Abstract
Objective
To determine the effects of including diagnostic and utilization data from a secondary payer on readmission rates and hospital profiles.
Data Sources/Study Setting
Veterans Health Administration (VA) and Medicare inpatient and outpatient administrative data for veterans discharged from 153 VA hospitals during FY 2008–2010 with a principal diagnosis of acute myocardial infarction, heart failure, or pneumonia.
Study Design
We estimated hospital-level risk-standardized readmission rates derived using VA data only. We then used data from both VA and Medicare to reestimate readmission rates and compared hospital profiles using two methods: Hospital Compare and the CMS implementation of the Hospital Readmissions Reduction Program (HRRP).
Data Collection/Extraction Methods
Retrospective data analysis using VA hospital discharge and outpatient data matched with Medicare fee-for-service claims by scrambled Social Security numbers.
Principal Findings
Less than 2 percent of hospitals in any cohort were classified discordantly by the Hospital Compare method when using VA-only compared with VA/Medicare data. In contrast, using the HRRP method, 13 percent of hospitals had differences in whether they were flagged as having excessive readmission rates in at least one cohort.
Conclusions
Inclusion of secondary payer data may cause changes in hospital profiles, depending on the methodology used. An assessment of readmission rates should include, to the extent possible, all available information about patients' utilization of care.
Keywords: Readmissions, Veterans Affairs (U.S.), quality assessment, public reporting, Medicare
Hospital readmission has received increased attention from policy makers and researchers since the finding that unplanned readmissions cost Medicare $17.4 billion in 2004 (Jencks, Williams, and Coleman 2009). Rates of 30-day readmissions for selected medical conditions are now publicly reported for hospitals reimbursed by Medicare (i.e., those acute hospitals in the Inpatient Prospective Payment System [IPPS]; Centers for Medicare and Medicaid Services 2012a), and for Veterans Health Administration (VA) hospitals. As of October 2012, the Centers for Medicare and Medicaid Services (CMS), through the Hospital Readmissions Reduction Program (HRRP), began to reduce payments to IPPS hospitals with excess readmissions among patients initially hospitalized for acute myocardial infarction (AMI), heart failure (HF), or pneumonia (PN; Centers for Medicare and Medicaid Services 2012a; Kocher and Adashi 2011). The estimated reduction in payments during the first year of the program was $280 million (Federal Register 2012).
These developments necessitate accurate estimation of readmission rates. However, fragmentation of health care delivery across multiple health care systems and payers may make it difficult to track a patient's history of inpatient admissions and readmissions comprehensively. For instance, among Medicare beneficiaries, only 11 percent have their health care paid by Medicare alone; 15 percent have supplemental coverage through Medicaid, 34 percent through private employer-sponsored plans, and the remainder through other federal plans or self-purchased (Kaiser Family Foundation 2009). VA enrollees frequently receive health care through their Medicare benefits. Of the one-third of veterans eligible for both VA and Medicare, 46 percent use both for outpatient care, and more than 60 percent receive Medicare-reimbursed inpatient care (Hynes et al. 2007). Although prior studies have described the importance of using multiple data sources to estimate the disease burden of a population (Byrne et al. 2006; Rosen et al. 2005), and others have calculated readmission rates using multiple payer data from the Healthcare Cost and Utilization Project (HCUP; Wier et al. 2011), no studies to date have directly examined the effects of including readmissions data from an additional payer.
The goal of this study was to investigate the effects of including outside payer data in an assessment of a health care system's readmission rates. We conducted this study in the VA as it has comprehensive inpatient and outpatient administrative data that can be readily linked to Medicare claims. Compared with a baseline assessment of readmissions that uses VA-only data, the addition of Medicare data may have two direct effects. First, if a patient is discharged from the VA and then readmitted to a Medicare-reimbursed hospital, correct identification of this readmission outcome can be made, whereas with VA-only data it cannot, as these data would not be able to detect hospitalizations outside of the VA system. Second, diagnoses coded in Medicare claims prior to a VA index hospitalization may reveal additional risk information that can be incorporated into a hospital's case mix, enabling more accurate comparison of readmission rates across hospitals. We hypothesize that these effects will (1) increase observed readmission rates; (2) increase the prevalence of diagnostic and procedure-based risk factors used to predict readmission; (3) affect the ratings of hospitals based on the VA Hospital Compare readmission measure; and (4) change which hospitals would be identified as having excess readmissions under the methodology used by CMS to penalize IPPS hospitals.
Although the VA in its role as both a payer and provider makes it unusual in the context of the larger health care environment, the insights gained from studying VA readmissions can be informative to other hospital settings. For instance, Medicare-reimbursed hospitals implementing quality improvement programs to reduce readmissions may be unable to track their patients' readmissions to other hospitals, even though these would be accounted for in Medicare payment reduction calculations (Nasir et al. 2010). As a result, hospitals may not appropriately prioritize their quality improvement interventions. In addition, 16 states currently have a legislative mandate for all-payer claims database reporting (Miller and Peters 2013) that is often used for performance measurement but still may lack complete claims from either one payer source or a variety of payers (Love, Custer, and Miller 2010). Thus, their readmission rates may be underestimated; the extent to which this occurs within hospitals across different conditions and across hospitals will vary, but it will undoubtedly change hospital profiles to some degree.
