Abstract
Objective
To examine receipt of early childhood caries preventive services (ECCPS) in two states' Medicaid programs before and after the implementation of reimbursement to medical primary care providers (M-PCPs).
Data Sources
Enrollment and claims data from the Florida and Texas Medicaid programs for children ≤54 months of age during the period 2006–2010.
Study Design
We conducted time trend-adjusted, difference-in-differences analyses by using modified Poisson regressions combined with generalized estimating equations (GEEs) to analyze the effect of M-PCP reimbursement on the likelihood that an enrollee had an ECCPS visit after controlling for age, sex, health status, race/ethnicity, geographic location, and enrollment duration.
Data Extraction Methods
Enrollment data were linked to claims data to create a panel dataset with child-month observations.
Principal Findings
Reimbursement to M-PCPs was associated with an increased likelihood of ECCPS receipt in general and topical fluoride application specifically in both states.
Conclusions
Reimbursement to M-PCPs can increase access to ECCPS. However, ECCPS receipt continues to fall short of recommended care, presenting opportunities for performance improvement.
Keywords: Medicaid, reimbursement, early childhood caries, preventive services
Early childhood caries (ECC) is a significant national problem that disproportionately affects low-income children, and its prevalence is increasing (Tomar and Reeves 2009). ECC has significant short- and long-term adverse consequences (Tinanoff and Reisine 2009). ECC is associated with increased risk of future caries (Gray, Marchment, and Anderson 1991; Reisine, Litt, and Tinanoff 1994; O'Sullivan and Tinanoff 1996), missed school days (Gift, Reisine, and Larach 1992; Hollister and Weintraub 1993), hospitalization and emergency room visits (Sheller, Williams, and Lombardi 1997; Griffin et al. 2000), and, in rare cases, death (Casamassimo et al. 2009). These adverse outcomes are avoidable through ECC preventive services (ECCPS). A randomized clinical trial found that fluoride varnish treatment, combined with parent counseling, can reduce caries by up to 50 percent in high-risk children (Weintraub et al. 2006).
National guidelines recommend that children have a dental visit by 12 months of age and receive preventive care at regular intervals thereafter (American Academy of Pediatrics Section on Pediatric Dentistry and Oral Health 2008; American Academy of Pediatric Dentistry 2013). The most common recall interval is 6 months. However, the American Academy of Pediatric Dentistry recommends that children at higher caries risk get check-ups, including topical fluoride application, more often (American Academy of Pediatric Dentistry 2013). Medicaid eligibility has been identified as a risk factor for ECC (American Dental Association 2011). Untreated dental caries occurs among 25 percent of children living in poverty compared with 10.5 percent of children living above poverty (Dye, Li, and Thorton-Evans 2012). Comprehensive dental benefits are required in Medicaid and the Children's Health Insurance Program, which cover 35 percent of all U.S. children (DeNavas-Walt, Proctor, and Smith 2012), but only 31 percent of publicly insured children ages 0–5 years receive dental services (Centers for Medicare and Medicaid Services 2012).
Although ECC is largely preventable (Savage et al. 2004; Weintraub et al. 2006; Azarpazhooh and Main 2008), it is difficult to reach preschool aged children for caries prevention. Publicly insured, preschool aged children are more likely to receive medical care than dental care (Bouchery 2012a,b). Consequently, 44 state Medicaid programs have implemented policies to reimburse medical primary care providers (M-PCPs), typically including physicians, physician assistants, and advanced registered nurse practitioners, to provide ECCPS. The specific services reimbursed varies across states but may include an examination of the oral cavity, caries risk assessment, anticipatory guidance, topical fluoride application, and referral to a dental home (American Academy of Pediatrics 2013).
Despite widespread adoption, there is little scientific evidence on the effects of M-PCP reimbursement on ECCPS receipt, with published studies from only two states. A North Carolina study examined ECCPS receipt subsequent to policy implementation and found steady growth in the number of medical visits that included ECCPS, but it did not use a pre–post study design to evaluate changes in ECCPS receipt (Rozier et al. 2010). Studies of Wisconsin's Medicaid program, which used pre–post designs, found that M-PCP reimbursement was associated with increased claims rates for fluoride varnish treatment with almost one-half of the increase associated with M-PCPs (Okunseri et al. 2009, 2010).
This study extends existing research by analyzing the effect of M-PCP reimbursement on ECCPS receipt for Medicaid-enrolled children in Texas and Florida, which are the second and fourth most populous states, respectively, and account for 15 percent of Medicaid-enrolled children nationally (Kaiser Family Foundation 2013; U.S. Census Bureau 2011). These states are among the most diverse with significant representation of African-American and Hispanic populations (Brewer and Suchan 2001), which disproportionately experience low access to dental care (Edelstein and Chinn 2009). In 2008, the Florida and Texas Medicaid programs implemented M-PCP ECCPS reimbursement for children ages 0–4 years. We used secondary data from these programs to test our central hypothesis that M-PCP reimbursement has improved access to ECCPS.
Methodologically, we extend existing research by including a control group of children not subject to M-PCP reimbursement and adopting an analytic strategy that allows us to better isolate the treatment effect by controlling for intrinsic differences between the treatment and control groups, secular time trends, and differential time trends between the two groups. In addition to controlling for standard demographic characteristics, we also control for the children's health status and explicitly incorporate enrollment duration into our model.
Policy Background
Effective April 15, 2008, Florida Medicaid reimbursed M-PCPs for ECCPS for children ages 6–42 months (Florida Agency for Health Care Administration 2008). Providers submit claims for reimbursement using Current Procedural Terminology (CPT) code 99499, modifier SC, which represents a bundled set of services, including oral evaluation and risk assessment, fluoride varnish application, parental counseling, and referral to a dentist. Reimbursement was $27.00 during the study period and was consistent with reimbursement to dental providers who received $16.00 for Current Dental Terminology (CDT) code 0145, which is “oral evaluation for a patient under 3 years of age and counseling with primary caregiver,” and $11.00 for CDT code 1206, which is “topical application of fluoride varnish” (American Dental Association 2012). The oral evaluation includes taking oral and physical health histories, evaluation of caries risk, development of an oral health regimen, and parental counseling. M-PCPs can bill for CPT 99499 SC every 3 months concurrently with a Child Health Check-Up visit, immunizations, or as a standalone visit. Florida's policy was implemented as an administrative change and did not require legislative action. ECCPS training is offered and encouraged, but not required, for reimbursement (Florida Agency for Health Care Administration 2011).
Effective September 1, 2008, Texas Medicaid reimbursed M-PCPs for ECCPS for children ages 6–35 months. Provider training is required, and providers submit claims using CPT code 99429, modifier U5, which covers intermediate oral evaluation, fluoride varnish application, anticipatory guidance, and referral to a dental home. The procedure must be billed in conjunction with a medical check-up code (99381, 99382, 99391, 99392) and was reimbursed at $34.16 (in addition to the check-up reimbursement). This policy was implemented as part of a comprehensive program to increase the percentage of children getting dental check-ups, which in turn is part of a broader set of initiatives implemented in response to a class action lawsuit that alleged that Texas did not adequately provide Medicaid Early Periodic Screening, Diagnosis, and Treatment (EPSDT) services (Frew v. Suehs 2011; Texas Health and Human Services Commission 2011). Texas Medicaid also implemented the First Dental Home initiative in March 2008, which targets pediatric and general dentists. First Dental Home visits include caries risk assessment, prophylaxis, oral hygiene instructions for the child's primary caregiver, fluoride varnish application, anticipatory guidance, and establishment of a recall schedule. Dental providers bill for this visit using CDT code D0145 and must complete training to receive the enhanced reimbursement of $144.97.
