Abstract
Objective
To compare the effect of problem solving therapy against a health-promotion intervention (dietary practices) on health-related quality of life (HRQOL) and examine if there is a differential effect on non-Latino Whites and African-Americans between the two interventions. This paper also explores participant characteristics (problem solving style and physical functioning) as potential predictors of HRQOL.
Methods
Secondary analysis of data from a randomized depression prevention trial involving 247 older adults (154 non-Latino Whites, 90 African-Americans, 3 Asians). Participants were randomly assigned to receive either problem solving therapy for primary care (PST-PC) or coaching in healthy dietary practices (DIET).
Results
Both PST-PC and DIET improved HRQOL over two years and did not differ significantly from each other. African-Americans in both conditions had greater improvements in mental health-related quality of life (MHRQOL) compared to non-Latino Whites. In addition, higher social problem solving and physical functioning were predictive of improved MHRQOL.
Conclusions
PST-PC and DIET have the potential to improve health-related quality of life in a culturally relevant manner. Both hold promise as effective and potentially scalable interventions that could be generalized to highly disadvantaged populations in which little attention to HRQOL has been paid.
Keywords: African-Americans, health-related quality of life, problem solving therapy, older adults, health promotion
INTRODUCTION
The mental health needs of older adults are especially complex due to co-occurring physical health problems1–3 that contribute to compromised health-related quality of life (HRQOL). HRQOL has been defined as an individual’s perception of physical and mental health.4 This multidimensional construct is viewed as a critical indicator of health because it focuses on the person’s self-perceptions of his/her health, which is beneficial in lowering distress and enhancing well-being.4–6 Evaluating and tracking HRQOL in high-risk populations can help to identify subgroups at increased risk of poor physical or mental health and inform the development of effective health-promotion and disease-prevention interventions.7
Depressive and anxiety disorders can have a significant impact on HRQOL in old age. Late-life depression is associated with a wide array of adverse consequences, including psychological suffering, functional impairment, and increased mortality rates.8–10 Similarly, late-life anxiety is associated with significant impairment in social, family, and occupational functioning, poor perceived emotional and physical health, well-being, and low satisfaction with daily life.11,12
Given the subjective nature of HRQOL, psychological factors are likely to impact the cognitive processes involved in such reports. Therefore, psychological interventions could have a positive influence on overall HRQOL. Problem solving therapy (PST) is an evidenced-based intervention that teaches depressed patients the problem solving skills necessary to manage day-to-day problems.13 In addition to treating mental illness effectively in late-life,13 PST has sufficient flexibility to address multiple domains of HRQOL such as disability14 and chronic medical illness.15 However, as suggested below, it is not yet clear that PST represents an optimal approach to address HRQOL in older African-Americans.
Race adds to variation observed in the prevalence and impact of both physical and mental illness in older adults. Older non-Latino Whites have significantly higher lifetime prevalence of depression and anxiety than African-Americans, but 12-month rates are similar across the two groups.3,16 In contrast, the prevalence of heart disease, stroke, cancer, and diabetes is significantly higher in older African-Americans than in older non-Latino Whites.17 Taken together, disparities in mental and physical health put older African-Americans at greater risk of having poorer overall HRQOL than non-Latino Whites.18 Although many studies have examined factors associated with HRQOL, the impact of mental health and health promotion interventions on HRQOL has not been fully investigated.
There is growing evidence to suggest that health-promoting behaviors can lead to improved mental and physical health outcomes.19 Health-promoting behaviors, defined as those activities in which individuals engage to maintain or improve their well-being (e.g. getting adequate nutrition), have been shown to improve HRQOL4 and are needed for vulnerable, disadvantaged populations.20 Older African-Americans have expressed a distrust of conventional mental health professionals as a result of perceived mistreatment by mental health providers and institutions.21 Given that older African-Americans have low rates of mental health service use,22 experience high stigma,23 and have high rates of comorbidities,17 health promotion interventions may be a culturally acceptable alternative that could potentially impact HRQOL.
In this study, we did not have a specific hypothesis for several reasons. First, the dearth of randomized, health-related quality of life trials in older adults raises the question of which intervention to use. Second, the multicomponent nature of health-related quality of life makes hypothesizing difficult. Since PST has shown to be an effective mental health treatment in older adults with multiple comorbid physical conditions, it could have a greater impact on health-related quality of life compared to DIET. However, health promotion interventions have value in their own right, and African-Americans could prefer health promotion interventions over a traditional psychotherapeutic approach such as PST. Therefore, DIET could have a greater impact on health-related quality of life than PST among African-Americans. The goals of the current study were three-fold: First was to compare the effect of PST to a health promotion intervention which coaches individuals in healthy dietary practices (DIET) on HRQOL. Second was to examine whether there was a race effect on HRQOL between PST and DIET. The third aim, which was exploratory, was to explore participant characteristics (e.g. problem solving style and functional impairment) as potential predictors of HRQOL.
METHODS
Participants
All participants were subjects in a National Institute of Minority Health and Health Disparities (NIMHD) and National Institute of Mental Health (NIMH) sponsored trial to determine the ability of PST vs. DIET to prevent or delay episodes of major depression in individuals with subsyndromal depression. A detailed description of the study methods is provided elsewhere.24 A total of 247 participants (154 non-Latino Whites, 90 African-Americans, and 3 Asians) were enrolled in the parent randomized, mental illness prevention trial.24 Older adults who are already symptomatic are at increased risk for developing major depression.25 Therefore, only mildly symptomatic individuals were recruited in order to maximize the efficiency of the depression prevention trial. Eligible participants were 50+ years of age and met criteria for subsyndromal depression as defined by a score of 11 or greater on the Center for Epidemiologic Studies Depression Scale,26 and absence of a major depressive episode during the previous year. Excluded from study participation were individuals with a Mini-Mental State Score27 less than 24 (to exclude probable dementia) and a history of an episode of alcohol or other substance use disorder within the past 12 months, bipolar disorder, other psychotic disorder, or neurodegenerative disorder based on the Structured Clinical Interview for DSM-IV Disorders.28 Participants were recruited through multiple referral sources (e.g. community agencies, primary care, print and electronic media, etc.). For the purposes of this secondary study, the 3 Asian participants were only included in the analyses comparing the effect of PST with DIET on HRQOL over time. They were excluded from all subsequent analyses when examining the differential effect of race between the two interventions.