Methods
Data Sources
This was a retrospective database analysis of veterans aged 65 years and older who were initially hospitalized in an acute-care VA hospital for selected conditions. Veterans under 65 years were not included in the study as readmission rates for only those 65 years and older are reported on the VA and CMS Hospital Compare websites. Administrative data for VA fiscal years (FYs) 2006–2010 (October 1 2005–September 30, 2010) inpatient stays, outpatient encounters, procedures, and surgeries were obtained from the VA National Patient Care Database (VA Information Resource Center 2012b). After identifying index hospitalizations to VA hospitals, we obtained their respective inpatient and outpatient Medicare claims data from the Medicare Provider Analysis and Review (MedPAR) file, Carrier Research Identifiable File (RIF), and Outpatient RIF (VA Information Resource Center 2012a). Any MedPAR records pertaining to skilled nursing facilities (SNFs) and long-stay hospital beds were excluded from the analysis. Medicare records were linked to VA records by scrambled Social Security numbers (VA Information Resource Center 2012a). The VA Information Resource Center (VIReC) provided all Medicare data. Data during FY 2008–2010 were used to identify index hospitalizations, risk factors, and readmissions, while data from FY 2006–2007 were used solely for identifying risk factors. The VA Boston Healthcare System Institutional Review Board approved this study.
Identification of Index Hospitalizations and Readmissions
We first identified index hospitalizations using VA-only inpatient data. An index hospitalization was defined as an acute inpatient discharge during FY 2008–2010 in which the principal diagnosis was AMI, HF, or PN. These condition cohorts were defined in accordance with CMS readmission methodology (Krumholz et al. 2008a,b,c). Similar to prior VA studies (Rosen et al. 2012), nonacute “bedsections” were eliminated from the acute-care files. Distinct episodes of care were combined and treated as continuous if the patient had a same- or next-day subsequent admission to the same hospital for the same condition. Similar to CMS, we excluded in-hospital deaths, discharges against medical advice, and—for the AMI cohort only—discharges on the same day as admission. If a patient was transferred to another acute-care facility, we identified the latter admission as the index hospitalization, but retained the diagnoses from the former admission to capture all the care that the patient received. We then excluded any index hospitalization having another same-cohort index discharge within 30 days prior, to avoid classifying one admission as both an index and a readmission within the same cohort. The three index cohorts were created independently, allowing the possibility of classifying a hospitalization as an index in one cohort and a readmission in another cohort.
After identifying index hospitalizations using VA-only data, we then created a new set of index hospitalizations using both VA and Medicare acute inpatient discharge records. Index hospitalizations in the VA/Medicare analysis were identified as described above, with two additional exclusions: first, a potential VA index hospitalization was excluded if it was preceded by a Medicare same-cohort admission 30 days prior and, second, if it resulted in a transfer to a Medicare-reimbursed hospital. As we were most interested in the effect of Medicare data on VA readmission rates, hospitalizations in Medicare were not eligible to be index hospitalizations.
A readmission was defined as the first inpatient acute-care hospitalization occurring within the 30-day postindex discharge period. In the VA-only analysis, readmission was to a VA hospital only, whereas in the VA/Medicare analysis, a readmission could be either to a VA or Medicare-reimbursed hospital. We excluded any hospitalization for certain revascularization procedures following an AMI index discharge as readmissions, as these may be planned.
Risk Factors and Risk-Adjustment Models
We also followed the CMS methodology in identifying risk factors for each condition cohort, aggregating International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes into 189 mutually exclusive condition categories (CCs). For each index hospitalization, we created a yes/no flag indicating whether each CC was present or not. Eligible diagnoses included secondary diagnoses during the index hospitalization (excluding some that were possible complications of care, such as septicemia/shock, “other infectious diseases,” or diabetes with acute complications), as well as any inpatient or outpatient diagnoses within 1 year prior to the index date of admission. In addition to selected CCs, the AMI model also adjusted for age, gender, history of certain cardiac procedures (coronary artery bypass graft [CABG] and percutaneous coronary intervention), and location of the MI (anterior or other). The HF and PN models adjusted for age, gender, and history of CABG. In the VA-only analysis, we used VA administrative data from FY 2006–2010 to identify patient risk factors, allowing for the full 1-year look-back period for a FY 2008 discharge having up to a 1-year length of stay (i.e., the first eligible index admission date was October 1, 2006). In the VA/Medicare analysis, we used both VA and Medicare data from the same period (FY 2006–2010).
