Abstract
Background
The institutions with high volume of pancreatic surgery report morbidity rate from 30% to 50% and mortality less than 5% after pancreaticoduodenectomy (PD). At the present, the most significant cause of morbidity and mortality is pancreatic fistula (PF).
Aim
The purpose of the study is to identify the most important clinical factors which may predict PF development and eventually suggest alternative approaches to the pancreatic stump management.
Patients and methods
A retrospective analysis of a clinical data base of a tertiary care Hospital was performed. From 2002 to 2012 a single Surgeon prospectively performed 150 pancreaticoduodenectomies for cancer. Four different techniques were used: end to end pancreaticojejunostomy, end to side pancreaticojejunostomy, pancreatic duct occlusion and duct to mucosa anastomosis. The intraoperative gland texture was classified as soft, firm and hard. The duct size was preoperatively (CT scan) and intraoperatively recorded and classified: < 3 mm small, 3–6 mm medium, > 6 mm large. The histopathological characteristic of the gland fibrosis was graduate as low 1, moderate 2, high 3.
Conclusion
Relationships between pre and intraoperative duct size measurement, pancreatic texture and pancreatic fibrosis grading were highly significant. Small duct and soft pancreas with low grade fibrosis are the most important risk factors for pancreatic fistula development.
The proper selection of pancreatic stump management or the decision to refer the high risk patients to high volume Center can be suggested by the elevated correspondence of pre and intraoperative duct diameter with the related pancreatic fibrosis grade and gland consistency. Preoperative assessment of the pancreatic duct makes possible to predict the risk of pancreatic fistula.
Keywords: Pancreas, Surgery, Fistula, Pancreatoduodenectomy, Cancer
Introduction
The current standard treatment for resectable pancreatic head or periampullary cancer is surgical resection followed by adjuvant chemotherapy. However, only a small percentage of Patients is able to undergo potential curative surgery. But even in resectable Patients, the 5 years survival rate is 5–40%. For Patients at advanced, surgical unresectable stages, median survival ranges from 6 to 12 months. Pancreatic resection is technically demanding procedure. Post operative mortality after pancreaticoduodenectomy is currently less than 5% in experienced high volume Centers. However, postoperative morbidity rate remains high approaching 30–50% (1, 2). At present pancreatic leak is the most significant complication from which 40% of Patients death are the result of septic or of hemorrhagic complications. Rates up to 20% are reported from Centers specialized in pancreatic surgery without reduction in the past decade (3, 4). However, the definition of pancreatic fistula is not standardized and universally accepted. Differences in the incidence of pancreatic fistulae from 10% to 29% are reported depending on the definition of this complication (5). Pancreatic juice can originate either from the main pancreatic duct or from the pancreatic cut surface. While pancreatic enteric anastomotic leaks with concomitant enzyme activation are life threatening complications leading to sepsis and massive hemorrhage, stump leaks are usually not clinically important (10). The International Study Group on pancreatic fistula (ISGPF) (6) recently defined the pancreatic fistula as any measurable volume of fluid on or after post operative day 3, with amylase content greater than 3 times the serum amylase activity. ISGPF established that the most appropriate definition and grading of pancreatic fistula (grade A, B and C) should be based on the clinical impact. On the Patient’s hospital course and eventual outcome, Pratt (7) concluded that with an increasing fistula grading there is a negative clinical and economic impact on Patients. Recently, Strasberg (8) re-defined true pancreatic fistula as pancreatic anastomotic failure (PAF) and pancreatic occlusion failure (POF) as pancreatic fistula non associated with disruption of the pancreaticojejunal anastomosis. Asymptomatic fistulae with drain amylase and no change in the Patients clinical course should not always be considered as the result of anastomotic failure, but pancreatic stump leak with an expected benign clinical course (9). The dramatic consequences of a technical reconstructive failure suggested a number of methods for reducing the incidence of pancreatic fistula, involving site of reconstruction, anastomotic techniques, sutures, biologic adhesives and transanastomotic stents. Many studies have attempted to examine prognostic risk factors for anastomotic leaks after duodenopancreatectomy. However, until now all different pancreatojejunal reconstructions failed to give clear evidence of specific superiority. In an attempt to study the management of pancreatic remnant, we prospectively used 4 different surgical techniques in the treatment of the pancreatic stump. In this study we report the results of 150 consecutive duodenopancreatectomies performed in a single Center surgical population by one Surgeon. The purpose of our study is to investigate the different treatment of the pancreatic stump, with the aim of producing a clinically applicable system for the appropriate selection of pancreaticoduodenectomy (PD) operations for cancer.
Patients and methods
All Patients admitted to “San Camillo-Forlanini” Hospital of Rome during the last decades were identified in the Department of surgery data base. From January 2002 to January 2012, 150 consecutive Patients underwent a standard (Whipple-Child) or pylorus preserving radical pancreaticoduodenectomy (Traverso - Longmire) for malignant pathologies of the pancreatic head or the periampullary region. Only Patients operated by the same Surgeon were recorded. Selection criteria for pancreaticoduodenectomy were as follows:
periampullary or pancreatic cancer;
preoperative imaging negative for disseminated disease;
suitability for major operations.
Serum chemistries and disease specific molecular markers (CEA, CA 19-9, CA125) were obtained in the preoperative clinic. Imaging studies employed abdominal ultrasonography, total body computed tomography (CT), abdominal magnetic resonance (RMN) and endoscopic retrograde cholangiopancreatography (ERCP) with brushing for cytology, and endoscopic transduodenal ultrasonography with pancreatic fine needle biopsy. An endoscopic stent or nosebiliary drainage were positioned whenever required. An intended curative resection was performed up to stage IV (Japan Society Classification of Pancreatic Cancer)The final assessment of resectability was made at operation considering: retroperitoneal extension of the tumors, liver metastases, involvement of superior mesenteric artery or superior mesenteric vein and portal vein. An intraoperative pathological examination was performed on the lymph nodes of the inferior vena cava and aorta, and on the lymph nodes of the 5th and 6th station according to the Japanese classification, in Patients undergoing pylorus preserving surgery. An intraoperative pathological examination of the common hepatic duct and the pancreatic stump was made to assess the radicality of the resection. Three drains were placed at the end of surgery: two were placed near the transected pancreas, while another drain was placed near the hepaticojejunostomy. All specimens were evaluated by the staff Pathologist. Histopathologic diagnosis, tumor size, tumor differentiation, lymph node status and negative or positive surgical margins were reported. A secondary review by a dedicated pancreatic Pathologist was carried out in 38 Patients submitted to duct to mucosa anastomosis, in order to determine the degree of tissue fibrosis (Grade 1,2 and 3) in the specimens of the pancreatic stump. The senior Pathologist evaluated only the microscopic slides and was blinded towards all histopathologic, operative and clinical data of the Patients.
