Abstract
Purpose :
To compare the visual and optical outcomes of four multifocal intraocular lenses (IOLs) with three different near additions of +3.00 diopters (D), +3.75 D and +4.00 D.
Methods :
In this prospective study, 133 eyes of 88 patients were implanted with one of the following IOLs: AcrySof® ReSTOR® SN6AD1 (+3.00 D) for Group A, AcrivaUD Reviol BB MF 613 or BB MFM 611 (+3.75 D) for Group B, and AcrySof® ReSTOR® SN6AD3 (+4.00 D) for Group C. The visual acuity, refraction, intraocular pressure, tomography and corneal endothelial cell density (ECD) were compared between the three groups preoperatively and at 6 month postoperatively. Defocus curve, contrast sensitivity and higher order aberrations (HOAs) at 6 month postoperative visit were measured and compared.
Results :
There were no statistically significant differences in distance visual acuity, refraction, intraocular pressure or ECD among the three groups after 6 months (P > 0.05). The photopic contrast sensitivity in Group C was statistically better than in Group A (P < 0.05). The scotopic ocular aberration in Group B was statistically greater compared to that in Group A (P < 0.05). The highest near-visual peaks were -0.06 logMAR at a -2.50 D (40 cm) in Group A, -0.07 logMAR at -3.00D (33 cm) in Group B, and -0.06 logMAR at -3.50 D (29 cm) in Group C. Statistically significant differences in near and intermediate visual acuities were observed among the three groups at -2.00 D (50 cm), -2.50 D (40 cm), -3.50 D (29 cm) and -4.00 D (25 cm) (P < 0.01).
Conclusion :
AcrySof® ReSTOR® SN6AD1 IOLs (+3.00 D) and SN6AD3 (+4.00 D) IOLs provided the best intermediate and near vision, respectively. Both intermediate and near vision were comparatively better in the eyes with AcrivaUD Reviol BB MFM 611 IOLs or BB MF 613 IOLs (+3.75 D).
Keywords: Cataract surgery, multifocal intraocular lens, near addition.
INTRODUCTION
Multifocal intraocular lens (IOL) implantation is a popular presbyopia-correcting strategy to reduce dependence on reading spectacles by providing adequate vision over a range of distances [1-3]. Nowadays, several designs of multifocal IOL with range of near additions, such as +3.00 diopter (D), +3.50 D, +3.75 D, or +4.00 D, are available [4, 5]. In previous studies, the AcrySof® ReSTOR® SN6AD1 IOL (Alcon Corp., Fort Worth, Texas, United States) and Acry-Sof® ReSTOR® SN6AD3 IOL (Alcon Corp., Fort Worth, Texas, United States) with near additions of +3.00 D and +4.00 D have been demonstrated to be efficient aspheric IOL models [6, 7]. AcrivaUD Reviol (VSY Biotechnology, Amsterdam, Netherlands) is a recent addition to the diffractive multifocal intraocular lens designs with +3.75 D near add power which is available in two models: BB MF 613 and BB MFM 611. Having the identical optic design, these two models claim to yield satisfactory far, intermediate and near vision; the BB MFM 611 model is previously been shown to provide effective visual acuities and contrast sensitivities [8]. The aim of the current study is to evaluate and compare the visual and optical performances of eyes implanted with four multifocal IOL models having three different near additions, +3.00 diopters (D) (AcrySof® ReSTOR® SN6AD1), +3.75 D (AcrivaUD Reviol BB MF 613 and BB MFM 611) or +4.00 D (AcrySof® ReSTOR® SN6AD3).
PATIENTS AND METHODS
Study Design
This prospective single-center study comprised of cataract patients who underwent routine phacoemlsification with multifocal IOL implantation between the period January 2009 and December 2012 at the Shinagawa LASIK Center, Tokyo, Japan. Patients with either incipient or moderate cataract causing a significant reduction in visual qualities were included in the study. Presence of ocular pathology other than cataract, previous intraocular surgery, and significant corneal aberrations were exclusion criteria. One hundred and thirty-three eyes of 88 patients (58 women and 30 men) were recruited. The sample eyes were randomly divided into three groups: Group A eyes received multifocal IOLs with AcrySof® ReSTOR® SN6AD1 IOLs (+3.00 D); Group B eyes received AcrivaUD Reviol BB MF 613 or BB MFM 611 IOLs (+3.75 D); Group C eyes received AcrySof® ReSTOR® SN6AD3 IOLs (+4.00 D). Group A consisted of 29 eyes from 19 patients; Group B, 42 eyes from 30 patients; and Group C, 62 eyes from 39 patients. All subjects read and signed informed consent that explained the surgical procedure, possible risks, and their rights. The study was performed in accordance with the ethics codes established by the Ethical Board Committee in Japan.
