As we are witnessing a global increase in terrorist acts perpetrated for political, religious, or socioeconomic goals with the aim to create fear, coercion, or intimidation, the question about the mental and physical implications of such violent acts has become paramount for healthcare systems (1). For example, studies have shown that about one in five victims who survive a terrorist attack will develop posttraumatic stress disorder that is characterized by symptoms such as intrusive memories and nightmares of the violent act, feeling emotionally numb and easily startled (2, 3). Other frequent terror-induced mental disorders are depression and substance abuse or the mere fear of further violent acts. The “physiologic storm” launched through intense emotional stress, including terrorist acts, comprises acute increases in heart rate (HR) and blood pressure, constriction of heart vessels, inflammation activation, and thickening of the blood, all of which underlie the triggering of a heart attack and sudden death (4, 5). Compared with the accumulated knowledge of the more acute health effects of terrorist acts, the consequences for physical health of chronic exposure to the fear of becoming a victim of or witnessing terrorist acts are far from being elucidated. The paper by Shenhar-Tsarfaty et al. (6) in PNAS is thus a major step forward in sensitizing health care professionals and policy makers alike for the sequels of perpetuated fear of terror (FOT) for heart health.
According to estimates of the World Health Organization, cardiovascular diseases (CVD), including heart attacks and stroke, are projected to remain the single leading cause of death by 2030 worldwide; moreover, by that time coronary heart disease (CHD) and depression will be ranking among the three leading causes of global burden of disease (7). To the extent that millions of people are directly or indirectly exposed via the mass media to FOT and that this exposure seems unlikely to wane in the foreseeable future, we can only speculate about a significant additional share to the global burden of CVD and mental disorders, including depression, inflicted by terrorism.
Whereas CHD is a disease of the blood vessels insufficiently supplying the heart muscle with oxygen, depression is an emotional disorder characterized by symptoms such as loss of interest in joyful activities, fatigue, and poor appetite. What may seem like two distinct disorders with relevance for global health actually show considerable coincidence. For example, up to 40% of patients with CHD report clinically relevant symptoms of depression, which, in turn, are associated with poor prognosis of the heart disease (8). Studying the nature of the mutual relationship between psychosocial factors like depression and CVD lies at the core of behavioral cardiology (9).