Data Sources and Variable Specification
Study Sample and Data Sources
The study populations of interest (the “treatment” groups) were children ages 6–42 months in Florida and 6–35 months in Texas enrolled for at least 1 month between January 1, 2006–December 31, 2010. The respective age ranges reflect those for which M-PCPs can be reimbursed in each state. Because we did not have a comparison group of children the same age who were not subject to the policy change, we identified as control groups children in close age proximity of 1–12 months older than the oldest children in the treatment groups: ages 43–54 months in Florida and 36–47 months in Texas. We used person-level administrative enrollment data provided by the Florida and Texas Medicaid programs to identify our samples and extracted the children's age, sex, race/ethnicity, place of residence, and monthly enrollment. Enrollment records were linked to claims data that included ICD-9-CM diagnosis codes, CDT codes, and CPT codes. The Florida Medicaid sample represents children enrolled in the fee-for-service (FFS) and primary care case management (PCCM) program components; children enrolled in managed care were excluded due to lack of claims data (20 percent of age-eligible children). Children with missing managed care encounter data were older (28.7 months vs. 27.2 months) and more likely to be nonHispanic black and reside in urban areas. We retained children who moved between program components, omitting months with managed care enrollment, and our models controlled for enrollment duration in the FFS/PCCM components. Texas Medicaid data represent children enrolled in the PCCM and managed care programs.
We constructed our analytic data file using child-month observations, which offer important advantages over child-year observations for greater precision in estimating population-averaged treatment effects. First, the policy changes occurred in the middle of a calendar year; therefore, we can more precisely measure the before and after periods. Second, the timing of children's visits to medical and dental providers is influenced by recommended periodicity schedules and perceived needs, both of which vary according to the child's age. Periodicity schedules for children <3 years old for both well-child and ECCPS visits are defined in months rather than years (i.e., clinical guidelines recommend multiple visits per year). Aggregating the data could result in omitting important information. Third, many children have partial-year enrollments, and monthly data allow for a more refined analysis of service receipt within the context of the child's current enrollment span; instead of controlling for the overall number of months a child was enrolled during the year, we are able to control for the number of months enrolled to date for each child-month observation. After omitting observations with missing data for any of the variables used in the multivariate analyses, the resulting sample sizes were 1,029,867 children representing 12,810,136 child-month observations in Florida and 2,087,192 children representing 32,101,885 child-month observations in Texas. Our Institutional Review Board approved this project.
Variables and Measures
ECCPS Visits
Our outcome variable is a dichotomous indicator of whether the child had an ECCPS visit during the month with either a dental or medical provider. ECCPS provided by M-PCPs were identified by CPT code 99499 SC in Florida and CPT code 99429 U5 in Texas, respectively. To identify ECCPS from dental providers, we used CDT codes that reflect standard diagnostic and preventive services: oral evaluation (D0145, D0120, D0150), prophylaxis (D1120), topical fluoride or fluoride varnish (D1201, D1203, D1206), and oral hygiene instructions (D1330). We counted a visit as an ECCPS visit if any of these services was provided because the primary concern has been the large percentage of children who receive no preventive services. This broad definition leads to a higher prepolicy rate, resulting in a more conservative estimate of the impact of M-PCP reimbursement. To test the sensitivity of our results to this approach, we also defined a narrow definition of ECCPS from dental providers restricted to topical fluoride or fluoride varnish. We focus on fluoride application due to its demonstrated efficacy in caries prevention (Weintraub et al. 2006; Azarpazhooh and Main 2008) and because it is the most frequently reimbursed M-PCP oral health service (American Academy of Pediatrics 2013). We refer to these two definitions as ECCPS-Broad and ECCPS-Fluoride.
Reimbursement Policy
A variable was created that is equal to 1 for the postpolicy period (April 2008–December 2010 for Florida; September 2008–December 2010 for Texas) and 0 for the prepolicy period. For Texas, this variable also captures the First Dental Home initiative implemented 6 months earlier. The pre–post periods for the First Dental Home and M-PCP initiatives are largely overlapping, making it difficult to tease out independent effects; thus, we examined the combined effect.
Time Trends
As described in the next section, our identification strategy uses a difference-in-differences approach that adjusts for time trends. Our time trend variables include a count variable with values 1–60 for each month of the observation period and the square of this variable to allow for nonlinearity. We also included a set of 12 dichotomous indicators for each calendar month to control for seasonality in service use.
Individual Health and Demographic Characteristics
We used the Clinical Risk Groups, which has been validated for identifying children with special health care needs (CSHCN), to classify children into health status groups (Bethell and Read 2002; Neff et al. 2002). For classification, children ≤12 months old must be enrolled ≥3 months, and children >12 months old must be enrolled ≥6 months. Children were classified into one of five categories: healthy, significant acute conditions (e.g., meningitis and traumatic brain injury), minor chronic conditions (e.g., attention deficit disorder), moderate chronic conditions (e.g., asthma and diabetes), or major chronic conditions (e.g., cystic fibrosis and cancer). We also controlled for the children's age cohort in 6-month intervals, race/ethnicity, and sex. An indicator of rural versus urban place of residence was constructed using categorization D of the Rural-Urban Commuting Areas (RUCA) codes (Economic Research Service USDA 2000; WWAMI Rural Health Research Center).
Enrollment Duration
We controlled for enrollment duration by calculating for each child-month the number of continuous months that the child was enrolled through that month. Months of continuous enrollment was reset to 1 in the first month of each new enrollment spell for children with multiple spells. We then created a categorical variable signifying how long a child had been continuously enrolled: <6 months, 6–11 months, 12–23 months, or ≥24 months.
Analytic Approach
To identify the treatment effect of M-PCP reimbursement on ECCPS visits, we used difference-in-differences (DD) estimation, which controls for bias stemming from intrinsic differences between the treatment and control groups as well as intervening time factors between the pre- and post-intervention periods. We examined two treatment groups: the “full” treatment group of children meeting the age eligibility for M-PCP reimbursement (6–42 months in Florida; 6–35 months in Texas) and a “restricted” treatment group comprised of the oldest 12-month subset in each state (31–42 months in Florida; 24–35 months in Texas). Due to changes in oral cavity development and differences in dental service utilization as children age, the restricted treatment group is a closer comparison to the control group. However, the M-PCP reimbursement policies target the youngest children precisely because they traditionally have had especially low dental service utilization; therefore, it is important to also examine the treatment effect on the entire targeted population. Consequently, we estimated and report models for both treatment groups.