Multifocal IOLs
Table 1 summarizes the specifications of each multifocal IOL used. All IOL models have a 6.0mm optic zone. Aspheric surfaces are designed to produce negative spherical aberration to compensate for the positive spherical aberration of the cornea. Both AcrySof® ReSTOR® SN6AD1 and AcrySof® ReSTOR® SN6AD3 consist of peripheral refractive zone and 3.6 mm apodized diffractive central design. The corresponding diffractive structures of the AcrySof® ReSTOR® SN6AD1 and AcrySof® ReSTOR® SN6AD3 have 9 and 12 steps, providing near additions of +3.00 D and +4.00 D, respectively. AcrivaUD Reviol BB MF 613 and BB MFM 611 have different diffractive ring distributions for intermediate and near vision with + 3.75 D near addition.
Table 1.
Intraocular lens characteristics.
| AcrySofÒ ReSTORÒ SN6AD1 |
AcrivaUD Reviol MF 613 |
AcrivaUD Reviol MFM 611 |
AcrySofÒ ReSTORÒ SN6AD3 |
|
|---|---|---|---|---|
| Type | Diffractive-refractive | Diffractive | Diffractive | Diffractive-refractive |
| Profile | Aspheric | Aspheric | Aspheric | Aspheric |
| Addition | +3.00 Diopters(D) | +3.75 D | +3.75 D | +4.00 D |
| Optic zone | 6.0 mm | 6.0 mm | 6.0 mm | 6.0 mm |
| Light distribution | 40–90% of light to distance focus |
65% of light to distance focus |
65% of light to distance focus |
40–90% of light to distance focus |
| Haptic design | C | C | Plate | C |
| Overall diameter | 13.0 mm | 13.0 mm | 11.0 mm | 13.0 mm |
| Range | +6.00 D to +34.00 D | 0.00 D to +45.00 D | 0.00 D to +45.00 D | +6.00 D to +34.00 D |
| Material | Hydrophobic acrylate | Hydrophilic acrylic (25%) with hydrophobic surface |
Hydrophilic acrylic (25%) with hydrophobic surface |
Hydrophobic acrylate |
| Blue filter | Yes | No | No | Yes |
| A-constant | 118.9 | 118.0 | 118.0 | 118.9 |
Surgical Technique
The IOLMaster (Carl Zeiss Meditec, Jena, Germany) was used for preoperative biometry and IOL power calculations. Femtosecond laser (CatalysTM Precision Laser System, Optimedica Corp., Sunnyvale, California, United States) was routinely used for the continuous curvilinear capsulorrhexis (CCC) and lens fragmentation [9]. Phacoemulsification was performed using Infinity phacoemulsification machine (Alcon Corp., Fort Worth, Texas, United States). The steepest corneal meridian was selected for the surgical incision. After aspirating the residual cortex, study assigned multifocal IOL was implanted into the intact capsular bag. All surgeries were performed by the same surgeon (M.T.).
Postoperative Treatments
In all cases, post-operative medications comprised a 500 mg oral levofloxacin (Daiichi Sankyo, CravitTM, Tokyo, Japan) once a day for three days, 0.1% diclofenac sodium eye drops (Nitto Medic, Toyama, Japan), 0.1% dexametha-sone metasulfobenzoate sodium (Nitto Medic, D•E•XTM, Toyama, Japan), and 0.5% moxifloxacin hydrochloride (Alcon Corp., VegamoxTM, Fort Worth, Texas, United States) 5 times a day for 1 week. The diclofenac was reduced to 4 times a day for 1 month after first week. Latter two were switched to topical 0.1% fluorometholone ophthalmic suspension (Nitto Medic, Toyama, Japan) and 0.3% ofloxin ophthalmic solution (Nitto Medic, Toyama, Japan) 4 times a day for up to 1 month and discontinued thereafter.
