Abstract
Aim
Closed treatment of atrophic mandible fractures often results in malunion, pseudoarthrosis and pain. Open reduction and rigid internal fixation (ORIF) is still indicated for displaced atrophic mandible fractures. The Authors report a treatment protocol that allows to gain the best results using reconstruction plates, autologous bone grafting and free fibula flap reconstruction when necessary.
Methods
Retrospective analysis of 15 patients with atrophic mandible fractures who underwent treatment between 2007 and 2011. 7 cases did not receive any treatment because of their general condition, while the others 8 were surgically managed by external approach. In all cases load-bearing osteosynthesis plates with locking screws were used; in 2 of them contextual bone grafts were performed; in 1 case mandible reconstruction needed harvesting a free fibula flap.
Results
In 6 out of 8 cases complete functional and morphological restoration were obtained without any major complication. In 1 case suppurative infection and necrosis of the bone graft occurred, which made necessary its removing, leaving in situ only the reconstruction plate. In another case, during the first year after surgical treatment, atrophic mandible resorption occurred from one angle to the other, resulting in loss of the anchoring reconstruction plate.
Conclusions
ORIF is the gold standard procedure for the of atrophic mandible fractures, because it guarantees best morpho-functional outcomes and predictability. Nevertheless the Authors suggest contextual bone grafting in case of substance loss, or a poor quality bone or for dental implant surgery and free fibula flap in selected cases.
Keywords: Mandibular atrophy, Mandibular fracture, Edentulous mandible, Reconstruction plate, Rigid fixation
Introduction
Improving living conditions has lead to a growth of the life expectancy, shifting to a greater number of elderly and, consequently, to an increased number of age-related diseases, such as fractures of the atrophic mandibles (1). Bone atrophy can be considered as the end stage of the edentulism. Teeth lost brings to a series of biological processes until the leak of the alveolar bone.
The most involved causes are represented by falls, domestic accidents, assaults and car crashes but, differently by a dentate one, an edentulous atrophic mandible results also more vulnerable to very minor traumas, such as those that occur during normal chewing, pathological fracture (i.e. impacted teeth or cysts) (Figure 1).
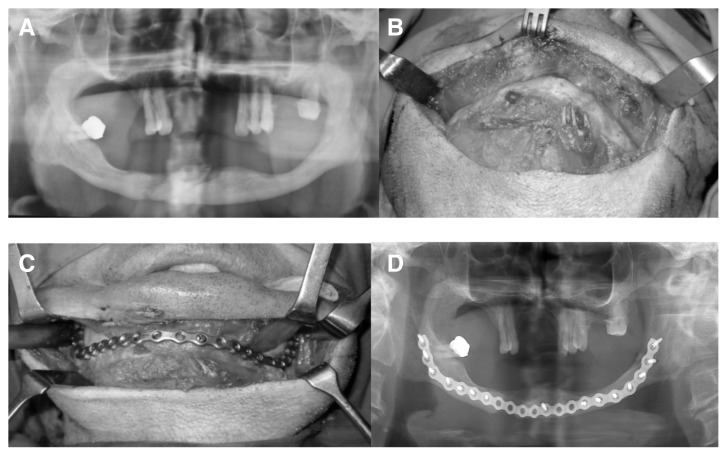
Fig. 1 A, B, C, D.
A case of pathological fracture due to an impacted canine complicated by infection. (A) The OPT before surgical treatment shows the line fracture in corresponding to the impacted canine. (B) Surgical exposure of the site via submandibular approach. (C) Use of a large profile plate (locking reconstruction 2.0 mm plate with 2.4 mm screws) from angle to angle to stabilize the fracture, according to the load-bearing principle. (D) Post-operative panoramic visualizing the reduction of the fracture and the good adaptation of the reconstruction plate to the bone.
Fractures of the atrophic mandibles are often bilateral, more frequently at the body region (2) and have also a decreased ability to heal and high rate of complications. Since ever, atrophic mandible fractures have represented a challenge for the maxillofacial surgeon, in consideration of general (geriatric population mainly involved) (3) and local conditions: reduced vascularized and bone mass, decreased osteogenesis, poor quality bone tissues, smaller cross-sections and contact areas of the fractured ends determine a prolonged healing. A direct relationship between the bony height at the fracture site and the rate of post-operative complications has been demonstrated (4) (Table 1).
Table 1.
