Abstract
Background: This study was designed to clarify the influence of metformin on serum carbohydrate antigen 199 (CA199) levels and its associated factors in Chinese type 2 diabetes mellitus (T2DM) patients.
Subjects and Methods: In total, 1,253 T2DM patients were enrolled, including a non-metformin group (n=616), a short-term metformin group (at least 1 week to 2 years; n=325), and a long-term metformin group (≥2 years; n=312). Their clinical and biochemical characteristics were collected and compared. After 1 year, the biochemical parameters were re-examined in 296 patients. Sex hormones were determined, and associations between CA199 and other variables were assessed.
Results: At baseline, the incidence of abnormal CA199 levels was 14.7%, 8.9%, and 4.7% in the non-metformin, short-term metformin, and long-term metformin groups, respectively. CA199 levels in females were significantly higher than in males (P<0.01) and decreased significantly with the time of taking metformin (25.60±13.68 U/mL in non-metformin controls vs. 17.62±10.87 U/mL in the short-term group vs. 10.54±8.14 U/mL in the long-term group; P=0.000). The correlation and multiple stepwise regression analysis revealed that glycosylated hemoglobin, metformin, gender, total cholesterol, and follicle-stimulating hormone were independent impact factors on CA199 concentrations (all P<0.05). Binary logistic regression revealed that the risk of abnormal CA199 concentrations of the total population with short-term metformin or long-term metformin treatment decreased 11% (odds ratio=0.89; P=0.001) and 30% (odds ratio=0.70; P=0.000), respectively, at baseline. After a 1-year follow-up, the incidence of high CA199 level decreased in both the short-term and the long-term metformin group compared with that of controls (P<0.05). The extent of CA199 decrease in the long-term metformin group was the greatest (−17% vs. −4.9% in the short-term group vs. 3% in controls, P=0.000), and the group's risk of high blood CA199 level was reduced 67% (odds ratio=0.33; P=0.023). The reduction in women was more apparent than that in men (−18% vs. −5%, P=0.000).
Conclusions: Metformin therapy reduced the CA199 level in Chinese T2DM patients, and its greatest decrease occurred in women with longer therapeutic time.
Introduction
Carbohydrate antigen 199 (CA199) is a tumor-associated antigen that was originally defined by a monoclonal antibody produced by a hybridoma prepared from murine spleen cells immunized with a human colorectal cancer cell line. Although the serum level of CA199 is elevated in various nonmalignant gastrointestinal diseases,1 its specificity is improved with an increased cutoff value of CA199.2 Thus CA199 still plays a very important role in the diagnosis of digestive system cancer. Furthermore, versus other tumor markers, CA199 was shown to possess the best diagnostic ability for pancreatic cancer (PC).3 It is widely used in the clinical screening and early diagnosis of PC because of its simplicity, low cost, and speed.
As a consequence of the obesity epidemic, diabetes mellitus is increasing globally. Type 2 diabetes mellitus (T2DM) accounts for more than 95% of the cases in the Chinese Han population. T2DM had been proven to be linked to an increased risk of several human cancers, such as liver, pancreatic, colorectal, endometrial, and breast carcinoma as well as non-Hodgkin's lymphoma.4–7 Meanwhile, T2DM is likely the third modifiable risk factor for PC after cigarette smoking and obesity.8 As a traditional biguanide medicine, metformin has been widely used in the treatment of T2DM for more than half a century. Because of its excellent hypoglycemic effect and cardiovascular protective effects, metformin became the first-line approach for medical care of T2DM recommended by multiple international guidelines.9,10 Additionally, increasing numbers of evidence-based studies suggested that metformin administration was associated with reduced risk of several common neoplasms, including colon, pancreas, breast, and lung cancer. At present, the incidence of PC in female T2DM patients is higher than that in males.11 Metformin was demonstrated to decrease the incidence and mortality of PC in patients with T2DM.12 However, there is no relevant literature discussing whether serum CA199 levels have a gender difference and the effect of metformin on it in Chinese T2DM populations. Thus, the aim of this study was to investigate the impact of metformin on serum CA199 levels in Chinese T2DM patients and to identify the factors that affect its efficacy.