Statistical analysis
The statistical analysis was performed using the R software with the gmodels library.
A Chi-square test using the Monte-Carlo simulation was used to evaluate the factors’ dependency in the datasets. The Monte-Carlo simulation, that produce a reference distribution based on random generated samples of the same size as the tested sample, was used to handle the datasets with small size.
Statistical significance was set at p value < 0.05.
All deaths within 30 days of surgery were considered surgical mortality.
Patient demographics
One hundred and fifty Patients underwent pancreaticoduodenectomy in the period of study. There were 89 men and 61 women. The median age was 63 years (range 33–86). Forty-nine Patients were aged 70 or older.
Primary lesions
Primary lesions were pancreatic cancers (n = 110, 73.4%), ampullary cancers (n=19, 12.6%), bile duct cancers (n=14, 9.4%) and duodenal cancers (n=7, 4.6%).
Surgical resections
A total of 150 pancreaticoduodenectomies were performed. One hundred and three Patients (69.2%) underwent pylorus preserving procedure while forty seven Patients (30.8%) underwent conventional pancreaticoduodenectomy. Changes in pattern of practice of pancreatic stump management are shown in Table 1.
Table 1.
MANAGEMENT OF PANCREATIC STUMP IN 150 PTS. SUBMITTED TO PD FOR CANCER.
| Operations | n° | Years | Groups |
|---|---|---|---|
| End-to-end PJ anastomosis | 32 | 2002–2004 | A |
| End-to-side PJ anastomosis | 44 | 2005–2007 | B |
| Duct occlusion | 33 | 2008–2010 | C |
| Duct-to-mucosa anastomosis | 41 | 2011–2012 | D |
|
| |||
| All | 150 | ||
PJ: pancreatic jejunostomy.
Surgical procedure
The standard radical procedure included:
- en-bloc cholecistectomy and section of hepatic duct with extemporaneous histological examination;
- section of the pancreas on the left margin of the mesenteric-portal vein axis and pancreatic stump frozen section examination;
- preservation of the pylorus and lymphatic frozen examination (Traverso-Longmire procedure) or gastric resection (Whipple-Child procedure);
- exposure of the ligament of Treitz, section of the first jejunal vessels and section of the first jejunal loop.
Eventually partial or total mesenteric portal vein and hepatic artery resection justifying R0 resection with dissection margin free from cancer cells, in borderline resectable disease is indicated when:
encasement of a short segment of the hepatic artery responding to neoadjuvant therapy;
venous infiltration less than 180° in the circumference, in the absence of thrombosis;
venous involvement > 180° without thrombosis responding to neoadjuvant chemotherapy.
The approach to the borderline resectable disease is to use preoperative systemic chemotherapy followed by surgery and IORT to maximize the potential R0 resections. En-bloc radical lymphadenectomy with clearance of common and proper hepatic artery, celiac artery, hepatoduodenal ligament, posterior pancreaticoduodenal lymph nodes, lymph nodes on the right and anterior margin of the SMA from its origin to the inferior pancreaticoduodenal artery. Removal of preaortic and precaval lymph nodes from the celiac artery to the inferior mesenteric artery. All radical procedures do not include removal of Gerota fascia and circumferential skeletonization of the SMA, usually associated with diarrhea and higher morbidity without survival advantage. Pancreatic, biliary and duodenal or gastric anastomoses are performed in sequence on the same jejunal limb. Based on the current evidence suggesting that pancreaticojejunostomy and pancreaticogastrostomy are equivalent in term of postoperative outcome, pancreaticogastrostomy was never performed (10–12). End to side hepatico jejunostomy is performed 20 cm downstream of the pancreatic anastomosis with absorbable 4-0 sutures. End to side duodenal or gastric jejunal anastomosis is performed at 30 cm from the biliary anastomosis with 4-0 absorbable sutures.
Pancreatic jejunostomy (end-to-side anastomosis)
After a sharp cut vertical section of the neck, the pancreatic stump is exposed for 2–3 cm and two 3-0 stiches are passed through the marginal side of the gland within 1 cm of the section line. After a section of the pancreatic stump for frozen examination, hemostasis with 5-0 absorbable sutures is performed. A catheter can be inserted in to the pancreatic duct to record the duct’s diameter and to overturn the stump.
Only suturing materials with the greatest tensile strength are used for the pancreaticojejunostomy: poly-dioxanone (PDS) or polypropylene (Prolene). In fact, a pancreatic fistula can occur more often when rapid absorbable threads are used and can develop once the sutures have been digested by pancreatic fluids. The outer layer of the anastomosis is started stiching with interrupted suture the posterior aspect of the pancreatic parenchima and the jejunal seromuscolar layer, leaving a pancreatic section margin free of 0.5–1 cm. The jejunum is opened 1 cm from the outer suture line and the internal layer of suturing is performed including the pancreatic section margin and the full jejunal wall. The outer layer is completed with interrupted sutures.
Pancreatic jejunostomy (end-to-end anastomosis)
The pancreatic stump should be freed for several centimeters in preparation for telescoping the end of the jejunum over it. A posterior outer layer of interrupted 4-0 suture is placed sewing the posterior pancreatic parenchima to the jejunal seromuscolar wall. The cut surface of the jejunum is sewed to the inner margin of the pancreas. An additional anterior layer of interrupted suture is placed to pull the jejunal wall up over the pancreatic parenchima for approximately 1–2 cm.
Occlusion of the duct of Wirsung
After identification of the main pancreatic duct, a 4-0 purse string suture is made on the pancreatic duct which is cannulated with a proper catheter. The pancreatic stump is then closed with interrupted sutures to prevent secretion leaks from minor ducts. Two or three ml of the occluding substance are slowly injected and the catheter is gradually retracted. Purse string suture is then tied. Many chemical substances have been investigated in the past: Ethibloc® (Ethicon, Norderstedt, Germany), Neoprene glue (Du Pont de Nemours Italiana, Cologno Monzese, Italy), Fibrin glue (Tissucol® Baxter, Deerfield, Il, USA) (13–15). Lower morbidity was recorded with the application of mechanical stapler during the pancreatic transaction or with identification and direct ligation of main pancreatic duct (16, 17). We investigated the obliteration of the duct with Cianoacrilate (Glubran 2® GEM, Viareggio, Italia).
