Abstract
Successfully addressing the problem of falls among people with multiple sclerosis (MS) will require the translation of research findings into practice change. This process is not easy but can be facilitated by using frameworks such as RE-AIM during the process of planning, implementing, and evaluating MS falls-prevention interventions. RE-AIM stands for Reach, Effectiveness, Adoption, Implementation, and Maintenance. Since its initial publication in 1999, the RE-AIM framework has become widely recognized across a range of disciplines as a valuable tool to guide thinking about the development and evaluation of interventions intended for widespread dissemination. For this reason, it was selected by the International MS Falls Prevention Research Network to structure initial discussions with clinicians, people with MS, and representatives of professional and MS societies about the factors we need to consider in the development of an MS falls-prevention intervention for multisite testing that we hope will someday be disseminated widely. Through a combination of small-group work and large-group discussion, participants discussed four of the five RE-AIM elements. A total of 17 recommendations were made to maximize the reach (n = 3), adoption (n = 5), implementation (n = 4), and maintenance (n = 5) of the intervention the Network is developing. These recommendations are likely to be useful for any MS rehabilitation researcher who is developing and testing interventions that he or she hopes will be widely disseminated.
Researchers conducting investigations on prevention of accidental falls among people with multiple sclerosis (MS) span the continuum from basic to applied science. Regardless of whether we are seeking to understand physiological risks for falls1 or the falls-prevention behaviors of people with MS,2 we all are focused on the same ultimate endpoint: building evidence to strengthen practice and improve the lives of people with MS. To achieve this lofty goal, we know that we will have to work very hard to translate our efforts into practice.3,4 Some authors have suggested that it can take well over 15 years for research findings to result in actual practice changes.3 This time lag has remained relatively stable over many years despite greater access to research literature via the Internet, a long-standing emphasis on evidence-based practice, and a growing demand from health-care funders to demonstrate that investing in rehabilitation leads to real results.
The research–practice gap is not unique to MS rehabilitation or care, or even falls prevention more broadly.4,5 It is a pervasive problem across health care and many other sectors of society (eg, education, justice, social services). In response, several authors have developed and tested conceptual frameworks and theoretical models to shrink this gap and increase the likelihood that research uptake will be quicker and more effective.6 One of the more well-established frameworks, particularly in public health, is called RE-AIM.7 RE-AIM stands for Reach, Effectiveness, Adoption, Implementation, and Maintenance.7 Since its initial publication in 1999, the RE-AIM framework has become widely recognized across a range of disciplines as a valuable tool to guide thinking about the development and evaluation of interventions intended for widespread dissemination. Therefore, this framework was selected by the International MS Falls Prevention Research Network (IMSFPRN) to structure initial discussions with a range of stakeholders about the factors we need to consider as we move forward to develop an MS falls-prevention intervention for multisite testing.
The idea for IMSFPRN came about in 2013, when the authors of this article began discussing the need to pool our expertise to accelerate advancement of the evidence about effective ways to prevent falls among people with MS. We recognized that despite our efforts and those of others around the world,8–11 our success in reducing the number, severity, and consequences of falls experienced by people with MS has been limited. We also knew that working together in a coordinated way would advance knowledge more quickly than any individual research team would alone. The inaugural meeting of the IMSFPRN was held in March 2014 in Kingston, Ontario, Canada, with the support of a planning grant from the Canadian Institutes of Health Research. The introduction to the special issue in which this article appears12 provides a brief overview of the aims and structure of the event.
During the meeting, we discussed and made decisions about elements of a research protocol for an international, multisite MS falls-prevention intervention trial. We invited clinicians, people with MS, and representatives of professional and MS societies to participate in our meeting and help us think about what we needed to do to maximize the likelihood of successfully translating an MS falls-prevention intervention into widespread use at some point in the future. We used the RE-AIM framework to structure these discussions. The purpose of this article is to summarize the recommendations stemming from this consultation. These recommendations will be used by the IMSFPRN as we move forward with our efforts.
