Abstract
Young black gay/bisexual and other men who have sex with men (YB-GBMSM) living with HIV are at risk for poor engagement in HIV care. Relatively little is known about factors that impact engagement outcomes at various stages along the HIV care continuum in this specific population. The purpose of this analysis was to examine associations between various psychosocial factors and likelihood of engagement at each stage of the care continuum, among a geographically diverse sample of 132 YB-GBMSM living with HIV. Negative self-image, a component of HIV stigma, had an inverse association with early care seeking after HIV diagnosis (OR=1.05; 95% CI 1.01–1.10). Negative self-image was also inversely associated with adherence to medical appointments (OR=0.95; 95% CI 0.91–0.99), while employment (OR=0.30; 95% CI 0.12–0.75) and ethnic identity affirmation (OR=0.28; 95% CI 0.12–0.68) were both positively associated with appointment adherence. HIV-positive identity salience was associated with a higher likelihood of being on antiretroviral therapy (OR=1.06; 95% CI 1.02, 1.09). These findings highlight the importance of processes related to identity development, as both barriers and facilitators of engagement in care for HIV-positive YB-GBMSM.
Introduction
Rates of new HIV infection continue to rise among adolescents and young adults between 13 and 24 years of age.1 These trends are largely driven by escalating rates among young gay/bisexual men and other men who have sex with men (Y-GBMSM), and this increase is most dramatic for young black GBMSM (YB-GBMSM). Between 2006 and 2009, HIV incidence among YB-GBMSM increased by 48%, which was the largest increase seen in any demographic or risk-group category.2 In 2009, YB-GBMSM made up 54% of new infections among Y-GBMSM, although black Americans comprise only 13% of the US population.1 Reducing such disparities is a major focus of the domestic HIV agenda, as reflected in the 2010 National HIV/AIDS Strategy.3
Policy and research initiatives are increasingly concentrating not only on reducing HIV incidence and prevalence, but also on improving engagement in care and clinical outcomes after diagnosis.4 Engagement in HIV care has been conceptualized as a continuum or cascade that includes the following stages: (1) HIV diagnosis, (2) linkage to care, (3) retention in care, (4) initiation on antiretroviral therapy (ART), and (5) viral suppression.5 Optimizing engagement in care has been shown to decrease individual morbidity and mortality, and to dramatically reduce the risk of HIV transmission to others.6 However, population-based studies of engagement at the national level have yielded sobering results, as only 19–28% of HIV-positive individuals are estimated to have achieved viral suppression.5,7,8 Engagement is even worse among adolescents and young adults at every stage; less than 6% of HIV-positive youth between 13 and 29 years of age are estimated to be virally suppressed.9
Despite their disproportionate representation among people living with HIV, relatively little research has focused on understanding and optimizing the continuum of engagement in care specifically among YB-GBMSM. Young age, black race, and gay/bisexual identity may have independent and/or synergistic associations with likelihood of engagement at various stages. Younger individuals living with HIV are consistently found to be at the highest risk for non-engagement at each stage of the continuum.10 Black race has also been associated with poorer engagement in some studies, although this relationship is inconsistent and varies by geographic setting.6,8,11 Some of this variation may be due to diversity within black populations, as prior work has documented differences in HIV testing, for example, between foreign-born and US-born black adults.12 Among adults, GBMSM have been found to have higher rates of engagement relative to the other risk behavior-based groups such as heterosexual women or injection drug users; however, this protective effect does not hold true for black GBMSM.13 These findings highlight the importance of characterizing and understanding engagement within specific subgroups of GBMSM and understanding ways in which culturally-specific barriers and facilitators interact and operate to influence care utilization for a given population.
In attempting to optimize engagement, it is important to build an understanding of the ways in which different characteristics of individuals may impact their engagement in care at various stages. The continuum/cascade has been critiqued as a provider-driven conceptualization, as analysis of these endpoints (e.g., retention, adherence, viral suppression) and their correlates is frequently based on clinic-level data that is collected for other purposes.14 Such research often focuses exclusively on demographic (e.g., race, age, sex) and clinical correlates of engagement in care. In contrast, qualitative research grounded in patients' experiences has highlighted the importance of cognitive and psychosocial processes as influences on engagement at various stages.14 We have conceptualized both the sociodemographic and potential psychosocial influences on engagement in care within a theoretical framework based on Social Action Theory (SAT) (Fig. 1). SAT has previously been applied to research and intervention design in Y-GBMSM, and lends itself to the incorporation of individual-level contextual influences and developmental processes that are critical during adolescence and young adulthood.15–19 SAT proposes that health outcomes and health promoting behaviors such as engagement in HIV care are influenced by contextual influences, which in turn affect self-change processes and subsequently health behaviors and outcomes.19 In the original description of this theory, contextual influences refer to the physical, social, biological, and mood/arousal factors that constitute the context of an individual's health behavior. The self-change processes refer to goals, expectations, and strategies that serve as mechanisms for behavior change. SAT focuses on applying psychology to public health in a way that emphasizes interactions between social context and individual psychological processes.16
FIG. 1.
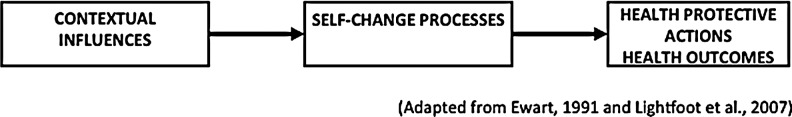
Social Action Theory conceptual framework.
