Abstract
Introduction
We report the case of a patient who presented with subcutaneous emphysema, dyspnea and cough 7 days after total thyroidectomy for cancer. In addition we review the Literature and discuss the therapeutic challenges as well as management options.
Case report
A 17-year old female patient underwent a total thyroidectomy with right cervical lymph adenectomy for papillar cancer. Lung metastases are present. On postoperative day 7 she presented with face and neck swelling due to subcutaneous emphysema, dyspnea and persistent cough. The radiological evaluation revealed a tear on the right antero-lateral wall of the trachea. The patient underwent surgical exploration of the neck which confirmed the tracheal rupture and showed an important tracheal necrosis all around the tear. Due to the impossibility to make primary closure of the trachea or a tracheal resection, the tear was repaired with muscular flap interposition, (around the trachea as a scarf ), using the contralateral clavicular part of sternocleidomastoid muscle and prethyroid muscles bilaterally. The postoperative course was uneventful and the patient is alive 20 months after surgery and iodine induced adjuvant therapy.
Conclusion
Delayed tracheal rupture should be suspected in all patients who present subcutaneous emphysema after thyroid surgery. The lesion should be promptly treated with primary closure or tracheal resection when possible. Muscular flap interposition could be a safe alternative option when the other procedures are contraindicated.
Keywords: Total thyroidectomy, Tracheal rupture, Tracheal surgery, Muscular flap transposition
Introduction
Tracheal rupture is rare, very often caused by penetrating neck trauma. Iatrogenic tracheal rupture is extraordinarily rare, mostly described after bronchoscopic procedures or esophageal and neck dissection (1). Tracheal injury during thyroidectomy is described in many series and usually is promptly treated during the procedure (2). Delayed tracheal rupture after total thyroidectomy represents a very rare but life-threatening post-operative complication (1, 3, 4). Two are the possible causes: an extreme peeling of the tracheal wall for neoplastic involvement or the necrosis of a parietal neoplastic residual (3). Detailed history, symptoms radiologic and bronchoscopic exams make the diagnosis and if these data are widely known, the therapeutic approach is still debated. Some Authors (5) propose a conservative approach, but the “en bloc” tracheal resection proposed by Grillo (6) is considered the gold standard of treatment. When this approach is not feasible, musculo-cutaneous or muscular flaps result a safe therapeutic option (7, 8). We present a case of tracheal necrosis after total thyroidectomy successfully treated with muscular flap coverage.
Case report
M. F., a young woman 17 years old, affected by papillar thyroid carcinoma, with right latero-cervical adenopathies and lung metastases, underwent elsewhere total thyroidectomy with functional right lymphadenectomy and cranial nerves preservation. An important neoplastic involvement of the right antero-lateral tracheal wall was present intraoperatively and the surgeon must heavily shave the tracheal wall with electrocautery instrument to completely resect the tumour. There was no evidence intraoperatively of thermal damage on the tracheal wall. The early post-operative period was uneventful.
