) that occur twice a year. Most Hindu fasting periods extend from dawn to moon-rise or from dawn to star-rise. This is in contradiction to the Jain religion, which requires fasting from dusk to dawn, but is similar to fasting advised in Islam and Buddhism. The day-long nature of Hindu fasts however makes it distinct from the month-long fasts of Ramadan and Buddhist Lent. Unlike in Islam, there are no universal rules laid down for Hindu fasts, and their observance varies from region to region, family to family, and the person to person. This heterogeneity has prevented a systematic study of the metabolic effect of these fasts so far.
Few health care professionals realize the importance of this issue in people with diabetes. Intermittent fasting is associated with proven health benefits. However, fasting, without taking adequate safe guards, may predispose persons on glucose-lowering medication to hypoglycemia. Persons who abstain from water and other liquids during the hot Indian summer run the risk of dehydration, dyselectrolytemia, and hypotension.[4] Over-indulgence in high-fat, high-carbohydrate, calorie-rich foods, after completion of the fasting period, may cause peaks of hyperglycemia and worsen glycemia variability. These issues pose a challenge for the diabetes care provider, who is expected to craft an individualized dietary, physical activity and medical prescription, which is able to achieve adequate glycemic control on both fasting and non-fasting days, without either hypo- or-hyper-glycemia. This communication aims to provide guidance in this regards.
PRE-FAST COUNSELING/ASSESSMENT
Discussion about fasting should be initiated prior to the fast. This should include the potential discomforts and risks of fasting, and means of mitigating them.
The person's exact perspective of fasting, including duration of fast, allowance for liquids and snacks during the day, acceptance of sublingual foods and freedom to break the fast in case of significant discomfort must be clarified. Pre-fast counseling should include an explanation of the symptoms of hypoglycemia and hypoglycemia awareness training (HAT).[5]
Pre-fast assessment, comprises comprehensive history-taking, physical examination, and investigations aimed at identifying stigmata of target-organ damage, so that strategies can be made to optimize health during fasts. Factors that may increase the risk of hypoglycemia, hypoglycemia unawareness, and dehydration must be noted.
The concept of shared decision making and person-centeredness must be followed, in letter and in spirit while considering whether a particular individual can fast safely or not.
NON-PHARMACOLOGICAL THERAPY
Lifestyle modification is the primary mode of therapy in type 2 diabetes. Fasting in itself is a lifestyle modification. If utilized properly, intermittent fasting can provide multiple health-related benefits, apart from the socio-religious goals that it aims for.[6]
The composition of the pre-fast meal should be such that it provides enough “slow-release” calories to take care of the fasting period. Complex carbohydrates with low glycemic index and proteins fulfill this need. Simple suggestions such as addition of unprocessed cereals, fruits, nuts, and lentils, to the pre-fast meal, reduce its glycemic index and allow energy availability for a longer period. Adequate water and fluids must be taken prior to the fast especially in cases where fluid intake will be restricted throughout the day. Serving of meal supplements may be added to pre-fast meals or intra fast liquids, to prevent hypoglycemia.
Physical activity should be restricted during fasting periods. While routine daily activities can easily be performed, elective moderate to highly vigorous exercise should be rescheduled. Stress management is an important component of non-pharmacological diabetes care. Religious fasting offers an opportunity to practice meditation, reduce stress, and facilitate better glycemic control.
APPROACH TO MODIFICATION OF PHARMACOLOGICAL THERAPY DURING FASTING
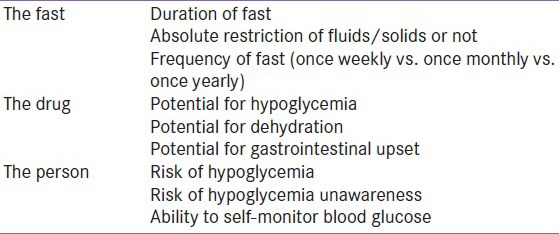
Strategies for modification of suggestion during therapy, during fasting, well depend upon the nature of both the drug and the fast [Table 1], as well as the person's profile.
Table 1.