Although less commonly studied compared to traditional demographic and clinical indicators,20 there is support in the literature for relationships behind HIV engagement outcomes and psychological constructs that correspond to the SAT framework. The qualitative study cited above found depression, social support, and the development of an HIV-positive identity to be critical to understanding the continuum of engagement in care among adults in San Francisco, illustrating how, consistent with the SAT, contextual influences (mood/arousal, or depression) can lead to self-change processes (strategies such social support and identity acceptance) with implications for healthcare utilization behavior.12 Another qualitative study from the Bronx similarly found health behavior skills, affective factors, and socio-cultural factors to be important in patients' descriptions of barriers and facilitators of retention in HIV care.21 Background contextual factors such as individuals' identity constructs were also salient in a previous analysis from our parent study (ATN 070), in which gay identity and ethnic identity influenced adherence to medical appointments, with some evidence that HIV-positive identity might also play a role.22 Finally, a significant body of work has examined associations between SAT-related psychosocial factors and medication adherence, which is a health promoting behavior that is also a part of the continuum of engagement in care. Depression, stigma, and social support are among the factors that have most commonly been associated with adherence to ART, and these can similarly be viewed as background contextual factors (depression and stigma) and self-change processes (utilizing social support) consistent with the SAT model.23
The current study represents a secondary analysis of data collected as part of a cross-sectional mixed-methods research study conducted within the Adolescent Medicine Trials for HIV/AIDS Interventions (ATN). The overall goal of the parent study, ATN 070 [“Psychosocial Needs of HIV+ Young Men who have Sex with Men (YMSM)”] was to examine the psychosocial and developmental needs of young MSM living with HIV; self-reported measures of adherence to healthcare were also examined. In light of the critical need for more information about predictors of engagement in HIV care among YB-GBMSM, the objective of this exploratory secondary analysis was to examine psychosocial correlates of engagement in care at different stages along the continuum. Although we did not have all of the necessary data to test the model in full, we used the SAT framework to guide the selection of potential predictor variables as part of an exploratory analysis.
Methods
Study design and procedures
Data collection was conducted at 14 adolescent medicine clinical care sites [Baltimore, Bronx, Chicago (2 sites), DC, Ft. Lauderdale, Los Angeles, Manhattan, Memphis, Miami, New Orleans, Philadelphia, Tampa, San Francisco] between March and June of 2009. The research protocol was approved by the institutional review boards at all institutions involved in the collection and analysis of data. Male adolescents and young adults aged 16–24 who were living with HIV and receiving care within one of the clinical settings above, were approached by study coordinators to assess eligibility. Inclusion criteria were (1) biologically male at birth and identification as male at time of study participation; (2) HIV-infected as documented by medical record review or verbal verification with referring professional; (3) HIV infection acquired horizontally through sexual or substance use behavior; (4) age 16–24 at time of consent/assent; (5) ability to understand both written and spoken English; and, (6) at least one sexual encounter involving either anal or oral penetration with a male partner during the 12 months prior to study participation.
Study coordinators conducted a brief screening interview in order to determine eligibility. Upon verification of eligibility, study coordinators obtained signed consent/assent and enrolled participants in the study utilizing a confidential code that contained no identifying personal information. An appointment to complete a 90-min audio computer assisted self-interview (ACASI) was scheduled for each participant. Data were saved in an encrypted format using ENTRUST encryption software and were not available for review by any clinical site personnel. The encrypted data were transmitted to a central data operations center where data were unencrypted and entered into a study database. Compensation for participation was determined by each site and was in line with typical incentives provided for similar studies at the site.
Measures: Background factors
Demographics
We focused our analysis exclusively on those participants who endorsed a black/African American racial identity, including those with multiple racial identities; all analyses that follow (including calculation of reliability coefficients) refer specifically to the black/African American subset of the overal 070 sample. Demographic variables included in this analysis, which are listed as individual-level contextual factors in our SAT theoretical model (Fig.1), were age, housing status, education, and employment. Age was measured as a continuous numerical variable that was self-reported by participants. Housing status was measured by a single question, “Where do you live now?”, to which respondents had the opportunity to describe their housing arrangements as “own house/apartment”, “parent's house/apartment”, “family member's house/apartment”, “another person's house/apartment”, “foster/group home”, “boarding home/shelter/halfway house”, or “other”. In our analysis, we combined these into four categorical values: “Lives alone”, “Lives with family”, “Lives with someone else”, and “Shelter”. Education was based on the single question, “What is the highest grade you have completed?” with responses categorized as “Less than high school education”, “High school education”, or “More than high school education” and dichotomized (less than high school versus high school or more) for the multivariable analysis. Finally, employment was measured by asking “Are you currently working?” with three possible answers: “Yes, full-time”, “Yes, part-time”, or “No”. Full-time and part-time employment were combined (and compared to not working) in the multivariable analysis.
Ethnic identity
Ethnic identity was assessed using the multi-group ethnic identity measure (MEIM).24 The MEIM is a 14-item scale including three items that require the participant to choose an ethnic group for himself as well as for each parent. Since our analysis was restricted to black/African American youth, we disregarded these closed-ended questions and utilized the remaining 11 items, which fall into two subscales: Ethnic Identity Search (a developmental and cognitive component) and Affirmation, Belonging, and Commitment (an affective component). Participants could answer items with a four-point scale (1=strongly disagree; 2=disagree; 3=agree; 4=strongly agree). Scores from each item are averaged so that the total score on each subscale ranges from 1–4. Higher scores on each subscale indicate a stronger connection to one's ethnic identity. The MEIM has been used in multiple studies with diverse youth, demonstrating good reliability across a range of ethnicities and ages.25 Cronbach's alphas for our current study were acceptable: Ethnic Identity Search (α=0.70); Affirmation, Belonging, and Commitment (α=0.86).
