INTRODUCTION
Adolescent brain development
The brain undergoes significant structural and functional changes between childhood and adolescence, with maturation commencing in early adulthood (Pfefferbaum et al., 1994). Gray-matter volume generally decreases after puberty, which has been linked to elimination of weak synaptic connections. At the same time, white-matter fiber tracts appear to continue developing, which allows for more efficient and rapid communication between brain regions (Giedd, 2004; Lebel et al., 2012). Maturation typically begins in lower-order sensorimotor regions, while brain regions associated with higher-order cognitive functioning (e.g., frontal-subcortical brain regions) develop later in adolescence (Sowell et al., 1999, 2004; Shaw et al., 2008; Giedd and Rapoport, 2010; Stiles and Jernigan, 2010). Healthy brain development throughout childhood and adolescence is important for optimal neurocognitive performance, with even subtle changes in neurodevelopmental trajectories (e.g., changes in brain structural volume, cortical thickness, demyelination) affecting cognitive, emotional, and social functioning (Nagy et al., 2004; Casey et al., 2008). Altered brain development due to exposure of neurotoxins during adolescence, particularly alcohol, could set the stage for cognitive problems into adulthood, conferring functional consequences throughout life.
Prevalence of adolescent alcohol use and drinking patterns
Alcohol is the most commonly used substance during adolescence. According to the 2013 Monitoring the Future Study, 30% of youth in the United States have used alcohol by eighth grade. These rates more than double during adolescence, with 69% of adolescents reporting alcohol use by the time they graduate high school. Heavy episodic drinking is also common among youth, with 24% of 12th-graders endorsing binge drinking (i.e., four or more drinks for females and five or more drinks for males) in the past 2 weeks and 28% admitting being drunk in the past 30 days (Johnston et al., 2013). Given the substantial neural development occurring during this time period, along with findings on neurotoxic associates of alcoholism in many adult studies (for review, see Sullivan and Pfefferbaum, 2005; Oscar-Berman and Marinkovic, 2007), further exploration of the impact of alcohol use on brain maturational changes is critical.
This chapter will review the most recent literature regarding the effects of adolescent alcohol use on neurocognition. We will present data from neuropsychologic and neuroimaging studies examining the relationship between alcohol use during adolescence and brain structure and function.
BRAIN STRUCTURAL CHANGES IN ADOLESCENTALCOHOL USE
Gray-matter volume
Brain regions that undergo significant neurodevelopment during adolescence (e.g., cerebral cortex, particularly the prefrontal region; limbic system; and cerebellum) have been identified as being vulnerable to the effects of alcohol use during adolescence (Squeglia et al., 2009a).To elucidate the effect of alcohol use on adolescent gray-matter development, several cross-sectional magnetic resonance imaging (MRI) studies have been completed focusing on these regions.
The hippocampus has been of interest because of its involvement in memory consolidation. The first investigations of the effect of alcohol use on human adolescent hippocampi reported that adolescents and young adults (ages 13–21) diagnosed with alcohol use disorders had smaller bilateral hippocampal volumes than demographically matched controls; those initiating drinking at a younger age and who had a longer duration of alcohol use disorder had even smaller hippocampal volume (De Bellis et al., 2000). Another study (Nagel et al., 2005) reported similar results, with smaller left hippocampal volumes observed in alcohol-using adolescents compared to controls, even after excluding teens with co-occurring conduct disorder. However, hippocampal volume did not correlate with alcohol use (i.e., age of onset of regular drinking, years of regular drinking, drinks consumed per month, alcohol withdrawal symptoms, estimated typical peak blood alcohol concentration, or lifetime number of abuse/dependence criteria), suggesting possible premorbid differences between groups in hippocampal volume. Taken together, these studies suggest that the hippocampus plays a role in alcohol use disorders among adolescents; however, it is unclear if aberrations in hippocampal volume precede, or are a consequence of, alcohol use.
The frontal lobe is associated with higher-order executive functioning, emotional regulation, integration of novel stimuli, and cognitive flexibility. In adults, heavy alcohol use is associated with smaller prefrontal regions (Pfefferbaum et al., 1997). Initial findings in adolescent populations have found that the prefrontal cortex may be more vulnerable to the effects of alcohol than other brain regions, because this area of the brain continues to develop throughout adolescence and young adulthood. Significantly smaller gray- and white-matter volume has been reported in the prefrontal cortex in adolescents with comorbid alcohol use and psychiatric disorders when compared with demographically matched controls (De Bellis et al., 2005). These findings were replicated in a study examining adolescents who did not meet criteria for comorbid mood or attention disorders (Medina et al., 2008). A gender by alcohol interaction was found, with alcohol-dependent girls having smaller prefrontal cortex and white-matter volumes than controls, and alcohol-dependent boys having larger prefrontal and white-matter volumes than controls. These findings suggest that gender may moderate the relationship between adolescent alcohol use on prefrontal neuromaturation, with females having more pronounced negative sequelae from continued drinking.
The cerebellum, which plays a crucial role in both motor and cognitive functions, has also been associated with alcohol-related damage (Sullivan and Pfefferbaum, 2005); however, the effect of alcohol use on adolescent cerebellar structure is less clear. In a group of healthy, non-alcohol use-disordered teens, greater binge drinking during adolescence was linked to smaller cerebellar volumes, above and beyond variability attributable to risk factors for binge drinking (Lisdahl et al., 2013). These findings replicated previous work showing boys with an alcohol use disorder had smaller cerebellar volumes than control boys.
Although these studies are not prospective in nature, they suggest smaller gray-matter volume is related to alcohol use, whether it is as a predisposing factor or a consequence of heavy drinking. The underlying biologic mechanism of alcohol-related changes in brain development remains unclear and speculative without longitudinal study.
Cortical thickness
Normal adolescent brain development involves substantial cortical thinning, which has been linked to elimination of weak synaptic connections (Giedd, 2004; Stiles and Jernigan, 2010). Yet, limited work has examined how alcohol affects normal cortical thinning during this developmental period. Squeglia and colleagues (2011b) examined how heavy episodic drinking in adolescents aged 16–19 related to indices of cortical thickness. Binge-by-gender interactions were seen for cortical thickness in four left frontal brain regions, where female bingers had thicker cortices than female controls and male bingers had thinner cortices than male controls. Thicker left frontal cortices (i.e., less mature cortices) corresponded with poorer visuospatial, inhibition, and attention performances for female bingers and worse attention for male bingers. The finding that female drinkers had thicker cortices than male drinkers is particularly notable, considering female cortices begin thinning 1–2 years earlier than males on average (Giedd, 2004; Lenroot and Giedd, 2006), and could suggest an even greater deleterious effect of drinking on female brain maturation than statistical comparisons indicated. Longitudinal investigations are needed to elucidate the temporal sequence of events, as well as the underlying mechanism driving cortical thinning during adolescence.