Preoperative and Postoperative Examinations
Patients were examined preoperatively and at 1day, 7 days, 1 month, 3 months and 6 months postoperatively. Uncorrected and corrected near and distance visual acuities (UDVA) were measured at all postoperative visits by the same masked optometrist. Clinical refraction was performed at each visit using sphere, cylinder, and manifest spherical equivalent (MRSE) notations. Defocus curve was obtained using a previously reported method [10-12]. Visual acuities were converted to logMAR for statistical analysis. Contrast sensitivity was measured using the TakagiTM Contrast Glare Tester CGT-1000 (Takagi Seiko, Nagano-Ken, Japan) with best spectacle correction under photopic (illumination of 21 candela (cd)/m2) and scotopic (illumination of 11 cd/m2) conditions [13]. Wave-Front AnalyzerTM KR-1W (Topcon Corp., Tokyo, Japan) was utilized to measure higher order aberrations (HOAs) under photopic (4-mm pupil diameter) and scotopic (6-mm pupil diameter) conditions. Postope-rative complications, if any, were evaluated using comprehensive ocular examinations that included slit lamp biomicroscopy, funduscopy, intraocular pressure (Computer-ized Tonometer, Topcon, Japan), tomography (PentacamTM, Oculus Optikgeräte GmbH, Wetzlar, Germany) and corneal endothelial cell count (Noncon RoboTM FA3609; Konan Medical, Irvine, California, USA) [14].
Statistical Analysis
Statistical analysis was performed with JMP 9 statistical package (SAS Institute, Inc., Cary, NC, USA) software. Descriptive statistical results are presented as mean and standard deviation. Categorical variables were compared using the Pearson’s chi-square test. Where applicable, Oneway Anova with Tukey’s HSD test was used to compare the results among the three groups. The Kruskal-Wallis test with Steel-Dwass test was used to compare the three IOL groups for non-parametric variables. Results with P < 0.05 were considered statistically significant.
RESULTS
Table 2 illustrates the preoperative characteristics of the eyes. There were no statistical differences between the groups in terms of gender, age, IOL power, UDVA, sphere, cylinder, MRSE, UNVA, intraocular pressure or corneal endothelial cell density (ECD) preoperatively (P > 0.05). The mean values of CDVA and CNVA in Group B eyes were statistically significantly better than in the eyes of Group C (P = 0.0258 and P = 0.0266, respectively).
Table 2.
Preoperative conditions of the three groups.
| Parameters | Group A (+3.00D) |
Group B (+3.75D) |
Group C (+4.00D) |
P Values Among Three Groups |
P Values of Post Hoc Comparison | ||
|---|---|---|---|---|---|---|---|
| A vs B | A vs C | B vs C | |||||
| Gender (F/M, eyes) | 15 / 14 | 30 / 12 | 46 / 16 | 0.0972 | |||
| Age, years | 61.39±6.53 | 60.60±6.63 | 61.53±5.43 | 0.6490 | |||
| IOL power, D | 18.07±5.15 | 15.39±6.37 | 16.35±6.23 | 0.2800 | |||
| UDVA, LogMAR | 0.77±0.50 | 0.82±0.56 | 0.87±0.52 | 0.5681 | |||
| CDVA, LogMAR | 0.06±0.18 | 0.01±0.19 | 0.07±0.17 | 0.0312 | NS | NS | 0.0258 |
| Sphere, D | -1.43±5.54 | -3.02±5.25 | -2.86±5.02 | 0.2547 | |||
| Cylinder, D | -1.06±0.79 | -0.85±0.63 | -0.95±0.68 | 0.7300 | |||
| MRSE, D | -1.96±5.41 | -3.44±5.27 | -3.33±5.11 | 0.3494 | |||
| UNVA, LogMAR | 0.84±0.32 | 0.70±0.41 | 0.85±0.32 | 0.4600 | |||
| CNVA, LogMAR | 0.13±0.16 | 0.09±0.18 | 0.14±0.19 | 0.0239 | NS | NS | 0.0266 |
| IOP, mmHg | 12.60±2.81 | 13.2±2.79 | 13.20±2.67 | 0.7153 | |||
| ECD, cells/mm2 | 2749.21±305.65 | 2717.60±346.45 | 2704.11±322.92 | 0.7848 | |||
UDVA, uncorrected distance visual acuity; CDVA, corrected distance visual acuity; MRSE, manifest refraction spherical equivalent; UNVA, uncorrected near visual acuity; CNVA, corrected near visual acuity; D, diopter; IOP, intraocular pressure; ECD, corneal endothelial cell density; NS, no significance. P, statistical difference among the three groups.
Table 3 shows 6-month postoperative conditions of the eyes No statistical differences were observed for UDVA, CDVA, sphere, cylinder, MRSE, intraocular pressure or corneal endothelial cell density among the three groups (P ( 0.05). The mean values of UNVA and CNVA in the eyes of Group C were significantly better than in the eyes of Group A (P = 0.0284 and P = 0.0062, respectively).
