Abstract
This paper investigates the degree to which choice inconsistencies documented in the context of Medicare Part D plan choice vary across consumers and geographic regions. Our main finding is that there is surprisingly little variation: regardless of age, gender, predicted drug expenditures or the predictability of drug demand consumers underweight out of pocket costs relative to premiums and fail to consider the individualized consequences of plan characteristics; as a result, they frequently choose plans which are dominated in the sense that an alternative plan provides better risk protection at a lower cost. We find limited evidence that the sickest individuals had more difficulty with plan choice, and we document that much of the variation in potential cost savings across states comes from variation in choice sets, not variation in consumers’ ability to choose.
The Medicare Modernization Act of 2003, better known as the legislation that added the Part D prescription drug benefit to the Medicare program, represents the single most significant expansion of public insurance programs in the U.S. in the past 40 years. The most novel, and controversial, feature of this legislation was the use of multiple private insurance providers to deliver this new public insurance product. This unprecedented privatization of the delivery of a public insurance product raises a host of important policy questions. Primary among these is the impact of allowing choice across so many private insurance options.
While standard economic theory would suggest that allowing a wide variety of plan choices would increase welfare, a recent body of work suggests that such “choice overload” can lead to inferior decision-making, as nicely reviewed in Sheena Iyengar and Emir Kamenica (2006). Our previous work (Jason Abaluck and Jonathan Gruber 2011) investigated the prescription drug insurance plan choices made by elders for the newly formed Part D program in 2006. In this paper, we extend that earlier analysis to consider heterogeneity in choice inconsistency.
Part D beneficiaries can choose from three types of private insurance coverage for their drug expenditures. Our study focuses on the most important of these, stand-alone plans called Medicare Prescription Drug Plans (PDP). In 2006, there were 1429 total PDPs offered throughout the nation, with most states offering about forty PDPs. The majority of PDPs are offered by a dozen national or near national companies. Under Part D, recipients were entitled to basic coverage of prescription drugs by a plan with a structure actuarially equivalent to the following: none of the first $250 in drug costs each year; 75% of costs for the next $2,250 of drug spending (up to $2,500 total); 0% of costs for the next $3,600 of drug spending (up to $5,100 total, the “donut hole”); and 95% of costs above $5,100 of drug spending. Over 90% of beneficiaries in 2006, however, were not enrolled in the standard benefit design, but rather are in plans with low or no deductibles, flat payments for covered drugs following a tiered system, or some form of coverage in the donut hole. Overall, Part D sponsors had great flexibility in terms of plan design. Many insurance companies sponsored multiple plans of differing levels of premiums and coverage generosity.
Our primary data source is a longitudinal sample of prescription drug records from the Wolters Kluwer (WK) Company. They are the largest “switch” operator in the prescription drug market: they collect the electronic claims from pharmacies and pass them on to the Pharmacy Benefit Managers (PBMs) and insurance companies that will pay the claims. WK keeps a longitudinal file that tracks prescription drug use for more than 100 million persons in the U.S. They have made available to us for research purposes a longitudinal sample of prescription claims for any individuals age 65 and over in 2005. These data are crucial because they are the only available data (of which we are aware) that contain information both on specific drug utilization by elders and on plan choice. Information about specific drug utilization is key because plan costs vary tremendously based on drug utilization, as we discuss below.
These data have a number of strengths and weaknesses, as described in Abaluck and Gruber (2011). They provide a very large longitudinal sample of elders before and during the first year of the Part D program that is nationally representative. On the other hand, there is some imprecision in matching elders to their Part D insurance plan, and there is a high rate of sample attrition that is potentially due to switching to pharmacies outside the WK sample. In our earlier work we carefully document that this is unlikely to be driving our findings.
We match these WK data to information provided by CMS on plan details and beneficiary costs. This allows us to fully parameterize any elder's plan choice set based on their location. We have used these data to build a “cost calculator” that mimics the calculator provided on Medicare's web site. This calculator uses a given set of prescriptions for a given elder to compute their projected out of pocket spending in each plan available in their county. Our analysis evaluates plan choice using both the elder's actual 2006 prescription drug spending, as well as a predicted measure based on 2005 spending; the results are robust to both.