Brief Overview of the RE-AIM Framework
The RE-AIM framework originated in the field of public health as a guide to improve the process of reporting issues that influence the implementation and generalizability of health promotion and public health interventions.13 Since its original development, RE-AIM has been used to inform program planning as well as implementation, evaluation, and reporting.14 In recent years, it has also been recognized as a valuable tool for promoting knowledge translation.15
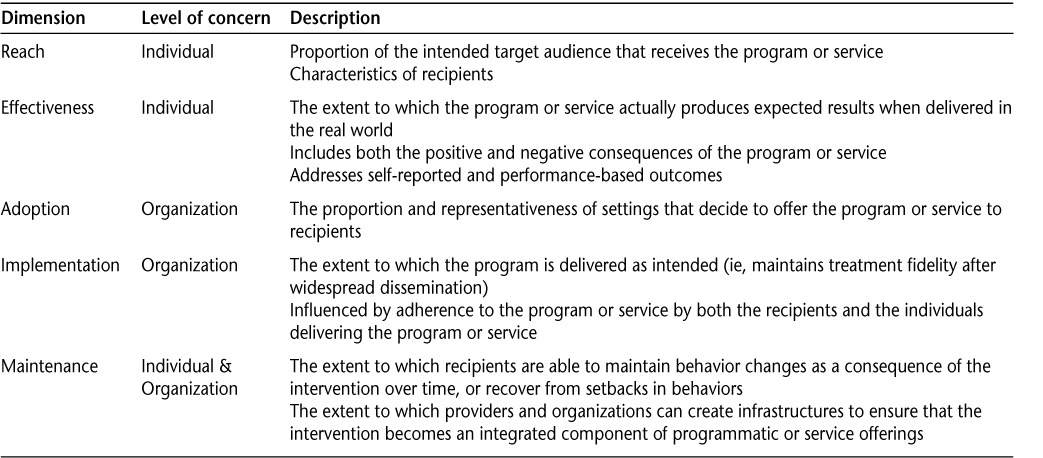
As a planning tool, RE-AIM enables investigators and program developers to carefully and systematically consider a range of factors, beyond efficacy, that could influence the widespread dissemination of a program, service, or policy.16 These factors, typically referred to as dimensions within the framework, are reach, effectiveness, adoption, implementation, and maintenance.7 Across these dimensions, both individual-level and organizational-level factors are considered.7 For example, maintenance of an intervention requires individuals to continue to engage and organizations to create infrastructures to support ongoing delivery. Table 1 provides a summary of the dimensions of the RE-AIM framework. The RE-AIM website (www.re-aim.org) has a wide range of tools and resources to assist investigators, program planners, and policy developers use the framework. The planning tool is particularly helpful (http://www.re-aim.hnfe.vt.edu/resources_and_tools/measures/planningtool.pdf).
Table 1.
Of particular importance to our work, the RE-AIM framework emphasizes that the actual impact of an intervention will depend on the combined effects of the five dimensions, not any one of them alone. In other words, even if our Network designs the very best falls-prevention intervention protocol, and demonstrates its efficacy through carefully controlled and rigorous scientific methods, it can still fail to have an impact if we do not address issues of reach, effectiveness, adoption, implementation, and maintenance. Glasgow15 has effectively illustrated how the dimensions of RE-AIM work together to influence the actual impact of an intervention. We used his work as a guide to generate an MS falls-prevention example for the Network's meeting and this article (Table 2). It is important to note that for the purposes of Glasgow's illustration and our example, the dimensions of RE-AIM are reordered to reflect the order in which processes occur when an intervention is rolled out for widespread distribution.
Table 2.
