Abstract
Objective:
To present an evidence-based case report on the prognosis of a patient with sciatica.
Case:
A 43-year-old man presented with right-sided buttock and lower extremity pain and numbness of 10 weeks’ duration. Magnetic resonance imaging revealed a lumbosacral disc herniation. Straight leg raise testing provoked the patient’s right sciatic pain, and neurologic examination revealed a diminished right Achilles tendon reflex and mild hypoesthesia along the patient’s outer right foot.
Outcome:
PubMed was searched and two cohort studies relevant to sciatic prognosis were found. These articles were critically appraised for their validity, importance, and applicability in making a prognostic estimate for this particular patient. Based on the appraised research evidence, and the confidence intervals calculated therein, the overall prognosis for sciatic pain recovery with conservative care was estimated as favourable for this patient, though sensory recovery (even with surgical care) was not.
Summary:
This case report illustrates how to use research literature in estimating the clinical prognosis for an individual patient, and how this can be useful towards clinical decision-making concerning treatment.
Keywords: sciatica, prognosis, chiropractic, evidence based practice, case reports
Abstract
Objectif :
Présenter une étude de cas fondée sur des éléments probants au sujet du pronostic d’un patient souffrant de sciatique.
Cas :
Un homme de 43 ans souffre de douleurs et d’engourdissements au niveau de la fesse droite et des membres inférieurs depuis dix semaines. L’imagerie par résonance magnétique permet de constater une hernie discale lombo-sacrée. Lorsqu’on lève la jambe, tenue droite, du patient, le mouvement provoque chez lui une douleur sciatique, et un examen neurologique permet de constater une perte de réflexe au niveau du tendon d’Achille droit et une légère hypoesthésie sur l’extérieur du pied droit.
Résultat :
À la suite d’une recherche dans PubMed, on a trouvé deux études par cohortes pertinentes sur le pronostic sciatique. Ces études ont fait l’objet d’un examen critique afin de déterminer leur validité, leur importance et leur applicabilité en matière de pronostic pour ce patient. Selon les preuves de recherche évaluées et les intervalles de confiance calculés, on a estimé le pronostic global de soulagement de la douleur sciatique au moyen de traitements conservateurs comme favorable pour ce patient, mais c’est l’inverse pour le rétablissement sensoriel (même avec des soins chirurgicaux).
Résumé :
Dans cette étude de cas, on montre la façon d’utiliser les ouvrages sur la recherche pour établir un pronostic clinique d’un patient, et l’utilité de cette approche par rapport aux décisions cliniques relatives au traitement.
Keywords: sciatique, pronostic, chiropratique, pratique basée sur des données probantes, études de cas
Introduction
Sciatica is a disorder characterized by radiating leg pain that follows a dermatomal pattern, accompanied at times by sensory symptoms.1 In about 90% of cases, it is caused by a herniated disc with nerve root compression, and generally is considered to have a favourable prognosis.1 However, most prognostic estimates of sciatica are based on data from individual studies, as systematic reviews on this topic are scarce. Moreover, evidence regarding specific prognostic factors for sciatic recovery, particularly in non-surgically treated patients, is conflicting.2 For the chiropractor, communicating patient prognoses is nevertheless a routine part of proper informed consent procedure.3 Presented here in an ‘evidence-based’ format,4 this case report will chronicle how research literature was used in estimating the clinical prognosis of a patient with a lumbar disc herniation and sciatica.
Case Report
A 43-year-old man presented with a chief complaint of right-sided buttock and lower extremity pain of 10 weeks’ duration. It began two days after working out at the gym. The pain was constant and described as if the nerves in his entire leg from the buttock down were being “pulled apart,” accompanied by “numbness” along his right posterolateral thigh, lower leg, and foot. The pain severity was graded as a seven out of 10; and his overall Bournemouth Questionnaire5 score totalled 40 out of 70, where zero equals no disability and 70 equals complete disability. The buttock and lower extremity symptoms were most intense first thing in the morning (e.g. when getting out of bed). Standing up and walking around was somewhat palliative. Other provocative features included prolonged sitting and/or twisting movements (e.g. turning over in bed and getting in/out of a car). Two weeks earlier, a magnetic resonance imaging (MRI) study had been performed, revealing a lumbosacral disc herniation with impingement of the right S1 nerve root (Figure 1). Because heat therapy and over-the-counter anti-inflammatories (Ibuprofen) had not provided any relief, his nurse practitioner had prescribed ice and a stronger anti-inflammatory drug (Celebrex), and referred him for chiropractic treatment.
