Abstract
Objective:
To present an evidence-based case report on the diagnosis of a patient with suspected lumbar spinal stenosis (LSS).
Case:
A 64-year-old man presented with signs and symptoms suggestive of LSS, but physical examination and diagnostic imaging findings were inconclusive. Other co-morbidities included diabetes, congestive heart failure, and left hip joint osteoarthritis.
Outcome:
PubMed was searched for systematic reviews of diagnostic studies on LSS. Two recent articles were found and appraised with respect to their validity, importance, and applicability in diagnosing the current patient. Copies of his magnetic resonance imaging were also obtained and used in combination with the appraised literature, including diagnostic test specificities and likelihood ratios, to confirm an LSS diagnosis.
Summary:
This case illustrates how research evidence can be used in clinical practice, particularly in the diagnosis of an individual patient.
Keywords: lumbar spinal stenosis, diagnosis, chiropractic, evidence based practice, case reports
Abstract
Objectif :
Présenter une étude de cas fondée sur des éléments probants au sujet d’un patient souffrant possiblement d’une sténose du canal rachidien lombaire (SCRL).
Cas :
Un homme de 64 ans s’est présenté avec des signes et des symptômes laissant croire à une SCRL, mais les résultats de l’examen clinique et de l’imagerie ne sont pas concluants. Le patient souffre de comorbidités, notamment du diabète, une insuffisance cardiaque congestive et de l’arthrose à la hanche gauche.
Résultat :
On a réalisé une recherche dans PubMed pour trouver des évaluations systématiques d’études diagnostiques sur la SCRL. On a trouvé et évalué deux récents articles afin d’établir leur validité, importance et applicabilité pour diagnostiquer le trouble de santé du patient en question. On a aussi obtenu et utilisé des copies des IRM en combinaison avec les ouvrages évalués, notamment la spécificité d’un test diagnostique et les rapports de vraisemblance, pour confirmer la SCRL.
Résumé :
Ce cas montre comment les résultats de recherche peuvent servir dans la pratique clinique, en particulier dans le diagnostic du trouble de santé d’un patient.
Keywords: sténose du canal rachidien lombaire, diagnostic, chiropratique, pratique basée sur des données probantes, études de cas
Introduction
The North American Spine Society defines lumbar spinal stenosis (LSS) as “a clinical syndrome of buttock or lower extremity pain, which may occur with or without back pain, associated with diminished space available for the neural and vascular elements in the lumbar spine.”1 When symptomatic, its characteristic provocative and palliative features include exercise or positionally induced neurogenic claudication (i.e. radiating leg pain with walking or prolonged standing) that is typically relieved with forward flexion, sitting, and/or lying down. Yet despite these characteristic features, there is no generally accepted “gold standard” for the diagnosis of LSS.2 Moreover, its radiographic findings often correlate poorly with patient symptoms.3 As a consequence, a wide range of clinical, electrodiagnostic, and radiological tests are used.4 Complicating matters are the various differential diagnoses for LSS such as vascular claudication, referred lumbar and/or radicular pain, compression fractures, and hip osteoarthritis, which commonly co-exist in older adults.3 For the chiropractor, an accurate diagnosis is important because it determines how these patients will be managed.
