This review considers the potential utility of positron emission tomography (PET) tracers in the setting of response monitoring in breast cancer, with a special emphasis on glucose metabolic changes assessed with 18F-fluorodeoxyglucose. It discusses the different PET timing and metabolic criteria to define response that have been evaluated in previous studies. The development of new radiotracers of specific molecular pathways of breast cancer cells is also a challenging and promising research area.
Keywords: Breast, Cancer, Positron emission tomography, 18F-Fluorodeoxyglucose, Response, Monitoring
Abstract
This review considers the potential utility of positron emission tomography (PET) tracers in the setting of response monitoring in breast cancer, with a special emphasis on glucose metabolic changes assessed with 18F-fluorodeoxyglucose (FDG). In the neoadjuvant setting of breast cancer, the metabolic response can predict the final complete pathologic response after the first cycles of chemotherapy. Because tumor metabolic behavior highly depends on cancer subtype, studies are ongoing to define the optimal metabolic criteria of tumor response in each subtype. The recent multicentric randomized AVATAXHER trial has suggested, in the human epidermal growth factor 2-positive subtype, a clinical benefit of early tailoring the neoadjuvant treatment in women with poor metabolic response after the first course of treatment. In the bone-dominant metastatic setting, there is increasing clinical evidence that FDG-PET/computed tomography (CT) is the most accurate imaging modality for assessment of the tumor response to treatment when both metabolic information and morphologic information are considered. Nevertheless, there is a need to define standardized metabolic criteria of response, including the heterogeneity of response among metastases, and to evaluate the costs and health outcome of FDG-PET/CT compared with conventional imaging. New non-FDG radiotracers highlighting specific molecular hallmarks of breast cancer cells have recently emerged in preclinical and clinical studies. These biomarkers can take into account the heterogeneity of tumor biology in metastatic lesions. They may provide valuable clinical information for physicians to select and monitor the effectiveness of novel therapeutics targeting the same molecular pathways of breast tumor.
Implications for Practice:
18F-Fluorodeoxyglucose (FDG)-positron emission tomography (PET) is a molecular imaging exam. It can monitor breast cancer response to therapy earlier than the tumor shrinking observed with conventional imaging. This review focuses on the advantages and limits of FDG-PET for early determination of response, both in the neoadjuvant and metastatic settings. It discusses the different PET timing and metabolic criteria to define response that have been evaluated in previous studies. The development of new radiotracers of specific molecular pathways of breast cancer cells is also a challenging and promising research area to monitor the effectiveness of the new target treatments emerging in breast cancer.
Introduction
Positron emission tomography (PET) allows noninvasive visualization and quantitative assessment of many biologic processes that are modulated during therapy of breast cancer. Of these, evaluation of glucose metabolism with 18F-fluorodeoxyglucose (FDG) is the most widely used and has an evolving role in breast cancer management [1]. Because glucose metabolic changes occur earlier than tumor shrinking [2], the ability of FDG-PET to predict treatment response in individual patients has been an active field of research for many years, particularly in the neoadjuvant setting. For the same reason, but also in the context of the heterogeneity of breast cancer metastases, FDG-PET/computed tomography (CT) has been implemented in the follow-up of metastatic breast cancer. In all cases, accurate early differentiation of responders from nonresponders using FDG-PET/CT is clinically relevant to avoid unnecessary drug toxicities and to allow an early switch of noneffective treatment.
Besides FDG, new radiotracers of specific molecular pathways of breast cancer have recently emerged. These biomarkers of receptor expression, tumor cell proliferation, or angiogenesis may provide valuable clinical information to select the most efficient treatment and to monitor the effectiveness of novel therapeutics.
Materials and Methods
We searched for studies that evaluated the value of PET for monitoring the response to therapy of breast cancer. The search was performed using the electronic database PubMed (http://www.pubmed.com) until May 2014. The search strategy included the keywords “PET” or “PET/CT”; “breast cancer” or “breast carcinoma”; “response” or “monitoring”; “neoadjuvant” or “primary” or “metastatic”; “chemotherapy” or “hormone therapy” or “endocrine therapy”; “HER2” or “triple negative” or “luminal”; “18F-FDG” or “FDG” or “FES” or “FLT” or “15O-water”; and “glucidic metabolism” or “blood flow” or “angiogenesis.” Studies were considered eligible if they included women with breast cancer who were initiated with chemotherapy or endocrine therapy either in the neoadjuvant or metastatic settings with baseline and interim PET. Both prospective and retrospective studies were included on the condition that they were published in English in a peer-reviewed journal. Except for the ACRIN 6688 and ZEPHIR trials, both presented at the 2014 American Society of Clinical Oncology (ASCO) meeting, unpublished data, case reports, abstracts, and letters were not sought.
We screened the titles and abstracts of all potentially relevant articles to determine eligibility. All studies matching the eligibility criteria were retrieved, and bibliographies were checked for other relevant publications. The bibliographies of relevant review articles were also hand-searched to identify additional studies. If few articles were available on a precise question being address in the present review, they are mentioned. If many articles were eligible, only the ones considered to be “major articles” are mentioned. Articles were considered major either because they correspond to first pilot studies that were later corroborated, because of their good design and high impact factor of the journal in which they were published, or because of a relatively higher number of women included compared with other studies. We also searched for meta-analysis.
Although systematic literature search protocols were applied to provide an overview of the area of the present subject, the PRISMA Statement guidelines could not be entirely applied because of the extended field of the topic, the methodological heterogeneity in the literature existing, and the lack of evidence on this subject. Moreover, combining data from these heterogeneous studies would not have been appropriate.
FDG-PET in the Neoadjuvant Setting
Neoadjuvant chemotherapy (NAC) is used in large but operable breast cancer to downstage the primary tumor and increase the rate of breast conservative surgery [3, 4]. NAC also provides the opportunity to evaluate in vivo the breast tumor sensitivity to therapeutics. Women who achieve a pathological complete response (pCR) in the breast and axillary nodes at the end of NAC seem to have significantly improved survival [5, 6]. However, this conclusion depends on breast cancer subtype [6]. Thus, pathological examination at the end of NAC has been used as a surrogate of survival for assessing treatment efficacy, but pathological response cannot be determined until surgery. An earlier tumoral response assessment could allow for adjusting the treatment to the individual tumor response during NAC.
Because of delayed tumor shrinking and difficulties in differentiating residual fibrosis from active tumor, conventional imaging (CI) is of limited accuracy to assess the response to NAC [2]. Because glucose metabolism is increased in breast cancer, the monitoring of the metabolic response with FDG-PET has been proposed for the early prediction of pCR [7–15]. PET uptake measures can provide a continuous indicator of response and carries information beyond the standard dichotomous evaluations usually used in other response assessments. Although interesting papers published by Dunnwald et al. [16] have shown that FDG uptake kinetic analysis may hold an advantage over static uptake measures for response assessment, the most-used parameter is the percentage decrease of the tumor maximal standard uptake value (SUV) between baseline and post-treatment exam (ΔSUV). Indeed, this parameter is easier to measure than FDG kinetic parameters in routine practice and is more reproducible among centers than absolute SUV values [17]. A study by Schwarz-Dose et al. [12], prospectively including 104 women, found that a ΔSUV superior to 45% after the first cycle predicts a pathological response with a sensitivity of 73%, a specificity of 63%, a positive predictive value (PPV) of 36%, and a negative predictive value (NPV) of 90%. Similar results were found after the second cycle of NAC, using a threshold of 55%.
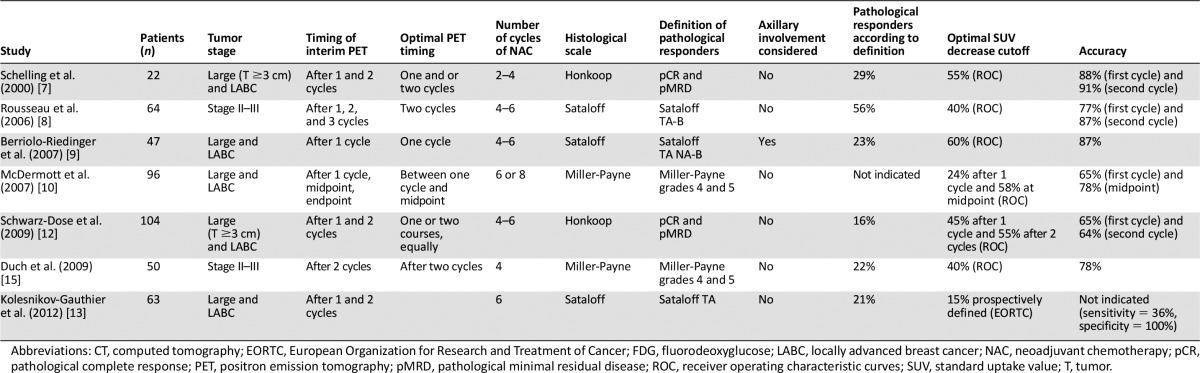
Three meta-analyses were published [18–20]: results indicate that FDG-PET has reasonable sensitivity to make early predictions regarding histopathological response to NAC in breast cancer, all tumor subtypes included. Mghanga et al. [20] included 15 studies (745 patients). The pooled sensitivity, specificity, PPV, and NPV were 80.5%, 78.8%, 79.8%, and 79.5%, respectively. Mghanga et al. concluded that FDG-PET is valuable for early monitoring of breast cancer response to NAC, with a trend toward a higher sensitivity after the second course than after the first course. This meta-analysis also underlined the great heterogeneity of the monocentric studies. Indeed, the definition of the pathological response largely varies from one study to another, considering or not axillary lymph nodes involvement (Table 1). Differences in PET timing were also observed. Consequently, the thresholds of ΔSUV to define metabolic response largely differ across studies, ranging from 40% to 88% SUV decrease (Table 1). In addition to the predictive value of FDG-PET, this exam also carries an independent prognostic value: a high tumor SUV can help discriminate patients at high risk of tumor relapse [21, 22].
Table 1.