We used hierarchical generalized linear models (HGLMs) to estimate the probability of readmission as a function of patient demographics, CCs, and certain clinical characteristics as described above, clustered at the hospital level (Krumholz et al. 2008a,b,c). We created two models for each condition cohort: the first, the VA-only model, used the index hospitalizations, risk factors, and readmissions identified from VA data only; the second, the VA/Medicare model, used index hospitalizations (VA only), risk factors, and readmissions derived from both data sources. We compared model discrimination using the c-statistic, as well as the range of predicted readmission probabilities.
Creating Hospital Compare Classifications
We classified hospitals as having risk-standardized readmission rates (RSRRs) that were “worse-than-expected,” “as-expected,” or “better-than-expected” in accordance with the methodology used in VA and CMS Hospital Compare. For each index hospitalization, the HGLM estimated the “predicted” probability of readmission using fixed effects (i.e., CCs and patient characteristics) and hospital-level random effects. The model also estimated the “expected” probability of readmission, using only fixed effects. We then calculated the average predicted probabilities, and the average expected probabilities, among all index hospitalizations within a hospital to arrive at a hospital's predicted-to-expected (P/E) readmission ratio. A hospital having a P/E ratio greater than 1 is considered to be performing worse than a “typical” VA hospital, after adjustment for patient case mix. We did not report the P/E ratio or performance category of hospitals with fewer than 25 index hospitalizations during the 3-year period due to small sample sizes, although they were still included in HGLM estimation and in hospital sampling for bootstrapping confidence intervals. Each hospital's risk-standardized readmission rate was calculated as its P/E ratio multiplied by the national observed cohort-specific readmission rate. The RSRR is fundamentally the same as the P/E ratio in indicating a hospital's readmission performance, but because it is a more intuitive way to report results, it is used on the Hospital Compare sites.
We then calculated the 95 percent confidence interval (CI) of each hospital's RSRR with 1,000 bootstrap samples. Each iteration contained an unrestricted random sample of hospitals from the original sample. Hospitals selected more than once within a sample were retained and treated as distinct. The HGLM was then reestimated to generate a hospital-level RSRR in each bootstrapped sample; the 2.5th and 97.5th percentile of each hospital's RSRR distribution defined the lower and upper limit of the 95 percent CI. Hospitals whose upper 95 percent CI was less than the national observed readmission rate were classified as “better-than-expected,” while those with a lower bound greater than the national rate were classified as “worse-than-expected.” Hospitals whose 95 percent CI covered the national rate were classified “as-expected.” We constructed a 3 × 3 table showing the classification of hospitals between the VA-only and VA/Medicare analyses.
Identifying Hospitals with Excess Readmission Ratios under CMS Payment Rules
We classified VA hospitals as having an excess readmission ratio or not, in accordance with the CMS FY 2012 IPPS final rule (Centers for Medicare and Medicaid Services 2012b). Any hospital with a P/E ratio greater than 1 (i.e., an RSRR higher than the national observed readmission rate) in at least one of the three cohorts was classified as having an “excess readmission ratio.” For this study, which was to identify outlier hospitals, our classification was dichotomous (whether the hospital had an excess readmission ratio in at least one cohort), whereas the CMS rule incorporates the magnitude of excess readmissions up to a certain maximum penalty (1 percent of DRG payments in FY 2013, increasing to 3 percent in FY 2015). We constructed a 4 × 4 table showing the number of cohorts (0, 1, 2, or 3) in which hospitals had a P/E ratio greater than 1, in both the VA-only and VA/Medicare analyses. Any hospital not meeting the minimum volume threshold for a particular cohort was classified as not having excess readmissions in that cohort.
Results
Index Hospitalizations and Observed Readmission Rates
Our initial sample included 1,445,211 acute-care VA hospitalizations between FY 2008–2010. From these, we identified 10,636 (0.7 percent of sample) AMI index hospitalizations, 37,203 (2.6 percent) HF index hospitalizations, and 31,068 (2.1 percent) PN index hospitalizations using VA-only data. Observed 30-day readmission rates were 20.7, 22.5, and 17.7 percent, respectively.
After inclusion of Medicare claims data, we eliminated 2.3 percent of the AMI index cohort, 1.9 percent of the HF cohort, and 0.9 percent of the AMI cohort. These were cases where the patient was either transferred to a Medicare-reimbursed hospital or had a same-cohort Medicare-reimbursed hospitalization within 30 days prior to the potential VA index admission. Observed readmission rates for AMI, HF, and PN increased to 24.2, 26.5, and 20.8 percent, respectively, after accounting for readmissions to Medicare-reimbursed hospitals and VA exclusions. Figure1 shows the number of exclusions, index hospitalizations, and readmissions derived from VA-only and VA/Medicare data.
Figure 1.