White-matter integrity
White matter allows for efficient information processing and quick communication between cortical regions. Unlike gray-matter maturation, which follows an inverted U-shaped curve with reductions in cortical volume beginning in preadolescence (Pfefferbaum et al., 1994) and continuing throughout early adolescence (Giedd et al., 1999), white matter continues to increase linearly in volume until late adolescence and early adulthood (Lebel and Beaulieu, 2011). Structural MRI studies have found smaller overall white-matter volumes in adolescents with alcohol use disorders compared to matched controls, particularly prefrontal cortex white matter (De Bellis et al., 2005), although there is some evidence that the pattern varies by gender, with female drinkers showing smaller prefrontal volumes than males (Medina et al., 2008).
Diffusion tensor imaging (DTI) has provided a way to look at more subtle changes in white-matter fiber structure, which may be more appropriate for this developmental time period. Two common indices of the integrity of a fiber tract, fractional anisotropy (FA) and mean diffusivity (MD), provide an inference of white-matter coherence, compactness, and directional dependence of fiber structure (Le Bihan, 2003). Typically, higher FA and lower MD are seen with healthy white-matter development (Lebel et al., 2012). Given the more subtle differences (e.g., myelination, intracellular or extracellular fluid differences) that may be occurring during this window of development, micro-structural changes may not be observable with traditional MRI, and therefore studies have focused on FA and MD.
Differences in white-matter integrity have been found in adolescent binge drinkers when compared to healthy controls. Specifically, binge drinkers (approximately age 18) showed less white-matter integrity (i.e., lower FA) than controls in several white-matter regions, including cortical and subcortical projection fibers. Lower FA in six of these regions was linked to severity of substance use variables, specifically greater lifetime hangover symptoms and higher estimated peak blood alcohol concentrations (McQueeny et al., 2009). Worse white-matter integrity has also been found in adolescent marijuana users (ages 16–19) with co-occurring alcohol use in widespread fiber tracts across the brain, including cortical and subcortical tracts, along with corpus callosum (Bava et al., 2009, 2010). To disentangle the relationship between binge drinking and marijuana use during adolescence, Jacobus et al. (2009) examined white-matter integrity in 42 adolescents (ages 16–19) who were classified as binge drinkers, marijuana users who also were binge drinkers, and matched controls with minimal substance use. Both substance-using groups showed poorer white-matter health compared to non-using controls; however, in several regions (i.e., superior corona radiata, inferior fronto-occipital fasciculus, middle cerebellar peduncle, and the superior longitudinal fasciculus), binge drinkers demonstrated poorer white-matter health compared with the binge+marijuana users and controls (Jacobus et al., 2009), suggesting alcohol may have a more deleterious effect on white-matter maturation than marijuana.
Poorer white-matter integrity may be both a precursor and a consequence of heavy drinking. In 11–15-year olds who had never engaged in alcohol use, youth with positive family history of alcohol use disorders had poorer white-matter integrity in cortical and subcortical areas, and poorer performance on a task of delay discounting and reaction time when compared with youth who had no family history of alcohol use disorders (Herting et al., 2010). These pre-existing differences in white-matter integrity may contribute to future substance use and risk-taking behaviors. For example, lower white-matter integrity measured in 16–19-year old adolescents was related to more self-reported substance use and delinquency or aggression at an 18-month follow-up, highlighting the importance and potential clinical utility of the observed cross-sectional differences discussed above (Jacobus et al., 2013). In a prospective study (Bava et al., 2013), alcohol use from ages 18 to 20 predicted poorer white-matter integrity at follow-up 1.5 years later in young adults, suggesting that regular heavy alcohol use over development likely has deleterious effects on brain tissue above and beyond baseline differences that may relate to genetic predispositions.
BRAIN FUNCTION DIFFERENCES IN ADOLESCENTALCOHOL USERS
Functional MRI (fMRI) is a widely used, non-invasive, safe technique that estimates brain activation by measuring differences in blood oxygen level-dependent (BOLD) signals between pairs of experimental conditions. Higher BOLD response contrast signal indicates regions of the brain with greater neural activity to one condition compared with another.
Tapert and colleagues (2004c) found that adolescents who drank heavily for 1–2 years showed greater brain response than controls during a spatial working-memory task in bilateral parietal cortices, with lower response than controls in other regions, including the left precentral gyrus and bilateral cerebellar areas, despite no behavioral differences on task performance. This finding was more pronounced in adolescents who reported more severe withdrawal and hangover symptoms and had greater lifetime alcohol consumption. These abnormalities, in spite of similar task performance, indicate that subtle neural reorganization might occur in heavy-drinking adolescents early in their drinking trajectory. In contrast to these findings, alcohol-dependent female adolescents with 4–5 years of drinking history exhibited significantly less BOLD response than controls during the same spatial working-memory task in parietal and prefrontal regions of the brain (Tapert et al., 2001). The alcohol-dependent women also performed worse than controls on spatial working-memory trials, which was associated with greater alcohol withdrawal symptomatology, lower spatial working-memory response in the right parietal cortex, and poorer scores on neuropsychologic tests of memory and cognitive flexibility (Tapert et al., 2001). Although adolescents with shorter drinking histories were able to perform similarly to controls on spatial working-memory tasks despite differential neural activation (Tapert et al., 2004c), adolescents who had more long-term alcohol exposure showed greater behavioral deficits (Tapert et al., 2001). This suggests that the brain may initially be resilient to neural insults or compensate for them, whereas continued alcohol use may more severely interfere with normal neural functioning.
Adolescent drinkers differ from controls on tasks of verbal encoding, specifically, learning of novel word pairs. Relative to controls, 16–18-year old binge drinkers showed greater response in right superior frontal and bilateral inferior parietal cortices, but less response in occipital cortex during verbal encoding, suggesting greater engagement of working-memory systems during this task (Schweinsburg et al., 2010). In addition, controls showed activation in the left hippocampus during novel encoding, whereas binge drinkers did not, suggestive of disadvantaged processing of novel verbal information for bingers. Binge drinkers did not show performance differences during imaging, but had poorer recall of the word pairs they had seen during imaging, suggesting subtle differences in learning tactics. A follow-up investigation in 16–18-year-olds with or without histories of binge drinking and heavy marijuana use similarly found greater right superior frontal and inferior parietal BOLD response among binge drinkers, but no main effects for marijuana use (Schweinsburg et al., 2011). Taken together, these findings suggest binge drinking is associated with aberrant neural activity during verbal working memory.
