Abstract
Objective
This prospective study tested the hypothesis that psychological dysregulation in mid-adolescence (age 16) mediates the association between parent-child attachment in late childhood (age 10-12) and development of substance use disorder (SUD) in adulthood (age 22).
Method
The Youth Attachment to Parents Scale (YAPS) was developed in 10-12 year old boys and girls (N = 694) at baseline residing in western Pennsylvania. Psychological dysregulation was measured by the neurobehavior disinhibition trait. Substance use was assessed at ages 10-12, 12-14, 16 and 19. SUD was diagnosed at age 22 using the Structured Clinical Interview for DSM Disorders. The mediation of parent-child attachment and SUD by neurobehavior disinhibition was tested separately for mothers and fathers while controlling for baseline substance use.
Results
Psychological dysregulation mediates the association between attachment to mothers and SUD, and partially mediates the association between attachment to fathers and SUD. Significant mediation effects remains after controlling for baseline substance use.
Conclusion
Optimal prevention of SUD should include ameliorating both psychological dysregulation predisposing to SUD and quality of the parent-child relationship.
Keywords: Parent-child attachment, substance use disorder, psychological dysregulation
Introduction
Substance use (SU) and its medical/psychiatric outcome, substance use disorder (SUD) constituting abuse and dependence, exert a heavy toll on society. While it is not possible to precisely specify the cost, government-sponsored insurance programs are billed for over half of all hospital stays for problems directly caused by or co-occurring with SU and SUD (1). Expenditures exceed all other medical/psychiatric disorders (2), approximating six hundred billion dollars annually (3). Over two million emergency room visits in 2011 pertained to substance use (4). Enormous societal resources allocated for health services delivery are a consequence of the high prevalence of SUD. For example, lifetime prevalence of SUD in the U.S. consequent to habitual consumption of tobacco, alcohol, and illegal drugs is 25%, 20%, and 10% (5, 6, 7). Costs related to crime, accidents, underemployment, injury, disease transmission and loss of life further add to the societal burden. Accordingly, high priority is attached to elucidating the origins of SU/SUD within a developmental framework so that effective prevention can be implemented at targeting the predisposing factors.
Toward this goal, it is well known that deficient parenting skills (8), inconsistent and conflictual communication (9, 10), low supervision (11) and punitive discipline (12) amplify risk for initiating SU and subsequently developing SUD (13). In addition, neglectful parenting augments risk for these outcomes (14). Although neglectful parenting occurs for a variety of reasons, the common thread linking neglect to SU and SUD is a weak emotional bond between parents and child. Parental bonding to a newborn requires investment of resources and effort, whereas in older children, maintaining a strong parent-child bond is contingent on both parent and child. This mutually influencing process is especially important for elucidating the etiology of SUD, considering that characteristics of the child that commonly presage SUD (e.g. difficult temperament, ADHD, conduct problems) and characteristics of parents (e.g. SUD-related impairments) hamper maintenance of the parent-child bond.
Parental attachment, defined as an enduring emotional bond and engagement between child and parent (15), has not been systematically studied with respect to development of SUD. This is not surprising considering that attachment typically manifests by two years of age (15, 16) and peak incidence of SUD occurs almost two decades later (17). Hence, long-term tracking is required to document the influence of parent-child bonding on SU and SUD etiology. Furthermore, many factors occurring throughout the long period of development influence the quality of the parent-child relationship, such as changing life circumstances in the parent (e.g. divorce, job loss, medical illness, psychiatric disorder) and the child (e.g. friendships, school).
Instruments measuring attachment have been developed for young children (Strange Situation) (18), as well as for youths during middle childhood and adolescence (People in My Life Scale) (19, 20, 21). A gap exists, however, for measurement of attachment in pre-adolescent older children. This shortcoming impedes delineating SUD etiology within an ontogenetic framework, considering that first exposure to abusable substances often occurs during this developmental period or soon thereafter. Accordingly, the first aim of this study was directed at deriving an attachment scale for 10-12 year old children.
Additionally, behavior undercontrol in childhood, often manifesting in context of a psychiatric disturbance (e.g. ADHD, conduct disorder), predisposes adolescents to SU and SUD (22, 23) and is frequently linked to the parent-child relationship. In view of these findings, the hypothesis is advanced that psychological dysregulation at middle adolescence (age 16) mediates the association between attachment to parents during childhood (age 10-12) and SUD in early adulthood (age 22). Confirmation of this hypothesis advances understanding of SUD etiology, as well as informs prevention. Specifically, in conformance with the NIH Roadmap (24), confirmation of this hypothesis illustrates the need for a two-pronged approach to SUD prevention directed at potentiating acquisition of psychological self-regulation during ontogeny along with consolidating a strong parent-child affectional bond.
Methods
Subjects
Based on extensive evidence showing that children of SUD+ fathers are at greatly elevated risk for SUD, the proband was the biological father who either qualified for SUD diagnosis concomitant to consumption of illegal drugs (SUD+; N = 344) or had no adult onset Axis I or II psychiatric disorder (SUD−; N = 350). Fathers were recruited from the western region of Pennsylvania using public service announcements, advertising, and random digit telephone calls. Approximately 20% of the SUD+ men were recruited from treatment facilities. Forty-nine percent of all contacts with potential probands who met study criteria agreed to participate. Their sons were evaluated at age 10-12 and re-contacted for follow-up study when the sons attained 12-14, 16, 19, and 22 years of age. Four years after recruitment was initiated, the study was expanded to include daughters, resulting in a smaller female subsample. Exclusion criteria, limited to factors that could invalidate the results, were positive urine drug or breath alcohol screen, neurological disease, physical disability, uncorrected sensory impairment, psychosis, and fetal alcohol effects determined from mother’s report of her drinking history and direct physical examination of the child.