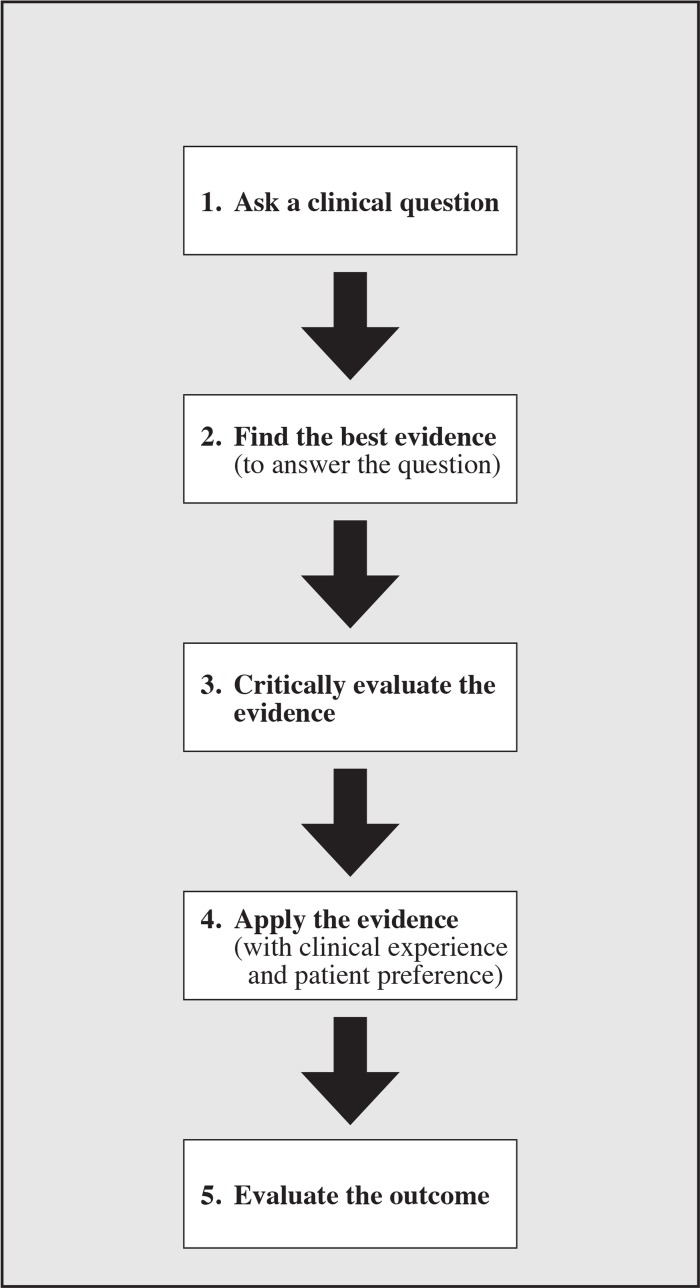
Using the five steps of evidence-based medicine5 (Figure 1), the following case report will demonstrate how current research literature informed the diagnosis of a patient presenting with suspected LSS.
Figure 1.
The five steps of evidence-based medicine (based on the model by Sackett et al.5).
Case Report
A 64-year-old obese man presented with a chief complaint of chronic left-sided low back and lower extremity pain. He described it as a constant ache down his leg to the mid-shin, accompanied by “pins and needles.” He also complained of “numbness” along his right anterolateral thigh. The pain severity on the left was graded between a six out of 10 at best and nine out of 10 at worst. His overall Back Bournemouth Questionnaire6 score totalled 58 out of 70, where zero equals no disability and 70 equals complete disability. Bending or twisting at the waist (e.g. shovelling or vacuuming), standing up from sitting, dancing, and prolonged standing were all described as provocative; topical analgesics, acupuncture, sitting, and riding an exercise bike were palliative. He originally injured his lower back eight years ago lifting heavy 10 kilogram metal frames at work. After re-injuring it again two years later, he was taken off work by his family physician, and had been on long-term disability ever since. A recent magnetic resonance imaging (MRI) study revealed multiple lower lumbar degenerative changes (as noted in the radiologist’s report), including a mild disc bulge at L3–4 and bilateral foraminal stenosis at L3–4 and L4–5. The patient had been taking daily oral analgesic (Percocet) and anti-inflammatory (Celebrex) medications; but because of ongoing lower back and leg pain, his physician referred him for chiropractic treatment.