Binge drinkers also show differences in processing of affective information. In a study examining more complex cognitive processing with a decision-making task (the Iowa Gambling Task) in binge drinkers ages 16–18, binge drinkers showed greater BOLD activity in the limbic brain regions (i.e., amygdala and insula) than matched controls. Greater drinking severity was positively related to BOLD activity in the insula and negatively related to BOLD activity in the orbitofrontal cortex (Xiao et al., 2013). This pattern of activation differences suggests that hyperreactivity in brain regions responsible for emotional and incentive-related behaviors is associated with risky behaviors like binge drinking.
Several recent prospective studies have shown pre-existing differences in neural activation prior to adolescent engagement in substance use. Specifically, brain activation patterns have been able to predict future alcohol use, alcohol-related impairments (e.g., “blackouts”), and substance use disorder symptomatology. In 12–14-year-old adolescents who were scanned before initiation of alcohol use, those adolescents who transitioned into to heavy alcohol use by age 18 had lower BOLD activation at baseline in frontal, temporal, and parietal cortices in response to a Go/No-Go task of response inhibition than matched controls (Norman et al., 2011). On the same Go/No-Go task in a different sample of 12–14-year-old substance-naïve adolescents, greater baseline activation during inhibitory processing was related to more alcohol-induced blackouts at a 5-year follow-up, suggesting a neurobiologic vulnerability to alcohol-induced memory impairment (Wetherill et al., 2012). In a slightly older group of 16–19-year-old teens, less ventromedial prefrontal activation and greater left angular gyrus activation predicted greater substance use (both alcohol and marijuana) at an 18-month follow-up (Mahmood et al., 2013). An interesting study by Nees and colleagues (2012) found that reward-related brain activation (e.g., ventral striatum), along with personality and behavioral traits, aided in the prediction of early-onset drinking in adolescents, further supporting the notion that pre-existing traits may leave certain youth vulnerable to addictive behaviors (Nees et al., 2012).
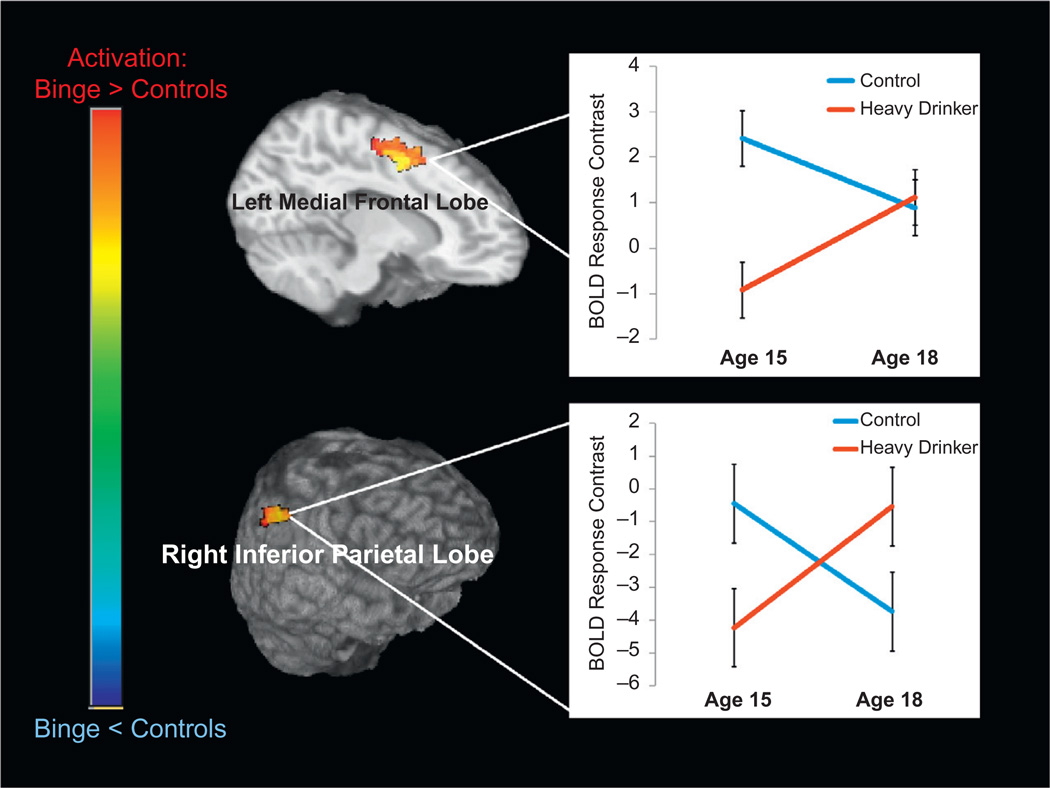
To our knowledge, only one study exists that has longitudinal fMRI data points examining adolescent alcohol use. In this study, 12–16-year-old adolescents were scanned before they ever used any alcohol or drugs and then were rescanned approximately 3 years later on the same scanner (Squeglia et al., 2012; Fig. 28.1). Those who transitioned into heavy use (n = 20) were matched to continuous non-drinkers (n = 20) over the follow-up on several alcohol risk and developmental factors. Adolescents who transitioned into heavy drinking over the follow-up showed less BOLD response during a visual working-memory task at baseline in frontal and parietal regions than matched controls; this local BOLD response increased after the initiation of heavy alcohol use. By contrast, continuous non-drinkers showed decreasing activation in these regions, as would be expected with maturation. Lower baseline activation predicted future alcohol use above and beyond common predictors of substance use (e.g., family history, age, gender), consistent with previous findings suggesting neural abnormalities predate initiation of heavy substance use (Mahmood et al., 2013; Wetherill et al., 2012). Taken together, these findings suggest that neural response patterns may be risk factors for future initiation of substance use, and that heavy drinking during adolescence is associated with subtle alterations in brain functioning.
Fig. 28.1.
Adolescents aged 12–16 years old were scanned before they ever used any alcohol or drugs and then were rescanned approximately 3 years later on the same scanner. Those who transitioned into heavy use (n = 20) were matched to continuous non-drinkers (n = 20) over the follow-up on several alcohol risk and developmental factors. Adolescents who transitioned into heavy drinking over the follow-up showed less blood oxygen level-dependent (BOLD) response during a visual working-memory task at baseline in frontal and parietal regions than matched controls; this local BOLD response increased after the initiation of heavy alcohol use. By contrast, continuous non-drinkers showed decreasing activation in these regions, as would be expected with maturation.