RELATIONSHIP BETWEEN THE HEIGHT AT FRACTURE SITE (DEGREE OF ATROPHY) AND SURGICAL COMPLICATION RATE (4).
| MANDIBULAR HEIGHT AT FRACTURE SITE | CLASS OF ATROPHY | COMPLICATIONS RATE |
|---|---|---|
| 16–20 mm | I | ↑ |
| 11–15 mm | II | ↑↑ |
| ≤ 10 mm | III | ↑↑↑ |
Major complications, for instance non-union or fibrous union, occur especially when the height of the site fracture is less than 20 mm (5). High percentage of this negative events (nonunion until 20%) has been reported by the Chalmers J. Lyons Academy first study (6). In the second study realized later by the same academy, even though about a 12.6% of delayed or fibrous unions were registered, open reduction and rigid internal fixation produced better outcomes (7). Thus, according to the literature, observation and closed treatments (circumandibular wires in patients wearing dentures or the use of acrylic maxillary and mandibular prostheses, called Gunning splints) leads more often to negative results: non-union, malunion, functional impairment for chewing, swallowing and speaking, which affect the quality of patients’ life. Moreover, due to their relatively low frequency compared to other type of facial skeleton injuries (less than 1%) (8), many surgeons have limited specific experience. The difficulties in surgical handling and plating, are strictly related to the degree of atrophy, particularly in case of a 20 mm or less thickness of the fracture site. Thus Luhr elaborated a classification related to the difficulty of surgical treatment. In 1996 Luhr et al. (5) reported the first study extended on a great number of patients (n.84) affected by atrophic mandible fractures. They demonstrated that good anatomical reduction and internal rigid fixation guarantee better outcomes than any conservative treatment. This happens because “rigidity seems to be the most important factor in fracture healing, particularly in fractures of the edentulous atrophic mandible”.
Therefore, following the open reduction and stable internal fixation principle, the specific aim of this study is to outline a decision algorithm treatment protocol that allows to reach the best clinical outcomes in management of fractures of the atrophic mandibles, based on specific considerations for each clinical case, especially for previous unsuccessfully treated patients.
Patients and methods
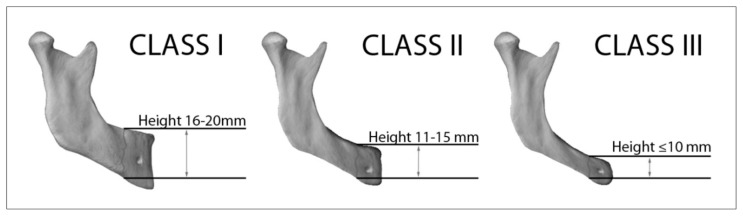
The present study consists of the retrospective analysis of 15 patients (10 males and 5 females) recovered in our Maxillofacial Unit for atrophic mandibular fractures from February 2007 to December 2011. For all of them detailed medical and dental history were taken, clinical and radiological examinations (orthopantomography or CT scan or both, according to the clinical judgment) were performed. Inclusion criteria were: 1) patients with fractures of the edentulous mandible and 2) a bony height ≤20 mm at the site of fracture (radiological revealed) according to the Luhr’s classification (5) (Figure 2; Table 1). All patients gave written consent to participate in scientific studies.
Fig. 2.
Luhr’s classification for fractures of the edentulous atrophic mandible (5).
Data were collected from the medical records of the patients. Causes of fracture included 6 accidental falls, 5 motor vehicle accidents, 3 cases of syncopes, 1 trauma secondary to assault. Clinically patients presented extraoral and intraoral ecchymosis, referred pain and sometimes did not swallow without discomfort. 7 patients out of 15 (46.7%) did not underwent any operation because of contraindications to general anesthesia, while the others 8 (53.3%) were surgically managed by an external approach. Their age ranged from 63 to 85 years. 2 patients (13.3%) had undergone to unsuccessful treatment previously for inadequate fixation and infection. 3 unilateral and 5 bilateral fractures were treated. All fractures were displaced: according to the amount of displacement, 2 were mild, 4 moderate and 2 severe (Table 2). All surgical approaches were extraoral submandibular. Temporary fixation was used to stabilize body segments when needed.
Table 2.