We begin by presenting basic facts on plan choice. For each individual in the data, we estimate the total cost of enrolling in each PDP plan in their county, adding both premiums and expected out of pocket costs. We then estimate the difference in total costs between the plan chosen by that individual and the lowest cost plan in their county.
Table 1 shows the share of individuals choosing the lowest cost plan available to them, and the savings to the typical elder from choosing that lowest cost plan. For the full sample, we find that only 12.2% of elders choose the lowest cost plan, and that the typical elder could save $296, or 30.1% of their total Part D costs by choosing the lowest cost plan rather than the plan that they did choose. Of course, individuals are not simply choosing a fixed payment stream when choosing a Part D plan; individuals who are highly risk averse may explicitly be choosing plans with higher mean expenditure to protect themselves against variance in expenditure. Yet this does not seem to be the case. Even if we only include plan choices where the variance is non-increasing, over 73% of enrollees could have chosen a lower cost plan, and the average enrollee could have saved 23.7% of their Part D expenditures without raising their variance.
Table 1.
| All Plans | Variance Improving | |||||
|---|---|---|---|---|---|---|
| (1) Percentage Minimizing | (2) Dollars Savings | (3) Percentage Savings | (4) Percentage Minimizing | (5) Dollars Savings | (6) Percentage Savings | |
| All | ||||||
| 12.17 | 296 | 31.01 | 26.89 | 237 | 23.42 | |
| Terciles of Age | ||||||
| 1 | 11.30 | 298 | 31.94 | 25.67 | 238 | 24.16 |
| 2 | 12.38 | 296 | 30.96 | 27.43 | 234 | 23.20 |
| 3 | 12.87 | 295 | 30.07 | 27.58 | 238 | 22.88 |
| Gender | ||||||
| F | 12.73 | 295 | 30.63 | 27.40 | 236 | 23.20 |
| M | 11.21 | 299 | 31.66 | 25.98 | 237 | 23.82 |
| Terciles of 2005 Expenditures | ||||||
| 1 | 10.65 | 217 | 34.26 | 27.33 | 159 | 25.14 |
| 2 | 13.04 | 264 | 30.75 | 27.31 | 208 | 23.27 |
| 3 | 12.84 | 424 | 27.68 | 25.55 | 358 | 21.84 |
| Terciles of Percent Chronic Drugs | ||||||
| 1 | 10.46 | 274 | 33.02 | 25.83 | 214 | 24.81 |
| 2 | 12.70 | 326 | 30.05 | 27.12 | 264 | 22.81 |
| 3 | 13.30 | 289 | 30.01 | 27.69 | 231 | 22.69 |
Notes: The first three columns give the percentage of patients choosing the cost minimizing plan, the average savings from switching to the cost minimizing plan, and the average savings as a percentage of realized out of pocket costs from switching to the cost minimizing plan. Columns (4)-(6) give the same numbers, but considering only plans which are variance-improving (i.e. whose variance is at least as small as the chosen plan). The % of acute drugs is computed as the proportion of claims in 2005 for a drug which also appears in the data in 2006.
We next extend these results on plan choice for a wide variety of elderly subgroups. We find a strikingly flat pattern of results by age, with some suggestion of improved choice at older ages. We also find little heterogeneity by gender. When we divide the sample by 2005 drug expenditure decile, there is more heterogeneity. As 2005 drug spending rises, the dollar savings from better choices rises, while the percentage savings falls. Those in the top decile would save on average almost three times as much as those in the bottom decile from better choices, but as a share of out of pocket spending this is only 5/7 as much.
An alternative potential determinant of choice consistency could be regularity of prescription drug use. MarkDuggan and Fiona Scott-Morton (2011) hypothesize that consumers may fail to take into account variation across plans in the coverage provided for acute drugs if they are not currently consuming those drugs. Our results provide weak support for this hypothesis but suggest that it is not a major driver of consumer error. We define the proportion of drugs which are chronic as the proportion of 2005 claims which are from drugs for which the consumer also has claims in 2006. Consumers are more likely to choose the cost minimizing plan if a greater proportion of their drugs are chronic: 13% of consumers choose the cost minimizing plan in the largest tercile of chronic drugs, while just 10% choose the cost minimizing plan in the lowest tercile. Nonetheless, potential cost savings vary little across tercile, ranging from 30% in the lowest tercile to 33% in the largest tercile.