Randomization
The parent study randomly assigned participants to one of two interventions using permuted-block randomization stratified by the presence/absence of a history of major depressive disorder (MDD) and by site of recruitment. This stratified randomized design was done for three reasons. First, a past history of MDD is a strong risk factor for future episodes. Second, there were differences in sociodemographic characteristics of participants (including race) recruited from each type of site. Third, there was the possibility that recruitment site could influence rates of occurrence of MDD. Random assignment was communicated by the statistician to the project co-coordinator but concealed from independent evaluators. There were no instances of the blind being inadvertently broken.
Interventions
The experimental group received manualized problem solving therapy for primary care (PST-PC).29 The first session lasted an hour and the subsequent sessions lasted 30 minutes each. Participants in DIET received coaching in healthy eating practices. Using a manualized educational intervention, interventionists reviewed general nutrition guidelines, helped with preparing weekly menus and grocery lists, and reviewed food intake since last visit. Topics discussed included access to healthy food, culturally specific and acceptable foods, and specific topics raised by participants. DIET is a culturally acceptable, active intervention that facilitated recruitment of African-American participants.
PST-PC and DIET had similar numbers of sessions (6–8 sessions) and semi-annual boosters (30–45 minutes at 3, 9, and 15 months). Both interventions included homework assignments, monitoring of adherence, and focused on concerns identified by each participant. Both were provided by interventionists trained at the NIMH-sponsored Advanced Center for Late Life Depression Prevention and Treatment at University of Pittsburgh School of Medicine and Graduate School of Public Health. Interventionists were six white social workers and mental health nurses. The same interventionists delivered both PST-PC and DIET, to avoid confounding intervention with clinician effects.
To ensure fidelity of intervention delivery, we used group supervision and one-on-one feedback using evaluations of randomly selected 20% of audiotapes of PST-PC and DIET sessions. PST-PC adherence ratings assessing quality were completed by the intervention supervisor, using two sessions for each case — an early session (1–3) and a later session (4–8). Following a batch of ratings, corrective feedback was provided. A majority (73%) of sessions of both PST-PC and DIET was rated as adherent. A treatment fidelity scale was also developed to document the absence of intervention contamination effects. Using this scale, ratings were completed on seven consecutive minutes of the session starting five minutes into the session. Sessions were rated independently by two raters for the presence of PST-PC elements and DIET elements. Based upon blind ratings, the two interventions were highly discriminable (κ=.91), even though delivered by the same interventionists. Interventions were delivered primarily face to face in settings requested by the participants themselves: primary care offices, community agencies, and participant homes. About 9% (n=173/1884) of sessions were delivered over the telephone. The protocol was overseen by a Data Safety Monitoring Board and reviewed and approved annually by the University of Pittsburgh’s Institutional Review Board.
Measures
The primary outcome of this analysis was HRQOL – measured by the 12-item Short Form Health Survey (SF-12)30 – administered by independent evaluators blind to randomized intervention assignment at baseline, and every 6 months subsequently until 24 months. The secondary outcomes of this study were problem solving skills – measured by the Social Problem Solving Inventory31 – and functional impairment – measured by the Late-Life Function and Disability Instrument.32
Short Form Health Survey (SF-12)
The SF-12 is a widely used measure of HRQOL that describes general physical health status and mental health distress.30 The utility of the SF-12 as a HRQOL instrument stems from its brevity and ability to explain −90% of the variance in the extensively validated SF-36.30 The 12 items in the questionnaire correspond to eight principal physical and mental health domains including general health perceptions; physical functioning; role limitations due to physical and emotional problems; bodily pain; energy-fatigue, social functioning and mental health. The 12 items are summarized into two scores, a Physical Health –Related Quality of Life score and a Mental Health-Related Quality of Life score. These provide an important contrast between physical and psychological health status.
Social Problem Solving Inventory
The Social Problem Solving Inventory (SPSI)31 provides a broad assessment of two different problem-orientation dimensions and three different problem-solving core behavior dimensions. The five scales are positive problem orientation (PPO), negative problem orientation (NPO), rational problem solving (RPS), impulsivity/carelessness style (ICS), and avoidance style (AS). The PPO scale assesses an individual’s tendency to view problems in a positive light; to see problems as challenges rather than threats; and the ability to detect and implement effective solutions. The NPO scale assesses maladaptive problem-solving approaches. The RPS scale assesses an individual’s tendency to use effective problem solving techniques. The ICS scale evaluates a tendency to solve problems by making impulsive, incomplete, and haphazard decisions. The AS scale measures maladaptive patterns of problem solving such as putting the problem off and waiting for problems to resolve themselves.31
Late-Life Function and Disability Instrument
The Late-Life Function & Disability Instrument (Late-Life FDI)32 is a 48-item measure that assesses and responds to meaningful change in two distinct outcomes: function – a person's ability to do discrete actions or activities (“can do”), and disability – a person's performance of socially defined life tasks (“does do”). It was designed to examine the impact of treatment and interventions that aim to improve function and minimize disability in older adults.