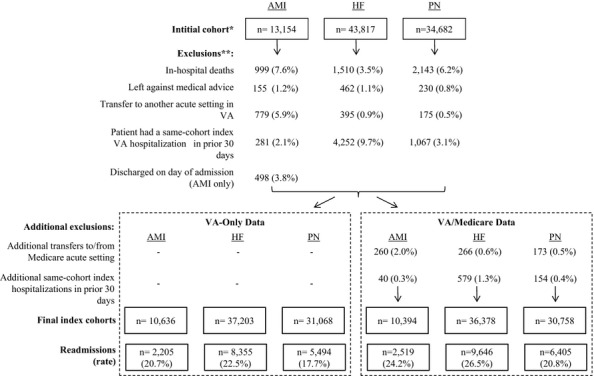
Identification of Index Hospitalizations and Readmissions Using VA-only versus VA/Medicare data: FY2008–2010 Note. *Represents all hospitalizations where principal diagnosis was indicative of the disease cohort. **Exclusions applicable to VA-only data are not mutually exclusive; percentages represent the proportion that meet the exclusion criterion out of the initial cohort.
Risk Factor Prevalence and Model Performance
Table1 reports the prevalence of selected risk factors for readmission (those with the top 10 highest and lowest relative change in any one cohort following the addition of Medicare data). Inclusion of Medicare data prior to the VA index hospitalization increased the prevalence of all CCs used in risk adjustment, although relative changes varied among risk factors and cohorts. For example, the prevalence of “other or unspecified heart disease” (CC 94) increased from 8.6 to 14.1 percent among HF index hospitalizations. “Acute coronary syndrome” (CC 81–82) increased from 20.7 to 26.1 percent among AMI index hospitalizations, and from 11.7 to 15.6 percent for HF index hospitalizations. Prevalence of other conditions increased only slightly; for example, “coronary atherosclerosis” (CC 84) increased from 84.0 to 85.0 percent among AMI index hospitalizations, and “diabetes mellitus with or without complications” (CC 15–20, 119–120) increased from 51.9 to 52.7 percent among AMI index hospitalizations, and from 57.1 to 58.1 percent among HF index hospitalizations. Model discrimination, after adding the Medicare data, was similar to models with VA-only data (shown in Appendix SA2), as were the ranges of predicted probabilities.
Table 1.
Characteristics and Prevalence of Selected Risk Factors for Patients at Index Admission: FY 2008–2010
| AMI | HF | PN | ||||
|---|---|---|---|---|---|---|
| VA-Only | VA/Medicare | VA-Only | VA/Medicare | VA-Only | VA/Medicare | |
| N | 10,636 | 10,394 | 37,203 | 36,378 | 31,068 | 30,758 |
| Age upon admission, mean (SD) | 77.0 (7.6) | 77.0 (7.6) | 77.9 (7.5) | 77.9 (7.5) | 78.2 (7.6) | 78.2 (7.6) |
| Male, % | 98.8 | 98.8 | 98.5 | 98.5 | 98.3 | 98.3 |
| Length of stay, days, mean (SD) | 6.2 (6.7) | 6.3 (6.7) | 5.4 (6.0) | 5.3 (6.0) | 6.1 (6.4) | 6.1 (6.4) |
| Prevalence of risk factors with largest relative change (% of index admissions) | ||||||
| Septicemia/shock (CC2) | – | – | – | – | 2.8 | 4.9 |
| Other or unspecified heart disease (CC 94) | – | – | 8.6 | 14.1 | ||
| Cardio-respiratory failure or shock (CC 79) | – | – | 9.5 | 15.2 | 9.6 | 14.6 |
| Pleural effusion/pneumothorax (CC 114) | – | – | – | – | 5.3 | 8.3 |
| Acute coronary syndrome (CC 81–82) | 20.7 | 26.1 | 11.7 | 15.6 | 4.7 | 6.8 |
| Vertebral fractures (CC 157) | – | – | – | – | 1.4 | 2.0 |
| Protein-calorie malnutrition (CC 21) | 2.3 | 2.9 | 3.0 | 4.1 | 5.7 | 7.1 |
| Fibrosis of lung or other chronic lung disorders (CC 109) | – | – | 5.2 | 6.9 | 8.5 | 10.8 |
| End-stage renal disease or dialysis (CC 129–130) | 2.0 | 2.4 | 1.1 | 1.5 | 1.3 | 1.6 |
| Valvular or rheumatic heart disease (CC 86) | 17.0 | 19.4 | 27.2 | 31.5 | 9.9 | 12.7 |
| Risk factors with least relative change | – | – | – | – | ||
| Drug/alcohol abuse/dependence/psychosis (CC 51–53) | – | – | 17.2 | 18.3 | 21.2 | 22.4 |
| Iron deficiency or other anemias and blood disease (CC 47) | 40.4 | 42.5 | 50.6 | 53.2 | 47.1 | 49.8 |
| Depression (CC 58) | – | – | 17.5 | 18.4 | ||
| Coronary atherosclerosis or angina (CC 83–84) | – | – | 73.5 | 75.5 | 45.2 | 47.7 |
| Other major cancers (CC 9–10) | – | – | – | – | 23.0 | 24.1 |
| Lung or other severe cancers (CC 8) | – | – | – | – | 9.4 | 9.8 |
| Diabetes mellitus (DM) or DM complications (CC 15–20, 119–120) | 51.9 | 52.7 | 57.1 | 58.1 | 40.7 | 42.0 |
| Anterior MI* | 3.3 | 3.4 | – | – | – | – |
| Coronary atherosclerosis (CC 84) | 84.0 | 85.0 | – | – | – | – |
| Other MI* | 5.5 | 5.5 | – | – | – | – |
Describes location of the MI (not CC-based).