Subjects and Methods
In total, 1,253 T2DM patients with normal renal and hepatic function were enrolled, including a non-metformin group (n=616; male:female ratio, 347:269), a short-term metformin group (at least 1 week to 2 years; n=325; male:female ratio, 163:162), and a long-term metformin group (≥2 years; n=312; male:female ratio, 169:143). The mean age was 57.06±11.02 years (range, 13–94 years), and the duration of diabetes was 9.34±6.12 years (range, 3 days–57 years). Nearly one-fourth of the patients (n=296) were followed up for 1 year. The study was approved by the Ethics Committee of the Shanghai Sixth People's Hospital. Written informed consent was obtained from all participants.
Serum CA199 levels were measured using the chemiluminescence method and Access GI monitor kit (Immulite® 2000; Siemens Healthcare Diagnostics, Erlangen, Germany) in all subjects. The normal range for serum CA199 is 0–37 U/mL in Chinese people, and the coefficient of variation is within 3%. A CA199 level higher than 37 U/mL was considered as abnormal. In cases of high CA199 levels, patients also underwent abdominal ultrasonography and computed tomography imaging to exclude a pancreatic tumor.
Gonadal hormones, including estradiol (E2), testosterone (T), follicle-stimulating hormone (FSH), and luteinizing hormone, were determined with a chemiluminescent microparticle immunoassay (Architect i2000SR; Abbott Laboratories, Rungis, France). Fasting plasma glucose was measured by the glucose oxidase method (automatic biochemistry analyzer; Beckman Coulter, Brea, CA). Glycosylated hemoglobin (HbA1c) was detected with a high-performance liquid chromatography assay (Bio-Rad, Hercules, CA). Other biochemical indexes representing the function of liver and kidney such as serum creatinine, alanine aminotransferase, and aspartate aminotransferase were assessed with an enzymatic assay on an automatic analyzer (model 7600-020 biochemistry automatic analyzer; Hitachi, Tokyo, Japan).
All results are expressed as mean±SE values. Differences between two groups were compared by Student's t test (unpaired). Differences among three groups were compared by one-way analysis of variance. Associations between serum CA199 and other variables were assessed with Spearman's correlation analysis and multiple stepwise regression analysis. The odds ratio (OR) value of metformin to decrease an elevated CA199 level was evaluated by binary logistic regression. Statistical analyses were performed using SPSS version 18.0 software (SPSS Inc., Chicago, IL). Statistical significance was set at P<0.05.
Results
The influence of gender on serum CA199 concentrations
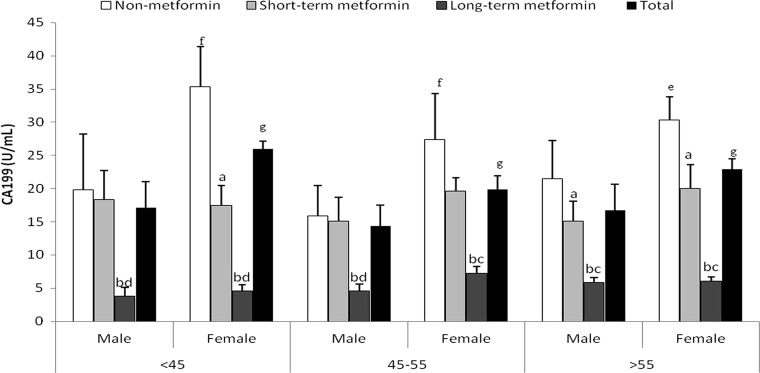
At baseline, in the non-metformin group, the short-term metformin group, the long-term metformin group, and the total group, the levels of CA199 in females were significantly higher than in males (P<0.05) (Table 1). Taking into account that the menopause age of Chinese women is usually between 45 and 55 years, all patients were divided into three age subgroups: <45 years (n=197; male:female ratio, 101:96), 45–55 years (n=343; male:female ratio, 179:164), and >55 years (n=713; male:female ratio, 348:365), and their CA199 levels were compared. The results indicated that the serum CA199 levels of females were obviously higher than those of males regardless of age (P<0.01) (Fig. 1).
Table 1.