We extend our analysis to control for other factors that might impact plan choice of elders by estimating a conditional logit model of plan choice where the utility of individual i from choosing plan j is given by:
| (1) |
Where πj is the premium for plan is the expected out of pocket costs for individual i if they are enrolled in plan j given the information available at the time when they choose, is the variance of out of pocket costs for individual i if they enroll in plan j, x represents any financial plan characteristics which impacts choice, ζb(j) is a full set of brand-specific dummies, and εij are i.i.d. type I extreme value random variables. Following Abaluck and Gruber (2011), we do not use actual (noisy and endogenous) out of pocket expenditures but a predicted measure based on 2005 utilization.
We include in our model several financial plan characteristics beyond premiums, out of pocket costs, and the variance of out of pocket costs. These are: the deductible of the plan; a dummy for whether the plan covers all donut hole expenditures; a dummy for whether the plan covers generic expenditures in the donut hole only; and a cost-sharing index. We also include a measure of plan quality: the share of the top 100 drugs used by elders that is included in the plan's formulary. Other differences across brands, including different quality ratings as well as consumer tastes by brand, are absorbed by a full set of brand-specific dummy variables.
We consider three tests of “choice inconsistencies”. The first is whether the coefficient on premiums and out of pocket costs are different; controlling for the risk characteristics of plans, individuals should be willing to pay exactly one dollar in additional premiums for coverage which reduces expected out of pocket costs by one dollar. The second is that λ ≠ 0; individuals should not care about deductibles, donut hole coverage or copays per se; they should only care about these factors to the extent that they impact the distribution of out of pocket costs. The third is that the coefficient on plan variance is non-negative, which should be true for risk averse individuals. In Abaluck and Gruber (2011), we develop the theoretical basis for these tests and offer compelling simulation evidence that they represent choice inconsistencies.
Table 2 summarizes our key results by showing the coefficients on premium and out of pocket costs, an F test of the joint significance of other plan characteristics, and the coefficient on plan variance. For the full sample, the results demonstrate the three choice inconsistencies discussed above: the responsiveness to premiums is five times as large as the responsiveness to out of pocket costs; plan characteristics continue to matter for choices even after controlling for their out of pocket cost consequences, and consumers appear unresponsive to variation across plans in the variance of out of pocket costs.
Table 2.
| Premium | OOP | Variance | F-test | |
|---|---|---|---|---|
| Age 1 | −0.4616 (.0109) | −0.1105 (.00 42) | −0.0008 (.00 19) | X2(5)=1570, p < .0001 |
| Age 2 | −0.4625 (.0062) | −0.1085 (.0024) | −0.0001 (.0008) | X2(5)=1658, p < .0001 |
| Age 3 | −0.5172 (.0110) | −0.1162 (.0042) | −0.0009 (.0016) | X2(5)=1751, p < .0001 |
| Female | −0.4671 (.0104) | −0.1109 (.0039) | 0.0002 (.0016) | X2(5)=1726, p < .0001 |
| Male | −0.4855 (.0078) | −0.1119 (.0030) | −0.0008 (.0010) | X2(5)=3176, p < .0001 |
| Expend 1 | −0.6722 (.0130) | −0.1462 (.0223) | 0.0030 (.0021) | X2(5)=2709, p < .0001 |
| Expend 2 | −0.5536 (.0112) | −0.1473 (.0085) | −0.0015 (.0017) | X2(5)=1909, p < .0001 |
| Expend 3 | −0.3955 (.0105) | −0.0847 (.0029) | −0.0009 (.0012) | X2(5)=1421, p < .0001 |
| Acute | −0.5206 (.0124) | −0.1076 (.0059) | −0.0006 (.0026) | X2(5)=1673, p < .0001 |
| Chronic | −0.4620 (.0072) | −0.1111 (.0026) | −0.0006 (.0008) | X2(5)=3261, p < .0001 |
Notes: This table reports the coefficients on premiums, expected out of pocket costs, and the variance of out of pocket costs from the conditional logit model in equation (1), as well as an F-test for the significance of financial plan characteristics. Premiums and out of pocket costs are in hundreds of dollars, the variance is multiplied by 106. Age 1, Age 2, Age 3, Expend 1, Expend 2 and Expend 3 denote respective terciles of the age and expenditure distributions. Acute and Chronic are defined in the text. Standard errors are in parentheses.
