Abstract
Aim
To evaluate the incidence of Poly Implant Prosthése (PIP) rupture as assessed by magnetic resonance imaging (MRI), the prevalence of the detected signs and the potential correlation with breast carcinoma.
Patients and methods
67 patients with silicone breast implants and clinical indications for breast MRI were evaluated for a total of 125 implants: 40 (32%) PIP in 21 patients and 85 non-PIP in 46 patients (68%), the latest considered as control group. A 1.5-T MR imaging device was used in order to assess implant integrity with dedicated sequences and in 6 cases a dynamic study was performed for characterizing breast lesions. Two radiologists with more than 5 years’ experience in the field of MRI evaluated in consensus all MR images searching for the presence of clear signs of intra or extra-capsular implant rupture.
Results
20/40 (50%) PIP implants presented signs of intra-capsular rupture: linguine sign in 20 cases (100%), tear-drop sign in 6 (30%). In 12/20 cases (60%), MRI signs of extra-capsular rupture were detected. In the control group, an intra-capsular rupture was diagnosed in 12/85 cases (14%) associated with extra-capsular one in 5/12 cases (42%). Among the six cases with suspected breast lesions, in 2/21 patients with PIP implants (10%) a breast carcinoma was diagnosed (mucinous carcinoma, n=1; invasive ductal carcinoma, n=1). In 4/46 patients (9%) with non-PIP implants, an invasive ductal carcinoma was diagnosed.
Conclusion
The rupture rate of PIP breast implants is significantly higher than non-PIP (50% vs 14%). MRI represents the most accurate imaging tool for evaluating breast prostheses and the linguine sign is the most common MRI sign to be searched. The incidence of breast carcinoma does not significantly differ between the PIP and non-PIP implants and a direct correlation with breast cancer can not been demonstrated.
Keywords: Breast, Implants, PIP, MRI
Introduction
In recent years, aesthetic breast augmentation and breast reconstruction after mastectomy have increased requests for implant surgery (1).
Different kinds of breast implants exist and usually implantable silicone devices are used at this purpose (2).
Despite the routine use of silicone breast implants, complications such as capsular contraction and intra-capsular or extra-capsular rupture can occur and they can lead to surgical removal and replacement of the implants after several years (2).
Clinical examination fails to detect implant rupture in more than 50% of cases; therefore the use of imaging techniques is mandatory and magnetic resonance imaging (MRI) represents the most accurate tool in this field (1, 3–7).
The recent Poly Implant Prosthése (PIP; La Seynesur-Mer, France) breast implant scandal has led to renewed debates about the safety of implantable silicone prostheses for breast augmentation (2). In fact, PIP breast implants were manufactured by the eponymous French company and distributed worldwide beginning in 2001 until 2010 when they were banned.
Different rupture rates have been reported in the medical literature with values ranging from 7 to 35%, although different biasing factors can influence these data (8). Therefore, the medical literature still has few data regarding the PIP problem or the assessment of complications from the use of this kind of implants.
Besides, in patients with PIP breast implants, a possible association with lymphoma, specifically anaplastic large cell lymphoma, and rare cases of breast carcinoma have been reported. However, a direct link between PIP implants and neoplastic disease has not been established in the literature (9–11).
The aim of our study is to evaluate the incidence of PIP implant rupture as assessed by MR imaging, the prevalence of the detected signs and the potential correlation with breast carcinoma.
Patients and methods
Patient population
This prospective, single-centre study was carried out between June 2012 and July 2013. Sixty-seven consecutive patients (age range, 26–64 years; mean age ± standard deviation (SD), 43.7 ± 9.8 years) with silicone breast implants and clinical indications for breast MRI were evaluated for a total of 125 implants: 40 (32%) PIP in 21 patients and 85 non-PIP in 46 patients (68%), the latest considered as control group. Clinical indications for breast MRI were represented by suspected implant rupture basing on clinical assessment or mammographic and/or ultrasound (US) examinations, implant age of = 7 years, and presence of breast lesion detected by mammographic or US examinations (n=6). All patients with positive MRI associated with suspected clinical signs were referred for surgery which was performed within twenty days of diagnosis. All patients with negative MRI were referred for a six-month follow-up MR examination. The study followed the principles of Helsinki declaration and a written informed consent was obtained in all cases.
MRI protocol
Magnetic resonance images were acquired with a 1.5-T MR imaging device (Philips, Achieva 1.5) equipped with a 4-channel phased array coil (SENSE-body coil). Breast MRIs were performed regardless of menstrual cycle phase, except for the 6 cases where breast tissue study was associated.
