Abstract
Objective
The coefficients of friction (COFs) of aesthetic ceramic and stainless steel brackets used in conjunction with stainless steel archwires were investigated using a modified linear tribometer and special computer software, and the effects of the bracket slot size (0.018 inches [in] or 0.022 in) and materials (ceramic or metal) on the COF were determined.
Methods
Four types of ceramic (one with a stainless steel slot) and one conventional stainless steel bracket were tested with two types of archwire sizes: a 0.017 × 0.025-in wire in the 0.018-in slots and a 0.019 × 0.025-in wire in the 0.022-in slot brackets. For pairwise comparisons between the 0.018-in and 0.022-in slot sizes in the same bracket, an independent sample t-test was used. One-way and two-way analysis of variance (ANOVA) and Tukey's post-hoc test at the 95% confidence level (α = 0.05) were also used for statistical analyses.
Results
There were significant differences between the 0.022-in and 0.018-in slot sizes for the same brand of bracket. ANOVA also showed that both slot size and bracket slot material had significant effects on COF values (p < 0.001). The ceramic bracket with a 0.022-in stainless steel slot showed the lowest mean COF (µ = 0.18), followed by the conventional stainless steel bracket with a 0.022-in slot (µ = 0.21). The monocrystalline alumina ceramic bracket with a 0.018-in slot had the highest COF (µ = 0.85).
Conclusions
Brackets with stainless steel slots exhibit lower COFs than ceramic slot brackets. All brackets show lower COFs as the slot size increases.
Keywords: Brackets, Archwires, Coefficient of friction, Tribometer
INTRODUCTION
Orthodontic tooth movement is frequently carried out by bonding a bracket to the tooth surface and placing an archwire in the bracket slot. Under tension, this archwire applies a gentle force to the tooth that moves it in the desired direction. During this process, sliding friction is generated between the archwires and brackets as the wires guide the brackets during mesiodistal movement of an individual tooth or when archwires are passed through posterior crown attachments.1
The magnitude of the force applied to the teeth should be optimized to obtain the fastest possible tooth movement.2 For example, in some cases, forces less than or greater than this optimal value can cause tooth movement to slow or even stop completely. During orthodontic therapy, friction at the bracket slots and archwire contact areas can prevent the practitioner from obtaining these optimal force values, affecting both the treatment duration and the effects of therapy on the surrounding structures of the teeth.3 It was reported that in some situations, the effective force should be increased six fold to overcome frictional resistance.4 Thus, increased frictional resistance can require the orthodontist to use excessive force, which can result in anchorage loss, patient discomfort, and injury to tooth-supporting tissues during treatment.5 Understanding of the friction phenomenon is therefore essential for understanding what actually happens at the bracket/archwire interface under many different conditions. To date, several methods have been developed for the quantitative evaluation of friction in orthodontics. One accepted method for quantitative characterization of friction is to define a coefficient of friction (COF) at the bracket/archwire interface,6,7,8,9,10,11,12 which is defined as the proportionality constant between the frictional force and the applied load (that is, the normal force).13
In orthodontics, the sliding friction can be affected by various factors such as the bracket and wire materials, surface conditions of the archwires and the bracket slot, wire cross section, torque at the wire-bracket interface, type and force of ligation, inter-bracket distance, saliva, and different oral functions.5 Currently, there are three major groups of bracket materials: metal, plastic, and ceramic. Commonly used metal brackets are made of stainless steel and have been shown in many studies to have the most ideal frictional characteristics among the three materials. Ceramic brackets have come into widespread use because of their aesthetic characteristics. However, studies have reported higher COFs for these brackets, along with greater frictional resistance, rougher surfaces, and a greater tendency to retard tooth movements compared to stainless steel brackets.6,14 Many researchers have shown increased frictional resistance, especially with polycrystalline ceramic and plastic brackets.15,16 Therefore, aesthetic brackets with metal slots were developed to decrease the frictional forces and overcome these drawbacks of ceramic materials.16 Stainless steel archwires also show better results than beta-titanium or nickel-titanium archwires in terms of their frictional characteristics.4,6
Although more sensitive measurements could provide researchers with a better understanding of the problems that cause increased frictional forces, simple universal testing machines have generally been used to measure and compare the frictional forces generated by the brackets and archwires in most previous studies on this subject.3,7,8,17,18 In the field of orthodontics, investigations on friction have been roughly classified into four groups according to the type of friction test setup: (1) archwires sliding through contact flats, (2) archwires sliding through brackets parallel to the bracket slot, (3) archwires sliding through brackets with different second- and third-order angulations, and (4) brackets submitted to a force with a certain degree of tipping allowed.19
Our hypothesis was that testing the friction with a linear tribometer modified particularly for this subject would show no significant difference in the resistance to sliding of stainless steel archwires through 0.018-inches [in] and 0.022-in slots in aesthetic brackets. The tribometer and experimental test set-up used in this study were modified to measure an archwire sliding through a bracket, as in clinical applications, and the COF was chosen as the measure of the bracket/archwire interface friction. In particular, the tribometer was modified to allow the measurement arm to move in a linear direction, and a specially developed computer software program was used to measure and calculate the COF of the tested specimen. Although conventional circular-motion pin-on-disk tribometers are generally used to calculate the dynamic friction, the linear measurement technique used in this study can evaluate the time-dependent changes in the friction values, which are important in clinical practice. Therefore, the purposes of this in vitro study were to measure the COFs generated by aesthetic bracket/stainless steel archwire combinations with two different slot sizes using a modified linear tribometer and special computer software and to compare these COFs to those of conventional stainless steel metal brackets.