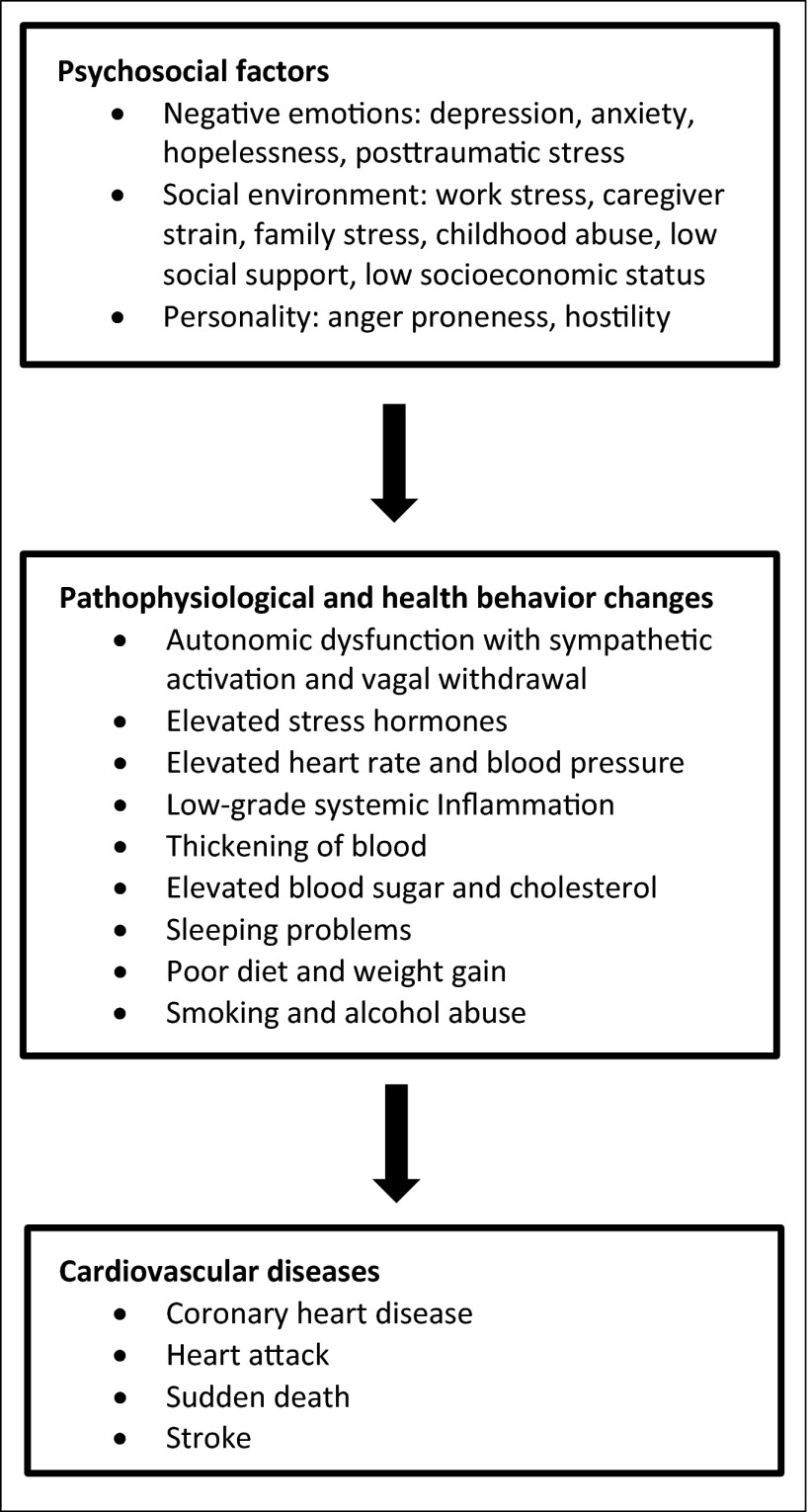
“Behavioral cardiology” is a term that has been coined for a medical discipline claiming that heart disease is not fateful and “all in the genes,” but much develops from an unhealthy lifestyle that includes smoking, too little physical exercise, and eating too much, as well as from psychosocial factors. Fig. 1 shows acknowledged psychosocial risk factors for CVD, which explain as much of the relative risk in heart disease-related outcomes as do traditional CVD risk factors, such as diabetes, high cholesterol, and high blood pressure (8, 9). Should the findings about cardiovascular harm from FOT reported by Shenhar-Tsarfaty et al. (6) be replicated in future studies, FOT would seem a likely candidate to be included in the list of psychosocial risk factors among the category of negative emotions.
Fig. 1.
The behavioral cardiology view of CVDs. Depicted are the pathophysiologic and behavioral mechanisms which link psychosocial factors to an increased risk of CVD (8, 9).
Pursuing a truly bench-to-bedside approach, behavioral cardiology is in the vanguard of the translational medicine movement (10). Specifically, the crucial question about the biobehavioral pathways through which psychosocial factors impact heart health (Fig. 1) and how these can be modified to benefit humans has been attracting researchers for many decades, spanning various fields from basic molecular science (11) to clinical psychotherapy (12). The study by Shenhar-Tsarfaty et al. (6) bears witness to the fact that this scientific endeavor is vigorously continuing. In a carefully conducted and methodologically sound large-scale study, applying sophisticated statistics, the authors investigated the effect of perceived FOT, tapping feelings of worry about personal and family safety and tension in crowded places, on heart health in healthy employees from Israel, whose population has been exposed to the stress of terror attacks for many decades. Despite the study’s strengths, the specifics of the study design may have influenced the results, as populations with more sick and older people and from societies with shorter periods of time to adjust to ongoing threat might respond physiologically differently to FOT.