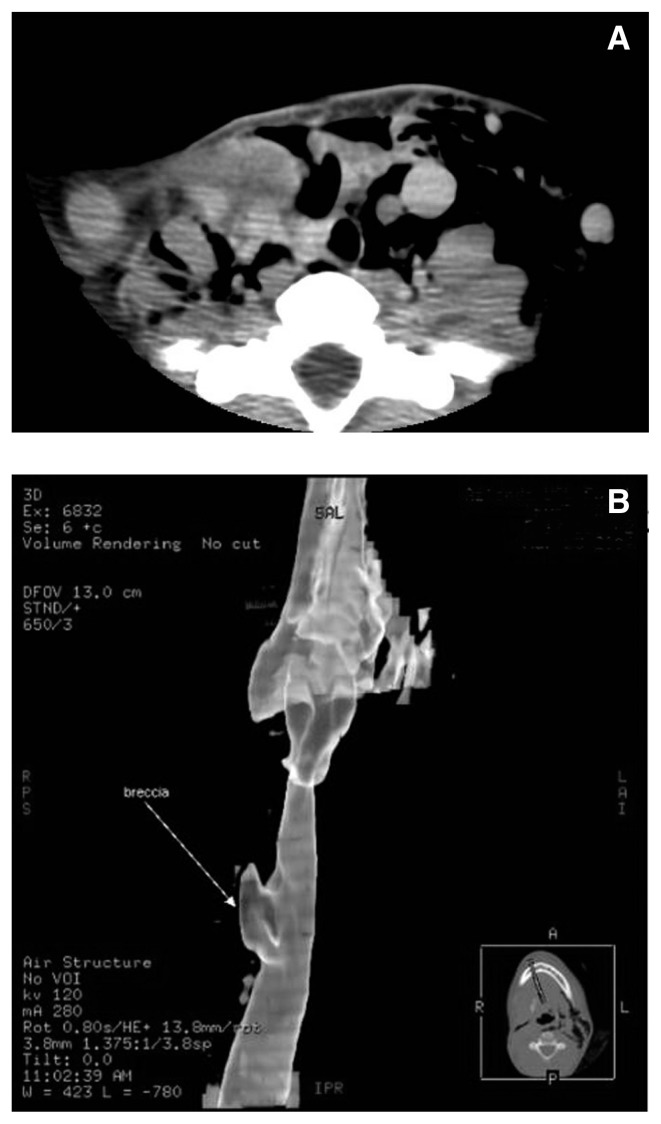
On 7th post-operative day she came to our observation presenting dyspnea, dysphonia, subcutaneous emphysema and cough. Physical examination at the time of re-admission revealed a patient in respiratory distress with subcutaneous emphysema extended on supraclavicular area and the neck bilaterally. A further evaluation of the neck and chest with computed tomography (CT) showed a wide pneumomediastinum with extensive subcutaneous emphysema and a suspected tear on the right lateral tracheal wall 2 cm under the glottis, caudally extended for 3 cm. (Figure 1A–B). A bronchoscopy confirmed these data and revealed important necrotic areas on the tracheal distal wall (Figure 2).
Fig. 1 A, B.
(A) CT image showed extensive subcutaneous emphysema and a wide defect on the right antero-lateral wall of the trachea. (B) 3-D reconstruction with evidence of the tracheal tear (white arrow).
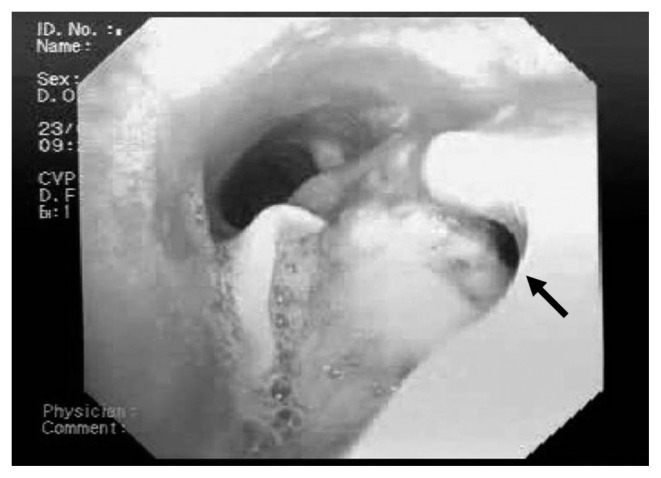
Fig. 2.
Pre-operative bronchoscopy demonstrates an important lack of tissue (black arrow) on the tracheal wall and abundant necrotic tissue on tear edges.