MATERIALS AND METHODS
The sample size in this study was calculated using a significance level of 0.05 and a power of 90% to detect meaningful differences among the mean COF values of the groups. After a pilot study, the power analysis (NCSS 2007 and PASS 2008 statistical software; NCSS, Kaysville, UT, USA) showed that nine samples from each group were required. To allow for any sample dropout, a sample size of ten was chosen for each group.
Four types of ceramic brackets were tested: one ceramic bracket with stainless steel slots (Clarity; 3M/Unitek, Monrovia, CA, USA), one monocrystalline alumina ceramic bracket (Pure; Ortho Technology, Tampa, FL, USA), and two polycrystalline alumina ceramic brackets (Transcend, 3M/Unitek; InVu, TP Orthodontics, La Porte, IN, USA). A conventional stainless steel bracket (Gemini, 3M/Unitek) was also tested as a control. The specifications of the brackets are listed in Table 1.
Table 1.
Descriptions and manufacturers of the materials used in this study
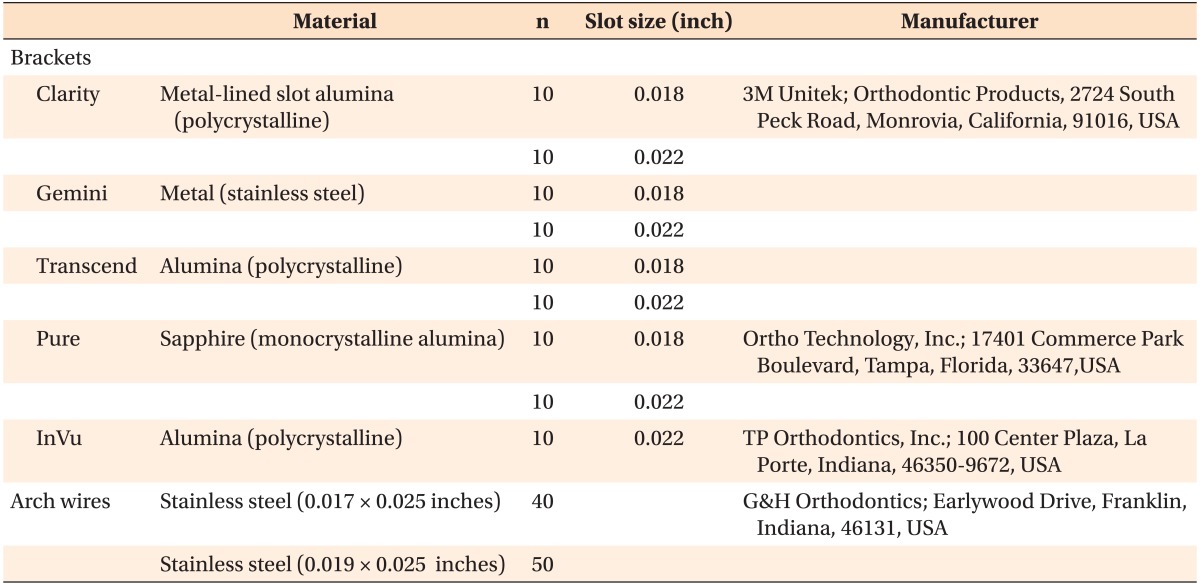
All of the brackets used in this study were maxillary premolar brackets. COF testing was performed with two types of stainless steel straight-length archwires: 0.017 × 0.025-in archwires for the 0.018-in slot brackets and 0.019 × 0.025-in archwires for the 0.022-in slot brackets (Table 1). One of the brackets (InVu) had only a 0.022-in slot. For each group, ten freshly prepared combinations of the archwire and bracket were tested.
Measurement technique
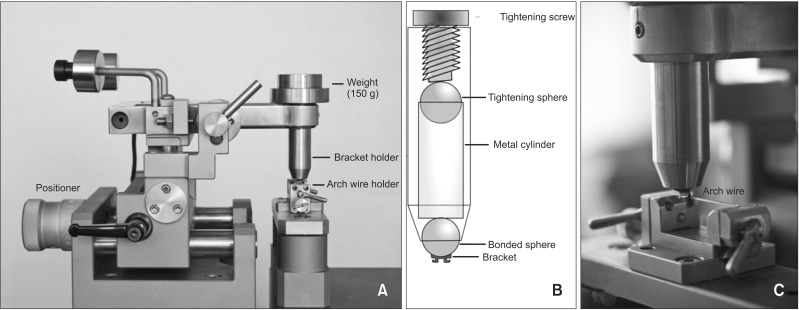
A standard CSM pin-on-disk tribometer (CSM Instruments, Peseux, Switzerland) was modified to allow linear reciprocating wear testing, as shown in Figure 1. In particular, a specially adapted archwire holding block was mounted on frictionless bearings above the circular motor in such a way as to allow the archwire to move in a direction perpendicular to the bracket bearing load arm.
Figure 1.
Modified CSM tribometer test equipment (A), schematic drawing of the bracket holder part (B), and close-up view of bracket (upper) and archwire (lower) holding parts (C).
