Abstract
Aim:
In the less dense bone, it is difficult to obtain implant anchorage. The present study was undertaken to determine the survival rate of Maestro™ implants placed in d3 and d4 bones.
Materials and Methods:
Fourteen patients (10 males and 4 females) were selected for the study and implants were evaluated for posttreatment changes in at 3, 6, 9 and 12 months from implant placement. The implant probing depth and mobility were recorded 3 and 6 months after prosthesis placement. Also, peri-implant bone level was assessed at the baseline and 12 months postoperatively, followed by a statistical analysis.
Results:
The mean plaque and gingival indices showed a reduction at repeated intervals. The mean sulcular bleeding showed a slight reduction which was statistically significant. An overall mean bone loss was observed after 12 months follow-up, which was statistically not significant. The overall survival rate of implants was reported as 92.3%.
Conclusion:
The specific implant used in the study is advantageous in the soft bone condition.
Clinical Significance:
Although, there is a great evidence of implant failure in compromised jaw quality, the newer designs and approaches suggest that the poor quality is not a contraindication.
Keywords: Clinico-radiographical, implants, low-density, maestro
Introduction
The root form implants are widely demonstrated in the literature. The density of bone site is a determining factor in treatment planning and initial progressive bone loading during prosthetic reconstruction.[1] Amongst the various classifications proposed, the Misch's[2] and Lekholm's and Zarb's[3] categorization of bone quality were more clinically applicable. But, irrespective of the difference, all the bone types were treated with the standard protocol. In 1988, Misch[4] described four groups independent of the regions of the jaws, based on macroscopic cortical and trabecular bone characteristics as follows: D1: Dense cortical bone; D2: Thick dense to porous cortical bone; D3: Thin porous cortical bone on crest; D4: Fine trabecular bone and D5: Immature bone.
Achieving the initial stability is the key criteria for osseointegration. It is difficult to obtain anchorage in the less dense bone which results in low success rate. In a meta-analysis, it was found that bone quality was responsible for 7.7% of all implant losses.[5] Compromised bone may cause both early and late failures. With the ever-increasing number of manufacturers with innovative fixture designs and patients who accept the modality as a permanent rehabilitation for missing teeth, the greater research with the improved designs on the soft bone is the need of the hour. The present study was done to determine the survival of Maestro™ in the d3 and d4 jaw bone by evaluating annual peri-implant soft tissue health and the bone height around the implants. Because the bone is strongest in compression and 65% weaker in shear, a square thread shape is designed such that it results in 10 times less shearing force than with a conventional V-shaped thread.[6]
Materials and Methods
Fourteen patients (10 males and 4 females) were selected from the Out Patient Department of Periodontics, Bapuji Dental College and Hospital, Davangere, India on a written consent-to-treat agreement. The patients aged in the range of 18–50 years with a single missing tooth, well-compliant with the oral hygiene instructions and with good dental and general health; but who did not present with parafunctional habits, insufficient interarch space, diabetes and heavy smoking were subjected to Computerized Tomographic (CT) scanning as per the standard protocol.[7] The distance from contiguous tooth and proximity from the vital anatomical structures was assessed first. It is established in the literature that the d3 and d4 type is found mostly in the posterior maxilla,[2,8] anterior maxilla and posterior mandible.[2] As per the Hounsfield units calibration;[2] six, five and three cases were selected for the anterior maxilla, posterior maxilla and posterior mandible respectively [Figures 1 and 2]. Additionally, the pretreatment records included the periodontal status, diagnostic casts, periapical and panoramic radiographs, clinical photographs and surgical stent.
Figure 1.
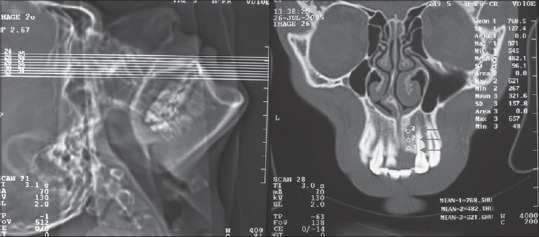
Computed tomography Case I: Scout view and bone density at proposed implant crestal (c), middle (M) and apical (A) level
Figure 2.