A key assumption of standard DD models is that the time trends for the dependent variable would be identical for the treatment and control groups in the absence of the intervention. Our use of monthly data allowed us to compare the time trends for the treatment and control groups in the prepolicy period, and this assumption was not consistently upheld. Across Florida and Texas for the full and restricted samples, three of the four cases showed statistically significant, sizable time trend differences. For the Florida sample, we estimated a positive time trend effect for the control group that was one-third of the time trend effect for the full treatment group and two-thirds of the time trend effect for the restricted treatment group. In Texas, the time trend effect for the control group was 59 percent of that compared to the full treatment group. Only for the Texas restricted and control samples did the time trends appear similar. Consequently, we constructed time trend-adjusted DD models that took into account differences in the time trends. The time trend adjustment is illustrated by the following general equations:
| 1 |
and
 |
2 |
where Y reflects the outcome of interest, policy is a pre–post dichotomous indicator, treatment is a dichotomous indicator of whether the individual is in the treatment or control group, time is a count variable for time measured monthly, X is a vector of covariates, and u is the error term. Equation (1) reflects a linear time trend adjustment, and equation (2) allows for a nonlinear time trend. This approach modifies the standard DD approach by using our monthly data to estimate separate time trends for the treatment and control groups observed in the pre- and postpolicy periods, thereby allowing us to extrapolate the prepolicy time trends for the treatment and control groups into the postpolicy period to measure more accurately any intrinsic differences between the treatment and control groups. The standard DD estimator is given by the coefficient on the interaction term between the policy and treatment variables (δ). The time trend-adjusted treatment effects corresponding to equations (1) and (2) can be determined through the standard DD algebraic calculations and are given in equations (3) and (4) below:
| 3 |
and
| 4 |
where φ1 and φ2 are the coefficients on the triple interaction terms between the policy, treatment and time or time squared variables, respectively and time is any given month in the postpolicy period.
Because it is uncommon for children to have more than one ECCPS visit per month, we specified our outcome variable as a binary indicator of zero versus one or more visits and used modified Poisson regression combined with generalized estimating equations (GEE). It has been demonstrated elsewhere that the traditional DD estimator extends to nonlinear models (Karaca-Mandic, Norton, and Dowd 2012; Puhani 2012). GEEs are frequently used in panel data analyses when there are repeated measures for the same individual over time and the measures are likely to be correlated (Liang and Zeger 1986). GEEs also provide population-averaged effects rather than individual predictors, which is appropriate because our aim was to examine overall program effects. We specified a Poisson distribution with a log link and robust estimation of standard errors. Using modified Poisson regression to analyze correlated observations produces results similar to those from log binomial regression while overcoming common convergence problems (Zou 2004; Yelland, Salter, and Ryan 2011). SAS 9.3.1 (SAS Institute Inc., Cary, NC, USA) was used for dataset preparation, and Stata/MP 12.1 (StataCorp, LP, College Station, TX, USA) was used to conduct the analyses.
Results
Descriptive Results
Figure1 summarizes per member month (PMM) receipt of ECCPS over time for the full treatment, restricted treatment and control groups for ECCPS-Broad and ECCPS-Fluoride. Overall, both the pre- and postpolicy rates were considerably lower in Florida than in Texas. For example, ECCPS-Broad receipt for the full treatment group in Florida in January 2006 was 0.008 PMM compared to 0.055 PMM in Texas, increasing to 0.028 PMM and 0.130 PMM, respectively, in December 2010. The prepolicy ECCPS-Fluoride rates were lower than the ECCPS-Broad rates (e.g., 0.003 PMM vs. 0.008 PMM in Florida and 0.039 PMM vs. 0.055 PMM in Texas for the full treatment groups in January 2006), indicating that a subset of children who had any ECCPS service from dentists received fluoride services specifically. The prepolicy ECCPS rates were highest for children in the control group and lowest for children in the full treatment groups (e.g., 0.032 PMM vs. 0.008 PMM in Florida and 0.092 PMM vs. 0.055 PMM in Texas in January 2006). In Florida, the full treatment group showed a discernible increase in rates during the postpolicy period compared to both the restricted treatment and control groups, and fluoride receipt among the full treatment group exceeded that among the restricted treatment and control groups by the end of the observation period. In Texas, both the full and restricted treatment groups demonstrated substantial increases in ECCPS receipt during the postpolicy period, exceeding the control group rates by the end of the observation period. In both states, the policy apparently had a greater impact on increasing rates for fluoride specifically compared to the broader set of ECCPS.
Figure 1.
ECCPS-Broad Visits Per Member Month, Treatment and Control Groups*;
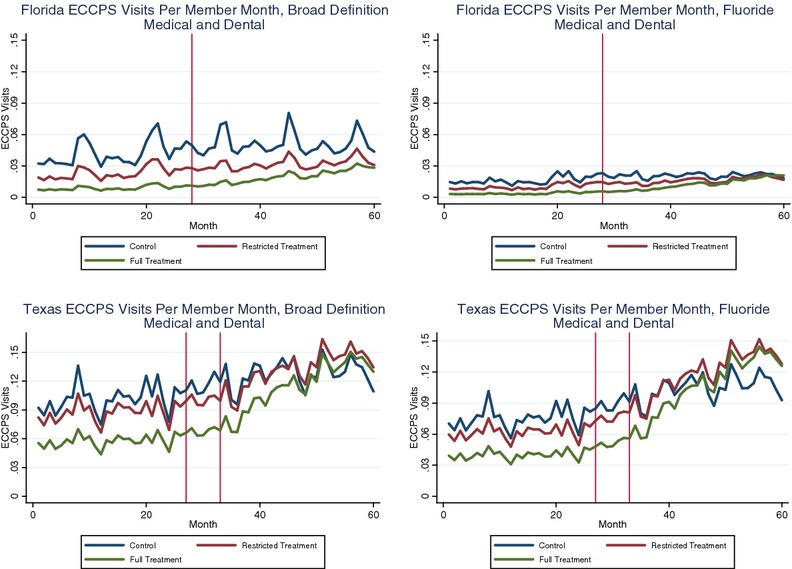
Note. *;The month of policy implementation in each state is indicated by the vertical lines. In Texas, there are two vertical lines: the first indicates the implementation of the First Dental Home targeted at dental providers, and the second indicates the implementation of M-PCP reimbursement targeted at medical providers.
Figure2 breaks out the ECCPS-Broad and ECCPS-Fluoride time trends for the full treatment group by dental and medical providers. In Texas, ECCPS-Broad from both dental providers and M-PCPs increased. In Florida, there was modest growth in ECCPS-Broad from dental providers, but most of the increase was attributable to M-PCPs. The relative contribution of M-PCPs in the postpolicy period was considerably greater in Florida compared to Texas. For example, in September 2010, the M-PCP ECCPS-Broad rate was approximately 75 percent of the dental provider rate in Florida (0.014 PMM and 0.018 PMM, respectively) compared to 29 percent in Texas (0.032 PMM and 0.112 PMM, respectively). The impact of M-PCPs on ECCPS-Fluoride rates in Florida was even greater: the M-PCP rate was 0.014 PMM in September 2010, twice the rate of 0.007 PMM from dental providers. In Texas, the ECCPS-Broad and ECCPS-Fluoride rates were more similar in the postpolicy period (compared to Florida) because the First Dental Home Initiative encompassed a bundled set of services, including fluoride.