Data Analysis
All analyses were performed using the intent-to-treat principle, with comparisons made according to the assigned intervention groups. All data were examined for normality prior to analyses and transformations were used where necessary. Baseline demographics and clinical differences between interventions and between races were tested using t-tests for continuous variables and chi-square for categorical. To characterize and compare the trajectories between PST-PC and DIET, mixed models were used with intervention, time and the potential interactions among intervention and time. Models first considered both linear and quadratic time effects in order to test for nonlinear trajectories and then linear time effects only. Best fit model was determined comparing Bayesian Information Criterion (BIC) values between models. If there was a significant baseline difference between interventions, the baseline value was used as a covariate and change over time was modeled in the remaining time points. In analyses examining race as moderator, race and the interactions among race and other variables were included in the above models. If there were baseline race differences, then baseline value was again used as covariate, and change was modeled over the remaining time points. SPSI31 and Late-Life FDI32 measures were examined as time-varying covariates in the mixed model to examine predictors of HRQOL.
RESULTS
Sociodemographic Characteristics
Table 1 shows baseline sociodemographic and clinical characteristics of participants who were randomized to either PST-PC or DIET. The groups did not differ significantly on any demographic and clinical variables. Table 2 shows the baseline sociodemographic and clinical measures of non-Latino White and African-American participants. African-Americans reported greater social and medical disadvantage, such as having significantly fewer years of formal education, lower household income, greater rate of obesity, and lower physical health-related quality of life. African-American and non-Latino White participants were similar on the SPSI31 with the one exception of a higher positive problem orientation (a measure of active coping and resilience) among African-Americans. No race differences were observed in functional impairment.
Table 1.
Contrast of sociodemographic and clinical characteristics in PST-PC and DIET participants
| PST-PC N=125 |
DIET N=122 |
||
|---|---|---|---|
|
Sociodemographics Age (years) |
65.78 (10.94) | 65.39 (10.99) | t(245)=0.28, p=0.78 |
| %Female | 68.80 (n=86) | 73.77 (n=90) | c2 (1)=0.52, p=0.47 |
| Race %ASIAN PACIFIC |
1.60 (n=2) | 0.82 (n=1) | Fisher Exact p=0.54 |
| %AFRICAN-AMERICAN | 33.60 (n=42) | 39.34 (n=48) | |
| %NON-LATINO WHITE | 64.80 (n=81) | 59.84 (n=73) | |
| Education (years) | 14.41 (2.84) | 14.68 (2.65) | t(245)=−0.78, p=0.44 |
| Marital Status %co-habitating/married |
46.40 (n=58) | 45.90 (n=56) | χ2 (3) =1.68, p=0.64 |
| %divorced/separated | 16.80 (n=21) | 22.13 (n=27) | |
| %never married | 13.60 (n=17) | 9.84 (n=12) | |
| %widowed | 23.20 (n=29) | 22.13 (n=27) | |
| %Employed | 41.60 (n=52) | 38.52 (n=47) | χ2 (1) =0.13, p=0.72 |
| Median Household Income | 50509.8 (25786.5) [n=123] Range:10902.0–115882 |
45545.2 (21598.7) [n=120] Range:12818.0–127361 |
t(241)=1.62, p=0.11 |
|
Health Cumulative Illness Rating Scale (CIRSG) Total (scale range: 0–52) |
7.69 (3.62) [n=124] | 7.99 (4.16) [n=121] | t(243)=−0.60, p=0.55 |
| Count (scale range=0–13) |
4.88 (2.06) [n=124] | 5.02 (2.38) | t(244)=−0.48, p=0.63 |
| Heart + Vascular (scale range=0–8) |
2.00 (1.49) [n=124] | 1.89 (1.51) | t(244)=0.60, p=0.55 |
| Body Mass Index (BMI) Total |
30.54 (6.57) | 30.61 (7.26) [n=120] | t(243)=−0.07, p=0.94 |
| % ≥ 30 | 45.60 (n=57) | 51.67 (n=62) | χ2 (1)=0.68, p=0.41 |
| HRQOL PHRQOL (t score: mean=50, std=10) |
41.31 (11.77) [n=100] |
42.87 (11.76) [n=107] |
t(205)=0.95, p=0.34 |
| MHRQOL (t score: mean=50, std=10) |
42.35 (9.80) [n=100] | 43.71 (8.98) [n=107] | t(205)=1.04, p=0.30 |
|
Cognitive Status Mini-Mental Status Examination (MMSE: scale range=0–30) |
28.09 (1.74) [n=124] | 28.38 (1.54) | t(244)=-1.38, p=0.17 |
|
Mental Health Hamilton Rating Scale for Depression (17 Items) (HRS17: scale range=0–52) |
11.60 (4.03) [n=124] |
10.79 (3.51) | t(244)=1.68, p=0.09 |
| Center for Epidemiologic Studies Depression Scale (CESD: scale range=0–60) |
21.89 (8.29) [n=124] |
20.40 (7.47) | t(244)=1.48, p=0.14 |
| Beck Depression Inventory (BDI:scale range=0–63)) |
11.08 (5.88) [n=117] |
9.88 (5.51) [n=116] |
t(231)=1.60, p=0.11 |
| Brief Symptom Inventory Anxiety** (scale range=0–4) |
0.51 (0.47) [n=119] |
0.52 (0.54) [n=116] |
t(233)=−0.16, p=0.87 |
| % History of major depressive disorder | 32.80 (n=41) | 34.43 (n=42) | χ2 (1)=0.02, p=0.89 |
| % History of anxiety disorder | 21.60 (n=27) | 20.49 (n=25) | χ2 (1)=0.00, p=0.95 |
| %Current anxiety disorder | 21.60 (n=27) | 27.05 (n=33) | χ2 (1)=0.72, p=0.40 |
| Social Problem Solving Inventory (SPSI) SPSI Total (standard score: mean=100, std=15) |
99.79 (13.72) [n=105] |
103.11 (12.97) [n=109] |
t(212)=−1.82, p=0.07 |
| Positive Problem Orientation (standard score: mean=100, std=15) |
95.81 (16.42) [n=113] |
99.75 (14.68) [n=116] |
t(227)=−1.92, p=0.06 |
| Referral Source Kingsley Center, Healthy Black Family Project, Healthy Hearts and Souls, Giant Eagle Screening, Barbershop |
17.89 (n=22) | 19.83 (n=24) | χ2 (5)3.56, p=0.61 |
| Mental Health Specialist | 4.07 (n=5) | 4.13 (n=5) | |
| Primary Care | 43.09 (n=53) | 47.11 (n=57) | |
| Research (research program or registry) | 10.57 (n=13) | 9.92 (n=12) | |
| Self-referred (media, brochure, presentation, peer educator) |
18.70 (n=23) | 10.74 (n=13) |
Table 2.