How the dimensions of RE-AIM could interact to influence the final impact of an efficacious multiple sclerosis falls-prevention intervention that is disseminated
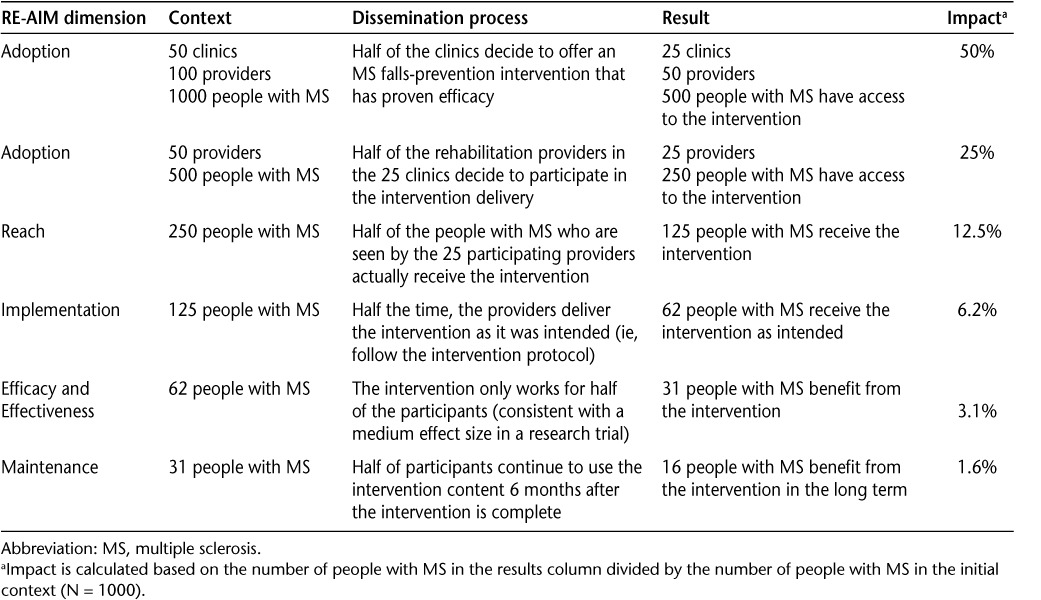
As the rows in Table 2 demonstrate, the impact of our future MS falls-prevention intervention will be dramatically reduced if adoption is only moderate across settings (eg, MS clinics, outpatient facilities, etc.) (Row 1) and if some rehabilitation providers decide against offering it as part of their services (Row 2). Then, if some providers do not consistently offer the intervention to eligible individuals and/or deviate from a proven protocol (Rows 3 and 4), the impact of the intervention will be further eroded. Efficacy, effectiveness, and maintenance may further reduce the potential impact of our future intervention. We know that not all interventions work for all people (Row 5), or work to the extent or level that we hope they might. If our intervention is only partially efficacious, and/or participants do not continue to adhere to intervention processes or recommendations (Row 6), then the potential impact will be further reduced. Even with 50% success within each dimension of RE-AIM, the population-level impact of an efficacious intervention will be shockingly low. This knowledge can be demoralizing for researchers, or it can motivate us to attend to RE-AIM dimensions in our work. The members of the IMSFPRN chose to be motivated and work to positively influence the extent to which our future MS falls-prevention intervention will be one that settings and rehabilitation providers will want and be able to offer, as well as one that people with MS will choose to participate in and will have content they can integrate into their lives over the long term. The remainder of this article summarizes the recommendations that stemmed from our meeting about how to maximize the impact of the MS falls-prevention intervention we have started to develop.
Recommendations to Maximize the Impact of an MS Falls-Prevention Intervention
The inaugural meeting of the IMSFPRN involved the authors of this article in addition to 25 other participants, including other researchers engaged in MS, falls, or related areas; local MS clinic staff (neurologist, physiotherapist, nurse); an occupational therapist and a nurse who provide falls-prevention training to regional health-care providers through the local public health department; people with MS and a family member; representatives from the Canadian Association of Occupational Therapists, Canadian Physiotherapy Association, and the MS Society of Canada; and several local occupational therapists and physiotherapists with an interest in neurorehabilitation or falls prevention. For our purposes, local refers to Kingston, Ontario, and regional refers to the area between Toronto and Ottawa, Ontario. Meeting participants were selected for their diversity in disciplinary perspectives, involvement with people with MS, and knowledge of community falls-prevention programming, and because of the variability in the types of settings in which they worked (eg, clinic, community, organization).