After degreasing of the brackets and archwires with acetone, the brackets were bonded on a metal sphere that was sandblasted and seated inside of the upper head of the tribometer. The bracket could be moved around this sphere before it was stabilized with a screw. This process helped to eliminate the effects of excessive inclination values (binding) by allowing the bracket slot to move in three dimensions. A force of 150 g was loaded on the upper head, which could move up and down freely to simulate the effect of orthodontic ligatures on the friction.6
A straight-length archwire was seated in the middle of the slot with the help of 0.022 × 0.025-in and 0.018 × 0.025-in stainless steel guidance wires for the 0.022-in and 0.018-in slot brackets, respectively. These guidance wires were seated on the lower head before the tested archwire. The bracket was then positioned on the wire, and the final position stabilized with a screw. After the bracket was stabilized, the guidance wire was dismantled. Then, the archwire to be tested was mounted in place and stabilized with two screw clamps. The test was ready to begin when the bracket was approximated and the archwire was seated in the middle of the bracket slot. The bracket was moved on the stainless steel archwire at a speed of 17 µm/s (~1 mm/min) for 10 mm to measure the dynamic friction. Special software was used to collect the data and calculate the COF for each bracket/archwire combination. Ten measurements were recorded every second during the sliding tests, and the mean frictional values from approximately 6,000 readings were automatically calculated for each bracket/archwire combination.
All samples were tested under dry conditions at room temperature (24℃). The tribometer was covered with a glass box to prevent outside noise from affecting the sensitive measurements during testing. Apart from the standard test parameters (frequency, contact pressure, and time) the environmental parameters (24℃ temperature and 50% relative humidity) were also kept under control in a laboratory with an HVAC (heating, ventilation, and air conditioning) system.
The surface morphology of the tested bracket/archwire couples was examined under a stereo light microscope (SMZ 1500; Nikon, Tokyo, Japan) to evaluate the wear patterns of the material surfaces. From each group, selected samples were also photographed (Digital Sight DS-L1, Nikon) at 30× magnification.
Statistical analysis
The data were analyzed using a statistical software package program (SPSS, ver. 12.0; SPSS Inc., Chicago, IL, USA). Because the data were normally distributed in all groups according to the Shapiro-Wilk normality test, Student's t-test for independent samples was used to compare the COFs for the 0.018-in and 0.022-in slot sizes in the same-brand brackets (except for the InVu brackets). In addition, to determine the effects of the slot size (0.018 in or 0.022 in) and bracket slot material (ceramic or stainless steel) on the COFs of the groups, one-way and two-way analysis of variance (ANOVA) was used. This test was followed by Tukey's honestly significant difference (HSD) test for multiple comparison of means, ranked at p < 0.05, to determine differences among the different groups.
RESULTS
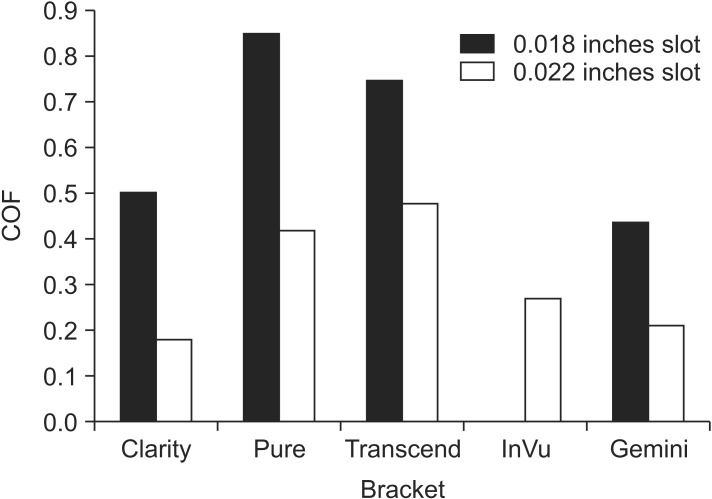
The means, standard deviations, and minimum and maximum values (range) of the COFs measured in vitro for the groups are listed in Table 2. The lowest mean COF value (µ = 0.18) was found for 0.022-in ceramic brackets with stainless steel slots (Clarity), followed by the stainless steel bracket (Gemini) groups (µ = 0.21). The mean COF values of all of the 0.018-in slot groups were nearly twofold greater than those of their 0.022-in slot counterparts (Figure 2). Pairwise comparisons with an independent sample t-test revealed that all of the 0.018-in slot bracket groups showed significantly higher COF values than their counterparts in the 0.022-in slot bracket groups (Table 2).
Table 2.
Descriptive statistics and comparisons of the measured coefficients of friction (µ)*
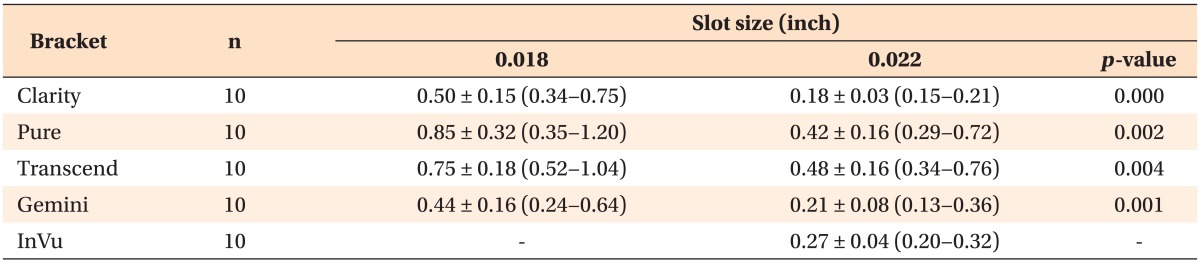
Values are presented as mean ± standard deviation (minimum-maximum).
*For the 0.018-inches and 0.022-inches slot sizes with the same brand brackets obtained from independent t-tests.