On examination, he had difficulty getting out of a chair (i.e. Minor’s sign) and walked with an antalgic left-sided limp. His lumbar spine range of motion while seated was painful and limited by 50% in extension, 50% in left rotation, and 25% in right and left lateral flexion. Motion palpation revealed restricted sacroiliac joints, along with lumbar paraspinal and gluteal muscle spasm on the left. Several orthopaedic tests7 including the Straight Leg Raise, Double Leg Raise, Yeoman’s, and seated Kemp’s provoked his left-sided low back pain and leg pain, while Nachlas’ revealed tight quadriceps muscles, bilaterally. Lower limb neurologic exam including motor, reflex, sensory, Babinski, and vibratory testing was unremarkable, except for diminished Achilles tendon reflexes, graded as +1 on the right and 0 on the left.
Based on his age, history, and physical examination findings, the working diagnosis was LSS. Before a definitive diagnosis could be established, however, other co-morbidities with possible overlapping symptoms needed to be considered. For instance, his positive Straight Leg Raise and Double Leg Raise test results, along with reported MRI findings of L3–4 and L4–5 foraminal stenosis, suggested an underlying diagnosis of lumbar radiculopathy. His medical history included diagnoses of type II diabetes and congestive heart failure, making peripheral neuropathy and/or vascular claudication possible differentials. He also had a history of severe and painful left hip joint osteoarthritis, and was on a surgical wait list for total hip arthroplasty. The question for this patient, therefore (as far as his chiropractic management was concerned), was how to confirm a clinical diagnosis of LSS?
Clinical Question
To answer this, the following foreground question was posed: Based on this patient’s history and physical examination findings, how likely is it that he actually has (or does not have) LSS?
Using the mnemonic, PICO (i.e. Patient/problem, Intervention, Comparison, and Outcome[s] of interest),5 this question can be broken down as follows:
P = A 64-year-old man with suspected LSS.
I = Positive/negative history and physical examination findings.
C = None.
O = Diagnostic likelihood of LSS.
Literature Search
The best evidence to answer a clinical question about diagnosis is a systematic review of diagnostic studies.8 To begin, therefore, a search of the English language literature (from inception to January 27, 2014; limited to human studies) was conducted using the PubMed database. Because of interest in diagnostic studies, the subheading ‘diagnosis’ was selected under the medical subject heading ‘spinal stenosis,’ and this was combined using the Boolean operator ‘AND’ with the text word ‘lumbar.’ This search yielded 1,096 hits. After filtering the search to ‘systematic reviews’ from the past ‘10 years,’ 18 total citations were produced. Inclusion criteria consisted of systematic reviews containing current information on the accuracy of clinical diagnostic tests for LSS. Six of the retrieved studies were deemed potentially relevant based on their titles, and abstract review identified two as pertinent.3,4 Of the articles excluded, two were reviews of radio-graphic LSS parameters only,2,9 one was not a systematic review,1 and the other had been updated since its original publication.10 Therefore, two recent systematic reviews pertaining to the accuracy of clinical diagnostic tests for LSS were identified and retrieved. The entire literature search, including retrieval of manuscripts, took less than 30 minutes.
Critical Evaluation of the Evidence
In both systematic reviews retrieved,3,4 the clinical tests/symptoms found to be most useful in the diagnosis of LSS included the following: absence of pain when seated, improvement when bending forward, bilateral buttock or leg pain, neurogenic claudication, a wide-based gait, abnormal Romberg test, and a score of seven or higher on a diagnostic support tool of history and physical examination findings. (The corresponding sensitivities, specificities, likelihood ratios [LRs], and 95% confidence intervals [CIs] of all these tests are shown in Table 1; the ‘diagnostic support tool’ for LSS11 is shown in more detail in Table 2.) Before these results could be applied to the current patient, the two systematic reviews were first appraised using a template provided by Sackett et al.5 Specifically, the papers were appraised with respect to their (i) validity, (ii) importance, and (iii) applicability to the diagnosis of the current patient.
Table 1.