Attrition, defined as failure to locate the individual or his/her refusal to participate between baseline and age 22 follow-up, was 35%. The demographic characteristics of the retained and attrited subjects are shown in Table 1. Ethnicity, sex distribution, and rate of parental SUD did not differ between these two segments of the sample. IQ measured by the Wechsler Intelligence Scale for Children, 3rd edition (WISC-III-R) (25) was, on average, six points lower in participants who attrited. However, both attrited and retained subjects scored in the average range of intelligence. The participants who attrited before age 22 also scored three points lower on the Hollingshead index (26). Nevertheless, retained and attrited participants were at baseline derived from the lower middle socioeconomic stratum.
Table 1.
Characteristics of the Sample at Baseline (10-12 years of age)
| Retained | Attrited | |||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | |
|
|
|
|||||
| Family Socioeconomic Status | 42.1 | 13.8 | 39.0 | 13.3 | 2.8 | .005 |
| Full-Scale IQ | 108.8 | 16.1 | 102.9 | 15.6 | 4.5 | <.001 |
|
| ||||||
| N | % | N | % | χ 2 | p | |
|
|
||||||
| Ethnicity | 1.0 | .59 | ||||
| European American | 319 | 74 | 166 | 71 | ||
| African American | 99 | 23 | 60 | 26 | ||
| Other | 11 | 3 | 8 | 3 | ||
| Sex | 5.0 | .03 | ||||
| Male | 305 | 71 | 185 | 79 | ||
| Female | 124 | 29 | 49 | 21 | ||
| Risk Group | 3.0 | .57 | ||||
| SUD+ fathers | 201 | 47 | 115 | 49 | ||
| SUD− fathers | 228 | 53 | 119 | 51 | ||
Note: SUD+ and SUD− fathers indicate fathers with DSM-III-R lifetime substance use disorder and fathers with no Axis I or II psychiatric disorders, respectively. Range of Family SES: 6 to 66. Range of IQ: 68 to 150.
Measures
Youth Attachment to Parents Scale (YAPS) (age 10-12)
The YAPS was designed to measure trust, communication, and alienation specific to the child’s relationship with each parent. These measurement domains parallel the People in My Life (PIML) scale (19, 20). The items comprising the YAPS were selected from the Revised Parent-Adolescent Communication Form (27), Child’s Relationship with Caretaker Scale (27), Supervision/Involvement Scale (28), Children’s Report on Parental Behavior Inventory (29), and the Dyadic Scale in the Family Assessment Measure (30). Using a 4-point Likert format, the children rated their relationship with each parent. The items comprising the YAPS are presented in Table 2.
Table 2.
Factor structure of the Youth Attachment to Parents Scale Attachment to Father – Attachment to Mother
| Loadings | ||||||
|---|---|---|---|---|---|---|
| Factor Matrix | Father | Mother | ||||
| 1st Order Factors | C | A | T | C | A | T |
|
| ||||||
| C1. Can you discuss your beliefs with your father/mother without feeling afraid | .58 | .09 | .14 | .59 | .04 | .16 |
| C2. Is your father/mother a good listener | .47 | .21 | .20 | .57 | .23 | .09 |
| C3. Are you very satisfied with how your father/mother and you talk together | .53 | .21 | .17 | .57 | .15 | .11 |
| C4. If you were in trouble, could you tell your father/mother | .59 | .11 | .17 | .59 | .12 | .16 |
| C5. Do you openly show your father/mother that you like him | .46 | .22 | .16 | .50 | .15 | .17 |
| C6. Does your father/mother try to understand what you think | .53 | .20 | .10 | .52 | .20 | .08 |
| C7. Do you think you can tell your father/mother how you feel about some things | .34 | .05 | .15 | .40 | .11 | .10 |
| C8. Do you tell your father/mother about your person problems | .56 | .17 | .18 | .59 | .12 | .24 |
| C9. Do you keep your feelings to yourself rather than tell your father/mother | .39 | .10 | .18 | .45 | .10 | .15 |
| C10. If you get upset, does your father/mother try to find our what is the matter | .43 | .21 | .13 | .39 | .15 | .10 |
| C11. Does your father/mother encourage you to think about things yourself | .47 | .20 | .06 | .39 | .15 | .07 |
| C12. Can you let your father/mother know what is bothering you | .67 | .12 | .17 | .68 | .08 | .14 |
| C13. If you do something wrong, does your father/mother need to listen to your side | .50 | .26 | .17 | .47 | .23 | .20 |
| C14. Does your father/mother make you feel free to say what you think | .49 | .14 | .21 | .50 | .13 | .18 |
| C15. How often have you thought your father/mother was really good | .34 | .18 | .19 | .38 | .15 | .12 |
| C16. How often does your father/mother find time to listen to you when you want | .44 | .23 | .18 | .46 | .15 | .19 |
| A1. My father/mother makes me feel better after I talk over my worries | .37 | .44 | .23 | .32 | .41 | .21 |
| A2. My father/mother understands my problems and my worries | .35 | .55 | .20 | .34 | .54 | .14 |
| A3. My father/mother gives me a lot of care and attention | .32 | .60 | .23 | .24 | .58 | .13 |
| A4. My father/mother seems proud of the things I do | .18 | .59 | .16 | .15 | .58 | .11 |
| A5. My father/mother isn’t interested in changing me, but likes me as I am | .13 | .42 | .20 | .09 | .45 | .14 |
| A6. I like to talk to and be with my father/mother much of the time | .24 | .56 | .20 | .20 | .49 | .18 |
| T1. When I’m upset, my father/mother usually knows why | .25 | .21 | .43 | .23 | .10 | .39 |
| T2. When I’m upset, I know my father/mother really cares | .17 | .13 | .68 | .08 | .06 | .62 |
| T3. When I have a problem, my father/mother helps me solve it | .19 | .13 | .63 | .10 | .01 | .65 |
| T4. My father/mother is available when I want to talk to him/her | .23 | .20 | .51 | .16 | .08 | .54 |
| T5. My father/mother expects too much of me | .21 | .18 | .43 | .18 | .18 | .40 |
| T6. Even if my father/mother disagrees, he still listen to my point of view | .20 | .22 | .50 | .20 | .21 | .47 |
| T7. My father/mother really trusts me | .15 | .11 | .69 | .14 | .14 | .51 |
| T8. I can count on my father/mother to help me in a crisis | .15 | .14 | .69 | .16 | .16 | .63 |
| T9. We don’t really trust each other | .11 | .10 | .42 | .12 | .15 | .44 |
|
| ||||||
| 2nd Order Factor | Attachment | Attachment | ||||
|
| ||||||
| Communication | .79 | .77 | ||||
| Alienation | .78 | .68 | ||||
| Trust | .68 | .61 | ||||
Note: Bold values indicate largest loadings onto each factor and corresponding factor items. Factor items summed for 2nd order factor analysis. C = Communication, A = Alienation, T = Trust. Cronbach’s alpha: fathers = .91, mothers = .90.
