Abstract
Purpose :
Complications are the chief concern of patients and physicians when considering spine surgery. The authors seek to assess the incidence of complications in patients undergoing spine surgery and identify risk factors for their occurrence.
Methods :
Prospective study of patients undergoing spine surgery from 1 February 2013 to 1 February 2014. Epidemiological characteristics and complications during the surgical hospitalization were recorded and analyzed.
Results :
The sample comprised 95 patients (mean age, 59 years). Overall, 23% of patients were obese (BMI =30). The mean BMI was 25.9. Approximately 53% of patients had comorbidities. Complications occurred in 23% of cases; surgical site infections were the most common (9%). There were no significant differences between patients who did and did not develop complications in terms of age (60.6 vs 59.9 years, p = 0.71), sex (56% female vs 54% female, p = 0.59), BMI (26.6 vs 27.2, p = 0.40), or presence of comorbidities (52% vs 52.8%, p = 0.87). The risk of complications was higher among patients submitted to spine instrumentation than those submitted to non-instrumented surgery (33% vs 22%), p=0.8.
Conclusion :
Just over one-quarter of patients in the sample developed complications. In this study, age, BMI, comorbidities were not associated with increased risk of complications after spine surgery. The use of instrumentation increased the absolute risk of complications.
Keywords: Complication, outcome, risk, spine surgery.
INTRODUCTION
Complications are the main concern of patients and physicians at the time of spine surgery indication, and when they occur, may have personal and economic consequences, affecting the quality of life and future independence of patients [1]. Studies have shown that surgeons and gynecologists have a lower life expectancy than clinicians, and emotional stress may be a cause of this difference [2]. Surgical complications are a relevant cause of stress in surgeons.
Reducing the incidence of these complications is a constant concern of physicians and health managers. Reimbursement practices incorporating pay-for-performance measures seek to link patient outcomes to practitioner reimbursement. These financial incentives are part of a policy that aims to reduce hospital-acquired conditions and, therefore, hospitalization costs [3, 4].
The incidence and prevalence of complications in spine surgery have varied widely in literature, due to differences in methodology and patient samples among studies. Few prospective studies have assessed complications [3-5]. Furthermore, there is no consensus on potential risk factors for the development of complications in spine surgery [3-9].
A clear definition of risk of complications in spinal surgeries, in the setting of different demographics and comorbidities, is required for adequate therapeutic decision making, once it can help patients to decide weather submit to an invasive procedure with provided numeric information. Therefore, this study sought to assess the incidence of complications in spine surgery and identify patient-related risk factors and those related to the use of instrumentation.
METHODS
This study used a prospective observational design whereby all patients undergoing spine surgery at a tertiary referral center between 1 February 2013 and 1 February 2014 were observed from surgery to discharge and in hospital complications were recorded. Hospital do Servidor Público Estadual de São Paulo, SP, Brazil, covers about 3 million state servers and their relatives throughout São Paulo state. The Neurosurgery Department provides a 25-bed unit and offers residency program. Surgeries were indicated in the Spine clinic (elective cases) and in the emergency department of the hospital and included a wide range of procedures (ICD-9CM:01.2, 03.09, 03.32, 03.71, 80.51, 81.00-81.08, 81.30, 81.65, 81.66, 84.51, 84.60, 84.61, 84.62, 84.80, 84.84). No inclusion or exclusion criteria were applied; all patients undergoing any spine surgery procedure during the study period were eligible for admission. All patients received cefuroxime IV 60 minutes before incision and q 8h post-op, 6 doses total. Regarding deep-vein thrombosis prophylaxis, graduated compression stockings were used for all patients, and low molecular weight heparin was prescribed from day 3 post-op for those who could not walk.
For the purposes of this study, a complication in spinal surgery was defined as “any untoward event occurring to a patient while on the neurosurgical service” [10]. Complications were classified as general, specific, or technical (Table 1), as described by Fritzell, Hagg, and Nordwall [11], and further divided into two categories: major (adverse events with sequelae in discharge or requiring revision surgery during hospitalization) and minor complications (adverse events with no sequelae in discharge and not requiring revision surgery), a modified classification from Lebude B et al. [12].
Table 1.
Classification of complications in spine surgery.
| General | Specific | Technical |
|---|---|---|
| Mortality | Hematoma | Screw placement |
| Thrombosis | Infection superficial | Instrument-related |
| Hepatitis | Infection deep | Dislocation of transplant |
| Gastrointestinal | Nerve root injury/pain | |
| Urinary tract infection | Dural tear | |
| Pulmonary complication | Caudaequine syndrome | |
| Skin problem | Injury to sympathetics | |
| Psychological problems | Sex-related problems | |
| Coping problems | Retrograde ejaculation | |
| Donor site pain | ||
| Miscellaneous |
Fritzell P, Hagg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J 2003; 12: 178-189.