Figure 2.
ECCPS-Broad and ECCPS-Fluoride Visits Per Member Month by Provider Type, Full Treatment Group*;
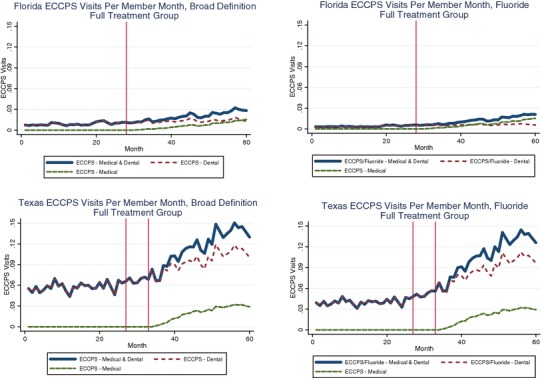
Note. *;The month of policy implementation in each state is indicated by the vertical lines. In Texas, there are two vertical lines: the first indicates the implementation of the First Dental Home targeted at dental providers, and the second indicates the implementation of M-PCP reimbursement targeted at medical providers.
Table1 reports by sample characteristics the percentage of enrollment months in which ECCPS-Broad were received before and after policy implementation for the full treatment and control groups in each state. In each state, there was a higher percentage of enrollment months with ECCPS receipt in the postpolicy period for both the treatment and control groups and within all subgroups. There were greater percentage increases for the treatment groups compared to the control groups. In Florida, there was a 130 percent increase (from 0.85 to 1.96 percent) in the treatment group compared to an 18 percent increase (from 3.96 to 4.67 percent) in the control group. In Texas, there was a 94 percent increase in the treatment group compared to a 20 percent increase in the control group. In addition, there were variations by sample characteristics. Hispanic and nonHispanic black children (vs. nonHispanic whites), CSHCN (vs. those classified as healthy), and children with longer enrollment spans were more likely before and after the policy to receive ECCPS.
Table 1.
Percentage of Enrollment Months with ECCPS Receipt before and after PCP Reimbursement by Child Characteristics
| Florida (12,810,136 Enrollment Months) | Texas (32,101,885 Enrollment Months) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Treatment | Control | Treatment | Control | |||||||||||||
| Prepolicy | Postpolicy | Prepolicy | Postpolicy | Prepolicy | Postpolicy | Prepolicy | Postpolicy | |||||||||
| Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | Total Months (N) | % with ECCPS | |
| Overall | 4,277,721 | 0.85 | 5,930,784 | 1.96 | 966,243 | 3.96 | 1,635,388 | 4.67 | 12,304,918 | 5.08 | 12,038,610 | 9.86 | 3,802,989 | 8.70 | 3,955,368 | 10.44 |
| Child's sex | ||||||||||||||||
| Female (ref) | 2,159,859 | 0.82 | 2,904,017 | 1.96 | 468,569 | 3.95 | 789,941 | 4.70 | 5,997,336 | 5.05 | 5,879,433 | 9.83 | 1,855,392 | 8.73 | 1,924,974 | 10.47 |
| Male | 2,117,862 | 0.89 | 3,026,767 | 1.97 | 497,674 | 3.96 | 845,447 | 4.65 | 6,307,582 | 5.10 | 6,159,177 | 9.88 | 1,947,597 | 8.66 | 2,030,394 | 10.42 |
| Child's race/ethnicity | ||||||||||||||||
| NonHispanic White (ref) | 1,228,957 | 0.81 | 1,737,766 | 1.78 | 280,248 | 3.75 | 503,723 | 3.80 | 2,090,897 | 2.98 | 2,120,278 | 6.78 | 576,825 | 6.23 | 626,004 | 8.12 |
| NonHispanic Black | 1,049,878 | 0.94 | 1,513,335 | 1.84 | 264,094 | 4.41 | 424,492 | 5.02 | 1,685,500 | 3.61 | 1,653,139 | 7.33 | 541,871 | 7.00 | 563,941 | 8.79 |
| Hispanic | 1,378,316 | 0.91 | 1,927,508 | 2.28 | 307,631 | 3.92 | 517,556 | 5.51 | 7,761,046 | 6.03 | 7,001,925 | 11.07 | 2,472,398 | 9.68 | 2,626,877 | 11.38 |
| Other/unknown | 620,570 | 0.68 | 752,175 | 1.83 | 114,270 | 3.50 | 189,617 | 3.94 | 767,475 | 4.37 | 1,263,268 | 11.61 | 211,895 | 8.24 | 138,546 | 9.99 |
| Child's health status | ||||||||||||||||
| Healthy (ref) | 2,541,015 | 0.86 | 3,392,766 | 1.86 | 598,549 | 4.11 | 989,963 | 4.58 | 7,486,924 | 4.91 | 7,189,359 | 9.28 | 2,455,304 | 8.43 | 2,491,563 | 10.14 |
| Significant acute | 431,801 | 0.86 | 684,755 | 2.30 | 63,623 | 4.65 | 125,300 | 6.18 | 2,001,483 | 5.50 | 2,144,882 | 11.47 | 429,079 | 10.18 | 501,252 | 11.78 |
| Minor chronic | 122,080 | 1.32 | 193,246 | 2.78 | 39,580 | 4.96 | 68,149 | 6.34 | 366,637 | 6.66 | 442,160 | 12.42 | 151,056 | 10.59 | 200,433 | 12.17 |
| Moderate chronic | 416,265 | 1.16 | 664,305 | 2.60 | 101,513 | 4.52 | 177,685 | 6.00 | 1,031,783 | 5.99 | 1,038,929 | 11.21 | 302,748 | 9.95 | 337,011 | 11.49 |
| Major chronic | 105,495 | 1.19 | 191,718 | 2.56 | 24,505 | 3.86 | 45,040 | 5.33 | 177,373 | 5.57 | 206,373 | 11.10 | 49,341 | 9.89 | 63,693 | 11.85 |
| Unassigned | 661,065 | 0.48 | 803,994 | 1.25 | 138,473 | 2.26 | 229,251 | 2.58 | 1,240,718 | 4.10 | 1,016,907 | 7.82 | 415,461 | 6.99 | 361,416 | 8.54 |
| Place of residence | ||||||||||||||||
| Urban (ref) | 3,779,864 | 0.81 | 5,254,203 | 1.90 | 847,981 | 3.71 | 1,447,686 | 4.39 | 10,403,923 | 5.27 | 10,222,378 | 10.19 | 3,218,233 | 8.86 | 3,362,617 | 10.54 |
| Rural | 497,857 | 1.16 | 676,581 | 2.50 | 118,262 | 5.70 | 187,702 | 6.82 | 1,900,995 | 4.01 | 1,816,232 | 7.96 | 584,756 | 7.82 | 592,751 | 9.90 |
| Continuous enrollment | ||||||||||||||||
| <6 months (ref) | 2,161,377 | 0.55 | 2,263,393 | 1.27 | 312,609 | 3.19 | 427,043 | 3.38 | 7,209,454 | 3.77 | 6,068,749 | 8.47 | 1,818,408 | 8.14 | 1,508,393 | 9.95 |
| 6–11 months | 1,216,676 | 0.88 | 1,475,927 | 1.93 | 277,157 | 4.25 | 284,868 | 4.18 | 3,309,246 | 6.24 | 3,363,444 | 10.67 | 969,235 | 8.76 | 894,835 | 10.18 |
| 12–23 months | 819,118 | 1.46 | 1,470,618 | 2.32 | 313,026 | 4.31 | 357,984 | 4.74 | 1,644,841 | 8.10 | 2,148,453 | 11.96 | 790,619 | 9.41 | 793,961 | 10.61 |
| ≥24 months | 80,550 | 2.54 | 720,846 | 3.51 | 63,451 | 4.73 | 565,493 | 5.85 | 141,377 | 9.47 | 457,964 | 12.34 | 224,727 | 10.39 | 758,179 | 11.57 |
Multivariate Results
Table2 reports the results from the modified Poisson regression modeling, using GEE, for ECCPS-Broad and ECCPS-Fluoride. Models estimated for the full and restricted treatment groups are reported. We estimated models using linear and nonlinear time trend specifications. The time squared triple interaction terms were insignificant in the nonlinear models for Florida, whereas these terms were significant for Texas. Therefore, we report the linear time trend specifications for Florida and the nonlinear time trend models for Texas. The results in the linear and nonlinear models were qualitatively similar, and the selected models reflect more conservative estimates of the treatment effects in both states. In all of the models, the coefficient on policy × treatment is negative, the coefficient on policy × treatment × time is positive, and the coefficient on policy × treatment × time2 is negative.