Refer to Table 1 for the explanation about each product.
Figure 2.
Mean coefficient of friction (COF) values of the brackets tested. Refer to Table 1 for the explanation about each product.
Since significant differences were found between the two slot sizes, the data for the 0.018-in and 0.022-in slot brackets were treated separately. The comparison between the groups for each slot size was made using one-way ANOVA (Table 3), which showed significant differences among the 0.018-in slot bracket groups. The grouping of these differences obtained from Tukey's HSD multiple-range test indicated that Gemini brackets had significantly lower COFs than the Pure and Transcend brackets in the 0.018-in slot group, except for the ceramic brackets with stainless steel slots (Clarity). In the 0.022-in slot group, Clarity brackets showed significantly lower COFs than the Transcend and Pure brackets. There were no significant differences among the Gemini, InVu, and Clarity brackets for this slot size (Table 3).
Table 3.
Results of one-way ANOVA for the 0.018-in and 0.022-in slot size bracket groups
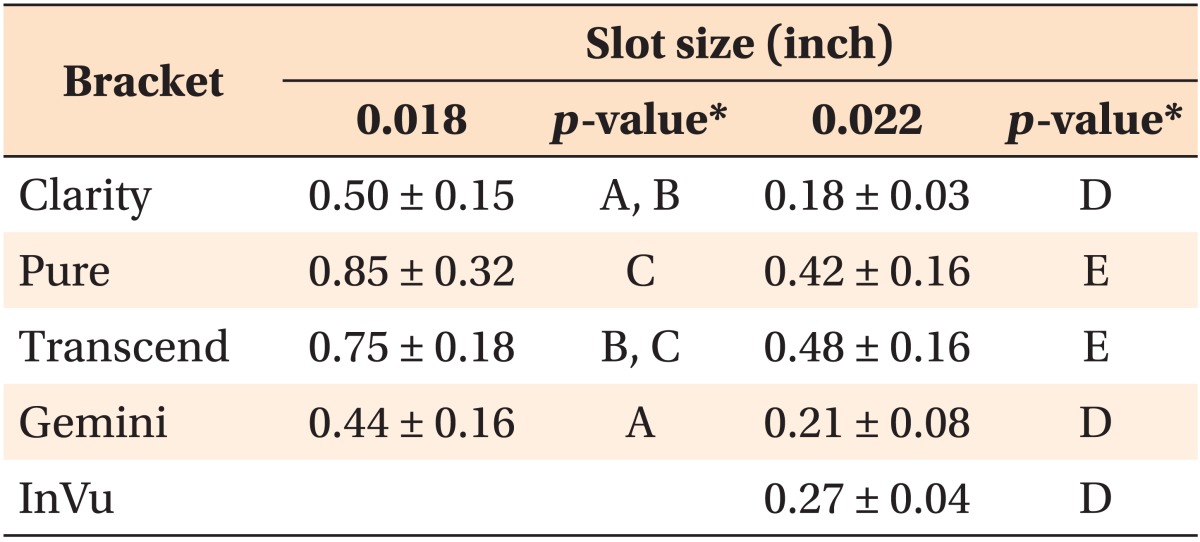
Values are presented as mean ± standard deviation.
The number of each bracket = 10.
ANOVA, Analysis of variance.
*Different letters in the 0.018-inches [in] (A to C) and 0.022-in slot size bracket groups (D and E) indicate statistically significant differences (p < 0.05) between the brackets with the same slot size according to Tukey's honestly significant difference post-hoc test.
Refer to Table 1 for the explanation about each product.
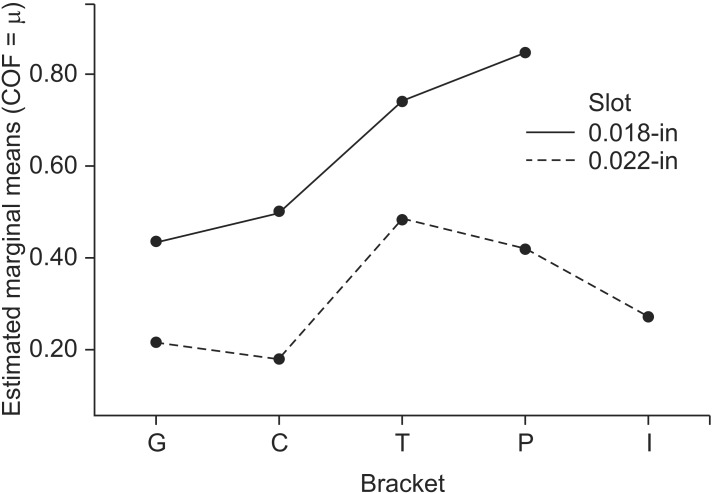
A two-way ANOVA was used to test the hypothesis that there were no significant differences among the COF values of the nine groups. A statistically significant difference was found between the nine groups tested (F = 17.97, p = 0.000) at the 95% confidence level. The grouping of these differences obtained from Tukey's HSD multiple range test is given in Table 4. Since the different groups included samples with two types of bracket slot sizes and several bracket materials, two-way ANOVA was chosen in order to find any interaction present between these variables, i.e., whether the effect of one variable is influenced by the other. Although the results revealed that the COF values were significantly affected by the bracket slot size (p < 0.001) and bracket material (p < 0.001) separately, no significant interaction between the bracket materials and slot sizes was found (Figure 3). In other words, the factorial ANOVA indicated that the 2-way interaction between the bracket materials (Clarity, Pure, Transcend, Gemini, and InVu) and slot sizes (0.018 in and 0.022 in) was not significant (p = 0.251) at the 95% confidence level.