DEMOGRAPHIC DATA AND CLINICAL FEATURES OF 8 PATIENTS AFFECTED BY ATROPHIC MANDIBULAR FRACTURES TREATED WITH 2.0 MM LARGE-PROFILE RECONSTRUCTION TITANIUM PLATE.
| Patients | Sex | Age | Class of atrophy | Site of fracture | Amount of displacement | Previous surgery | Bone graft |
|---|---|---|---|---|---|---|---|
| 1 | M | 74 | II | Body left | Mild | No | No |
| 2 | F | 77 | III | Body left, angle right | Moderate | No | No |
| 3 | M | 68 | I | Angle left | Moderate | Yes (malunion) | Iliac crest |
| 4 | M | 83 | III | Bilateral body | Moderate | No | No |
| 5 | F | 81 | II | Body right | Mild | No | No |
| 6 | M | 67 | III | Bilateral body | Severe | Yes (fistulization, infection) | Fibula |
| 7 | M | 85 | II | Both angles | Moderate | No | No |
| 8 | F | 63 | III | Bilateral Body | Severe | No | Iliac crest |
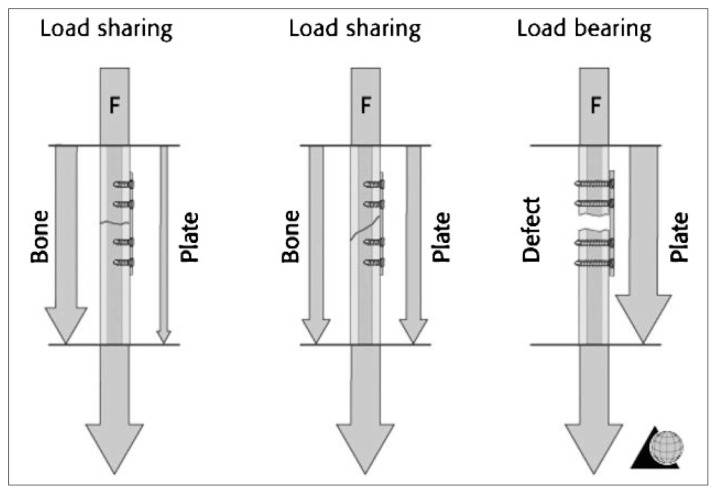
In all cases open reduction and rigid fixation were adopted; according to the load-bearing osteosynthesis principle (Figure 3), a 2.0 mm large-profile reconstruction titanium plate with 2.4 diameter locking screws was used, with at least three screws on either side of the fracture to achieve adequate plate stability (9). The length of plate depended on the type of fracture: from one angle to the symphisis in monolateral fracture, while angle to angle for bilateral fractures and severely atrophic mandible (III Luhr’s class) (Table 1), to fix plates on the buttress system of the mandible. In 5 cases (65%) only load-bearing osteosynthesis plates with locking screws were used. In 2 patients (25%), one case of malunion and another of highly displaced fracture in a severely atrophic mandible, contextual corticomedullary bone grafts were harvested from the iliac crest. The bone graft was indicated in the former to remove the fibrous segment, while to increase the vertical dimension in the latter for the subsequent prosthodontic rehabilitation. Satisfying bony union was reached for both.
Fig. 3.
Schematic representations to show the difference between the load-bearing and the load-sharing principles across a fracture site. In load-sharing fixation the bone and the plate share, equally or not, the working load (chewing forces in the case of mandible), while in load-bearing fixation the functional load is completely sustained by the plate.(Data from: Cienfuegos R, Cornelius CP, Ellis E 3rd, Kushner G. CMF mandible - load sharing versus load bearing - different levels of force distribution - AO Surgery reference. AO Foundation. Available at: http://www.aocmf.org/surgery-ref.aspx.).
Another case (12.5%) was a 67 years old male, affected by a bilateral (body regions) fracture of a severely atrophic mandible (class third of Luhr’s classification), happened for a syncopal episode, already treated using miniplates, which resulted in inadequate bony fixation and consequent non-union, infection and fistulization into the oral cavity. The patient, who was obviously edentulous, had also a significant reduced vertical dimension as a result of the severe degree of mandibular atrophy, but he expressed the desire to obtain good oral rehabilitation and aesthetic results by dental implant surgery. Considering the absence of general or specific contraindications to the operation, it was decided for harvesting a free fibula flap to improve bony healing, blood supply, immune response to local infections and vertical dimension for prosthetic purpose.
In all cases, pre-operative antibiotic prophylaxis was administered to each patient.