Duct-to mucosa pancreatic jejunostomy
When the duct of Wirsung is dilated more than 3 mm and the parenchyma is firm or hard, the duct to mucosa anastomosis is easy and safe. When dealing with a small duct, less than 3 mm, and with on soft tissue, the procedure is more complex, but, with the assistance of magnifying glasses, is still possible for an experienced Surgeon. After a record of the duct diameter, an appropriate stent is placed inside the duct to allow a safer anastomosis. The stent can be abandoned. However, leaving the stent inside the pancreatic anastomosis does not have a protective effect in terms of pancreatic fistula risk and morbidity (18, 19). The posterior suture layer is performed as described for the end - to side anastomosis. A small jejunal incision is made 0.5 cm from the outer posterior suture. In the case of a small duct (< 3 mm) five to six 5-0 or 6-0 stiches are passed from inside the pancreatic duct to the jejunal cut margin and tied. In the case of a bigger duct (> 3 mm) eight 5-0 stiches are used. The duct to mucosa pancreatic jejunostomy is completed by oversewing the anterior pancreatic margin and the jejunal limb. Unsewn small secondary ducts not included in the opening of the jejunal limb can determine a low risk, pure pancreatic leak, without clinical impact.
Main risk factors for pancreatic fistula
In 38 Patients submitted to duct to mucosa anastomosis (Group D) (Table 1), the diameter of the Wirsung duct was radiologically (CT scan) measured during the preoperative studies. In the same Patients duct diameter was carefully exposed and measured during the operation with insertion of a suitable gauge pancreatic catheter. Three groups of duct size were recorded: ≤3 mm small, 3–6 mm medium, > 6 mm large. The pancreas texture of all Patients was examined by the Surgeon and classified in three groups: soft, firm and hard. The histopathologic characteristic of gland fibrosis was graduated (grade 1 = low, grade 2 = moderate, grade 3 = high). Relationship between gland texture and pancreatic fibrosis was assessed. Variables, including radiological and in-traoperative duct size measure, pancreatic fibrosis and pancreatic texture were correlated with the risk of developing pancreatic fistula.
Perioperative management and assessment
All Patients were administered preoperative antibiotic prophylaxis and antithrombotic prophylaxis. Intravenous hyperalimentation and protease inhibitors were routinely used in all Patients for 7 days. Blood tests were obtained on 1, 3, 5 and 7 days after resection. All Patients underwent US or CT scan examinations when necessary to assess the presence of abdominal fluid collections. Infectious complications were treated with selected antibiotics according to blood culture and antibiograms. Hepaticojejunostomy leak was diagnosed when a drainage of > 50 ml of biliary fluid was recorded. The level of fluid amylase from all drains placed near the pancreatic and biliary anastomoses was determined every other day until the removal of the drains. Distinctive analysis between pancreatic enteric anastomotic leak and extravasation of non activated pancreatic juice from the side branch ducts of the pancreatic stump was performed.
Results
From January 2002 to January 2012, of the 150 Patients undergoing pancreatoduodenectomy for pancreatic and periampullary cancer, there were 89 men and 61 women (median age 63 years – range 33–86 years). All operations were performed by the same Surgeon who was experienced in pancreatic surgery. The mean time of operation was 360 ± 35.5 minutes. Intraoperative blood transfusion was requested during 65 procedures and the mean blood volume transfused was 655 ± 325 ml. In an attempt to obviate a pancreaticoenteric leakage, four different procedures were prospectively performed: group A, 32 end-to-end pancreaticojejunostomies (E-EPJ) (2002–2004); group B, 44 end-to-side pancreaticojejunostomies (E-SPJ) (2005–2007); group C, 33 pancreatic duct occlusion (PDO) (2008–2010); group D, 41 duct-to-mucosa anastomosis (DMA) (2011–2012) (Table 1). The intensive care stay was 3.3 ± 1.5 days. Total hospital stay was 15.5 ± 6.2 days. In Table 2 are shown the postoperative outcomes. The overall morbidity was 26.6% (40 Pts). The most frequent abdominal complication was pancreatic fistula which was observed in 25 Patients (16.6%): 5/32 (15.6%) in Patients who underwent E-EPJ, group A; 5/44 (11.3%) in Patients submitted to E-SPJ, group B; 15/33 (45.4%) Patients with PDO, group C; 0/41 (0%) in Patients who underwent DMA, group D. In the total of 41 Patients who were reconstructed with DMA, none developed abdominal or cardiopulmonary complications. Meanwhile almost an half of Patients with duct occlusion experienced a pancreatic fistula. Considering the ISGPE Grading, the 25 pancreatic fistulae were classified as follow: 16 (64%) grade A (6 PJ, 10 PDO); 6 (24%) grade B (3 PJ, 3 PDO); 3 (12%) grade C (2 PJ, 1 PDO). The incidence of PF with clinically significant impact (grade B-C) was therefore present in 9/25 (36%) Patients, 5 after PJ and 4 after PDO. In the 41 Patients with DMA, the incidence of pancreatic fistula was 0, independently from pancreatic texture or duct size. Abdominal collections were recorded in 8 (5.3%) Patients and hemorrhage in 4 (2.6%) Patients. Overall postoperative mortality was 6 % (9/150). In the last 100 consecutives cases the mortality was 1%. Reoperations or radiological drainages were performed in 10 Patients for abdominal abscess, hemorrhage and pancreaticoenteric anastomosis’ dehiscence. The consistency of the remnant pancreatic stump was strongly correlated with subsequent postoperative fistula rate in groups A–B (76 Patients, 50.6%) submitted to PJ anastomosis. In the non pancreatic fistula Patients of groups A and B, 16 (19.7%) pancreas were classified as soft, 29 (39.4%) Patients as firm and 21 (27.6%) as hard. In the pancreatic fistula group, 9 (11.8%) pancreas were classified as soft and 1 (1.3%) as firm. The relationship of intraoperative gland texture with pancreatic fistula development showed that firm and hard pancreatic consistency was significantly predictive of positive outcome. The pancreatic consistency and the fistula development were significantly correlated (p = 0,00016) (Table 3) (Fig. 1). The imaging preoperative assessment of the duct size of 38 Patients of group D revealed an elevated correspondence with the intraoperative measure. Applying the chi-square test and using the Montecarlo Simulation, the radiological and the intraoperative duct size were independent and not correlated (p = 0.76). However the two factors compared had almost the same frequency for all diameters reported (Table 4) (Fig. 2). The consistency of pancreas soft, firm and hard was highly correlated to the fibrosis grading 1, 2 and 3 (p = 9.9e-07). Most of pancreas with fibrosis grade 1 were soft. The majority of pancreas with fibrosis grade 2 were firm. Most of hard pancreas had a fibrosis grade 3 (Table 5) (Fig. 3). An analysis was performed in the 38 Patients with duct to mucosa anastomoses, correlating two major predictive variables: perioperative duct diameter measure and pancreatic fibrosis grading. Grade 1, grade 2, grade 3. The pancreatic fibrosis grade was significantly associated to the duct size (p = 9.9e-07). Most of the pancreas with fibrosis grade 1 had < 3 mm duct size. Fibrosis grade 2 was associated to 3–6 mm duct size. The majority of pancreas with fibrosis grade 3 had a duct size > 6 mm (Table 6) (Fig. 4). The correspondence between the preoperative duct diameter assessment and the fibrosis grade can suggest, in advance, the best surgical procedure: conventional anastomosis, separate “Roux en Y” limbs, duct occlusion, pancreaticogastrostomy or Patients transfer to high volume Center. In fact, the risk of developing pancreatic fistulas is very low when the pancreatic texture is firm or hard, the fibrosis grading is 2 or 3, and the diameter of the pancreatic duct is > 3 mm. Pancreatic duct size < 3 mm, consistency of pancreas soft and pancreatic fibrosis grade 1 are predictors of postoperative pancreatic fistula.