Table 4.
Comparisons of the mean COF values for all bracket groups obtained from two-way ANOVA
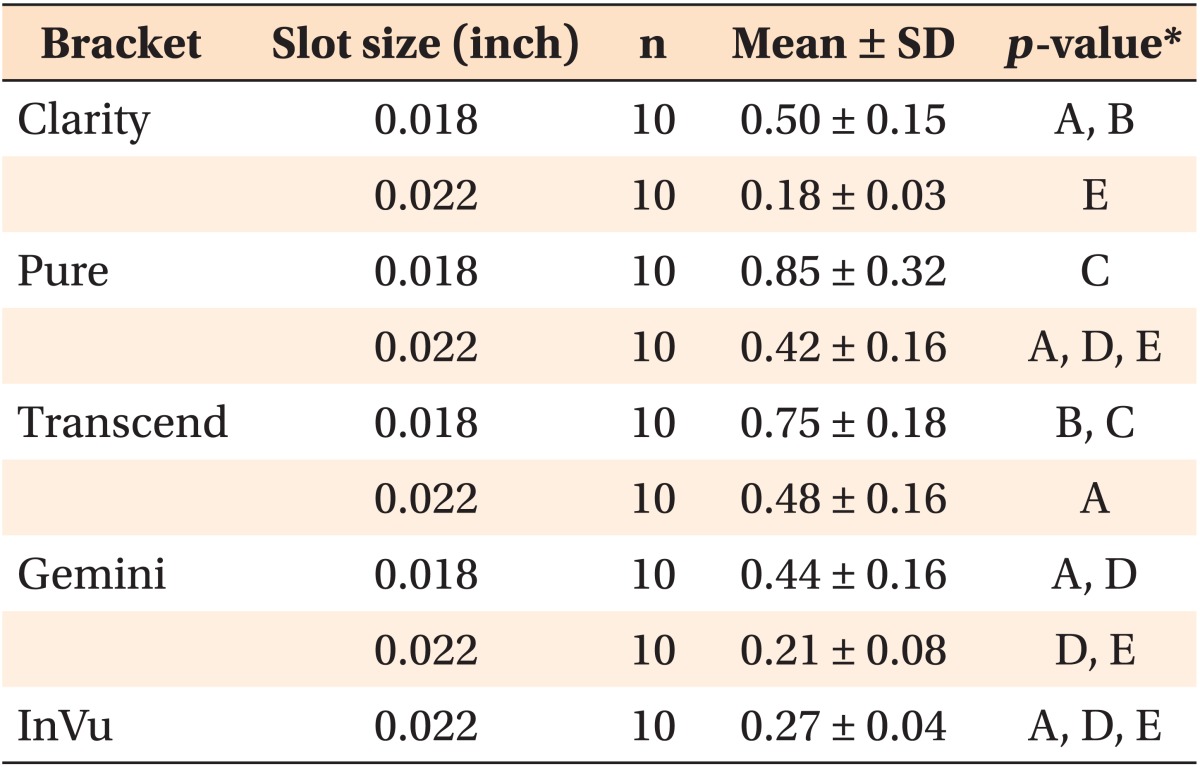
*Different letters in the 0.018-inches [in] (A to C) and 0.022-in slot size bracket groups (D and E) indicate statistically significant differences (p < 0.05) between the brackets with the same slot size according to Tukey's honestly significant difference post-hoc test.
COF, Coefficient of friction; ANOVA, analysis of variance; SD, standard deviation.
Refer to Table 1 for the explanation about each product.
Figure 3.
Profile plot showing no interaction between slot size (0.018 inches [in] and 0.022 in) and bracket material from the two-way analysis of variance. COF, Coefficient of friction; G, Gemini metal; C, Clarity metal-slot ceramic; I, InVu ceramic; P, Pure ceramic; T, Transcend ceramic brackets.
Refer to Table 1 for the explanation about each product.
Representative light microscope images of the tested brackets and the archwires surfaces at the contact are shown in Figure 4. For all bracket/archwire combinations, a few scratches and grooves were noticed on the surfaces of the archwires, probably from the archwire drawing process.
Figure 4.