Some of the studies evaluating the predictive value of ΔSUV with FDG-PET (/CT) on tumor pathological response at the end of neoadjuvant chemotherapy
Since the original works published by Sorlie and Perou [23–26], gene expression profiling has led to a new molecular classification of breast cancer. A more easy-to-use, biology-based classification has arisen in clinical practice [27–30]. Both classification systems demonstrated distinct breast cancer subtypes with predictive and prognostic significance. The influence of these entities on the tumor metabolic behavior became a matter of interest.
At baseline, FDG avidity correlates with high tumor grading, high mitotic activity, negative hormonal receptor status, tumor proliferation index assessed with Ki-67: it is thus a marker of tumor aggressiveness [9, 31]. A first paper of our institution, confirmed by other studies, demonstrated that both the tumor metabolism at baseline and the metabolic response after the first cycle of treatment are highly dependent on the tumoral subtype [32–34]. Thereafter, different metabolic patterns have been identified in each of the three main biologic subtypes of breast cancer.
HER2-Positive Subtype
Approximately 20% of invasive breast cancers overexpress human epidermal growth factor 2 (HER2). This subtype is highly proliferative, but its prognosis has been strongly improved with the advent of trastuzumab [35–37]. Because new therapies are available in this subtype (i.e., dual anti-HER2 blockage, the addition of an antiangiogenic drug), the early identification of poor-responding women after a first line of trastuzumab/cytotoxic drugs is an important clinical issue.
Initial results were conflicting because two studies demonstrated a good value of early FDG-PET/CT to predict pCR [38, 39], contrasting with the results of Koolen et al. [40, 41]. The two positive studies found that absolute residual SUV at interim PET was the best predictive marker. Groheux et al. [38] found that a tumor and axillary SUV <3.0 after two cycles of NAC was a good predictor of a pCR (PPV = 92%, NPV = 88%, accuracy = 90%). Although Humbert et al. [39] found tumor SUV <2.1 to be the optimal cutoff after the first cycle (PPV, NPV, and accuracy = 76%). Contrary to Humbert et al., trastuzumab was introduced after four cycles of NAC in Groheux’s study, explaining the lower early tumor response. Both studies found a lower predictive value of ΔSUV. Nevertheless, the strength of ΔSUV is to be less affected by technical factors than absolute SUV and to be more reproducible among centers in multicentric trials [17], and its predictive value can be improved by the exclusion of low metabolic tumors at baseline [39].
The neo-ALTTO study enrolled women with HER2+ breast cancer and compared metabolic response to neoadjuvant lapatinib and/or trastuzumab. In 66 women, FDG-PET/CT was performed at baseline; at weeks 2 and 6, pCR rate was twice as high for PET responders than nonresponders (week 2: 42% vs. 21%, p = .12; week 6: 44% vs. 19%, p = .005). The authors concluded that FDG-PET/CT is efficient for monitoring the tumor response to neoadjuvant anti-HER2 therapy alone [42].
Coudert et al. [43] planned the AVATAXHER multicentric phase 2 randomized trial to assess the benefit of adding bevacizumab after the second cycle of treatment in women who responding poorly (ΔSUV <70%) to trastuzumab/docetaxel. The addition of bevacizumab for women with a poor metabolic response increased the pCR rate from 24% to 43.8%. This is the first study suggesting that tailoring the NAC regimen to the early metabolic response might be of clinical benefit. The prognostic value of the metabolic response in this subtype has not been evaluated yet.
Triple-Negative Subtype
Approximately 15% of breast cancers are triple-negative (negative estrogen and progesterone receptors, no HER2 overexpression) [44]. It is a highly chemosensitive subtype with a pCR frequently reached, but the prognosis remains poor, particularly when pCR is not achieved at the end of NAC [6, 45, 46].
This aggressive subtype has the highest baseline SUV [32, 33, 47]. In the recent study of Groheux et al. [48], 50 patients were included. Interim FDG-PET/CT was performed after the second course of NAC. The mean ΔSUV of the primary tumor was −72% in the pCR group versus −38% in the non-pCR group (p < .0001). Using a 50% cutoff, ΔSUV was the best PET parameter to predict pCR, corroborating previous results [40, 49]. Interim PET was also associated with patient outcome: the 3-year event-free survival was 77.5% in metabolic responders (ΔSUV ≥ 42%) versus 47.1% in nonresponders (ΔSUV <42%).
The main limit is the heterogeneity of the NAC regimen used across studies and the usual switch to another regimen at midpoint of NAC in triple-negative (TN) breast cancer. Two previous studies showed that ΔSUV is dependent on the type and sequence of drugs used [32, 50]. Therefore, the observed metabolic response may not be sustained after the switch. Care must be taken when interpreting FDG-PET in settings of TN women with a midcourse switch.
Luminal/HER2-Negative Subtype
Despite a favorable prognosis, the luminal subtype usually has a low chemosensitivity. pCR is rarely achieved [29], and an intermediate tumor reduction allowing a conservative surgery is a more reasonable aim. Because NAC is controversial in this low chemosensitive subtype, there is a need for early biomarker to predict which luminal tumors will respond to NAC.
When primary tumor has a low pretherapy uptake, the ability of PET to detect it and to assess its response is limited [10, 51]: this limitation is usually observed in the luminal/HER2 subtype, which has the lowest baseline SUV and ∆SUV [32, 33]. Moreover, because pCR is rare in this subtype, previous studies failed to demonstrate its prediction with FDG-PET [41, 52, 53]. Koolen et al. [41] found that ΔSUV was predictive of “near pCR,” allowing few scattered cells, but the prognostic value of this definition is controversial [6]. In this subtype, the metabolic tumor volume could be more accurate than the SUV to predict the response [52, 54].
Because pCR is very uncommon, a study of our institution directly assessed the prognostic value of PET [53]. We demonstrated that tumor metabolism at baseline, and changes after the first course were early surrogate markers of 5 years of patient survival, independently of the pathologic response. We were able to identify a subgroup of patients with a high risk of relapse (5-year relapse-free survival [RFS] of 33%) based on a high baseline tumor metabolism and a low metabolic response following one cycle of chemotherapy. In contrast, patients with a low baseline tumor metabolism or a high baseline tumor metabolism followed by a good metabolic response had a low risk of relapse (5-year RFSs of 93% and 88%, respectively). Moreover, the baseline tumor metabolism was strongly correlated with tumor proliferation index: low-metabolic luminal tumors had low Scarff-Bloom-Richardson grade and Ki-67 expression, contrary to hypermetabolic ones, which presented increased proliferation indexes and mainly belonged to the luminal B subtype.
FDG-PET in the Metastatic Setting
Contrary to the neoadjuvant setting, the pathological response generally cannot be obtained in the metastatic setting. Because a change in tumor size is an indicator of outcome in the treatment of many solid tumors [55], it is the most frequently used surrogate endpoint to evaluate therapeutic effects in metastatic disease. Anatomic imaging is used for this purpose (predominantly ultrasound, CT, or magnetic resonance imaging [MRI]). The Response Evaluation Criteria in Solid Tumors (RECIST) have been defined [56] and updated [57] to standardize this response assessment.
However, criteria based on the size of tumors are limited because new targeted therapies are more cytostatic than cytotoxic. Moreover, change in tumor size is also not a good surrogate of bone lesion response, and the RECIST 1.1 criteria specify that bone lesions without soft tissue components cannot be considered as measurable [57]. This is a major limitation because bone is the preferential site of breast cancer metastases [58, 59].
In order to overcome this problem, the University of Texas M.D. Anderson Cancer Center has developed more specific response criteria for bone metastases response monitoring (MDA Criteria), combining quantitative (size measurement) and qualitative (sclerotic bone reaction) assessments [60, 61]. Despite such efforts, Hayashi et al. [62] found that the MDA criteria predicted progression-free survival at 6 months, but not earlier. Indeed, because morphologic imaging does not directly reflect tumor cell viability, but rather the secondary effect on bone adjacent tissue, morphologic changes are often delayed during chemotherapy [63] and do not seem to correlate with the presence of residual active tumor [64]. Moreover, a “flare” reaction can be assessed on CT or bone scan, corresponding to the sclerotic healing (Fig. 1), making the response evaluation difficult [60, 65].
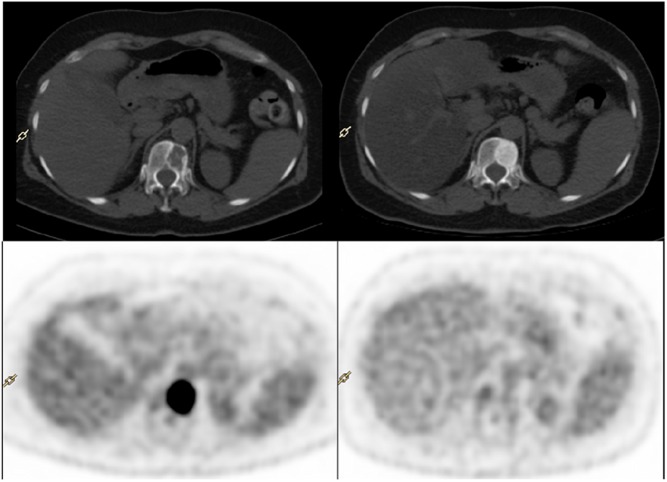
Figure 1.
Example of fluorodeoxyglucose-positron emission tomography (PET)/computed tomography (CT) exam before (left) and after (right) 3 months of eribulin and trastuzumab therapy in a woman with an osteolytic metastases of breast cancer, located on TH12 . After treatment, CT showed an important sclerotic reaction of the bone lesion, whereas PET showed no more metabolic activity. Both the anatomic and molecular imaging are in favor of a good response to systemic treatment.
In contrast, PET reflects cellular and molecular changes of tumor cells occurring before tumor shrinking, as demonstrated in 1993 by Wahl et al. [2]. In 2002, Stafford et al. [66] published preliminary results showing that changes in tumor FDG uptake with therapy were correlated with the overall clinical assessment of response (p < .01) and concluded that serial FDG-PET can help in bone response assessment. This was corroborated by Schwarz-Dose et al. [67], who included 11 patients with 26 metastatic lesions in first-line therapy: metabolic tumor changes, evaluated after the first and second courses of chemotherapy, correctly predicted the final clinical response in all women. Regarding the optimal timing for interim PET, Couturier et al. [68] had conflicting results: they found that PET changes after the third cycle of chemotherapy, but not after the first, predicting the clinical response after six cycles and overall survival. Tumor metabolic early change as a surrogate of survival in bone-dominant metastatic breast tumor response was later confirmed by Specht et al. [69]. A greater than 41% decline in SUV of the most hypermetabolic lesion at baseline was associated with a longer time to progression (p < .005). However, this study was retrospective with a large interval between PET exams ranging from 1 to 17 months. Cachin et al. [70] also found that a complete PET response after completion of high-dose chemotherapy (maximum three cycles) can more powerfully stratify for survival than conventional imaging (including CT).