Factors influencing approach to glucose lowering drug treatment during fasting
In infrequent fasts such as those held every year (Karva Chauth, Hoi, and Guru Purnima), ad-hoc drug substitution or dose adjustment can be performed on the day of the fast. For more frequent fasts (e.g. monthly Purnima, Ekadashi or Pradosha fasts, fortnightly and weekly fasts) the drug regimen should be crafted so as to allow fasting without necessitating frequent consultation with the health care provider. A significant degree of diabetes self-management education, person-provider communication, and patient empowerment is required in such cases. The large number of currently available pharmacotherapeutics allows an almost infinite variety of permutation and combinations. The astute clinician can easily craft a prescription that suits the individual patient's needs, ensures safety and tolerability, and provides efficient glucose lowering, while fasting. The approaches to modification of pharmacological therapy can be classified, for ease of understanding, as a substitution of drug, substitution of the drug class, down-titration of dose, and change in timing of administration.
All glucose-lowering drugs have an inherent tendency to cause hypoglycemia. These drugs can be classified as having a glucose-independent or a glucose-dependent mechanism of action. Drug with a glucose-dependent mechanism of action may need no change in dosage or in timing of administration during fasts.[7] Those with a glucose-independent action, which are more prone to causing hypoglycemic, such as sulfonylureas and insulin, may need down-titration of dose. Safer alternative, if available within the same class, such as third-generation sulfonylureas and insulin analogs, should be preferred. In situations where the risk of hypoglycemia is high, drugs acting independently of glucose must be avoided. In some cases, change of timing of administration of the dose may be helpful.
POST-FAST DEBRIEFING
Post-fast, a history should be taken to enquire about bio psychosocial health and quality of life during the fasting period, and elicit subtle symptoms of hypoglycemia or hypotension. This will help plan future therapeutic strategies.
INFREQUENT BUT BRIEF FASTS
While all fasts may not be exactly the same, we take Karva Chauth as a prototype for further discussion. The Karva Chauth is observed by most married women in North India, on the 4th day of the month of Kartik. This corresponds to the month of October/November in the Gregorian calendar. The fast begins at dawn or sunrise, may or not allow a glass of water or juice in the afternoon, and is broken only when moon is sighted. The duration of this fast is roughly 12–15 h, depending upon the latitude, and upon the clarity of the night sky.