Baseline demographics and clinical characteristics of non-Latino White and African-American participants.
| Non-Latino Whites N=154 |
African- Americans N=90 |
||
|---|---|---|---|
|
Sociodemographics Age (years) |
65.49 (11.71) | 65.83 (9.73) | t(242)=0.24, p=0.81 |
| %Female | 67.53 (n=104) | 77.78 (n=70) | χ2(1)=2.44, p=0.12 |
| Education (years) | 15.23 (n=2.78) | 13.32 (2.21) | t(220.0*)=−5.89, p<0.0001 |
| Marital Status %co-habitating/married |
57.14 (n=88) | 27.78 (n=25) | χ2(1)=21.74, p<0.001 |
| %divorced/separated | 14.29 (n=22) | 27.28 (n=25) | |
| %never married | 7.79 (n=12) | 17.78 (n=16) | |
| %widowed | 20.78 (n=32) | 26.67 (n=24) | |
| %Employed | 46.10 (n=71) | 30.00 (n=27) | χ2(1)=5.48, p=0.02 |
| Median Household Income | 58,273 (23,210) n=151 range: 14,539 – 127,361 |
31,003 (13,137) n=89 range: 10,902– 79,100 |
t(237.7*)=−11.62, p<0.001 |
|
Health Cumulative Illness Rating Scale (CIRSG) Total (scale range: 0–52) |
7.45 (3.78) n=152 |
8.42 (4.03) | t(240)=1.89, p=0.06 |
| Count (scale range=0–13) |
4.75 (2.21) n=153 |
5.22 (2.21) | t(241)=1.60, p=0.11 |
| Heart + Vascular (scale range=0–8) |
1.84 (1.52) n=153 |
2.11 (1.48) | t(241)=1.34, p=0.18 |
| Body Mass Index (BMI) Total |
29.14 (6.44) n=152 |
32.99 (7.04) | t(240)=4.34, p<0.001 |
| % ≥ 30 | 39.47 (n=60) | 63.33 (n=57) | χ2(1)=11.95, p<0.001 |
| % with Hypertension (systolic >=140 or diastolic >=90) | 45.95 (n=68) | 52.33 (n=45) | χ2(1)=0.65, p=0.42 |
| HRQOL PHRQOL (t score: mean=50, std=10) |
43.92 (11.34) n=133 |
38.81 (12.04) n=71 |
t(202)=−3.00, p=0.003 |
| MHRQOL (t score: mean=50, std=10) | 42.89 (9.16) n=133 |
43.26 (9.91) n=71 |
t(202)=0.27, p=0.79 |
|
Mental Health Social Problem Solving Inventory (SPSI) SPSI Total (standard score: mean=100, std=15) |
100.26 (13.43) n=137 |
103.72 (13.35) n=75 |
t(210)=1.80, p=0.07 |
| Positive Problem Orientation (standard score: mean=100, std=15) | 95.87 (15.23) n=142 |
100.94 (16.09) n=85 |
t(225)=2.38, p=0.02 |
| Negative Problem Orientation (standard score: mean=100, std=15) | 99.07 (14.56) n=137 |
97.41 (14.14) n=75 |
t(210)=−0.80, p=0.42 |
| Rational Problem Orientation (standard score: mean=100, std=15) | 96.75 (14.91) n=137 |
98.84 (15.64) n=75 |
t(210)=0.96, p=0.34 |
| Impulsivity/Carelessness Problem Orientation (standard score: mean=100, std=15) | 96.50 (13.23) n=137 |
94.44 (12.88) n=75 |
t(210)=−1.10, p=0.27 |
| Avoidance Style (standard score: mean=100, std=15) | 95.35 (13.02) n=137 |
92.35 (13.15) n=75 |
t(210)=−1.60, p=0.11 |
| Late-Life Functional Disability Instrument (FDI) FDI Frequency Scaled Score |
52.74 (6.66) n=118 |
51.61 (7.34) n=80 |
t(196)=−1.12, p=0.27 |
| FDI Limitation Scaled Score | 68.31 (12.60) n=118 |
65.54 (14.22) n=80 |
t(210)=−1.44, p=0.15 |
Satterthwaite method used due to unequal variances.