Diagnostic accuracy of history and physical examination findings for LSS.
| Clinical Finding | Sensitivity (95% CI) | Specificity (95% CI) | Positive LR (95% CI) | Negative LR (95% CI) |
|---|---|---|---|---|
| Absence of pain when seated3 | 0.47 (0.32–0.61) | 0.94 (0.85–1.00) | 7.4 (1.9–30) | 0.57 (0.43–0.76) |
| Improvement when bending forward3,4 | 0.52 (0.45–0.58) | 0.92 (0.88–0.95) | 6.4 (4.1–9.9) | 0.52 (0.46–0.60) |
| Bilateral buttock or leg pain3,4 | 0.51 (0.40–0.62) | 0.92 (0.87–0.97) | 6.3 (3.1–13) | 0.54 (0.43–0.68) |
| Neurogenic claudication3,4 | 0.82 (0.77–0.87) | 0.78 (0.73–0.83) | 3.7 (2.9–4.8) | 0.23 (0.17–0.31) |
| Wide-based gait3,4 | 0.42 (0.27–0.57) | 0.97 (0.91–1.00) | 13.0 (1.9–95) | 0.60 (0.46–0.78) |
| Abnormal Romberg test3,4 | 0.40 (0.25–0.54) | 0.91 (0.81–1.00) | 4.2 (1.4–13) | 0.67 (0.51–0.87) |
| Diagnostic support tool4 (LSS score ≥7) | 0.93 (0.89–0.96) | 0.72 (0.66–0.78) | 3.3 (2.7–4.0) | 0.10 (0.06–0.16) |
Table 2.
Prediction rule for identifying patients with LSS.11
| Clinical Finding | Risk score assigned | Risk score for current patient |
|---|---|---|
| History | ||
| Age (years) | ||
| • 60–70 | 1 | 1 |
| • >70 | 2 | 0 |
| Absence of diabetes | 1 | 0 |
| Neurogenic claudication | 3 | 3 |
| Exacerbation of symptoms when standing up | 2 | 2 |
| Symptom improvement when bending forward | 3 | 3 |
| Physical examination | ||
| Symptoms induced by having patients bend forward | −1 | 0 |
| Symptoms induced by having patients bend backward | 1 | 1 |
| Good peripheral artery circulation | 3 | Not performed |
| Abnormal Achilles tendon reflex | 1 | 1 |
| Straight leg raising positive for reproducing pain | −2 | −2 |
| Score interpretation | ||
| Score range | −2 to 17 | |
| Positive score | ≥7 | 9 |
(i) Are the results of these systematic reviews of diagnostic studies valid?
Both articles by Suri et al.3 and de Schepper et al.4 were qualitative systematic reviews of diagnostic studies. Both included a methods section that described finding and including all relevant studies, as well as an assessment of their individual validity. (Only diagnostic studies with clearly described clinical tests and reference standards were included.) Across these studies, a variety of diagnostic tests for LSS were evaluated; but between the two systematic reviews, there was consistency of results concerning the accuracy of these tests. Therefore based on the above criteria, the results of both systematic reviews were deemed valid.
(ii) Are the valid results of these systematic reviews important?
The results were deemed important for several reasons. First of all, the clinical findings listed in Table 1 were all found to be highly specific and some highly sensitive for LSS. Essentially, when a test or symptom has high specificity, a positive result will rule in the diagnosis.5 Likewise, a negative result for a test with high sensitivity will rule out the diagnosis. Secondly (when positive), these clinical findings were all shown to increase the likelihood of LSS by at least 3-fold or greater. LRs ≥2.0 have been considered to produce meaningful changes in the probsability of a given diagnosis.12 Thirdly, when the findings of ‘neurogenic claudication’ and the ‘diagnostic support tool’ are negative, the likelihood of LSS is reduced by 77% and 90% respectively. Finally because none of their CIs included the value of 1.0, these LRs were all shown to be statistically significant in the general population.5
(iii) Are the valid, important results of these systematic reviews applicable to our patient?