After surgery, patients were discharged on the second day, previous a post-operative panoramic radiograph to assess the quality of fracture reduction.
Results
Postoperative follow-up was managed by clinical and radiographic evaluations to demonstrate union of fracture fragments, in the immediate postoperative period, at 1month, at 6 months and 1 year. In 6 out of 8 cases (75%), 4 males and 2 females, complete fracture healings and morphological restorations were obtained without any major complication. 4 of them were treated only by rigid fixation using a reconstruction plate. For 1 case an iliac crest graft was harvested to improve a severe displaced fracture healing. Finally, also the patient who was treated by a free fibula flap achieved an optimal mending, completing the surgical procedure by oral rehabilitation with dental implants surgery, reaching a good functional and esthetic result as he required.
Although the antibiotic prophylaxis administered to each patient, during the follow-up suppurative infection and necrosis of the bone graft occurred in one case (12.5%), which made necessary a second operation to remove the infected tissues and make a surgical toilette, leaving only the titanium reconstruction plate (Table 3). In another case (12.5%), about a year after the surgical treatment, mandible resorption occurred from one angle to the other, causing loss of the anchoring reconstruction plate, so that its removing was necessary.
Table 3.
INCIDENCE OF COMPLICATIONS IN 8 PATIENTS AFFECTED BY ATROPHIC MANDIBULAR FRACTURES TREATED WITH RECONSTRUCTION PLATE BY EXTERNAL APPROACH.
| COMPLICATIONS | CASES (%) |
|---|---|
| Malunion | 0 (0%) |
| Non-union | 0 (0%) |
| Screw loss | 0 (0%) |
| Plate exposure | 0 (0%) |
| Damage of marginalis mandibulae nerve | 0 (0%) |
| Damage of infeorior alveolar nerve | 0 (0%) |
| Bone resorption | 1 (12.5%) |
| Infection | 1 (12.5%) |
There were no other complications related to the hardware: no case of screws loss, nor exposure of the bone plate or its instability.
Considering the external incision and the reduced mandibular thickness, no damage to the marginalis mandibulae nerve (branch of the VII) or to the alveolar inferior nerve (V) was revealed by clinical evaluations during all the follow-up period, following no any motor or sensory disturbance.
No maxillary-mandibular fixation was necessary and all patients were able to eat a soft diet few days after surgery.
Discussion and conclusions
There are some controversies regarding the best treatment options for fractures of atrophic mandibles, due to their low incidence if compared to other facial skeleton injuries, to limited bony quantity and quality, to general condition of elderly patients (10, 11). Moreover, other local factors influence the outcomes, especially lowering in blood supply (almost guaranteed by soft tissues attached to bones as showed by Bradley) (12, 13), which could justify a conservative approach. This was particularly true during the 1970s, when only non-rigid fixation was performed and blood supply was retained the most important agent to determine bone healing. On the contrary, experimental orthopedic studies done on dogs clearly demonstrated how a stable internal fixation was significant to ensure the ossification of homograft placed under compression, although a remarkably reduced vascularization to the site (14). Similar results derived from the comparison between fixed and non-fixed rib and skull onlay bone grafts positioned to the mandible in adult sheeps: 20 weeks later more bone volume was found in stabilized graft (15, 16). Even if a less aggressive surgical approach is possible, there is no certainty about how much blood supply can be preserved, although more technical difficulties: it does not give the possibility to visualize adequately bony fragments in order to obtain the best anatomical reduction and, consequently, a better rigid internal fixation (the fixation modality is really the unique variable that can be improved to gain good healing) (8), especially for a large profile plate. It can be assumed that much of the bone vascularization can be jeopardized in order to provide a more satisfying fixation, using an open approach to obtain direct visualization of the fragments, perfect reduction and excellent stability (5, 7, 17, 18). Furthermore, avoiding maxillary-mandibular fixation and allowing free mandibular movements, normal speech and immediate soft diet determine also much less discomfort to the patient.