Comparison of Baseline Biochemical Parameters and Serum Carbohydrate Antigen 199 Levels in Chinese Type 2 Diabetes Mellitus Patients by Gender
| Non-metformin | Short-term metformin | Long-term metformin | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | |
| n | 347 | 269 | 163 | 162 | 169 | 143 | 679 | 574 |
| Age (years) | 55.22±13.04 | 60.08±21.24b | 54.50±11.38 | 57.73±9.54ah | 56.24±10.23 | 59.58±10.47b | 55.72±12.66 | 59.12±11.45b |
| BMI (kg/m2) | 24.55±3.31 | 23.69±3.28b | 26.07±3.29c | 25.57±4.34h | 25.99±3.31d | 25.64±3.72h | 25.23±3.39c | 24.54±3.73b |
| DM duration (years) | 8.56±7.48 | 10.07±7.27a | 7.70±6.73 | 10.02±7.82a | 8.99±5.74 | 11.19±6.62b | 8.55±6.89 | 10.39±7.27b |
| FPG (mmol/L) | 8.28±2.96 | 8.01±2.74 | 8.31±2.59 | 8.51±2.95 | 8.03±2.66 | 8.25±2.62 | 8.18±2.80 | 8.27±2.74 |
| HbA1c (%) | 9.33±2.51 | 9.08±2.36 | 8.85±1.98 | 9.17±3.69 | 8.18±2.61de | 8.46±2.47 | 8.91±2.51 | 9.00±2.85 |
| GA (%) | 25.48±9.18 | 23.87±7.84a | 23.33±6.63c | 22.73±5.87 | 21.15±6.49d | 21.59±5.36ah | 23.90±8.21 | 23.14±6.87 |
| TC (mmol/L) | 4.67±1.04 | 4.97±1.15b | 4.67±1.21 | 5.11±1.11b | 4.55±0.97 | 4.88±1.03b | 4.62±1.07 | 4.96±1.12b |
| TG (mmol/L) | 1.66±1.21 | 1.63±1.39 | 2.19±1.82c | 2.06±1.62h | 1.94±1.51e | 1.93±1.12bh | 1.86±1.48 | 1.83±1.43g |
| HDL-C (mmol/L) | 1.04±0.28 | 1.23±0.54b | 0.99±0.22 | 1.16±0.29bg | 0.95±0.19d | 1.11±0.25bg | 1.00±0.25 | 1.17±0.34b |
| LDL-C (mmol/L) | 2.75±0.81 | 2.86±0.90 | 2.73±0.75 | 3.16±1.95a | 2.74±0.76 | 2.86±0.81 | 2.74±0.79 | 2.94±1.26b |
| ALT (U/L) | 25.54±20.32 | 23.96±17.48 | 29.25±17.72 | 25.34±17.26 | 26.16±17.82 | 24.28±16.80 | 26.43±19.32 | 24.26±17.01 |
| AST (U/L) | 21.20±10.64 | 22.77±13.24 | 21.76±10.45 | 22.03±10.09 | 20.43±9.32 | 21.35±12.27 | 21.10±10.42 | 22.02±12.31 |
| GGT (U/L) | 34.84±33.67 | 31.44±24.28 | 40.10±33.14 | 35.11±30.72 | 36.04±26.09 | 37.05±50.31 | 36.30±31.24 | 33.97±35.60 |
| BUN (mmol/L) | 6.17±7.16 | 5.75±23.91 | 6.74±14.29 | 4.97±1.33 | 5.47±1.55 | 4.97±1.35b | 6.15±8.73 | 5.37±2.99 |
| Cr (μmol/L) | 81.41±56.67 | 63.54±46.40b | 73.23±13.78d | 53.98±12.15b | 73.41±19.81d | 59.87±54.04b | 77.58±43.78 | 60.28±45.07b |
| UA (μmol/L) | 330.5±88.34 | 289.66±96.51b | 338.07±106. | 299.76±81.32b | 342.72±95.3 | 314.7±69.37bg | 336.30±96.07 | 299.14±88.32b |
| GFR (mL/min) | 101.3±25.23 | 96.07±26.19 | 100.15±23.4 | 97.02±23.56 | 99.13±24.52 | 93.60±23.25 | 100.0±25.08 | 95.56±24.30 |
| E2 (pmol/L) | 126.1±46.11 | 140.0±220.65 | 114.66±44.8 | 107.52±106.27 | 128.96±47.5 | 113.72±109.5 | 124.24±46.35 | 125.52±75.19 |
| T (nmol/L) | 13.97±6.49 | 1.25±1.05b | 13.24±5.29 | 1.31±0.74b | 13.76±5.76 | 3.43±20.20b | 13.77±6.09 | 1.75±9.55b |
| FSH (IU/L) | 11.34±12.68 | 48.44±27.47b | 8.05±3.68c | 41.68±24.97bg | 11.54±11.88e | 43.93±24.25b | 10.68±11.25 | 45.82±26.29b |
| LH (IU/L) | 7.00±5.88 | 25.78±24.08b | 5.72±3.22 | 20.14±14.04bg | 7.16±5.65 | 22.42±15.32b | 6.76±5.39 | 23.67±20.35b |
| PRL (μg/L) | 209.5±119.4 | 261.1±293.2a | 166.04±97.8d | 184.8±130.5 | 222.2±110.3 | 208.31±280.6 | 202.8±114.76 | 231.31±262.52a |
| CA199 (U/mL) | 20.08±23.56 | 30.34±59.66b | 15.26±9.65c | 18.19±11.89ah | 8.15±5.89df | 11.18±9.97bhi | 15.97±18.89 | 22.89±15.03b |
Data are mean±SE values.