Later, the development of integrated FDG-PET/CT has improved the accuracy of the response evaluation beyond that achievable by PET alone by adding information on bone morphological changes, particularly interesting for bone metastases (Fig. 1). Indeed, FDG uptake reflects the metabolic feature of bone metastases independently of their CT pattern (osteoblastic and osteoclastic) [64].
Tateishi et al. [71] retrospectively compared the prognostic value of morphologic and metabolic changes in bones metastases in patients with metastatic breast cancer, both evaluated with a FDG-PET/CT. One hundred and two women treated with first-line hormone-chemotherapy were included. PET/CT was performed at baseline and after treatment (mean: 28 days; range: 21–38 days). Only the metastatic lesion that exhibited the most substantial uptake was selected as the target lesion for response. Results showed that an increase in CT attenuation and a decrease in SUV of bone metastases were associated with response duration. Multivariate analysis showed that a decrease in SUV of 8.5% or more was the only significant predictor of long response duration. This ΔSUV threshold differs from that of Specht’s study (41%), possibly in relation with the difference of time between PET exams [69].
Thus, many studies have demonstrated that FDG-PET/CT is more accurate than morphologic CI for early monitoring of response to therapy, with a good prognostic stratification [64, 71]. FDG-PET/CT may emerge as a standard of care in bone metastatic breast cancer.
Evaluation of Response to Endocrine Therapy
Endocrine therapy is an efficient and low-toxicity treatment in metastatic hormone-positive (HR) breast cancer. It is often used as the first line treatment [72], but only 30%–50% of women with HR+ metastatic disease respond to first-line hormonotherapy [73, 74]. It may be explained by the heterogeneity of HR expression in the metastases, the sampling error of a one-site biopsy, and the presence of nonfunctional estrogen receptors (ERs). Thus, identification of other predictive biomarkers of the tumor hormone sensitivity remains an important clinical issue.
In responding tumors, an early increase in FDG uptake has been described 7–10 days after introduction of tamoxifen therapy [75]. This metabolic flare reaction may be explained by an initial increase in cell growth caused by an agonist effect of therapy and implies that ERs are functional. Thus, it is an early predictor of tumor sensitivity to endocrine therapy [75, 76]. In contrast, because antiaromatase therapy lowers estradiol level and thus reduces the tumor agonist effect, responding patients shows an early drop in tumor FDG uptake after antiaromatase induction [77]. Dehdashti et al. [78] demonstrated that an estradiol challenge (30 mg of estradiol), initiated before the antiaromatase therapy, can restore the metabolic flare that both predicts tumor response and longer overall survival. Only one study has evaluated the relevance of FDG-PET/CT for the delayed monitoring of metastatic breast cancer treated with endocrine therapy. PET/CT exams were performed at baseline and after 10 ± 4 weeks [79]. Using cutoffs of 25% SUV increase or decrease, progressive, stable, and partial metabolic response disease showed median progression-free survival times of 6, 27, and 20 months, respectively (p < .0001). FDG-PET/CT can thus be used for the delayed monitoring of response to hormone therapy, usually indicated for bone-dominant metastatic cancer, in which morphological modalities often fail to assess tumor response [60, 64].
Because antiaromatase therapy lowers estradiol level and thus reduces the tumor agonist effect, responding patients shows an early drop in tumor FDG uptake after antiaromatase induction. Dehdashti et al. demonstrated that an estradiol challenge, initiated before the antiaromatase therapy, can restore the metabolic flare that both predicts tumor response and longer overall survival
Limitations
All the studies previously mentioned were monocentric, and most of them were retrospective. They suffer from a lack of consensus on the optimal PET timing and metabolic criteria to use for response evaluation, compared with RECIST. Consequently, the 2012 NCCN Guidelines have pointed out this lack of standardization as a key limitation for using FDG-PET/CT in the metastatic setting of breast cancer, emphasizing the need of further prospective studies [80].
Currently, two sets of response criteria using PET are available: those developed by the European Organization for Research and Treatment of Cancer [81] and the PET Response Criteria in Solid Tumors (PERCIST) [82]. These criteria are still matters of debate. One first critical point is that the metabolic response is highly influenced by the cancer genomic and immunohistological subtype and by the treatment [32]. The optimal criteria therefore need to be adapted to each situation.
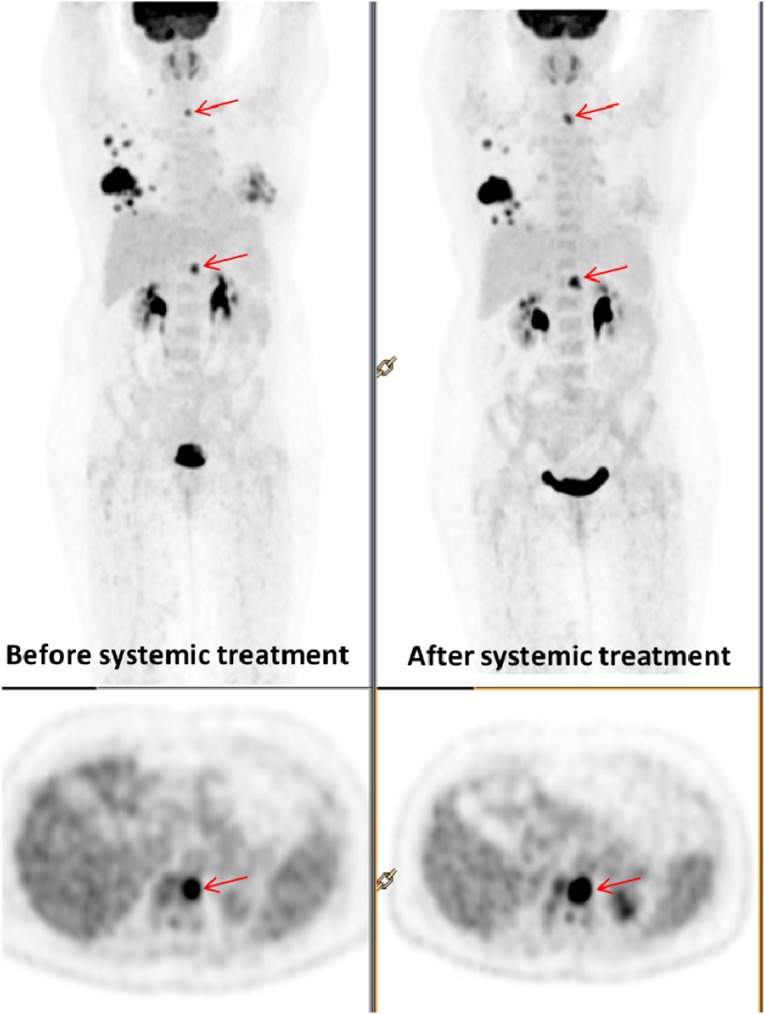
A second limit is that PERCIST, like RECIST, evaluates change of SUV only in the most active lesion(s), without considering the frequently observed intraindividual heterogeneity of the response among lesions in metastatic breast cancer. FDG-PET/CT being a whole body evaluation of metastases with a unique procedure is much more reliable than conventional imaging to identify a mixed response (Fig. 2). Huyge et al. [83] have performed serial FDG-PET/CT in women with bone-dominant metastatic breast cancer. Coexistence of responding and nonresponding metastatic lesions was observed in 43% of women with a trend toward an intermediate outcome in these patients, compared with women with homogeneous response or nonresponse.
Figure 2.
Discordant response between bone and visceral metastases on fluorodeoxyglucose (FDG)-positron emission tomography (PET) exams performed before (left) and after (right) 3 months of treatment with gemcitabine-trastuzumab. Baseline FDG-PET shows hypermetabolic activity in bilateral and multifocal breast tumors, lymph node involvement of right axilla, and bone metastases. After treatment, PET demonstrated an heterogeneous metabolic response with coexistence of responding (left breast, axillary nodes) and nonresponding metastatic bone lesions (red arrows, moderate increased in focal uptake of the two bone lesions).
To create the reproducibility that is needed in multicentric trials, further multicentric studies should thus be conducted to define robust standardized metabolic criteria in the monitoring of metastatic breast cancer, taking into account the various subtypes of breast cancer, the treatments used, and the heterogeneity of response among metastases.
New Tracers of Other Molecular Pathways for Breast Tumor Response Evaluation
Recent identification of molecular alterations in key proteins involved in breast cancer cell proliferation has led to the development of new target therapies. Specific biomarkers are required to evaluate these molecular pathways.
Furthermore, breast cancer is a heterogeneous tumor made up of different cell clones [84, 85]. Imaging tracers have the advantage of taking into account the heterogeneity of tumor biology in metastatic lesions, whereas biopsies are subject to sample error.
Contractor et al. have recently demonstrated that changes in FLT-PET uptake within 2 weeks after initiating the first or second cycle of docetaxel can predict the anatomic response at midtherapy (after three cycles) with good sensitivity and is correlated with the decrease of circulatory tumor cells.