Exploratory factor analysis (EFA) was conducted on items shown in Table 2 using SPSS 19 (31). Although confirmatory factor analysis (CFA) is frequently used when an a priori model is implied, replication of a hypothesized factor structure by a data-driven EFA provides stronger confirmation of the model (32). In the EFA, factors were extracted using the maximum likelihood estimation method with varimax rotation. The criteria used to determine retention of factors included scree plots, item loadings, proportion of item covariances accounted for by each factor, eigenvalue-greater-than-one rule, interfactor correlations and face validity based on the PIML. It was expected, based on previous literature, that (a) the EFA would result in three first-order factors corresponding to trust, communication, and alienation, (b) the factors are highly correlated, and thus (c) a single second-order factor (attachment) exists (19, 20, 33). This implied model (i.e., three first-order factors and one second-order factor) is just identified, which superficially imposes perfect fit in CFA (34). Thus, to statistically test the fit of this model, EFA was conducted on the first-order factors (each summed scores of their respective items) using the same criteria noted above. In addition, a factor difference ratio [(eigenvalue 1) − (eigenvalue 2) / (eigenvalue 2) − (eigenvalue 3)] of three or greater was required to accept a single higher order factor (35).
Eigenvalues on the scales measuring attachment to fathers are 1 = 8.89, 2 = 2.18, 3 = 1.46, 4 = 1.21, 5 = 1.09, +5 < 1. For mothers, they are 1 = 7.81, 2 = 2.29, 3 = 1.65, 4 = 1.19, 5 = 1.08, +5 < 1. Scree plots of the eigenvalues reveal a three-factor solution accounting for 40.4% and 38% of inter-item variance on the YAPS in fathers and mothers, respectively. The factors, shown in Table 2, indicate that each item loads on only one factor. However, the three first-order factors are significantly inter-correlated: communication and alienation (father r = .62, p < .001; mother r = .52, p < .001), communication and trust (father r = .53, p < .001; mother r = .46, p < .001), and alienation and trust (father r = .54, p < .001; mother r = .42, p < .001). Accordingly, a second order factor may therefore constitute a more parsimonious measure of attachment. To examine this possibility, EFA was performed on the scores of the first-order factors. The results, shown in the bottom of Table 2, reveal that the second order factor accounts for 70.7% of variance in fathers and 64.6% of variance in mothers. In addition, Cronbach’s alphas are .91 and .90, repectively, for fathers and mothers. Moreover, the factor difference ratio index values (father = 15.21; mother = 10.85) exceed the criterion to accept a higher order factor (35). Based on these findings, the second order factor score was used in the analyses.
Substance Use (age 10-12, 12-14, 16, 19)
Past thirty-day frequencies of cannabis, alcohol, and tobacco use were evaluated using the Drug Use Screening Inventory (DUSI-R) (36). A continuous substance use involvement index (SII) was also derived from the Drug Use Chart (37) as previously described using item response theory (38). The Drug Use Chart measures lifetime exposure to 42 psychoactive substances grouped into 10 drug categories aligned with the DSM-IV.
Substance Use Disorder
The Structured Clinical Interview for DSM-III-R (SCID) (39) was administered by trained master-level clinical associates when the participants reached 22 years of age. Notably, this approximates the peak incidence age for SUD (17). The “best estimate” procedure (40) was used by a committee consisting of a psychiatrist certified in addiction psychiatry, another psychiatrist or clinical psychologist, and the clinical associates who conducted the interviews to consensually formulate SUD diagnosis. The binary outcome variable was presence or absences of any type of SUD with exception of disorder related to nicotine and caffeine use. These latter disorders are not usually associated with social maladjustment. Thirty-three percent of the sample qualified for SUD (39% of children of SUD+ fathers; 29% of children of SUD− fathers).
Drug use evaluated by the DUSI-R and SII, and SUD diagnosis evaluated by the SCID, provided the predictive validity criteria of the YAPS. In this fashion, correspondence between the purposeful use of the YAPS and different prospective manifest processes, namely substance use and SUD, was evaluated (32).
Psychological Self-Regulation
The neurobehavior disinhibition (ND) trait (41) was measured at age 16 pursuant to the hypothesis that low psychological self-regulation mediates the association between attachment in childhood and SUD in adulthood. This trait has been previously demonstrated to predict SUD (41). The variables comprising the ND trait encompass executive cognitive functioning, affect regulation, and behavior control. The executive cognitive variable is the factor score derived from the Stroop, Porteus Maze, Vigilance, Forbidden Toys, and WISC-III-R Block Design test scores. The affect variable is the difficult temperament index (12) derived from the revised Dimensions of Temperament Survey (42). The behavior variable is the factor score of the number of symptoms endorsed in the conduct disorder, oppositional defiant disorder, and attention deficit/hyperactivity disorder sections of the Kiddie-Schedule for Affective Disorders and Schizophrenia interview (43), and score on the Disruptive Behaviors Disorders Rating Scale (44). Predictive, construct, concurrent, and discriminant validity of the ND trait have been documented (45).