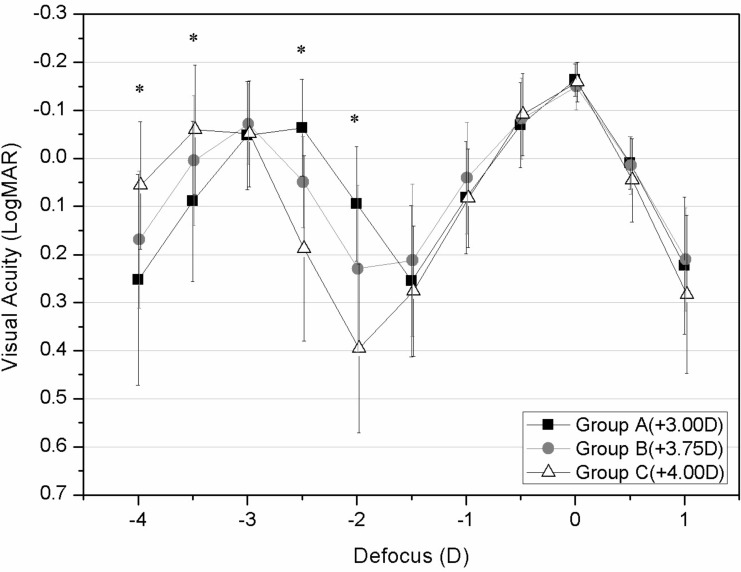
Defocus curves of the three groups at 6-month postoperatively are illustrated in Fig. (1). There was no statistically significant difference in visual acuities among the three groups when the defocus level was more than -1.50 D (67 cm and beyond). The highest near-visual peaks were -0.06 logMAR at a defocus level of -2.50 D (40 cm) in Group A, -0.07 logMAR at -3.00 D (33 cm) in Group B, and -0.06 logMAR at -3.50 D (29 cm) in Group C. The differences in visual acuity between the viewing distance range of -2.50 D (40 cm) and -2.00 D (50 cm) were statistically significant (P < 0.0001). The visual acuities in Group B were significantly better than those in Group C (P < 0.05), but statistically worse than those in Group A (P < 0.05).
Fig. (1).
Six-month postoperative visual acuity (mean and standard deviation) at different levels of defocus for three groups. ∗, significant different between thre groups (P < 0.05).
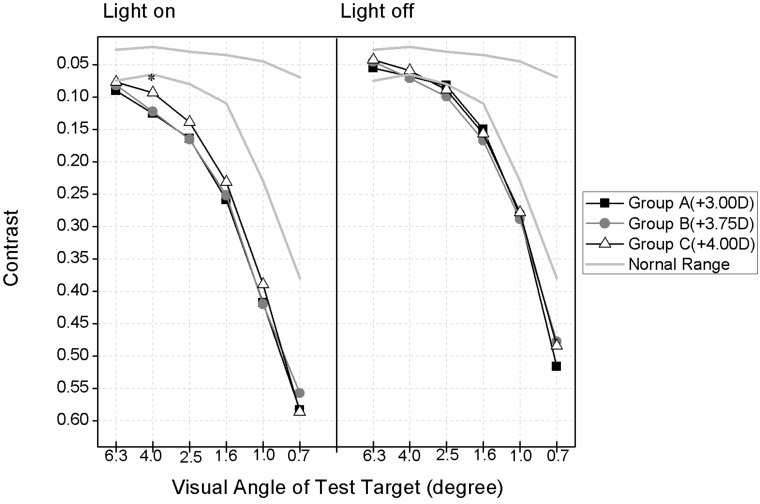
Fig. (2) shows the 6-month postoperative performances in terms of contrast sensitivity of the eyes in the different groups. At a visual angle of 4.0 degrees, the photopic contrast of the eyes in Group C was statistically better than that in Group A (P = 0.0237). No other variables showed statistically significant differences among the groups under photopic or mesopic condition (P ( 0.05).
Fig. (2).
Six-month postoperative contrast sensitivity under photopic (light on, 21 candela (cd)/m2) and mesopic (light off, 11 cd/m2) conditions of eyes implanted with different MIOLs. ∗, significant different between thre groups (P < 0.05).