Changes in Tumor Cell Proliferation
Proliferation is one of the key behaviors of cancer and is thus particularly attractive in cancer imaging. The most studied PET proliferation tracer is 18F-fluorothymidine (FLT). Its uptake depends on the activity of thymidine kinase-1, overexpressed during the S phase of the cell cycle [86, 87]. Its use is limited by a lower uptake than FDG [88], and a high physiological uptake in the liver and in bone marrow limits its use for evaluating metastases in these organs [88]. The main advantage of FLT is its lower accumulation caused by tumor inflammation [89–91], which may reduce the false-positive effects of inflammatory reaction encountered with FDG-PET. Small studies have shown that FLT could reflect treatment effectiveness earlier than anatomic imaging [92–94]. Contractor et al. have recently demonstrated that changes in FLT-PET uptake within 2 weeks after initiating the first or second cycle of docetaxel can predict the anatomic response at midtherapy (after three cycles) with good sensitivity [93] and is correlated with the decrease of circulatory tumor cells [94]. In the neoadjuvant setting, the few studies are contradictory. A recent study including 20 women has reported disappointing results: FLT breast tumor uptake at baseline was correlated with baseline Ki-67 (p = .006), but the decrease after the first cycle of NAC did not predict pathological response [95]. In contrast, preliminary results of the ACRIN 6688 multicentric trials, presented at the 2014 ASCO meeting, found that FLT-PET after the first cycle of NAC was marginally predictive of pCR in 51 women [96]. Further works are warranted to establish the exact clinical role of FLT for monitoring breast tumor response, compared with FDG.
Changes in Tumor Blood Flow and Angiogenesis
Angiogenesis is an important hallmark of tumor growth [97] and has become a therapeutic target in breast cancer. Imaging of changes in tumor flow during therapy is an important clinical issue to evaluate the efficacy of these drugs.
The Seattle group has assessed perfusion in breast cancer using 15O-labeled water [34, 98–101]. They determined that blood flow decrease after 2 months of therapy can predict tumor response and outcome in women receiving NAC [99, 100]. Moreover, locally advanced breast cancer tumors with a baseline flow-glycolytic metabolism mismatch (low tumor blood flow but high glycolytic metabolism) are more resistant to therapy, predicting a low likelihood of pCR and higher risk of early relapse [98, 101]. This mismatch is more common in triple-negative tumors [34].
In a few papers, determination of tumor blood flow and metabolism with a single injection of FDG was suggested to be an alternative to the less available 15O-water. Indeed, dynamic FDG-PET can indirectly evaluate blood flow using a two-compartment model [100, 102], but it requires an acquisition of 1 hour. Mullani et al. [103] used a shorter first-pass method to calculate blood flow by dynamic imaging 2 minutes after FDG injection: it was linearly correlated with the 15O-water method. Cochet et al. [104] demonstrated that, in breast cancer, blood flow determined with this first-pass FDG method was correlated with tumor angiogenesis evaluated by immunohistochemistry.
Other molecular pathways have been studied. αvβ3 integrin is a protein expressed on activated endothelial cells during angiogenesis. It is involved in tumor growth, local invasiveness, and metastatic spread [105]. Promising PET tracers have been developed to image this protein: 18F-galacto-RGD is the most studied one [105–107]. In breast cancer, a clinical study demonstrated elevated and highly variable αvβ3 expression in primary tumor, assessed with PET [105].
Vascular endothelial growth factor (VEGF) is a molecular target of the monoclonal antibody bevacizumab. When labeled with 89-zirconium (89Zr), bevacizumab preserves its VEGF-binding properties. 89Zr-Bevacizumab tumor uptake correlated with VEGF tumor levels [108] and might be valuable for prediction and evaluation of the effect of VEGF-targeting therapeutics. In the near future, the development of a PET/MRI integrated system will permit the combination of imaging of molecular targets using PET tracers and study of perfusion using MRI [109].
Estrogen Receptor Tumor Expression
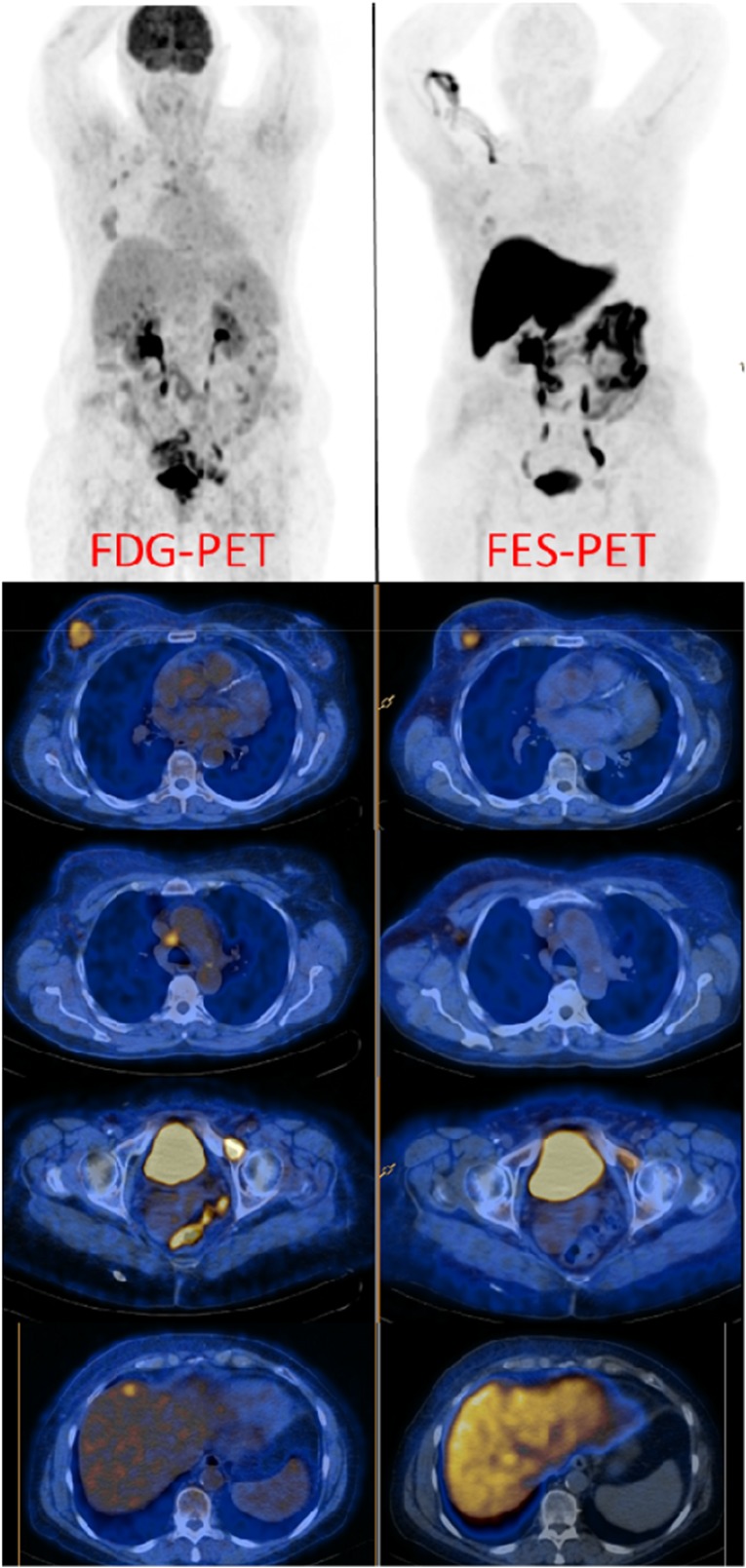
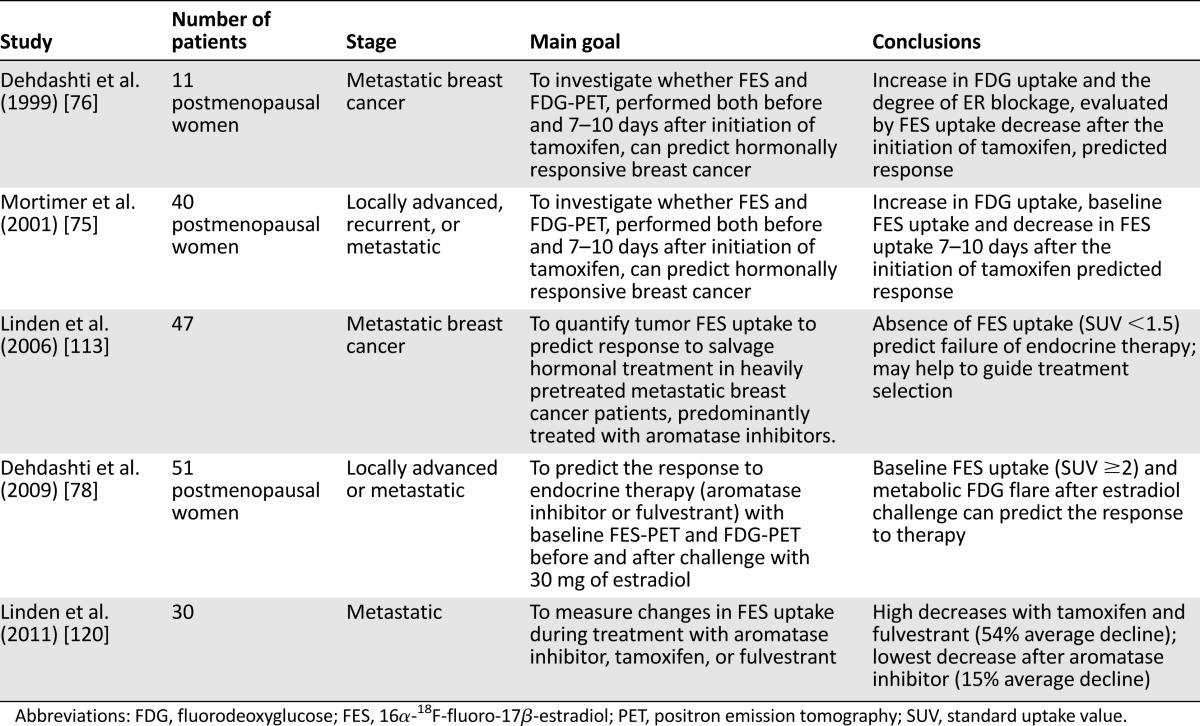
Approximately 70% of women with breast cancer have ER-positive tumors. Currently, because distant metastases are numerous and not easily accessible for biopsies [110], patients with metastatic breast cancer are usually stratified according to the immunohistochemistry analysis of the primary tumor, but approximately 40% of them have discordant ER expression across lesions [111]. PET with 16α-18F-fluoro-17β-estradiol (FES) can characterize and quantify the in vivo functional status of ER expression in all tumor lesions within one patient (Fig. 3). Its sensitivity and specificity to detect ER+ lesions are evaluated at 84% and 98%, respectively [112]. Four studies reported the predictive value of FES tumor uptake for response to endocrine therapy in 138 patients with metastatic breast cancer [75, 76, 78, 112, ] (Table 2). FES-PET was performed before introducing endocrine therapy. A tumor SUV higher than 1.5 at baseline predicts a clinical benefit with a PPV of 65% and a NPV of 88%. Thus, in patients with a previously ER+ tumor, low FES uptake in metastasis predicts nonresponse to endocrine therapy. One of these studies, including 40 women, also found that the decrease in FES uptake 7–10 days after induction of tamoxifen, corresponding to ER blockage, was greater in responders than nonresponders (55% ± 14% vs. 19% ± 17%, respectively) [75]. Nevertheless, the limited number of women included, the differences in optimal SUV cutoff, and the predictive value require additional studies.