Statistical Analysis
Predictive criterion validity of the YAPS was evaluated by computing its correlation with the DUSI-R and SII scores, and performing logistic regression between the YAPS and SUD diagnosis. Temporal stability of the factor was examined using Pearson correlation between YAPS score at age 10-12 and YAPS score at age 12-14. Effect size (46) of .10, .30, and .50 indicate low, medium, and strong validity. The statistical analyses were conducted using Mplus (47) and Sobel’s method (48) for examining mediation with the following parameters: 1) Independent variable (attachment at age 10-12) predicts dependent variable (SUD at age 22); 2) Attachment predicts putative mediator (ND trait at age 16); and 3) ND predicts SUD. Full mediation is present if the ND trait reduces the association between attachment and SUD to non-significance whereas partial mediation is present if the magnitude of association is reduced but still significant. The timing of the variables was selected to attain temporal precedence and increase the strength of the mediation model (49). Mediation analyses were conducted separately for attachment to mothers and fathers, while controlling for baseline (age 10-12) substance use measured by the Drug Use Chart. Additional mediation analyses were conducted separately for children having SUD+ and SUD− fathers. Differences in YAPS and ND scores between the two groups of subjects were analyzed using one-way ANOVA.
Results
The small portion of the sample living away from their biological fathers (N = 46) trended toward lower attachment scores (t = 1.857, p = .064). Removing these individuals from the analysis did not, however, change the results. Accordingly, the following description of results includes this subgroup.
Validity and Stability of the Youth Attachment to Parents Scale (YAPS)
Correlations between attachment and substance use frequency and involvement are shown in Table 3. As can be seen, attachment to fathers and mothers at age 10-12 correlates with cannabis use frequency at ages 16 and 19, but at age 12-14 this association is present for only the fathers. Attachment to fathers and mothers correlates with alcohol use frequency at age 19, but at age 12-14, this association is present for only the fathers. Tobacco smoking correlates with attachment to fathers and mothers at ages 12-14, 16 and 19. In addition, attachment to fathers and mothers correlates with substance use involvement at ages 16 and 19, but at age 12-14 this association is present for only the mothers. Attachment to the fathers (OR = .900, p < .001, 95% CI [.852, .951]) and mothers (OR = .921, p = .008, 95% CI [.867, .978] predicts SUD at age 22. Furthermore, the YAPS score at age 10-12 correlates with YAPS score at age 12-14 (fathers: r = .518, p < .001; mothers: r = .546, p < .001). These results, in combination with analyses reported above, document the predictive criterion validity and temporal stability of the YAPS.
Table 3.
Criterion Validity of the Youth Attachment to Parents Scale
| Attachment |
||||
|---|---|---|---|---|
| Substance Use | Age | Mean (SD) | Father | Mother |
| Cannabis Use Frequency | ||||
| 12-14 | .05 (.30) | −.17*** | −.06 | |
| 16 | .33 (.85) | −.16*** | −.16*** | |
| 19 | .88 (1.32) | −.19*** | −.17*** | |
| Alcohol Use Frequency | ||||
| 12-14 | .12 (.45) | −.08* | −.07 | |
| 16 | .33 (.65) | −.07 | −.03 | |
| 19 | 1.07 (1.07) | −.09* | −.08** | |
| Smoke Tobacco Frequency | ||||
| 12-14 | .19 (.74) | −.16*** | −.09* | |
| 16 | .63 (1.33) | −.10* | −.17*** | |
| 19 | 1.24 (1.70) | −.20*** | −.16*** | |
| Substance Use Involvement Index | ||||
| 12-14 | −.07 | −.13** | ||
| 16 | −.13** | −.16*** | ||
| 19 | −.18*** | −.17*** | ||
Note: Frequency of use in the past 30 days range on Likert scale: 0; 1 = 1-2; 2 = 3-9; 3 = 10-20; 4 = more than 20 times. Substance Use Involvement Index was constructed to be normally distributed. Correlations are Pearson r.