Gender and comorbid substance use are important considerations when examining the effect of alcohol use on brain functioning. Squeglia and colleagues (2011a) found binge drinking by gender interactions in BOLD activation to a spatial working-memory task, with female binge drinkers showing less activation than female controls, and male binge drinkers exhibiting greater BOLD response than male controls. For female binge drinkers, less activation was associated with poorer neurocognitive performance; however, the opposite was found for male binge drinkers (Squeglia et al., 2011a). These findings are consistent with previous work that suggests differences in brain activation between males and females, and increased vulnerability of females to alcohol-related brain changes (Caldwell et al., 2005). In teens with co-occurring alcohol and marijuana use disorder, Schweinsburg et al. (2005) found less inferior frontal and temporal activation and increased medial frontal activation compared to controls in response to the spatial working-memory task, suggesting altered neural processing in teens with comorbid alcohol and marijuana use (Schweinsburg et al., 2005).
Genetics, vulnerability, and brain function
Several studies have found pre-existing differences in neural structure and function in adolescents with a positive family history of substance use even before they initiated heavy drinking. These findings suggest neural structure and functioning may be a phenotypic risk factor for initiation of substance use. In a study of adolescents ages 12–14, youth who had a positive family history of alcoholism showed decreased inhibitory response in frontal brain regions during a task of inhibition when compared to youth with negative family history (Schweinsburg et al., 2004). Pre-existing differences in BOLD response were also found in youth who were family history-positive for substance use, such that family history-positive youth had greater BOLD activation in frontal regions, cingulate, and insula on a Stroop color-word task compared to controls (Silveri et al., 2011). These findings suggest family history-positive adolescents may have reduced inhibitory capacity prior to the onset of alcohol use, which could increase the likelihood of their engaging in future substance use.
Family history of alcoholism is also a factor affecting working-memory systems. Teens with a positive family history have lower BOLD activation during a verbal working-memory task relative to teens with a negative family history (Cservenka et al., 2012). Family history-positive teens also showed aberrations on a spatial working-memory task in prefrontal, parietal, and cerebellar regions, suggesting these alterations may be a general risk factor for family history-positive youth (Mackiewicz et al., 2013). Futhermore, youth with a denser family history of alcohol use disorders had alterations in spatial working memory, exhibiting less BOLD activation in response to a simple vigilance condition in frontal and cingulate regions and greater activation during the resting condition (Spadoni et al., 2008).
Functional connectivity analysis of brain activation enables questions to be addressed regarding relations between activation sites and forms the basis for making inferences about functional brain circuitry. In a multimodal imaging study using fMRI and DTI indices, lower functional and structural connectivity between frontal and cerebellar regions was found in family history-positive teens when compared to matched controls (Herting et al., 2011). This study supported preliminary evidence that adolescents with a family history may also have differences in regulating their default-mode network. A similar investigation examining connectivity between frontoparietal areas in teens ages 12–14 found poorer connectivity between posterior parietal and dorsolateral prefrontal brain regions in family history-positive youth compared to controls without a family history of alcoholism; however, differences in corresponding white-matter tracts were not observed (Wetherill et al., 2012).
Several more studies have looked at BOLD response to more complex reward anticipation and decision-making tasks in order to understand whether altered reward-related circuitry in mesolimbic brain regions contributes to alcohol use disorder vulnerabilities. During a decision-making task, family history-positive youth showed atypical neural response in the dorsolateral prefrontal cortex and cerebellar regions when compared to demographically matched youth (Cservenka and Nagel, 2012). During a task of monetary incentive, brain activation differences were not found between children of alcoholics and matched controls (Bjork et al., 2008). However, in a similar study examining children (ages 18–22) of alcoholics using a monetary incentive delay task, differences were found in the mesolimbic substrates in response to this task in children of alcoholics (Yau et al., 2012). Decreased nucleus accumbens response was found in response to reward anticipation in children of alcoholics with a positive family history and low alcohol use. Positive relationships between externalizing, nucleus accumbens activity, and current and lifetime alcohol consumption in children of alcoholics were also found. Discrepancies in these two studies are likely related to developmental trajectories of the reward system, where risk taking varies by age and interacts with environment (Bjork et al., 2008; Yau et al., 2012).
In a prospective investigation, teens who were higher in resiliency (flexible and adaptive behavioral responses) during early adolescence (ages 12–15) had later onset of drinking (ages 18–22) (Weiland et al., 2012). Negative relationships were identified between resiliency and BOLD activity in basal ganglia and thalamus during a working-memory task. The authors suggest that resiliency may be related to pre-existing neuroprotective factors, as resiliency was predictive of brain activation differences (Weiland et al., 2012). In sum, genetic and personality factors may predispose adolescents to initiate heavy drinking, and should be targeted in prevention efforts.
Cue reactivity, level of response, and brain function
Cue reactivity is a classically conditioned response to drug stimuli. There have been few studies of cue reactivity in the literature with adolescents, despite reports of craving in the presence of alcohol and other drugs. Understanding brain regions subserving reactivity and craving is important because it may elucidate brain functioning that is pre-existing and genetically linked (e.g., family history status). Cue reactivity may also result in shifted attention to alcohol cues in the environment after heavy use and compromised coping skills in the presence of alcohol. One study looked at relationships between drinking models (i.e., family, friends), family history of an alcohol use disorder, and personal alcohol use on valence to alcohol cues (Pulido et al., 2009b). The sample included social-drinking young adults ages 18–23 and found that positive response to cues was dependent on more personal experience (greater current drinking) compared to family history or environment (Pulido et al., 2009b). In a follow-up study, family history was not associated with brain activation to positive or negative alcohol expectancies per se in non-drinking youth; however, differences in brain response were related to more positive alcohol use expectancies, in that less neural differentiation was found between tasks (Pulido et al., 2009a).
In two of the earlier cue reactivity studies, alcohol-dependent young women (ages 18–24) showed greater BOLD response compared to non-abusers during alcohol word presentation trials in prefrontal, insular, subcallosal, and anterior cingulate regions. Increased craving was related to increased BOLD response among the alcohol-dependent women (Tapert et al., 2004a). Another investigation examined differences in activation in response to alcohol pictures. Teens with alcohol use disorders (ages 14–17) showed increased activation to alcoholic beverage pictures in anterior cingulate and prefrontal and limbic brain regions compared to demographically matched controls. Increased brain response was related to more drinks per month (Tapert et al., 2003), highlighting differences in brain activation in heavy users in response to cues, which then likely enhances the vulnerability of teens for future use. More work prior to transition into alcohol abuse and dependence is needed in this area.