As already performed in other series (1), the following sequences were obtained:
Axial turbo spin echo (TSE) T2 weighted images: matrix 512 × 512; FOV 350–470; scan% 75; slice number 50; thickness 3 mm; TR short (mean value 4864 ms); TE 120;
Axial-silicone-only images: matrix 512 × 512; scan% 80; TE 70 ms; TR short (mean value 9372 ms); TI 165 ms; slice number 40–50; thickness 3 mm;
Axial silicone suppression images: matrix 512 × 512; thickness 3 mm; slice number 35; FOV 350–400; RFOV 60; scan% 80; TE 2.4 ms; TR 4.9 ms;
Sagittal short tau inversion recovery (STIR) images: matrix 512 × 512; slice number 40; thickness 3 mm, FOV 350–400; RFV 60; TR 7500 ms, TE 70 ms; TI 160 ms.
In the 6 cases who needed also breast tissue evaluation, dynamic axial T1w high-resolution isotropic volume (THRIVE) sequences were performed before and after intravenous injection of 0.2 ml/kg of dimeglumine gadobenate (Multihance; Bracco, Milan, Italy) at a flow rate of 2.5 ml/s followed by 20 ml of saline solution with the following parameters:
- Three-dimensional (3D) dynamic, contrast-enhanced (CE) T1- weighted high resolution isotropic volume (THRIVE) sequences (TR/TE = 4. 4/2.0 ms, FOV = 250 × 450 × 150 mm (AP × RL × FH), matrix 168 × 300, 100 slices with 1.5-mm slice thickness, turbo factor 50, SENSE factor 1.6, 6 dynamic acquisitions, resulting in 1.5-mm3 isotropic voxels, a dynamic data acquisition time of 1 min 30 s, and a total sequence duration of 9 min).
Image analysis
Two radiologists with more than 5 years’ experience in the field of magnetic resonance imaging and virtual image reconstruction (MM, MT) evaluated in consensus MR sequences. All images were firstly analysed at a workstation equipped with dedicated software for MRI examination (View-forum R5.1 V1L1 2006). Then, all dicom images were transferred to and analyzed on a workstation (HP XW 6400) equipped with a software dedicated to image reconstruction (Vitrea 4.1, Vital Images, Minneapolis, Minnesota, US) in order to assess conventional MR images associated to 3D virtual navigation as already reported in another series (1). The virtual navigation program was applied and a real time navigation of 3D volume data was also performed in all cases. All images were evaluated searching for the presence of clear signs of intra or extra-capsular implant rupture, as already reported in literature: linguine sign, teardrop sign, key-hole sign, presence of siliconomas and free silicone particles within axillary or mammary lymph nodes (1).
For virtual navigation, the integrity of prosthetic capsule, the quality of the content and the presence of any abnormality or irregularity within the implants were evaluated (1). The duration of post-processing was 5 minutes and 7 minutes, respectively for MRI and virtual navigation.
Patients with signs of implant rupture were referred for surgery.
Results
All the examined 45 breast prostheses were represented by single lumen silicone implants positioned in the sub-pectoral site in all cases.
By using both MR images and intra-prosthetic virtual navigation, 20 out of the 40 (50%) PIP implants presented signs of intra-capsular rupture: linguine sign in 20 cases (100%) (Figure 1), tear-drop sign in 6 (30%). A peri-prosthetic fluid effusion was also detected in all cases. In 12 out of 20 cases (60%), MRI signs of extra-capsular rupture represented by siliconomas and silicone dissemination to axillary and internal mammary lymph nodes were detected (Figure 2).
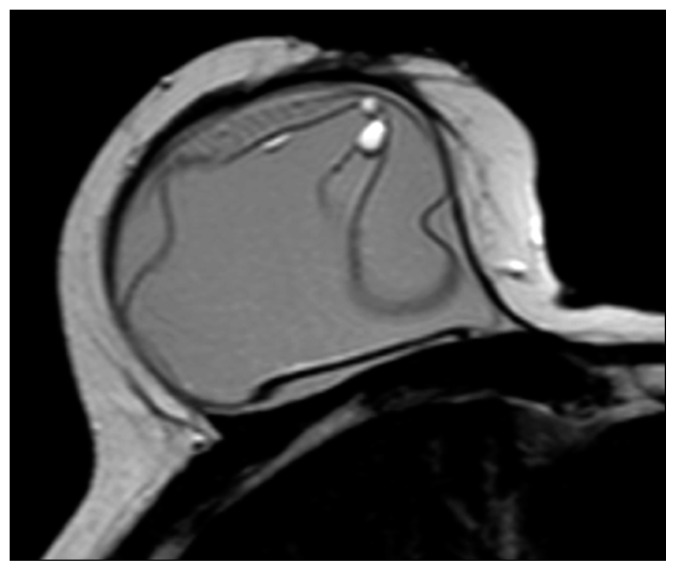
Fig. 1.