Based upon the pre-existing glucose-lowering therapy, one may follow any of the approaches listed in Table 2 to manage glycemia during these fasts.
Table 2.
Modification of glucose-lowering therapy during Karva Chauth
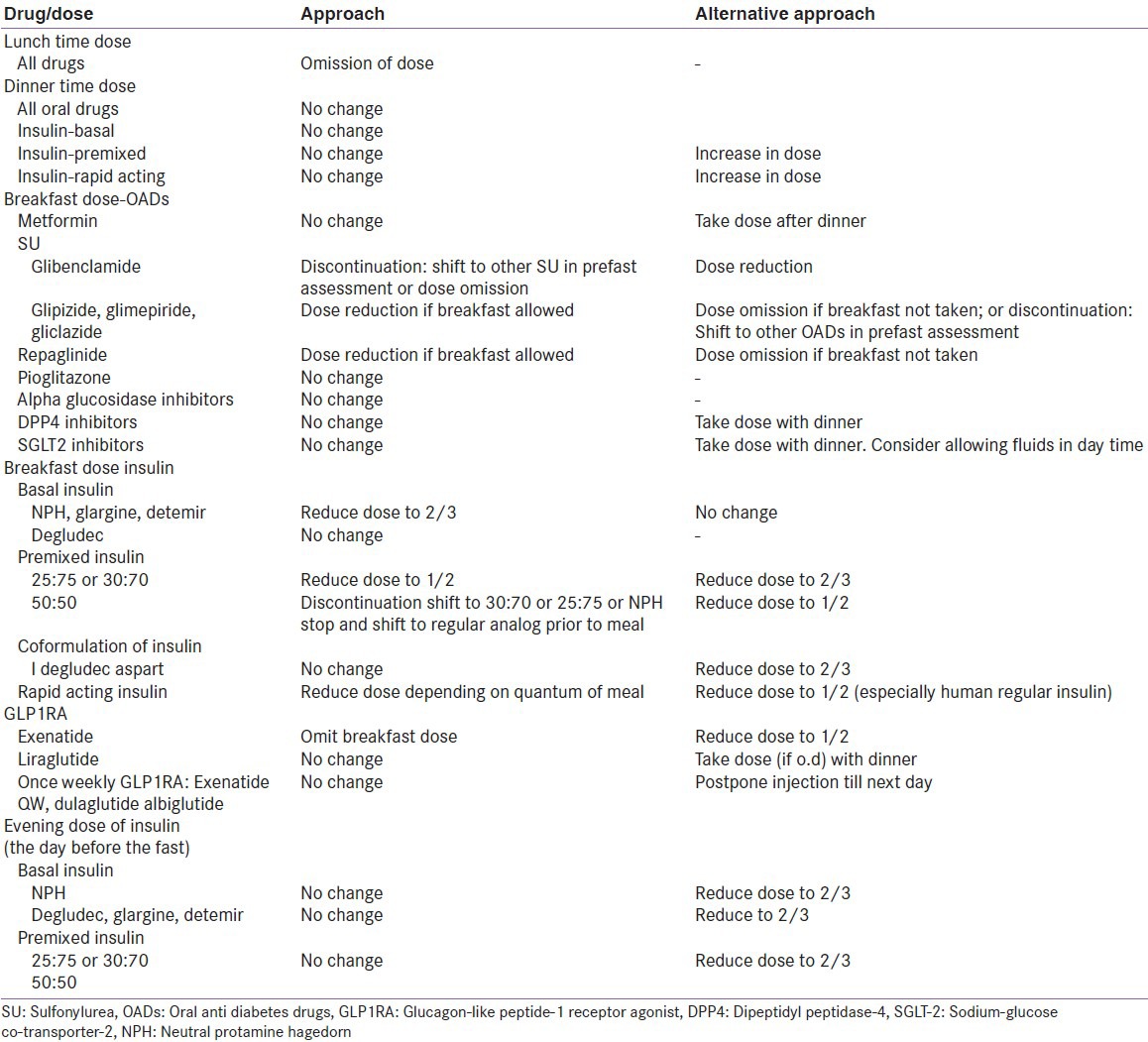
As this is an annual fast, observance of Karva Chauth does not justify changing therapy for the rest of the year. Routine therapy should be planned as per clinical requirement. Any lunch time therapy, e.g. metformin repaglinide, acarbose, voglibose or rapid action insulin will obviously have to be discontinued on the day of the day fast. Dinner time therapy usually needs no change, though persons may prefer to take their drugs after breaking the fast, instead of before. The early morning therapy usually needs no change, except when sulfonylurea or insulin has been prescribed. The safest sulfonylureas, with lesser risk of hypoglycemia, should be chosen, and prescribed in a lower dose on the day of fast. The availability of scored tablets facilitates this process. Fixed dose combination of sulfonylurea with metformin should also be taken in a lower dose on the day of fast.
The approach to insulin dosage depends upon the action profile of the molecule. Basal insulin usually needs no change in dosage, though a cautious physician may suggest a reduction to 2/3 dose, especially with NPH insulin. Premixed insulin, too, should be prescribed in a lower dose on the day of fast.[8] The decision to substitute therapy for 1 day may be difficult. Persons on a 50:50 ratio of premixed insulin, however, may benefit from a 30:70 ratio on that day. Persons on a basal bolus regime should reconsider the decision to fast, or should take a lower dose of rapid action insulin in the morning. SMBG is not forbidden in Hindu fasts, and people with diabetes should be advised to continue or strengthen SMBG practices during fasts.
INFREQUENT BUT PROLONGED FASTS
Navratra fasts, which last for 8–9 days, are commonly observed in the north and west India. Though considered as fasts, these are more like celebrations wherein foods rich in sweets and fats are consumed. Often there is significantly higher energy consumption during these days that may be evenly distributed throughout the day, unless one prefers to live on milk and fruits only. Glycemic control is often poor or inadequate in these fasts. Dietary modifications should be most helpful in these fasts for obvious reasons. Avoidance of fried and sweet foods, and their substitution with frequent servings of milk and milk products, fruits, boiled vegetables and permitted whole cereals, are a few of the healthy options possible. If regular meals are assured, daily medications may be continued as before (or the dose of glucose lowering drugs involving glucose-independent mechanisms should be reduced to 2/3).