P ≤ 0.05,
P ≤ .01,
P ≤ .001
Neurobehavior Disinhibition Mediates the Association Between Attachment to Parents and SUD
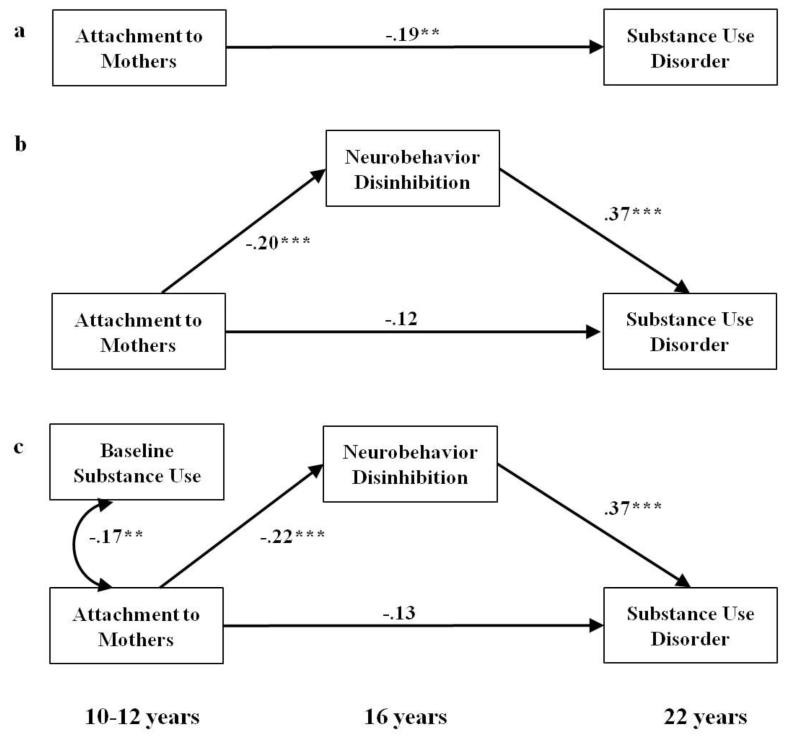
Figures 1 and 2 depict the path coefficients relating attachment, ND score and SUD. As observed in Figure 1a,b, 1) stronger attachment to mothers predicts lower rate of SUD; 2) stronger attachment to mothers predicts lower ND score; and 3) higher ND score predicts SUD. The association between attachment to mothers and development of SUD (β = −.192, p = .009) reduces to non-significance upon adding the ND mediator (β = −.118, p = .097). Hence, ND mediates the association between attachment to mother and SUD (β = −.073, z = −2.926, p = .003). After controlling for substance use at baseline, the model retained all significant path coefficients (see Figure 1c) and a significant mediation effect (β = −.083, z = −3.379, p = .001) with good fit (χ2 = 5.389, d.f. = 2, p = .068, CFI = .945, TLI = .835, RMSEA = .049).
Figure 1.
Neurobehavior Disinhibition Mediates Attachment to Mothers and Substance Use Disorder
Note: Results of mediation analysis depicting associations and standardized beta coefficients. Mediation analysis controlled for substance use at baseline (age 10-12) in (c).
* P ≤ 0.05, ** P ≤ .01, *** P ≤ .001
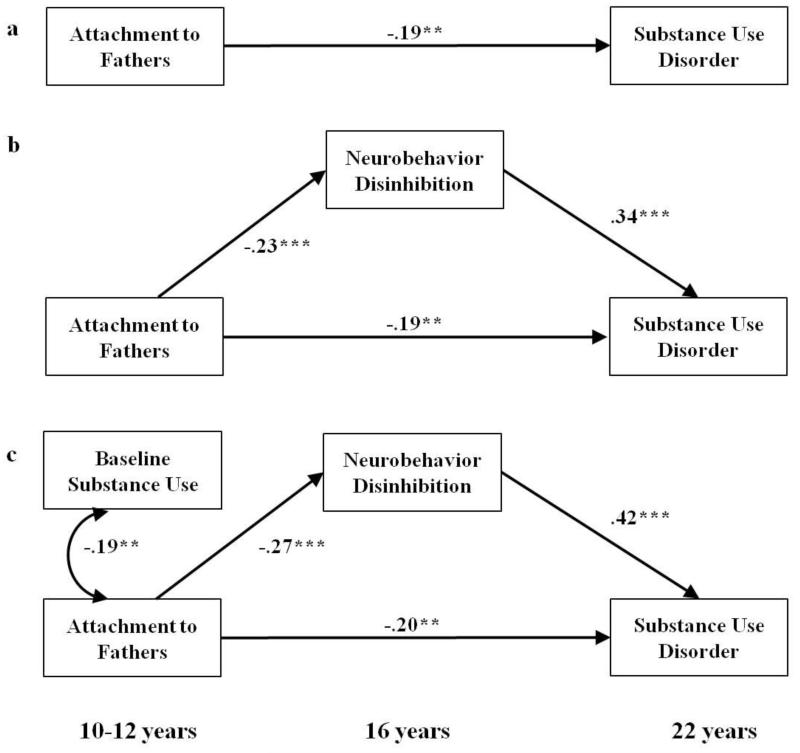
Figure 2.
Neurobehavior Disinhibition Mediates Attachment to Fathers and Substance Use Disorder
Note: Results of mediation analysis depicting associations and standardized beta coefficients. Mediation analysis controlled for substance use at baseline (age 10-12) in (c).
* P ≤ 0.05, ** P ≤ .01, *** P ≤ .001
Following the same procedure for fathers, it can be seen in Figure 2a,b that 1) stronger attachment to fathers at age 10-12 predicts lower rate of SUD; 2) stronger attachment to fathers predicts lower ND scores; and 3) higher ND predicts SUD outcome. The association between attachment to father and SUD (β = −.272, p < .001) remains significant upon adding ND as the mediator (β = −.194, p = .008). However, ND retains a significant mediation effect on the association between attachment to fathers and child’s SUD outcomes (β = −.076, z = −3.201, p = .001). Hence, ND is a partial mediator of the relationship between attachment to father and risk of developing SUD at age 22. The model retained all significant path coefficients (see Figure 2c) and a significant mediation effect after controlling for baseline substance use (β = −.112, z = −4.091, p < .001) with good fit (χ2 = 5.19, d.f. = 2, p = .075, CFI = .969, TLI = .908, RMSEA = .048).
Upon separating subjects having either SUD+ fathers or SUD− fathers, it was found that ND remained a mediator, except in the association between attachment to mothers and SUD in subjects with SUD+ fathers, where the mediation effect trended toward significance (β = −.090, z = −1.791, p = .073). Subjects having SUD+ fathers exhibited weaker attachment to fathers (F(1,571) = 10.094, p = .002) and mothers (F(1,577) = 4.522, p = .034) along with more severe ND (F(1,505) = 43.255, p < .001).