Each of the diagnostic tests listed in Table 1 were validated on LSS patients presenting to surgical and/or primary care medical clinics. Although LSS severity is expected to be high in these patient populations, the current patient also presented within a primary care setting,13 and was similar in age and symptomatology to those in the aforementioned studies. Therefore, the results from the systematic reviews were deemed applicable to this patient.
Application of the Evidence
Although gait analysis and Romberg testing were not performed, the current patient did exhibit several of the clinical findings listed in Table 1. These included an absence of pain when seated (LR 7.4; 95% CI, 1.9–30), improvement when bending forward (LR 6.4; 95% CI, 4.1–9.9), and neurogenic claudication (LR 3.7; 95% CI, 2.9–4.8). All three of these findings are highly specific for LSS, thereby ruling in the diagnosis. Using the diagnostic support tool11 shown in Table 2, the combined findings of age between 60–70, diabetes, neurogenic claudication, exacerbation of symptoms when standing up, symptom improvement when bending forward, provocation with bending backward, abnormal Achilles tendon reflexes, and a positive Straight Leg Raise, yielded a score of nine – a positive result (LR 3.3; 95% CI, 2.7–4.0). This finding also has good specificity for LSS. Furthermore, its LR can be interpreted and communicated to the patient as a 95% probability that he is between 2.7 and 4.0 times more likely to have LSS compared with a patient who tests negative with this diagnostic tool. The patient’s other LRs were interpreted in a similar manner.
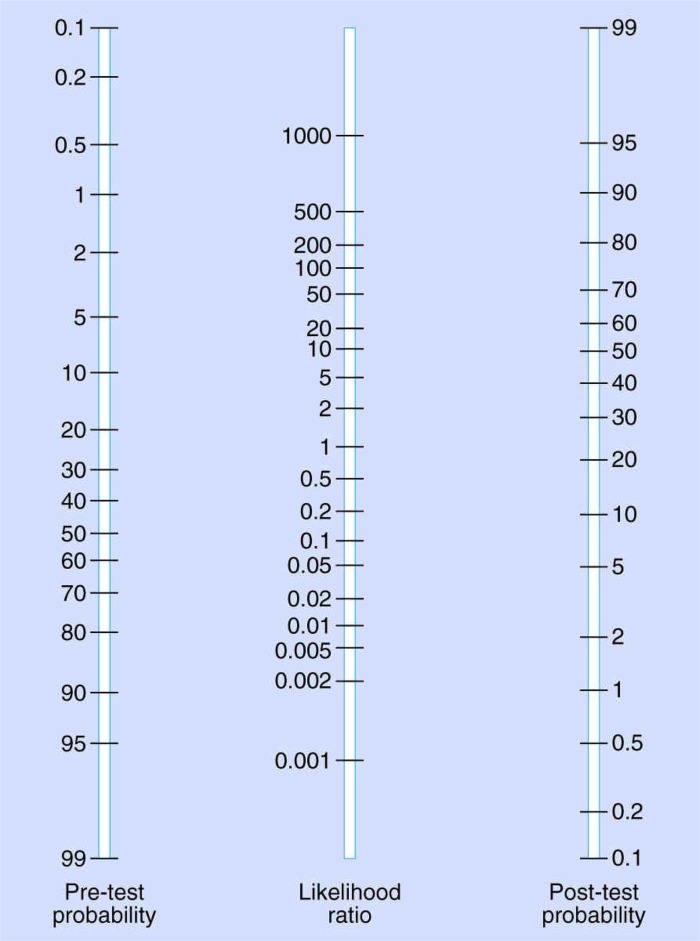
The post-test probability of actually having LSS was also determined using the patient’s positive LRs (see Figure 2). Depending on the diagnostic criteria used, the prevalence of radiographic LSS in the general population of adults’ aged 60–69 years ranges between 19.4% and 47.2%.14 Assuming a primary care clinic prevalence (or pre-test probability) of 19.4% and using only the finding of symptom improvement with sitting as an example, the probability of this patient’s LSS diagnosis would increase to approximately 70%. However, if the clinic prevalence of LSS were 47.2%, his post-test probability would be 90%. In either case, LSS was likely. To confirm the patient’s diagnosis, copies of his MR images were obtained, and these revealed further anatomical evidence of LSS (Figures 3 and 4).