AMI, acute myocardial infarction; HF, heart failure; PN, pneumonia.
Changes in Hospital Compare Ratings
We characterized the readmission performance of all VA hospitals having at least 25 index hospitalizations at risk of readmission during the study period (AMI; n = 94, HF; n = 129, PN; n = 130). In the AMI cohort, 93 (98.9 percent) hospitals were classified concordantly between the VA-only and VA/Medicare analyses, while one hospital changed from worse-than-expected to as-expected when Medicare data were included. In the HF cohort, 127 (98.5 percent) hospitals were classified concordantly, and two changed from better-than-expected to as-expected. Finally, in the PN cohort, 128 (98.5 percent) hospitals were classified concordantly, and two changed from as-expected to better-than-expected. These results are presented in Table2.
Table 2.
Change in Hospital Compare Performance Using VA-only versus VA/Medicare Data: FY 2008–2010
| VA/Medicare | ||||
|---|---|---|---|---|
| VA-Only | Worse-Than-Expected | As-Expected | Better-Than-Expected | Total |
| AMI | ||||
| Worse-than-expected | 0 | 1 | 0 | 1 |
| As-expected | 0 | 93 | 0 | 93 |
| Better-than-expected | 0 | 0 | 0 | 0 |
| Total | 0 | 94 | 0 | 94 |
| HF | ||||
| Worse-than-expected | 6 | 0 | 0 | 6 |
| As-expected | 0 | 119 | 0 | 119 |
| Better-than-expected | 0 | 2 | 2 | 4 |
| Total | 6 | 121 | 2 | 129 |
| PN | ||||
| Worse-than-expected | 8 | 0 | 0 | 8 |
| As-expected | 0 | 118 | 2 | 120 |
| Better-than-expected | 0 | 0 | 2 | 2 |
| Total | 8 | 118 | 4 | 130 |
Cell values indicate number of hospitals. Worse-than-expected: hospital's lower risk-standardized readmission rate (RSRR) confidence interval (CI) greater than the national observed rate. As-expected: hospital's RSRR CI covers the national observed rate. Better-than-expected: hospital's upper RSRR CI less than the national observed rate.
AMI, acute myocardial infarction; HF, heart failure; PN, pneumonia.
Changes in Hospitals with Excess Readmission Ratios under CMS Payment Rules
Table3 compares the distribution of the number of cohorts (between 0 and 3) in which hospitals had an excess readmission ratio using each data source. In the baseline VA-only analysis, 29 (22.3 percent) of 130 hospitals had a P/E ratio less than or equal to 1 in all three cohorts. Of these, six (20.7 percent) had an excess readmission ratio in at least one cohort after Medicare data were included. Conversely, 34 (26.2 percent) hospitals in the VA/Medicare analyses had no excess readmission ratio in any cohort. Of these, 11 (32.4 percent) had an excess readmission ratio in at least one cohort in the VA-only analysis. Overall, 17 (13.1 percent) of the 130 hospitals would see a change in whether they had an excess readmission ratio in at least one cohort.
Table 3.
Hospitals with Excess Readmission Ratios in VA-only versus VA/Medicare Analyses: FY 2008–2010
| VA/Medicare | |||||
|---|---|---|---|---|---|
| N Cohorts in Which Hospitals Had Excess Readmission Ratio | |||||
| VA-only | 0 | 1 | 2 | 3 | Total |
| 0 | 23 | 5 | 1 | 0 | 29 |
| 1 | 10 | 29 | 10 | 0 | 49 |
| 2 | 1 | 8 | 21 | 6 | 36 |
| 3 | 0 | 1 | 3 | 12 | 16 |
| Total | 34 | 43 | 35 | 18 | 130 |
Cell values indicate number of hospitals.
Discussion
Our study of VA readmission rates examined 3 years of data to determine the extent to which veterans' utilization of Medicare-reimbursed health care affected observed readmission rates and risk factor prevalence, and changed the performance classification of hospitals' readmission rates using two currently implemented methods. Overall, our findings indicate that risk-standardized readmission models are sensitive to the omission of outside payer data. While the increase in risk factor prevalence and effects on hospital profiling for any single clinical condition were modest, there was a substantial increase in observed readmission rates and a change in which 13 percent of VA hospitals would have been flagged as having excess readmission ratios in at least one cohort applying the CMS IPPS payment rule.