Table 2.
POSTOPERATIVE COURSE, COMPLICATIONS AND OUTCOME IN 150 PTS. SUBMITTED TO PD FOR CANCER.
| Main abdominal complications | A (32) E-EPJ | B (44) E-SPJ | C (33) PDO | D (41) DMA | Overall morbidity 40 (26,6 %) |
|---|---|---|---|---|---|
| Pancreatic fistula | 5 (15.6%) | 5 (11.3%) | 15( 45.4%) | 0 | 25 (16,6%) |
| Grade A | 4 | 2 | 10 | 0 | 16 (64%) |
| Grade B | 2 | 1 | 3 | 0 | 6 (24%) |
| Grade C | 1 | 1 | 1 | 0 | 3 (12%) |
| Biliary fistula | 0 | 0 | 0 | 0 | – |
| Abdominal collections | 3 | 2 | 3 | 0 | 8 (5,3%) |
| Hemorrage | 2 | 1 | 1 | 0 | 4 (2,6%) |
| Acute pancreatitis | 0 | 1 | 0 | 0 | 1 (0,7%) |
| Bowel obstruction | 1 | 1 | 0 | 0 | 2 (1,3%) |
| Post-op mortality | 5 | 3 | 1 | 0 | 9 (6 %) * |
Post-op mortality in the last 100 consecutive cases: 1%.
Table 3.
RELATIONSHIP OF INTRAOPERATIVE GLAND TEXTURE WITH THE PANCREATIC FISTULA DEVELOPMENT IN 76 PTS SUBMITTED TO PANCREATICOJEJU-NOSTOMY (GROUPS A–B).
| Consistency of pancreas | # cases | Pancreatic fistula n=10 | No pancreatic fistula n=66 |
|---|---|---|---|
| Soft | 25 | 9 (11,8%) | 16 (19,7%) |
| Firm | 30 | 1 (1,3%) | 29 (39,4%) |
| Hard | 21 | 0 | 21 (27,6%) |
p-value = 0.00016.
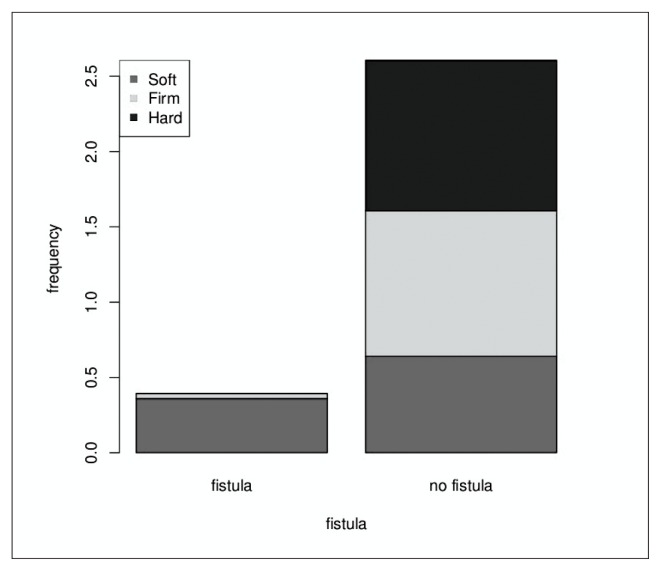
Fig. 1.
The two factors compared (the pancreas consistency and the fistula presence or absence) are significantly correlated (p-value = 0.00016).
The majority of cases were the fistula is reported corresponds to a soft pancreas consistency.
Table 4.
COMPARISON BETWEEN RADIOLOGICAL AND INTRAOPERATIVE DUCT SIZE MEASURE IN 38 PTS HAVING DUCT-TO-MUCOSA PANCREATICOJEJUNO-STOMY (GROUP D).
| Measurement | Duct size | ||
|---|---|---|---|
|
| |||
| < 3 mm small | 3–6 mm medium | > 6 mm large | |
| Radiological (CT scan) | 3 | 24 | 11 |
| Intraoperative | 2 | 22 | 14 |
The two factors compared are independent or not correlated.
p value = 0.76.
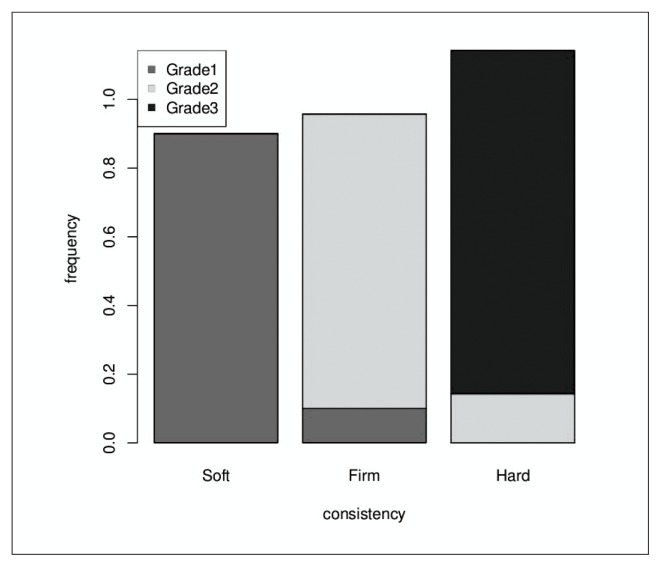
Fig. 2.