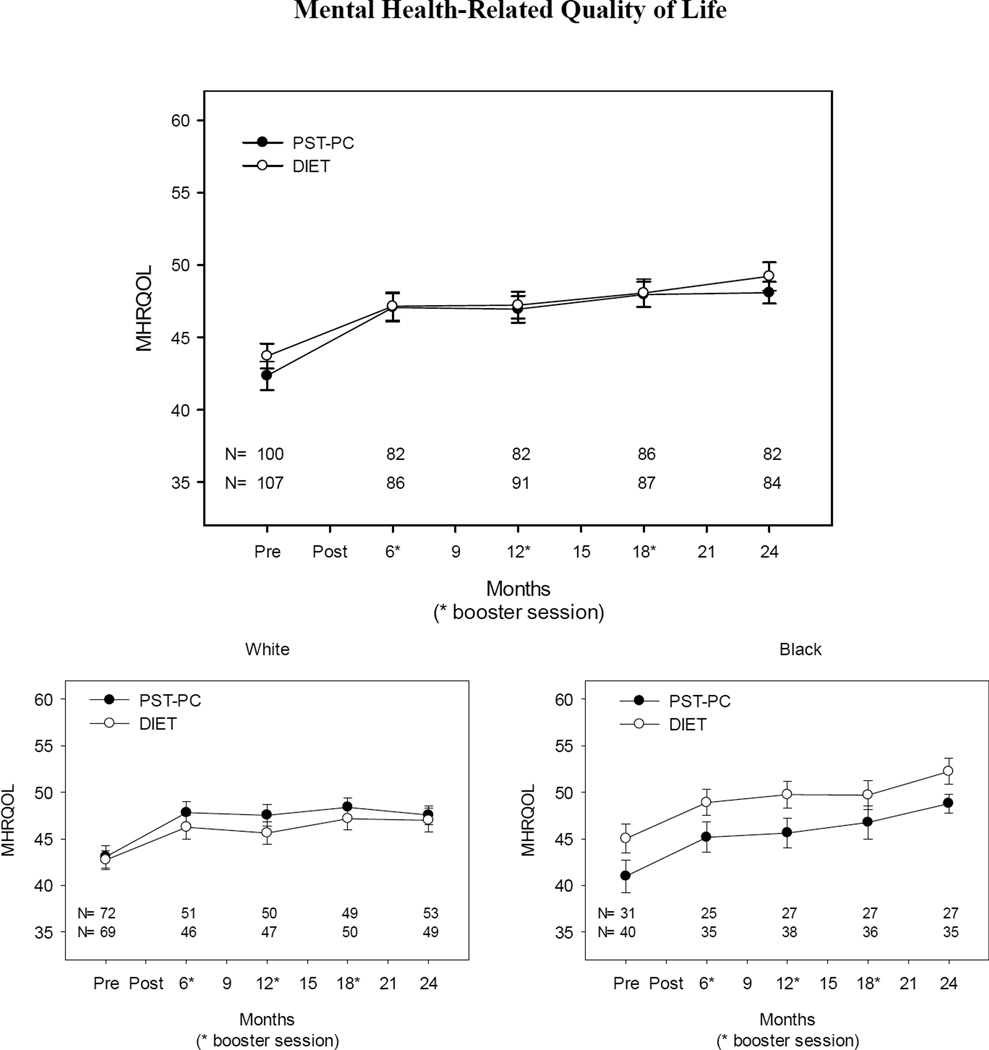
Mental Health-Related Quality of Life
Participants in both PST-PC and DIET demonstrated similar improvement in mental health-related quality of life (MHRQOL). There were significant quadratic and linear time effects. There were no significant intervention or intervention by time. When examining race as moderator, a trend in baseline difference in African-Americans between interventions was observed; thus, the model co-varied for baseline score and the change over remaining time points was examined. There was a significant time by race effect with African-Americans increasing to a greater extent over time relative to non-Latino Whites for post-intervention through 2 years, but no significant intervention or intervention by time effects, nor race, or race by intervention effects (Figure 1 shows raw mean ± standard error). African-Americans improved by approximately 3.5 points between 6 months and 2 years. This represents nearly an 8% improvement from the 6 month scores. Non-Latino Whites, on average, showed no improvement (<1% change from 6 month score).
Figure 1.
Mental Health-Related Quality of Life (PST versus DIET; African-Americans versus non-Latino Whites) Mental Health-Related Quality of Life
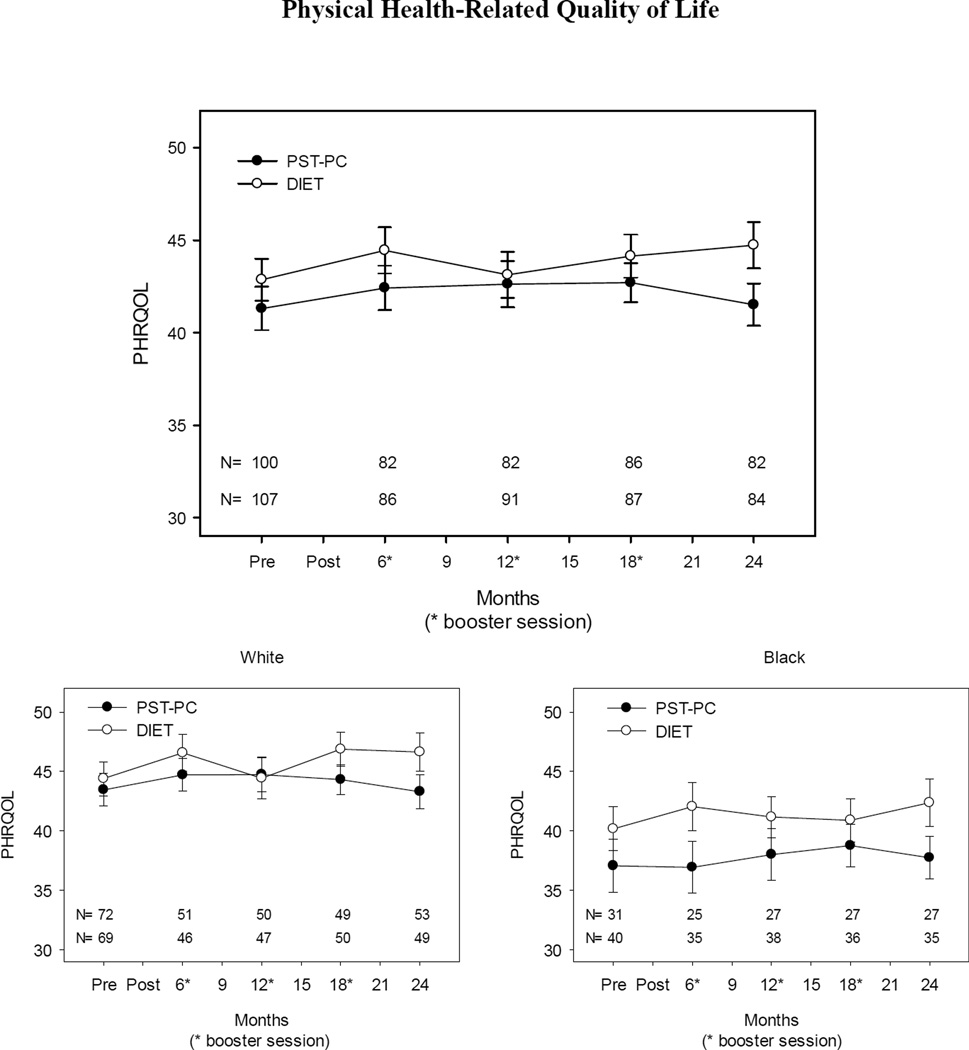
Physical Health-Related Quality of Life
Participants in both PST-PC and DIET demonstrated similar improvement in physical health-related quality of life (PHRQOL). There were significant quadratic and linear time effects. There were no intervention or intervention by time effects. When examining race as moderator, baseline difference in non-Latino Whites and African-Americans were observed; therefore, the model co-varying for baseline score was run. No significant time effects for post-intervention through 2 years and no significant intervention or intervention by time effects, nor race, race by intervention, race by time effects were detected (Figure 2 shows raw mean ± standard error).