A very discussed field is also represented by intraoral versus extraoral approach. Part of the literature suggests the intraoral solution as better18,19,20 while another part the extraoral (7, 21, 22). There is no doubt that the intraoral rout avoids both the risk of damaging the marginalis branch of the facial nerve and the external scar, allowing 1-layer mucosal closure, but the external access ensures an adequate fragments exposure and consequently a more careful surgical procedure (especially for making possible the adaptation of a large profile plate) (23). Therefore the external approach reduces the risk of contamination by oral microbes and prevents any injury to the inferior alveolar bundle, usually on top of the alveolar crest of atrophic mandibles. Clinical outcomes from this study support extraoral access as the one that achieves the best percentage of success, as well as placement of bone grafts when indicated to enhance regional conditions (bone healing, increase of blood supply and local immune response against infections). Afterwards this last solution would also permit a transoral access, even the risk to develop infections and, consequently, non-unions still remains (24).
Another technical issue is represented by which type of internal fixation is best. The introduction of mini-plates with monocortical screws in dentulous mandibular fractures have been represented a revolution, leading to the abandonment of compression plate (first used by Luhr to treat edentulous mandibular fractures) (5). Considering the reduced bite forces characterizing the edentulous mandibles, many Authors describe the best outcomes by using miniplates (2, 19, 25). Unfortunately these studies do not indicate the atrophy degree, fundamental to correctly analyze clinical data. As a matter of fact, other Authors report fractures of miniplates in dentulous atrophic mandible (7, 19, 26) realistically caused from fatigue failure due to cyclic loading and deformation (amplified by the minimal bone buttressing of these mandibles) which leads to break the plate. While a second miniplate widely increases the resistance to deformation, this requires adequate bone height (27, 28), usually not present in the atrophic mandible. Moreover, even if two plates could be accommodated, the too short distance between them do not produce an effective strengthening in reconstruction stability. However, according to the AO (29, 30), application of the load-bearing principle as reconstruction plate is recommended (Figure 4). Such plate must be positioned across the fracture site, secured with screws where the bone is stable and healthy, due to the fact that the mandible can share none or very little load in correspondence to the line fracture, caused by the lack of buttressing related to the atrophy (27, 28). In other words, a small bone requires a big plate and this work is in line with the AO recommendations. Naturally, as assessed by Müller et al. (24), the screws should be placed far away the fracture line, best in the angle and symphyseal regions (anatomical bone buttresses), possibly covering the plate with muscle tissue to avoid easy exposures or wound dehiscences. According to the literature, plating the lower border instead of the lateral surface is also feasible in order to reduce the risk of wound dehiscence and plate exposure (that prelude to infection and non-union), especially in high degree atrophy mandible (Luhr’s class III), although plate contouring is more difficult to realize (8).
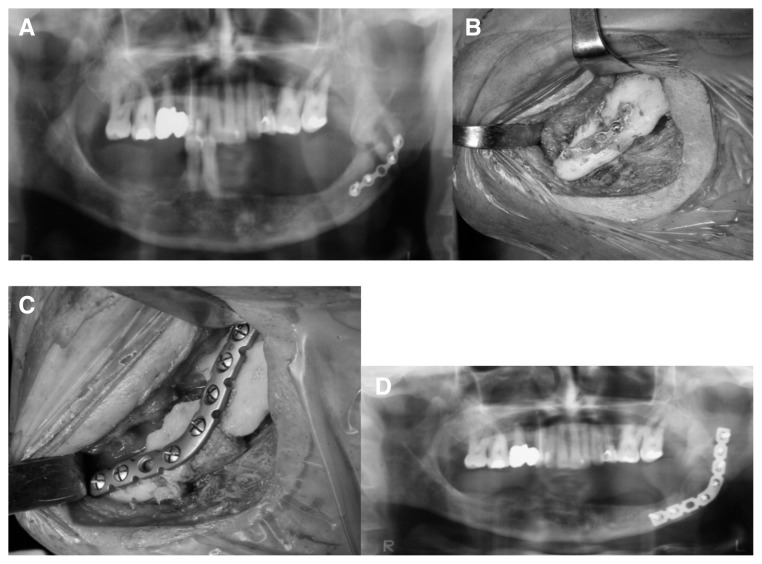
Fig. 4 A, B, C, D.
A case of an angle fracture malunion due to inadequate fixation (miniplate). (A) Pre-treatment panoramic radiograph showing malunion after internal fixation by one miniplate. (B) Intra-operative view showing the treatment with a 1.00 mm plate: evidence of fibrous tissue between the two fragments of the fracture. (C) Intra-operative view after the resection of the fibrous tissue followed by the reconstruction with an iliac crest bone graft and a rigid fixation with a macroplate. (D) Postoperative panoramic demonstrating the reduction and the fixation of the fracture provided by the reconstruction plate.