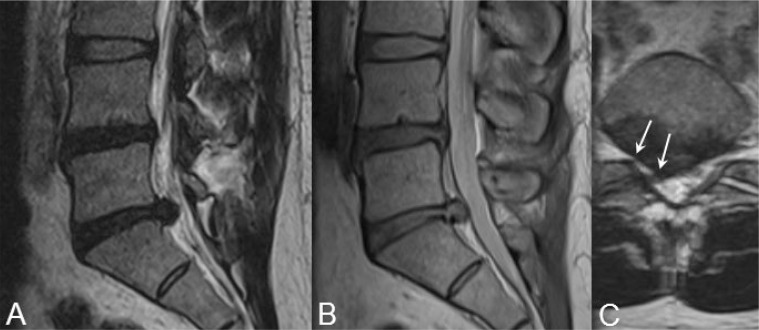
Figure 1.
T2-weighted (A) and proton density (B) sagittal MR images of the patient’s lower lumbar spine showing a contained intervertebral disc herniation at L5-S1. Mild-to-moderate disc dessication is also evident at both the L4–5 and L5-S1 levels. (C) T2-weighted coronal spot view of L5-S1 revealing a right paracentral disc protrusion, resulting in both displacement of the right S1 nerve root and intervertebral foraminal encroachment at L5-S1 on the right (arrows).
On examination, the patient’s lumbar spine range of motion was normal, except for some mild right-sided low back pain experienced during seated extension. Prone motion palpation of the lumbosacral and sacroiliac joints revealed bilateral hypomobility, along with pain and gluteal muscle spasm on the right. Hypertonicity was also noted within the right quadratus lumborum muscle. The Straight Leg Raise test6 (at approximately 30° of hip flexion) and the Yeoman’s test each elicited pain and paraesthesia down the patient’s right leg, while the Well Leg Raise, Double Leg Raise, Nachlas’, and Hibb’s tests were negative. Lower limb neurologic examination also revealed a diminished Achilles tendon reflex on the right (graded as +1), as well as mild hypoesthesia along the patient’s outer right foot (i.e. S1 dermatome). Based on his age, history, physical exam, and MRI findings, the working diagnosis was a right-sided lumbosacral disc herniation with sciatica.
Clinical Question
Cognitive dissonance refers to the mental and emotional responses experienced by a clinician when a patient scenario calls for knowledge that he/she does not possess.7 In this case, the author was uncertain about the prognosis for recovery in a patient with a lumbar disc herniation and sciatica. Clinical experience had taught that the natural course for this condition was variable – some patients improved, while others did not. Counselling such patients on expected outcomes, therefore, had often proved difficult. Adding to this uncertainty was the fact that the current patient had already been suffering with sciatica for 10 weeks. As a consequence, what was the likelihood that his symptoms would resolve? How long would it take? And would conservative treatment help, or would he require surgery? To answer these questions using an evidence-based approach, a more focused clinical question was needed.7 Because the main issue here was regarding prognosis, the following foreground question was posed: In a 43-year-old man with a lumbar disc herniation and sciatica, what is his prognosis for recovery with non-surgical/conservative care?
Using the mnemonic, PICO (i.e. Patient/problem, Intervention, Comparison, and Outcome[s] of interest),7 this question can be broken down as follows:
P = A 43-year-old man with sciatica.
I = Non-surgical/conservative care.
C = Natural course.
O = Prognosis for recovery.
Literature Search
The best evidence to answer a clinical question about prognosis is a systematic review of cohort studies.8 To begin, therefore, a search of the English language literature (from inception to March 5, 2014; limited to human studies) was conducted using the PubMed database. The medical subject headings ‘sciatica’ and ‘prognosis’ were combined using the Boolean operator ‘AND’, yielding 392 hits. After filtering the search to ‘systematic reviews,’ 23 total citations were produced. Based on their titles and abstracts, two of these were deemed pertinent.2,9 Inclusion criteria consisted of systematic reviews of cohort studies containing information on the prognosis of non-surgically treated patients with sciatica. Studies of surgical cohorts were excluded. Similar searches of the Cochrane Library and Cumulative Index to Nursing and Allied Health Literature were conducted, but no additional articles pertinent to this case were found. Therefore, two systematic reviews on the prognosis of conservatively treated patients with sciatica were identified and retrieved.