Sexual orientation identity
Sexual orientation identity was assessed using Mayfield's 23-item Internalized Homonegativity Inventory (IHNI),26 which requires participants to respond to questions using a five-point scale (1=strongly disagree; 2=disagree; 3=neither agree nor disagree; 4=agree; 5=strongly agree). The measure contains three subscales: Personal Homonegativity (11 items measuring negative emotions and attitudes towards one's own sexual orientation; total scores range from 11–66), Gay Affirmation (7 items measuring positive attitudes and feelings that being gay is important, normal, and fulfilling; total scores range from 7 to 35), and Morality of Homosexuality (5 items measuring negative attitudes regarding the moral implications of same-sex attraction and behavior; total scores range from 5 to 25). The IHNI has strong convergent, discriminant, and construct validity in prior studies.26 Cronbach's alphas for the current study were acceptable: Personal Homonegativity (α=0.93); Gay Affirmation (α=0.82); Morality of Homosexuality (α=0.68).
Identity as a young man living with HIV
Participants' identity as young men living with HIV was assessed using two different measures. The Negative Self-Image subscale of the HIV Stigma Scale was used to assess HIV-related self-image.27 This subscale consists of 13 items rated on a four-point scale (1=strongly agree; 2=agree; 3=disagree; 4=strongly disagree; total scores range from 13 to 52). Cronbach's alpha with our sample was high, consistent with previously published results (α=0.90). The Salience subscale of the HIV-Positive Identity Questionnaire28 was used to assess how central or salient living with HIV is to one's self-concept. Respondents rated their level of agreement with seven statements regarding thoughts/feelings about being HIV-positive on a five-point scale (1=strongly disagree; 2=disagree; 3=neutral; 4=agree; 5=strongly agree; total scores range from 7 to 35). Cronbach's alpha with our current sample was α=0.80.
Psychological distress
To create a proxy for psychological distress using our dataset, we first examined participants' self-report of seeking mental health care as a dichotomous “yes/no” variable (Have [you] ever seen a psychiatrist, psychologist, marriage and family therapist, or social worker about the way you were feeling or behaving?). Participants next had the option of answering “yes/no” to various indications for seeking mental health treatment, including suicidality, depression, drug use, anxiety, and problems coping with illness. The number of indications endorsed by each participant was taken as proxy for multiple psychological stressors and made into a sum variable for the measurement of psychological distress.
Measures: Self-change processes
Social support
Participants' access to, and satisfaction with their social support was assessed using the Social Support for Adolescents Scale.29 Our study utilized only the Emotional Support subscale, which asked participants to rate how helpful various individuals (including friends, family members, school personnel) were when they needed to talk about a personal problem (1=not at all; 2=somewhat; 3=a great deal). Total scores ranged from 8–24. Cronbach's alpha with our sample was α=0.70.
Motivational appraisals
Motivational appraisals were assessed using two different measures. The Future subscale of the Stanford Time Perspective Inventory30 was used to assess the degree to which participants were striving for future goals and rewards. The scale is made up of 13 items rated on a five-point scale (1=very untrue; 2=untrue; 3=neutral; 4=true; 5=very true; total scores range from 13 to 60); Cronbach's alpha for our study was α=0.73. The Life Outcome Expectancies measure was designed specifically for this study and was divided into two conceptual domains, Outcome Expectations and Efficacy. The Life Outcome Expectancies questions measured participants' perceived likelihood of reaching life milestones on a five-point scale (1=not at all; 2=a little; 3=somewhat; 4=very; 5=has already occurred) with a Cronbach's alpha of α=0.71. The Efficacy questions measured participants' perceived control over their life circumstances on a 4-point scale (1=poor; 2=fair; 3=good; 4=excellent) with a Cronbach's alpha of α=0.82.
Measures: Health promoting behaviors and health outcomes
We utilized our self-report data to create proxies for each of the stages along the HIV care continuum. These outcomes measures related to engagement in care are described below.
Time to care-seeking (Linkage)
We asked participants for the date of their diagnosis, as well as for the specific date when they first sought medical treatment for HIV. We conceptualized the time lag between the two dates as a proxy for measuring the time to linkage to care, recognizing several limitations: (1) self-report measure without corroboration of clinic visits, and (2) differential interpretation of “seeking” care which might involve making a call or finding a clinic but not actually enrolling in care, and (3) missing data. Based on the answers to this question, we grouped participants into the following categories of time to care-seeking: Same day, <1 month, 1–3 months, and>3 months.
Missed appointments (Retention)
Adherence to medical appointments was measured using a single self-reported item: How many doctor's appointments have you missed in the past 3 months? The 3-month time frame was used since optimal HIV care typically involves interaction with health care providers every 3 months. Responses to this single item were dichotomized into “no missed appointments” and “one or more missed appointments” in order to create a dependent variable that represented perfect adherence to medical appointments during the past 3 months.
ART utilization (Initiation on ART)
Utilization of ART was measured using a single self-reported item: “Are you currently taking pills or other medicines to treat your HIV?” which could be answered as yes or no.
Adherence to ART
Adherence to ART was measured using a single self-reported item: “How many times did you miss taking a dose of pills in the last month?” Of note, this question followed an introductory paragraph that made it clear that all questions in the section were referring specifically to ART medications. We dichotomized responses at each of the time points to differentiate between participants who had missed any doses in the specified time interval, versus those who had not.