P<0.05, bP<0.01 versus males; cP<0.05, dP<0.01 versus males of the non-metformin group; eP<0.05, fP<0.01 versus males of the short-term metformin group; gP<0.05, hP<0.01 versus females of the non-metformin group; iP<0.01 versus females of the short-term metformin group.
ALT, alanine aminotransferase; AST, aspartate aminotransferase; BMI, body mass index; BUN, blood urea nitrogen; CA199, carbohydrate antigen 199; Cr, serum creatinine; DM duration, duration of diabetes mellitus; E2, estradiol; FPG, fasting plasma glucose; FSH, follicle-stimulating hormone; GA, glycosylated serum albumin; GFR, glomerular filtration rate; GGT, γ-glutamyl transpeptidase; HbA1c, glycosylated hemoglobin; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; LH, luteinizing hormone; PRL, prolactin; T, testosterone; TC, total cholesterol; TG, triglyceride; UA, uric acid.
FIG. 1.
Comparison of serum carbohydrate antigen 199 (CA199) levels among three age subgroups in males and females. aP<0.05, bP<0.01 versus the non-metformin group; cP<0.05, dP<0.01 versus the short-term metformin group; eP<0.05, fP<0.01 versus males of the non-metformin group; gP<0.05 versus males of the total group.
Associated factors for serum CA199 levels
Spearman or Pearson correlation analysis showed that serum CA199 levels were positively associated with HbA1c (r=0.295, P<0.001), gender (r=0.125; P<0.001), total cholesterol (TC) (r=0.137; P<0.01), FSH (r=0.122; P<0.01), and luteinizing hormone (r=0.106; P<0.01) and negatively associated with metformin therapy (r=−0.369; P<0.01). Metformin therapy and gender were still significantly correlated with CA199 levels after adjusting for HbA1c and glycosylated serum albumin. Multiple stepwise regression analysis further revealed that HbA1c (β=0.201; P<0.001), metformin (β=−0.268; P<0.001), gender (β=0.132; P<0.001), TC (β=0.066; P<0.05), and FSH (β=0.139; P<0.001) were independent influencing factors of CA199 concentrations.
Characteristics of the metformin-treated and untreated groups at baseline and after 1 year
After a 1-year follow-up, the body mass index differed significantly among the three groups: 26.76±2.68 kg/m2 versus 24.12±3.3 kg/m2 in the non-metformin group, 25.52±3.62 kg/m2 versus 25.7±3.86 kg/m2 in the short-term metformin group, and 23.78±2.42 kg/m2 versus 25.77±3.45 kg/m2 in the long-term metformin group (all P<0.05). At follow-up, HbA1c levels were remarkably reduced in all groups: 9.05±2.14% versus 9.25±2.47% in the non-metformin group, 8.96±3.03% versus 9.05±3.03% in the short-term metformin group, and 7.52±2.59% versus 8.32±2.59% in the long-term metformin group (all P<0.05), after adjusting for FSH in females. However, no significant differences were found in T2DM duration, TC levels, and low-density lipoprotein cholesterol levels (P>0.05).
Metformin therapy affects serum CA 199 levels and the incidence of high blood CA199
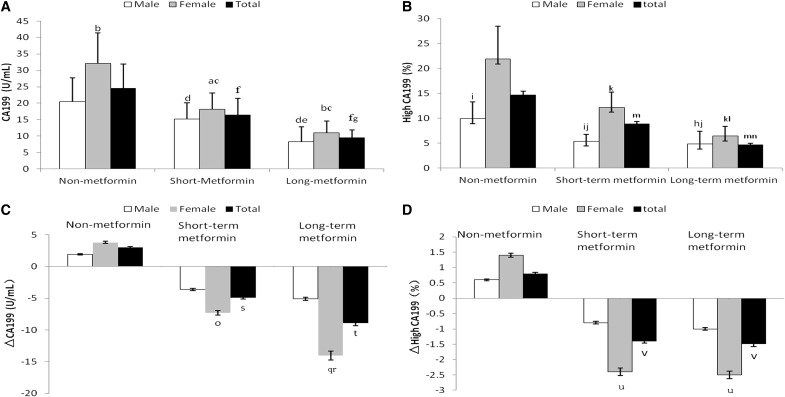
The serum CA199 levels of the short-term metformin group were lower than those of the non-metformin group in both men and women, and those of the long-term metformin group were further decreased compared with the short-metformin group (Fig. 2A).