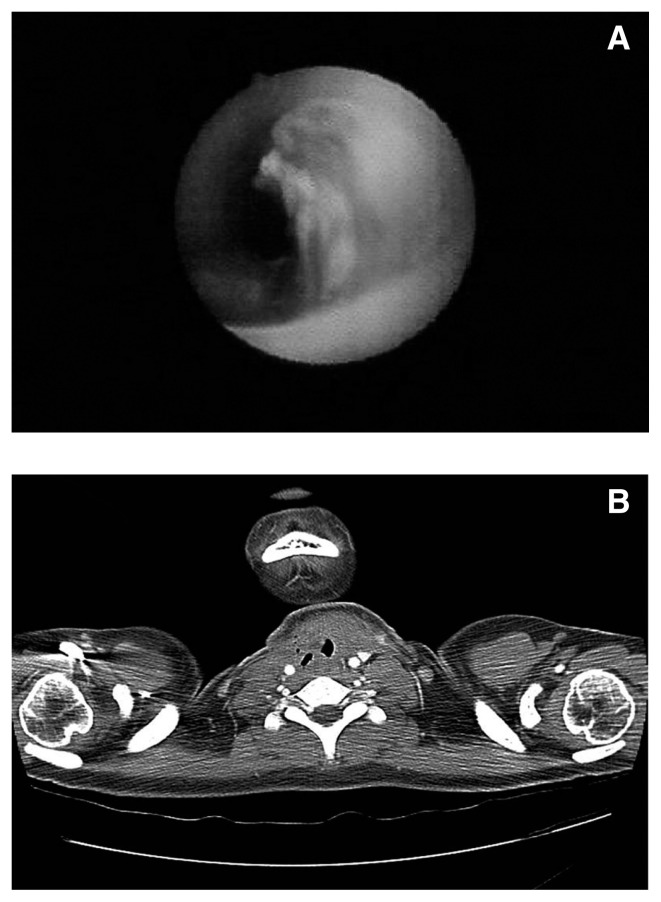
The patient underwent a surgical neck exploration that revealed a 3 cm-wide irregular tracheal defect on the right antero-lateral wall extending from the second tracheal ring down through the fifth tracheal ring with abundant necrotic tissue on tear’s edges. The site, the great extension of the tracheal tear and the wide necrosis contraindicated a primarily repair, as like as the lung metastases were considered a contraindication to a tracheal resection. A muscular flap, using the clavicular part of the left sternocleidomastoid muscle and left and right pre-thyroid muscles was performed, rounded as a scarf on the tracheal defect. After one week of mechanical ventilation with oro-tracheal intubation down to the repaired tear, a bronchoscopic control was done showing the good stability of the new “tracheo-muscle” wall, with early re-epithelialization of the inner muscle part (Figure 3A).
Fig. 3 A, B.
(A) Post-operative bronchoscopy reveals the total closure of the tracheal tear with early re-epithelialization of the inner muscle part. (B) CT image of the airways on 30th post-operative day reveals a normal tracheal tree with minimal residual non functional stenosis.
The patient was discharged home on 15th post-operative day. A neck CT after 1 month (Figure 3B) showed a good repair of the tear and a regular tracheal wall with minimal stenosis and without any functional respiratory deficit. After iodine-radio-induced therapy she is alive at 20-months of follow-up.
Discussion
The well standardized treatment of thyroid neoplasms could be complicated by surrounding structures involvement (20% of patients) (3). The tracheal involvement is the most common. Even if superficial and length - limited in most of the cases, it represents a worse prognostic factor in those of patients (0.5–2%) with intra-mucosal invasion. Tracheal injury after thyroidectomy is very rare, with an incidence of perforation of 0.06%. The trachea may be perforated at the time of surgery or may undergo necrosis in the early post-operative period, as in our report (3). Devascularization of the tracheal wall through thermal coagulation injury, as in our patient, or necrosis of an ischemic neoplastic residual are the most likely causes (3, 4). Acute perforations tend to occur on the lateral region, as in our case, presenting wound infection, subcutaneous emphysema and progressive respiratory failure.