Data analysis
Data were examined for non-normality. None of the psychosocial variables showed evidence of skewness and/or kurtosis. We used univariate, bivariate, and multivariate analyses to examine distributions and associations between psychosocial, sociodemographic, and engagement outcome variables. Univariate analyses included frequencies and measures of central tendency and variability (Table 1). We conducted Chi-square or t-tests to assess bivariate relationships between predictors and engagement outcome variables. We created a correlation matrix to assess for potential multicollinearity between predictor variables (data not shown). Associations that were significant at p<0.10 in bivariate analyses were retained in the multivariate models, as were the background demographic variables of age, education, time since diagnosis, and employment. Multivariate models were constructed using forward stepwise regression; demographic variables were included regardless of significance, however, the psychosocial covariates were only retained in the model if they remained significant and improved the model. Separate multivariate logistic regression models were developed for each outcome to explore associations between psychosocial predictors and engagement at different stages of the continuum (Tables 2–4). All data analysis was conducted using SPSS v.20 statistical software.
Table 1.
Demographic, Psychosocial and Care Engagement Characteristics
| Mean | SD | |
|---|---|---|
| Age in years | 20.9 | 1.9 |
| Time since diagnosis (years) | 2.5 | 1.7 |
| Education | N | % |
| Did not complete high school | 36 | 27.3 |
| High school graduate | 52 | 39.4 |
| Some college/technical school | 38 | 28.8 |
| College/technical school graduate | 6 | 4.6 |
| Employment | ||
| Full-time | 28 | 21.2 |
| Part-time | 33 | 25.0 |
| Not employed | 71 | 53.8 |
| Housing arrangement | ||
| Own house/apartment | 39 | 29.6 |
| Parent's house apartment | 51 | 38.6 |
| Family member(s) house/apt | 14 | 10.6 |
| Another person's house/apt | 9 | 6.8 |
| Foster/group home | 3 | 2.3 |
| Boarding home/shelter/halfway | 11 | 8.3 |
| Other | 5 | 3.8 |
| Psychosocial factors | ||
| Ethnic identity | ||
| Ethnic identity search | 14.2 | 3.0 |
| Affirmation, belonging and commitment | 23.2 | 3.5 |
| Sexual orientation identity | ||
| Personal homonegativity | 23.5 | 10.3 |
| Gay affirmation | 15.3 | 5.7 |
| Morality of homosexuality | 10.8 | 4.1 |
| HIV-positive identity | ||
| HIV stigma: Negative self-image | 37.7 | 8.8 |
| HIV-positive identity: salience | 93.2 | 12.8 |
| Social support | ||
| Emotional support | 16.8 | 3.5 |
| Psychological distress | 1.6 | 1.9 |
| Motivational appraisals | ||
| Future orientation | 47.2 | 6.2 |
| Outcome expectations | 60.6 | 7.6 |
| Efficacy | 24.3 | 3.2 |
| Engagement outcomes | N | % |
| Linkage (time to care-seeking) | ||
| Day of diagnosis | 51 | 42.9 |
| <1 month | 29 | 24.4 |
| 1–3 months | 14 | 11.8 |
| >3 months | 25 | 21.0 |
| Retention (missed appointments) | ||
| No missed appointment in last 3 months | 83 | 62.9 |
| One or more missed appointment in last 3 months | 49 | 37.1 |
| ART utilization | ||
| On ART | 61 | 46.2 |
| Not on ART | 71 | 53.8 |
| ART adherence | ||
| No missed doses in last month | 40 | 65.6 |
| Missed doses in last month | 21 | 34.4 |
Table 2.
Regression Model for Seeking Care on Day of Diagnosis
| Parameter | OR (95% CI) | p Value |
|---|---|---|
| Age | 1.07 (0.84, 1.35) | 0.58 |
| Education | 0.99 (0.41, 2.38) | 0.98 |
| Years since dx | 0.97 (0.75, 1.25) | 0.82 |
| Working | 1.05 (0.48, 2.30) | 0.91 |
| Negative self-image | 1.05 (1.01, 1.10) | 0.028 |
CI, confidence interval; OR, odds ratio.
Table 3.
Regression Model for One or More Missed Appointments in last 3 Months
| Parameter | OR (95% CI) | p Value |
|---|---|---|
| Age | 0.87 (0.67, 1.14) | 0.32 |
| Education | 0.61 (0.24, 1.57) | 0.31 |
| Years since dx | 1.30 (0.98, 1.73) | 0.07 |
| Working | 0.30 (0.12, 0.75) | 0.01 |
| Ethnic affirmation | 0.28 (0.12–0.68) | 0.005 |
| Negative self-image | 0.95 (0.91, 0.99) | 0.028 |
CI, confidence interval; OR, odds ratio.
Table 4.
Regression Model for Being on ART
| Parameter | OR (95% CI) | p Value |
|---|---|---|
| Age | 0.95 (0.75, 1.21) | 0.66 |
| Education | 1.13 (0.47, 2.75) | 0.78 |
| Years since dx | 1.08 (0.84, 1.40) | 0.53 |
| Working | 1.82 (0.81, 4.08) | 0.15 |
| HIV+ identity salience | 1.06 (1.02, 1.09) | 0.001 |
CI, confidence interval; OR, odds ratio.
Results
Sample characteristics
A total of 132 black/African American YB-GBMSM living with HIV participated in the study. Demographic characteristics and engagement outcomes are presented in Table 1. A large proportion of our participants (n=51, 42.9%) reported seeking care on the day that they were first diagnosed with HIV, and the majority reported seeking care within the first month (n=80, 67.3%). The majority reported no missed appointments in the last 3 months (n=83, 62.9%). Less than half of the sample was currently on ART (n=61, 46.2%), and of those participants, the majority (n=40, 65.6%) reported no missed doses in the last month.