Table 2.
Association of M-PCP Reimbursement with ECCPS Receipt, Modified Poisson Regression*
| Florida—Linear Time Trend | Texas—Nonlinear Time Trend | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ECCPS-Broad | ECCPS-Fluoride | ECCPS-Broad | ECCPS-Fluoride | |||||||||
| Coef. | Robust SE | p-value | Coef. | Robust SE | p-value | Coef. | Robust SE | p-value | Coef. | Robust SE | p-value | |
| Full treatment group | ||||||||||||
| Policy | 0.07478 | 0.02466 | .002 | 0.12679 | 0.03360 | <.001 | −0.34068 | 0.05065 | <.001 | −0.64864 | 0.05482 | <.001 |
| Treatment | −3.57800 | 0.03313 | <.001 | −3.13642 | 0.03959 | <.001 | −0.37071 | 0.00760 | <.001 | −0.48753 | 0.00871 | <.001 |
| Policy × Treatment | −0.14002 | 0.03184 | <.001 | −0.31241 | 0.04357 | <.001 | −1.72751 | 0.05919 | <.001 | −2.00962 | 0.06379 | <.001 |
| Time | 0.00620 | 0.00086 | <.001 | 0.00901 | 0.00121 | <.001 | −0.00064 | 0.00069 | .352 | −0.01034 | 0.00078 | <.001 |
| Policy × Time | −0.00187 | 0.00096 | .051 | −0.00291 | 0.00134 | .029 | 0.01955 | 0.00232 | <.001 | 0.04123 | 0.00252 | <.001 |
| Treatment × Time | 0.01219 | 0.00113 | <.001 | 0.01809 | 0.00164 | <.001 | −0.00139 | 0.00085 | .102 | −0.00213 | 0.00099 | .031 |
| Policy × Treatment × Time | 0.00719 | 0.00125 | <.001 | 0.01345 | 0.00178 | <.001 | 0.07775 | 0.00271 | <.001 | 0.09693 | 0.00293 | <.001 |
| Time2 | 0.00013 | 0.00002 | <.001 | 0.00042 | 0.00002 | <.001 | ||||||
| Policy × Time2 | −0.00027 | 0.00003 | <.001 | −0.00065 | 0.00003 | <.001 | ||||||
| Treatment × Time2 | 0.00014 | 0.00002 | <.001 | 0.00024 | 0.00003 | <.001 | ||||||
| Policy × Treatment × Time2 | −0.00075 | 0.00004 | <.001 | −0.00103 | 0.00004 | <.001 | ||||||
| Constant | −3.76890 | 0.01798 | <.001 | −4.62370 | 0.02501 | <.001 | −4.16310 | 0.00841 | <.001 | −4.19689 | 0.00918 | <.001 |
| Restricted treatment group | ||||||||||||
| Policy | 0.18676 | 0.02452 | <.001 | 0.25658 | 0.03300 | <.001 | −0.22055 | 0.05137 | <.001 | −0.45551 | 0.05582 | <.001 |
| Treatment | −0.96623 | 0.02066 | <.001 | −0.78674 | 0.02854 | <.001 | −0.18307 | 0.00845 | <.001 | −0.23128 | 0.00968 | <.001 |
| Policy × Treatment | −0.11606 | 0.03570 | .001 | −0.22956 | 0.04750 | <.001 | −0.60882 | 0.07198 | <.001 | −0.85831 | 0.07805 | <.001 |
| Time | 0.00780 | 0.00083 | <.001 | 0.01178 | 0.00114 | <.001 | 0.00550 | 0.00068 | <.001 | −0.00350 | 0.00077 | <.001 |
| Policy × Time | −0.00738 | 0.00093 | <.001 | −0.01005 | 0.00127 | <.001 | 0.01032 | 0.00236 | <.001 | 0.02842 | 0.00257 | <.001 |
| Treatment × Time | 0.00393 | 0.00117 | .001 | 0.00594 | 0.00163 | <.001 | −0.00068 | 0.00100 | .496 | −0.00317 | 0.00117 | .007 |
| Policy × Treatment × Time | 0.00311 | 0.00134 | .020 | 0.00607 | 0.00182 | .001 | 0.02442 | 0.00327 | <.001 | 0.04042 | 0.00355 | <.001 |
| Time2 | −0.00004 | 0.00002 | .023 | 0.00023 | 0.00002 | <.001 | ||||||
| Policy × Time2 | −0.00008 | 0.00003 | .018 | −0.00042 | 0.00004 | <.001 | ||||||
| Treatment × Time2 | 0.00004 | 0.00003 | .191 | 0.00014 | 0.00003 | <.001 | ||||||
| Policy × Treatment × Time2 | −0.00017 | 0.00004 | <.001 | −0.00040 | 0.00005 | <.001 | ||||||
| Constant | −3.77999 | 0.01889 | <.001 | −4.65044 | 0.02651 | <.001 | −2.83832 | 0.00843 | <.001 | −3.03620 | 0.00938 | <.001 |
Additional covariates not reported include the children's age, health status, race/ethnicity, sex, rural/urban location, and enrollment duration.