Computed tomography case II: Scout view and bonedensity at proposed implant crestal (c), middle (M) and apical (A) level
The preliminary impressions were made to fabricate a surgical guide stent. On the surgery day, the patients were covered with a surgical drape and were made to rinse with 10 ml of 0.2% chlorhexidine gluconate solution. This was followed by the surgical extraoral scrubbing with Betadine (5% povidine iodine). Under the appropriate block, a midcrestal incision was given to elevate the mucoperiosteal flap. The osteotomy was done using a NSK 20:1 gear reduction hand piece attached to ATR® physiodispenser at 1300 rpm starting speed under copious sterile saline irrigation [Figures 3-4].
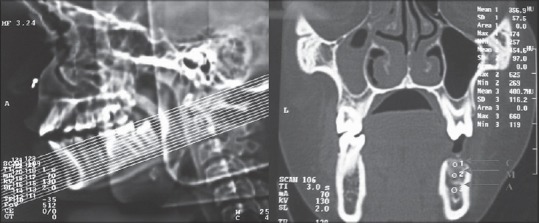
Figure 3.
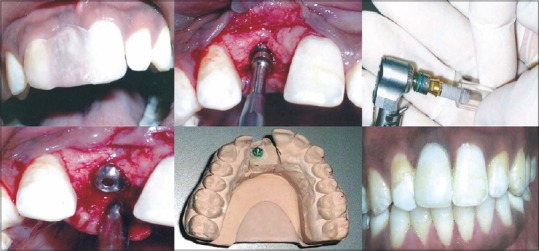
Case 1: Preoperative with stent, drilled osteotomy site, implant inserted, cover screw placed, crown fabricated on abutment, crown cemented
Figure 4.
Case 2: Pilot drill passed through stent, drilled osteotomy site, implant inserted, cover screw placed, flap repositioned, permucosal extension placed at uncovery stage, abutment milled for crown fabrication, crown delivered in occlusion
Following the drill sequencing on the manufacturer's instructions, the Maestro™ implants of selected size was removed from the sterile vial and engaged through a premounted abutment onto a hand piece adaptor. It was taken utmost care not to touch the implant and that no thread on the implant body is visible outside the bone crest. Thus, the final primary stability of the implant was checked at the end of the insertion. The particular system was opted for the study as it a root form, fine pitched threaded implant to provide a greater contact surface area. It is hypothesized that functional surface area will affect clinical health in poor-quality bone.[9] A 0.050” hex driver was used to remove the abutment mount and replaced with the cover screw. The flap was then repositioned, sutured and covered by a periodontal pack (COE pak™).
The cover screws were exposed after 4 and 6 months in mandible and maxilla respectively to be replaced by permucosal extension, followed by impressions with the medium viscosity Elite implant™ (Zhermack® Italy) using a custom tray; and the cemented metal-ceramic crown was delivered finally. The clinical parameters were analyzed statistically and a 3, 6, 9 and 12 months record of the modified plaque index,[10] gingival index,[11] modified sulcular bleeding index;[10] and clinical implant mobility scale[12] was done. The implant probing depth was checked using a True Pressure Sensitive® probe. The standardized long cone periapical radiographs using long cone were recorded similarly [Figure 5].
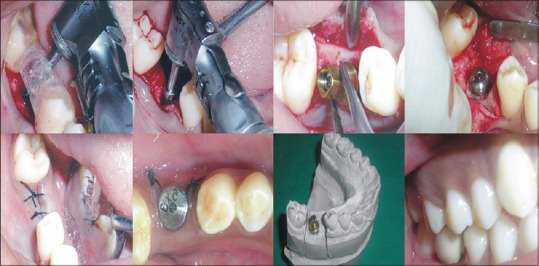
Figure 5.