The anthropometric variables of interest were age, gender, and body mass index (BMI), which was stratified in accordance with WHO guidelines as follows: BMI<18.5, underweight; 18.5–24.9, normal range; 25.0–29.9, over-weight; ≥30, obesity [13].
During admission, patients were asked to fill up a questionnaire with possible comorbidities and ongoing medications. If any patient had two measures higher than 140x90mmHg (blood pressure) or 126mg/dl (fasting blood glucose) during hospitalization, he was considered hypertensive or diabetic, respectively, despite no previous diagnosis.
Primary spinal diseases were classified etiologically as degenerative, traumatic, neoplastic, congenital, infectious, or inflammatory. The operated spinal segment was classified as cervical, thoracic, or lumbar.
The following variables were tested for correlation with complications: age, gender, BMI, comorbidities, and instrumentation.
This study was approved by the institutional Research Ethics Committee with protocol number 405320.
Statistical Analysis
Numerical variables were expressed by descriptive statistics (mean, standard deviation, range, and relative frequency). Student’s t-test was used to compare differences in age distribution between affected and unaffected patients, whereas the chi-square method was used to test for association between the presence of complications and age, gender, BMI, comorbidities, and instrumentation. The frequency of complications in relation to the variables comorbidities and instrumentation was assessed as a percentage (risk). Absolute risk difference and number needed to avoid complication related to instrumentation was calculated.
The significance level was set at p<0.05. All analyses were carried out in the SPSS for Windows 13.0 software environment.
RESULTS
Demographic and Surgical Data
Demographic data are shown in Table 2. Ninety-five patients underwent spine surgery during the study period and all patients were followed until hospital discharge. The mean age was 59 ±12.31years, and 46% of patients were >60 years old. Forty-three patients (45%) were male. The mean BMI was 25.9;overall, 41 patients were overweight (43.1%) and 22were obese (23.1%).
Table 2.
Summary of demographic data.
| Variable | N (%) |
|---|---|
| No. of patients | 95 |
| Age (years) Mean±SD Range |
59 ±12 31–88 |
| Sex Male Female |
43 (45) 52 (55) |
| BMI <18.5 18.5-24.9 25-29.9 ≥30 |
1 (1) 31 (33) 41 (43) 22 (23) |
Fifty patients (52.6%) had comorbidities. The most common comorbid conditions were hypertension, present in 36 patients, and diabetes mellitus, present in 7 (Table 3).
Table 3.
Summary of comorbidities.
| Comorbidity | N |
|---|---|
| Hypertension | 36 |
| Diabetes mellitus | 7 |
| Depression | 4 |
| Osteoporosis | 3 |
| Smoking | 3 |
| Gout | 2 |
| Alcoholism | 2 |
| Cancer | 2 |
| Stroke | 1 |
| Congestive heart failure | 1 |
| Benign prostatic hypertrophy | 1 |
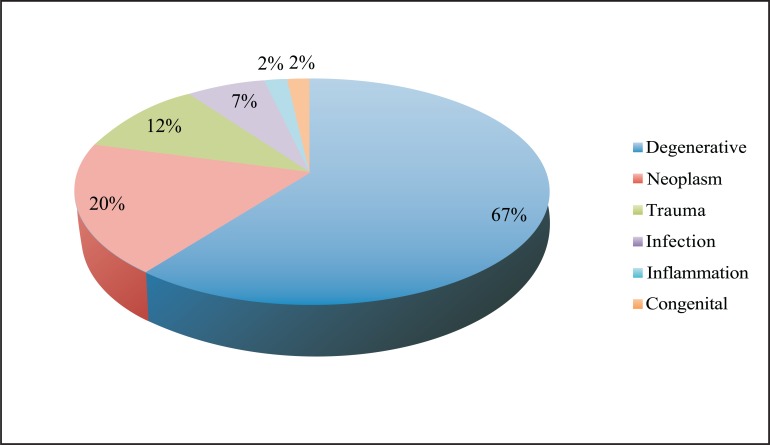
The most common etiology of spinal disease was degenerative(n=64), followed by neoplastic (n=19) and trauma (n=11) (Fig. 1). Regarding the affected spinal segment, 29.4% of procedures were performed on the cervical spine, 24.3% on the thoracic spine, and 46.3% on the lumbar spine.
Fig. (1).
Etiology of spine diseases.