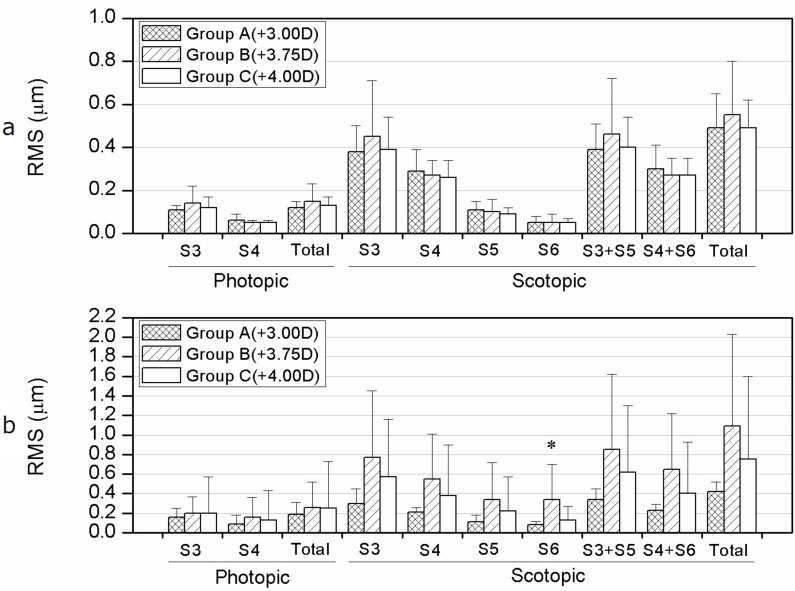
There was no statistically significant difference (P > 0.05) in the corneal HOAs among the groups (Fig. 3). Under the scotopic condition (6-mm pupil diameter), ocular S6 of Group B was statistically greater than in Group A eyes (P = 0.0317). No other components of corneal and coular HOA aberrations showed a statistical difference among the groups under photopic or mesopic conditions (P > 0.05).
Fig. (3).
Six-month postoperative high-order aberrations (HOAs) under photopic (4-mm pupil diameter) and mesopic (6-mm pupil diameter) conditions of eyes implanted with different MIOLs. a, the corneal HOAs of the eyes in three groups. b, the ocular HOAs of the eyes in three groups. ∗, significant different between thre groups (P < 0.05).
DISCUSSION
Unlike monofocal IOLs, multifocal IOLs can avoid the postoperative monovision and presbyopia in pseudophakic eyes. Multifocal IOLs could simultaneously provide practically good near, intermediate and distance vision through their refractive or diffractive optical designs with one or multiple addition powers [15]. In this study, three different near additions (+3.00 D, +3.75 D and +4.00 D) in four multifocal IOL designs were compared for their efficacy. The outcome information may be invaluable in choosing the suitable multifocal IOL models for a patient.
Excellent distance visual acuity was achieved in all study groups six months postoperatively. The mean UDVA and CDVA in all groups reached 0.00 logMAR and -0.14 logMAR or better demonstrating a good efficiency of tested IOLs for distance vision. Similaroutcomes were reported previously [5-8]. de Vries et al. [6] reported mean UDVA and CDVA of 0.04 logMAR and -0.04 logMAR in eyes implanted with AcrySof® ReSTOR® SN6AD1 IOLs, respectively. In eyes implanted with AcrySof® ReSTOR® SN6AD3 IOLs, UDVA and CDVA were 0.14 logMAR and -0.01logMAR, respectively. In another study by Izzet Can et al. [8], eyes implanted with AcrivaUD Reviol BB MFM 611 IOLs achieved mean uncorrected distance visions of 0.07 logMAR and mean CDVA of 0.02 logMAR. To the best of our knowledge, visual and optical outcome of AcrivaUD Reviol BB MF 613 IOL models have not been reported. Furthermore, this is the first study comparing the differences in outcome for various models of IOLs.
Unlike the similarity in distance visions, significant differences in near and intermediate visual acuities between the groups receiving different near add powers were observed. The mean UNVA and CNVA in eyes with any IOL model reached 0.21 logMAR and 0.03 logMAR or better. Statistically significant differences in both UNVA and CNVA were found between Group A and Group C. It should be noted that, near visual acuity was measured at a distance of 30 cm according to the custom in Japan [16], which was different from the 40 cm used in other countries.