Critical Evaluation of the Evidence
Atop the hierarchy of research evidence are systematic reviews (Table 1).10 In the review on prognosis by Pengel et al.,9 15 articles of inception cohorts with acute low back pain or sciatica were evaluated. Upon further review, however, only one of these actually included patients with sciatica. In this sample, leg pain and disability decreased over the first month by an average of 69% and 57%, respectively. Unfortunately, no long-term follow-up data were obtained. In a more recent systematic review, Ashworth et al.2 evaluated seven prospective cohorts of non-surgically treated sciatic patients. The data on individual prognostic factors for recovery were conflicting, however; and the natural course of sciatica (short-term or long-term) was not assessed. Therefore, both systematic reviews were unable to adequately answer the current clinical question. As a consequence, the next highest level of evidence for prognosis was required – that of individual cohort studies.
Table 1.
A hierarchy of research evidence (adapted from Haneline10).
| Study designs (in decreasing order of evidence strength): |
|---|
|
For this, a quick PubMed search was conducted combining the medical subject heading ‘sciatica’ with the text words ‘natural course OR inception cohort study.’ This produced only 14 hits, but the first one11 appeared quite relevant to the current case. A second paper12 from this same inception cohort was also found in the ‘related citations’ section of PubMed. Before applying the results from these two studies to the current patient, however, they were first appraised according to the standards proposed by Sackett et al.7.
Are the results of these prognosis studies valid?
Both studies by Suri et al.11,12 used a prospective inception cohort design, and included a clearly defined sample of consecutive patients (n = 154) with MRI-confirmed lumbar disc herniation and sciatica. In order to capture those at a common and early point in the course of their disease, symptom onset upon entry to the study was 12 weeks or less. Patient follow-up was also sufficient, and was carried out over the course of two years. Data were obtained for 73%, 70%, and 77% of the entire cohort for motor weakness, sensory deficit, and pain/disability levels, respectively. (Follow-up rates >70% are within the range of those generally considered acceptable for epidemiologic cohort studies.13) The investigators also used validated patient-report outcome measures in their follow-up assessments. To reduce bias, the questionnaires were mailed to each patient for completion. Finally, some prognostic factors for sciatic recovery were identified in both studies, but further validation was required. Nevertheless (based on the above criteria), the results of both cohort studies were deemed valid.
Are the valid results of these prognosis studies important?
The results were deemed important for two reasons. First of all, they showed that the prognosis for sciatic pain and motor recovery with non-surgical treatment was good. Secondly using the data provided, 95% confidence intervals (CIs) could be calculated for the results (see Table 2). This is important from an evidence-based standpoint because from these, a clinician can estimate the likelihood of sciatic outcomes over time, including the precision of these prognostic estimates for an individual patient. For example, 81% (95% CI, 72–90%) of patients in this cohort experienced resolution of leg pain, defined as a pain-free period for ≥1 month, following non-surgical treatment.12 The average time to resolution was six months. Extrapolating these findings to the general population, one can be 95% confident that had the total population of sciatic patients with disc herniations been included in this study, between 72–90% of those undergoing non-surgical treatment would have recovered. By two years, ongoing muscle weakness was also reported by only 25% (95% CI, 15–35%) of those who, treated surgically or non-surgically, had a motor deficit at baseline.11 The prognosis for sensory recovery was not as good, however, as 47% (95% CI, 32–62%) of patients with baseline deficits reported continuing sensory loss at two-year follow-up.11 Twenty-five percent (95% CI, 15–35%) of those who underwent non-surgical treatment also reported a recurrence of leg pain within one year after resolution.12
Table 2.
Calculating a confidence interval (CI) around a measure of prognosis.7
| Clinical measure | Standard error (SE) | Calculation of SE and CI |
|---|---|---|
| Proportion (e.g. % of patients recovered from sciatica11) | SE = √ {p × (1-p) / n}
|
If p = 79/97 = 0.81 (or 81%)
|
Can we apply this valid, important evidence about prognosis in caring for our patient?