PIP implant with intra-capsular rupture detected at TSE-T2 MR sequence and represented by “linguine sign”.
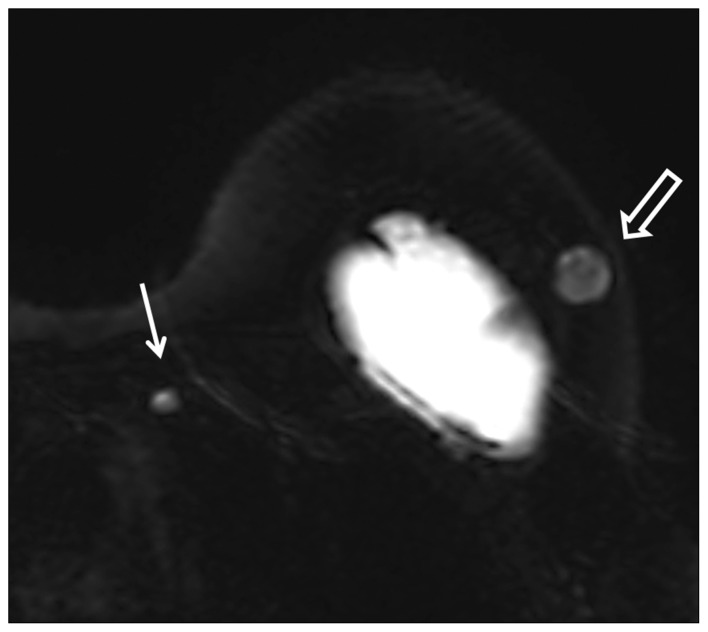
Fig. 2.
PIP implant with extra-capsular rupture detected at silicone-only MR sequence and represented by free peri-prosthetic silicone particles (empty arrow) and within an internal mammary lymph node (arrow).
In the control group, an intra-capsular rupture was diagnosed in 12 out of 85 cases (14%) associated with extra-capsular one in 5 out of 12 cases (42%).
Among the six cases with suspected breast lesions, in 2 out of the 21 patients with PIP implants (10%) a breast carcinoma was diagnosed (mucinous carcinoma, n=1; invasive ductal carcinoma, n=1). In 4 out of the 46 patients (9%) with non-PIP implants, an invasive ductal carcinoma was diagnosed.
All patients with MRI signs of intra or extra-capsular rupture and breast malignant lesions as confirmed by the pre-operative core needle biopsy were referred for surgery. The comparison with surgical findings confirmed the MRI diagnoses in all cases. All intact breast implants were not removed, also in the cases of PIP prostheses. All negatives were then confirmed at the six-month follow-up examination.
Discussion
The diagnosis of breast implant rupture is based on imaging techniques such as mammography, US, MRI which could be variously used as screening tests or as diagnostic techniques in symptomatic patients with different accuracy values (1, 3–6). The sensitivity of mammography for implant rupture ranges from between 25–30% and 68% (1, 3). In fact, mammography is useful in detecting migration of silicone away from the fibrous shell into the breast parenchyma along the pectoralis muscle or within the axillary lymph nodes but it is unable to recognize intra-capsular rupture because of the high opacity of silicone (1, 3).
US has a reported sensitivity and specificity of 50–77% and 55–84%, respectively, in detecting implant rupture. However, US represents one of the most “operator-dependent” techniques and it could not provide an accurate evaluation of the posterior wall of the breast implant because of silicone attenuation (12–15).
MRI has a reported sensitivity and specificity of 72–94% and 85–100%, respectively, for diagnosing silicone implant rupture because of its high spatial and soft-tissue resolution and the ability to set the signal from water, fat or silicone (1). Therefore, MRI represents the gold standard for the assessment of implant status and the latest step before the surgery in cases of rupture (16). The intra-prosthetic virtual navigation has been recently reported to be an additional promising tool in this field being able to improve MRI specificity (1).
In our experience, MRI allowed a correct diagnosis in all cases and therefore this crucial role for breast implant imaging has been confirmed.