To evaluate the visual behaviors of these multifocal IOL models at different viewing distances, a defocus curve was created by using different levels of defocus [12, 11, 17]. No difference was observed among the three groups in terms of visual acuities at a viewing distance range of 67 cm (-1.50 D) and beyond (P > 0.05). The highest near-visual peak in Group A eyes (+3.00 D) located at a distance of 40 cm (-2.50 D). AcrySof® ReSTOR® SN6AD1 IOLs provided the best vision at a viewing distance ranging between 40 cm and 50 cm (-2.00 D) (P < 0.0001). On the other hand, the highest near-visual peak in Group C eyes (+4.00 D) were located at the distance of 29 cm (-3.50 D). AcrySof® ReSTOR® SN6AD3 IOLs provided the best vision at a viewing distance ranging between 25 cm (-4.00 D) and 29 cm (P < 0.01).
AcrivaUD Reviol BB MFM 611 or BB MF 613 IOLs likewise provided satisfactory distance, intermediate and near visions during the entire range of viewing distances. The highest near-visual peak in Group B eyes (+3.75 D) was located at the distance of 33 cm (-3.00 D). AcrivaUD Reviol BB MFM 611 or BB MF 613 IOLs provided better visions than ReSTOR® SN6AD3 IOLs at a viewing distance range between 40 cm and 50 cm (-2.00 D) (P < 0.05). The best performance in intermediate vision among the three groups was observed in Group B (+3.75 D).
Previous studies have demonstrated that multifocal IOLs reduce the optical quality and negatively affect functional performance [18, 19]. The postoperative contrast sensitivities in this study were consistently lower than that of the normal range, especially under the photopic conditions which might be due to increased straylight leading to reduced optical performance [20, 21]. Except for the 4.0 degrees of photopic condition, no statistically significant difference in contrast sensitivity was observed between the groups in the current study,. Similar outcomes were reported in previous studies [6, 22]. It appears that different optic designs of the multifocal IOL models studied in this study resulted comparable straylights effects.
Postoperative wavefront aberrations of the various multifocal IOL models were evaluated. Only statistical difference was observed for S6 component of the aberration (P = 0.0317); all other corneal or ocular HOAs under photopic or scotopic vision (P > 0.05) showed no difference between the groups. Nevertheless, since two or more wavefronts could be produced simultaneously when light passes through a multifocal IOL, there was no certainty which particular wavefront was being measured by the Hartmann-Shack sensors during the test [23]. We used the Wave-Front AnalyzerTM to measure HOAs of the postoperative eyes [24]. The wavelength (840 nm) used in this technique which is longer than the visible wavelength that is used during the process of multifocal IOLs designing [25]. Thus, we believe that the HOAs recorded in this study is likely to have represented the optical characteristics of the distance segment [6, 25].
In recent days, people are ever more dependent on the intermediate and near vision than before to perform close-up tasks, such as browsing internet and reading messages on mobile phones. Since varieties of multifocal IOL models with different near additions are available, choosing a suitable one for a patient is often challenging. Although all models resulted in a satisfactory distance visions in the current study, difference in intermediate and near visual were observed. The authors believe that surgeons should consider patient’s nature of near vision tasks. For instance, if a patient prefers performing tasks at arms’ length, implantation of AcrySof® ReSTOR® SN6AD1 IOL may be recommended which offer good intermediate and distance vision. In contrast, if a patient is a handworker, a stronger near addition models such as AcrySof® ReSTOR® SN6AD3 IOLs may be advisable. While most of the patients would like to have an extended range clear vision, both AcrivaUD Reviol BB MFM 611 IOL and BB MF 613 IOL would be preferable.
CONCLUSION
In conclusion, multifocal IOL models with different near additions offered comparable distance visual outcome. While IOLs with +3.00 D (AcrySof® ReSTOR® SN6AD1) and and +4.00 D (SN6AD3) additions provided the best intermediate and near vision, respectively, IOL with +3.75 D (AcrivaUD Reviol BB MFM 611 and MF 613) offered better performance for both intermediate and near vision.
Table 3.
Six-month postoperative conditions of the three groups.