Figure 3.
FDG-PET exam (left) and FES-PET exam (right) of a woman with metastatic breast cancer. The tumor lesions, assessed with FDG-PET, showed heterogeneous expression of estrogen receptors: primary breast tumor had a high but heterogeneous uptake pattern of FES, mediastinal nodes showed no significant FES uptake, and the bone metastasis on the left ischiopubic branch showed weak FES uptake. The liver metastasis was not evaluable with FES-PET because of the high physiological uptake of the liver (images are obtained from Estrotepredic Programme Hospitalier de Recherche Clinique, coordinator: Dr. K. Kerrou, Hôpital Tenon, Assistance-Publique–Hôpitaux de Paris, Paris; Eudract: 2011-005043-27).
Abbreviations: FDG, fluorodeoxyglucose; FES, 16α-18F-fluoro-17β-estradiol; PET, positron emission tomography.
Table 2.
Studies evaluating the prediction of response with FES-PET in women with estrogen receptor-positive breast cancer
Many other PET tracers are being evaluated, for example 89Zr-trastuzumab [114–117]. The few studies published demonstrated a good uptake in HER2-positive liver, lung, bone, and brain metastases. The multicentric ZEPHYR trial, presented at the 2014 ASCO meeting, found promising first results for 89Zr-trastuzumab as a predictive marker for trastuzumab/emtansine (T-DM1) therapy in HER2+ breast cancer [118]. Promising works are also ongoing in progesterone-receptor imaging [119].
Conclusion
FDG-PET is a promising early imaging biomarker of the efficacy of breast treatment. First studies demonstrated that, in the neoadjuvant setting, the metabolic response can predict final pCR after the first cycles of NAC. However, breast cancer is a heterogeneous disease, and following studies showed that tumor metabolic behavior highly depends on the various biologic subtypes of breast cancer. In subgroup analysis, FDG-PET seems to correctly predict pCR in HER2-positive and TN subtypes, whereas it may rather be a surrogate marker of survival in luminal tumors. Rigorous prospective clinical trials are mandatory to define the optimal metabolic criteria of good and poor metabolic response for each of the three main biologic subtypes of breast cancer and answer questions about the optimal PET timing. Randomized clinical trials, evaluating different PET-based therapeutic strategies, are also needed to demonstrate a clinical benefit of an early tailoring of the neoadjuvant treatment.
In the metastatic setting, there is increasing clinical evidence that FDG-PET/CT is the most accurate and earlier imaging modality for assessment of the tumor response to treatment when both metabolic and morphologic tumor data are considered. Compared with other imaging modalities, whole-body FDG-PET/CT is particularly efficient in measuring bone metastasis response and may emerge as a standard of care.
Many therapies targeting specific molecular hallmarks of breast tumor cells have recently emerged, with encouraging and sometimes disappointing results. The concurrent development of new predictive surrogate markers of the efficacy of these treatments is required to reveal their true potential. In the future, new radiopharmaceuticals highlighting specific molecular pathways of an individual tumor may help physicians to select the optimal target therapy, leading to a more personalized treatment. The role of imaging biomarkers, compared with biological and molecular biomarkers of response (circulating tumor cells for example) will also have to be better defined.
Acknowledgment
This review is part of the PharmImage project.
Author Contributions
Conception/Design: Olivier Humbert, Alexandre Cochet, Bruno Coudert, Alina Berriolo-Riedinger, Salim Kanoun, François Brunotte, Pierre Fumoleau
Provision of study material or patients: Olivier Humbert
Collection and/or assembly of data: Olivier Humbert, Alexandre Cochet, Alina Berriolo-Riedinger
Data analysis and interpretation: Olivier Humbert, Alina Berriolo-Riedinger, François Brunotte, Pierre Fumoleau
Manuscript writing: Olivier Humbert, Alexandre Cochet, Bruno Coudert, Pierre Fumoleau
Final approval of manuscript: Olivier Humbert, Alexandre Cochet, Bruno Coudert, Alina Berriolo-Riedinger, Salim Kanoun, François Brunotte, Pierre Fumoleau
Disclosures
Bruno Coudert: Laboratory Roche (C/A); Pierre Fumoleau: Sanofi, Roche, GlaxoSmithKline, Janssen, Eisai, Debiopharm (C/A). The other authors indicated no financial relationships.
References
- 1.Groheux D, Espié M, Giacchetti S, et al. Performance of FDG PET/CT in the clinical management of breast cancer. Radiology. 2013;266:388–405. doi: 10.1148/radiol.12110853. [DOI] [PubMed] [Google Scholar]
- 2.Wahl RL, Zasadny K, Helvie M, et al. Metabolic monitoring of breast cancer chemohormonotherapy using positron emission tomography: Initial evaluation. J Clin Oncol. 1993;11:2101–2111. doi: 10.1200/JCO.1993.11.11.2101. [DOI] [PubMed] [Google Scholar]
- 3.Fisher B, Brown A, Mamounas E, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: Findings from National Surgical Adjuvant Breast and Bowel Project B-18. J Clin Oncol. 1997;15:2483–2493. doi: 10.1200/JCO.1997.15.7.2483. [DOI] [PubMed] [Google Scholar]
- 4.Gralow JR, Burstein HJ, Wood W, et al. Preoperative therapy in invasive breast cancer: Pathologic assessment and systemic therapy issues in operable disease. J Clin Oncol. 2008;26:814–819. doi: 10.1200/JCO.2007.15.3510. [DOI] [PubMed] [Google Scholar]
- 5.Kuerer HM, Newman LA, Smith TL, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17:460–469. doi: 10.1200/JCO.1999.17.2.460. [DOI] [PubMed] [Google Scholar]
- 6.von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–1804. doi: 10.1200/JCO.2011.38.8595. [DOI] [PubMed] [Google Scholar]
- 7.Schelling M, Avril N, Nährig J, et al. Positron emission tomography using [(18)F]Fluorodeoxyglucose for monitoring primary chemotherapy in breast cancer. J Clin Oncol. 2000;18:1689–1695. doi: 10.1200/JCO.2000.18.8.1689. [DOI] [PubMed] [Google Scholar]
- 8.Rousseau C, Devillers A, Sagan C, et al. Monitoring of early response to neoadjuvant chemotherapy in stage II and III breast cancer by [18F]fluorodeoxyglucose positron emission tomography. J Clin Oncol. 2006;24:5366–5372. doi: 10.1200/JCO.2006.05.7406. [DOI] [PubMed] [Google Scholar]
- 9.Berriolo-Riedinger A, Touzery C, Riedinger JM, et al. [18F]FDG-PET predicts complete pathological response of breast cancer to neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2007;34:1915–1924. doi: 10.1007/s00259-007-0459-5. [DOI] [PubMed] [Google Scholar]
- 10.McDermott GM, Welch A, Staff RT, et al. Monitoring primary breast cancer throughout chemotherapy using FDG-PET. Breast Cancer Res Treat. 2007;102:75–84. doi: 10.1007/s10549-006-9316-7. [DOI] [PubMed] [Google Scholar]
- 11.Kumar A, Kumar R, Seenu V, et al. The role of 18F-FDG PET/CT in evaluation of early response to neoadjuvant chemotherapy in patients with locally advanced breast cancer. Eur Radiol. 2009;19:1347–1357. doi: 10.1007/s00330-009-1303-z. [DOI] [PubMed] [Google Scholar]
- 12.Schwarz-Dose J, Untch M, Tiling R, et al. Monitoring primary systemic therapy of large and locally advanced breast cancer by using sequential positron emission tomography imaging with [18F]fluorodeoxyglucose. J Clin Oncol. 2009;27:535–541. doi: 10.1200/JCO.2008.17.2650. [DOI] [PubMed] [Google Scholar]
- 13.Kolesnikov-Gauthier H, Vanlemmens L, Baranzelli MC, et al. Predictive value of neoadjuvant chemotherapy failure in breast cancer using FDG-PET after the first course. Breast Cancer Res Treat. 2012;131:517–525. doi: 10.1007/s10549-011-1832-4. [DOI] [PubMed] [Google Scholar]
- 14.Duch J, Fuster D, Muñoz M, et al. PET/CT with [18F] fluorodeoxyglucose in the assessment of metabolic response to neoadjuvant chemotherapy in locally advanced breast cancer. Q J Nucl Med Mol Imaging. 2012;56:291–298. [PubMed] [Google Scholar]
- 15.Duch J, Fuster D, Muñoz M, et al. 18F-FDG PET/CT for early prediction of response to neoadjuvant chemotherapy in breast cancer. Eur J Nucl Med Mol Imaging. 2009;36:1551–1557. doi: 10.1007/s00259-009-1116-y. [DOI] [PubMed] [Google Scholar]
- 16.Dunnwald LK, Doot RK, Specht JM, et al. PET tumor metabolism in locally advanced breast cancer patients undergoing neoadjuvant chemotherapy: Value of static versus kinetic measures of fluorodeoxyglucose uptake. Clin Cancer Res. 2011;17:2400–2409. doi: 10.1158/1078-0432.CCR-10-2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boellaard R. Need for standardization of 18F-FDG PET/CT for treatment response assessments. J Nucl Med. 2011;52(suppl 2):93S–100S. doi: 10.2967/jnumed.110.085662. [DOI] [PubMed] [Google Scholar]
- 18.Cheng X, Li Y, Liu B, et al. 18F-FDG PET/CT and PET for evaluation of pathological response to neoadjuvant chemotherapy in breast cancer: A meta-analysis. Acta Radiol. 2012;53:615–627. doi: 10.1258/ar.2012.110603. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Zhang C, Liu J, et al. Is 18F-FDG PET accurate to predict neoadjuvant therapy response in breast cancer? A meta-analysis. Breast Cancer Res Treat. 2012;131:357–369. doi: 10.1007/s10549-011-1780-z. [DOI] [PubMed] [Google Scholar]