Figure 2.
Physical Health-Related Quality of Life (PST versus DIET; African-Americans versus non-Latino Whites) Physical Health-Related Quality of Life
Exploratory Analyses: Factors Associated with Improved HRQOL
Table 3 shows the results of our exploratory analyses to identify potential predictors of HRQOL. Better scores on both the Social Problem Solving Inventory (SPSI)31 and the Late-Life Function & Disability Instrument (Late-Life FDI)32 predicted better MHRQOL scores. Higher positive problem orientation (PPO) and rational problem solving (RPS) scores were associated with increased MHRQOL. Conversely, higher negative problem orientation (NPO), impulsivity/carelessness style (ICS), and avoidance style (AS) scores were associated with decreased MHRQOL (data not shown but available upon request). Higher scores on the Late-Life FDI functioning scale were associated with improved mental and physical health-related quality of life.
Table 3.
Factors Predicting HRQOL
| Mental Health Related Quality of Life Predictors1 | |
|---|---|
| Beta (stderr) | |
| Intercept | 6.765 (3.999) |
| MHRQOL baseline | 0.201 (0.045) |
| FDI Limit Scaled Score | 0.198 (0.029) |
| SPSI Total | 0.166 (0.032) |
| Race (African-American) | −2.025 (1.628) |
| Intervention(PST-PC) | 0.239 (1.465) |
| Week | −0.002 (0.013) |
| Intervention(PST-PC)*Race(African-American) | −0.775 (1.784) |
| Week*Race(African-American) | 0.042 (0.018) |
| Week*Intervention(PST-PC) | 0.002 (0.017) |
| Physical Health Related Quality of Life Predictors2 | |
| Beta (stderr) | |
| PHRQOL baseline | 2.012 (4.105) |
| FDI Limit Scaled Score | 0.612 (0.039) |
| SPSI Total | 0.172 (0.029) |
| Race (African-American) | 0.052 (0.032) |
| Intervention(PST-PC) | −3.039 (1.624) |
| Week | −0.321 (1.455) |
| Intervention(PST-PC)*Race(African-American) | −0.015 (0.013) |
| Week*Race(African | 1.052 (1.865) |
| Week*Intervention(PS-PC) | 0.008 (0.017) |
Note:
MHRQOL as outcome: Due to baseline differences, model uses baseline MHRQOL as covariate and time is modeled using post treatment scores.
PHRQOL as outcome: Due to baseline differences, model uses baseline PHRQOL as covariate and time is modeled using post treatment scores.
DISCUSSION
The results of this study indicate that both PST-PC and DIET are associated with improved HRQOL for older non-Latino Whites and African-Americans over two years. There were no significant differences found between the two interventions with respect to improving HRQOL. Despite the greater burden of social and medical disadvantages, African-Americans had greater improvements on MHRQOL compared to non-Latino Whites. Mental health interventions for the evidence-based management of depression have been found to have moderate effect sizes (~0.35), which corresponds to meaningful differences in response and remission rates.33,34 This is the magnitude of the effect observed in the current study. Thus, the results of this study are consistent with other treatment-oriented studies, but now in the context of MHRQOL. In addition, improvements in positive problem solving skills and physical functioning were identified as factors predicting improved MHRQOL. Given the lack of studies testing intervention effects on racial/ethnic minority elderly, this study presents a novel contribution to the HRQOL literature.
The finding that both PST-PC and DIET had comparable and sustained improvements in HRQOL over time is consistent with prior research.35 This study builds upon that previous study by showing long term benefits – 2 years post compared to 1 year – and a much more active health promotion comparison condition – 6–8 30-minute sessions compared to three, 30- minute videos. These results combined with the exploratory finding that improvements in positive problem orientation and physical functioning are associated with increased MHRQOL highlight the potential impact that learning-based, skills-enhancing interventions can have on older adults who tend have high rates of comorbidities. Teaching coping skills may improve HRQOL by enhancing resilience to stress, anxiety and diminishing the sense of loss of control at the core of depression. Similarly, teaching health promotion strategies for better nutrition may improve HRQOL by enhancing the ability to tackle problems associated with managing health issues.24,34 Thus, there may be a synergy between PST and health promotion approaches in improving HRQOL.
Educational and behavioral intervention programs, like DIET, enhance general well-being and bring mental health benefits to older adults faced with health-related challenges.7 This may help explain why there was a significant improvement in the MHRQOL of older African-Americans compared to older non-Latino Whites. To maximize the effectiveness of health promotion strategies, the intervention must be relevant, respectful, and specific to this population.36 Given that obesity is more prevalent in older African-Americans than in older non- Latino Whites,37 an intervention designed to coach older adults in healthy dietary practices could be seen as a culturally acceptable and salient health promotion strategy in older African-Americans that could potentially impact HRQOL. Participants in DIET were given the tools necessary to address the challenges of implementing healthy dietary practices and to tackle problems that may arise when managing health issues. It was a non-stigmatizing approach that addressed a problem in the African-American community in a way that optimized their problem solving style.