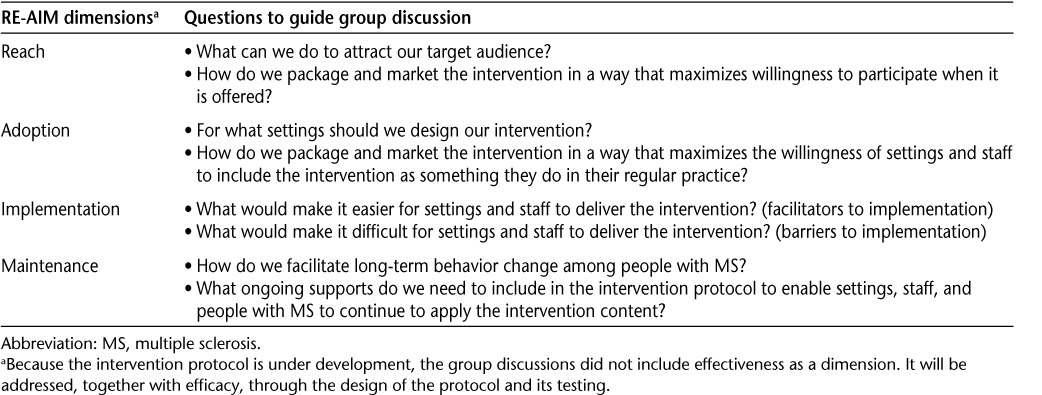
For the purpose of generating recommendations using the RE-AIM framework, participants were divided into small groups for discussion. Each subgroup was assigned a dimension of the RE-AIM framework and given a few key questions to guide their discussion (Table 3). To the extent possible, each subgroup was assigned a dimension that matched with the expertise of its members (eg, people with MS–Reach; clinicians–Adoption). Subgroups reported back to the main group at the end of this period. Effectiveness was not assigned to one of the groups, as the discussion of this dimension was the focus of a subsequent meeting with the authors of this article on a following day.
Table 3.
Questions posed to stakeholders to help the Network consider RE-AIM dimensions during the development of a multiple sclerosis falls-prevention intervention
Recommendations Generated
Based on the small-group discussions and large-group reflections, the following recommendations were made by the meeting participants to the Network members, and other MS falls-prevention researchers, to maximize the impact of their interventions once they are ready for widespread dissemination:
- To maximize the REACH to the target audience of people with MS:
- Use social media, newspapers, and other forms of marketing to let people with MS know about the intervention and how it can help them in their everyday lives. Use testimonials of people with MS who have completed the intervention to help promote it and show its relevance to outcomes that matter. Health-care providers are an important referral source, yet meeting participants recommended that other sources of referral needed to be included to access the target audience.
- Develop an intervention that will have a social component providing the opportunity for people with MS to engage with peers. Offering opportunities to engage with peers will extend the reach of the intervention.
- Find another name for “falls prevention” so the intervention is more appealing to people with MS.
- To maximize the ADOPTION by settings, policy makers, and providers:
- Be sure to engage community and home-based agencies, support groups, and other similar entities in intervention delivery, as it will be difficult for many primary-care or specialty clinics to commit to offering an MS falls-prevention intervention on a regular basis.
- Consider developing a blended intervention, for example, one that combines use of technology at home with group-based discussions and activities in a facility/clinic/agency.
- Make sure that there is consistent and ongoing training and support available to the providers who will deliver the intervention so that they feel confident in their abilities to implement it.
- Create champions for the intervention who can engage and support providers and settings throughout adoption, implementation, and maintenance. Champions must be able to facilitate and manage practice change and help providers take ownership of the intervention in their own setting. Consider policy makers as potential champions.
- Make sure that the intervention is feasible to deliver across settings (eg, common equipment and environmental demands, low cost, billable).
- To maximize the IMPLEMENTATION by providers:
- Clearly define the target audience for the intervention. Do not be ambiguous about whom the intervention targets or how to identify and select them. Avoid the term “community-dwelling,” since it does not translate well cross-culturally.