Thirty-six patients (38%) received instrumentation, whereas 59 (62%) did not.
Complications
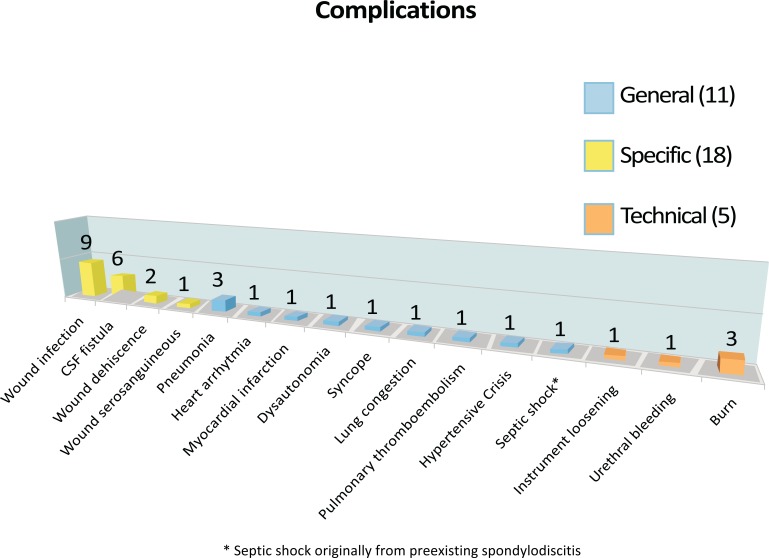
Overall, 25 patients (26%) had 34 complications. Risk of complication after a cervical procedure was 25% (7 patients of 28), 17% in thoracic and 32% in lumbar procedures.
Eleven patients (11.6%of the sample) had major complications, and 14 patients had minor complications (risk = 15%) (Fig. 2).
Fig. (2).
Frequency and classification of complications.
Of the 34 complications recorded, 11 (32%) were general, 18 (53%) were specific, and five (15%) were technical, as shown in Fig. (3). There were no neurological complications.
Fig. (3).
Summary of complications.
Seven patients (7.3%) underwent revision surgery: five due to infection, one due to CSF leak, and one due to screw displacement. Three patients (3.1%) died, all of septic shock (two secondary to surgical site infection and one due to underlying spondylodiscitis).
Association Between Anthropometric Variables and Complications
There were no significant differences in age (60.6 vs 59.9 years, p= 0.71), sex (56%female vs 54%female, p = 0.59), or mean BMI (26.6 vs 27.2, p=0.40) between patients who developed complications and those who did not, respectively (Table 4).
Table 4.
Comparison of demographic data between patients with and without complications.
| Data | Complications | P Value | |
|---|---|---|---|
| Present | Absent | ||
| Age (years) | 59.94 | 60.64 | 0.71 |
| Female gender | 54.2% | 56% | 0.59 |
| BMI | 27.28 | 26.62 | 0.40 |
Association Between Comorbidities and Complications
Of the 25 patients who developed complications, 52% had comorbidities; of the 70 patients who did not develop complications, 52.8% had comorbidities (p = 0.87).
The risk of complications was 24% among patients with comorbidities (12 of 50) and 26.6% in patients without comorbidities (12 of 45) (p= 0.31).
The risk of complications between hypertensive and non-hypertensive patients was the same (40%), p= 1.
Association Between Instrumentation and Complications
The risk of complications among patients who received instrumentation was 33%(12 of 36), versus 22% (13 of 59) among those who did not receive instrumentation (X2;p=0.87). The absolute difference of risk was 11%. At each 9 patients treated without instrumentation, 1 related complication could be avoided.
Multivariate Analysis
Since all associations between variables (age, sex, BMI, comorbidities and instrumentation) and complications did not reach statistical significance, multivariate analysis could not be concluded.
DISCUSSION
The postoperative complications of spine surgery have recently been an object of study due to growing concerns with reduction of hospital costs and improvement of healthcare services [3]. From a humanitarian standpoint, complications are also a major issue, due to their potential to cause suffering and stress to patients themselves, to their families, and to their surgeons. Stress has been implicated as a cause of decreased survival among surgeons as compared with clinicians [2].
The sample of the present study was similar to those of previous investigations: demographic characteristics, the percentage of overweight patients, the higher proportion of lumbar spine surgeries, and the percentage of patients who underwent instrumentation were similar to those of previous studies on complications in spine surgery [3, 5-7, 14].