While Luhr had obtained high percentage of solid union (96.5%) (5) using compression plates to stabilize atrophic mandible fractures, later locking plate/screw systems became available, which is the system used for this clinical research. They provide numerous advantages: not perfectly plate adaptation to the bone surface required (31), with consequent easier positioning, better vascularization of the cortical bone (32) and, thus better outcomes. Therefore, these locking systems provide more stability than the standard hardware (33), making possible to use smaller plates and decrease the rate of postoperative infection and failure, thanks to a reduced tendency for locking-head screws to be loosen under cyclic loading conditions (34).
As to immediate bone grafting as a treatment option, the literature reveals it was used in case of non-united and malunited fractures (34) because of its osteoconductive, osteoinductive and osteogenetic properties, or in order to achieve adequate stabilization when plate and screws were not available as fixation system (18, 35). Today, reaching the rigid fixation thanks to reconstruction plates and screw locking systems, the rationale for adopting a graft solution seems to be the bony healing facilitation and the bone augmentation for dental-implant rehabilitation (26, 36, 37). So that, we suggest iliac crest graft as a valid solution to improve body union, especially after failing of previous operations (such as in ostheosynthesis of atrophic mandible fracture by miniplates), to fill bony gaps for substance loss or to enable implantation. Moreover, for particular selected patients whose medical and vascular conditions make it possible, harvesting a free fibula flap represents the therapeutical pathway to solve harder cases. In fact, this procedure guarantees a new and more efficient soft tissue coverage and increases also the blood supply of the receiving site, very useful in case of severely atrophic mandible, poor quality of soft covering tissue, considerable bone loss, patients claiming implantation or particular aesthetic results. The presence of a new vascular supply to the site, produced by the micro-surgical revascularitazion of the flap to the recipient vessels, improves not only the healing process but also the local immune response. These biological effects allow the oral surgical approach, if indicated, and the treatment of previous failed operations, even if signs of infections and fistulization are clinically revealed, as it was in one case of this report.
As a result of this study and in agreement with most authors, considering the advances in the care of elderly and the improved pre and post-operative management, open reduction and rigid internal fixation (ORIF), according to load-bearing principle, guarantees the best bone healing and the quickest return to function, avoiding uncomfortable prolonged inter-maxillary fixation. Consequently this procedure could be considerated as the gold standard for the atrophic mandible fractures. Nevertheless we suggest contextual iliac crest bone grafting in case of substance loss, comminuted fractures, severely atrophied mandibles, failure of previous treatments, poor quality bone or to create good local conditions for dental implant surgery. We propose a free fibula flap as primary reconstruction in case of a considerable bone loss, not healthy soft tissues, severely atrophied mandibles, infected complications of inadequate previous treatments, implant surgery with aesthetic concerns, everywhere, health conditions of the patient allows for it. Observation and conservative treatment (wiring dentures or customized Gunning style splints) still remains the reasonable options for the patients who could not undergo to general anesthesia for medical reasons, even though they often hesitate in misalignments, malunions or non-unions of the fragments.
Footnotes
Best Communication Award at the XXV National Congress of the “Società Polispecialistica Italiana dei Giovani Chirurghi”, Bari, 13–15 June 2013
Conflict of interest. The authors declare no conflict of interest.
Funding. No financial support was received.