- 20.Mghanga FP, Lan X, Bakari KH, et al. Fluorine-18 fluorodeoxyglucose positron emission tomography-computed tomography in monitoring the response of breast cancer to neoadjuvant chemotherapy: A meta-analysis. Clin Breast Cancer. 2013;13:271–279. doi: 10.1016/j.clbc.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 21.Ohara M, Shigematsu H, Tsutani Y, et al. Role of FDG-PET/CT in evaluating surgical outcomes of operable breast cancer: Usefulness for malignant grade of triple-negative breast cancer. Breast. 2013;22:958–963. doi: 10.1016/j.breast.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Ahn SG, Lee M, Jeon TJ, et al. [18F]-fluorodeoxyglucose positron emission tomography can contribute to discriminate patients with poor prognosis in hormone receptor-positive breast cancer. PLoS One. 2014;9:e105905. doi: 10.1371/journal.pone.0105905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perou CM, Sørlie T, Eisen MB, et al. Molecular portraits of human breast tumours. Nature. 2000;406:747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 24.Sørlie T, Perou CM, Tibshirani R, et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA. 2001;98:10869–10874. doi: 10.1073/pnas.191367098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sorlie T, Tibshirani R, Parker J, et al. Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA. 2003;100:8418–8423. doi: 10.1073/pnas.0932692100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rouzier R, Perou CM, Symmans WF, et al. Breast cancer molecular subtypes respond differently to preoperative chemotherapy. Clin Cancer Res. 2005;11:5678–5685. doi: 10.1158/1078-0432.CCR-04-2421. [DOI] [PubMed] [Google Scholar]
- 27.Bhargava R, Striebel J, Beriwal S, et al. Prevalence, morphologic features and proliferation indices of breast carcinoma molecular classes using immunohistochemical surrogate markers. Int J Clin Exp Pathol. 2009;2:444–455. [PMC free article] [PubMed] [Google Scholar]
- 28.de Ronde JJ, Hannemann J, Halfwerk H, et al. Concordance of clinical and molecular breast cancer subtyping in the context of preoperative chemotherapy response. Breast Cancer Res Treat. 2010;119:119–126. doi: 10.1007/s10549-009-0499-6. [DOI] [PubMed] [Google Scholar]
- 29.Bhargava R, Beriwal S, Dabbs DJ, et al. Immunohistochemical surrogate markers of breast cancer molecular classes predicts response to neoadjuvant chemotherapy: A single institutional experience with 359 cases. Cancer. 2010;116:1431–1439. doi: 10.1002/cncr.24876. [DOI] [PubMed] [Google Scholar]
- 30.Darb-Esfahani S, Loibl S, Muller BM, et al. Identification of biology-based breast cancer types with distinct predictive and prognostic features: Role of steroid hormone and HER2 receptor expression in patients treated with neoadjuvant anthracycline/taxane-based chemotherapy. Breast Cancer Res. 2009;11:R69. doi: 10.1186/bcr2363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.García García-Esquinas M, García-Sáenz JA, Arrazola García J, et al. 18F-FDG PET-CT imaging in the neoadjuvant setting for stages II-III breast cancer: Association of loco‑regional SUVmax with classical prognostic factors. Q J Nucl Med Mol Imaging. 2014;58:66–73. [PubMed] [Google Scholar]
- 32.Humbert O, Berriolo-Riedinger A, Riedinger JM, et al. Changes in 18F-FDG tumor metabolism after a first course of neoadjuvant chemotherapy in breast cancer: Influence of tumor subtypes. Ann Oncol. 2012;23:2572–2577. doi: 10.1093/annonc/mds071. [DOI] [PubMed] [Google Scholar]
- 33.Keam B, Im SA, Koh Y, et al. Early metabolic response using FDG PET/CT and molecular phenotypes of breast cancer treated with neoadjuvant chemotherapy. BMC Cancer. 2011;11:452. doi: 10.1186/1471-2407-11-452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Specht JM, Kurland BF, Montgomery SK, et al. Tumor metabolism and blood flow as assessed by positron emission tomography varies by tumor subtype in locally advanced breast cancer. Clin Cancer Res. 2010;16:2803–2810. doi: 10.1158/1078-0432.CCR-10-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Piccart-Gebhart MJ, Procter M, Leyland-Jones B, et al. Trastuzumab after adjuvant chemotherapy in HER2-positive breast cancer. N Engl J Med. 2005;353:1659–1672. doi: 10.1056/NEJMoa052306. [DOI] [PubMed] [Google Scholar]
- 36.Gianni L, Eiermann W, Semiglazov V, et al. Neoadjuvant chemotherapy with trastuzumab followed by adjuvant trastuzumab versus neoadjuvant chemotherapy alone, in patients with HER2-positive locally advanced breast cancer (the NOAH trial): A randomised controlled superiority trial with a parallel HER2-negative cohort. Lancet. 2010;375:377–384. doi: 10.1016/S0140-6736(09)61964-4. [DOI] [PubMed] [Google Scholar]
- 37.Slamon DJ, Leyland-Jones B, Shak S, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–792. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 38.Groheux D, Giacchetti S, Hatt M, et al. HER2-overexpressing breast cancer: FDG uptake after two cycles of chemotherapy predicts the outcome of neoadjuvant treatment. Br J Cancer. 2013;109:1157–1164. doi: 10.1038/bjc.2013.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Humbert O, Cochet A, Riedinger JM, et al. HER2-positive breast cancer: 18F-FDG PET for early prediction of response to trastuzumab plus taxane-based neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2014;41:1525–1533. doi: 10.1007/s00259-014-2739-1. [DOI] [PubMed] [Google Scholar]
- 40.Koolen BB, Pengel KE, Wesseling J, et al. FDG PET/CT during neoadjuvant chemotherapy may predict response in ER-positive/HER2-negative and triple negative, but not in HER2-positive breast cancer. Breast. 2013;22:691–697. doi: 10.1016/j.breast.2012.12.020. [DOI] [PubMed] [Google Scholar]
- 41.Koolen BB, Pengel KE, Wesseling J, et al. Sequential (18)F-FDG PET/CT for early prediction of complete pathological response in breast and axilla during neoadjuvant chemotherapy. Eur J Nucl Med Mol Imaging. 2014;41:32–40. doi: 10.1007/s00259-013-2515-7. [DOI] [PubMed] [Google Scholar]
- 42.Gebhart G, Gámez C, Holmes E, et al. 18F-FDG PET/CT for early prediction of response to neoadjuvant lapatinib, trastuzumab, and their combination in HER2-positive breast cancer: Results from Neo-ALTTO. J Nucl Med. 2013;54:1862–1868. doi: 10.2967/jnumed.112.119271. [DOI] [PubMed] [Google Scholar]
- 43.Coudert B, Piergat JY, Mouret-Reynier MA, et al. Use of [18F]-FDG PET to predict response to neoadjuvant trastuzumab and docetaxel in patients with HER2-positive breast cancer, and addition of bevacizumab to neoadjuvant trastuzumab and docetaxel in [18F]-FDG PET-predicted non-responders (AVATAXHER): An open-label, randomized phase 2 trial. Lancet Oncol. 2014;15:1493–1502. doi: 10.1016/S1470-2045(14)70475-9. [DOI] [PubMed] [Google Scholar]
- 44.Boyle P. Triple-negative breast cancer: Epidemiological considerations and recommendations. Ann Oncol. 2012;23(suppl 6):vi7–vi12. doi: 10.1093/annonc/mds187. [DOI] [PubMed] [Google Scholar]
- 45.Carey LA, Dees EC, Sawyer L, et al. The triple negative paradox: Primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–2334. doi: 10.1158/1078-0432.CCR-06-1109. [DOI] [PubMed] [Google Scholar]
- 46.Liedtke C, Mazouni C, Hess KR, et al. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–1281. doi: 10.1200/JCO.2007.14.4147. [DOI] [PubMed] [Google Scholar]
- 47.Basu S, Chen W, Tchou J, et al. Comparison of triple-negative and estrogen receptor-positive/progesterone receptor-positive/HER2-negative breast carcinoma using quantitative fluorine-18 fluorodeoxyglucose/positron emission tomography imaging parameters: A potentially useful method for disease characterization. Cancer. 2008;112:995–1000. doi: 10.1002/cncr.23226. [DOI] [PubMed] [Google Scholar]
- 48.Groheux D, Hindié E, Giacchetti S, et al. Early assessment with 18F-fluorodeoxyglucose positron emission tomography/computed tomography can help predict the outcome of neoadjuvant chemotherapy in triple negative breast cancer. Eur J Cancer. 2014;50:1864–1871. doi: 10.1016/j.ejca.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 49.Groheux D, Hindié E, Giacchetti S, et al. Triple-negative breast cancer: Early assessment with 18F-FDG PET/CT during neoadjuvant chemotherapy identifies patients who are unlikely to achieve a pathologic complete response and are at a high risk of early relapse. J Nucl Med. 2012;53:249–254. doi: 10.2967/jnumed.111.094045. [DOI] [PubMed] [Google Scholar]