FIG. 2.
Metformin therapy affects (A) serum carbohydrate antigen 199 (CA199) levels and (B) the incidence of high serum CA199 concentrations in the three groups at baseline and (C) the decreasing percentage of CA199 levels and (D) the high CA199 proportions of the three groups after 1 year of follow-up. (A) aP<0.05, bP<0.01 versus males; cP<0.01 versus females of the non-metformin group; dP<0.01 versus males of the non-metformin group; eP<0.01 versus males of the metformin group; fP<0.01 versus the total of the non-metformin group; gP<0.05 versus the total of the short-term metformin group. (B) hP<0.05, iP<0.01 versus females; jP<0.01 versus males of the non-metformin group; kP<0.01 versus females of the non-metformin group; lP<0.01 versus females of the short-term metformin group; mP<0.01 versus the total of the non-metformin group; nP<0.05 versus the total of the non-metformin group. (C) oP<0.05, qP<0.01 versus females of the non-metformin group; rP<0.05 versus females of the short-term metformin group; sP<0.05, tP<0.01 versus the total of the non-metformin group. (D) uP<0.05 versus females of the non-metformin group; vP<0.05 versus the total of the non-metformin group.
Subjects in the non-metformin group were divided into several groups based on different antidiabetes regimens, and their CA199 levels were compared. The results indicated that there was no difference among these groups (P=0.475).
In the overall population, the total incidence of abnormal CA199 levels was 9.1%; among them, females accounted for 12.7%, and males accounted for 5.8%. At baseline, regardless of whether the patient was in the non-metformin, short-term metformin, or long-term metformin group, the incidence of high CA199 levels in female patients increased significantly compared with that in males, and the incidence decreased significantly with the time of taking metformin (14.7% vs. 8.9% vs. 4.7%, P<0.01) (Fig. 2B).
After a 1-year follow-up, the long-term metformin group achieved the greatest CA199 decrease compared with the short-term group and the non-metformin controls (P<0.05) (Fig. 2C). The range of CA199 decrease in females among the three groups showed a significant difference, but there was no difference in males (Fig. 2C). The decreasing range in metformin-treated females was more apparent than that in males (−18% vs. −5%, P=0.000).
The large decreases in blood CA199 range of the short-term (–1.4%) and long-term (–1.5%) metformin groups were significantly higher than those of the non-metformin controls (0.8%) (both P<0.05), but there was no difference between the short-term and long-term metformin groups (P>0.05) (Fig. 2D). Similarly, the incidence of high blood CA199 levels in females of the two metformin-treated groups was reduced significantly compared with the non-metformin controls. However, there was no difference between the two metformin-treated groups, and there was no difference of the extent of CA199 decrease in males (Fig. 2D).
Risk analysis of metformin to decrease serum CA199 levels
Binary logistic regression revealed that the risk of elevating CA199 levels of metformin-treated groups decreased in both male (short-term metformin group, OR=0.91; 95% confidence interval [CI], 0.88–0.92; P=0.001; and long-term metformin group, OR=0.73; 95% CI, 0.66–0.75; P=0.001) and female (short-term metformin group, OR=0.83; 95% CI, 0.80–0.88; P=0.001; and long-term metformin group, OR=0.61; 95% CI, 0.60–0.70; P<0.001) patients at baseline. After 1 year of therapy, the risk of abnormal CA199 levels in the long-term metformin group was reduced 43% in men and 73% in women patients (OR=0.57; 95% CI, 0.51–0.60; P=0.033; and OR=0.27; 95% CI, 0.20–0.36; P=0.001, respectively) after adjusting for sex, HbA1c, and TC. However, only female subjects showed significant risk reduction of CA199 in the short-term metformin group (OR=0.62. 95% CI, 0.59–0.68; P=0.032) (Table 2).
Table 2.