Discussion
Two main findings emerged from this study. First, the Youth Attachment to Parents Scale (YAPS) was shown to have sound construct, predictive criterion validity, temporal stability, as well as excellent internal reliability. Hence, the YAPS is a useful measure of child’s attachment to fathers and mothers. And second, applying the YAPS in prospective analysis, it was demonstrated that psychological dysregulation in mid-adolescence mediates the association between attachment in late childhood and SUD in early adulthood. Thus, conforming to findings obtained in young children (50, 51, 52), it can be concluded that quality of parent-child attachment in late childhood is integral to risk for developing SUD. Notably, however, the role of attachment on development of SUD is not identical in the mother-child and father-child relationship.
These results add to a substantial literature documenting the importance of the parent-child relationship on child’s risk for SUD. However, whereas previous studies have shown that parenting style (53) and parenting skills (54, 55) are related to the child’s propensity to engage in socially non-normative and illegal behaviors including substance use (10, 21, 56, 57), the present study demonstrates the importance of affective bonding during the developmental period proximal to adolescence, when opportunities for substance use initiation markedly increase.
Suboptimal parent-child attachment hampers caregiver motivation to invest in the child’s well-being and accordingly impedes consistent and effective supervision and protection (58). Where low attachment is the outcome of parental disengagement and neglect, the child’s risk for antisocial behavior, which often occurs in conjunction with substance abuse, is greatly increased (59). Even in the absence of neglect, the results obtained in this study indicate that low attachment needs to be taken into account along with parenting skills and discipline practices to reduce the child’s SUD risk. In effect, family-based prevention programs should support a positive father-child and mother-child relationship as the foundation for receptivity to and motivation for behavior change in each member of the dyad.
The results reported herein underscore the importance of longitudinal research to clarify how parents and children reciprocally influence each other during attachment formation and its maintenance with respect to charting the developmental trajectory to SUD. For example, insecure attachment at five years of age predicts emergence of callous-unemotional disposition (60), which in turn, impacts on parental involvement (61). Inasmuch as valid instruments for measuring attachment in early, middle, and late childhood, as well as adolescents are now available, it is therefore feasible to monitor quality of the parent-child bond within an ontogenetic model of SUD etiology (62, 63). Moreover, considering that quality of attachment fluctuates concomitant to changes in parent (e.g. progressive adverse effects of substance use and SUD) and child’s characteristics (e.g. sexual, physical, and neurological maturation), it is important to monitor the strength and stability of the dyadic relationship so that interventions can be implemented in a timely fashion. Thus, while the dyadic bond may weaken consequent to disengagement by the parent or the child, the outcome remains increased risk for SU and SUD.
The findings reported herein must be considered in the context of study limitations. Convergent validity of the YAPS was not tested directly, although the three component scales align with other instruments measuring attachment, specifically the PIML (19, 20) and the Inventory of Parent and Peer Attachment (33). An assessment of peer attachment and items consistent with the peer attachment scale of the PIML were not available in the sample. Also, consequent to the long timespan of this longitudinal investigation, 35% of the sample did not return for the age 22 assessment. Whereas the analyses investigating differences between retained and attrited subjects do not point to systematic differences, the possibility of biased results cannot be completely discounted. In addition, caution needs to be exercised in interpreting the correlations between attachment and substance use since quantity consumed during each occasion was not measured. Furthermore, attachment was measured only from the child’s perspective. Future research needs to elucidate the congruity between parents and children. Whether parental report of attachment is a superior predictor of SUD in the child also remains to be investigated. Lastly, the limited number of girls in the sample precluded examining whether males and females differ with respect to the role of attachment on development of SUD (e.g., the ratio of N to parameters in the factor analysis is insufficient to obtain robust estimates).
In summary, this investigation demonstrated that the Youth Attachment to Parents Scale has content, construct, and criterion validity. Using this scale, it was found that psychological dysregulation measured by the neurobehavior disinhibition trait in mid-adolescence (age 16) mediates the association between low attachment during late childhood (age 10-12) and SUD in early adulthood (age 22). Prevention programs thus may improve by incorporating interventions that target the child’s vulnerability (ND) while concomitantly promoting affective bonding between the child and parents.
Footnotes
Supported by National Institute on Drug Abuse grants P50-DA05605, K02-DA017822, K05-DA031248, and R42-DA022127
References
- 1.Kassed CA, Levit KR, Hambrick MM. HCUP Statistical Brief #39: Hospitalizations Related to Drug Abuse. Agency for Healthcare Research and Quality; Rockville, MD: [Last accessed on August 6, 2013]. Oct, 2007. 2005. Available at http://www.hcupus.ahrg.gov/reports/statbriefs/sb39.pdf. [PubMed] [Google Scholar]