Figure 2.
Nomogram for determining the post-test probability of a target disorder.5 To determine post-test probability, a line would be drawn between the patient’s pre-test probability (left), through the LR of the diagnostic test (centre), and extended through to the post-test probability (right). Source: reprinted with permission from D.L. Sackett, S.E. Straus, W.S. Richardson, W. Rosenberg, and R.B. Haynes, Evidence-Based Medicine, 2nd ed., p. 79, M. Parkinson, © 2000 Churchill Livingstone.
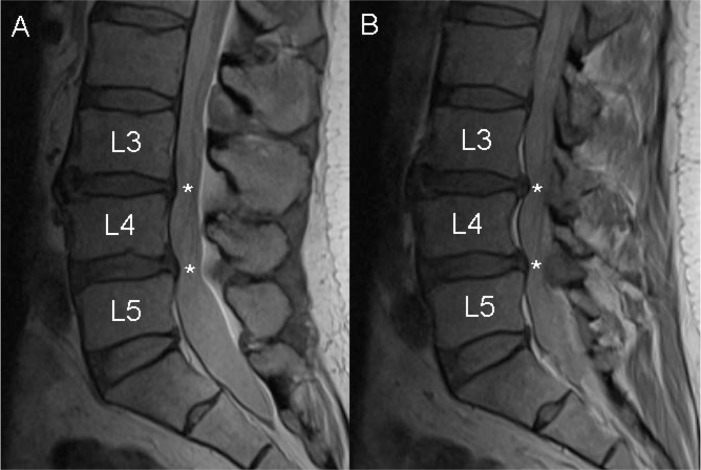
Figure 3.
Proton density sagittal (A) and left para-sagittal (B) MR images of the patient’s lumbar spine showing mild-to-moderate intervertebral disc dessication and protrusion into the thecal sac at L3–4 and L4–5 (asterisks).
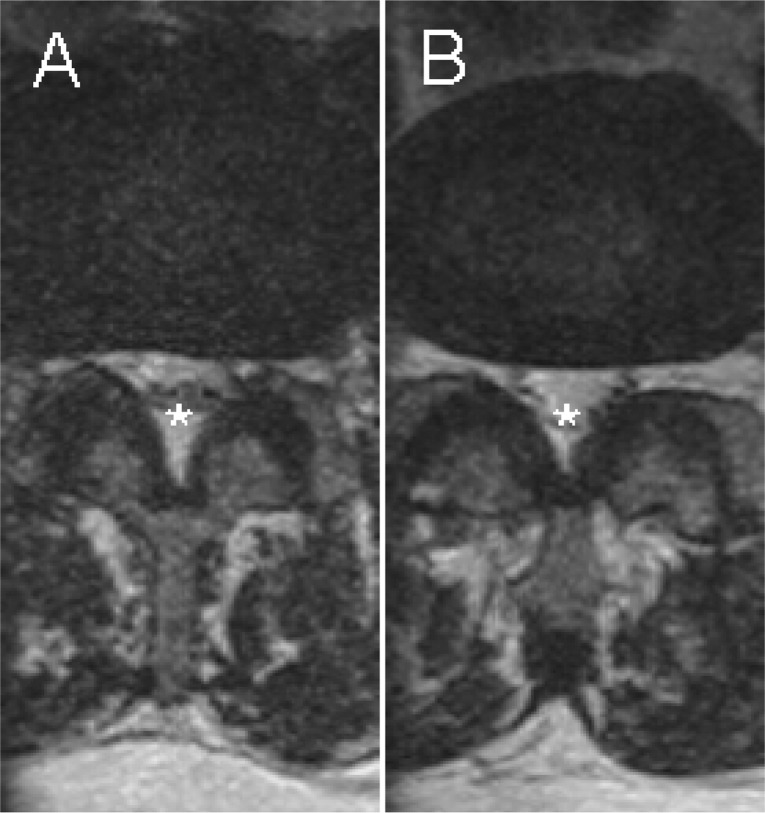
Figure 4.