Risk Analysis of Metformin to Reduce Serum Carbohydrate Antigen 199 Levels
| Unadjusted OR (95% CI) | P | OR adjusted for sex, HbA1c, and TC (95% CI) | P | |
|---|---|---|---|---|
| Baseline | ||||
| Male | ||||
| Non-metformin | 1 | — | 1 | — |
| Short-term metformin | 0.89 (0.86–0.93) | 0.001 | 0.91 (0.88–0.92) | 0.001 |
| Long-term metformin | 0.71 (0.63–0.79) | 0.001 | 0.73 (0.66–0.75) | 0.001 |
| Female | ||||
| Non-metformin | 1 | — | 1 | — |
| Short-term metformin | 0.81 (0.79–0.87) | 0.001 | 0.83 (0.80–0.88) | 0.001 |
| Long-term metformin | 0.63 (0.60–0.69) | 0.000 | 0.61 (0.60–0.70) | 0.000 |
| Total | ||||
| Non-metformin | 1 | — | 1 | — |
| Short-term metformin | 0.88 (0.87–0.91) | 0.001 | 0.89 (0.87–0.92) | 0.001 |
| Long-term metformin | 0.68 (0.64–0.73) | 0.000 | 0.70 (0.65–0.75) | 0.000 |
| Follow-up | ||||
| Male | ||||
| Non-metformin | 1 | — | 1 | — |
| Short-term metformin | 0.72 (0.71–0.83) | 0.103 | 0.74 (0.71–0.83) | 0.076 |
| Long-term metformin | 0.52 (0.49–0.55) | 0.036 | 0.57 (0.51–0.60) | 0.033 |
| Female | — | — | ||
| Non-metformin | 1 | 1 | ||
| Short-term metformin | 0.63 (0.59–0.66) | 0.034 | 0.62 (0.59–0.68) | 0.032 |
| Long-term metformin | 0.29 (0.18–0.27) | 0.001 | 0.27 (0.20–0.36) | 0.001 |
| Total | ||||
| Non-metformin | 1 | — | 1 | — |
| Short-term metformin | 0.68 (0.43–1.07) | 0.096 | 0.66 (0.42–1.05) | 0.081 |
| Long-term metformin | 0.35 (0.14–0.87) | 0.025 | 0.33 (0.13–0.86) | 0.023 |
CI, confidence interval; HbA1c, glycosylated hemoglobin; OR, odds ratio; TC, total cholesterol.
Discussion
This was the first study to demonstrate that metformin reduced serum CA199 levels in a time–effect pattern and with a gender difference in Chinese T2DM patients.
CA199 is a well-known member of the Lewis antigen family,13–16 and it is also the most commonly used biomarker for diagnosis and monitoring of the therapeutic response to PC. The CA199 level in diabetes patients was found to be elevated in acute metabolic situations and correlated very well with blood glucose concentrations.17 In our study, the incidence of high blood CA199 and the blood CA199 levels in women were significantly higher than those of men regardless of whether considering the overall population, the long-term metformin group, the short-term metformin group, or the non-metformin group. In the correlation analysis, it was significantly associated with gender. Multiple stepwise regression analysis further revealed that gender was an independent influencing factor of CA199 concentrations. These results demonstrated that there was a sexual difference of CA199 concentrations in diabetes patients.
Why was there a gender difference in serum CA199 levels in subjects with T2DM? First of all, the differential influence of liver and kidney function on serum CA199 levels between females and males should be taken into account. In this study, the creatinine levels in females were obviously lower than those of of males, but there were no significant differences in uric acid, blood urea nitrogen, alanine aminotransferase, and aspartate aminotransferase. However, the correlation analysis revealed that creatinine was not associated with serum CA199 levels. Therefore, the influence of kidney function could be excluded.
Second, differences in age and diabetes duration in T2DM patients may affect the serum CA199 levels. The age and diabetes duration in female patients were statistically higher than those of males, but correlation analysis showed that there were no significant association among age, diabetes duration, and the serum CA199 concentrations. Thus, the effect of age and diabetes duration on serum CA199 levels could be eliminated.