- 2.The National Center on Addiction and Substance Abuse at Columbia University (CASA) Addiction Medicine: Closing the Gap Between Science and Practice. New York, NY: [Last accessed on August 6, 2013]. 2012. Available at http://www.casacolumbia.org/download.aspx?path=/UploadedFiles/s1oqyaj0.pdf. [Google Scholar]
- 3.Volkow ND. Testimony Before the House Subcommittee on Labor-HHS-Education Appropriations. National Institute on Drug Abuse; [Last accessed on August 6, 2013]. 2013. Fiscal Year 2013 Budget Request. Available at http://www.drugabuse.gov/about-nida/legislative-activities/testimony-to-congress/2012/03/fiscal-year-2013-budget-request. [Google Scholar]
- 4.Substance Abuse and Mental Health Service Administration . Drug Abuse Warning Network, 2011. Substance Abuse and Mental Health Services Administration; Rockville, MD: 2013. National Estimates of Drug-Related Emergency Department Visits. HHS Publication No. (SMA) 13-4760, DAWN Series D-39. [Google Scholar]
- 5.Breslau N, Johnson EO, Hiripi E, Kessler R. Nicotine dependence in the United States: prevalence, trends, and smoking persistence. Arch Gen Psychiatry. 2001;58(9):810–816. doi: 10.1001/archpsyc.58.9.810. [DOI] [PubMed] [Google Scholar]
- 6.Compton WM, Thomas YF, Stinton FS, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV drug abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related condition. Arch Gen Psychiatry. 2007;64(5):566–576. doi: 10.1001/archpsyc.64.5.566. [DOI] [PubMed] [Google Scholar]
- 7.Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2007;64(7):830–840. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- 8.Haggerty KP, Skinner M, Fleming CB, Gainey RR, Catalano RF. Long-term effects of the Focus on Families project on substance use disorders among children of parents in methadone treatment. Addiction. 2008;103(12):2008–2016. doi: 10.1111/j.1360-0443.2008.02360.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tobler AL, Komro KA. Trajectories of parental monitoring and communication and effects on drug use among urban young adolescents. J Adolesc Health. 2010;46(6):560–568. doi: 10.1016/j.jadohealth.2009.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moore GF, Rothwell H, Segrott J. An exploratory study of the relationship between parental attitudes and behaviour and young people’s consumption of alcohol. Subst Abuse Treat Prev Policy. 2010;5:6. doi: 10.1186/1747-597X-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clark DB, Thatcher DL, Maisto SA. Supervisory neglect and adolescent alcohol use disorders: Effect on AUD onset and treatment outcome. Addict Behav. 2005;30(9):1737–1750. doi: 10.1016/j.addbeh.2005.07.017. [DOI] [PubMed] [Google Scholar]
- 12.Blackson TC, Tarter RE, Mezzich AC. Interaction between childhood temperament and parental discipline practices on behavioral adjustment in preadolescent sons of substance abuse and normal fathers. Am J Drug Alcohol Abuse. 1996;22(3):335–348. doi: 10.3109/00952999609001663. [DOI] [PubMed] [Google Scholar]
- 13.Johnson JG, Cohen P, Kasen S, Smailes E, Brook JS. Association of maladaptive parental behavior with psychiatric disorder among parents and their offspring. Arch Gen Psychiatry. 2001;58(5):453–460. doi: 10.1001/archpsyc.58.5.453. [DOI] [PubMed] [Google Scholar]
- 14.Dunn MG, Tarter RE, Mezzich AC, Vanyukov M, Kirisci L, Kirillova G. Origins and consequences of child neglect in substance abuse families. Clin Psychol Rev. 2002;22(7):1063–1090. doi: 10.1016/s0272-7358(02)00132-0. [DOI] [PubMed] [Google Scholar]
- 15.Ainsworth MD. Attachment beyond infancy. Am Psychol. 1989;44(4):709–716. doi: 10.1037//0003-066x.44.4.709. [DOI] [PubMed] [Google Scholar]
- 16.Ainsworth MD. Patterns of infant-mother attachments: Antecedents and effects on development. Bull N Y Acad Med. 1985;61(9):771–791. [PMC free article] [PubMed] [Google Scholar]
- 17.Wagner FA, Anthony JC. From first drug use to drug dependence: Developmental periods of risk for dependence upon marijuana, cocaine, and alcohol. Neuropsychopharmacology. 2002;26(4):479–488. doi: 10.1016/S0893-133X(01)00367-0. [DOI] [PubMed] [Google Scholar]
- 18.Ainsworth MD, Blehar MC, Waters E, Wall S. Patterns of Attachment. Erlbaum Associates; Hillsdale, NJ: 1978. [Google Scholar]
- 19.Cook EL, Greenberg MT, Kusche CA. Paper presented in Society for Research in Child Development. Indianapolis, IN: 1995. People in my life: Attachment relationships in middle childhood. [Google Scholar]
- 20.Ridenour TA, Greenberg MT, Cook ET. Structure and validity of people in my life: A self-report measure of attachment in late childhood. J Youth Adolesc. 2006;35(6):1037–1053. doi: 10.1007/s10964-006-9070-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ridenour TA, Clark DB, Cottler LB. The illustration-based Assessment of Liability and EXposure to Substance use and Antisocial behavior for children. Am J Drug Alcohol Abuse. 2009;34(4):242–252. doi: 10.1080/00952990902998715. [DOI] [PubMed] [Google Scholar]
- 22.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: Antisocial activities and drug use. J Child Psychol and Psychiatry. 2004;45(2):195–211. doi: 10.1111/j.1469-7610.2004.00214.x. [DOI] [PubMed] [Google Scholar]
- 23.Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: Common and specific influences. Ann Rev Clin Psychol. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- 24.Zerhouni E. Medicine. The NIH Roadmap. Science. 2003;302(5642):63–72. doi: 10.1126/science.1091867. [DOI] [PubMed] [Google Scholar]
- 25.Wechsler D. Wechsler Intelligence Scale for Children. 3rd edition Psychological Corporation; New York: 1991. [Google Scholar]
- 26.Hollingshead A. Four Factor Index of Social Status. Yale University Press; New Haven, CT: 1975. [Google Scholar]
- 27.Stouthamer-Loeber M, Loeber R, Wei E, Farrington DP, Wikstrorm PO. Risk and promotive effects in the explanation of persistent serious delinquency in boys. J Consult Clin Psychol. 2002;70(1):111–123. doi: 10.1037//0022-006x.70.1.111. [DOI] [PubMed] [Google Scholar]