To understand the overall treatment effect, however, it is necessary to examine the combined effects rather than the individual coefficients. We used the coefficients to calculate the treatment effects represented by equations (3) and (4) for Florida and Texas, respectively. To facilitate interpretation, we exponentiated the resulting values to represent the treatment effects as incidence rate ratios (IRRs), which can be interpreted in the same manner as relative risks. A value greater than one indicates the treatment group is more likely to have an ECCPS visit compared to the control group, and a value less than one indicates the treatment group is less likely to have an ECCPS visit compared to the control group. In Table3, we report the average treatment effect during the postpolicy period as well as the treatment effects at 6, 12, 18, and 24 months after policy implementation. Our results indicate overall positive treatment effects in both states with smaller effects among the restricted treatment groups compared to the full treatment groups. On average, children in the full treatment group were 20 percent more likely in Florida (IRR = 1.20) and 25 percent more likely in Texas (IRR = 1.25) to have an ECCPS-Broad visit. In Florida, the treatment effect was more pronounced for fluoride with an IRR of 1.33. In Texas, the results for ECCPS-Broad and ECCPS-Fluoride were similar. Among the restricted treatment group, the average treatment effect was a 16 percent increase in the likelihood of an ECCPS-Broad visit in Texas compared to 2 percent in Florida with similar results for ECCPS-Fluoride. An examination of the IRRs at 6, 12, 18, and 24 months after policy implementation indicates an increasing trend over time for Florida and a positive but decreasing trend for Texas, consistent with the linear and nonlinear specifications, respectively. The restricted treatment group in Florida experienced an immediate negative treatment effect in the first 6 months of the postpolicy period, which became positive within 12 months of policy implementation.
Table 3.
PostPolicy Treatment Effects Reported as Incidence Rate Ratios
| Florida | Texas | |||||||
|---|---|---|---|---|---|---|---|---|
| Full Treatment | Restricted Treatment | Full Treatment | Restricted Treatment | |||||
| Broad ECCPS | Fluoride | Broad ECCPS | Fluoride | Broad ECCPS | Fluoride | Broad ECCPS | Fluoride | |
| Average treatment effect | 1.20 | 1.33 | 1.02 | 1.04 | 1.25 | 1.22 | 1.16 | 1.15 |
| No. of months postpolicy | ||||||||
| 6 | 1.10 | 1.14 | 0.99 | 0.97 | 1.16 | 1.20 | 1.08 | 1.11 |
| 12 | 1.15 | 1.24 | 1.01 | 1.01 | 1.28 | 1.29 | 1.15 | 1.17 |
| 18 | 1.20 | 1.34 | 1.02 | 1.04 | 1.33 | 1.29 | 1.20 | 1.19 |
| 24 | 1.25 | 1.45 | 1.04 | 1.08 | 1.32 | 1.20 | 1.25 | 1.18 |
Sensitivity Testing
Although the nonlinear time trend adjustment model was a better fit for the Texas data, we repeated the analyses using a linear time trend specification for comparison purposes. The treatment effects were greater in the linear specification with average treatment effects for ECCPS-Broad of IRR = 1.41 and IRR = 1.20 for the full and restricted treatment groups, respectively. In addition, we estimated models with the policy = 1 period starting 6 months earlier with the First Dental Home implementation instead of waiting until M-PCP reimbursement also was in effect; the results were qualitatively similar. We also estimated the models without the time trend adjustment; in these models, the standard DD estimator represented by the coefficient on policy × treatment was positive and significant, indicating an overall positive treatment effect in the post policy period. Because we observed relatively flat ECCPS rates for dental providers in Florida, we estimated models that regressed ECCPS from dental providers on policy to evaluate whether there was a substitution effect: that is, whether M-PCP ECCPS provision was associated with decreased provision by dentists. For the full treatment group, the coefficients on policy × treatment and policy × treatment × time were statistically significant, and we found an average negative treatment effect of 3 percent (IRR = 0.97) for ECCPS-Broad and 13 percent (IRR = 0.87) for ECCPS-Fluoride. For the restricted treatment group, the average treatment effects also were negative, but not statistically significant. Thus, our results suggest a potential substitution effect among the full treatment group.
Because the treatment and control groups were based on the children's age, it was possible for children to age out of the treatment group into the control group. Thus, we conducted sensitivity analyses that evaluated the results separately for children who aged into the control group (“switchers”) to those who were exclusively in either the treatment or the control group during the observation period (“non-switchers”). We did not omit children who switched between the treatment and control groups in our main analyses because the non-switchers were disproportionately younger and enrolled for shorter enrollment duration than the switchers and, therefore, the resulting sample would not have been representative of the overall population. We hypothesized that our more inclusive approach would result in more conservative treatment effect estimates. In both states, in the full treatment groups, there were large, positive average treatment effects among the non-switchers for ECCPS-Broad (IRR = 2.7 in Texas and IRR = 3.1 in Florida) and ECCPS-Fluoride (IRR = 2.8 in Texas and IRR = 3.2 in Florida). These effects were statistically significant except for ECCPS-Fluoride in Florida. Smaller positive average treatment effects were observed among the switchers. There was greater variation among the restricted treatment group, which had a greater proportion of children who were switchers. In Florida, the average treatment effects were positive for switchers and non-switchers, but the results were not statistically significant for non-switchers. In the Texas restricted treatment group, there were negative average treatment effects among non-switchers and positive average treatment effects among switchers. In models without the time trend adjustment, the standard DD estimator was positive and significant for switchers and non-switchers in the full and restricted treatment groups. Collectively, our sensitivity tests support the robustness of our findings of positive average treatment effects in the Florida and Texas Medicaid programs.
Discussion
We found statistically significant treatment effects of M-PCP reimbursement on ECCPS receipt after controlling for intrinsic differences between the treatment and control groups, time trends, demographic and health characteristics, and enrollment duration. Both the pre- and postpolicy ECCPS rates in Texas Medicaid were substantially higher than those in Florida. This is consistent with annual EPSDT data from the Centers for Medicare and Medicaid Services indicating that Texas Medicaid is among the states with the highest percentages of children receiving dental services and Florida has the lowest percentage (Centers for Medicare and Medicaid Services 2012). It is noteworthy that both states had positive, statistically significant average treatment effects for both ECCPS-Broad and ECCPS-Fluoride. Moreover, our extensive sensitivity analyses suggest that, on net, our estimated treatment effects are likely conservative. These observations lend confidence that our findings from these two states may be generalizable to the broad range of prevailing utilization rates in other states.
Despite the observed gains, ECCPS receipt still falls short of recommended care. Professional guidelines recommend that children have their first dental visit by age 1 year with recall visits at least every 6 months for children at increased caries risk (American Academy of Pediatric Dentistry 2013). Two visits per year per child translate into a recommended dental visit rate of 0.167 PMM. In 2010, average ECCPS receipt was 0.026 PMM for the full treatment group and 0.051 for the control group in Florida, or 16 and 30 percent of the recommended rate, respectively. The comparable rates for Texas were 0.137 PMM for the treatment group and 0.131 PMM for the control group, or 82 and 78 percent of the recommended rate, respectively. ECCPS receipt in most states is likely between these rates given that Florida and Texas represent the lower and upper ranges of Medicaid dental utilization. Therefore, there is significant opportunity to further improve access to ECCPS among preschool-aged children.