Level of response to alcohol is linked to pre-existing genetic characteristics. Research has shown that individuals requiring higher doses of alcohol to feel desired effects are more likely to develop an alcohol use disorder (Schuckit and Smith, 1996), and there are likely underlying neural substrates that impact cognitive and affective processes related to level of response. In a sample of adolescents ages 15–17 with varying degrees of alcohol use (over half with a family history of alcohol use disorder), BOLD activation to a visual working-memory task predicted level of response to alcohol. In several cases (e.g., frontal gyrus, temporal gyrus, insula), increased BOLD activation was related to needing more drinks to achieve an effect similar to that of early-drinking episodes (Tapert et al., 2004b).
NEUROCOGNITIVE PERFORMANCE IN ADOLESCENTALCOHOL USERS
The current literature suggests that heavy drinking during adolescence has a subtle but significant deleterious effect on adolescent neurocognitive functioning. Several cross-sectional investigations have identified poorer performance in many neurocognitive domains, including attention and information processing (Tarter et al., 1995; Ferrett et al., 2010; Thoma et al., 2011), memory (Brown et al., 2000; Ferrett et al., 2010), visuospatial functioning (Sher et al., 1997; Giancola et al., 1998), language abilities (Moss et al., 1994), and executive functioning (Moss et al., 1994; Thoma et al., 2011), in heavy adolescent drinkers when compared with non-drinking controls. Taken together, these findings suggest a wide-reaching pattern of deleterious effects of alcohol use on neurocognitive abilities spanning childhood to late adolescence (Ferrett et al., 2010; Thoma et al., 2011; Parada et al., 2012).
In addition to cross-sectional studies examining neurocognitive functioning, several longitudinal investigations have been conducted, which have helped disentangle premorbid factors from consequences of heavy alcohol use. In 1999, Tapert and colleagues examined adolescents ages 13–19 recruited from inpatient treatment programs. Over 4 years of follow-up neurocognitive assessments, teens with greater alcohol and drug use following treatment had poorer neurocognitive functioning, particularly on measures of attention and visuospatial functioning (Tapert and Brown, 1999). In a follow-up study tracking participants for 8 years, from approximately age 16 to 24, greater alcohol and drug use predicted worsened attention, learning, and visuospatial functioning over the follow-up period (Tapert et al., 2002).
These findings have been replicated in a prospective study that characterized at-risk adolescents prior to ever initiating alcohol use. Alcohol-naïve adolescents, 12–14 years old, performed neuropsychological testing in follow-up study over 3 years. At follow-up (around age 16), approximately half of the sample transitioned to heavy or moderate drinking. For girls, more drinking days over the follow-up interval predicted worse visuospatial performance at follow-up; for boys, more hangover symptoms were associated with worse performance on a test of sustained attention at follow-up (Squeglia et al., 2009b). Assessment of long-term (10-year) patterns of alcohol and other drug use in teenagers from ages 16 to 27 revealed that heavier substance use patterns were related to poorer learning, memory, attention, and visuospatial processing, similar to findings in adult alcoholics (Sullivan and Pfefferbaum, 2005; Oscar-Berman and Marinkovic, 2007). For alcohol specifically, more alcohol use (with little other substance use) was related to worse short-term verbal memory. Interestingly, the authors also found that withdrawal symptoms at each follow-up visit were associated with poorer learning and memory performance (Hanson et al., 2011).
The idea that postdrinking withdrawal and hangover symptoms play a deleterious role in brain functioning is increasingly being explored in the literature, as these symptoms may be more detrimental than the quantity of alcohol consumed and may present a more accurate marker of drinking quantity. Greater hangover symptoms have been found to be predictive of worsened attention and visuospatial functioning (Tapert et al., 2002; Squeglia et al., 2009b). Negative relationships between alcohol withdrawal symptoms and learning and memory performance have also been found. For instance, among adolescent alcohol users ages 15–19, greater hangover symptoms were associated with poorer performance on measures of immediate and delayed recall (Mahmood et al., 2010).
Adolescent alcohol use affects higher-order, more complex cognitive functioning. Tenth-grade adolescent binge drinkers in China showed poorer performance on a task of risky decision making, particularly in their hypersensitivity to reward. Youth with a family history of alcoholism may be genetically linked to pre-existing differences in cognitive development (Johnson et al., 2008), mirroring findings from the neuroimaging literature. Weaknesses in executive functioning abilities have been found in youth between the ages of 3 and 14 years with a family history of alcoholism, suggesting that preexisting differences contribute to risk for alcoholism (Nigg et al., 2004). Even with pre-existing differences, studies have clearly shown a link between substance use and poorer neurocognitive functioning with varying degrees of substance misuse (e.g., binge drinking, dependence).
SUMMARYAND CONCLUSIONS
Alcohol use is common during adolescence, with almost a quarter of all American high school seniors endorsing recent binge drinking. This trend is concerning, as adolescents undergo significant neural development, particularly in frontal regions of the brain that are involved in higher-order cognition. Adolescents who engage in heavy alcohol use show alterations in both gray- and white-matter brain structures, and aberrations in brain activity (Table 28.1). These differences in structure and function are related to poorer neurocognitive performance on tests of attention, working memory, spatial functioning, verbal and visual memory, and executive functioning. Adolescents who engage in heavy episodic drinking (binge drinking), as well as those who have greater withdrawal and hangover symptoms, tend to show the greatest deviations in functioning. Family history of alcohol is related to cognitive disadvantages that may leave youth more vulnerable to the neurotoxic effects of alcohol use.
Table 28.1.
Summary of findings on the effect of alcohol on adolescent brain development
| Cognition | ↓ Visuospatial functioning, learning and memory, attention |
| Brain volume | ↓ Hippocampus, prefrontal cortex, cerebellum volume |
| Cortical thickness | ↑ Frontal cortices (females), ↓ frontal cortices (males) |
| White-matter integrity | ↓ White-matter integrity |
| Brain activation | ↓ Activation before initiating alcohol use; ↑ activation post heavy drinking |
Large-scale, prospective studies should help identify pre-existing brain differences in youth prior to initiating alcohol use, as well as identification of imaging indices and biomarkers that are able to predict future problematic drinking and co-occurring psychopathology. Gender is also an important variable to consider in both structural and functional neuroimaging because girls and boys peak in brain development at different ages and girls may be slightly more vulnerable to the effects of alcohol than boys. As alcohol is commonly used with other drugs, future studies should look at the co-occurring effect of alcohol with marijuana and other drug use. Use of these findings should be implemented in intervention and prevention measures. Remediation programs must be developed to help enhance cognition and decrease the likelihood of engagement in future substance use behaviors. Although these programs are employed with adults (Rupp et al., 2012) and are beginning to be explored prior to initiation of problematic alcohol use (Hollen, 1998), limited work has been done with adolescents with alcohol use histories. Prospective neuroimaging investigations to help disentangle pre-existing differences from toxicity continue to be important for future investigations. The investigation of how cognitive intervention may prevent future substance use involvement by targeting neural substrates underlying alcohol-related neurotoxicity is an essential next step in translating imaging and cognitive findings to clinical application.