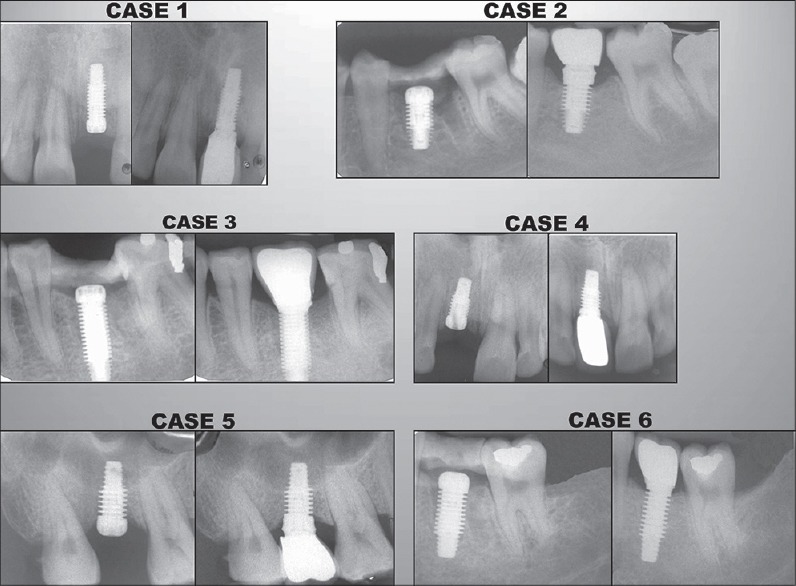
IOPA radiographs compared at implant placement with 12 months post-operative: Case1, case2, case 3, case 4, case 5; and case 6
Results
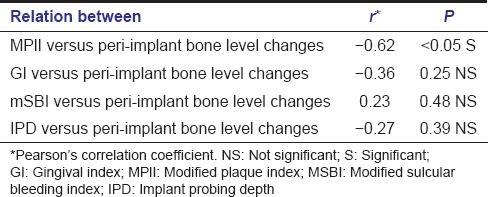
Out of the 11 implants placed in the maxillary and three in the mandibular jaw, one failed after 3 months. Out of the 13 cases included in the study, one dropped out and was excluded after 4 months. Plaque score [Table 1] and gingival index values [Table 1] showed a slight reduction at continuous intervals until 12 months postoperatively but was statistically insignificant. The mean sulcus bleeding score [Table 1] reduced to 0.12 ± 0.17 at the end of 1 year, which was statistically significant. There was a decreased mean implant probing depth [Table 2] from the baseline. The mean vertical bone level changes (combined mesial and distal) were reported reduced from 1.19 ± 1.35 mm at the baseline to 1.37 ± 0.89 mm at the end of 1 year. [Table 3]. Thus, a significant correlation was analyzed between the plaque index and the peri-implant bone loss [Table 4]; and an implant success of 92.3% in low-density bone in the study.
Table 1.
Posttreatment changes in modified plaque, GI and MSBI score
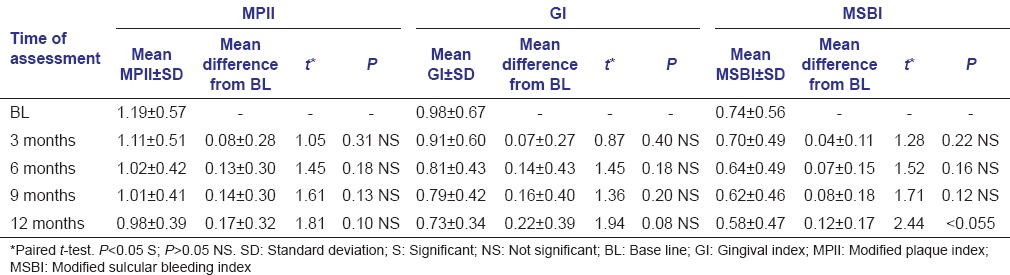
Table 2.