The rate of postoperative complications in spine surgery varies widely in the literature. Campbell et al. recently reported an incidence of 52%, with a predominance of minor complications (approximately twice as frequent as major complications), as seen in the present sample [3]. A systematic review of the literature revealed that retrospective studies report a lower incidence of complications than prospective studies (16% vs 19.9%) [5]. The present study, which used a prospective design, found an incidence of 26%, with a predominance of specific complications (53%), which is also consistent with previous studies [3].
Advanced age and obesity have been associated with complications, but many of the studies that found this association reported inconsistent and divergent results, and most were retrospective [6, 9, 15-19]. Lee et al. demonstrated an increased incidence of complications among patients aged >65 years on multivariate analysis of a prospective database of spine surgery cases [9]. Regarding obesity, a few retrospective studies have found it to be associated with an increased complication rate in spine surgery, but most prospective studies – and one nationwide database study – failed to demonstrate such association [6, 20, 21]. In the present study, advanced age and obesity were not associated with an increased complication rate.
Overall, 52% of patients in the present sample had presented comorbidities, with a predominance of cardiovascular diseases. The presence of comorbidities did not affect the incidence of complications in this sample.
The correlation between comorbidities and complications in spine surgery is poorly defined in the literature. Most studies are retrospective or based on population data. Li et al. and Deyo et al. reported an association between presence of comorbidities and increased complication rate [7, 22]. Only one prospective study has assessed the impact of comorbidities on complications, finding that an increase in the number of comorbidities was correlated with an increase in the incidence of complications [3]. The present study – which, as noted above, was prospective in nature –did not find any association between comorbidities and complications. We did not use any specific comorbidity score in the analyses, due to the disproportional predominance of cardiovascular diseases seen in our sample.
In the present sample, the rate of complications was higher in patients who underwent instrumentation than in patients who were not instrumented (33% vs 22% respectively), but the difference did not reach statistical significance (p=0.8). In the other hand, evaluating the absolute risk differenceof complication, instrumentation increased it by 11%. Thus at each 9 patients treated with instrumentation, one will develop a complication. Several studies have demonstrated an association between instrumentation and complications [3, 14, 22].
Although multivariate analysis would be important to identify independent risk factors for complications, it could not be concluded, since association between variables and complications did not reach statistical significance.
Nasser et al. published a systematic review of 105 studies on complications in spine surgery, most of which were retrospective [5]. The majority of studies that evaluated associations between complications and variables studied only one potential risk factor, such as age, obesity, comorbidities, or instrumentation. Conversely, our prospective study evaluated all of these potential associations. We did not evaluate complications in specific surgical procedures because this would demand a greater number of patients.
Some factors may explain the divergence between the present study and previous investigations regarding the association between comorbidities, instrumentation and complications. These elements act as limitations of our study and should be addressed. Since a consistent definition of operative complications lacks in literature, we used a wide-ranging concept of complications herein; our sample was originated from a high-complexity tertiary referral center, which for sure does not represent general population submitted to spine surgery; we presented a small sample size; we included a broad range of etiologies of spinal diseases (whereas the literature has largely focused on degenerative diseases) and a wide range of comorbidities in this study, such as lifestyle habits (smoking and alcoholism). As previous mentioned, the study was conducted in a hospital with residency program; since operator experience may be a risk factor for complication, residents assistance may have increased our incidence of complications. Until large, multicenter studies are conducted, clustered data from multiple prospective investigations may reveal the true incidence of complications in spine surgery.
CONCLUSION
Just over one-quarter of patients in the sample developed complications. Most of these were specific and minor, but 11% of patients experienced major complications, which caused prolonged hospital stay and increased suffering. The sample-wide risk of death was 3%.