Increases in observed readmission rates were related to cases in which a veteran had a readmission to a Medicare-reimbursed hospital, but not a VA hospital, in the 30-day postindex period. These readmissions would not have been detected using VA-only data, leading to underestimation of national VA observed rates (i.e., a readmission outcome of “no” when the true outcome was “yes”). Further changes in observed rates were driven, to a lesser degree, by additional VA index hospitalization exclusions related to the addition of Medicare data, as the set of index hospitalizations between analyses was slightly different. Exclusion of a potential VA index hospitalization due to a prior 30-day same-cohort Medicare hospitalization occurred most often in the HF cohort (1.3 percent of initially identified index hospitalizations). In addition, it was necessary to exclude VA index hospitalizations in cases where the patient was transferred to a Medicare-reimbursed hospital, rather than discharged to a nonacute setting as indicated by VA-only data. This occurred most frequently in the AMI cohort (2.0 percent of initially identified index hospitalizations). Had these transfers not been identified, the transferring VA hospital would have been unfairly flagged for any readmission occurring within 30 days of the transfer. A reliable discharge destination variable may be useful for identifying these transfers from VA administrative data.
Increases in the prevalence of risk factors were generally modest despite the well-documented high rate of dual utilization among VA enrollees. Prior studies (Byrne et al. 2006; Rosen et al. 2005) have found that estimates of veterans' disease burden increased significantly with the inclusion of Medicare data (i.e., individual patients often had diagnoses coded in Medicare claims records that were missing from VA administrative records). Several factors could explain differences in these findings. First, our sample represented elderly veterans who were hospitalized for one of three serious medical conditions—AMI, HF, or PN—while prior studies were more representative of the general VA patient population. Second, these prior studies used different methods (i.e., Verisk DxCG Relative Risk Scores) to estimate general disease burden related to health care cost, while our study used selected CCs and other clinical and demographic characteristics thought to be associated with risk of readmission. The modest additional risk information gained from Medicare claims likely explains why there was no improvement in model discrimination in the VA/Medicare analyses.
This study is particularly relevant to VA policy with respect to using readmissions as a hospital performance measure. The VA now publicly reports hospital RSRRs for veterans age 65 and older on VA Hospital Compare, and these are calculated using index hospitalizations, readmissions, and risk factors obtained from VA-only data. Our results show that users of VA Hospital Compare would see little difference in hospital performance ratings after inclusion of Medicare data, as the additional data changed the performance rating of less than 2 percent of hospitals in any cohort. However, we recommend that VA Hospital Compare incorporate Medicare data into its results regardless of this particular result, to improve the accuracy and comprehensiveness of readmission outcomes and risk factors. Interestingly, CMS Hospital Compare does include VA and Medicare data to identify index hospitalizations, risk factors, and readmissions for profiling VA and Medicare-reimbursed hospitals. However, VA hospital performance is presented relative to several thousand nonfederal hospitals, limiting its value for comparing VA hospitals directly with one another. The P/E ratios (and therefore RSRRs) of low-volume VA hospitals in CMS Hospital Compare are determined almost entirely by the national mean (i.e., mostly by Medicare-reimbursed hospitals), because the random effects are estimated using shrinkage estimators (Ash et al. 2011; Tilson and Hoffman 2012). In these models, the shrinkage estimators pull the estimated random effects of small hospitals toward the mean, resulting in a low-volume hospital's predicted number of readmissions (fixed and random effects) being similar to its expected number of readmissions (fixed effects only), and thus a P/E ratio close to 1. Finally, if the VA were to follow the lead of CMS and implement an all-condition (as opposed to the current three disease cohorts) measure, the effects of including Medicare data may be more substantial if dual utilization patterns were different among the general VA patient population compared with the disease-specific cohorts in this study.
Inclusion of Medicare data would have more noticeable hospital profiling implications—affecting one of every eight VA hospitals—if the VA were to adopt the CMS IPPS payment rule to identify hospitals with excess readmissions across multiple cohorts. Of note, this scenario is not unlikely, given the budgetary constraints currently faced by the VA and the increasing emphasis on reducing VA readmission rates through numerous quality improvement initiatives. The P/E ratios used to identify hospitals with excess readmission ratios are affected by the inclusion of additional risk-adjustment diagnoses and readmission outcomes. Inaccurate estimation of hospital P/E ratios due to omission of Medicare data would have several negative consequences. Hospitals with truly “good” RSRRs may be unfairly penalized, low performing hospitals may escape penalties, and confidence in readmission rates as a quality measure could decline. If the VA adopts a readmission policy that incorporates a similar methodology (i.e., a P/E point estimate without a CI), all available non-VA utilization should be incorporated.