History and symptoms must be highly considered, both with flexible bronchoscopy to visualize the site of lack and neck CT to study the surrounding organs. Surgery must not be delayed, but there is no wide agreement in Literature about the correct surgical approach in these cases. The tracheal repair depends by some factors: patient’s conditions, site and length of the tear and, most of all tissue status, often compromised by the previous surgical resection. Some Authors (1, 5) consider the conservative approach as safe, peeling the tracheal wall and suturing it if damaged. Grillo et al. (6) demonstrated that this approach increases late tracheal lesions rate, e.g. tracheal necrosis, due to surgical and anesthesiological damage with tracheal wall ischemia and parietal neoplastic residual necrosis, as in our case. The same Authors indicate the tracheal resection, better if “en bloc” with the tumour, with end-to-end tracheal anastomosis as the gold standard of therapy in tracheal late rupture (6). The tracheal resection at the onset of the complication, even if remains the gold standard procedure, is not preferable due to a major failure rate (6). When the tracheal resection is not feasible or contraindicated, the use of muscular and musculo-cutaneous flap represents a safe alternative procedure to repair the tracheal defect. Many Authors (7, 8) present their experiences with muscular flap coverage in ENT and thoracic surgery and many are the muscles used: sternohyoid, sternocleido-mastoid with periostal fascia, down to serratus anterior and latissimus dorsi for distal airways defects. This tissue plastically adheres to the airway lesion and permits to maintain its rigidity, obtaining a good result and potentially preventing, with its vascular feeding, further complications (1, 3). In our case we performed successfully a muscular flap coverage due to the patient’s metastatic condition and, most of all, to the great extension of the tracheal lesion and the site of the tear, that contraindicated direct suture and even a tracheal resection.
Conclusion
The tracheal necrosis after total thyroidectomy represents a rare but dangerous and life-threatening complication for the patient and needs an early and correct repair. The gold standard of therapy is the tracheal resection and anastomosis, better en bloc with the thyroid tumour. When this surgical approach is not feasible or contraindicated, a muscular flap transposition could be a safe alternative procedure, in particular for extended lesions, resulting easy to perform, with low complications rate, a good surgical result and a correct airways stabilization.
Footnotes
Competing interest. The authors declare that they have no competing interests.
Authors’ contribution. SS selected the case and wrote the paper; DB and MM collected the case and read and correct the paper; MT and MMe collected and selected the figures for the paper; WG and DA selected the references and read and correct the paper; GG followed the patient in her any further oncologic treatment; DDA, the chief, corrected the final version.
References
- 1.Mazeh H, Suwanabol PA, Schneider DF, Sippel RS. Late manifestation of tracheal rupture after thyroidectomy: case report and Literature review. Endocrine practice. 2012;18:e73–6. doi: 10.4158/EP11344.CR. [DOI] [PubMed] [Google Scholar]
- 2.Iacconi P. Inadvertent tracheal perforation during thyroidectomy. [letter concerning Br J Surg. 2006; 93:55–6] Br J Surg. 2006;93:770–1. doi: 10.1002/bjs.5480. [DOI] [PubMed] [Google Scholar]
- 3.Bertolaccini L, Lauro C, Priotto R, Terzi A. It sometimes happens: late tracheal rupture after total thyroidectomy. ICVTJ. 2012;14:500–1. doi: 10.1093/icvts/ivr126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conzo G, Stanzione F, Della Pietra C, Palazzo A, Candillo G, Fiorelli A, Santini M. Tracheal necrosis, oesophageal fistula: unusual complications of thyroidectomy. Report of two cases and literature review. Ann Ital Chir. 2012;83:259–64. [PubMed] [Google Scholar]
- 5.Mullan GP, Georgalas C, Arora A, Narula A. Conservative management of a major post-intubation tracheal injury and review of current management. Eur Arch Otorhinolaryngol. 2007;264:685–8. doi: 10.1007/s00405-006-0234-4. [DOI] [PubMed] [Google Scholar]
- 6.Grillo HC. Surgery of the trachea. BC Decker; 2004. pp. 249–270. [Google Scholar]
- 7.Asakura K, Shido F, Harabuchi Y, Shirasaki H, Wakashima J, Kataura A. Sternocleidomastoid muscle-clavicle myoosseous flap for single-stage reconstruction of postoperative tracheal defects in patients with invasive thyroid tumor. Three case reports. ORL J Otorhinolaryngol Relat Spec. 1997;59:238–42. doi: 10.1159/000276945. [DOI] [PubMed] [Google Scholar]
- 8.Masuda M, Kamizono K, Ejima M, Fujimura A, Uryu H, Kadota H. Tracheal reconstruction with modified infrahyoid myocutaneous flap. Laryngoscope. 2012;122:992–6. doi: 10.1002/lary.23194. [DOI] [PubMed] [Google Scholar]