There are limits to our study that should be considered when interpreting our results. Although both states require the reimbursed M-PCP procedure to include an oral evaluation, parent counseling, and fluoride varnish application, we did not observe whether and to what extent there is variation in the actual content of the visit. A separate study using provider surveys, observation, or medical record reviews would be required to explore this further. The Florida Medicaid analyses were limited by lack of managed care claims data. Because the impacts of managed care on utilization vary based on the characteristics of the specific managed care program, we are reluctant to speculate on the implications for our findings. Our analysis of M-PCP reimbursement in Texas Medicaid was confounded by the almost simultaneous implementation of the First Dental Home targeting dental providers for the same age group. However, we believe this confounding was offset by the benefit of being able to observe the impact of more comprehensive reform. We prospectively identified as a limitation the violation of the DD model assumption of identical time trends in ECCPS receipt for the treatment and control groups prior to the intervention. The use of monthly data allowed us to overcome this limitation by extrapolating the prepolicy time trends for the treatment and control groups into the postpolicy period to thereby measure more accurately any intrinsic differences. Our treatment and control groups were not mutually exclusive because children could age from the treatment group into the control group. However, sensitivity tests conducted among children who were exclusively in either the treatment or control categories indicated positive average treatment effects among this subgroup that were substantially larger than the average treatment effects in the full treatment sample. Finally, our analyses focused on the effects of reimbursement policies. However, other factors, such as administrative burdens, time constraints, and lack of confidence in providing ECCPS, serve as barriers to ECCPS provision by both dental and medical providers (Borchgrevin, Snyder, and Gehshan 2008; Gehshan, Snyder, and Paradise 2008; Herndon et al. 2010; Isong et al. 2011).
Despite these limitations, our analyses provide the most rigorous evidence to date of the impact of M-PCP reimbursement on ECCPS receipt and provide strong support of positive effects for access to ECCPS in general and fluoride in particular. These services are critical to reducing the prevalence of ECC among low-income children, thereby improving their health outcomes and quality of life. However, opportunities for continued improvement remain, and ongoing research is needed to identify the most effective strategies for improving the percentage of preschool-aged Medicaid enrollees who receive ECCPS.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported by NIH/NIDCR Grant Number R03DE021701. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. The authors appreciate the support of the Florida Agency for Health Care Administration and the Texas Health and Human Services Commission, which provided the data used in these analyses. The authors are grateful to Sandra Decker, who provided helpful feedback on an earlier draft, and to two anonymous referees for their constructive and insightful suggestions. Finally, the authors would like to acknowledge and thank Howard Xu for excellent programming assistance in preparing the analytic datasets.
Disclosures: None.
Disclaimers: None.
Supporting Information
Appendix SA1: Author Matrix.
References
- American Academy of Pediatric Dentistry. 2013. Guideline on Periodicity of Examination, Preventive Dental Services, Anticipatory Guidance/Counseling, and Oral Treatment for Infants, Children, and Adolescents “[accessed on December 7, 2013]. Available at http://www.aapd.org/policies/
- American Academy of Pediatrics. 2013. State Medicaid Payment for Caries Prevention Services by Non-Dental Professionals ” [accessed on December 19, 2013]. Available at http://www2.aap.org/oralhealth/docs/OHReimbursementChart.pdf.
- American Academy of Pediatrics Section on Pediatric Dentistry and Oral Health. Policy Statement: Preventive Oral Health Intervention for Pediatricians. Pediatrics. 2008;122(6):1387–94. doi: 10.1542/peds.2008-2577. [DOI] [PubMed] [Google Scholar]
- American Dental Association. 2011. Caries Risk Assessment Form: Age 0-6 ” [accessed on December 19, 2013]. Available at http://www.ada.org/sections/professionalResources/pdfs/topics_caries_under6.pdf.
- American Dental Association. CDT 2013: Dental Procedure Codes. Chicago, IL: American Dental Association; 2012. [Google Scholar]
- Azarpazhooh A. Main PA. Fluoride Varnish in the Prevention of Dental Caries in Children and Adolescents: A Systematic Review. Journal of Canadian Dental Association. 2008;74(1):73–9. [PubMed] [Google Scholar]
- Bethell C. Read D. 2002. Oregon Health and Science University “ Approaches to Identifying Children and Adults with Special Health Care Needs: A Resource Manual for State Medicaid Agencies and Managed Care Organizations.”: The Child and Adolescent Health Measurement Initiative [accessed on May 5, 2012]. Available at http://cahmi.org/ViewDocument.aspx?DocumentID=120.
- Borchgrevin A, Snyder A. Gehshan S. 2008. “ The Effects of Medicaid Reimbursement Rates on Access to Dental Care ” [accessed on June 9, 2013]. Available at http://nashp.org/sites/default/files/CHCF_dental_rates.pdf?q=Files/CHCF_dental_rates.pdf.
- Bouchery E. 2012a. Centers for Medicare and Medicaid Services “ Utilization of Dental Services among Medicaid-Enrolled Children.” MAX Medicaid Policy Brief #9.
- Bouchery E. 2012b. Centers for Medicare and Medicaid Services “ Utilization of Well-Child Care among Medicaid-Enrolled Children.” MAX Medicaid Policy Brief #10.
- Brewer CA. Suchan TA. Mapping Census 2000: The Geography of U.S. Diversity. Washington, DC: U.S. Government Printing Office; 2001. [Google Scholar]
- Casamassimo PS, Thikkurissy S, Edelstein BL. Maiorini E. Beyond the DMFT: The Human and Economic Cost of Early Childhood Caries. Journal of the American Dental Association. 2009;140(6):650–7. doi: 10.14219/jada.archive.2009.0250. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. Statistical Abstract of the United States, 2012. Washington, DC: U.S. Census Bureau; 2011. [Google Scholar]
- Centers for Medicare and Medicaid Services. 2012. . “ Early and Periodic Screening, Diagnosis, & Treatment: 2011 National Data ” [accessed on April 29, 2013]. Available at http://www.medicaid.gov/Medicaid-CHIP-Program-Information/By-Topics/Benefits/Early-Periodic-Screening-Diagnosis-and-Treatment.html.
- DeNavas-Walt C, Proctor BD. Smith J. Income, Poverty, and Health Insurance Coverage in the United States: 2011. Washington: Bureau of the Census; 2012. [Google Scholar]
- Dye BA, Li X. Thorton-Evans G. Oral Health Disparities as Determined by Selected Healthy People 2020 Oral Health Objectives for the United States, 2009-2010. NCHS Data Brief. 2012;104:1–8. [PubMed] [Google Scholar]
- Economic Research Service USDA. 2000. . “ Rural-Urban Commuting Area Codes ” [accessed on May 27, 2013]. Available at http://www.ers.usda.gov/Data/RuralUrbanCommutingAreaCodes/
- Edelstein BL. Chinn CH. Update on Disparities in Oral Health and Access to Dental Care for America's Children. Academic Pediatrics. 2009;9(6):415–9. doi: 10.1016/j.acap.2009.09.010. [DOI] [PubMed] [Google Scholar]
- Florida Agency for Health Care Administration. 2008. . “ Coverage of Fluoride Varnish Application by Non-Dentists. Florida Medicaid Remittance Banner Announcements & Health Care Alerts ” [accessed on May 27, 2013]. Available at http://portal.flmmis.com/FLPublic/Provider_ProviderSupport/Provider_ProviderSupport_ProviderAlerts/tabId/43/Default.aspx.