This study can also inform policy decisions outside the VA. For example, Medicare-reimbursed hospitals with excess readmissions are subject to payment reductions. Many Medicare-reimbursed hospitals have information only on readmissions at their hospital; readmissions to other Medicare-reimbursed hospitals are unknown (Nasir et al. 2010). Thus, at the individual hospital level, hospitals may be underestimating their own readmission rates, and by different amounts for different conditions, resulting in the potential for incorrect prioritization of quality improvement efforts.
Our results may also be relevant for states that use all-payer claims databases to calculate outcome measures such as readmission rates. Sixteen states currently maintain or are developing all-payer claims databases, typically used to calculate trends in health care utilization and hospital performance metrics (Love, Custer, and Miller 2010), inform quality improvement efforts by providing more comprehensive information about the diseases leading to readmission (Friedman, Jiang, and Elixhauser 2008), and identify regional variation in population-level readmission rates (Finison 2010). Policy makers should be aware that hospital readmission rates calculated in the absence of comprehensive data from all payers (e.g., from the VA or out-of-state hospitals) are likely to be inaccurate, potentially misleading, and may affect hospital profiles, particularly with respect to payment penalties. Nonetheless, all-payer claims databases are an important first step in facilitating more accurate hospital profiling and appropriately targeted quality improvement initiatives. We recommend that all states devote resources to developing such databases to improve quality assessment at their hospitals. Of note, should this type of data integration occur in non-VA settings, changes in performance ratings are likely to be driven by additional knowledge of readmission outcomes rather than improved information about patient risk.
A major strength of our study is that the VA is an ideal system to test these effects because it routinely collects reliable longitudinal data (Rosen et al. 2005) and a high proportion of veterans utilize outside health care systems (most notably, Medicare) for which data are available to VA researchers. This study also has certain limitations. We examined only Medicare as an additional source of utilization, omitting other secondary sources, such as Medicaid, TRICARE, Medicare Advantage, or commercial insurance. In 2011, over 80 percent of elderly VA enrollees had Medicare coverage and about 25 percent of enrollees had non-VA coverage in two or more federal plans (Kizer 2012). For this reason, we believe the positive findings of this study may still underestimate the true effects.
In conclusion, veterans discharged from VA acute-care hospitals often return for subsequent care to both VA and Medicare-reimbursed hospitals. The inclusion of Medicare data led to changes in hospitals' P/E ratios across one or more cohorts, resulting in substantial changes to which hospitals were identified as having excess P/E ratios under the methodology used by CMS for payment penalties. These findings may be of interest to other health care systems whose patients utilize multiple systems or payers. An assessment of a health care system's readmission rates should include, to the extent possible, all available information about patients' care from outside sources.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was funded by VA Health Services Research and Development grant # IIR 09-369.
Disclosures: None.
Disclaimers: None.
Supporting Information
Appendix SA1: Author Matrix.
Appendix SA2: Model Performance in VA-only and VA/Medicare Analyses: FY 2008–2010.
References
- Ash A, Fienberg S, Louis T, Normand S, Stukel T. Utts J. 2011. The COPSS-CMS White Paper Committee. Statistical Issues on Assessing Hospital Performance ” [accessed on June 6, 2013]. Available at http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Downloads/Statistical-Issues-in-Assessing-Hospital-Performance.pdf.
- Byrne MM, Kuebeler M, Pietz K. Petersen LA. Effect of Using Information from Only One System for Dually Eligible Health Care Users. Medical Care. 2006;44(8):768–73. doi: 10.1097/01.mlr.0000218786.44722.14. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Acute Care Hospital Inpatient Prospective Payment System. Washington, DC: Department of Health and Human Services; 2012a. Payment System Fact Sheet Series. [Google Scholar]
- Centers for Medicare and Medicaid Services. 2012b. Hospital Readmissions Reduction Program [accessed on May 9, 2013]. Available at http://cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html/
- Federal Register. 2012. “ Medicare Program. Hospital Inpatient Prospective Payment Systems for Acute Care Hospitals and the Long-Term Care Hospital Prospective Payment System and Fiscal Year 2013 Rates; Hospitals' Resident Caps for Graduate Medical Education Payment Purposes; Quality Reporting Requirements for Specific Providers and for Ambulatory Surgical Centers; Final Rule ” [accessed on May 9, 2013]. Available at http://www.gpo.gov/fdsys/pkg/FR-2012-08-31/pdf/2012-19079.pdf.