Regression analyses
We created a correlation matrix to assess the possibility of multicollinearity between predictor variables; all correlation coefficients were <0.70 (data not shown). The regression models examining the association between psychosocial factors and engagement outcomes are presented in Tables 2–4. For “Time to Care-Seeking.” variables entered into the regression model included demographics (age, education, time since diagnosis, and employment) and Negative Self-Image, which was significant at p=0.06 in the bivariate analysis. Negative Self-Image remained significantly associated with seeking care on the day of HIV diagnosis (OR 1.05; 95% CI 1.01–1.10) in the logistic regression models; this was an inverse association, with a less negative self-image predicting a higher likelihood of same-day care seeking.
For the “Missed Appointments” outcome, the variables included in the model were the aforementioned demographic variables, ethnic identity affirmation, personal homonegativity, negative self-image, psychological distress, and social support. Working (OR 0.30; 95% CI 0.12–0.75) and Ethnic Identity Affirmation (OR 0.28; 95% CI 0.12–0.68) were significant predictors of having fewer missed appointments. Greater Negative self-image (OR 0.95; 95% CI 0.91–0.99) was a significant predictor of having more missed appointments.
For the “ART Utilization” outcome, variables included in the model based on bivariate analyses were demographics, social support, Life Outcome Expectancy, and HIV-Positive Identity Salience. HIV-positive identity salience was a significant predictor of ART utilization (OR 1.06; 95% CI 1.02–1.09) in the regression model.
Finally, for the “Adherence” outcome of missed doses within the last month, variables included in the model were demographics and Gay Affirmation, Personal Homonegativity, and Helplessness. None of these were significant in the regression model (data not shown).
Discussion
YB-GBMSM are entering into HIV care in increasing numbers, and it is critically important to link, retain, and treat these youth in order to prevent HIV-related morbidity and mortality. Despite these widely acknowledged epidemiologic trends and policy priorities, few studies have focused on understanding engagement in care for this specific population. This exploratory study sought to fill this gap by examining different stages of engagement in care and their unique psychosocial correlates within an exclusive sample of YB-GBMSM. Overall, our sample reported high rates of early care-seeking and retention in care. Less than half of our respondents were currently on ART, but of those, the majority reported good adherence. At each stage, different variables from our SAT-informed conceptual framework were significantly associated with engagement in medical care.
The Negative Self-Image component of HIV stigma was significantly negatively associated with early care-seeking on the day of diagnosis. HIV stigma has been similarly described as a barrier to timely linkage in prior, mostly qualitative research, including one study focused on adolescents, which found that healthcare providers perceived stigma to be a major barrier to linkage to care in that age group.31 Qualitative studies focused on barriers to linkage in adults, including studies from both providers' and patients' points of view, have also cited stigma as a critical obstacle at this early stage in the continuum.10,32 Our quantitative findings complement this body of research and similarly suggest that interventions to facilitate timely linkage to care should address internalized stigma in newly diagnosed individuals.
Our measure of retention, missed appointments within the last 3 months, was associated with three of the constructs in our model: The Negative Self-image component of stigma, the Affirmation, Belonging, and Commitment component of ethnic identity, and employment status. Once again, Negative Self-image was associated with a poorer engagement outcome, in this case, higher likelihood of a missed appointment in the last 3 months. This is consistent with other research that has linked patients' perceptions of stigma to interruptions in HIV care in adult populations.33 Affirmation, Belonging, and Commitment to one's ethnic group was associated with fewer missed appointments, consistent with a previously reported analysis in the larger ATN 070 cohort (which was not limited to black youth).22 These results are also consistent with other literature in general adolescent and youth populations, where ethnic identity affirmation is associated with positive adjustment and healthy development, particularly for minority youth.24,34
Employment status (working either full-time or part-time, compared to those participants who did not work at all) also had a positive effect on adherence to medical appointments. This effect was not attenuated or explained by participants' ages or education levels. Although employment may not be instinctively viewed as a psychosocial factor, a substantial body of youth-focused research discusses employment as a key contextual factor with implications for adolescent health and development. However, prior literature on the relationship between youth employment and health outcomes is mixed. Some studies, which predominantly focus on younger, in-school youth, have found higher rates of substance use and sexual risk to be associated with youth employment.35,36 On the other hand, other research highlights benefits of employment as part of youth development and adult identity formation.37 Since our sample was primarily out of school, with an average age of 20, employment was developmentally normative for most of our participants and may reflect a successful transition to adulthood, which has been positively related to engagement outcomes in a prior qualitative study focused on YB-GBMSM.38 Maintaining employment requires a degree of maturity and reliability that may also have a positive impact on engagement in care. Furthermore, employment in older adolescents and emerging adults who may no longer live at home is likely related to greater economic stability, which could also facilitate appointment adherence.
HIV-positive identity salience was positively associated with being on ART. The directionality of this association is unclear; it could be that taking daily medications served as a reminder of one's HIV status, making it more salient in the consciousness of those who have been started on ART. On the other hand, salience of HIV-positive identity, or any chronic illness identity is generally consistent with positive, active coping and adjustment. As the decision to initiate a patient on ART is based in large part on providers' subjective assessments of their psychological stability and ability to adhere, it could be that the salience construct is selecting for well-adjusted participants who are deemed ready to begin ART by their physicians.
