Abstract
Mesenteric cysts are rare and can occur at any age. They can manifest with abdominal pain or compressive mass effect. The exact etiology is unknown. Ultrasonography, computed tomography and laparoscopy are used in diagnosing mesenteric cysts. Laparoscopic excision of a mesenteric cyst is possible and should be considered as the treatment of choice. We present a case of mesenteric pseudocyst of small bowel treated by laparoscopic excision.
Keywords: Mesenteric pseudocyst, Laparoscopic surgery, Jejunal surgery
Introduction
Intra-abdominal cysts and pseudocysts are rare lesions (1). This condition was noticed in 1507 by Italian anatomist Benevenni while doing an autopsy on an 8 year old boy. Tillaux operated the first case in 1880 and actually 820 cases have been reported in literature (2). Incidence of the disease is about 1/100.000 according to Kurtz et al., but other authors record lower frequency, about 1/250.000 hospital admissions. The disease is much more frequent in children under the age of 10 years (1 patient per 4.000–34.000 hospital admissions) (1). In adults mesenteric cysts occur especially in the fourth decade of life. Frequency is equal between males and females according to Kurtz et al. and there was no difference according to race. In contrast to those reports Maliszewski et al. found a higher incidence in females (1). Mesenteric cysts in the paediatric age group occur more often in males (62.5%) and most cases were younger than 10 years (3). Mesenteric cysts are frequently asymptomatic (2), but sometimes patients may present with symptoms such as abdominal pain or discomfort, abdominal distension, nausea, vomiting, flatulence, constipation or diarrhea (1). Rarely these can be complicated with rupture or intestinal obstruction (2). Complicated midgut volvulus is a surgical emergency with high mortality rate (4). Intestinal volvulus caused by a mesenteric cyst typically affects children, with acute abdominal symptoms (2). Most of midgut volvulus in adults is a silent form of congenital midgut malrotation, but it also can be acquired from other medical conditions, such as adhesion bands, tumors, and mesenteric cysts (4). The most common presentation of mesenteric cyst was abdominal pain (63%), followed by abdominal mass (44%)(2). The most frequent sites of mesenteric cysts are: small bowel mesentery (50–80%) followed by large bowel mesentery (15–30%) (1), usually in the right colon. Very few cases have been reported of tumours found in mesentery of descending colon, sigmoid or rectum (5). The size of mesenteric cysts varies from a few centimeters to 10 cms. Cysts bigger than 10 cms are defined as giant mesenteric cysts. The exact etiology of mesenteric cysts is unknown (2). The most widely recognized classification was proposed in 1950 by Beahrs et al. (3): there are four categories of mesenteric cysts:
embryonic and developmental;
traumatic and acquired (1) (cyst wall composed mainly of fibrous tissue without a lining membrane)(6);
infective and degenerative;
neoplastic.
Recently Ros et al. reviewed 41 cases of mesenteric and omental cysts and proposed another histological classification correlated with the radiological findings. They classified cysts into five groups: Lymphangiomas, enteric duplication cysts, enteric cysts, mesothelial cysts, non pancreatic pseudocysts (they used the term “pseudocysts” in the classification of mesenteric cysts for the first time).
The last classification of intra-abdominal cysts was proposed in 2000 by Perrot et al. based on the histological identity of the internal epitelium and consists of 6 groups:
lymphatic cysts: simple cyst and lymphangoma (1) (this is the only exception that mostly occurs in the first decade of life (up to 12 yrs of age) with male predominance) (5);
mesothelial cysts: malignant mesothelioma, simple cyst, benign mesothelioma (1) (this is frequently associated with a history of previous pelvic inflammatory process or surgery and endometriosis) (5);
enteric cysts (including enteric duplication);
urogenital cyst;
mature cystic teratoma (dermoid cysts);
pseudocysts (infectious, traumatic and degenerative) (1).
To prevent confusion with much more common pancreatic pseudocyst, mesenteric pseudocysts are called as non-pancreatic pseudocysts (7). Non-pancreatic pseudocysts are masses without an inner cellular lining; they are thought to be the sequelae of a mesenteric or omental hematoma or abscess that did not resorb. They are unrelated to pancreatitis. Pathologically, pseudocysts are thick-walled, usually septated cystic masses with either hemorrhagic or prulent contents (8). The incidence of malignancy is about 3% (1).
Clinical imaging modalities (Ultrasound, Computed tomography or Magnetic Resonance imaging) may help in arriving at the exact diagnosis (2).
Sonographically, a hypoechoic mass is frequently seen filled with echogenic debrids. CT and MR imaging show a thick-walled cystic mass that may contain a fluid-fluid level resulting from hemorrhagic or purulent contents (8) and show no postcontrast enhancement. Non pancreatic pseudocysts have a fibrous wall, without epitelium, and a serous (pale yellow) or mucoid (brownish red) content. Their origin can be inflammatory or traumatic (9). The differential diagnosis, required prior to each operation, includes: peritoneal cyst, lymphangioma, endometriosis, ascites, pancreatic pseudocyst, haemangioma, cystic mesenteric panniculitis, hydatid cyst, cystic teratoma and urogenital cyst (1).