- Finison K. Tri-State Variation in Health Services Utilization & Expenditures in Northern New England, Commercially Insured Population Under Age 65 in Maine, New Hampshire, & Vermont. Portland, ME: Onpoint Health Data; 2010. [Google Scholar]
- Friedman B, Jiang HJ. Elixhauser A. Costly Hospital Readmissions and Complex Chronic Illness. Inquiry. 2008;45(4):408–21. doi: 10.5034/inquiryjrnl_45.04.408. [DOI] [PubMed] [Google Scholar]
- Hynes DM, Koelling K, Stroupe K, Arnold N, Mallin K, Sohn MW, Weaver FM, Manheim L. Kok L. Veterans' Access to and Use of Medicare and Veterans Affairs Health Care. Medical Care. 2007;45(3):214–23. doi: 10.1097/01.mlr.0000244657.90074.b7. [DOI] [PubMed] [Google Scholar]
- Jencks SF, Williams MV. Coleman EA. Rehospitalizations among Patients in the Medicare Fee-For-Service Program. New England Journal of Medicine. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation. Medicare: A Primer. Menlo Park, CA: Kaiser; 2009. [Google Scholar]
- Kizer KW. Veterans and the Affordable Care Act. Journal of the American Medical Association. 2012;307(8):789–90. doi: 10.1001/jama.2012.196. [DOI] [PubMed] [Google Scholar]
- Kocher RP. Adashi EY. Hospital Readmissions and the Affordable Care Act: Paying for Coordinated Quality Care. Journal of the American Medical Association. 2011;306(16):1794–5. doi: 10.1001/jama.2011.1561. [DOI] [PubMed] [Google Scholar]
- Krumholz H, Normand S, Keenan P, Lin Z, Bhat K, Wang Y, Ross J, Schuur J, Stauffer B, Bernheim S, Epstein A, Herrin J, Federer J, Mattera J, Wang Y, Mulvey G. Schreiner GC. 2008a. Yale University/Yale-New Haven Hospital Center for Outcomes Research and Evaluation Hospital 30-Day Heart Failure Readmission Measure: Methodology.” Submitted by; prepared for Centers for Medicaid and Medicare.
- Krumholz HM, Normand ST, Keenan PS, Desai MM, Lin Z, Drye EE, Bhat K. Schreiner GC. 2008b. Yale University/Yale-New Haven Hospital Center for Outcomes Research and Evaluation “ Hospital 30-Day Pneumonia Readmission Measure: Methodology.” Submitted by; prepared for Centers for Medicaid and Medicare.
- Krumholz HM, Normand ST, Keenan PS, Desai MM, Lin Z, Drye EE, Curtis JP, Bhat KR. Schreiner GC. 2008c. Yale University/Yale-New Haven Hospital Center for Outcomes Research and Evaluation “ Hospital 30-Day Acute Myocardial Infarction Readmission Measure: Methodology.” Submitted by; prepared for Centers for Medicaid and Medicare.
- Love D, Custer W. Miller P. All-Payer Claims Databases: State Initiatives to Improve Healthcare Transparency. The Commonwealth Fund. 2010;99:10. [PubMed] [Google Scholar]
- Miller P. Peters A. APCD Legislation: Review of Current Practices and Critical Elements. Durham, NH: APCD Council; 2013. [Google Scholar]
- Nasir K, Lin Z, Bueno H, S-L T, Normand EE, Drye PSKeenan. Krumholz HM. Is Same Hospital Readmission Rate a Good Surrogate for All-Hospital Readmission Rate? Medical Care. 2010;48:477–81. doi: 10.1097/MLR.0b013e3181d5fb24. [DOI] [PubMed] [Google Scholar]
- Rosen AK, Gardner J, Montez M, Loveland S. Hendricks A. Dual-System Use: Are There Implications for Risk Adjustment and Quality Assessment? American Journal of Medical Quality. 2005;20(4):182–94. doi: 10.1177/1062860605275791. [DOI] [PubMed] [Google Scholar]
- Rosen AK, Itani KM, Cevasco M, Kaafarani HM, Hanchate A, Shin M, Shwartz M, Loveland S, Chen Q. Borzecki A. Validating the Patient Safety Indicators in the Veterans Health Administration: Do They Accurately Identify True Safety Events? Medical Care. 2012;50(1):74–85. doi: 10.1097/MLR.0b013e3182293edf. [DOI] [PubMed] [Google Scholar]
- Tilson S. Hoffman G. Addressing Medicare Hospital Readmissions. Washington, DC: Congressional Research Service; 2012. [Google Scholar]
- VA Information Resource Center. 2012a. . “ VA/CMS Data Overview ” [accessed on May 9, 2013]. Available at http://www.virec.research.va.gov/Index-VACMS.htm.
- VA Information Resource Center. 2012b. . “ VHA National Patient Care Database (NPCD) ” [accessed on May 9, 2013]. Available at http://www.virec.research.va.gov/NPCD/Overview.htm.
- Wier LM, Barrett ML, Steiner C. Jiang HJ. 2011. All-Cause Readmissions by Payer and Age, 2008. HCUP Statistical Brief #115. Agency for Healthcare Research and Quality, Rockville, MD ” [accessed on May 9, 2013]. Available at http://www.hcup-us.ahrq.gov/reports/statbriefs/sb115.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Model Performance in VA-only and VA/Medicare Analyses: FY 2008–2010.