- Florida Agency for Health Care Administration. 2011. . “ Florida Medicaid Provider Bulletin ” [accessed on May 27, 2013]. Available at http://portal.flmmis.com/FLPublic/Provider_ProviderSupport/Provider_ProviderSupport_ProviderBulletins/tabId/40/Default.aspx.
- Frew v. Suehs. 2011. 775 F. Supp. 2d 930. U.S. Dist. Court, ED Texas, Sherman Division.
- Gehshan S, Snyder M. Paradise J. Filling an Urgent Need: Improving Children's Access to Dental Care in Medicaid and CHIP. Washington, DC: National Academy for State Health Policy and Kaiser Commission on Medicaid and the Uninsured; 2008. [Google Scholar]
- Gift HC, Reisine ST. Larach DC. The Social Impact of Dental Problems and Visits. American Journal of Public Health. 1992;82(12):1663–8. doi: 10.2105/ajph.82.12.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MM, Marchment MD. Anderson RJ. The Relationship between Caries Experience in the Deciduous Molars at 5 Years and in First Permanent Molars of the Same Child at 7 Years. Community Dental Health. 1991;8(1):3–7. [PubMed] [Google Scholar]
- Griffin SO, Gooch BF, Beltran E, Sutherland JN. Barsley R. Dental Services, Costs, and Factors Associated with Hospitalization for Medicaid-Eligible Children, Louisiana 1996-97. Journal of Public Health Dentistry. 2000;60(1):21–7. doi: 10.1111/j.1752-7325.2000.tb03287.x. [DOI] [PubMed] [Google Scholar]
- Herndon JB, Tomar SL, Lossius MN. Catalanotto FA. Preventive Oral Health Care in Early Childhood: Knowledge, Confidence, and Practices of Pediatricians and Family Physicians in Florida. Journal of Pediatrics. 2010;157(6):1018–24. doi: 10.1016/j.jpeds.2010.05.045. e1–2. [DOI] [PubMed] [Google Scholar]
- Hollister MC. Weintraub JA. The Association of Oral Status with Systemic Health, Quality of Life, and Economic Productivity. Journal of Dental Education. 1993;57(12):901–12. [PubMed] [Google Scholar]
- Isong IA, Silk H, Rao SR, Perrin JM, Savageau JA. Donelan K. Provision of Fluoride Varnish to Medicaid-Enrolled Children by Physicians: The Massachusetts Experience. Health Services Research. 2011;46(6 Pt 1):1843–62. doi: 10.1111/j.1475-6773.2011.01289.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation. 2013. . “ Monthly Medicaid Enrollment for Children ” [accessed on April 29, 2013]. Available at http://statehealthfacts.org/comparemaptable.jsp?ind=612&cat=4.
- Karaca-Mandic P, Norton EC. Dowd B. Interaction Terms in Nonlinear Models. Health Services Research. 2012;47(1 Pt 1):255–74. doi: 10.1111/j.1475-6773.2011.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY. Zeger SL. Longitudinal Data-Analysis Using Generalized Linear-Models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- Neff JM, Sharp VL, Muldoon J, Graham J, Popalisky J. Gay JC. Identifying and Classifying Children with Chronic Conditions Using Administrative Data with the Clinical Risk Group Classification System. Ambulatory Pediatrics. 2002;2(1):71–9. doi: 10.1367/1539-4409(2002)002<0071:iaccwc>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Okunseri C, Szabo A, Jackson S, Pajewski NM. Garcia RI. Increased Children's Access to Fluoride Varnish Treatment by Involving Medical Care Providers: Effect of a Medicaid Policy Change. Health Services Research. 2009;44(4):1144–56. doi: 10.1111/j.1475-6773.2009.00975.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okunseri C, Szabo A, Garcia RI, Jackson S. Pajewski NM. Provision of Fluoride Varnish Treatment by Medical and Dental Care Providers: Variation by Race/Ethnicity and Levels of Urban Influence. Journal of Public Health Dentistry. 2010;70(3):211–9. doi: 10.1111/j.1752-7325.2010.00168.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Sullivan DM. Tinanoff N. The Association of Early Dental Caries Patterns with Caries Incidence in Preschool Children. Journal of Public Health Dentistry. 1996;56(2):81–3. doi: 10.1111/j.1752-7325.1996.tb02401.x. [DOI] [PubMed] [Google Scholar]
- Puhani PA. The Treatment Effect, the Cross Difference, and the Interaction Term in Nonlinear “Difference-in-Differences” Models. Economics Letters. 2012;115(1):85–7. [Google Scholar]
- Reisine S, Litt M. Tinanoff N. A Biopsychosocial Model to Predict Caries in Preschool Children. Pediatric Dentistry. 1994;16(6):413–8. [PubMed] [Google Scholar]
- Rozier RG, Stearns SC, Pahel BT, Quinonez RB. Park J. How a North Carolina Program Boosted Preventive Oral Health Services for Low-Income Children. Health Affairs (Millwood) 2010;29(12):2278–85. doi: 10.1377/hlthaff.2009.0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage MF, Lee JY, Kotch JB. Vann WF., Jr Early Preventive Dental Visits: Effects on Subsequent Utilization and Costs. Pediatrics. 2004;114(4):e418–23. doi: 10.1542/peds.2003-0469-F. [DOI] [PubMed] [Google Scholar]
- Sheller B, Williams BJ. Lombardi SM. Diagnosis and Treatment of Dental Caries-Related Emergencies in a Children's Hospital. Pediatric Dentistry. 1997;19(8):470–5. [PubMed] [Google Scholar]
- Texas Health and Human Services Commission. 2011. . “ Frew V. Suehs Strategic Medical and Dental Initiatives Summary Update “[accessed on June 4, 2013]. Available at http://www.hhsc.state.tx.us/about_hhsc/AdvisoryCommittees/Frew/Reports/April-2011.pdf.
- Tinanoff N. Reisine S. Update on Early Childhood Caries since the Surgeon General's Report. Academic Pediatrics. 2009;9(6):396–403. doi: 10.1016/j.acap.2009.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomar SL. Reeves AF. Changes in the Oral Health of US Children and Adolescents and Dental Public Health Infrastructure since the Release of the Healthy People 2010 Objectives. Academic Pediatrics. 2009;9(6):388–95. doi: 10.1016/j.acap.2009.09.018. [DOI] [PubMed] [Google Scholar]
- Weintraub JA, Ramos-Gomez F, Jue B, Shain S, Hoover CI, Featherstone JD. Gansky SA. Fluoride Varnish Efficacy in Preventing Early Childhood Caries. Journal of Dental Research. 2006;85(2):172–6. doi: 10.1177/154405910608500211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WWAMI Rural Health Research Center . “ RUCA Data ” [accessed on May 27, 2013]. Available at http://depts.washington.edu/uwruca/ruca-uses.php.
- Yelland LN, Salter AB. Ryan P. Performance of the Modified Poisson Regression Approach for Estimating Relative Risks from Clustered Prospective Data. American Journal of Epidemiology. 2011;174(8):984–92. doi: 10.1093/aje/kwr183. [DOI] [PubMed] [Google Scholar]
- Zou G. A Modified Poisson Regression Approach to Prospective Studies with Binary Data. American Journal of Epidemiology. 2004;159(7):702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