We did not find any significant associations with adherence, as measured by self-report of missed doses within the last day, week or month. This was somewhat surprising given the extensive body of research associating ART adherence in youth with psychosocial constructs including some of those measured here, namely, stigma,23 psychological distress,39 and social support.40 Of note, however, the power to assess relationships with this outcome was limited, as the sample size that could report on adherence was restricted to those who had been prescribed ART (less than half of our total sample). Additionally, our measure of psychological distress was based on self-report of mental health care-seeking, which is likely a less sensitive measure of psychological symptomatology than traditional measures of depression that were not available in this dataset.
Relating these findings to our SAT conceptual framework, it was notable that many of the predictors that emerged as significant were the individual-level contextual processes, including psychological constructs that related to participants' identities and self-perceptions (e.g., negative self-image, HIV-positive identity salience, and ethnic identity affirmation), while self-change processes did not appear to be significantly associated with any of our engagement outcomes. At first glance, these findings might imply that the SAT model could be simplified or streamlined for use in this population. It is interesting that other, primarily intervention-focused, applications of SAT to youth and/or HIV-positive populations have focused much more on the self-change processes than the individual contextual factors. However, our parent study was much more focused on assessment of psychological, especially identity-related factors; it may therefore be that our measures of self-change processes were not as strong or precise to capture the importance or effects of these constructs.
Our findings regarding the importance of identity and self-perception complement a recent qualitative investigation of engagement in HIV care among adults in San Francisco, which also highlighted the importance of participants' changing perspectives on HIV, and changing HIV identity as key features of the subjective experience of engaging in HIV care through the continuum, particularly in the immediate post-diagnosis period.14 These authors concluded that interventions to improve engagement in care should address the formation of a healthy HIV-positive identity as a part of the continuum of care. Such research demonstrates that a diagnosis of HIV affects individuals' identity beliefs across age groups; however, identity-related processes are likely to be even more salient for our study population, as they were surveyed during adolescence and emerging adulthood, in which identity formation is a central process.41 For these reasons, not only HIV-related identity constructs, but also constructs related to other parts of respondents' identities (such as ethnic identity) were also important to their ability to engage in healthcare.
Implications
This study represents an early, exploratory step toward understanding relationships between psychosocial factors and engagement in care among YB-GBMSM. However, our findings have potential implications for intervention at multiple levels. By analyzing predictors of engagement among YB-GBMSM who are already in care, we have begun to identify factors that might facilitate retention or alternatively, lead to disengagement. For individual patients and providers, the importance of psychological constructs related to self-perception and identity suggest that integration of mental health support services at various stages along the continuum is important for preventing disengagement from HIV care among YB-GBMSM. Given the salience of ethnic identity in particular, it is critical that mental health and primary care providers be culturally competent and culturally affirming in their treatment of YB-GBMSM. Providers must also be attuned to the potential for negative self-image related to HIV stigma, and should inquire about patients' perceptions of their HIV status as they change over time. Outside of the clinical care setting, additional health promotion interventions should be developed specifically for HIV-positive YB-GBMSM to affirm ethnic identity and assist in coping with HIV-related stigma, as a strategy for optimizing engagement in care.
Institution or community-level interventions aiming to improve linkage to care in YB-GBMSM might focus on our observation that a large proportion of our sample reported attempts to initiate care-seeking on the day of diagnosis. Newer technologies that facilitate translating patients' efforts to seek care into actual linkage, such as point of care CD4/viral load testing, or linkage case management, could be especially helpful for these youth. Finally, the protective effect of work on adherence to medical appointments suggests that at the community level, developing and linking YB-GBMSM to life skills programs that facilitate stable employment may have additional benefit for keeping youth in medical care. Education and awareness programs to decrease stigma against people living with HIV in the wider community could also be helpful for linkage and retention in care among YB-GBMSM.
Strengths and limitations
Our study examined multiple psychosocial constructs as influences on different stages of engagement in HIV care, among a clinical sample of YB-GBMSM living with HIV from various geographic regions across the country. Unlike many other prior studies, we have focused exclusively on YB-GBMSM, with the goal of uncovering findings that are specific to the demographic group with the highest HIV risk. An additional strength was that the majority of measures used were well-established instruments with strong psychometric properties.
Despite these strengths, several limitations bear mention, particularly with respect to measurement. As our analysis was based on a secondary analysis of a self-report dataset, we did not have the requisite information to assess engagement as it is traditionally measured by guidelines such as those put forth by the Institute Of Medicine and the Centers for Disease Control and Prevention.42,43 However, the use of self-report measures can still give valuable insight into engagement in care, perhaps even uncovering additional dimensions of engagement beyond data collected through official channels.14 These were also subject to social desirability and recall biases; future studies in this vein should consider combining clinical chart abstraction data with rigorous psychosocial assessments to test the findings that we have presented. It should also be noted that our participants were recruited from clinical settings, and therefore represented a sample that is more likely to be engaged in care to some degree. Different psychosocial barriers and facilitators may be more salient for YB-GBMSM who are completely out of care. We did not have data about the respondents' disease severity either at diagnosis or at the time of the survey, which would have the potential to affect many of the theoretical relationships discussed here.
A few of the measures had borderline α values: Morality of Homosexuality (α=0.68), Ethnic Identity Search (α=0.70), and Social Support (α=0.70), which has implications for our findings as well. None of these emerged as statistically significant in our analyses; perhaps these associations would have been stronger if our measures were more reliable for this sample of participants. Finally, we should make note of that the fact that several statistically significant associations had odds ratios that bordered one. This may have been partially attributable to a relatively small sample size; however, the clinical significance of these trends remains to be explored in more depth in future research.