References
- 1.Ellis E, 3rd, Price C. Treatment protocol for fractures of the atrophic edentulous mandible. J Oral Maxillofac Surg. 2008;66:421–35. doi: 10.1016/j.joms.2007.08.042. [DOI] [PubMed] [Google Scholar]
- 2.Mugino H, Takagi S, Oya R, Nakamura S, Ikemura K. Miniplate osteosynthesis of fractures of the edentulous mandible fractures. Clin Oral Investig. 2005;9:266–70. doi: 10.1007/s00784-005-0012-5. [DOI] [PubMed] [Google Scholar]
- 3.Marciani RD. Invasive management of the fractured atrophic edentulous mandible. J Oral Maxillofac Surg. 2001;59:792–95. doi: 10.1053/joms.2001.24736. [DOI] [PubMed] [Google Scholar]
- 4.Wittwer G, Adeyemo WL, Turbani D, Ploder O. Treatment of atrophic mandibular fractures bases on the degree of atrophy-experience with different plating systems: a retrospective study. J Oral Maxillofac Surg. 2006;64:230–34. doi: 10.1016/j.joms.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 5.Luhr HG, Reidick T, Merten HA. Results of treatment of fractures of the atrophic edentulous mandible by compression plating a retrospective evaluation of 84 consecutive cases. J Oral Maxillofac Surg. 1996;54:250–54. doi: 10.1016/s0278-2391(96)90733-8. [DOI] [PubMed] [Google Scholar]
- 6.Bruce RA, Strachan DS. Fractures of the edentulous mandible: The Chalmers J. Lyons Academy study. J Oral Surg. 1976;34:973. [PubMed] [Google Scholar]
- 7.Bruce RA, Ellis E. The second Chalmers J. Lyons Academy study of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1993;351:904–11. doi: 10.1016/s0278-2391(10)80113-2. [DOI] [PubMed] [Google Scholar]
- 8.Madsen MJ, Haug RH. A biomechanical comparison of 2 techniques for reconstructing atrophic edentulous mandible fractures. J Oral Maxillofac Surg. 2006;64:457–65. doi: 10.1016/j.joms.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 9.Pereira-Filho VA, da Silva BN, Nunes Reis JM, Spin-Neto R, Real Gabrielli MF, Monnazzi MS. Effect of the number of screws on the stability of locking mandibular reconstruction plates. Int J Oral Maxillofac Surg. 2013;42:732–35. doi: 10.1016/j.ijom.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Seper L, Piffko J, Joos U, Meyer U. Treatment of fractures of the atrophic mandible in the elderly. J Am Geriatr Soc. 2004;52:1583–84. doi: 10.1111/j.1532-5415.2004.52430_5.x. [DOI] [PubMed] [Google Scholar]
- 11.Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865–77. doi: 10.1016/j.jamcollsurg.2006.08.026. [DOI] [PubMed] [Google Scholar]
- 12.Bradley JC. Age changes in the vascular supply of the mandible. Br Dent J. 1972;132:142–44. doi: 10.1038/sj.bdj.4802812. [DOI] [PubMed] [Google Scholar]
- 13.Bradley JC. A radiological investigation into the age changes of the inferior dental artery. Br J Oral Surg. 1975;13:82–90. doi: 10.1016/0007-117x(75)90027-x. [DOI] [PubMed] [Google Scholar]
- 14.Petrokov V. Die acromio-claviculare Lucation. Bruns Beitrklin Chir. 1959;199:143–77. [PubMed] [Google Scholar]
- 15.LaTrenta GS, McCarthy J, Breitbart AS, et al. The role of rigid skeletal fixation in bone graft augmentation of the craniofacial skeleton. Plast Reconstr Surg. 1989;84:578–88. [PubMed] [Google Scholar]
- 16.Lin KY, Bartlett SP, Yaremchuk M, et al. The effect of rigid fixation on the survival of onlay bone grafts: An experimental study. Plast Reconstr Surg. 1990;86:449–56. doi: 10.1097/00006534-199009000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Kunz C, Hammer B, Prein J. Fractures of the edentulous mandible: management and complications (in German) Mund Kiefer Gesichtschir. 2001;5:227–32. doi: 10.1007/s100060100304. [DOI] [PubMed] [Google Scholar]
- 18.Obwegeser HL, Sailer HF. Another way of treating fractures of the edentulous mandible. J Maxillofac Surg. 1973;1:213–221. doi: 10.1016/s0301-0503(73)80045-1. [DOI] [PubMed] [Google Scholar]
- 19.Iatrou I, Samaras C, Lygidakis NT. Miniplate osteosynthesis for fractures of the edentulous mandible: a clinical study, 1989–1996. J Craniomaxillofac Surg. 1998;26:400–4. doi: 10.1016/s1010-5182(98)80075-9. [DOI] [PubMed] [Google Scholar]