ACKNOWLEDGMENTS
This review was supported in part by NIAAA (R01 AA013419, 1U01 AA021692, and 1U01 AA021695) and NIDA (F32 DA032188).
Footnotes
DISCLOSURE STATEMENT
The authors are not aware of any affiliations, memberships, funding, or financial holdings that might be perceived as affecting the objectivity of this review.
REFERENCES
- Bava S, Frank LR, McQueeny T, et al. Altered white matter microstructure in adolescent substance users. Psychiatry Res. 2009;173:228–237. doi: 10.1016/j.pscychresns.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bava S, Jacobus J, Mahmood O, et al. Neurocognitive correlates of white matter quality in adolescent substance users. Brain Cogn. 2010;72:347–354. doi: 10.1016/j.bandc.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bava S, Jacobus J, Thayer R, et al. Longitudinal changes in white matter integrity among adolescent substance users. Alcohol Clin Exp Res. 2013;37:E181–E189. doi: 10.1111/j.1530-0277.2012.01920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjork JM, Knutson B, Hommer DW. Incentive-elicited striatal activation in adolescent children of alcoholics. Addiction. 2008;103:1308–1319. doi: 10.1111/j.1360-0443.2008.02250.x. [DOI] [PubMed] [Google Scholar]
- Brown SA, Tapert SF, Granholm E, et al. Neurocognitive functioning of adolescents: effects of protracted alcohol use. Alcohol Clin Exp Res. 2000;24:164–171. [PubMed] [Google Scholar]
- Caldwell LC, Schweinsburg AD, Nagel BJ, et al. Gender and adolescent alcohol use disorders on BOLD (blood oxygen level dependent) response to spatial working memory. Alcohol Alcohol. 2005;40:194–200. doi: 10.1093/alcalc/agh134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, Hare TA. The adolescent brain. Ann N Y Acad Sci. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cservenka A, Nagel BJ. Risky decision-making: an FMRI study of youth at high risk for alcoholism. Alcohol Clin Exp Res. 2012;36:604–615. doi: 10.1111/j.1530-0277.2011.01650.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cservenka A, Herting MM, Nagel BJ. Atypical frontal lobe activity during verbal working memory in youth with a family history of alcoholism. Drug Alcohol Depend. 2012;123:98–104. doi: 10.1016/j.drugalcdep.2011.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD, Clark DB, Beers SR, et al. Hippocampal volume in adolescent-onset alcohol use disorders. Am J Psychiatry. 2000;157:737–744. doi: 10.1176/appi.ajp.157.5.737. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Narasimhan A, Thatcher DL, et al. Prefrontal cortex, thalamus, and cerebellar volumes in adolescents and young adults with adolescent-onset alcohol use disorders and comorbid mental disorders. Alcohol Clin Exp Res. 2005;29:1590–1600. doi: 10.1097/01.alc.0000179368.87886.76. [DOI] [PubMed] [Google Scholar]
- Ferrett HL, Carey PD, Thomas KG, et al. Neuropsychological performance of South African treatment-naive adolescents with alcohol dependence. Drug Alcohol Depend. 2010;110:8–14. doi: 10.1016/j.drugalcdep.2010.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giancola PR, Mezzich AC, Tarter RE. Executive cognitive functioning, temperament, and antisocial behavior in conduct disordered adolescent females. J Abnorm Psychol. 1998;107:629–641. doi: 10.1037//0021-843x.107.4.629. [DOI] [PubMed] [Google Scholar]
- Giedd JN. Structural magnetic resonance imaging of the adolescent brain. Ann N Y Acad Sci. 2004;1021:77–85. doi: 10.1196/annals.1308.009. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Rapoport JL. Structural MRI of pediatric brain development: what have we learned and where are we going? Neuron. 2010;67:728–734. doi: 10.1016/j.neuron.2010.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN, Blumenthal J, Jeffries NO, et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci. 1999;2:861–863. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- Hanson KL, Cummins K, Tapert SF, et al. Changes in neuropsychological functioning over 10 years following adolescent substance abuse treatment. Psychol Addict Behav. 2011;25:127–142. doi: 10.1037/a0022350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herting MM, Schwartz D, Mitchell SH, et al. Delay discounting behavior and white matter microstructure abnormalities in youth with a family history of alcoholism. Alcohol Clin Exp Res. 2010;34:1590–1602. doi: 10.1111/j.1530-0277.2010.01244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herting MM, Fair D, Nagel BJ. Altered frontocerebellar connectivity in alcohol-naive youth with a family history of alcoholism. Neuroimage. 2011;54:2582–2589. doi: 10.1016/j.neuroimage.2010.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollen PJ. Intervention booster: adding a decision-making module to risk reduction and other health care programs for adolescents. J Pediatr Health Care. 1998;12:247–255. doi: 10.1016/s0891-5245(98)90205-x. [DOI] [PubMed] [Google Scholar]
- Jacobus J, McQueeny T, Bava S, et al. White matter integrity in adolescents with histories of marijuana use and binge drinking. Neurotoxicol Teratol. 2009;31:349–355. doi: 10.1016/j.ntt.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobus J, Thayer RE, Trim RS, et al. White matter integrity, substance use, risk taking in adolescence. Psychol Addict Behav. 2013;27:431–442. doi: 10.1037/a0028235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson CA, Xiao L, Palmer P, et al. Affective decision-making deficits, linked to a dysfunctional ventromedial prefrontal cortex, revealed in 10th grade Chinese adolescent binge drinkers. Neuropsychologia. 2008;46:714–726. doi: 10.1016/j.neuropsychologia.2007.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the future national results on adolescent drug use: Overview of key findings, 2012. Ann Arbor: Institute for Social Research, The University of Michigan; 2013. [Google Scholar]
- Le Bihan D. Looking into the functional architecture of the brain with diffusion MRI. Nat Rev Neurosci. 2003;4:469–480. doi: 10.1038/nrn1119. [DOI] [PubMed] [Google Scholar]
- Lebel C, Beaulieu C. Longitudinal development of human brain wiring continues from childhood into adulthood. J Neurosci. 2011;31:10937–10947. doi: 10.1523/JNEUROSCI.5302-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C, Gee M, Camicioli R, et al. Diffusion tensor imaging of white matter tract evolution over the lifespan. Neuroimage. 2012;60:340–352. doi: 10.1016/j.neuroimage.2011.11.094. [DOI] [PubMed] [Google Scholar]