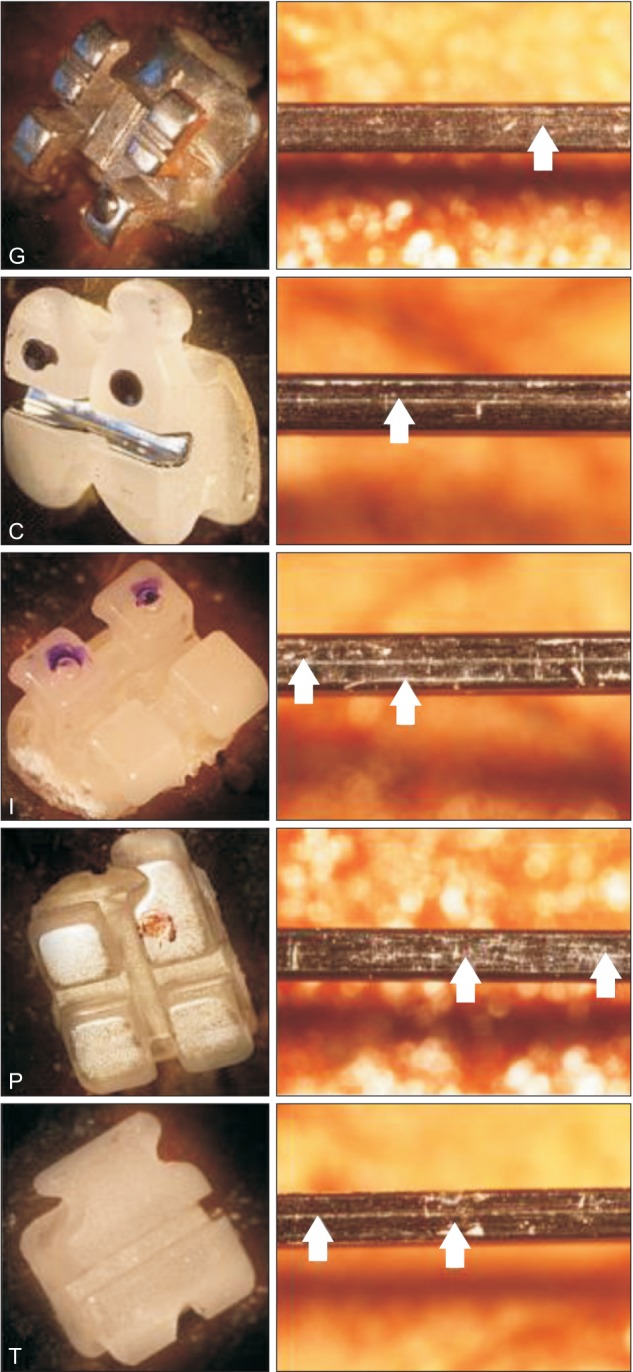
Post-experiment light microscope images of the tested brackets (left) and the archwires coupled with them (right). Arrows show the wear areas on the archwires. Letters indicate the group labels (G, Gemini metal; C, Clarity metal-slot ceramic; I, InVu ceramic; P, Pure ceramic; T, Transcend ceramic brackets).
Refer to Table 1 for the explanation about each product.
DISCUSSION
The friction between archwires and brackets is influenced by many a variable, of which only a small fraction can be understood. Furthermore, there is no standardized method for precisely measuring the friction coefficients of the materials used in orthodontics.
Nonetheless, there are two main approaches for studying the frictional resistance between archwires and orthodontic brackets. One is in vivo simulations which estimate the friction from the speed of a single tooth or a group of teeth sliding along the archwire as in canine or en masse retraction cases; or by resolving the anterior crowding in alignment phase.20 However, in vivo studies can only measure the relative friction of the tested materials and are heavily influenced by uncontrollable biological factors which may be patient-related and thus may produce unstable results.9 The other approach is in vitro simulations which directly measures frictional forces as one tooth or a group of teeth move a certain distance along an archwire.2,13 Our study was performed with in vitro simulations in standardized laboratory condition to reinforce the shortcomings of in vivo environment and minimize the misleading effects of patient-related factors.
In some recent studies, fretting devices have been used to evaluate the surface properties and COFs of orthodontic materials.10,11 However, modifications of these test apparatuses are needed to test orthodontic appliances, such as the specific holders and special software used in this study. This option could be particularly useful for tooth movement applications, where linear sliding is a better simulation of true clinical conditions than conventional circular motion. Indeed, the results of this study showed that the modified linear tribometer generated COF values with relatively low standard deviations and a low spread between the minimum and maximum value (Table 2).
Frictional coefficients were measured under dry conditions in this study. Controversy persists among different investigators regarding the effects of the simulation of intraoral lubrication. For example, it was reported that artificial saliva increased friction,21 but other investigators have claimed that wet conditions had no effect at all on several materials.9,12 For this reason, dry conditions were chosen in this study.
An in vitro study showed that friction increased with repeated use of individual bracket and archwire combinations.22 Therefore, each bracket and archwire combination in the present study was used only once to prevent any increase in frictional forces caused by material wear. The total unidirectional sliding distance was 10 mm to simulate the tooth movement in many clinical applications.
The data obtained in this in vitro study should be extrapolated to clinical conditions only with great care because of the complexity of the oral environment. Changes in the ligation force, inter-bracket distance, temperature, humidity, biological factors, and acidity (saliva) all cause variations in the friction values, as do changes in the mechanical and masticatory stresses placed on a bracket/archwire assembly in the oral cavity. These changes are impossible to simulate in a laboratory. Nevertheless, the comparative data obtained from in vitro testing are useful for guiding the selection of bracket/archwire combinations to obtain good sliding mechanics in orthodontic applications.
In this study, 0.022-in ceramic brackets with stainless steel slots and conventional stainless steel brackets showed the lowest COFs among all samples. This confirms the results of a previous study comparing the frictional forces generated by metal, conventional polycrystalline ceramic, and stainless steel slot aesthetic brackets, which showed that the frictional forces decreased when stainless steel inserts were used inside ceramic bracket slots.23 There have also been other studies that found better frictional characteristics of aesthetic brackets with stainless steel slots compared to those of conventional ceramic brackets, and the obtained results were even comparable with those of metal brackets.18,24
For ceramic brackets, no significant differences were found between the COFs of the polycrystalline (Transcend) and monocrystalline (Pure) brackets in the 0.018-in slot groups. This supports the results of a previous in vitro study,8 which showed by scanning electron microscopy that monocrystalline alumina brackets were smoother than polycrystalline brackets, although they reported no difference in frictional characteristics. However, other investigators showed that monocrystalline alumina brackets tended to produce less friction than polycrystalline brackets.25
One of the polycrystalline ceramic brackets (InVu) showed significantly lower COFs than the other ceramic brackets (Transcend, Pure) in the 0.022-in groups. This result is in accordance with a previous report26 that polycrystalline injection molded ceramic brackets were smoother and thus exhibited less friction than other ceramic brackets.