In the present study, age, BMI and comorbidities were not associated with an increased risk of complications. However, the use of instrumentation increases the absolute risk of complications in 11%.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Hart R, Cabalo A, Bess S. Comparison of patient and surgeon perceptions of adverse events following adult spinal deformity surgery. Spine (Phila Pa1976) 2013;38(9):732–6. doi: 10.1097/BRS.0b013e31827ae242. [DOI] [PubMed] [Google Scholar]
- 2.Nishi M, Miyake H, Kato T , et al. Life span of Japanese male medical doctors. J Epidemiol. 1999;9(5):315–9. doi: 10.2188/jea.9.315. [DOI] [PubMed] [Google Scholar]
- 3.Campbell PG, Yadla S, Nasser R , et al. Patient comorbidity score predicting the incidence of perioperative complications assessing the impact of comorbidities on complications in spine surgery. J Neurosurg Spine. 2012;16(1):37–43. doi: 10.3171/2011.9.SPINE11283. [DOI] [PubMed] [Google Scholar]
- 4.Campbell PG, Malone J, Yadla S , et al. Comparison of ICD-9-based, retrospective, and prospective assessments of perioperative complications assessment of accuracy in reporting. Clinical article. J Neurosurg Spine. 2011;14:16–22. doi: 10.3171/2010.9.SPINE10151. [DOI] [PubMed] [Google Scholar]
- 5.Nasser R, Yadla S, Maltenfort MG , et al. Complications in spine surgery. A review. J Neurosurg Spine. 2010;13:144–57. doi: 10.3171/2010.3.SPINE09369. [DOI] [PubMed] [Google Scholar]
- 6.Patel N, Bagan B, Vadera S , et al. Obesity and spine surgery relation to perioperative complications. J Neurosurg Spine. 2007;6:291–7. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 7.Li G, Patil CG, Lad SP , et al. Effects of age and comorbidities on complication rates and adverse outcomes after lumbar laminectomy in elderly patients. Spine (Phila Pa1976) 2008;33:1250–5. doi: 10.1097/BRS.0b013e3181714a44. [DOI] [PubMed] [Google Scholar]
- 8.Gaudelli C, Thomas K. Obesity and early reoperation rate after elective lumbar spine surgery a population-based study. Evid Based Spine Care J. 2012;3(2):11–6. doi: 10.1055/s-0031-1298613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee MJ, Konodi MA, Cizik AM , et al. Risk factors for medical complication after spine surgery a multivariate analysis of 1591 patients. Spine J. 2012;12(3):197–206. doi: 10.1016/j.spinee.2011.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamilton A, editor. Spine Surgery Techniques, Complication Avoidance and Management Benzel EC. New York Churchill Livingstone. 1999;1:19. [Google Scholar]
- 11.Fritzell P, Hagg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J. 2003;12:178–89. doi: 10.1007/s00586-002-0493-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lebude B, Yadla S, Albert T , et al. Defining “complications” in spine surgery neurosurgery and orthopedic spine surgeons'survey. J Spinal Disord Tech. 2010;23:493–500. doi: 10.1097/BSD.0b013e3181c11f89. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Obesity preventing and managing the global epidemic. Report of a World Health Organization Consultation. Geneva World Health Organization WHO Obesity Technical Report Series n. 284. 2000;p:256. [PubMed] [Google Scholar]
- 14.Charosky S, Guigui P, Blamoutier A , et al. Complications and risk factors of primary adult scoliosissurgery. Spine. 2012;37(8):693–700. doi: 10.1097/BRS.0b013e31822ff5c1. [DOI] [PubMed] [Google Scholar]
- 15.Carreon LY, Puno RM, Dimar JR 2nd , et al. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A:2089–92. doi: 10.2106/00004623-200311000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Cassinelli EH, Eubanks J, Vogt M , et al. Risk factors for the development of perioperative complications in elderly patients undergoing lumbar decompression and arthrodesis for spinal stenosis an analysis of 166 patients. Spine (Phila Pa 1976). 2007;32:230–5. doi: 10.1097/01.brs.0000251918.19508.b3. [DOI] [PubMed] [Google Scholar]
- 17.Cotton BA, Pryor JP, Chinwalla I , et al. Respiratory complications and mortality risk associated with thoracic spine injury. J Trauma. 2005;59:1400–7. doi: 10.1097/01.ta.0000196005.49422.e6. [DOI] [PubMed] [Google Scholar]
- 18.Cloyd JM, Acosta FL , Jr, Cloyd C, Ames CP. Effects of age on perioperative complications of extensive multilevel thoracolumbar spinal fusion surgery. Clinical article. J Neurosurg Spine. 2010;12:402–8. doi: 10.3171/2009.10.SPINE08741. [DOI] [PubMed] [Google Scholar]
- 19.Kalanithi PS, Patil CG, Boakye M. National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine (Phila Pa 1976). 2009;34:1963,–9. doi: 10.1097/BRS.0b013e3181ae2243. [DOI] [PubMed] [Google Scholar]
- 20.Shamji MF, Cook C, Pietrobon R, Tackett S, Brown C, Isaacs RE. Impact of surgical approach on complications and resource utilization of cervical spine fusion a nationwide perspective to the surgical treatment of diffuse cervical spondylosis. Spine J. 2009;9:31–8. doi: 10.1016/j.spinee.2008.07.005. [DOI] [PubMed] [Google Scholar]
- 21.Yadla S, Malone J, Campbell PG , et al. Obesity and spine surgery reassessment based on a prospective evaluation of perioperative complications in elective degenerative thoracolumbar procedures. Spine J. 2010;10:581–7. doi: 10.1016/j.spinee.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 22.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303:1259–65. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]