When comparing demographic and clinical characteristics, there were many similarities between the current patient and the study sample12,14 including age, clinical features (i.e. MRI-confirmed disc herniation with sciatica), duration of symptoms, and leg pain severity. Conservative treatment in the study sample12,14 also consisted of the following: education, physiotherapy, chiropractic, massage, over-the-counter and/or prescription drugs, and/or cortisone injections (if necessary); a minority of patients (n = 21) were referred for surgery. Within the current multidisciplinary context,15 the patient in this case would have had access to these same therapies as well. Based on all these factors, therefore, the results of the two cohort studies were deemed applicable.
Application of the Evidence
Using the aforementioned results and their calculated 95% CIs, an estimation of the patient’s sciatic prognosis was made. As for his leg pain, there was between a 72–90% chance he would recover within six months with non-surgical/conservative care;12 however, there was also between a 15–35% chance his pain would recur within a year.12 Concerning his sensory symptoms, there was between a 32–62% probability he would still perceive sensory loss, whether treated surgically or non-surgically, even after two years of follow-up.11 Thus despite a chance of recurrence, his overall prognosis for pain recovery with conservative care was good, though sensory recovery (even with surgical care) was not as good.
Evaluation of the Outcome
Because this case report was written as part of an ‘observation-only’ clinical placement,16 the above prognostic estimates were not actually communicated to the patient. Had they been, the discussion would subsequently have revolved around whether to treat him conservatively or to refer him for surgery. Currently, there is general consensus that in the absence of progressive neurologic deterioration, initial sciatic treatment should be conservative for at least 6–8 weeks.1 Early surgery may provide a faster recovery of leg pain, but no clear differences in outcome have been shown after one or two years.1,17 Similarly, Suri et al.11 found no significant differences in baseline characteristics or treatment outcome for patients treated surgically or non-surgically. Regarding efficacy of individual conservative therapies, no one type has been shown to be clearly superior to another (including no treatment) for sciatica.18 In this case and others, therefore, clinical experience and patient preference – hallmarks of evidence-based medicine7 – would be important features in the decision-making process.
Limitations
This case report has some limitations. First, only two cohort studies were selected for final appraisal; consequently, other articles relevant to the prognosis of sciatica and/or disc herniations may have been omitted (e.g. Jensen et al.19). Second, non-response bias in the studies by Suri et al.11,12 could have somewhat compromised the validity of their results. For instance, if all non-responders in their study had undergone non-surgical/conservative care without sciatic resolution (i.e. ‘worst-case’ scenario), only 79 out of 133 total patients would have actually recovered within that first year;12 the prognostic estimate of recovery would therefore have reduced from 81% (95% CI, 72–90%) to 59% (95% CI, 48–70%). In a ‘best-case’ scenario, however, if all non-responders had recovered, the recovery rate would have been as high as 115 out of 133 or 87% (95% CI, 80–94%). Finally, the prognostic estimates in this case report may not be generalizable to other chiropractic patients or practices. For example, the study cohort11,12,14 and current patient15 each presented within primary care medical facilities. Treatment in these settings may differ from that of more traditional chiropractic clinics. As such, the applicability of the aforementioned prognostic estimates may be limited toward these patients.
Summary
Prognostic information that is valid, precise, and generalizable can be very useful when counselling patients on the likely course of their disorder and/or when making decisions concerning treatment.7 As for sciatica, systematic reviews on its prognosis are few, and further validation studies on prognostic factors for non-surgically treated patients are needed. Nevertheless, the prognoses of pain and sensory recovery were estimated for a patient with a lumbar disc herniation and sciatica, in this case using evidence from two individual cohort studies.