The position of the archwire in the bracket slot also affects the frictional forces. It was reported that notching and binding significantly affected frictional forces.27 Minimal contacts between the slots' side walls and the archwires are desired in order to standardize the forces generated by notching and binding. Therefore, guidance wires that could be fully seated in bracket slots were seated just before the tested archwires to minimize this contact area and prevent any effects of the archwire positions on the results of this study. This technique helped position the bracket slots to prevent any excessive contact (binding) between the tested wires and the slot walls during the measurements. This technique is similar to the precise alignment and leveling phase in orthodontic treatment.
It has been reported that slot size has no influence on frictional resistance.7 However, in a study frictional resistance was found to decrease as the slot size increased from 0.018 in to 0.022 in because of reduced binding, most likely from the increased archwire stiffness.28 Moreover, a mathematical model showed that smaller bracket slots could cause more binding to occur compared to larger bracket slots if the initial alignment and leveling were not sufficiently precise.29 This opinion is supported by the results of the present study, because all of the 0.022-in slot brackets with 0.019 × 0.025- in stainless steel archwires showed lower COFs than their 0.018-in slot counterparts with 0.017 × 0.025-in stainless steel wires. The wear patterns of the archwires in representative post-experiment images are also consistent with the COFs found in the study (Figure 4). Greater wear was seen for the 0.017 × 0.025-in stainless steel archwire/ceramic bracket combinations that caused higher frictional forces.
Based on the results of the present study and the aforementioned studies, it seems logical that a larger clearance between slot walls and archwires would result in a smaller possibility of binding during in vitro tests. The lateral clearances between bracket slots and archwires were different in the 0.018-in and 0.022-in groups in this study: 0.001 in and 0.003 in, respectively. As stated before, one of the main aims of this study was to test bracket/archwire combinations for actual clinical applications. However, it should be borne in mind that maximally filling the slots with archwires (small clearance) results in greater control of the teeth at the expense of severe binding, whereas minimally filling the slots (large clearance) results in poor control and relatively little binding. Nevertheless, to choose the ideal bracket/archwire combination, clinicians should consider the individual patient's requirements, such as their anchorage needs, root control, and the amount of space closure needed.
CONCLUSION
The COFs of stainless steel and ceramic brackets with stainless steel slots were similar when tested under in vitro conditions using a modified linear tribometer and special computer software. However, brackets with ceramic slots generated higher COFs than ceramic brackets with stainless steel slots, which will be a valuable alternative to conventional stainless steel brackets in patients with aesthetic demands. All of the brackets/archwire combinations tested in this study showed lower COFs as the slot size increased from 0.018 in to 0.022 in.
Since the low standard deviations and a low spread between the minimum and maximum COF values, the modified tribometer and experimental set-up used in this study could be accepted as a valid test technique to measure the bracket/archwire interface friction in orthodontic applications.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Frank CA, Nikolai RJ. A comparative study of frictional resistances between orthodontic bracket and arch wire. Am J Orthod. 1980;78:593–609. doi: 10.1016/0002-9416(80)90199-2. [DOI] [PubMed] [Google Scholar]
- 2.Braun S, Bluestein M, Moore BK, Benson G. Friction in perspective. Am J Orthod Dentofacial Orthop. 1999;115:619–627. doi: 10.1016/s0889-5406(99)70286-6. [DOI] [PubMed] [Google Scholar]
- 3.Cacciafesta V, Sfondrini MF, Ricciardi A, Scribante A, Klersy C, Auricchio F. Evaluation of friction of stainless steel and esthetic self-ligating brackets in various bracket-archwire combinations. Am J Orthod Dentofacial Orthop. 2003;124:395–402. doi: 10.1016/s0889-5406(03)00504-3. [DOI] [PubMed] [Google Scholar]
- 4.Drescher D, Bourauel C, Schumacher HA. Frictional forces between bracket and arch wire. Am J Orthod Dentofacial Orthop. 1989;96:397–404. doi: 10.1016/0889-5406(89)90324-7. [DOI] [PubMed] [Google Scholar]
- 5.Read-Ward GE, Jones SP, Davies EH. A comparison of self-ligating and conventional orthodontic bracket systems. Br J Orthod. 1997;24:309–317. doi: 10.1093/ortho/24.4.309. [DOI] [PubMed] [Google Scholar]
- 6.Kusy RP, Whitley JQ, Prewitt MJ. Comparison of the frictional coefficients for selected archwire-bracket slot combinations in the dry and wet states. Angle Orthod. 1991;61:293–302. doi: 10.1043/0003-3219(1991)061<0293:COTFCF>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Kusy RP, Whitley JQ. Effects of sliding velocity on the coefficients of friction in a model orthodontic system. Dent Mater. 1989;5:235–240. doi: 10.1016/0109-5641(89)90067-5. [DOI] [PubMed] [Google Scholar]