T2-weighted coronal spot view MR images of L3–4 (A) and L4–5 (B) showing disc protrusion, bilateral facet joint osteoarthritis, and ligamentum flavum hypertrophy, with resultant central canal (asterisks), lateral recess, and intervertebral foraminal stenosis (most severe at L3–4), bilaterally.
Evaluation of the Outcome
Various conservative and surgical treatment options are available to patients with LSS.1 However, because this case report was written within the context of an ‘observation-only’ clinical placement,15 the author did not actually communicate a diagnosis (or plan of management) to the patient. (Instead, he was referred to one of the other chiropractors at the centre.) Nevertheless, this evidence-based case report illustrates how research literature can be retrieved relatively quickly, appraised, and used in the management of an individual patient.
Limitations
This case report has some limitations. Firstly, gait analysis and Romberg testing7 were not performed as part of the neurological exam on this patient. Though specific and predictive of LSS, the clinical findings of a ‘wide-based gait’ and ‘abnormal Romberg test’ would not have altered the patient’s final LSS diagnosis. Furthermore, in a recently published guideline16 the North American Spine Society has concluded that there is insufficient evidence regarding the diagnostic accuracy of the Romberg test for LSS. Secondly, the literature search for this case report was limited to PubMed. By not searching other databases such as the Cochrane Library and/or the Cumulative Index to Nursing and Allied Health Literature, other pertinent systematic reviews of diagnostic studies may have been missed. Thirdly, other systematic review appraisal checklists such as the Amstar17 were not employed in this case. Instead, the author relied on the template provided in the textbook by Sackett et al.5. Finally, the results of this case report may not be generalizable to other chiropractic patients or practices. For instance, this patient presented within a primary care, community health centre setting.13 Integrated chiropractic services such as this have only been described within one other city in all of Canada.18 What is more, many of the diagnostic tests highlighted in this case require further validation within non-specialized clinical settings,3 once again limiting these results toward other chiropractic patients.
Summary
According to Sackett et al.,5 “evidence-based medicine is the conscientious, explicit, and judicious use of the current best evidence in making decisions about the care of individual patients.” In this case, a 64-year-old man presented with signs and symptoms suggestive of LSS, including several co-morbidities. However, by using the results of two recent systematic reviews – and in particular, their specificities and LRs – a more accurate diagnosis of LSS was reached.
Footnotes
Consent: The patient has provided written consent to having his personal health information, including radiographs, published.
References
- 1.Watters WC, 3rd, Baisden J, Gilbert TJ, Kreiner S, Resnick DK, Bono CM, Ghiselli G, Heggeness MH, Mazanec DJ, O’Neill C, Reitman CA, Shaffer WO, Summers JT, Toton JF, North American Spine Society Degenerative lumbar spinal stenosis: an evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis. Spine J. 2008;8(2):305–310. doi: 10.1016/j.spinee.2007.10.033. [DOI] [PubMed] [Google Scholar]