Despite a well-documented distrust of conventional mental health professionals21 and stigma concerning mental illness,23 African-Americans enrolled in PST-PC exhibited greater improvements in MHRQOL compared to non-Latino Whites in PST-PC. Behavioral activation and developing active coping strategies are important components of PST. This form of psychotherapy may seem less stigmatizing and culturally relevant since it matches and enhances African-American’s ability to detect and implement effective solutions to problems encountered in everyday life.
Caution is warranted in interpreting our results due to limitations associated with the sample, study methods, and design. First, the study design did not include a “usual care” or no-intervention control condition. The lack of a no-intervention control condition was a pragmatic decision reflecting the unfortunate reality that “usual care” is often “no care” or “poor care,” especially for racial/ethnic minorities.24 The community advisory board at the University of Pittsburgh warned that it would be a barrier to participation for many African-Americans. Since a no-intervention control was not included in the design of the study, the possibility of a regression to the mean or a non-specific effect of study participation cannot be excluded. Second, repeated assessments could have led to reported symptom attenuation. Participants tend to report fewer symptoms upon retesting to avoid further questions or by learning more about the purpose of the interview.38 Third, participants had all consented to be in a study in which they were willing to be randomized to either a mental health treatment intervention or a health promotion intervention. These individuals represent a select subgroup, and conclusions drawn may not be generalizable to the population at large.
While these results should be viewed with some caution, they suggest potential directions for further inquiry. Adding a no-intervention control condition would help to clarify the question of whether the findings were a result of the interventions used or a regression to the mean. Incorporating Latino and Asian elderly would address the paucity of research examining HRQOL in older, high-risk, highly disadvantaged populations. Older Latinos have high prevalence of anxiety and depression16 and high mental health service use disparities.22 Older Asians also report high stigma39 and believe that mental illness is a result of medical illness.40 Thus, health promotion interventions could have a great impact on HRQOL in these communities.
This study provides preliminary findings that may help to inform the use of interventions aimed at improving HRQOL in racial/ethnic minority older adults with subsyndromal depression. Mental health services provided to African-Americans may include problem solving techniques or alternatively apply culturally relevant health promotion interventions that target salient health problems (e.g. obesity) as an approach to engage older African-Americans in mental health services. Such targeted health promotion interventions might be considered for other disadvantaged populations in implementing culturally acceptable psychosocial interventions with the potential to positively impact HRQOL.
ACKNOWLEDGMENTS
This research was supported by K23 MH098025; P60 MD000207; P30 MH090333; UL1RR024153, UL1TR000005, and the UPMC Endowment in Geriatric Psychiatry.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No disclosures to report.
References
- 1.Institute of Medicine. The mental health and substance use workforce for older adults: In whose hands? Washington, DC: National Academies Press; [PubMed] [Google Scholar]
- 2.Bartels SJ, Naslund JA. The underside of the silver tsunami--older adults and mental health care. N Engl J Med. 2013;368:493–496. doi: 10.1056/NEJMp1211456. [DOI] [PubMed] [Google Scholar]
- 3.Woodward AT, Taylor RJ, Abelson JM, Matusko N. Major depressive disorder among older African Americans, Caribbean blacks, and non-Hispanic whites: secondary analysis of the National Survey of American Life. Depress Anxiety. 2013;30(6):589–597. doi: 10.1002/da.22041. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control and Prevention. [Retrieved June 5, 2013];Health-related quality of life. 2006 from http://www.cdc.gov/hrqol/index.htm.
- 5.Franks P, Muennig P, Lubetkin E, Jia H. The burden of disease associated with being African-American in the United States and the contribution of socio-economic status. Soc Sci Med. 2006;62(10):2469–2478. doi: 10.1016/j.socscimed.2005.10.035. [DOI] [PubMed] [Google Scholar]
- 6.Jang Y, Chiriboga DA, Borenstein AR, Small BJ, Mortimer JA. Health-related quality of life in community-dwelling older Whites and African Americans. J Aging Health. 2009;21(2):336–349. doi: 10.1177/0898264308329001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thornton KA, Tuck I. Promoting the mental health of elderly African Americans: A case illustration. Arch Psychiat Nurs. 2000;14:191–198. doi: 10.1053/apnu.2000.8659. [DOI] [PubMed] [Google Scholar]
- 8.Preisig M, Merikangas KR, Angst J. Clinical significance and comorbidity of subthreshold depression and anxiety in the community. Acta Psychiatr Scand. 2001;104(2):96–103. doi: 10.1034/j.1600-0447.2001.00284.x. [DOI] [PubMed] [Google Scholar]
- 9.Schulz R, Drayer RA, Rollman BL. Depression as a risk factor for non-suicide mortality in the elderly. Biol Psychiatry. 2002;52(3):205–225. doi: 10.1016/s0006-3223(02)01423-3. [DOI] [PubMed] [Google Scholar]
- 10.Yang Y, George LK. Functional disability, disability transitions, and depressive symptoms in late life. J Aging Health. 2005;17(3):263–292. doi: 10.1177/0898264305276295. [DOI] [PubMed] [Google Scholar]
- 11.Kertz SJ, Woodruff-Borden J. Human and economic burden of GAD subthreshold GAD worry in a primary care sample. J Clin Psychol Med Settings. 2011;18(3):281–290. doi: 10.1007/s10880-011-9248-1. [DOI] [PubMed] [Google Scholar]
- 12.Porensky EK, Dew MA, Karp JF, et al. The burden of late-life generalized anxiety disorder: effects on disability, health-related quality of life, and healthcare utilization. Am J Geriatr Psychiatry. 2009;17(6):473–482. doi: 10.1097/jgp.0b013e31819b87b2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Areán P, Hegel M, Vannoy S, Fan M, Unüzter J. Effectiveness of problem-solving therapy for older primary care patients with depression: results from the IMPACT Project. Gerontologist. 2008;48(3):311–323. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- 14.Kiosses DN, Areán PA, Teri L, Alexopoulos GS. Home-delivered problem adaptation therapy (PATH) for depressed, cognitively impaired, disabled elders: A preliminary study. Am J Geriatr Psychiatry. 2010;18:988–998. doi: 10.1097/JGP.0b013e3181d6947d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alexopoulos GS, Raue PJ, Sirey JA, Areán PA. Developing an intervention for depressed, chronically medically ill elders: a model from COPD. Int J Geriatr Psychiatry. 2008;23(5):447–453. doi: 10.1002/gps.1925. [DOI] [PubMed] [Google Scholar]
- 16.Jimenez DE, Alegría M, Chen C-N, Chan D, Laderman M. Prevalence of psychiatric illnesses in older ethnic minority adults. J Am Geriatr Soc. 2010;58(2):256–264. doi: 10.1111/j.1532-5415.2009.02685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. [Retrieved June 5, 2013];Healthy aging: Preventing disease and improving quality of life among older Americans: At a glance 2006. 2006 from http://www.cdc.gov/nccdphp/aag/aag_aging.htm.