Posttreatment changes in IPD
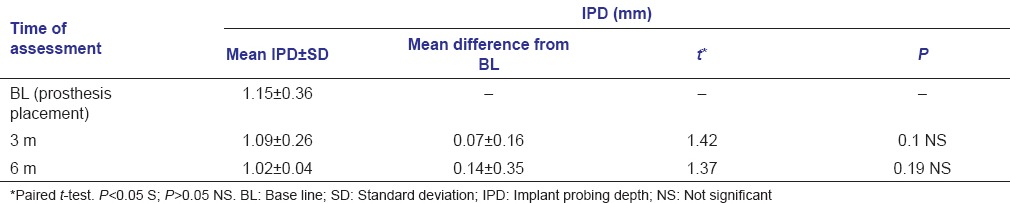
Table 3.
Radiographic peri-implant bone level assessment
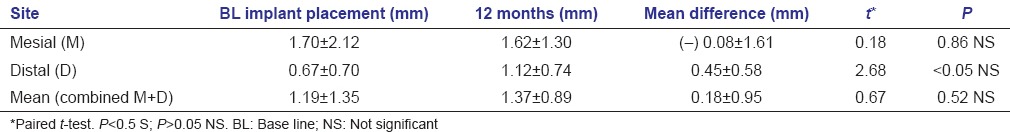
Table 4.
Relationship between clinical and radiographic parameters
Discussion
The criteria of success in implant dentistry remains complex. The implant with rigid fixation is said to be successful clinically if it is immobile, with the absence of associated pain, infections, neuropathy, and paresthesia.[12] A predictable survival in all the bone densities was evaluated previously using fixture from the system used in this study.[6] An implant or a tooth diagnosed as a clinical failure is easier to describe than one that is a success.
Although, implant failure can be attributed to many factors, most variables can be eliminated if accepted surgical procedures are followed. Bone quality is an exception. While the very dense bone at the implantation site can affect osseointegration by time of the osteotomy, the compromised bone, on the other hand, may cause both early and late failures.[5] In a landmark study, the authors reported a 35% Branemark's fixture loss in any region of the mouth when bone density was poor.[13] Similar results were observed by another author who reported 78% of failures in the soft bone types.[14] However, the present study refuted the hypothesis that implants are the least predictable in compromised host bone that was preassessed with CT scan in all patients.
Wide implants as were used in this study are advocated for the situation. In a study,[15] the authors claimed that the design alterations in the form of wide diameter fixtures were more suited to treat the areas of inadequate bone height, areas of poor bone quality and for the immediate replacement of nonosseointegrated implants. Unlike the original Branemark screw, which had a V-shaped thread pattern, the Maestro™ implant has a square crest and a flank angle of 3° that serves to decrease the shear force and increase compressive load.[16] A failure was reported in one case in our study. The patient was noncompliant to the attempt at tobacco cessation prior to inclusion in the study. The findings of the study corroborated with the previous retrospective evaluation, in which authors claimed an overall failure rate of 11.3% with Branemark systems implants placed in smokers.[17] The reason stated by the authors was that the smokers and ex-smokers had lower trabecular bone mineral content when compared to never-smokers.