- 2.Steurer J, Roner S, Gnannt R, Hodler J, LumbSten Research Collaboration Quantitative radiologic criteria for the diagnosis of lumbar spinal stenosis: a systematic literature review. BMC Musculoskelet Disord. 2011;12:175. doi: 10.1186/1471-2474-12-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suri P, Rainville J, Kalichman L, Katz JN. Does this older adult with lower extremity pain have the clinical syndrome of lumbar spinal stenosis? JAMA. 2010;304(23):2628–2636. doi: 10.1001/jama.2010.1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Schepper EIT, Overdevest GM, Suri P, Peul WC, Oei EHG, Koes BW, Bierma-Zeinstra SMA, Luijsterburg PAJ. Diagnosis of lumbar spinal stenosis: an updated systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 2013;38(8):E469–E481. doi: 10.1097/BRS.0b013e31828935ac. [DOI] [PubMed] [Google Scholar]
- 5.Sackett DL, Straus SE, Richardson WS, Rosenberg W, Haynes RB. Evidence-based Medicine: How to Practice and Teach EBM. 2nd ed. . London: Churchill Livingstone; 2000. [Google Scholar]
- 6.Bolton JE, Breen AC. The Bournemouth Questionnaire: a short-form comprehensive outcome measure. I. Psychometric properties in back pain patients. J Manipulative Physiol Ther. 1999;22(8):503–510. doi: 10.1016/s0161-4754(99)70001-1. [DOI] [PubMed] [Google Scholar]
- 7.Evans RC. Illustrated Essentials in Orthopedic Physical Assessment. St. Louis: Mosby; 1994. [Google Scholar]
- 8.Miller PJ, Jones-Harris AR. The evidence-based hierarchy: is it time for change? A suggested alternative. J Manipulative Physiol Ther. 2005;28(6):453–457. doi: 10.1016/j.jmpt.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 9.Andreisek G, Imhof M, Wertli M, Winklhofer S, Pfirrmann CW, Hodler J, Steurer J, Lumbar Spinal Stenosis Outcome Study Working Group Zurich A systematic review of semiquantitative and qualitative radiologic criteria for the diagnosis of lumbar spinal stenosis. AJR Am J Roentgenol. 2013;201(5):W735–W746. doi: 10.2214/AJR.12.10163. [DOI] [PubMed] [Google Scholar]
- 10.de Graaf I, Prak A, Bierma-Zeinstra S, Thomas S, Peul W, Koes B. Diagnosis of lumbar spinal stenosis: a systematic review of the accuracy of diagnostic tests. Spine (Phila Pa 1976) 2006;31(10):1168–1176. doi: 10.1097/01.brs.0000216463.32136.7b. [DOI] [PubMed] [Google Scholar]
- 11.Konno S, Hayashino Y, Fukuhara S, Kikuchi S, Kaneda K, Seichi A, Chiba K, Satomi K, Nagata K, Kawai S. Development of a clinical diagnosis support tool to identify patients with lumbar spinal stenosis. Eur Spine J. 2007;16(11):1951–1957. doi: 10.1007/s00586-007-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pinksy LE, Wipf JE, Ramsey SD. Evidence-Based Clinical Practice: Concepts and Approaches. Boston: Butterworth-Heinemann; 2000. [Google Scholar]
- 13.Langs Community Health Centre: About Langs. Available from: http://www.langs.org/about-langs/ [Accessed 5 December 2013].
- 14.Kalichman L, Cole R, Kim DH, Li L, Suri P, Guermazi A, Hunter DJ. Spinal stenosis prevalence and association with symptoms: the Framingham Study. Spine J. 2009;9(7):545–550. doi: 10.1016/j.spinee.2009.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.MSc Advanced Professional Practice (Clinical Sciences) Anglo-European College of Chiropractic; Bournemouth: Available from: http://www.aecc.ac.uk/cpd/postgrad/app-clinical.aspx [Accessed 19 March 2014]. [Google Scholar]
- 16.Kreiner DS, Shaffer WO, Baisden JL, Gilbert TJ, Summers JT, Toton JF, Hwang SW, Mendel RC, Reitman CA. An evidence-based clinical guideline for the diagnosis and treatment of degenerative lumbar spinal stenosis (update) Spine J. 2013;13(7):734–743. doi: 10.1016/j.spinee.2012.11.059. [DOI] [PubMed] [Google Scholar]
- 17.Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, Porter AC, Tugwell P, Moher D, Bouter LM. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007;7:10. doi: 10.1186/1471-2288-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baskerville NB, Keenan D. How Chiropractors began working in a Community Health Centre in Ottawa. J Can Chiropr Assoc. 2005;49(1):13–20. [PMC free article] [PubMed] [Google Scholar]