We then extend this analysis to consider whether our results are consistent across subgroups: we consider terciles of age, gender, terciles of 2005 drug expenditures, and acute vs. chronic patients (where acute patients are defined as patients for whom fewer than 35% of claims were from drugs which were also consumed in 2006). As in the case of the efficient frontier analysis, the results are remarkably consistent across different demographic groups. The choice inconsistencies noted above are present in all specifications, and the magnitude of the coefficients varies little.
One possible exception is individuals with higher costs in 2005. In the efficient frontier analysis, we showed that these individuals have higher absolute cost savings, and the logit analysis shows that their choices are noisier in the sense that the premium and out of pocket cost coefficients are both smaller than in other specifications, meaning that a smaller fraction of choices are explained by variation in financial characteristics. The logit result suggests that in addition to having more to lose by choosing the wrong plan, sicker individuals also choose worse (this is a difficult conclusion to establish firmly since the definition of “sick” in this case precludes a comparison of sick and healthy individuals facing identical trade-offs).
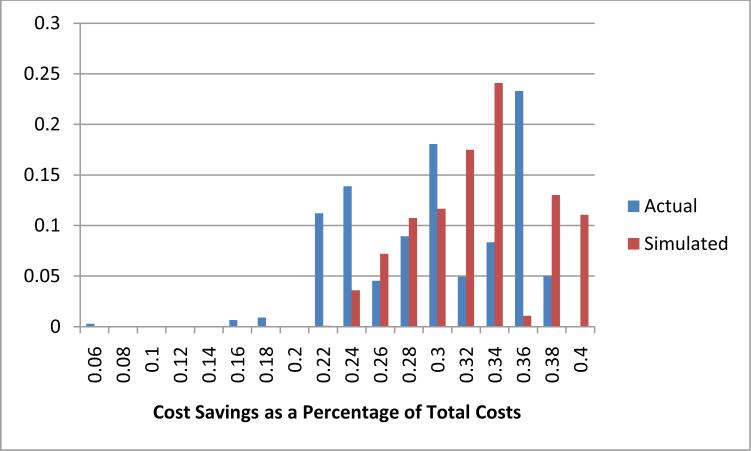
Finally, in Figure 1, we consider the effects by state. Once again, there is surprisingly little variation. In the vast majority of states, the average savings from switching to the lowest total cost plan are between 20% and 40% of total costs. The states in which potential cost savings are less than 20% are also states in which there is the least scope for error. This point is demonstrated by the “Simulated” column, which simulates choices using a fixed logit model for each state; this exercise shows us what the results would look like if all of the variation across states were due to variation in choice sets rather than variation in consumer behavior, and it is very close to the actual results. So even in the case of geographic variation, it appears that the variation we document is driven largely by variation in choice set characteristics and not by heterogeneity across consumers in their ability to choose from a given choice set.
Figure 1.
Distribution of Cost Savings by State
Our previous work documented several choice inconsistencies in Medicare Part D plan choice, and the results reported here suggest that they are pervasive: regardless of age, gender, predicted drug expenditures or the predictability of drug demand consumers underweight out of pocket costs relative to premiums and fail to give sufficient attention to individualized aspects of plans; as a result, they frequently choose plans which are dominated in the sense that alternative plans provide better risk protection at lower cost. There is some evidence that choosing appropriate plans might be especially difficult for the sickest individuals.
Acknowledgments
We are grateful to Jim Hendrix, Chris Messner, Pallavi Mudumby, Steven Pieri and John Porell from Wolters Kluwer for providing data and to the National Institute of Aging for financial support under grant number R01 AG031270.
References
- Abaluck Jason, Gruber Jon. Choice Inconsistencies among the Elderly: Evidence from Plan Choice in the Medicare Part D Program. American Economic Review. 2011 doi: 10.1257/aer.101.4.1180. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duggan M, Morton FS. Imperfect Consumer Choice and Pricing in Medicare Part D. American Economic Review Papers and Proceedings. 2011 Forthcoming. [Google Scholar]
- Iyengar SS, Kamenica E. Choice Overload and Simplicity Seeking. University of Chicago Graduate School of Business Working Paper; 2006. [Google Scholar]