- 8.Saunders CR, Kusy RP. Surface topography and frictional characteristics of ceramic brackets. Am J Orthod Dentofacial Orthop. 1994;106:76–87. doi: 10.1016/S0889-5406(94)70024-9. [DOI] [PubMed] [Google Scholar]
- 9.Stannard JG, Gau JM, Hanna MA. Comparative friction of orthodontic wires under dry and wet conditions. Am J Orthod. 1986;89:485–491. doi: 10.1016/0002-9416(86)90006-0. [DOI] [PubMed] [Google Scholar]
- 10.Willems G, Clocheret K, Celis JP, Verbeke G, Chatzicharalampous E, Carels C. Frictional behavior of stainless steel bracket-wire combinations subjected to small oscillating displacements. Am J Orthod Dentofacial Orthop. 2001;120:371–377. doi: 10.1067/mod.2001.116088. [DOI] [PubMed] [Google Scholar]
- 11.Clocheret K, Willems G, Carels C, Celis JP. Dynamic frictional behaviour of orthodontic archwires and brackets. Eur J Orthod. 2004;26:163–170. doi: 10.1093/ejo/26.2.163. [DOI] [PubMed] [Google Scholar]
- 12.Kusy RP, Whitley JQ. Influence of fluid media on the frictional coefficients in orthodontic sliding. Semin Orthod. 2003;9:281–289. [Google Scholar]
- 13.Kusy RP, Whitley JQ. Friction between different wire-bracket configurations and materials. Semin Orthod. 1997;3:166–177. doi: 10.1016/s1073-8746(97)80067-9. [DOI] [PubMed] [Google Scholar]
- 14.Zinelis S, Eliades T, Eliades G, Makou M, Silikas N. Comparative assessment of the roughness, hardness, and wear resistance of aesthetic bracket materials. Dent Mater. 2005;21:890–894. doi: 10.1016/j.dental.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 15.Bazakidou E, Nanda RS, Duncanson MG, Jr, Sinha P. Evaluation of frictional resistance in esthetic brackets. Am J Orthod Dentofacial Orthop. 1997;112:138–144. doi: 10.1016/s0889-5406(97)70238-5. [DOI] [PubMed] [Google Scholar]
- 16.Cha JY, Kim KS, Hwang CJ. Friction of conventional and silica-insert ceramic brackets in various bracket-wire combinations. Angle Orthod. 2007;77:100–107. doi: 10.2319/092705-333R.1. [DOI] [PubMed] [Google Scholar]
- 17.Reicheneder CA, Baumert U, Gedrange T, Proff P, Faltermeier A, Muessig D. Frictional properties of aesthetic brackets. Eur J Orthod. 2007;29:359–365. doi: 10.1093/ejo/cjm033. [DOI] [PubMed] [Google Scholar]
- 18.Cacciafesta V, Sfondrini MF, Scribante A, Klersy C, Auricchio F. Evaluation of friction of conventional and metal-insert ceramic brackets in various bracket-archwire combinations. Am J Orthod Dentofacial Orthop. 2003;124:403–409. doi: 10.1016/s0889-5406(03)00501-8. [DOI] [PubMed] [Google Scholar]
- 19.Pizzoni L, Ravnholt G, Melsen B. Frictional forces related to self-ligating brackets. Eur J Orthod. 1998;20:283–291. doi: 10.1093/ejo/20.3.283. [DOI] [PubMed] [Google Scholar]
- 20.Franchi L, Baccetti T, Camporesi M, Lupoli M. Maxillary arch changes during leveling and aligning with fixed appliances and low-friction ligatures. Am J Orthod Dentofacial Orthop. 2006;130:88–91. doi: 10.1016/j.ajodo.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 21.Pratten DH, Popli K, Germane N, Gunsolley JC. Frictional resistance of ceramic and stainless steel orthodontic brackets. Am J Orthod Dentofacial Orthop. 1990;98:398–403. doi: 10.1016/S0889-5406(05)81647-6. [DOI] [PubMed] [Google Scholar]
- 22.Kapur R, Sinha PK, Nanda RS. Frictional resistance in orthodontic brackets with repeated use. Am J Orthod Dentofacial Orthop. 1999;116:400–404. doi: 10.1016/s0889-5406(99)70224-6. [DOI] [PubMed] [Google Scholar]
- 23.Russell JS. Aesthetic orthodontic brackets. J Orthod. 2005;32:146–163. doi: 10.1179/146531205225021024. [DOI] [PubMed] [Google Scholar]
- 24.Kusy RP, Whitley JQ. Frictional resistances of metal-lined ceramic brackets versus conventional stainless steel brackets and development of 3-D friction maps. Angle Orthod. 2001;71:364–374. doi: 10.1043/0003-3219(2001)071<0364:FROMLC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 25.De Franco DJ, Spiller RE, Jr, von Fraunhofer JA. Frictional resistances using Teflon-coated ligatures with various bracket-archwire combinations. Angle Orthod. 1995;65:63–72. doi: 10.1043/0003-3219(1995)065<0063:FRUTLW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Omana HM, Moore RN, Bagby MD. Frictional properties of metal and ceramic brackets. J Clin Orthod. 1992;26:425–432. [PubMed] [Google Scholar]
- 27.Burrow SJ. Friction and resistance to sliding in orthodontics: a critical review. Am J Orthod Dentofacial Orthop. 2009;135:442–447. doi: 10.1016/j.ajodo.2008.09.023. [DOI] [PubMed] [Google Scholar]
- 28.Rock WP, Wilson HJ. The effect of bracket type and ligation method upon forces exerted by orthodontic archwires. Br J Orthod. 1989;16:213–217. doi: 10.1179/bjo.16.3.213. [DOI] [PubMed] [Google Scholar]
- 29.Kusy RP, Whitley JQ. Influence of archwire and bracket dimensions on sliding mechanics: derivations and determinations of the critical contact angles for binding. Eur J Orthod. 1999;21:199–208. doi: 10.1093/ejo/21.2.199. [DOI] [PubMed] [Google Scholar]