| Parameters | Group A (+3.00D) | Group B (+3.75D) | Group C (+4.00D) |
P Values Among Three Groups |
P Values of Post Hoc Comparison | ||
|---|---|---|---|---|---|---|---|
| A vs B | A vs C | B vs C | |||||
| UDVA, LogMAR | -0.02±0.13 | -0.05±0.10 | 0.00±0.13 | 0.3339 | |||
| CDVA, LogMAR | -0.16±0.04 | -0.14±0.07 | -0.16±0.04 | 0.3341 | |||
| Sphere, D | 0.82±0.50 | 0.96±0.47 | 0.78±0.53 | 0.2800 | |||
| Cylinder, D | -0.90±0.48 | -0.64±0.53 | -0.71±0.40 | 0.0903 | |||
| MRSE, D | 0.38±0.47 | 0.64±0.45 | 0.43±0.48 | 0.0628 | |||
| UNVA, LogMAR | 0.21±0.17 | 0.18±0.14 | 0.12±0.14 | 0.0129 | NS | 0.0284 | NS |
| CNVA, LogMAR | 0.01±0.03 | 0.03±0.10 | 0.00±0.02 | 0.0062 | NS | 0.0062 | NS |
| IOP, mmHg | 10.26±2.58 | 11.14±2.55 | 11.52±2.69 | 0.1513 | |||
| ECD, cells/mm2 | 2656.09±318.36 | 2365.00±380.13 | 2573.07±388.28 | 0.2751 | |||
UDVA, uncorrected distance visual acuity; CDVA, corrected distance visual acuity; MRSE, manifest refraction spherical equivalent; UNVA, uncorrected near visual acuity; CNVA, corrected near visual acuity; D, diopter; IOP, intraocular pressure; ECD, corneal endothelial cell density. P, statistical difference among the three groups; NS, no significance.
ACKNOWLEDGEMENTS
Declared none.
CONFLICT OF INTEREST
Dr. Tomita is a consultant for VSY Biotechnology Inc. The authors report no other conflict of interest in this work.
REFERENCES
- 1.Dexl AK, Zaluski S, Rasp M, Grabner G. Visual performance after bilateral implantation of a new diffractive aspheric multifocal intraocular lens with a 3. D addition. Eur J Ophthalmol. 2013;24(1):35–43. doi: 10.5301/ejo.5000315. [DOI] [PubMed] [Google Scholar]
- 2.Alió JL, Plaza-Puche AB, Montalban R, Javaloy J. Visual outcomes with a single-optic accommodating intraocular lens and a low-addition-power rotational asymmetric multifocal intraocular lens. J Cataract Refract Surg. 2012;38(6):978–85. doi: 10.1016/j.jcrs.2011.12.033. [DOI] [PubMed] [Google Scholar]
- 3.Lubiκski W, Podboraczyκska-Jodko K, Gronkowska-Serafin J, Karczewicz D. Visual outcomes three and six months after implantation of diffractive and refractive multifocal IOL combinations. Klinika Oczna. 2011;113(7-9):209–15. [PubMed] [Google Scholar]
- 4.Rabsilber TM, Rudalevicius P, Jasinskas V, Holzer MP, Auffarth GU. Influence of +3.0 D and +4.00 D near addition on functional outcomes of a refractive multifocal intraocular lens model. J Cataract Refract Surg. 2013;39(3):350–57. doi: 10.1016/j.jcrs.2012.09.026. [DOI] [PubMed] [Google Scholar]
- 5.Alió JL, Grabner G, Plaza-Puche AB , et al. Postoperative bilateral reading performance with 4 intraocular lens models 6-month results. J Cataract Refract Surg. 2011;37(5):842–52. doi: 10.1016/j.jcrs.2010.11.039. [DOI] [PubMed] [Google Scholar]
- 6.de Vries NE, Webers CA, Montés-Micó R, Ferrer-Blasco T, Nuijts RM. Visual outcomes after cataract surgery with implantation of a +3.0 D or +4.00 D aspheric diffractive multifocal intraocular lens Comparative study. J Cataract Refract Surg. 2010;36(8):1316–22. doi: 10.1016/j.jcrs.2010.01.036. [DOI] [PubMed] [Google Scholar]
- 7.Toto L, Carpineto P, Falconio G , et al. Comparative study of Acrysof ReSTOR multifocal intraocular lenses +4.0 D and +3.00 D Visual performance and wavefront error. Clin Exp Optom. 2013;96(3):295–302. doi: 10.1111/j.1444-0938.2012.00815.x. [DOI] [PubMed] [Google Scholar]
- 8.Can I, Bostancκ Ceran B, Soyugelen G, Takmaz T. Comparison of clinical outcomes with 2 small-incision diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2012;38(1):60–7. doi: 10.1016/j.jcrs.2011.07.036. [DOI] [PubMed] [Google Scholar]