- 50.Schneider-Kolsky ME, Hart S, Fox J, et al. The role of chemotherapeutic drugs in the evaluation of breast tumour response to chemotherapy using serial FDG-PET. Breast Cancer Res. 2010;12:R37. doi: 10.1186/bcr2591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Doot RK, Dunnwald LK, Schubert EK, et al. Dynamic and static approaches to quantifying 18F-FDG uptake for measuring cancer response to therapy, including the effect of granulocyte CSF. J Nucl Med. 2007;48:920–925. doi: 10.2967/jnumed.106.037382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Groheux D, Hatt M, Hindié E, et al. Estrogen receptor-positive/human epidermal growth factor receptor 2-negative breast tumors: Early prediction of chemosensitivity with (18)F-fluorodeoxyglucose positron emission tomography/computed tomography during neoadjuvant chemotherapy. Cancer. 2013;119:1960–1968. doi: 10.1002/cncr.28020. [DOI] [PubMed] [Google Scholar]
- 53.Humbert O, Berriolo-Riedinger A, Cochet A, et al. Prognostic relevance at 5 years of the early monitoring of neoadjuvant chemotherapy using (18)F-FDG PET in luminal HER2-negative breast cancer. Eur J Nucl Med Mol Imaging. 2014;41:416–427. doi: 10.1007/s00259-013-2616-3. [DOI] [PubMed] [Google Scholar]
- 54.Hatt M, Groheux D, Martineau A, et al. Comparison between 18F-FDG PET image-derived indices for early prediction of response to neoadjuvant chemotherapy in breast cancer. J Nucl Med. 2013;54:341–349. doi: 10.2967/jnumed.112.108837. [DOI] [PubMed] [Google Scholar]
- 55.Bruzzi P, Del Mastro L, Sormani MP, et al. Objective response to chemotherapy as a potential surrogate end point of survival in metastatic breast cancer patients. J Clin Oncol. 2005;23:5117–5125. doi: 10.1200/JCO.2005.02.106. [DOI] [PubMed] [Google Scholar]
- 56.Therasse P, Arbuck SG, Eisenhauer EA, et al. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92:205–216. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 57.Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 58.Coleman RE. Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res. 2006;12:6243s–6249s. doi: 10.1158/1078-0432.CCR-06-0931. [DOI] [PubMed] [Google Scholar]
- 59.Harvey HA, Cream L. Biology of bone metastases: Causes and consequences. Clin Breast Cancer. 2007;7(suppl 1):S7–S13. doi: 10.3816/cbc.2007.s.001. [DOI] [PubMed] [Google Scholar]
- 60.Hamaoka T, Madewell JE, Podoloff DA, et al. Bone imaging in metastatic breast cancer. J Clin Oncol. 2004;22:2942–2953. doi: 10.1200/JCO.2004.08.181. [DOI] [PubMed] [Google Scholar]
- 61.Hamaoka T, Costelloe CM, Madewell JE, et al. Tumour response interpretation with new tumour response criteria vs the World Health Organisation criteria in patients with bone-only metastatic breast cancer. Br J Cancer. 2010;102:651–657. doi: 10.1038/sj.bjc.6605546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hayashi N, Costelloe CM, Hamaoka T, et al. A prospective study of bone tumor response assessment in metastatic breast cancer. Clin Breast Cancer. 2013;13:24–30. doi: 10.1016/j.clbc.2012.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Avril N, Sassen S, Roylance R. Response to therapy in breast cancer. J Nucl Med. 2009;50(suppl 1):55S–63S. doi: 10.2967/jnumed.108.057240. [DOI] [PubMed] [Google Scholar]
- 64.Du Y, Cullum I, Illidge TM, et al. Fusion of metabolic function and morphology: Sequential [18F]fluorodeoxyglucose positron-emission tomography/computed tomography studies yield new insights into the natural history of bone metastases in breast cancer. J Clin Oncol. 2007;25:3440–3447. doi: 10.1200/JCO.2007.11.2854. [DOI] [PubMed] [Google Scholar]
- 65.Schneider JA, Divgi CR, Scott AM, et al. Flare on bone scintigraphy following Taxol chemotherapy for metastatic breast cancer. J Nucl Med. 1994;35:1748–1752. [PubMed] [Google Scholar]
- 66.Stafford SE, Gralow JR, Schubert EK, et al. Use of serial FDG PET to measure the response of bone-dominant breast cancer to therapy. Acad Radiol. 2002;9:913–921. doi: 10.1016/s1076-6332(03)80461-0. [DOI] [PubMed] [Google Scholar]
- 67.Schwarz-Dose J, Bader M, Jenicke L, et al. Early prediction of response to chemotherapy in metastatic breast cancer using sequential 18F-FDG PET. J Nucl Med. 2005;46:1144–1150. [PubMed] [Google Scholar]
- 68.Couturier O, Jerusalem G, N’Guyen JM, et al. Sequential positron emission tomography using [18F]fluorodeoxyglucose for monitoring response to chemotherapy in metastatic breast cancer. Clin Cancer Res. 2006;12:6437–6443. doi: 10.1158/1078-0432.CCR-06-0383. [DOI] [PubMed] [Google Scholar]
- 69.Specht JM, Tam SL, Kurland BF, et al. Serial 2-[18F] fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) to monitor treatment of bone-dominant metastatic breast cancer predicts time to progression (TTP) Breast Cancer Res Treat. 2007;105:87–94. doi: 10.1007/s10549-006-9435-1. [DOI] [PubMed] [Google Scholar]
- 70.Cachin F, Prince HM, Hogg A, et al. Powerful prognostic stratification by [18F]fluorodeoxyglucose positron emission tomography in patients with metastatic breast cancer treated with high-dose chemotherapy. J Clin Oncol. 2006;24:3026–3031. doi: 10.1200/JCO.2005.04.6326. [DOI] [PubMed] [Google Scholar]
- 71.Tateishi U, Gamez C, Dawood S, et al. Bone metastases in patients with metastatic breast cancer: Morphologic and metabolic monitoring of response to systemic therapy with integrated PET/CT. Radiology. 2008;247:189–196. doi: 10.1148/radiol.2471070567. [DOI] [PubMed] [Google Scholar]
- 72.Beslija S, Bonneterre J, Burstein HJ, et al. Third consensus on medical treatment of metastatic breast cancer. Ann Oncol. 2009;20:1771–1785. doi: 10.1093/annonc/mdp261. [DOI] [PubMed] [Google Scholar]
- 73.Mouridsen H, Gershanovich M, Sun Y, et al. Superior efficacy of letrozole versus tamoxifen as first-line therapy for postmenopausal women with advanced breast cancer: Results of a phase III study of the International Letrozole Breast Cancer Group. J Clin Oncol. 2001;19:2596–2606. doi: 10.1200/JCO.2001.19.10.2596. [DOI] [PubMed] [Google Scholar]
- 74.Howell A, Robertson JF, Quaresma Albano J, et al. Fulvestrant, formerly ICI 182,780, is as effective as anastrozole in postmenopausal women with advanced breast cancer progressing after prior endocrine treatment. J Clin Oncol. 2002;20:3396–3403. doi: 10.1200/JCO.2002.10.057. [DOI] [PubMed] [Google Scholar]
- 75.Mortimer JE, Dehdashti F, Siegel BA, et al. Metabolic flare: Indicator of hormone responsiveness in advanced breast cancer. J Clin Oncol. 2001;19:2797–2803. doi: 10.1200/JCO.2001.19.11.2797. [DOI] [PubMed] [Google Scholar]
- 76.Dehdashti F, Flanagan FL, Mortimer JE, et al. Positron emission tomographic assessment of “metabolic flare” to predict response of metastatic breast cancer to antiestrogen therapy. Eur J Nucl Med. 1999;26:51–56. doi: 10.1007/s002590050359. [DOI] [PubMed] [Google Scholar]
- 77.Kurland BF, Gadi VK, Specht JM, et al. Feasibility study of FDG PET as an indicator of early response to aromatase inhibitors and trastuzumab in a heterogeneous group of breast cancer patients. EJNMMI Res. 2012;2:34. doi: 10.1186/2191-219X-2-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dehdashti F, Mortimer JE, Trinkaus K, et al. PET-based estradiol challenge as a predictive biomarker of response to endocrine therapy in women with estrogen-receptor-positive breast cancer. Breast Cancer Res Treat. 2009;113:509–517. doi: 10.1007/s10549-008-9953-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mortazavi-Jehanno N, Giraudet AL, Champion L, et al. Assessment of response to endocrine therapy using FDG PET/CT in metastatic breast cancer: A pilot study. Eur J Nucl Med Mol Imaging. 2012;39:450–460. doi: 10.1007/s00259-011-1981-z. [DOI] [PubMed] [Google Scholar]
- 80.Carlson RW, Allred DC, Anderson BO, et al. Metastatic breast cancer, version 1.2012: Featured updates to the NCCN guidelines. J Natl Compr Canc Netw. 2012;10:821–829. doi: 10.6004/jnccn.2012.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Young H, Baum R, Cremerius U, et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: Review and 1999 EORTC recommendations. Eur J Cancer. 1999;35:1773–1782. doi: 10.1016/s0959-8049(99)00229-4. [DOI] [PubMed] [Google Scholar]
- 82.Wahl RL, Jacene H, Kasamon Y, et al. From RECIST to PERCIST: Evolving Considerations for PET response criteria in solid tumors. J Nucl Med. 2009;50(suppl 1):122S–150S. doi: 10.2967/jnumed.108.057307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Huyge V, Garcia C, Alexiou J, et al. Heterogeneity of metabolic response to systemic therapy in metastatic breast cancer patients. Clin Oncol (R Coll Radiol) 2010;22:818–827. doi: 10.1016/j.clon.2010.05.021. [DOI] [PubMed] [Google Scholar]
- 84.Heim S, Teixeira MR, Dietrich CU, et al. Cytogenetic polyclonality in tumors of the breast. Cancer Genet Cytogenet. 1997;95:16–19. doi: 10.1016/s0165-4608(96)00322-6. [DOI] [PubMed] [Google Scholar]
- 85.Teixeira MR, Pandis N, Bardi G, et al. Karyotypic comparisons of multiple tumorous and macroscopically normal surrounding tissue samples from patients with breast cancer. Cancer Res. 1996;56:855–859. [PubMed] [Google Scholar]