In the literature the advised surgical procedure is excision of the tumour (1). Once removed, mesenteric cysts rarely recur, and patients have a good prognosis. Bowel resection is required only in 33% of adult patients (2). The most common surgical procedure of treatment is excision during laparotomy (1). However, laparoscopic treatment of mesenteric cysts is a safe, preferred method of treatment and is a less-invasive surgical technique. Laparoscopic plays a vital role in the diagnosis of cysts, its site, origin and has a therapeutic role in the same sitting (5).
For many years the mesenteric cyst operation was performed with laparotomy. This changed in 1993, when Mackenzie performed laparoscopic excision (1).
There aren’t enough exections of laparoscopic excision of mesenteric cysts to provide a good evaluation of this technique. Shimura et al. has reported two cases of successful resection of mesenteric cysts; Vu et al. have also documented total laparoscopic excision of mesenteric cyst where cyst content was aspirated after adequate mobilization for easy extraction. Dursun et al. have reported a case of laparoscopic enucleation of mesenteric cyst of the ileum. Though the operating time is longer with laparoscopy, it has advantages of minimal access, which includes less postoperative pain, shorter hospital stay, early return to normal activity and better cosmesis (5). Laparoscopic excision of a mesenteric cyst is possible and should be considered as the treatment of choice. Following surgery, patient prognosis is excellent and recurrence is low (0% to 13,6%) (2). Mesenteric cysts have good prognosis and no recurrence have been reported following complete excision of the cyst. There are no study available to compare and contrast laparoscopic excision of mesenteric cysts in the small bowel versus colonic/sigmoid mesentery (5).
Case report
This report presents a case of a woman with an intra-abdominal cyst and unspecific symptoms, who was operated on with the laparoscopic approach.
The patient was admitted to the Department of General and Thoracic Surgery in S. Anna Hospital in Cona (Ferrara) with three months history of pain in the right quadrants of the abdomen irradiated in the right thigh. Additionally, the patient complained fever (38°C), loss of appetite, nausea and cramping pain, absence of neutrophilia. The patient has performed MRI in 2011 for low back pain with detection of right ovarian cyst. Seven months before she was Hospitalized for exertional dyspnea (ECG and cardiac enzymes were negative) with a diagnosis of anxiety syndrome. She was not menstruating and pregnancy was excluded. Transvaginal ultrasound was negative. There was no signs of peritoneum irritation in the physical examination. no significant medical history.
In the following days the patient performs treatment with Esopral and Buscopan (ineffective). Ultrasound of the abdomen and ultrasound of the abdominal wall were negative. Finally, CT revealed an intra-abdominal mass of 4 cm in diameter adhered to jejunal loops of non-unique interpretation. Other organs of the abdomen and pelvis were free of abnormalities. After taking history and physical examination, imaging exams and blood tests we proposed laparoscopy to the patient.
Exploration of the abdominal cavity identifies lesion of 4 cm within the mesentery of the last jejunal loops. The tumor did not appear to infiltrate neighboring structures. No other intraabdominal pathology noted. Segmental resection of intestinal loop and its mesentery, including the cystic lesion, was performed. The intestinal continuity was restored with mechanical jejunal-ileal anastomosis. Prophylactic appendectomy was also performed.
Microscopic examination of the excised cyst revealed Mesenteric pseudocyst, with adiponecrosis and xanthogranulomatous inflammation. Our patient’s cyst can be framed, according to Beahrs et al., Ros et al. and de Perrot et al. classifications, as mesenteric pseudocyst with prulent content.
Most such lesions are post-traumatic or infectious, in our patient trauma of the abdomen was not reported. Patient denied signs and symptoms of any possible previous abdominal inflammatory diseases. The patient had an uneventful postoperative course, and she was discharged 8 days after the operation. At 5 weeks follow up she was symptom free.
Discussion and conclusion
The case we reported, the patient came to the operating table without a proper diagnosis of disease. The diagnostic methods of imaging may allow the correct diagnosis, however, due to the rarity of the lesion is not always possible to resolve the diagnostic question. In our case, laparoscopy has had both a diagnostic and therapeutic significance as already reported by other authors. This surgical technique also offers the advantages of laparoscopy already known.
In line with other authors, we confirm that laparosopic approach, when possible, is the treatment of choice for these types of diseases.
Fig. 1.
Mesenteric jejunal pseudocyst surgical specimen.
