Abstract
Background.
Patients with a newly diagnosed glioblastoma multiforme (GBM) have a high risk of recurrent disease with a dismal outcome despite intensive treatment of sequential surgery and chemoradiotherapy with temozolomide (TMZ), followed by TMZ as a single agent. Bevacizumab (BV) may increase response rates to chemotherapy in the recurrent treatment setting of GBM. We hypothesized that a neoadjuvant treatment strategy for patients with newly diagnosed GBM using chemoradiotherapy plus BV would improve resectability and thus survival. We performed a phase II trial of the treatment strategy of BV plus chemoradiation to determine the safety of this combination in patients who had already undergone primary surgery for their GBM.
Methods.
After a biopsy (6 patients) or a resection (13 patients) of a newly diagnosed GBM, 19 patients received radiotherapy (30 fractions of 2 Gy) in combination with daily TMZ 75 mg/m2 and BV 10 mg/kg on days 1, 14, and 28, followed by 6 monthly cycles of TMZ 150–200 mg/m2 on days 1–5.
Results.
The overall response rate was 26%. Three patients had a complete response after resection, and in two patients, a complete response after resection followed by chemoradiation plus BV was seen. No grade 3–4 toxicities were observed during combination treatment. The median progression-free survival was 9.6 months (95% confidence interval [CI]: 4.3–14.4 months). The median overall survival was 16 months (95% CI: 8.1–26.3 months), similar to a matched control group that received standard chemoradiotherapy from our institution.
Conclusion.
Combination of bevacizumab with radiotherapy and TMZ is safe and feasible in patients with newly diagnosed GBM, but because of low response rates, this treatment strategy does not favor a neoadjuvant approach.
Author Summary
Discussion
We hypothesized that neoadjuvant treatment strategies for patients with a newly diagnosed GBM using chemoradiotherapy plus bevacizumab may improve resectability and thus survival. However, neoadjuvant treatment is rarely applied for these patients because the most effective way to reduce intracranial pressure is still surgery. Tumor volume itself and the marked brain edema associated with GBM are responsible for elevated intracranial pressure with associated morbidity and mortality. Because of the risk of death through cerebral herniation and the fast growth of the tumor, most GBM patients are currently operated on within 1 or 2 weeks after initial diagnosis.
We hypothesized that BV treatment results in immediate and significant reduction of cerebral edema in patients with GBM and may provide the opportunity to postpone surgical resection while reducing tumor volume through a neoadjuvant strategy, eventually resulting in improved locoregional tumor control and improved survival.
The outcome of patients with GBM may benefit from this strategy with a more radical primary resection that will ultimately reduce the chance of residual disease. Tumor recurrence occurs in 90%–95% close to the resection margin. This is attributed to the findings of increased tumor cell density along the margin, with a sharp drop noted as the distance from the resection cavity increases. In view of this high locoregional tumor recurrence rate, it is worth increasing surgical efficiency to improve locoregional control. Neoadjuvant strategies have been successful at improving margin-free tumor resections and local control in patients with other solid tumors.
Because the addition of bevacizumab to treatment in the recurrent GBM setting leads to an immediate and significant reduction of cerebral edema and tissue hypoxia and normalization of the tumor vasculature, we hypothesized that neoadjuvant BV in combination with chemoradiation would improve the surgical outcome of GBM.
Because of the goal of our feasibility trial, BV administrations were not continued during adjuvant temozolomide cycles.
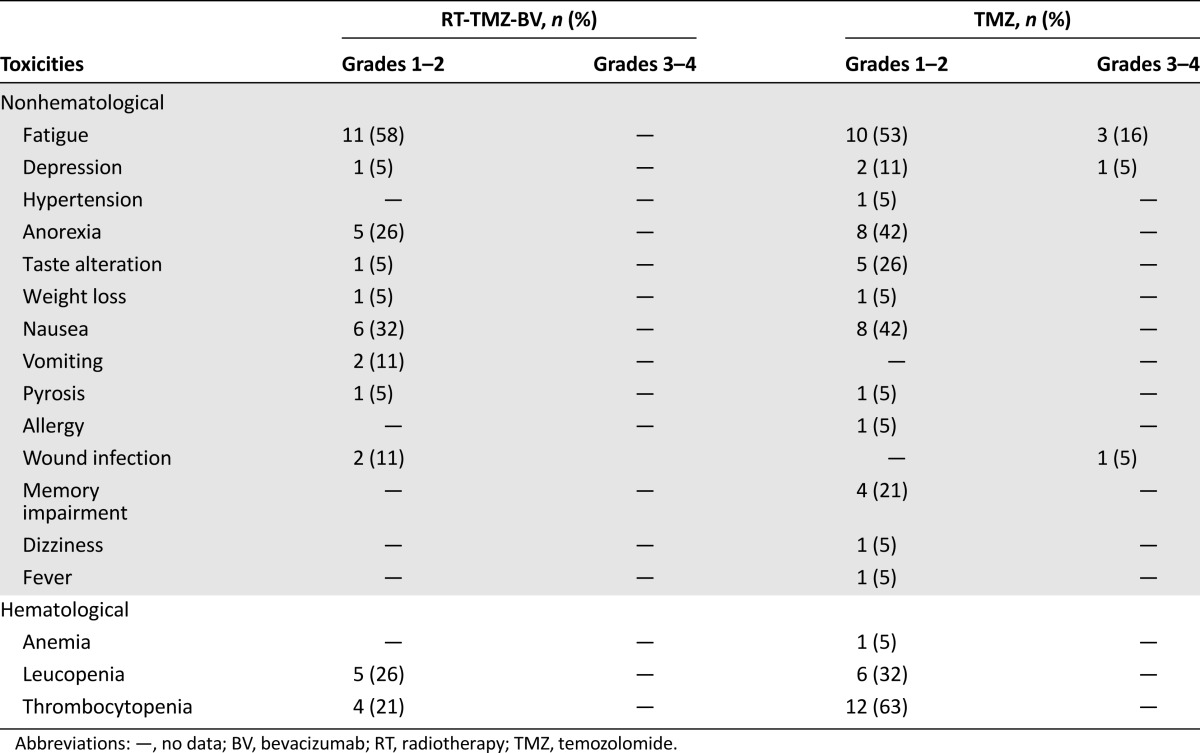
Analysis of toxicity data from our small group of 19 patients did not reveal any grade 3–4 toxicity during the experimental treatment phase of BV in combination with chemoradiotherapy (Table 1). The experimental treatment was well tolerated and was not complicated by known BV-related side effects, In comparison with the standard treatment for GBM in the European Organization for Research and Treatment of Cancer and National Cancer Institute of Canada (EORTC-NCIC) trial, we found slightly more grade 1–2 side effects but no grade 3–4 side effects. Patient characteristics in our study are comparable to the standard patient characteristics in daily practice and, for example, in the EORTC-NCIC trial. Our findings indicate that limiting the addition of BV to the concomitant treatment phase only is safe and feasible, but because of low response rates, this treatment strategy does not favor a neoadjuvant approach.
Table 1.
Treatment-related toxicity in all 19 patients treated with chemoradiotherapy combined with bevacizumab and adjuvant temozolomide
Supplementary Material
Footnotes
Access the full results at: vanLinde-14-418.theoncologist.com
Nederlands Trial Register Identifier: CCMO NL20411.018.07
Sponsor(s): No
Principal Investigator: Myra E. van Linde
IRB Approved: Yes
Author disclosures available online.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