Finally, the effect of sex hormones on serum CA199 levels should be considered. The present study further indicated that the serum CA199 levels increased with the elevation of FSH, and FSH was also an independent associated factor of CA199. However, there was no significant association among E2, T, and serum CA199 levels. Consequently, these results suggested that one of the reasons that CA199 levels were higher in women than that in men may come from the effect of the circulating FSH levels, but not E2 or T. So far, there is no report about the impact of sex hormones on serum CA199 levels in T2DM patients with normal renal and hepatic function. As for metformin administration, whether metformin could regulate serum FSH levels directly or indirectly by adjusting E2 and T secretion, thus leading to the differences of CA199 levels between men and women, is still unclear. Therefore, it is essential and worthwhile to investigate the mechanism linking serum CA199 with sex hormone levels.
The results of the present study revealed that both at baseline and after a 1-year follow-up, the serum CA199 levels of the long-term metformin-treated group was significantly lower than those of the short-term metformin group and the non-metformin group, and those of the short-term metformin group was lower than those of the non-metformin group. The incidence of high CA199 differed with the duration of taking metformin at baseline. Binary logistic regression revealed that the risk of elevated CA199 levels in patients treated with short-term metformin or long-term metformin decreased 11% and 30%, respectively, at baseline compared with controls. After a 1-year follow-up, the incidence of high CA199 concentrations of the short-term and long-term metformin groups decreased significantly compared with the non-metformin controls, but there was no difference between the two metformin-treated groups. The decreasing extent of CA199 levels in the long-term metformin group was the greatest, the change in females was more apparent than that in males, and the risk of high CA199 levels was reduced 67% after adjusting for HbA1c, sex, and TC level. The correlation and multiple stepwise regression analysis further indicated that metformin therapy was an independent impact factor of serum CA199 concentrations. These results suggest that metformin attenuated serum CA199 levels in a time–effect pattern and with sex difference. The greatest reduction happened in female patients of the long-term metformin group.
Based on a large amount of clinical evidence, metformin became a recommended first-line oral antihyperglycemic agent for medical care of T2DM. Evans et al.18 were the first to report that there was a potential association between metformin use and reduced cancer incidence with a dose–response relationship. Since then, evidence has emerged from several research areas (epidemiological, preclinical, and clinical) suggesting that metformin is useful in the prevention and treatment of various kinds of tumors, including PC.
PC is one of the most lethal malignant diseases because of its high rate of advanced stage at diagnosis and the lack of effective medical treatment. To date, the 5-year survival rate after surgical resection has slowly risen to about 20%, but only 10–15% of patients are candidates for resection. So, more than 95% of all PC patients succumb to their illness within 2 years of diagnosis.19 Therefore, PC was still one of the leading causes of cancer-related deaths.
Risk factors for PC included family history, obesity, smoking, chronic pancreatitis, and diabetes mellitus. After smoking and obesity, T2DM is likely the third modifiable risk factor for PC.8 It has been reported that the prevalence of diabetes and impaired glucose tolerance in PC cases is as high as 80%.20,21 In other words, there is a clear linkage between diabetes mellitus and PC. CA199 is widely used in the clinical screening and early diagnosis of PC, and metformin decreased CA199 levels with a time–effect relationship, especially for the female T2DM patients shown by the present study. Therefore, metformin reduces the incidence of PC in T2DM patients, and female patients will get a greater benefit from this traditional hypoglycemic medicine. These results are of important clinical significance for the early prevention and treatment of PC, at least in populations suffering from T2DM.
The present study has several limitations. First, the sample size of the group of follow-up patients was relatively small. More patients of the above-mentioned three groups should be called back, and the biochemical indexes including CA199 should be reviewed to prove our findings. Second, although there was follow-up for these participants in this study, the follow-up period was quite short. The efficacy of metformin and its related mechanisms on CA199 concentrations and future occurrence of PC are still not entirely clear. Therefore, it is necessary to extend the follow-up time. Long-term follow-up of these patients should be carried out to further clarify the outcomes of metformin on serum CA199 levels and incidence of PC.
In summary, there is a gender difference of serum CA199 levels in Chinese T2DM patients, and CA199 levels in females were significantly higher than those in males. Metformin therapy reduced serum CA199 levels and the incidence of high CA199 levels in T2DM patients, its greater decline effect occurred in women with longer therapeutic time, and its effect was independent of glycemic control and liver and kidney function.