The radiological and the intraoperative measurement have almost the same frequency for all the diameters reported (< 3 mm, 3–6 mm, > 6 mm).
Table 5.
COMPARISON BETWEEN PANCREATIC FIBROSIS AND GLAND TEXTURE IN 38 PTS HAVING DUCT-TO-MUCOSA PANCREATICOJEJUNOSTOMY (GROUP D).
| # Patients | Pancreatic fibrosis grade | Gland texture | ||
|---|---|---|---|---|
|
| ||||
| Soft | Firm | Hard | ||
| 10 | 1 | 9 | 1 | 0 |
| 14 | 2 | 0 | 12 | 2 |
| 14 | 3 | 0 | 0 | 14 |
p-value= 9.9e-07.
Fig. 3.
The two factors compared (the gland texture and the pancreatic fibrosis grade) are significantly correlated (p-value = 9.9e-07). Most of the cases with fibrosis grade 1 have a soft pancreas. The majority of cases with fibrosis grade 2 have a firm pancreas. In most cases a hard pancreas consistency corresponds to pancreatic fibrosis grade = 3.
Table 6.
RELATIONSHIP OF PANCREATIC FIBROSIS AND INTRAOPERATIVE DUCT SIZE MEASURE IN 38 PTS HAVING DUCT-TO-MUCOSA PANCREATICOJEJUNO-STOMY (GROUP D).
| # Patients | Pancreatic fibrosis grade | Pancreatic duct size | ||
|---|---|---|---|---|
|
| ||||
| < 3 mm | 3–6 mm | > 6 mm | ||
| 10 | 1 | 7 | 3 | 0 |
| 14 | 2 | 0 | 10 | 4 |
| 14 | 3 | 0 | 4 | 10 |
p-value= 9.9e-07.
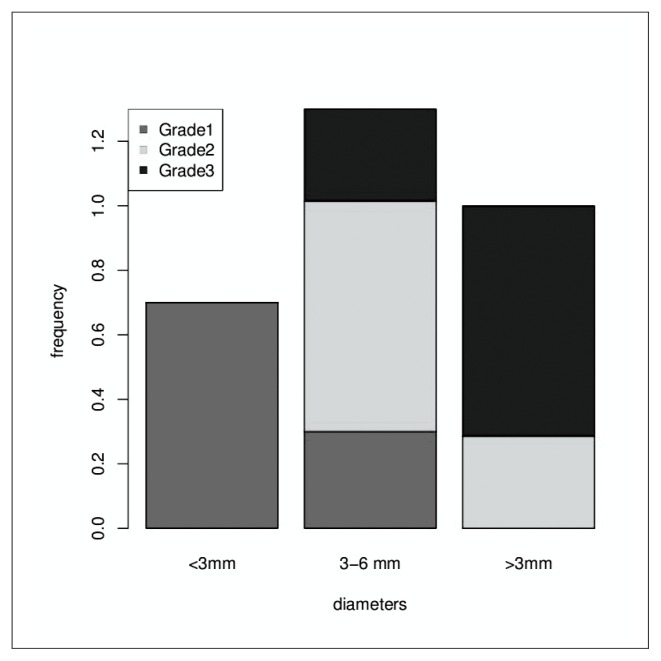
Fig. 4.
The two factors compared (the duct size and the pancreatic fibrosis grade) are significantly associated (p-value = 9.9e-07). Most of the cases with fibrosis grade = 1 have a < 3mm duct size. On the contrary, the majority of cases with fibrosis grade = 2 have a duct size 3–6 mm and cases with fibrosis grade = 3 have a duct size > 6 mm.
Discussion and conclusion
Bassi et al. (5, 6) reported 26 definitions of pancreatic fistula published between 1991 and 2000. Each definition was based on daily pancreatic fluid output, amylase concentration and the postoperative time of fistula development. A special study group of expert pancreatic Surgeons defined the pancreatic anastomotic fistula as persistent drainage of more than 30 or 50 ml/day of an amylase rich fluid after postoperative day 3, with amylase content greater than 3 times the serum amylase activity. Three grades of fistula severity are classified according to the ISGPF clinical criteria (6):
- GRADE A: transient, asymptomatic fistula with elevated drain amylase levels without clinical relevance;
- GRADE B: symptomatic fistula that require diagnostic evaluation and therapeutic management;
- GRADE C: severe fistula requiring aggressive diagnostic management and therapeutic interventions.
Major pancreatic fistula is defined as the drainage of more than 200ml of fluid or the development of an intra-abdominal abscess. In duct to mucosa anastomosis a parenchymal pancreatic leakage can drain amylase fluids for a few days. These non anastomotic leaks tend to resolve spontaneously in a few days and do not require surgical explorations, while true anastomotic leaks tend not to resolve spontaneously or after weeks or months. Classical risk factors associated with pancreatic fistula after pancreatoduodenectomy for cancer include patients related risk factors such as age > 70 years, male sex, low creatinine clearance, jaundice and malnutrition, or pancreas and disease related risk factors, such as pancreatic head or periampullary tumors, pancreatic fibrosis, pancreatic texture, duct size, or Surgeons experience and volume Center for complex surgery (20–22). However it has been widely accepted that pancreatic fistula is mainly associated with pancreatic texture and duct size (23–26). In fact, pancreatic fistula rate is near 0% for Patients with a hard pancreas and large duct and near 20% for those with a soft pancreas and a small duct. There are 3 risk factors associated with soft pancreas:
most soft pancreas have a small duct. In this situation secure duct-to-mucosa anastomosis is quite difficult;
soft pancreas is easily injured by stitches directly or for tissue ischemia;
soft pancreas has a normal exocrine function with juice rich in proteolytic enzymes and the increase in amylase drains may be provided by realimentation.