- Create a manualized intervention to support program fidelity. Through the manual, describe intervention content (eg, topics) and processes (eg, activities, sequencing, duration, theoretical justification). Provide a rationale for each component of the intervention (ie, why it should work) within the manual to positively influence program fidelity.
- Ensure that the duration of the intervention fits with the operations at the setting and does not require additional financial and space resources to deliver as intended.
- Provide resources for intervention participants that follow accepted health literacy guidelines. Avoid using jargon and ensure that the intervention is sensitive to different educational levels and ways of accessing materials (eg, electronic and paper).
- Make sure that the intervention uses a team approach so that its delivery can be shared by different professionals. Do not apply discipline-specific restrictions about who can or cannot deliver the intervention. Carefully consider issues of funding and how to get buy-in from different professionals on the team.
- To maximize the MAINTENANCE among participants and providers:
- Be attentive to branding and promotion of the intervention. Provide something that providers and participants want to be associated with.
- Use behavior change theory to guide intervention development and delivery, and provider training, with particular attention to maintenance.
- Build in ongoing contact, supports, or small reminders (eg, via text, phone calls) to encourage long-term maintenance. Consider inclusion of ongoing coaching and consultation through webinars or social media to keep people motivated to use the intervention materials. Engage caregivers in the intervention to support long-term maintenance.
- Consider having a certification process for providers who can deliver the intervention; create mechanisms where providers feel like a part of the IMSFPRN. It is important to make sure that there is an infrastructure and a long-term connection with participants.
- Document the cost-effectiveness and cost-benefit of the intervention so that policy makers, organizations, and governments can see tangible results and continue providing funding.
Conclusion
As members of the IMSFPRN, we are committed to developing and testing an MS falls-prevention intervention that builds on existing knowledge, is feasible and suitable for widespread dissemination, and is viewed as valuable and practical by people with MS, rehabilitation providers, organizational decision makers, and funders. Based on the experiences of others, we believe that using the RE-AIM framework early in our work will help us develop an intervention and a protocol that will maximize our ability to translate our future research into practice.17–20 Knowledge translation is complex3,4 but possible if we proceed systematically and engage key stakeholders in our work. Researchers who conduct falls-prevention research with older adults have used the RE-AIM framework to identify ways to improve reach, adoption, effectiveness, implementation, and maintenance of their programs.18–20 MS falls-prevention researchers now must do the same so we can maximize the potential for any efficacious interventions we identify to be used in practice and have a positive impact on the lives of people with MS.
PracticePoints.
Using the RE-AIM framework provides a structured way of planning for maximum reach, effectiveness, adoption, implementation, and maintenance of MS falls-prevention interventions.
Engaging a range of stakeholders in the examination of each component of the RE-AIM framework raises issues that researchers may not consider on their own.
The application of RE-AIM during intervention development may help reduce the research–practice gap for effective MS falls-prevention interventions.
Footnotes
Financial Disclosures: The authors have no conflicts of interest to disclose. Dr. Finlayson and Dr. Coote are members of the editorial board of the IJMSC.
Funding/Support: This work was supported, in part, by a Canadian Institutes of Health Research Planning Grant (Funding Reference Number 129594).