FREQUENT FASTS
While ad hoc modifications may be suitable for infrequent fasting, regular fasts need a different therapeutic strategy. For purposes of discussing this clinical challenge, we take an example of a weekly fast in which food is absolutely restricted from dawn to dusk. These include weekly Somvaar or Mangalvaar (Monday or Tuesday) fasts, observed for pre-determined periods of time, sometimes extending up to 16 weeks. The possible modification in glucose lowering therapy, distinct from those planned for infrequent fasts, are discussed in Table 3.
Table 3.
Modification of glucose-lowering therapy in persons who fast frequently
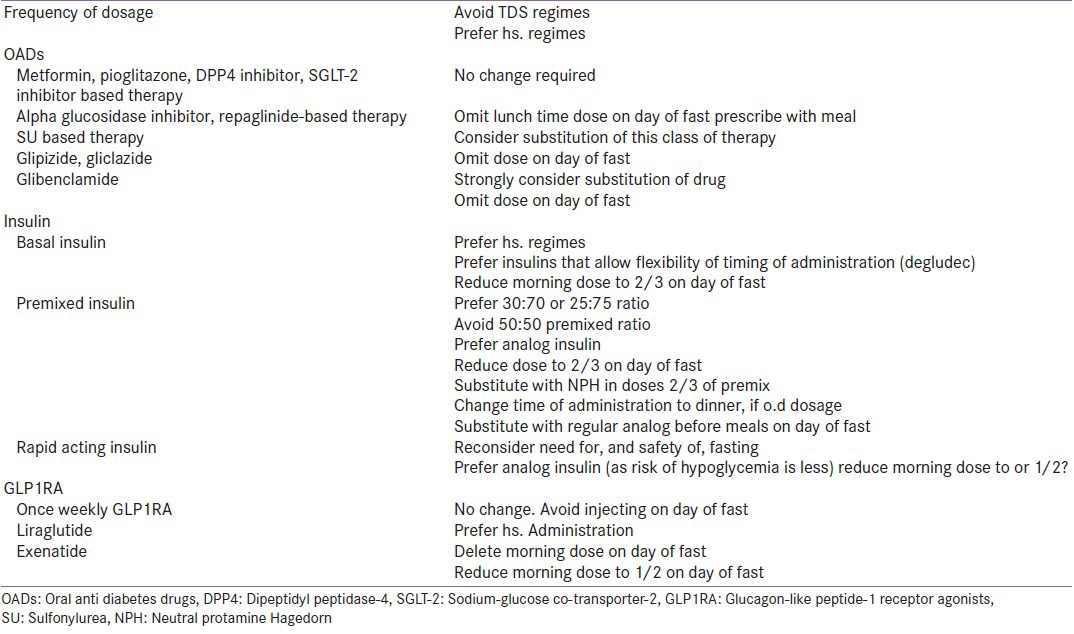
In persons wishing to keep frequent fasts, the overall diabetes prescription should be crafted keeping this in mind. The emphasis should be on safer classes of drugs, and safer molecule. Drugs with a high propensity to hypoglycemia or gastrointestinal intolerance should be avoided as should insulin regimens that mandate a 3 + 3 meal pattern. The need for SGLT2 inhibitors should be reassessed in persons who abstain from liquids for long periods of time. Once daily therapy, which can be administered without regards to meal timings, e.g. pioglitazone, most DPP4 inhibitors, insulin degludec, and liraglutide,[9] should preferably be administered after breaking of the fast, at night. Once weekly injectable GLP1 receptor agonists should be scheduled on non-fasting days.
Persons who take a single meal during the day of fasting, such as a brunch consumed on Somvaar or mangalvaar (Monday or Tuesday) fasts, may benefit from a single dose of a short-acting drug which targets post-prandial glycemia. Alpha-glucosidase inhibitors, repaglinide or glipizide are appropriate choices for this.