Specifically, Shenhar-Tsarfaty et al. (6) found that pertinent FOT relates to annual increases in HR (that is, pulse). The importance of this finding for health outcomes is underscored by the fact that resting HR has been shown to be a potent proxy measure for an increased risk of CVD and all-cause mortality in prospective population-based studies (13). In behavioral cardiology terms, the novelty and major strength of the paper by Shenhar-Tsarfaty et al. (6) is the longitudinal assessment of HR, while taking into account an extensive number of demographic, lifestyle, physical performance/morbidity, and psychosocial factors. Particularly, the relation between FOT and annual increase in HR was not accounted for by depression, anxiety, job burnout, and sleep problems.
Although theirs is not an experimental study, Shenhar-Tsarfaty et al. (6) further set out to identify specific biobehavioral mechanisms potentially linking FOT with HR focusing on the chronic low-grade systemic inflammatory state and its regulation through the cholinergic anti-inflammatory reflex. The latter aspect refers to the observation that the vagus nerve modulates the innate immune response by inhibiting overshooting production of proinflammatory cytokines by immunocompetent cells via stimulation of the α7 subunit of the nicotinic acetylcholine receptor (14). Chronic psychosocial stress and negative emotions decrease vagal tone and activate the sympathetic branch of the autonomic nervous system. Shenhar-Tsarfaty et al. (6) found that the effect of circulating levels of highly-sensitive C-reactive protein (CRP), arguably the most accepted biomarker of chronic low-grade systemic inflammation, adds to the one of FOT, such that the risk of an increase in HR over time was greatest in individuals high in both FOT and CRP levels.
Production and release of CRP by hepatocytes is induced by proinflammatory cytokines activating nuclear transcription factors as part of the innate immune response that becomes activated in states of chronic psychosocial stress (15). It has been suggested that CRP is both a marker and inductor of CVD. Importantly, minor (“low-grade”) elevations of CRP levels in the blood have been shown to predict sudden death and add prognostic information on future risk of CHD above and beyond traditional risk factors (16). In a strict sense, the longitudinal
Shenhar-Tsarfaty et al. elegantly demonstrate that low-grade inflammation and its control by cholinergic signaling affect resting HR, whereas inflammation together with FOT predict HR increase over time.
design of the study by Shenhar-Tsarfaty et al. (6) does not allow drawing causal inferences about the direction of the relations between annual increases in values of FOT, CRP, and HR. Nevertheless, the primary result from this study provides one plausible mechanism by which chronic stress-related arousal, as evidenced by low-grade inflammation and decreased vagal tone, might impair cardiovascular health and increase mortality risk.
Regarding basal HR values, Shenhar-Tsarfaty et al. (6) found higher inflammatory status and, expectedly, sports activities to be predictive. In contrast, FOT or any other psychosocial variable did not emerge as a significant predictor of basal HR. Nonetheless, and of high interest, performing an investigation on a subgroup of volunteers, the authors found lower cholinergic signaling in those with CRP levels in the high-risk range of CVD compared with those with lower levels, thereby corroborating the cholinergic anti-inflammatory effect. Cholinergic signaling further predicted resting HR in men.
Taken together, the results from the study by Shenhar-Tsarfaty et al. (6) elegantly demonstrate that low-grade inflammation and its control by cholinergic signaling affect resting HR, whereas inflammation together with FOT predict HR increase over time. Heart rate is an easily collectible measure of cardiovascular function that can be lowered by means that increase vagal activity, such as regular physical exercise, some medications, and mind-body therapies (13, 17). These procedures can feasibly be applied in clinical settings with implications important to translational medicine. That is, the monitoring of HR increases over time might help to identify individuals at an increased risk to develop CVD and to die prematurely as a consequence of sustained exposure to terror threats. The screening for trajectories in HR over time might serve as a decision tool to initiate preventive efforts to possibly maintain or even improve health in areas struck by terrorism, where poor health-care resources are also often an issue.