- 86.Kenny LM, Vigushin DM, Al-Nahhas A, et al. Quantification of cellular proliferation in tumor and normal tissues of patients with breast cancer by [18F]fluorothymidine-positron emission tomography imaging: Evaluation of analytical methods. Cancer Res. 2005;65:10104–10112. doi: 10.1158/0008-5472.CAN-04-4297. [DOI] [PubMed] [Google Scholar]
- 87.Soloviev D, Lewis D, Honess D, et al. [(18)F]FLT: An imaging biomarker of tumour proliferation for assessment of tumour response to treatment. Eur J Cancer. 2012;48:416–424. doi: 10.1016/j.ejca.2011.11.035. [DOI] [PubMed] [Google Scholar]
- 88.Kenny LM, Al-Nahhas A, Aboagye EO. Novel PET biomarkers for breast cancer imaging. Nucl Med Commun. 2011;32:333–335. doi: 10.1097/MNM.0b013e32834471ff. [DOI] [PubMed] [Google Scholar]
- 89.van Waarde A, Cobben DC, Suurmeijer AJ, et al. Selectivity of 18F-FLT and 18F-FDG for differentiating tumor from inflammation in a rodent model. J Nucl Med. 2004;45:695–700. [PubMed] [Google Scholar]
- 90.van Waarde A, Elsinga PH. Proliferation markers for the differential diagnosis of tumor and inflammation. Curr Pharm Des. 2008;14:3326–3339. doi: 10.2174/138161208786549399. [DOI] [PubMed] [Google Scholar]
- 91.Yue J, Chen L, Cabrera AR, et al. Measuring tumor cell proliferation with 18F-FLT PET during radiotherapy of esophageal squamous cell carcinoma: A pilot clinical study. J Nucl Med. 2010;51:528–534. doi: 10.2967/jnumed.109.072124. [DOI] [PubMed] [Google Scholar]
- 92.Pio BS, Park CK, Pietras R, et al. Usefulness of 3′-[F-18]fluoro-3′-deoxythymidine with positron emission tomography in predicting breast cancer response to therapy. Mol Imaging Biol. 2006;8:36–42. doi: 10.1007/s11307-005-0029-9. [DOI] [PubMed] [Google Scholar]
- 93.Contractor KB, Kenny LM, Stebbing J, et al. [18F]-3′-Deoxy-3′-fluorothymidine positron emission tomography and breast cancer response to docetaxel. Clin Cancer Res. 2011;17:7664–7672. doi: 10.1158/1078-0432.CCR-11-0783. [DOI] [PubMed] [Google Scholar]
- 94.Contractor K, Aboagye EO, Jacob J, et al. Monitoring early response to taxane therapy in advanced breast cancer with circulating tumor cells and [(18)F] 3´-deoxy-3´-fluorothymidine PET: A pilot study. Biomarkers Med. 2012;6:231–233. doi: 10.2217/bmm.12.11. [DOI] [PubMed] [Google Scholar]
- 95.Woolf DK, Beresford M, Li SP, et al. Evaluation of FLT-PET-CT as an imaging biomarker of proliferation in primary breast cancer. Br J Cancer. 2014;110:2847–2854. doi: 10.1038/bjc.2014.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Kostakoglu L. Phase II study of 3′-deoxy-3′-18F fluorothymidine PET/CT (FLT-PET) in the assessment of early response in locally advanced breast cancer (LABC): Preliminary results of ACRIN 6688. Poster presented at: Annual Meeting of the American Society of Clinical Oncology; May 30 to June 3, 2014; Chicago, IL. [Google Scholar]
- 97.Folkman J. Tumor angiogenesis: Therapeutic implications. N Engl J Med. 1971;285:1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 98.Mankoff DA, Dunnwald LK, Gralow JR, et al. Blood flow and metabolism in locally advanced breast cancer: Relationship to response to therapy. J Nucl Med. 2002;43:500–509. [PubMed] [Google Scholar]
- 99.Mankoff DA, Dunnwald LK, Gralow JR, et al. Changes in blood flow and metabolism in locally advanced breast cancer treated with neoadjuvant chemotherapy. J Nucl Med. 2003;44:1806–1814. [PubMed] [Google Scholar]
- 100.Dunnwald LK, Gralow JR, Ellis GK, et al. Tumor metabolism and blood flow changes by positron emission tomography: Relation to survival in patients treated with neoadjuvant chemotherapy for locally advanced breast cancer. J Clin Oncol. 2008;26:4449–4457. doi: 10.1200/JCO.2007.15.4385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Eby PR, Partridge SC, White SW, et al. Metabolic and vascular features of dynamic contrast-enhanced breast magnetic resonance imaging and (15)O-water positron emission tomography blood flow in breast cancer. Acad Radiol. 2008;15:1246–1254. doi: 10.1016/j.acra.2008.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tseng J, Dunnwald LK, Schubert EK, et al. 18F-FDG kinetics in locally advanced breast cancer: Correlation with tumor blood flow and changes in response to neoadjuvant chemotherapy. J Nucl Med. 2004;45:1829–1837. [PubMed] [Google Scholar]
- 103.Mullani NA, Herbst RS, O’Neil RG, et al. Tumor blood flow measured by PET dynamic imaging of first-pass 18F-FDG uptake: A comparison with 15O-labeled water-measured blood flow. J Nucl Med. 2008;49:517–523. doi: 10.2967/jnumed.107.048504. [DOI] [PubMed] [Google Scholar]
- 104.Cochet A, Pigeonnat S, Khoury B, et al. Evaluation of breast tumor blood flow with dynamic first-pass 18F-FDG PET/CT: Comparison with angiogenesis markers and prognostic factors. J Nucl Med. 2012;53:512–520. doi: 10.2967/jnumed.111.096834. [DOI] [PubMed] [Google Scholar]
- 105.Beer AJ, Niemeyer M, Carlsen J, et al. Patterns of alphavbeta3 expression in primary and metastatic human breast cancer as shown by 18F-Galacto-RGD PET. J Nucl Med. 2008;49:255–259. doi: 10.2967/jnumed.107.045526. [DOI] [PubMed] [Google Scholar]
- 106.Beer AJ, Haubner R, Sarbia M, et al. Positron emission tomography using [18F]Galacto-RGD identifies the level of integrin alpha(v)beta3 expression in man. Clin Cancer Res. 2006;12:3942–3949. doi: 10.1158/1078-0432.CCR-06-0266. [DOI] [PubMed] [Google Scholar]
- 107.Beer AJ, Haubner R, Wolf I, et al. PET-based human dosimetry of 18F-galacto-RGD, a new radiotracer for imaging alpha v beta3 expression. J Nucl Med. 2006;47:763–769. [PubMed] [Google Scholar]
- 108.Gaykema SB, Brouwers AH, Lub-de Hooge MN, et al. 89Zr-bevacizumab PET imaging in primary breast cancer. J Nucl Med. 2013;54:1014–1018. doi: 10.2967/jnumed.112.117218. [DOI] [PubMed] [Google Scholar]
- 109.O’Flynn EA, DeSouza NM. Functional magnetic resonance: Biomarkers of response in breast cancer. Breast Cancer Res. 2011;13:204. doi: 10.1186/bcr2815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chung GG, Zerkowski MP, Ghosh S, et al. Quantitative analysis of estrogen receptor heterogeneity in breast cancer. Lab Invest. 2007;87:662–669. doi: 10.1038/labinvest.3700543. [DOI] [PubMed] [Google Scholar]
- 111.Amir E, Miller N, Geddie W, et al. Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol. 2012;30:587–592. doi: 10.1200/JCO.2010.33.5232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.van Kruchten M, de Vries EG, Brown M, et al. PET imaging of oestrogen receptors in patients with breast cancer. Lancet Oncol. 2013;14:e465–e475. doi: 10.1016/S1470-2045(13)70292-4. [DOI] [PubMed] [Google Scholar]
- 113.Linden HM, Stekhova SA, Link JM, et al. Quantitative fluoroestradiol positron emission tomography imaging predicts response to endocrine treatment in breast cancer. J Clin Oncol. 2006;24:2793–2799. doi: 10.1200/JCO.2005.04.3810. [DOI] [PubMed] [Google Scholar]
- 114.Dijkers EC, Kosterink JG, Rademaker AP, et al. Development and characterization of clinical-grade 89Zr-trastuzumab for HER2/neu immunoPET imaging. J Nucl Med. 2009;50:974–981. doi: 10.2967/jnumed.108.060392. [DOI] [PubMed] [Google Scholar]
- 115.Dijkers EC, Oude Munnink TH, Kosterink JG, et al. Biodistribution of 89Zr-trastuzumab and PET imaging of HER2-positive lesions in patients with metastatic breast cancer. Clin Pharmacol Ther. 2010;87:586–592. doi: 10.1038/clpt.2010.12. [DOI] [PubMed] [Google Scholar]
- 116.Gaykema SB, Brouwers AH, Hovenga S, et al. Zirconium-89-trastuzumab positron emission tomography as a tool to solve a clinical dilemma in a patient with breast cancer. J Clin Oncol. 2012;30:e74–e75. doi: 10.1200/JCO.2011.38.0204. [DOI] [PubMed] [Google Scholar]
- 117.Gaykema SB, Schröder CP, Vitfell-Rasmussen J, et al. 89Zr-trastuzumab and 89Zr-bevacizumab PET to evaluate the effect of the HSP90 inhibitor NVP-AUY922 in metastatic breast cancer patients. Clin Cancer Res. 2014;20:3945–3954. doi: 10.1158/1078-0432.CCR-14-0491. [DOI] [PubMed] [Google Scholar]
- 118.Gebhart G. PET/CT with 89Zr-trastuzumab and 18F-FDG to individualize treatment with trastuzumab emtansine (T-DM1) in metastatic HER2-positive breast cancer. Oral abstract presented at: Annual Meeting of the American Society of Clinical Oncology; May 30 to June 3, 2014; Chicago, IL. [Google Scholar]
- 119.Dehdashti F, Laforest R, Gao F, et al. Assessment of progesterone receptors in breast carcinoma by PET with 21-18F-fluoro-16α,17α-[(R)-(1′-α-furylmethylidene)dioxy]-19-norpregn-4-ene-3,20-dione. J Nucl Med. 2012;53:363–370. doi: 10.2967/jnumed.111.098319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Linden HM, Kurland BF, Peterson LM, et al. Fluoroestradiol positron emission tomography reveals differences in pharmacodynamics of aromatase inhibitors, tamoxifen, and fulvestrant in patients with metastatic breast cancer. Clin Cancer Res. 2011;17:4799–4805. doi: 10.1158/1078-0432.CCR-10-3321. [DOI] [PMC free article] [PubMed] [Google Scholar]