Multiple specific signs of implant rupture have already been reported in literature. The signs of intra-capsular rupture are mainly represented by the “linguine” sign, “teardrop” sign, “keyhole” sign and “sub-capsular line” sign. The “linguine sign” consists of curvilinear hypo-intense lines within the hyper-intense silicone filled implant. It is due to the collapse of the implant shell in silicone gel and it represents the most reliable sign of intra-capsular rupture.
The “teardrop sign”, the “keyhole” and the “sub-capsular line” signs occur when small amounts of silicone are located between the inner shell and the fibrous capsule (1, 3).
On the other side, the diagnosis of extra-capsular rupture relies on the detection of free silicone particles outside the implant, within the breast glandular tissue or the axillary or mammary lymph nodes. In our series, the linguine sign has been confirmed to be the most common MR sign of implant rupture.
Numerous studies reported the use of MRI also for evaluating PIP implants which are characterized by mechanical fragility of shells and accelerated biodegradability of gels (2, 17–19).
Berry and Staneck reported a PIP implant rupture rate of 15.9–33.8% and Maijers and Niessen a rupture prevalence rate of 24 percent after 10 years (8).
Quaba et al. reported an overall rupture rate of 35.2% per patient and 21.3% per implant over an average period of 7.8 years and confirmed the unacceptably high failure rate for PIP implants in a single surgeon series of 676 patients (8). An interesting finding that has arisen from the study performed by Quaba is the significant difference in rupture rates depending on pocket placement of the implants. The rupture rates per implant almost double when the implant is placed in the sub-pectoral position probably because of the increased strain over the upper part of the implants by the pectoralis major muscle over time in implants that already have weakened shells.
In our series, a rupture rate of 50% was found for PIP implants; this value is slightly higher as compared with the other percentages reported in the medical literature and significantly higher than the 14% rupture rate of non-PIP implants in our series. All prostheses were sub-pectoral positioned and had a mean age of more than 7 years; these data could explain the high rate of rupture and resulted to be confident with other studies reported in this field (8).
In the study reported by Oulharj et al. on a series of 828 cases, the rupture rate of PIP implants was 7.73% (11). This value can be explained by the choice to preventively remove PIP implants even in the absence of evidence of rupture. Differently, in our experience, all intact implants were not surgically removed and underwent follow-up MRI control.
With regard to the potential association between PIP implants and neoplastic disease, two and four cases of breast carcinoma occurred respectively in the group of PIP and non-PIP implants, with no significant difference between the two groups. Therefore, as also reported in the medical literature, no association between PIP prostheses and breast cancer can been demonstrated (9–11).
Our study has some important limitations, mainly represented by the small size of the examined sample; the occurrence of only single lumen sub-pectoral silicone gel implants; the lack of a true gold standard because of the use of a six month follow up MR as a negative confirmation; the impossibility to evaluate inter-reader variability and the selection bias mainly represented by a single sample including only symptomatic patients.
Conclusion
In conclusion, the rupture rate of PIP breast implants is significantly higher than non-PIP (50% vs 14%). MRI represents the most accurate imaging tool for evaluating breast prostheses and the linguine sign is the most common MRI sign to be searched. The incidence of breast carcinoma does not significantly differ between the PIP and non-PIP implants and a direct correlation with breast cancer can not been demonstrated.