Conclusions
Our findings suggest that a more complete understanding of engagement in care among YB-GBMSM includes psychological and contextual factors that go beyond the demographic and clinical covariates that are typically collected in analyses of the HIV care continuum. Perhaps more importantly, these variables/factors vary across the continuum of care—so depending on the specific stage of engagement that is being targeted, interventions may need to address a range of different factors. Ensuring that these young men stay engaged in care is paramount for optimizing the health of YB-GBMSM living with HIV. Future research should include broader representation of the HIV care continuum among YB-GBMSM, including those who are not yet in care and larger numbers of youth who are on ART. Ultimately, this line of research can lead to an improved understanding of the complex nature of engagement in care for YB-GBMSM, in order to inform the design of culturally and developmentally appropriate clinical services to optimize engagement in care for this unique and high-risk group.
Contributor Information
Collaborators: the Adolescent Medicine Trials Network for HIV/AIDS Interventions
Acknowledgments
The Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) is funded by grants 5 U01 HD 40533 and 5 U01 HD 40474 from the National Institutes of Health through the National Institute of Child Health and Human Development (Bill Kapogiannis, MD; Sonia Lee, PhD) with supplemental funding from the National Institutes on Drug Abuse (Nicolette Borek, PhD) and Mental Health (Susannah Allison, PhD; Pim Brouwers, PhD). We acknowledge the contribution of the investigators and staff at the following sites that participated in this study: The following ATN sites participated in this study: University of South Florida, Tampa (Emmanuel, Rebolledo, Callejas), Children's Hospital of Los Angeles (Belzer, Flores, Tucker), Children's National Medical Center (D'Angelo, Hagler, Trexler), Children's Hospital of Philadelphia (Douglas, Tanney, DiBenedetto), John H. Stroger Jr. Hospital of Cook County and the Ruth M. Rothstein CORE Center (Martinez, Bojan, Jackson), University of Puerto Rico (Febo, Ayala-Flores, Fuentes-Gomez), Montefiore Medical Center (Futterman, Enriquez-Bruce, Campos), Mount Sinai Medical Center (Steever, Geiger), University of California-San Francisco (Moscicki, Molaghan, Irish), Tulane University Health Sciences Center (Abdalian, Kozina, Baker), University of Maryland (Peralta, Flores, Gorle), University of Miami School of Medicine (Friedman, Maturo, Major-Wilson), Children's Diagnostic and Treatment Center (Puga, Leonard, Inman), St. Jude's Children's Research Hospital (Flynn, Dillard), Children's Memorial Hospital (Garofalo, Cagwin, Brennan).
This study was scientifically reviewed by the ATN's Behavioral Leadership Group (BLG). The authors wish to acknowledge the input and support of the ATN Coordinating Center for Network scientific and logistical support (Craig Wilson, MD; Cynthia Partlow, MEd); the ATN Data and Operations Center at Westat (Jim Korelitz, PhD; Barbara Driver, RN, MS); and the ATN Community Advisory Board and the youth who participated in the study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control and Prevention. Vital signs–HIV infection, testing, and risk behaviors among youths–United States. Morbid Mortal Weekly Rep 2012;61:971–976 [PubMed] [Google Scholar]
- 2.Prejean J, Song R, Hernandez A, et al. and Hall HIGroup HIVIS. Estimated HIV incidence in the united states, 2006–2009. PloS One 2011;6:e17502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States. 2010 [Google Scholar]
- 4.The White House Office of the Press Secretary. Executive order–HIV care continuum initiative. 2013
- 5.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis 2011;52:793–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mugavero MJ, Amico KR, Horn T, Thompson MA. The state of engagement in HIV care in the United States: From cascade to continuum to control. Clin Infect Dis 2013;57:1164–1171 [DOI] [PubMed] [Google Scholar]
- 7.Hull MW, Wu Z, Montaner JS. Optimizing the engagement of care cascade: A critical step to maximize the impact of HIV treatment as prevention. Curr Opin HIV AIDS 2012;7: 579–586 [DOI] [PubMed] [Google Scholar]
- 8.Hall HI, Gray KM, Tang T, Li J, Shouse L, Mermin J. Retention in care of adults and adolescents living with HIV in 13 U.S. areas. J Acq Immune Defic Syndromes 2012;60: 77–82 [DOI] [PubMed] [Google Scholar]
- 9.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: Exaggerated health disparities. AIDS Patient Care STDs 2014;28:128–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bauman LJ, Braunstein S, Calderon Y, et al. . Barriers and facilitators of linkage to HIV primary care in New York City. J Acq Immune Defic Syndromes 2013;64:20–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muthulingam D, Chin J, Hsu L, Scheer S, Schwarcz S. Disparities in engagement in care and viral suppression among persons with HIV. J Acq Immune Defic Syndromes 2013;63:112–119 [DOI] [PubMed] [Google Scholar]
- 12.Ojikutu B, Nnaji C, Sithole J, Schneider KL, Higgins-Biddle M, Cranston K, Earls F. All black people are not alike: Differences in HIV testing patterns, knowledge, and experience of stigma between U.S.-born and non-U.S.-born blacks in Massachusetts. AIDS Patient Care STDs 2013;27:45–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Christopoulos KA, Das M, Colfax GN. Linkage and retention in HIV care among men who have sex with men in the united states. Clin Infect Dis 2011;52:214–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christopoulos KA, Massey AD, Lopez AM, et al. . “Taking a half day at a time:” Patient perspectives and the HIV engagement in care continuum. AIDS Patient Care STDs 2013;27:223–230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Traube DE, Holloway IW, Smith L. Theory development for HIV behavioral health: Empirical validation of behavior health models specific to HIV risk. AIDS Care 2011;23:663–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ewart CK. Social action theory for a public health psychology. Am Psychol 1991;46:931–946 [DOI] [PubMed] [Google Scholar]