- 20.Alpert B. Discussion of Eyrich GK, Gratz KW, Sailer HF. Surgical treatment of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1997;5:1087–8. doi: 10.1016/s0278-2391(97)90284-6. [DOI] [PubMed] [Google Scholar]
- 21.Champy M, Wilk A, Schnebelen JM. Treatment of mandibular fractures by means of osteosynthesis without intermaxillary immobilization according to FX Michelet’s technique [in German] Zahn Mund Kieferheilkd Zentralb. 1975;63:339–41. [PubMed] [Google Scholar]
- 22.Toma VS, Mathog RH, Toma RS, et al. Transoral versus extraoral reduction of mandible fractures: A comparison of complication rates and other factors. Otolaryngol Head Neck Surg. 2003;128:215–19. doi: 10.1067/mhn.2003.59. [DOI] [PubMed] [Google Scholar]
- 23.Madsen MJ, Haug RH, Chrstensen BS, Aldridge E. Management of atrophic mandible fractures. Oral Maxillofac Surg Clin North Am. 2009;2:175–83. doi: 10.1016/j.coms.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 24.Müller S, Burgers R, Ehrenfeld M, Gosau M. Macroplate fixation of fractures of the edentulous atrophic mandible: immediate function and masticatory rehabilitation. Clin Oral Invest. 2011;15:151–156. doi: 10.1007/s00784-009-0375-0. [DOI] [PubMed] [Google Scholar]
- 25.Thaller SR. Fractures of the edentulous mandible: a retrospective review. J Craniofac Surg. 1993;4:491–4. doi: 10.1097/00001665-199304000-00008. [DOI] [PubMed] [Google Scholar]
- 26.Eyrich GK, Gratz KW, Sailer HF. Surgical treatment of fractures of the edentulous mandible. J Oral Maxillofac Surg. 1997;55:1081–7. doi: 10.1016/s0278-2391(97)90284-6. [DOI] [PubMed] [Google Scholar]
- 27.Choi B-H, Huh J-Y, Suh C-H, et al. An in vitro evaluation of miniplate fixation techniques for fractures of the atrophic edentulous mandible. Int J Oral Maxillofac Surg. 2005;34:174–177. doi: 10.1016/j.ijom.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 28.Sikes JW, Smith BR, Mukherjee DP. An in vitro study of the effect of bony buttressing on fixation strength of a fractured atrophic edentulous mandible model. J Oral Maxillofac Surg. 2000;58:56–61. doi: 10.1016/s0278-2391(00)80017-8. [DOI] [PubMed] [Google Scholar]
- 29.Spiessl B. Internal fixation of the mandible. New York: Springer-Verlag; 1989. p. 23. [Google Scholar]
- 30.Schilli W, Stoll P, Bähr W, et al. Mandibular fractures. In: Prein J, editor. Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group. New York: Springer; 1998. p. 87. [Google Scholar]
- 31.Haung RH, Street CC, Goltz M. Does plate adaptation affect stability? A biomechanical comparison of locking and non-locking plates. J Oral Maxillofac Surg. 2002;60:1319–26. doi: 10.1053/joms.2002.35732. [DOI] [PubMed] [Google Scholar]
- 32.Prein J, Rahn BA. Scientific and technical background. In: Prein J, editor. Manual of Internal Fixation in the Cranio-Facial Skeleton: Techniques Recommended by the AO/ASIF Maxillofacial Group. New York: Springer; 1998. p. 9. [Google Scholar]
- 33.Gutwald R, Büscher P, Schramm A, et al. Biomechanical stability of an internal mini-fixation system in maxillofacial osteosynthesis. Med Biol Eng Compu. 1999;37( Suppl 2):S280–6. [Google Scholar]
- 34.Sikes JW, Smith BR, Mukherje DP, et al. Comparison of fixation strengths of locking head and conventional screws. J Oral Maxillofac Surg. 1998;56:468–73. doi: 10.1016/s0278-2391(98)90715-7. [DOI] [PubMed] [Google Scholar]
- 35.Thoma KH. Progressive atrophy of the mandible complicated by fractures: its reconstruction. Oral Surg. 1960;13:4–11. doi: 10.1016/0030-4220(60)90386-8. [DOI] [PubMed] [Google Scholar]
- 36.Miloro M, Quinn PD. Prevention of recurrent pathologic fracture of the atrophic mandible using inferior border grafting: report of two cases. J Oral Maxillofac Surg. 1994;52:414–20. doi: 10.1016/0278-2391(94)90453-7. [DOI] [PubMed] [Google Scholar]
- 37.Louis P, Holmes J, Fernandes R. Resorbable mesh as a containment system in reconstruction of the atrophic mandible fracture. J Oral Maxillofac Surg. 2004;62:719–23. doi: 10.1016/j.joms.2003.12.012. [DOI] [PubMed] [Google Scholar]