Acknowledgments
We thank the individuals who participated in this study and Dr. Li Shen, who polished the language expression of this article. This work was supported by grants from the National Natural Science Foundation of China (grant 81070650 to F.L. and grant 31171128 to J.Y.).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Levy C, Lymp J, Angulo P, et al. : The value of serum CA199 in predicting cholangiocarcinomas in patients with primary sclerosing cholangitis. Dig Dis Sci 2005;50:1734–1740 [DOI] [PubMed] [Google Scholar]
- 2.Nazli O, Bozdag AD, Tansug T, et al. : The diagnostic importance of CEA and CA199 for the early diagnosis of pancreatic carcinoma. Hepatogastroenterology 2000;47:1750–1752 [PubMed] [Google Scholar]
- 3.Liao Q, Zhao YP, Yang YC, et al. : Combined detection of serum tumor markers for differential diagnosis of solid lesions located at the pancreatic head. Hepatobiliary Pancreat Dis Int 2007;6:641–645 [PubMed] [Google Scholar]
- 4.Pollak M: Insulin and insulin-like growth factor signalling in neoplasia. Nat Rev Cancer 2008;8:915–928 [DOI] [PubMed] [Google Scholar]
- 5.Larsson SC, Mantzoros CS, Wolk A: Diabetes mellitus and risk of breast cancer: a meta-analysis. Int J Cancer 2007;121:856–862 [DOI] [PubMed] [Google Scholar]
- 6.Smith U, Gale EA: Cancer and diabetes: are we ready for prime time? Diabetologia 2010;53:1541–1544 [DOI] [PubMed] [Google Scholar]
- 7.Vigneri P, Frasca F, Sciacca L, et al. : Diabetes and cancer. Endocr Relat Cancer 2009;16:1103–1123 [DOI] [PubMed] [Google Scholar]
- 8.Li D: Diabetes and pancreatic cancer. Mol Carcinog 2012;51:64–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American Diabetes Association: Standards of medical care in diabetes—2013. Diabetes Care 2013;36(Suppl 1):S11–S66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinese Diabetes Society: China Guideline for Type 2 Diabetes—2010. Beijing: Peking University, 2011 [Google Scholar]
- 11.Trna J, Dítӗ P, Adamcová A, et al. : Diabetes mellitus in pancreatic cancer patients in the Czech Republic: sex differences. Exp Diabetes Res 2012;2012:414893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sadeghi N, Abbruzzese JL, Yeung SJ, et al. : Effect of metformin on survival of diabetic patients with pancreatic adenocarcinoma [abstract]. J Clin Oncol 2011;29(Suppl):4063 [Google Scholar]
- 13.Jiang XT, Tao HQ, Zou SC: Detection of serum tumor markers in the diagnosis and treatment of patients with pancreatic cancer. Hepatobiliary Pancreat Dis Int 2004;3:464–468 [PubMed] [Google Scholar]
- 14.Ziske C, Schlie C, Schmidt-Wolf IG, et al. : Prognostic value of CA199 levels in patients with inoperable adenocarcinoma of the pancreas treated with gemcitabine. Br J Cancer 2003;89:1413–1417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schlieman MG, Ho HS, Bold RJ: Utility of tumor markers in determining respectability of pancreatic cancer. Arch Surg 2003;138:951–955; discussion 955–956 [DOI] [PubMed] [Google Scholar]
- 16.Micke O, Bruns F, Schäfer U, et al. : Predictive value of carbohydrate antigen 199 in pancreatic cancer treated with radiochemotherapy. Int J Radiat Oncol Biol Phys 2003;57:90–97 [DOI] [PubMed] [Google Scholar]
- 17.Benhamou PY, Vuillez JP, Halimi S, et al. : Influence of metabolic disturbances of diabetes mellitus on serum CA199 tumor marker. Diabet Metab 1991;17:39–43 [PubMed] [Google Scholar]
- 18.Evans JM, Donnelly LA, Emslie-Smith AM, et al. : Metformin and reduced risk of cancer in diabetic patients. BMJ 2005;330:1304–1305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edwards BK, Brown ML, Pickle LW, et al. : Annual report to the nation on the status of cancer, 1975–2002, featuring population-based trends in cancer treatment. J Natl Cancer Inst 2005;97:1407–1427 [DOI] [PubMed] [Google Scholar]
- 20.Wakasugi H, Funakoshi A, Iguchi H: Clinical observations of pancreatic diabetes caused by pancreatic carcinoma, and survival period. Int J Clin Oncol 2001;6:50–54 [DOI] [PubMed] [Google Scholar]
- 21.Pannala R, Leirness JB, Bamlet WR, et al. : Prevalence and clinical profile of pancreatic cancer-associated diabetes mellitus. Gastroenterology 2008;134:981–987 [DOI] [PMC free article] [PubMed] [Google Scholar]