Footnotes
The author declares no conflict of interest.
See companion article on page E467.
References
- 1.Institute for Economics and Peace . Global Terrorism Index 2014: Measuring and Understanding the Impact of Terrorism. Sydney: Institute for Economics and Peace; 2014. [Google Scholar]
- 2.Shalev AY, Freedman S. PTSD following terrorist attacks: A prospective evaluation. Am J Psychiatry. 2005;162(6):1188–1191. doi: 10.1176/appi.ajp.162.6.1188. [DOI] [PubMed] [Google Scholar]
- 3.DiGrande L, Neria Y, Brackbill RM, Pulliam P, Galea S. Long-term posttraumatic stress symptoms among 3,271 civilian survivors of the September 11, 2001, terrorist attacks on the World Trade Center. Am J Epidemiol. 2011;173(3):271–281. doi: 10.1093/aje/kwq372. [DOI] [PubMed] [Google Scholar]
- 4.Burg MM, et al. The ‘perfect storm’ and acute coronary syndrome onset: Do psychosocial factors play a role? Prog Cardiovasc Dis. 2013;55(6):601–610. doi: 10.1016/j.pcad.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meisel SR, et al. Effect of Iraqi missile war on incidence of acute myocardial infarction and sudden death in Israeli civilians. Lancet. 1991;338(8768):660–661. doi: 10.1016/0140-6736(91)91234-l. [DOI] [PubMed] [Google Scholar]
- 6.Shenhar-Tsarfaty S, et al. Fear and C-reactive protein cosynergize annual pulse increases in healthy adults. Proc Natl Acad Sci USA. 2015;112:E467–E471. doi: 10.1073/pnas.1418264112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.von Känel R. Psychosocial stress and cardiovascular risk: Current opinion. Swiss Med Wkly. 2012;142:w13502. doi: 10.4414/smw.2012.13502. [DOI] [PubMed] [Google Scholar]
- 9.Rozanski A. Behavioral cardiology: Current advances and future directions. J Am Coll Cardiol. 2014;64(1):100–110. doi: 10.1016/j.jacc.2014.03.047. [DOI] [PubMed] [Google Scholar]
- 10.Woolf SH. The meaning of translational research and why it matters. JAMA. 2008;299(2):211–213. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- 11.Cho JH, et al. Molecular evidence of stress-induced acute heart injury in a mouse model simulating posttraumatic stress disorder. Proc Natl Acad Sci USA. 2014;111(8):3188–3193. doi: 10.1073/pnas.1400113111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ye S, et al. Long-term outcomes of enhanced depression treatment in patients with acute coronary syndromes. Am J Med. 2014;127(10):1012–1016. doi: 10.1016/j.amjmed.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cook S, Togni M, Schaub MC, Wenaweser P, Hess OM. High heart rate: A cardiovascular risk factor? Eur Heart J. 2006;27(20):2387–2393. doi: 10.1093/eurheartj/ehl259. [DOI] [PubMed] [Google Scholar]
- 14.Rosas-Ballina M, Tracey KJ. The neurology of the immune system: neural reflexes regulate immunity. Neuron. 2009;64(1):28–32. doi: 10.1016/j.neuron.2009.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hänsel A, Hong S, Cámara RJ, von Känel R. Inflammation as a psychophysiological biomarker in chronic psychosocial stress. Neurosci Biobehav Rev. 2010;35(1):115–121. doi: 10.1016/j.neubiorev.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 16.Pearson TA, et al. Centers for Disease Control and Prevention American Heart Association Markers of inflammation and cardiovascular disease: Application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107(3):499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 17.Cramer H, et al. Effects of yoga on cardiovascular disease risk factors: A systematic review and meta-analysis. Int J Cardiol. 2014;173(2):170–183. doi: 10.1016/j.ijcard.2014.02.017. [DOI] [PubMed] [Google Scholar]