References
- 1.Koes BW, van Tulder MW, Peul WC. Diagnosis and treatment of sciatica. BMJ. 2007;334:1313–1317. doi: 10.1136/bmj.39223.428495.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashworth J, Konstantinou K, Dunn KM. Prognostic factors in non-surgically treated sciatica: a systematic review. BMC Musculoskelet Disord. 2011;12:208. doi: 10.1186/1471-2474-12-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Standard of Practice S-013: Consent. Toronto: College of Chiropractors of Ontario; Available from: http://www.cco.on.ca/site_documents/S-013.pdf [Accessed 6 March 2014]. [Google Scholar]
- 4.Bolton JE. Evidence-based case reports. J Can Chiropr Assoc. 2014;58(1):6–7. [PMC free article] [PubMed] [Google Scholar]
- 5.Bolton JE, Breen AC. The Bournemouth Questionnaire: a short-form comprehensive outcome measure. I. Psychometric properties in back pain patients. J Manipulative Physiol Ther. 1999;22(8):503–510. doi: 10.1016/s0161-4754(99)70001-1. [DOI] [PubMed] [Google Scholar]
- 6.Evans RC. Illustrated Essentials in Orthopedic Physical Assessment. St. Louis: Mosby; 1994. [Google Scholar]
- 7.Sackett DL, Straus SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-based Medicine: How to Practice and Teach EBM. 2nd ed. London: Churchill Livingstone; 2000. [Google Scholar]
- 8.Miller PJ, Jones-Harris AR. The evidence-based hierarchy: is it time for change? A suggested alternative. J Manipulative Physiol Ther. 2005;28(6):453–457. doi: 10.1016/j.jmpt.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Pengel LHM, Herbert RD, Maher CG, Refshauge KM. Acute low back pain: systematic review of its prognosis. BMJ. 2003;327:323–325. doi: 10.1136/bmj.327.7410.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haneline MT. Evidence-Based Chiropractic Practice. MA: Jones and Bartlett Publishers Inc; 2007. [Google Scholar]
- 11.Suri P, Rainville J, Gellhorn A. Predictors of patient-reported recovery from motor or sensory deficits two years after acute symptomatic lumbar disk herniation. PM R. 2012;4(12):936–944. doi: 10.1016/j.pmrj.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Suri P, Rainville J, Hunter DJ, Li L, Katz JN. Recurrence of radicular pain or back pain after nonsurgical treatment of symptomatic lumbar disk herniation. Arch Phys Med Rehabil. 2012;93(4):690–695. doi: 10.1016/j.apmr.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fewtrell MS, Kennedy K, Singhal A, Martin RM, Ness A, Hadders-Algra M, Koletzko B, Lucas A. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Arch Dis Child. 2008;93(6):458–461. doi: 10.1136/adc.2007.127316. [DOI] [PubMed] [Google Scholar]
- 14.Suri P, Hunter DJ, Jouve C, Hartigan C, Limke J, Pena E, Li L, Luz J, Rainville J. Nonsurgical treatment of lumbar disk hernation: are outcomes different in older adults? J Am Geriatr Soc. 2011;59(3):423–429. doi: 10.1111/j.1532-5415.2011.03316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Langs Community Health Centre: About Langs. Available from: http://www.langs.org/about-langs/ [Accessed 5 December 2013].
- 16.MSc Advanced Professional Practice (Clinical Sciences) Anglo-European College of Chiropractic; Bournemouth: Available from: http://www.aecc.ac.uk/cpd/postgrad/app-clinical.aspx [Accessed 19 March 2014]. [Google Scholar]
- 17.Jacobs WCH, van Tulder M, Arts M, Rubinstein SM, van Middelkoop M, Ostelo R, Verhagen A, Koes B, Peul WC. Surgery versus conservative management of sciatica due to a lumbar herniated disc: a systematic review. Eur Spine J. 2011;20(4):513–522. doi: 10.1007/s00586-010-1603-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Luijsterburg PAJ, Verhagen AP, Ostelo RWJG, van Os TAG, Peul WC, Koes BW. Effectiveness of conservative treatments for the lumbosacral radicular syndrome: a systematic review. Eur Spine J. 2007;16(7):881–899. doi: 10.1007/s00586-007-0367-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jensen TS, Albert HB, Soerensen JS, Manniche C, Leboeuf-Yde C. Natural course of disc morphology in patients with sciatica: an MRI study using a standardized qualitative classification system. Spine (Phila Pa 1976) 2006;31(14):1605–1612. doi: 10.1097/01.brs.0000221992.77779.37. [DOI] [PubMed] [Google Scholar]