- 18.Skarupski KA, de Leon CF, Bienias JL, et al. Black-white differences in health-related quality of life among older adults. Qual Life Res. 2007;16(2):287–296. doi: 10.1007/s11136-006-9115-y. [DOI] [PubMed] [Google Scholar]
- 19.Jennings-Sanders A. Using health fairs to examine health promotion behaviors of older African Americans. ABNF J. 2003;14(1):13–16. [PubMed] [Google Scholar]
- 20.Icard LD, Bourjolly JN, Siddiqui N. Designing social marketing strategies to increase African American's access to health promotion programs. Health Soc Work. 2003;28(3):214–223. doi: 10.1093/hsw/28.3.214. [DOI] [PubMed] [Google Scholar]
- 21.Suite DH, La Bril R, Primm A, Harrison-Ross P. Beyond misdiagnosis, misunderstanding and mistrust: Relevance of the historical perspective in the medical and mental health treatment of people of color. J Natl Med Assoc. 2007;99(8):879–885. [PMC free article] [PubMed] [Google Scholar]
- 22.Jimenez DE, Cook B, Bartels SJ, Alegría M. Disparities in mental health service use of racial and ethnic minority elderly adults. J Am Geriatr Soc. 2013;61:18–25. doi: 10.1111/jgs.12063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Conner KO, Copeland VC, Grote NK, et al. Mental health treatment seeking among older adults with depression: the impact of stigma and race. American Journal of Geriatric Psychiatry. 2010;18:531–543. doi: 10.1097/JGP.0b013e3181cc0366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds CF, Thomas SB, Morse J, et al. Treatment in psychiatry: Early intervention to preempt major depressive episodes in at-risk older Blacks and Whites. Psychiatr Serv. 2014;65(6):765–773. doi: 10.1176/appi.ps.201300216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuijpers P, Smit F. Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies. Acta Psychiatr Scand. 2004;109(5):325–331. doi: 10.1111/j.1600-0447.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- 26.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 27.Folstein MF, Folstein SE, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. J Psychiat Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 28.First M, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IVAxis II Personality Disorders (SCID-II),Version 2.0. New York: New York State Psychiatric Institute; 1994. [Google Scholar]
- 29.Areán P, Hegel M, Unützer J. Problem-Solving Therapy for Older Primary Care Patients: Maintenance Group Manual for Project IMPACT. Los Angeles: University of California, Los Angeles; 1999. [Google Scholar]
- 30.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Haley SM, Jette AM, Coster WJ, et al. Late Life Function and Disability Instrument: II Development and evaluation of the function component. J Gerontol-A. 2002;57:M217–M222. doi: 10.1093/gerona/57.4.m217. [DOI] [PubMed] [Google Scholar]
- 32.D'Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychol Assessment. 1990;2:156–163. [Google Scholar]
- 33.Bruce ML, Ten Have TR, Reynolds CF, III, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 34.Patel V, Weiss HA, Chowdhary N, et al. Effectiveness of an intervention led by lay health counsellors for depressive and anxiety disorders in primary care in Goa India (MANAS): a cluster randomized controlled trial. Lancet. 2010;376:2086–2095. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lam CL, Fong DY, Chin WY, et al. Brief problem-solving treatment in primary care (PST-PC) was not more effective than placebo for elderly patients screened positive of psychological problems. Int J Geriatr Psychiatry. 2010;25:968–980. doi: 10.1002/gps.2435. [DOI] [PubMed] [Google Scholar]
- 36.Stahl ST, Albert SM, Dew MA, Lockovich MH, Reynolds CF., 3rd Coaching in healthy dietary practices in at-risk older adults: a case of indicated depression prevention. Am J Psychiatry. 2014;171(5):499–505. doi: 10.1176/appi.ajp.2013.13101373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29(1):6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 38.Lucas CP, Fisher P, Piacentini J, et al. Features of interview questions associated with attenuation of symptom reports. J Abnorm Child Psych. 1999;27:429–437. doi: 10.1023/a:1021975824957. [DOI] [PubMed] [Google Scholar]
- 39.Georg Hsu LK, Wan YM, Chang H, et al. Stigma of depression is more severe in Chinese Americans than Caucasian Americans. Psychiatry. 2008;71:210–218. doi: 10.1521/psyc.2008.71.3.210. [DOI] [PubMed] [Google Scholar]
- 40.Jimenez DE, Bartels SJ, Cardenas V, Dhaliwal SS, Alegría M. Cultural beliefs and mental health treatment preferences of ethnically diverse older adult consumers in primary care. Am J Geriatr Psychiatry. 2012;20(6):533–542. doi: 10.1097/JGP.0b013e318227f876. [DOI] [PMC free article] [PubMed] [Google Scholar]