References
- 1.Moschetta M, Telegrafo M, Capuano G, Rella L, Scardapane A, Angelelli G, et al. Intra-prosthetic breast MR virtual navigation: a preliminary study for a new evaluation of silicone breast implants. Magn Reson Imaging. 2013;31(8):1292–7. doi: 10.1016/j.mri.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Yildirimer L, Seifalian AM, Butler PE. Surface and mechanical analysis of explanted Poly Implant Prosthèse silicone breast implants. Br J Surg. 2013 May;100(6):761–7. doi: 10.1002/bjs.9094. [DOI] [PubMed] [Google Scholar]
- 3.Colombo G, Ruvolo V, Stifanese R, Perillo M, Garlaschi A. Prosthetic breast implant rupture: imaging-pictorial essay. Aesth Plast Surg. 2011;35:891–900. doi: 10.1007/s00266-011-9694-z. [DOI] [PubMed] [Google Scholar]
- 4.Di Benedetto G, Cecchini S, Grassetti L, Baldassarre S, Valeri G, Leva L, et al. Comparative study of breast implant rupture using mammography, sonography, and magnetic resonance imaging: correlation with surgical findings. Breast J. 2008;14:532–7. doi: 10.1111/j.1524-4741.2008.00643.x. [DOI] [PubMed] [Google Scholar]
- 5.Hölmich LR, Kjøller K, Vejborg I, Conrad C, Sletting S, McLaughlin JK, et al. Prevalence of silicone breast implant rupture among Danish women. Plast Reconstr Surg. 2001;108:848–58. doi: 10.1097/00006534-200109150-00006. [DOI] [PubMed] [Google Scholar]
- 6.Ahn CY, Shaw WW. Regional silicone-gel migration in patients with ruptured implants. Ann Plast Surg. 1994;33:201–8. doi: 10.1097/00000637-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 7.Song JW, Kim HM, Bellfi LT, Chung KC. The effect of study design biases on the diagnostic accuracy of magnetic resonance imaging for detecting silicone breast implant ruptures: a meta-analysis. Plast Reconstr Surg. 2011;127:1029–44. doi: 10.1097/PRS.0b013e3182043630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quaba O, Quaba A. PIP silicone breast implants: rupture rates based on the explantation of 676 implants in a single surgeon series. J Plast Reconstr Aesthet Surg. 2013;66(9):1182–7. doi: 10.1016/j.bjps.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Berry MG, Stanek JJ. The PIP mammary prosthesis: a product recall study. J Plast Reconstr Aesthet Surg. 2012;65(6):697–704. doi: 10.1016/j.bjps.2012.02.019. [DOI] [PubMed] [Google Scholar]
- 10.De Jong D, Vasmel WLE, de Boer JP, et al. Anaplastic large-cell lymphoma in women with breast implants. JAMA - J Am Med Assoc. 2008;300:2030–5. doi: 10.1001/jama.2008.585. [DOI] [PubMed] [Google Scholar]
- 11.Oulharj S, Pauchot J, Tropet Y. PIP breast implant removal: a study of 828 cases. J Plast Reconstr Aesthet Surg. 2014 Mar;67(3):302–7. doi: 10.1016/j.bjps.2013.12.016. [DOI] [PubMed] [Google Scholar]
- 12.Caskey CI, Berg WA, Anderson ND, Sheth S, Chang BW, Hamper UM. Breast implant rupture: diagnosis with US. Radiology. 1994;190:819–23. doi: 10.1148/radiology.190.3.8115633. [DOI] [PubMed] [Google Scholar]
- 13.Harris KM, Ganott MA, Shestak KC, Losken HW, Tobon H. Silicone implant rupture: detection with US. Radiology. 1993;187:761–8. doi: 10.1148/radiology.187.3.8497626. [DOI] [PubMed] [Google Scholar]
- 14.DeBruhl ND, Gorczyca DP, Ahn CY, Shaw WW, Bassett LW. Silicone breast implants: US evaluation. Radiology. 1993;189:95–8. doi: 10.1148/radiology.189.1.8372224. [DOI] [PubMed] [Google Scholar]
- 15.Cilotti A, Marini C, Iacconi C, Mazzotta D, Moretti M, Giaconi C, et al. Ultrasonographic appearance of breast implant complications. Ann Plast Surg. 2006;56:243–7. doi: 10.1097/01.sap.0000198560.24518.e7. [DOI] [PubMed] [Google Scholar]
- 16.Maijers MC, Niessen FB, Veldhuizen JF, Ritt MJ, Manoliu RA. MRI screening for silicone breast implant rupture: accuracy, inter- and intraobserver variability using explantation results as reference standard. Eur Radiol. 2014;24(6):1167–75. doi: 10.1007/s00330-014-3119-8. [DOI] [PubMed] [Google Scholar]
- 17.Aktouf A, Auquit-Auckbur I, Coquerel-Beghin D, Delpierre V, Milliez PY. Breast augmentation by poly implant prothèses silicone implants: retrospective study about 99 patients. Rupture analysis and management. Ann Chir Plast Esthet. 2012;57:558–66. doi: 10.1016/j.anplas.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 18.Maijers MC, Niessen FB. Prevalence of rupture in poly implant prothèse silicone breast implants, recalled from the European market in 2010. Plast Reconstr Surg. 2012;129(6):1372–8. doi: 10.1097/PRS.0b013e31824f0108. [DOI] [PubMed] [Google Scholar]
- 19.Collis N, Litherland J, Enion D, Sharpe DT. Magnetic resonance imaging and explantation investigation of long-term silicone gel implant integrity. Plast Reconstr Surg. 2007;120:1401–6. doi: 10.1097/01.prs.0000279374.99503.89. [DOI] [PubMed] [Google Scholar]