The key to excellent outcomes after pancreaticoduodenectomy is a reduction of active fistulas. To reduce the risk of pancreatic leakage, a selection of proper pancreaticojejunostomy according to pancreatic texture and duct size is mandatory. Although substantial progresses in reducing the rate of pancreatic fistula have been made in the last years, preoperative improved understanding of the risk factors has been disappointing. Identifying glands at high risk for a leak can trigger modification in surgical technique, earlier removal of drains, thus avoiding infections and favoring faster realimentation and earlier Patients discharge from the Hospital. Many studies showed different results when considering the type of pancreaticojejunostomy, provided that all anastomoses are associated with a different incidence of pancreatic fistula. We report the experience with pancreatic fistula in a series of 150 consecutive pancreatoduodenectomies, prospectively performed by one Surgeon with different reconstructive techniques. We also investigated the most common technical procedures according to preoperative and perioperative risk factors reported in the literature. The number of pancreatoduodenectomies performed in a single Center every year is clearly correlated to the mortality risk. In Italy the mortality after PD is 12,4% in low volume Centers and 2,6% in high volume Centers (18). However there are many questions: how many procedures should be performed in order to define a high volume Center and how many Surgeons usually perform the operations in high volume Centers? Finally, until the country health authorities regulate the concentration of complex procedures into a few high volume Centers, all Surgeons are authorized to perform all complex procedures provided that they are following the guidelines on pancreatic surgery published by the most experienced Centers. Some Authors suggest the use of a stent inside the pancreatic anastomosis with or without an external pancreatic drainage. The stent should allow a safer anastomosis and would protect the anastomosis. However the internal stent has no protective effect in terms of pancreatic fistula risk, total morbidity or mortality as suggested by some Authors (19, 27). Generally no significant differences are recorded in terms of morbidity and mortality using the duct occlusion method with adsorbable or non readsorbable material, but the incidence of pancreatic fistula is up to 50% higher. Therefore the duct occlusion method is used to reduce mortality in low volume Hospitals in case of soft pancreas with a small size duct, although with a higher risk of postoperative diabetes. Duct occlusion procedure, pancreatic transection with stapler or simple suture ligation of the duct are sometimes indicated in the case of reoperation for hemorrhage or sepsis due to pancreatic leak. So far, insufficient evidence exists to show that duct occlusion procedure can replace pancreaticojejunostomy. Moreover, Patients with pancreatic duct occlusion develop pancreatic exocrine insufficiency with malabsorption (13–17). Pancreaticogastrostomy seems to carry several advantages in terms of reducing the incidence of pancreatic fistula, as reported by many cohort studies. In contrast, all RCT studies failed to show an advantage over the pancreaticojejunostomy in terms of perioperative outcome (28–30). Pancreaticojejunostomy is the most commonly used method of pancreaticoenteric anastomosis after pancreaticoduodenectomy. The anastomosis can be performed as an end-to-end anastomosis with invagination of the pancreatic stump or as an end-to-side anastomosis with or without duct-to-mucosa suturing. An internal or external stent can be placed in the pancreatic duct and the jejunal loop can be positioned in an antecolic, retrocolic or retromesenteric fashion. An isolate Roux loop pancreaticojejunostomy and a separate hepaticojejunal anastomosis are suggested to reduce the incidence and the severity of pancreatic leakage (31). At the moment, there is evidence that an isolated Roux loop pancreaticojejunostomy can not minimize the incidence of pancreatic fistula (34). Binding pancreaticojejunostomy could significantly decrease post operative complications (35) compared with the end-to-end pancreaticojejunostomy (32). The main concern of this techniques is the difficulty in controlling the tighteness of tying the binding ligature (33). The end-to-end anastomosis with a 4 cm pancreatic stump invagination in to the jejunum and a jejunal mucosa controlled cauterization to prevent the secretions from the jejunal mucosa was performed by Chen (34) with few complications. Duct to mucosa pancreaticojejunal anastomosis was previously recommended for Patients with duct size > 3 mm, whereas recently this technique is performed regardless of the duct size using magnification (35). Although a prospective study reported by Bassi (36) evidenced no significant difference in the pancreatic fistula rate between end to side and duct to mucosa pancreaticojejunostomy, many Authors found that the duct to mucosa anastomosis (37, 38) is safer, particularly with wide pancreatic ducts, usually associated with firm or hard pancreatic tissue (37, 38). However, based on the current evidence, it is unclear which pan-creaticojejunostomy technique is superior to significantly decrease pancreatic fistula rates and related complications. Three conditions are important for successful pancreaticojejunal anastomosis:
tension-free anastomosis;
adequate blood supply of the pancreatic stump;
fluid passage of pancreatic juice into the jejunum.
The development of a pancreaticojejunal fistula is more common in Patients with duodenal or ampullary carcinoma compared to Patients with the diagnosis of pancreatic cancer, because Patients with pancreatic cancer are more likely to have a late diagnosis cancer and to develop parenchimal fibrosis and duct’s dilatation. Tumor side, tumor size and histopathologic characteristics are related to the texture of the gland and to the duct size. The risk of pancreatic fistula appears to be multifactorial involving demographic, preoperative or intraoperative stenting, type of anastomosis, pathologic factors and drainages, but at the end only the texture of the pancreatic gland and the correspondent duct size are significantly associated with pancreaticojejunal anastomotic leakage. Patients with an high grade of fibrosis, firmer texture gland and wide duct have a lower incidence of fistula formation. Patients with soft gland and small duct, particularly Patients with duodenal or ampullary tumors, have a higher incidence of pancreatic fistula. Whereas pancreatic consistency is a more subjective assessment by the Surgeon, the duct size is directly related to the gland fibrosis and texture. Imaging preoperative assessment of the duct size and of the related gland texture can suggest to introduce a significant variable in the surgical technique or to transfer the Patients from low volume to high volume Center for complex procedures. According to Surgeons experience the pancreatic fistula rate is related to pancreatic texture and duct size. The pancreatic fistula rate is lower in both Groups of Patients with firm or hard pancreas and 3–5 mm or > 6 mm duct size (39–41).
In conclusion, we make the following considerations: radiological preoperative assessment of the duct size and selection of proper pancreatic anastomotic techniques, according to pancreatic duct size and related pancreatic texture and fibrosis grading, may reduce the pancreatic fistula rate, particularly with the employment of the duct to mucosa pancreaticojejunostomy. However, the key to excellent outcomes is certainly to refer the “high risk” Patients to high volume Center.