DISCUSSION
While evidence-based guidelines are available for many aspects of diabetes care, religious fasting poses a unique challenge. This is especially true for intermittent fasting, in which a randomized controlled trial is difficult to design. In lieu of this, guidance can be obtained from a thorough understanding of the physiology of fasting, the pathophysiology and clinical manifestation of diabetes, and the pharmacokinetic/dynamic properties of available glucose-lowering drug. Concordance can be achieved between the person's wish to fast and the action-profile of prescribed drug therapy, in a safe and well-tolerated manner, in most cases.
Drugs with a low risk of hypoglycemia may not need change of dosage or timing of administration. If there is concern about hypoglycemia or gastrointestinal tolerance, however, one may change the timing administration. This is a feasible, and rational, approach with newer drugs that have a longer half-life such as insulin degludec, SGLT2 inhibitors, and once weekly GLP1RAs. Drugs associated with risk of hypoglycemia may be down-titrated on the morning of the fast, discontinued for 1 day, or substituted with a safer/shorter-acting molecule. Substitution is a better option in persons who wish to fast at frequent (e.g.; weekly) intervals.
CONCLUSION
Diabetes care professionals have a responsibility to provide safe, effective, person-centerd treatment that respects individual attitudes wishes and needs. The current communication is a small step in this direction. The authors recognize the social phenomenon of fasting in Hinduism and its impact on metabolic and glycemic health in diabetes. They suggest a pragmatic logic-based approach to the management of people with diabetes who wish to fast. It is hoped that this effort will stimulate research in this field, which in turn will create evidence-based approaches to help manage this clinical challenge.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Latt TS, Baruah MP, Sahay R. Nutritional recommendations for type 2 diabetes during Buddhist Lent (War Dwin) J Med Nutr Nutraceutical. 2013;2:84–5. [Google Scholar]
- 2.Jaleel MA, Raza SA, Fathima FN, Jaleel BN. Ramadan and diabetes: As-Saum (The fasting) Indian J Endocrinol Metab. 2011;15:268–73. doi: 10.4103/2230-8210.85578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hinduism. [Last accessed on 2014 Dec 08]. Available from: http://www.en.wikipedia.org/wiki/Hinduism .
- 4.Kelwade J, Sethi BK, Vaseem A, Nagesh VS. Sodium glucose co transporter 2 inhibitors and Ramadan: Another string to the bow. Indian J Endocrinol Metab. 2014;18:874–5. doi: 10.4103/2230-8210.141397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fatima J, Karoli R, Chandra A, Naqvi N. Ramadan fasting in patients with type 2 diabetes mellitus: Experience from a teaching hospital. Indian J Endocrinol Metab. 2012;16:323–4. doi: 10.4103/2230-8210.93784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaleel MA, Fathima FN, Jaleel BN. Nutrition, energy intake-output, exercise, and fluid homeostasis during fasting in Ramadan. J Med Nutr Nutraceutical. 2013;2:63–8. [Google Scholar]
- 7.Bashir MI, Pathan MF, Raza SA, Ahmad J, Khan AK, Ishtiaq O, et al. Role of oral hypoglycemic agents in the management of type 2 diabetes mellitus during Ramadan. Indian J Endocrinol Metab. 2012;16:503–7. doi: 10.4103/2230-8210.97994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hassanein M, Belhadj M, Abdallah K, Bhattacharya AD, Singh AK, Tayeb K, et al. Management of type 2 diabetes in Ramadan: Low-ratio premix insulin working group practical advice. Indian J Endocrinol Metab. 2014;18:794–9. doi: 10.4103/2230-8210.140242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pathan MF, Sahay RK, Zargar AH, Raza SA, Khan AK, Siddiqui NI, et al. South Asian Consensus Guideline: Use of GLP-1 analogue therapy in diabetes during Ramadan. Indian J Endocrinol Metab. 2012;16:525–7. doi: 10.4103/2230-8210.98003. [DOI] [PMC free article] [PubMed] [Google Scholar]