Conclusion
An overall success of 92.3% and 100% success in posterior sites was evaluated 1 year postoperatively. Except for one case, which was deemed a failure, all the implants showed an absence of clinical mobility. A mean mesial peri-implant bone gain mesially, but slight average mean annual bone loss (0.18 mm with a standard deviation of 0.95) was reported. Within the limits of the study, a significant correlation between plaque index and the mean peri-implant annual bone loss was shown. A few more studies with the similar implant type and incorporating a larger sample size, as well as greater follow up post loading are needed in the future.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Misch CE. Density of bone: Effect on treatment plans, surgical approach, healing, and progressive boen loading. Int J Oral Implantol. 1990;6:23–31. [PubMed] [Google Scholar]
- 2.Misch CE. Bone density: A key determinant for clinical success. In: Misch CE, editor. Contemporary Implant Dentistry. St. Louis: Mosby; 1999. pp. 109–18. [Google Scholar]
- 3.Lekholm U, Zarb GA. Patient selection and preparation. In: Branemark PI, Zarb GA, Albrektsson T, editors. Tissue Integrated Prostheses. Chicago: Quintessence; 1985. pp. 199–209. [Google Scholar]
- 4.Misch CE. Bone character: Second vital implant criterion. Dent Today. 1988;7:39–40. [Google Scholar]
- 5.Esposito M, Hirsch JM, Lekholm U, Thomsen P. Biological factors contributing to failures of osseointegrated oral implants. (I). Success criteria and epidemiology. Eur J Oral Sci. 1998;106:527–51. doi: 10.1046/j.0909-8836..t01-2-.x. [DOI] [PubMed] [Google Scholar]
- 6.Misch CE, Dietsh-Misch F, Hoar J, Beck G, Hazen R, Misch CM. A bone quality-based implant system: First year of prosthetic loading. J Oral Implantol. 1999;25:185–97. doi: 10.1563/1548-1336(1999)025<0185:ABQISF>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Schwarz MS, Rothman SL, Rhodes ML, Chafetz N. Computed tomography: Part II. Preoperative assessment of the maxilla for endosseous implant surgery. Int J Oral Maxillofac Implants. 1987;2:143–8. [PubMed] [Google Scholar]
- 8.Sogo M, Ikebe K, Yang TC, Wada M, Maeda Y. Assessment of bone density in the posterior maxilla based on Hounsfield units to enhance the initial stability of implants. Clin Implant Dent Relat Res. 2012;14(Suppl 1):e183–7. doi: 10.1111/j.1708-8208.2011.00423.x. [DOI] [PubMed] [Google Scholar]
- 9.Strong JT, Misch CE, Bidez MW, Nalluri P. Functional surface area: Thread – form parameter optimization for implant body design. Compendium. 1998;19:4–9. [Google Scholar]
- 10.Mombelli A, Van Oosten MA, Schurch E, Lang NP. The microbiota associated with successful or failing osseointegrated titanium implants. Oral Microbiol Immunol. 1987;2:145–51. doi: 10.1111/j.1399-302x.1987.tb00298.x. [DOI] [PubMed] [Google Scholar]
- 11.Apse P, Zarb GA, Schmitt A, Lewis DW. The longitudinal effectiveness of osseointegrated dental implants. The Toronto study: Peri-implant mucosal response. Int J Periodontics Restorative Dent. 1991;11:94–111. [PubMed] [Google Scholar]
- 12.Misch CE. The implant quality scale: A clinical assessment of the health disease assessment of the health disease continuum. In: Misch CE, editor. Contemporary Implant Dentistry. 2nd ed. St Louis: Mosby; 1999. pp. 21–2. [Google Scholar]
- 13.Jaffin RA, Berman CL. The excessive loss of Branemark fixtures in type IV bone: A 5-year analysis. J Periodontol. 1991;62:2–4. doi: 10.1902/jop.1991.62.1.2. [DOI] [PubMed] [Google Scholar]
- 14.Engquist B, Bergendal T, Kallus T, Linden U. A retrospective multicenter evaluation of osseointegrated implants supporting overdentures. Int J Oral Maxillofac Implants. 1988;3:129–34. [PubMed] [Google Scholar]
- 15.Langer B, Langer L, Herrmann I, Jorneus L. The wide fixture: A solution for special bone situations and a rescue for the compromised implant. Part 1. Int J Oral Maxillofac Implants. 1993;8:400–8. [PubMed] [Google Scholar]
- 16.Boggan RS, Strong JT, Misch CE, Bidez MW. Influence of hex geometry and prosthetic table width on static and fatigue strength of dental implants. J Prosthet Dent. 1999;82:436–40. doi: 10.1016/s0022-3913(99)70030-2. [DOI] [PubMed] [Google Scholar]
- 17.Bain CA, Moy PK. The association between the failure of dental implants and cigarette smoking. Int J Oral Maxillofac Implants. 1993;8:609–15. [PubMed] [Google Scholar]