References
- 1.Kuhlmann KF, de Castro SM, Wesseling JG. Surgical treatment of pancreatic adenocarcinoma; actual survival and prognostic factors in 343 patients. Eur J Cancer. 2004;40:549–558. doi: 10.1016/j.ejca.2003.10.026. [DOI] [PubMed] [Google Scholar]
- 2.Stojadinovic A, Brooks A, Hoos A, Jaques DP, Colon KC, Brennan MF. An evidence-based approach to the surgical management of rectable pancreatic adenocarcinoma. J Am Coll Surg. 2003;196:954–964. doi: 10.1016/S1072-7515(03)00010-3. [DOI] [PubMed] [Google Scholar]
- 3.Yang YM, Tian XD, Zhuang Y, Wang WM, Wan YL, Huang YT. Risk factors of pancreatic leakage after pancreaticoduodenectomy. World J Gastroenterol. 2005;11:2456–2461. doi: 10.3748/wjg.v11.i16.2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Balcom JHIV, Rather DW, Warshaw AL, Chang Y, Fernandez del Castillo C. Ten year experience with 733 pancreas resections. Arc Surg. 2001;136:391–398. doi: 10.1001/archsurg.136.4.391. [DOI] [PubMed] [Google Scholar]
- 5.Bassi C, Butturini G, Molinari E, Mascetta G, Salvia R, Falconi M, Gumbs A, Pederzoli P. Pancreatic fistula rate after pancreatic resection. The importance of definition. Digest Surg. 2004;21(1):54–9. doi: 10.1159/000075943. [DOI] [PubMed] [Google Scholar]
- 6.Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an intenational study group (ISPGF) definition. Surgery. 2005;138:8–13. doi: 10.1016/j.surg.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Pratt WB, Maithel SK, Vanounou T, Huang ZS, Callery MP, Vollmer CM., Jr Clinical and economic validation of the International Study Group of Pancreatic Fistula (ISGPF) classification scheme. Ann Surg. 2007;245(3):443–51. doi: 10.1097/01.sla.0000251708.70219.d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strasberg SM, Drebin JA, Mokadam NA, Green DW, Jones KL, Ehlers JP, Linehan D. Prospective trial of a blood supply-based technique of pancreaticojejunostomy: effect on anastomotic failure in the Whipple procedure. J Am Coll Surg. 2002;194(6):746–58. doi: 10.1016/s1072-7515(02)01202-4. [DOI] [PubMed] [Google Scholar]
- 9.Shyr YM, Su CH, Wu CW, Lui WY. Does drainage fluid amylase reflect pancreatic leakage after pancreaticoduodenectomy? World J Surg. 2003;27(5):606–10. doi: 10.1007/s00268-003-6841-y. Epub 2003 Apr 28. [DOI] [PubMed] [Google Scholar]
- 10.Molinari E, Bassi C, Salvia R, Butturini G, Crippa S, Talamini G, Falconi M, Pederzoli P. Amylase value in drains after pancreatic resection as predictive factor of postoperative pancreatic fistula: results of a prospective study in 137 patients. Ann Surg. 2007;246(2):281–7. doi: 10.1097/SLA.0b013e3180caa42f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McKay A, Mackenzie S, Sutherland FR, Bathe OF, Doig C, Dort J, Vollmer CM, Jr, Dixon E. Meta-analysis of pancreaticojejunostomy versus pancreaticogastrostomy reconstruction after pancreaticoduodenectomy. Br J Surg. 2006;93(8):929–36. doi: 10.1002/bjs.5407. [DOI] [PubMed] [Google Scholar]
- 12.Wente MN, Shrikhande SV, Müller MW, Diener MK, Seiler CM, Friess H, Büchler MW. Pancreaticojejunostomy versus pancreaticogastrostomy: systematic review and meta-analysis. Am J Surg. 2007;193(2):171–83. doi: 10.1016/j.amjsurg.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 13.Tran K, Van Eijck C, Di Carlo V, Hop WC, Zerbi A, Balzano G, Jeekel H. Occlusion of the pancreatic duct versus pancreaticojejunostomy: a prospective randomized trial. Ann Surg. 2002;236(4):422–8. doi: 10.1097/00000658-200210000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Suc B, Msika S, Fingerhut A, Fourtanier G, Hay JM, Holmières F, Sastre B, Fagniez PL French Associations for Surgical Research. Temporary fibrin glue occlusion of the main pancreatic duct in the prevention of intra-abdominal complications after pancreatic resection: prospective randomized trial. Ann Surg. 2003;237(1):57–65. doi: 10.1097/00000658-200301000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lillemoe KD, Cameron JL, Kim MP, Campbell KA, Sauter PK, Coleman JA, Yeo CJ. Does fibrin glue sealant decrease the rate of pancreatic fistula after pancreaticoduodenectomy? Results of a prospective randomized trial. Gastrointest Surg. 2004;8(7):766–72. doi: 10.1016/j.gassur.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Ahren B, Tranberg KG, Andrei-Sandberg A, Bengmark S. subtotal pancreatectomy for cancer: closure of pancreatic remnant with staplers. HBP Surgery. 1990;2:29–35. doi: 10.1155/1990/73475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bilimoria MM, Cormier JN, Mun Y, Lee JE, Evans DB, Pisters PW. Pancreatic leak after left pancreatectomy is reduced following main pancreatic duct ligation. Br J Surg. 2003;90(2):190–6. doi: 10.1002/bjs.4032. [DOI] [PubMed] [Google Scholar]
- 18.Roder JD, Stein HJ, Böttcher KA, Busch R, Heidecke CD, Siewert JR. Stented Versus Nonstented Pancreaticojejunostomy After Pancreatoduodenectomy: a Prospective Study. Annals of Surgery. 1999;229(1):41–48. doi: 10.1097/00000658-199901000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Winter JM, Cameron JL, Campbell KA. Does pancreatic duct stenting decrease the rate of pancreatic fistula following pancreatico duodenectomy? Results of a prospective randomized trial. J Gastrointest Surg. 2006;10:1280–1290. doi: 10.1016/j.gassur.2006.07.020. [DOI] [PubMed] [Google Scholar]