- Lenroot RK, Giedd JN. Brain development in children and adolescents: insights from anatomical magnetic resonance imaging. Neurosci Biobehav Rev. 2006;30:718–729. doi: 10.1016/j.neubiorev.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Lisdahl KM, Thayer R, Squeglia LM, et al. Recent binge drinking predicts smaller cerebellar volumes in adolescents. Psychiatry Res. 2013;211:17–23. doi: 10.1016/j.pscychresns.2012.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackiewicz Seghete KL, Cservenka A, Herting MM, et al. Atypical spatial working memory and task-general brain activity in adolescents with a family history of alcoholism. Alcohol Clin Exp Res. 2013;37:390–398. doi: 10.1111/j.1530-0277.2012.01948.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood OM, Jacobus J, Bava S, et al. Learning and memory performances in adolescent users of alcohol and marijuana: interactive effects. J Stud Alcohol Drugs. 2010;71:885–894. doi: 10.15288/jsad.2010.71.885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmood OM, Goldenberg D, Thayer R, et al. Adolescents’ fMRI activation to a response inhibition task predicts future substance use. Addict Behav. 2013;38:1435–1441. doi: 10.1016/j.addbeh.2012.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McQueeny T, Schweinsburg BC, Schweinsburg AD, et al. Altered white matter integrity in adolescent binge drinkers. Alcohol Clin Exp Res. 2009;33:1278–1285. doi: 10.1111/j.1530-0277.2009.00953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina KL, McQueeny T, Nagel BJ, et al. Prefrontal cortex volumes in adolescents with alcohol use disorders: unique gender effects. Alcohol Clin Exp Res. 2008;32:386–394. doi: 10.1111/j.1530-0277.2007.00602.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss HB, Kirisci L, Gordon HW, et al. A neuropsychologic profile of adolescent alcoholics. Alcohol Clin Exp Res. 1994;18:159–163. doi: 10.1111/j.1530-0277.1994.tb00897.x. [DOI] [PubMed] [Google Scholar]
- Nagel BJ, Schweinsburg AD, Phan V, et al. Reduced hippocampal volume among adolescents with alcohol use disorders without psychiatric comorbidity. Psychiatry Res. 2005;139:181–190. doi: 10.1016/j.pscychresns.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagy Z, Westerberg H, Klingberg T. Maturation of white matter is associated with the development of cognitive functions during childhood. J Cogn Neurosci. 2004;16:1227–1233. doi: 10.1162/0898929041920441. [DOI] [PubMed] [Google Scholar]
- Nees F, Tzschoppe J, Patrick CJ, et al. Determinants of early alcohol use in healthy adolescents: the differential contribution of neuroimaging and psychological factors. Neuropsychopharmacology. 2012;37:986–995. doi: 10.1038/npp.2011.282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT, Glass JM, Wong MM, et al. Neuropsychological executive functioning in children at elevated risk for alcoholism: findings in early adolescence. J Abnorm Psychol. 2004;113:302–314. doi: 10.1037/0021-843X.113.2.302. [DOI] [PubMed] [Google Scholar]
- Norman AL, Pulido C, Squeglia LM, et al. Neural activation during inhibition predicts initiation of substance use in adolescence. Drug Alcohol Depend. 2011;119:216–223. doi: 10.1016/j.drugalcdep.2011.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oscar-Berman M, Marinkovic K. Alcohol: effects on neurobehavioral functions and the brain. Neuropsychol Rev. 2007;17:239–257. doi: 10.1007/s11065-007-9038-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parada M, Corral M, Mota N, et al. Executive functioning and alcohol binge drinking in university students. Addict Behav. 2012;37:167–172. doi: 10.1016/j.addbeh.2011.09.015. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Mathalon DH, Sullivan EV, et al. A quantitative magnetic resonance imaging study of changes in brain morphology from infancy to late adulthood. Arch Neurol. 1994;51:874–887. doi: 10.1001/archneur.1994.00540210046012. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum A, Sullivan EV, Mathalon DH, et al. Frontal lobe volume loss observed with magnetic resonance imaging in older chronic alcoholics. Alcohol Clin Exp Res. 1997;21:521–529. doi: 10.1111/j.1530-0277.1997.tb03798.x. [DOI] [PubMed] [Google Scholar]
- Pulido C, Anderson KG, Armstead AG, et al. Family history of alcohol-use disorders and spatial working memory: effects on adolescent alcohol expectancies. J Stud Alcohol Drugs. 2009a;70:87–91. doi: 10.15288/jsad.2009.70.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulido C, Mok A, Brown SA, et al. Heavy drinking relates to positive valence ratings of alcohol cues. Addict Biol. 2009b;14:65–72. doi: 10.1111/j.1369-1600.2008.00132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupp CI, Kemmler G, Kurz M, et al. Cognitive remediation therapy during treatment for alcohol dependence. J Stud Alcohol Drugs. 2012;73:625–634. doi: 10.15288/jsad.2012.73.625. [DOI] [PubMed] [Google Scholar]
- Schuckit MA, Smith TL. An 8-year follow-up of 450 sons of alcoholic and control subjects. Arch Gen Psychiatry. 1996;53:202–210. doi: 10.1001/archpsyc.1996.01830030020005. [DOI] [PubMed] [Google Scholar]
- Schweinsburg AD, Paulus MP, Barlett VC, et al. An fMRI study of response inhibition in youths with a family history of alcoholism. Ann N Y Acad Sci. 2004;1021:391–394. doi: 10.1196/annals.1308.050. [DOI] [PubMed] [Google Scholar]
- Schweinsburg AD, Schweinsburg BC, Cheung EH, et al. fMRI response to spatial working memory in adolescents with comorbid marijuana and alcohol use disorders. Drug Alcohol Depend. 2005;79:201–210. doi: 10.1016/j.drugalcdep.2005.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweinsburg AD, McQueeny T, Nage BJ, et al. A preliminary study of functional magnetic resonance imaging response during verbal encoding among adolescent binge drinkers. Alcohol. 2010;44:111–117. doi: 10.1016/j.alcohol.2009.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweinsburg AD, Schweinsburg BC, Nagel BJ, et al. Neural correlates of verbal learning in adolescent alcohol and marijuana users. Addiction. 2011;106:564–573. doi: 10.1111/j.1360-0443.2010.03197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw P, Kabani NJ, Lerch JP, et al. Neurodevelopmental trajectories of the human cerebral cortex. J Neurosci. 2008;28:3586–3594. doi: 10.1523/JNEUROSCI.5309-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Martin ED, Wood PK, et al. Alcohol use disorders and neuropsychological functioning in first-year undergraduates. Exp Clin Psychopharmacol. 1997;5:304–315. doi: 10.1037//1064-1297.5.3.304. [DOI] [PubMed] [Google Scholar]