- 17.Rotheram-Borus MJ, Lee MB, Murphy DA, Futterman D, Duan N, Birnbaum JM, Lightfoot M. Teens linked to Care C. Efficacy of a preventive intervention for youths living with HIV. Am J Public Health 2001;91:400–405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lightfoot M, Rotheram-Borus MJ, Tevendale H. An HIV-preventive intervention for youth living with HIV. Behav Modif 2007;31:345–363 [DOI] [PubMed] [Google Scholar]
- 19.Traube DE, Holloway IW, Schrager SM, Kipke MD. Utilizing social action theory as a framework to determine correlates of illicit drug use among young men who have sex with men. Psychol Addictive Behav 2012;26:78–88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Axelrad JE, Mimiaga MJ, Grasso C, Mayer KH. Trends in the spectrum of engagement in HIV care and subsequent clinical outcomes among men who have sex with men (MSM) at a Boston community health center. AIDS Patient Care STDs 2013;27:287–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith LR, Fisher JD, Cunningham CO, Amico KR. Understanding the behavioral determinants of retention in HIV care: A qualitative evaluation of a situated information, motivation, behavioral skills model of care initiation and maintenance. AIDS Patient Care STDs 2012;26:344–355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harper GW, Fernandez IM, Bruce D, Hosek SG, Jacobs RJ, Adolescent Medicine Trials Network for HIVAI. The role of multiple identities in adherence to medical appointments among gay/bisexual male adolescents living with HIV. AIDS Behav 2013;17:213–223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rao D, Kekwaletswe TC, Hosek S, Martinez J, Rodriguez F. Stigma and social barriers to medication adherence with urban youth living with HIV. AIDS Care 2007;19:28–33 [DOI] [PubMed] [Google Scholar]
- 24.Phinney J. The multiground ethnic identity measure: A new scale for use with diverse groups. J Adoles Res 1992;7:156–176 [Google Scholar]
- 25.Roberts R, Phinney J, Masse L, Chen Y, Roberts C, Romero A. The structure of ethnic identity of young adolescents from diverse ethnocultural groups. J Early Adolesc 1999;19:301–322 [Google Scholar]
- 26.Mayfield W. The development of an internalized homonegativity inventory for gay men. J Homosex 2001;41:53–76 [DOI] [PubMed] [Google Scholar]
- 27.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Res Nursing Health 2001;24:518–529 [DOI] [PubMed] [Google Scholar]
- 28.Carter T. HIV-positive identity and health behaviors in adolescents living with HIV. Dissertation in Psychology 2005, University of Miami [Google Scholar]
- 29.Cauce AM, Felner RD, Primavera J. Social support in high-risk adolescents: Structural components and adaptive impact. Am J Community Psychol 1982;10:417–428 [DOI] [PubMed] [Google Scholar]
- 30.Zimbardo P, Boyd J. Putting time in perspective: A valid, reliable individual-differences metric. J Personality Soc Psychol 1999;77:1271–1288 [Google Scholar]
- 31.Fortenberry JD, Martinez J, Rudy BJ, Monte D. Adolescent Trials Network for HIV/AIDS Interventions. Linkage to care for HIV-positive adolescents: A multisite study of the adolescent medicine trials units of the adolescent trials network. J Adolesc Health 2012;51:551–556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fagan JL, Beer L, Garland P, Valverde E, Courogen M, Hillman D, Brady K, Bertolli J, Never In Care P. The influence of perceptions of HIV infection, care, and identity on care entry. AIDS Care 2012;24:737–743 [DOI] [PubMed] [Google Scholar]
- 33.Magnus M, Herwehe J, Murtaza-Rossini M, Reine P, Cuffie D, Gruber D, Kaiser M. Linking and retaining HIV patients in care: The importance of provider attitudes and behaviors. AIDS Patient Care STDs 2013;27:297–303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yasui M, Dorham C, Dishion T. Ethnic identity and psychological adjustment: A validity analysis for European, American, and African American adolescents. J Adolesc Res 2004;19:807–825 [Google Scholar]
- 35.Yeung WJJ, Rauscher E. Youth early employment and behavior problems: Human capital and social network pathways to adulthood. Sociol Perspect 2014;57:382–403 [Google Scholar]
- 36.Bauermeister JA, Zimmerman MA, Gee GC, Caldwell C, Xue Y. Work and sexual trajectories among African American youth. J Sex Res 2009;46:290–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Irwin CE, Jr, Burg SJ, Uhler Cart C. America's adolescents: Where have we been, where are we going? J Adolesc Health 2002;31:91–121 [DOI] [PubMed] [Google Scholar]
- 38.Hussen SA, Andes K, Gilliard D, Chakraborty R, Del Rio C, Malebranche DJ. Transition to adulthood and antiretroviral adherence among HIV-positive young black men who have sex with men. Am J Public Health 2014; June12: e1–e7[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med 2005;10:166–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Naar-King S, Templin T, Wright K, Frey M, Parsons JT, Lam P. Psychosocial factors and medication adherence in HIV-positive youth. AIDS Patient Care STDs 2006;20:44–47 [DOI] [PubMed] [Google Scholar]
- 41.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 2000;55:469–480 [PubMed] [Google Scholar]
- 42.Institute of Medicine of the National Academies. Monitoring HIV care in the United States: A strategy for generating national estimates of HIV care and coverage. 2012 [PubMed]
- 43.Centers for Disease Control and Prevention. Vital signs: HIV prevention through care and treatment—United States. Morbid Mortal Weekly Rep 2011;601618–601623 [Google Scholar]