- 20.Marcus SG, Cohen H, Ranson JH. Optimal management of the pancreatic remnant after pancreaticoduodenectomy. Ann Surg. 1995;221(6):635–648. doi: 10.1097/00000658-199506000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muscari F, Suc B, Kirzin S, Hay JM, Fourtanier G, Fingerhut A, Sastre B, Chipponi J, Fagniez PL, Radovanovic A. Risk factors for mortality and intra-abdominal complications after pancreatoduodenectomy: multivariate analysis in 300 patients. Surgery. 2006;139(5):591–8. doi: 10.1016/j.surg.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 22.Lin JW, Cameron JL, Yeo CJ, Riall TS, Lillemoe KD. Risk factors and outcomes in postpancreaticoduodenectomy pancreaticocutaneous fistula. J Gastrointest Surg. 2004;8(8):951–9. doi: 10.1016/j.gassur.2004.09.044. [DOI] [PubMed] [Google Scholar]
- 23.Mok KT, Wang BW, Liu SI. Management of pancreatic remnant with strategies according to the size of pancreatic duct after pancreaticoduodenectomy. Br J Surg. 1999;86(8):1018–9. doi: 10.1046/j.1365-2168.1999.01206.x. [DOI] [PubMed] [Google Scholar]
- 24.Sato N, Yamaguchi K, Chijiiwa K, Tanaka M. Risk analysis of pancreatic fistula after pancreatic head resection. Arch Surg. 1998;133(10):1094–8. doi: 10.1001/archsurg.133.10.1094. [DOI] [PubMed] [Google Scholar]
- 25.Hamanaka Y, Nishihara K, Hamasaki T, Kawabata A, Yamamoto S, Tsurumi M, Ueno T, Suzuki T. Pancreatic juice output after pancreatoduodenectomy in relation to pancreatic consistency, duct size, and leakage. Surgery. 1996;119(3):281–7. doi: 10.1016/s0039-6060(96)80114-0. [DOI] [PubMed] [Google Scholar]
- 26.Al Sharaf K, Ihse I, Dawiskiba S, Andrein Sandberg A. characteristics of the gland remnant predict complications after subtotal pancreatectomy. Digestive Surgery. 1997;14(2):101–106. [Google Scholar]
- 27.Sohn TA, Yeo CJ, Cameron JL, Pitt HA, Lillemoe KD. Do preoperative biliary stents increase postpancreaticoduodenectomy complications? J Gastrointest Surg. 2000;4(3):258–67. doi: 10.1016/s1091-255x(00)80074-8. [DOI] [PubMed] [Google Scholar]
- 28.Takano S, Ito Y, Watanabe Y, Yokoyama T, Kubota N, Iwai S. Pancreaticojejunostomy versus pancreaticogastrostomy in reconstruction following pancreaticoduodenectomy. Br J Surg. 2000;87(4):423–7. doi: 10.1046/j.1365-2168.2000.01395.x. [DOI] [PubMed] [Google Scholar]
- 29.Aranha GV, Hodul P, Golts E, Oh D, Pickleman J, Creech S. A comparison of pancreaticogastrostomy and pancreaticojejunostomy following pancreaticoduodenectomy. J Gastrointest Surg. 2003 Jul-Aug;7(5):672–82. doi: 10.1016/s1091-255x(02)00432-8. [DOI] [PubMed] [Google Scholar]
- 30.Duffas JP, Suc B, Msika S, Fourtanier G, Muscari F, Hay JM, Fingerhut A, Millat B, Radovanowic A, Fagniez PL French Associations for Research in Surgery. A controlled randomized multicenter trial of pancreatogastrostomy or pancreatojejunostomy after pancreatoduodenectomy. Am J Surg. 2005;189(6):720–9. doi: 10.1016/j.amjsurg.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 31.Kaman L, Sanyal S, Behera A, Singh R, Katariya RN. Isolated roux loop pancreaticojejunostomy vs single loop pancreaticojejunostomy after pancreaticoduodenectomy. Int J Surg. 2008;6(4):306–10. doi: 10.1016/j.ijsu.2008.04.007. Epub 2008 May 8. [DOI] [PubMed] [Google Scholar]
- 32.Peng SY, Mou YP, Liu YB, Su Y, Peng CH, Cai XJ, Wu YL, Zhou LH. Binding pancreaticojejunostomy: 150 consecutive cases without leakage. J Gastrointest Surg. 200;7(7):898–900. doi: 10.1007/s11605-003-0036-6. [DOI] [PubMed] [Google Scholar]
- 33.Peng SY, Wang JW, Lau WY, Cai XJ, Mou YP, Liu YB, Li JT. Conventional versus binding pancreaticojejunostomy after pancreaticoduodenectomy: a prospective randomized trial. Ann Surg. 2007;245(5):692–8. doi: 10.1097/01.sla.0000255588.50964.5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen HW, Lai EC, Su SY, Cai YF, Zhen ZJ, Lau WY. Modified technique of pancreaticojejunal anastomosis with invagination following pancreaticoduodenectomy: a cohort study. World J Surg. 2000;32(12):2695–700. doi: 10.1007/s00268-008-9760-0. [DOI] [PubMed] [Google Scholar]
- 35.Wada K, Traverso LW. Pancreatic anastomotic leak after the Whipple procedure is reduced using the surgical microscope. Surgery. 2006;139(6):735–42. doi: 10.1016/j.surg.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 36.Bassi C, Falconi M, Molinari E, Mantovani W, Butturini G, Gumbs AA, Salvia R, Pederzoli P. Duct-to-mucosa versus end-to-side pancreaticojejunostomy reconstruction after pancreaticoduodenectomy: results of a prospective randomized trial. Surgery. 2003;134(5):766–71. doi: 10.1016/s0039-6060(03)00345-3. [DOI] [PubMed] [Google Scholar]
- 37.Greene BS, Loubeau JM, Peoples JB, Elliott DW. Are pancreatoenteric anastomoses improved by duct-to-mucosa sutures? Am J Surg. 1991;161(1):45–9. doi: 10.1016/0002-9610(91)90359-l. discussion 49–50. [DOI] [PubMed] [Google Scholar]
- 38.Hosotani R, Doi R, Imamura M. Duct-to-mucosa pancreaticojejunostomy reduces the risk of pancreatic leakage after pancreatoduodenectomy. World J Surg. 2002;26(1):99–104. doi: 10.1007/s00268-001-0188-z. [DOI] [PubMed] [Google Scholar]
- 39.Yang YM, Tian XD, Zhuang Y, Wang WM, Wan YL, Huang YT. Risk factors of pancreatic leakage after pancreaticoduodenectomy. World J Gastroenterol. 2005;11(16):2456–61. doi: 10.3748/wjg.v11.i16.2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shrikhande SV, D’Souza MA. Pancreatic fistula after pancreatectomy: evolving definitions, preventive strategies and modern management. World J Gastroenterol. 2008;14(38):5789–96. doi: 10.3748/wjg.14.5789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lai ECH, Lau SHY, Lau WY. Measures to prevent pancreatic fistula after pancreatoduodenectomy: a comprehensive review. Arch Surg. 2009;144(11):1074–1080. doi: 10.1001/archsurg.2009.193. [DOI] [PubMed] [Google Scholar]