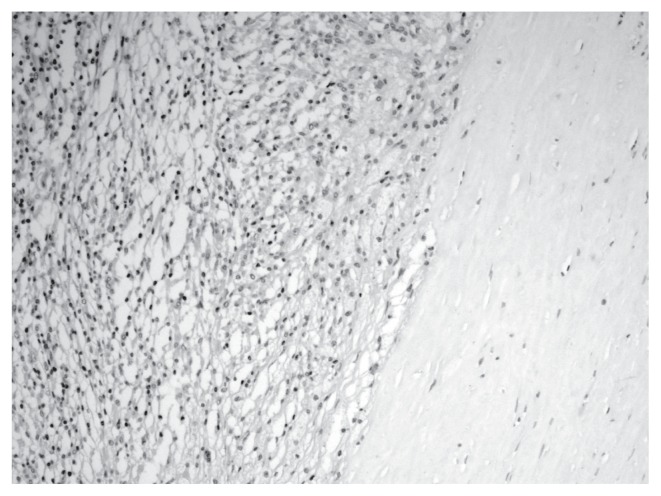
Fig. 2.
Xanthogranulomatous inflammation left, fibrous tissue of pseudo capsule to the right, absence of epithelial tissue.
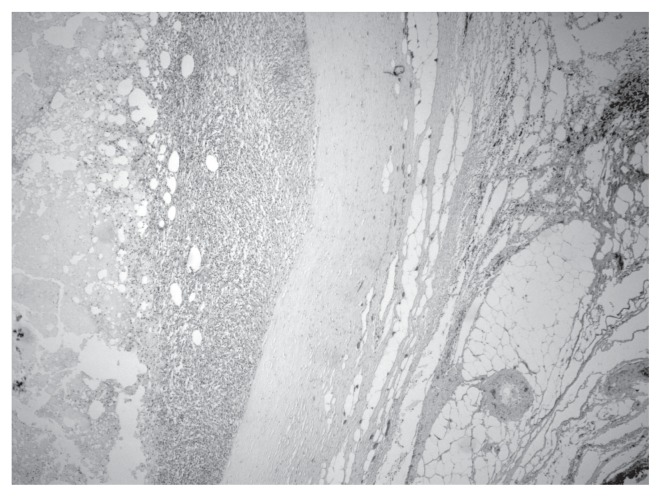
Fig. 3.
From right to left: mesenteric adipose tissue, fibrous pseudocapsule, xanthogranulomatous inflammation, area of central necrosis.
References
- 1.Kurnicki Jacek, Swiatkiewicz Janusz, Wrzesinska Natalia, Skorski Maciej. Laparoscopic treatment of a huge mesenteric pseudocyst- case report. Videosurgery and other miniinvasive techniques. 2011;6(3):167–172. doi: 10.5114/wiitm.2011.24696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goyal Sunder, Verma Ram Kumar, Singh Sohan Pal, Ahsan Mohmad Mozeeb. Mesenteric Cyst of Trasverse Mesocolon: a rare case: Report and Review of Literature. Arch Clin Exp Surg. 2013;2:200–203. [Google Scholar]
- 3.Prakash Advait, Agrawal Amit, Gupta Rahul K, Sanghvi Beejal, Parelkar Sandesh. Early management of mesenteric cyst prevents catastrophes: a single centre analysis of 17 cases. African Journal of Paediatric Surgery. 2010;7(3):140–143. doi: 10.4103/0189-6725.70411. [DOI] [PubMed] [Google Scholar]
- 4.Ko Kai-Hsiung, Chu Shi-Jye, Tsai Shih-Hung. Midgut volvulus as delayed consequence of posttraumatic mesenteric pseudocyst. The American Journal of Emergency Medicine. 2009;27(8):1025.e3–1025.e6. doi: 10.1016/j.ajem.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 5.Bhandarwar Ajay H, Tayade Mukund B, Borisa Ashok D, Kasat Gaurav V. Laparoscopic excision of mesenteric cyst of sigmoid mesocolon. Journal of Minimal Access Surgery. 2013;9(1):37–39. doi: 10.4103/0972-9941.107138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iida Toshio, Suenaga Masahiro, Takeuchi Yuki, Kobayashi Toru, Tobinaga Jyunichi, Sakai Mitsuru, Takenaka Hiroharu, Nomura Hisahiro, Oguma Koaki. Mesenteric pseudocyst of the sigmoid colon. Journal of Gastroenterology. 2003;38:1081–1085. doi: 10.1007/s00535-003-1200-1. [DOI] [PubMed] [Google Scholar]
- 7.Cizginer Sevdenur, Tatli Servet, Snyder Eric L, Goldberg Joel E, Silverman Stuart G. CT and MR imaging Features of a non pancreatic Pseudocyst of the mesentery. European Journal of General Medicine. 2009;6(1):49–51. [Google Scholar]
- 8.Stoupis C, Ros PR, Abbitt PL, Burton SS, Gauger J. Bubbles in the Belly: Imaging of Cystic Mesenteric or Omental Masses. Scientific Exhibit. 1994;14(4):729–737. doi: 10.1148/radiographics.14.4.7938764. [DOI] [PubMed] [Google Scholar]
- 9.Gallego Josè C, Gonzalez Josè M, Fernandez-Virgos Amelia, del Castillo Marcelino. Retrorectal mesenteric cyst (non pancreatic pseudocyst) in adult. European Journal of Radiology. 1996;23:135–137. doi: 10.1016/0720-048x(96)01024-8. [DOI] [PubMed] [Google Scholar]