References
- 1.Sosnoff JJ, Finlayson M, McAuley E, Morrison S, Motl RW. Home-based exercise program and fall-risk reduction in older adults with multiple sclerosis: phase 1 randomized controlled trial. Clin Rehabil. 2014;28:254–263. doi: 10.1177/0269215513501092. [DOI] [PubMed] [Google Scholar]
- 2.Cameron MH, Asano M, Bourdette D, Finlayson ML. People with multiple sclerosis use many fall prevention strategies but still fall frequently. Arch Phys Med Rehabil. 2013;94:1562–1566. doi: 10.1016/j.apmr.2013.01.021. [DOI] [PubMed] [Google Scholar]
- 3.Green LW, Ottson JM, Garcia C, Hiatt RA. Diffusion theory and knowledge dissemination, utilization, and integration in public health. Ann Rev Public Health. 2009;30:151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- 4.Tetroe JM, Graham ID, Scott V. What does it mean to transform knowledge into action in falls prevention research? Perspectives from the Canadian Institutes of Health Research. J Safety Res. 2011;42:423–426. doi: 10.1016/j.jsr.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 5.Fixsen D, Scott V, Blase K, Naoom S, Wagar L. When evidence is not enough: the challenge of implementing fall prevention strategies. J Safety Res. 2011;42:419–422. doi: 10.1016/j.jsr.2011.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Estabrooks CA, Thompson DS, Lovely JJ, Hofmeyer A. A guide to knowledge translation theory. J Contin Educ Health Prof. 2006;26:25–36. doi: 10.1002/chp.48. [DOI] [PubMed] [Google Scholar]
- 7.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–1327. doi: 10.2105/ajph.89.9.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gunn HJ, Newell P, Haas B, Marsden JF, Freeman JA. Identification of risk factors for falls in multiple sclerosis: a systematic review and meta-analysis. Phys Ther. 2013;93:504–513. doi: 10.2522/ptj.20120231. [DOI] [PubMed] [Google Scholar]
- 9.Nilsagård Y, Lundholm C, Denison E, Gunnarsson LG. Predicting accidental falls in people with multiple sclerosis—a longitudinal study. Clin Rehabil. 2009;23:259–269. doi: 10.1177/0269215508095087. [DOI] [PubMed] [Google Scholar]
- 10.Kasser SL, Jacobs JV, Foley JT, Cardinal BJ, Maddalozzo GF. A prospective evaluation of balance, gait, and strength to predict falling in women with multiple sclerosis. Arch Phys Med Rehabil. 2011;92:1840–1846. doi: 10.1016/j.apmr.2011.06.004. [DOI] [PubMed] [Google Scholar]
- 11.Finlayson ML, Peterson EW. Falls, aging, and disability. Phys Med Rehabil Clin N Am. 2010;21:357–373. doi: 10.1016/j.pmr.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 12.Sosnoff JJ, Finlayson ML. International MS Falls Prevention Research Network: report from the front lines. Int J MS Care. 2014;16:161. doi: 10.7224/1537-2073.2014-061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health. 2013;103:e38–e46. doi: 10.2105/AJPH.2013.301299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kessler RS, Purcell EP, Glasgow RE, Klesges LM, Benkeser RM, Peek CJ. What does it mean to employ the RE-AIM model? Evaluation Health Prof. 2013;36:44–66. doi: 10.1177/0163278712446066. [DOI] [PubMed] [Google Scholar]
- 15.Glasgow RE. Knowledge translation measurement . . . concepts, strategies, and tools: reach, effectiveness, adoption, implementation, and maintenance. SEDL's Center on Knowledge Translation Disability and Rehabilitation Research [serial online] 2013. http://www.ktdrr.org/conference2013/expo/docs/Glasgow_oct.30.13.pdf.
- 16.Glasgow RE, McKay HG, Piette JD, Reynolds KD. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Counsel. 2001;44:119–127. doi: 10.1016/s0738-3991(00)00186-5. [DOI] [PubMed] [Google Scholar]
- 17.Bruun DM, Bjerre E, Krustrup P et al. Community-based recreational football: a novel approach to promote physical activity and quality of life in prostate cancer survivors. Int J Environment Res Public Health. 2014;11:5567–5585. doi: 10.3390/ijerph110605567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li F, Harmer P, Stock R et al. Implementing an evidence-based fall prevention program in an outpatient clinical setting. J Am Geriatr Soc. 2013;61:2142–2149. doi: 10.1111/jgs.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shubert TE, Altpeter M, Busby-Whitehead J. Using the RE-AIM framework to translate a research-based falls prevention intervention into a community-based program: lessons learned. J Safety Res. 2011;42:509–516. doi: 10.1016/j.jsr.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 20.Goodwin V, Jones-Hughes T, Thompson-Coon J, Boddy K, Stein K. Implementing the evidence for preventing falls among community-dwelling older people: a systematic review. J Safety Res. 2011;42:443–451. doi: 10.1016/j.jsr.2011.07.008. [DOI] [PubMed] [Google Scholar]