- Silveri MM, Rogowska J, McCaffrey A, et al. Adolescents at risk for alcohol abuse demonstrate altered frontal lobe activation during Stroop performance. Alcohol Clin Exp Res. 2011;35:218–228. doi: 10.1111/j.1530-0277.2010.01337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Holmes CJ, et al. In vivo evidence for post adolescent brain maturation in frontal and striatal regions. Nat Neurosci. 1999;2:859–861. doi: 10.1038/13154. [DOI] [PubMed] [Google Scholar]
- Sowell ER, Thompson PM, Leonard CM, et al. Longitudinal mapping of cortical thickness and brain growth in normal children. J Neurosci. 2004;24:8223–8231. doi: 10.1523/JNEUROSCI.1798-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spadoni AD, Norman AL, Schweinsburg AD, et al. Effects of family history of alcohol use disorders on spatial working memory BOLD response in adolescents. Alcohol Clin Exp Res. 2008;32:1135–1145. doi: 10.1111/j.1530-0277.2008.00694.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Jacobus J, Tapert SF. The influence of substance use on adolescent brain development. Clin EEG Neurosci. 2009a;40:31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Spadoni AD, Infante MA, et al. Initiating moderate to heavy alcohol use predicts changes in neuropsychological functioning for adolescent girls and boys. Psychol Addict Behav. 2009b;23:715–722. doi: 10.1037/a0016516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Schweinsburg AD, Pulido C, et al. Adolescent binge drinking linked to abnormal spatial working memory brain activation: differential gender effects. Alcohol Clin Exp Res. 2011a;35:1831–1841. doi: 10.1111/j.1530-0277.2011.01527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Sorg SF, Schweinsburg AD, et al. Binge drinking differentially affects adolescent male and female brain morphometry. Psychopharmacology (Berl) 2011b;220:529–539. doi: 10.1007/s00213-011-2500-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Pulido C, Wetherill RR, et al. Brain response to working memory over three years of adolescence: Influence of initiating heavy drinking. J Stud Alcohol Drugs. 2012;73:749–760. doi: 10.15288/jsad.2012.73.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiles J, Jernigan TL. The basics of brain development. Neuropsychol Rev. 2010;20:327–348. doi: 10.1007/s11065-010-9148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan EV, Pfefferbaum A. Neurocircuitry in alcoholism: A substrate of disruption and repair. Psychopharmacology (Berl) 2005;180:583–594. doi: 10.1007/s00213-005-2267-6. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Brown SA. Neuropsychological correlates of adolescent substance abuse: four-year outcomes. J Int Neuropsychol Soc. 1999;5:481–493. doi: 10.1017/s1355617799566010. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Brown GG, Kindermann SS, et al. fMRI measurement of brain dysfunction in alcohol-dependent young women. Alcohol Clin Exp Res. 2001;25:236–245. [PubMed] [Google Scholar]
- Tapert SF, Granholm E, Leedy NG, et al. Substance use and withdrawal: neuropsychological functioning over 8 years in youth. J Int Neuropsychol Soc. 2002;8:873–883. doi: 10.1017/s1355617702870011. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Cheung EH, Brown GG, et al. Neural response to alcohol stimuli in adolescents with alcohol use disorder. Arch Gen Psychiatry. 2003;60:727–735. doi: 10.1001/archpsyc.60.7.727. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Brown GG, Baratta MV, et al. fMRI BOLD response to alcohol stimuli in alcohol dependent young women. Addict Behav. 2004a;29:33–50. doi: 10.1016/j.addbeh.2003.07.003. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Pulido C, Paulus MP, et al. Level of response to alcohol and brain response during visual working memory. J Stud Alcohol. 2004b;65:692–700. doi: 10.15288/jsa.2004.65.692. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Schweinsburg AD, Barlett VC, et al. Blood oxygen level dependent response and spatial working memory in adolescents with alcohol use disorders. Alcohol Clin Exp Res. 2004c;28:1577–1586. doi: 10.1097/01.alc.0000141812.81234.a6. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Mezzich AC, Hsieh YC, et al. Cognitive capacity in female adolescent substance abusers. Drug Alcohol Depend. 1995;39:15–21. doi: 10.1016/0376-8716(95)01129-m. [DOI] [PubMed] [Google Scholar]
- Thoma RJ, Monnig MA, Lysne PA, et al. Adolescent substance abuse: the effects of alcohol and marijuana on neuropsychological performance. Alcohol Clin Exp Res. 2011;35:39–46. doi: 10.1111/j.1530-0277.2010.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiland BJ, Nigg JT, Welsh RC, et al. Resiliency in adolescents at high risk for substance abuse: flexible adaptation via subthalamic nucleus and linkage to drinking and drug use in early adulthood. Alcohol Clin Exp Res. 2012;36:1355–1364. doi: 10.1111/j.1530-0277.2012.01741.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wetherill RR, Bava S, Thompson WK, et al. Frontoparietal connectivity in substance-naive youth with and without a family history of alcoholism. Brain Res. 2012;1432:66–73. doi: 10.1016/j.brainres.2011.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao L, Bechara A, Gong Q, et al. Abnormal affective decision making revealed in adolescent binge drinkers using a functional magnetic resonance imaging study. Psychol Addict Behav. 2013;27:443–454. doi: 10.1037/a0027892. [DOI] [PubMed] [Google Scholar]
- Yau WY, Zubieta JK, Weiland BJ, et al. Nucleus accumbens response to incentive stimuli anticipation in children of alcoholics: relationships with precursive behavioral risk and lifetime alcohol use. J Neurosci. 2012;32:2544–2551. doi: 10.1523/JNEUROSCI.1390-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]