- 9.Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation of the nucleus with different softening grid sizes on effective phaco time in cataract surgery. J Cataract Refract Surg. 2012;38(11):1888–94. doi: 10.1016/j.jcrs.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 10.Buckhurst PJ, Wolffsohn JS, Naroo SA. Multifocal intraocular lens differentiation using defocus curves. Invest Ophthalmol Vis Sci. 2012;53(7):3920–6. doi: 10.1167/iovs.11-9234. [DOI] [PubMed] [Google Scholar]
- 11.Gupta N, Wolffsohn JS, Naroo SA. Optimizing measurement of subjective amplitude of accommodation with defocus curves. J Cataract Refract Surg. 2008;34(8):1329–38. doi: 10.1016/j.jcrs.2008.04.031. [DOI] [PubMed] [Google Scholar]
- 12.Wolffsohn JS, Jinabhai AN, Kingsnorth A , et al. Exploring the optimum step size for defocus curves. J Cataract Refract Surg. 2013;39(6):873–80. doi: 10.1016/j.jcrs.2013.01.031. [DOI] [PubMed] [Google Scholar]
- 13.Pesudovs K. Takagi Glare Tester CGT-1000 for contrast sensitivity and glare testing in normal individuals and cataract patients. J Refract Surg. 2007;23(5):492–8. doi: 10.3928/1081-597X-20070501-13. [DOI] [PubMed] [Google Scholar]
- 14.Price MO, Fairchild KM, Price FW ., Jr Comparison of manual and automated endothelial cell density analysis in normal eyes and DSEK eyes. Cornea. 2013;32(5):567–73. doi: 10.1097/ICO.0b013e31825de8fa. [DOI] [PubMed] [Google Scholar]
- 15.Bellucci R. Multifocal intraocular lenses. Curr Opin Ophthalmol. 2005;16(1):33–7. doi: 10.1097/00055735-200502000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Tomita M, Kanamori T, Waring GO 4th , et al. Simultaneous corneal inlay implantation and laser in situ keratomileusis for presbyopia in patients with hyperopia, myopia, or emmetropia Six-month results. J Cataract Refract Surg. 2012;38(3):495–506. doi: 10.1016/j.jcrs.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 17.Petermeier K, Messias A, Gekeler F, Szurman P. Effect of +300 diopter and +400 diopter additions in multifocal intraocular lenses on defocus profiles, patient satisfaction, and contrast sensitivity. J Cataract Refract Surg. 2011;37(4):720–6. doi: 10.1016/j.jcrs.2010.11.027. [DOI] [PubMed] [Google Scholar]
- 18.Vaquero M, Encinas JL, Jimenez F. Visual function with monofocal versus multifocal IOLs. J Cataract Refract Surg. 1996;22(9):1222–5. doi: 10.1016/s0886-3350(96)80071-x. [DOI] [PubMed] [Google Scholar]
- 19.Montés-Micó R, España E, Bueno I, Charman WN, Menezo JL. Visual performance with multifocal intraocular lenses Mesopic contrast sensitivity under distance and near conditions. Ophthalmology. 2004;111(1):85–96. doi: 10.1016/S0161-6420(03)00862-5. [DOI] [PubMed] [Google Scholar]
- 20.Montés-Micó R, Alió JL. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J Cataract Refract Surg. 2003;29(4):703–11. doi: 10.1016/s0886-3350(02)01648-6. [DOI] [PubMed] [Google Scholar]
- 21.Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35(6):992–7. doi: 10.1016/j.jcrs.2009.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Santhiago MR, Wilson SE, Netto MV , et al. Modulation transfer function and optical quality after bilateral implantation of a +300 D versus a +400 D multifocal intraocular lens. J Cataract Refract Surg. 2012;38(2):215–20. doi: 10.1016/j.jcrs.2011.08.029. [DOI] [PubMed] [Google Scholar]
- 23.Charman WN, Montés-Micó R, Radhakrishnan H. Can we measure wave aberration in patients with diffractive IOLsκ. J Cataract Refract Surg. 2007;33(11):1997. doi: 10.1016/j.jcrs.2007.06.052. [DOI] [PubMed] [Google Scholar]
- 24.Kuroda T, Fujikado T, Maeda N, Oshika T, Hirohara Y, Mihashi T. Wavefront analysis of higher-order aberrations in patients with cataract. J Cataract Refract Surg. 2002;28(3):438–44. doi: 10.1016/s0886-3350(01)01176-2. [DOI] [PubMed] [Google Scholar]
- 25.Charman WN, Montés-Micó R, Radhakrishnan H. Problems in the measurement of wavefront aberration for eyes implanted with diffractive bifocal and multifocal intraocular lenses. J Refract Surg. 2008;24(3):280–6. doi: 10.3928/1081597X-20080301-10. [DOI] [PubMed] [Google Scholar]