- 28.Jacob T, Moser RP, Windle M, Loeber R, Stouthamer-Loeber M. A new measure of parenting practices involving preadolescent- and adolescent- aged children. Behav Modif. 2000;24(5):611–634. doi: 10.1177/0145445500245001. [DOI] [PubMed] [Google Scholar]
- 29.Schaefer E. Children’s reports of parental behavior: An inventory. Child Dev. 1965;36:413–424. [PubMed] [Google Scholar]
- 30.Skinner H, Steinhauer P, Santa-Barbara J. The family assessment measure. Can J Community Ment Health. 1983;2(2):91–105. [Google Scholar]
- 31.IBM Corp. IBM SPSS Statistics for Windows, Version 19.0. IBM Corp.; Armonk, NY: 2010. [Google Scholar]
- 32.Bollen KA. Structural Equations with Latent Variables. John Wiley and Sons; New York: 1989. [Google Scholar]
- 33.Armsden GC, Greenberg MT. The Inventory of Parent and Peer Attachment: Individual differences and their relationship to psychological well-being in adolescence. J Youth Adolesc. 1987;16(5):427–454. doi: 10.1007/BF02202939. [DOI] [PubMed] [Google Scholar]
- 34.Chen F, Sousa KH, West SG. Testing measurement invariance of second-order factor models. Structural Equation Modeling. 2005;12(3):471–492. [Google Scholar]
- 35.Hattie J. Methodology review: Assessing unidimensionality of tests and items. Applied Psychological Measurement. 1985;9(2):139–164. [Google Scholar]
- 36.Tarter RE. Evaluation and treatment of adolescent substance abuse: A decision tree method. Am J Drug Alcohol Abuse. 1990;16(1-2):1–46. doi: 10.3109/00952999009001570. [DOI] [PubMed] [Google Scholar]
- 37.Center for Education and Drug Abuse Research. Drug Use Chart. 1989 Unpublished Manuscript. [Google Scholar]
- 38.Kirisci L, Vanyukov MM, Dunn MG, Tarter RE. Item response theory modeling of substance use: An index based on 10 drug categories. Psychol Addict Behav. 2002;16(4):290–298. [PubMed] [Google Scholar]
- 39.Spitzer RL, Williams JBW, Gibbon M, First MB. User’s guide for the structural clinical interview for DSM-III-R. American Psychiatric Association; Washington, DC: 1990. [Google Scholar]
- 40.Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: A methodological study. Arch Gen Psychiatry. 1982;39(8):879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- 41.Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov MM, Gardner W, Blackson T, Clark DB. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry. 2003;160(6):1078–1085. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- 42.Windle M. The Revise Dimensions of Temperament Survey (DOTS-R): Simultaneous group confirmatory factor analysis for adolescent gender groups. Psychol Access. 1992;4(2):228–234. [Google Scholar]
- 43.Orvaschel W, Puig-Antich J, Chambers W, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J Am Acad Child Psychiatry. 1982;21(4):392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- 44.Pelham W, Murphy D. The DBD Rating Scale: A Parent and Teacher Rating Scale for the Disruptive Behavior Disorder of Childhood in DSM-III-R. University of Pittsburgh Medical School, Department of Psychiatry; 1987. [Google Scholar]
- 45.Mezzich AC, Tarter RE, Feske U, Kirisci L, McNamee RL, Day BS. Assessment of risk for substance use disorder consequent to consumption of illegal drugs: Psychometric validation of the neurobehavior disinhibition trait. Psychol Addict Behav. 2007;21(4):508–515. doi: 10.1037/0893-164X.21.4.508. [DOI] [PubMed] [Google Scholar]
- 46.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd Edition Lawrence Erlbaum Associates; Hillsdale, NJ: 1988. [Google Scholar]
- 47.Muthen LK, Muthen BO. Mplus User’s Guide. Sixth Edition Muthen & Muthen; Los Angeles, CA: 1998-2011. [Google Scholar]
- 48.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhart S, editor. Social Methodology. American Sociological Association; Washington D.C.: 1982. pp. 290–312. [Google Scholar]
- 49.Mackinnon DP. Introduction to Statistical Mediation Analysis. Lawrence Erlbaum Associates; New York, NY: 2008. [Google Scholar]
- 50.Contreras JM, Kerns KA, Weimer BL, Gentzler AL, Tomich PL. Emotion regulation as a mediator of associations between mother-child attachment and peer relationships in middle childhood. J Fam Psychol. 2000;14(1):111–124. doi: 10.1037//0893-3200.14.1.111. [DOI] [PubMed] [Google Scholar]
- 51.Drake K, Belsky J, Fearon RM. From early attachment to engagement with learning in school: The role of self-regulation and persistence. Dev Psychol. 2013 doi: 10.1037/a0032779. In Press. [DOI] [PubMed] [Google Scholar]
- 52.Heikamp T, Trommsdorff G, Druey MD, Huber R, von Suchodoletz A. Kindergarten childen’s attachment security, inhibitory control, and the internalization of rules of conduct. Front Psychol. 2013;4:133. doi: 10.3389/fpsyg.2013.00133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoeve M, Dubas JS, Gerris JRM, van der Laan PH, Smeenk W. Maternal and paternal parenting styles: Unique and combined links to adolescent and early adult delinquency. J Adolesc. 2011;34(5):813–827. doi: 10.1016/j.adolescence.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 54.Bailey JA, Hill KG, Guttmannova K, Oesterle S, Hawkins JD, Catalano RF, McMahon RJ. The association between parent early adult drug use disorder and later observed parenting practices and child behavior problems: Testing alternate models. Dev Psychol. 2013;49(5):887–899. doi: 10.1037/a0029235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Henry DB, Tolan PH, Gorman-Smith D. Longitudinal family and peer group effects on violence and nonviolent delinquency. J Clin Child Psychol. 2001;30(2):172–186. doi: 10.1207/S15374424JCCP3002_5. [DOI] [PubMed] [Google Scholar]
- 56.Castro FG, Brook JS, Brook DW, Rubenstone E. Paternal, perceived maternal, and youth risk factors as predictors of youth stage of substance use a longitudinal study. J Addict Dis. 2006;25(2):65–75. doi: 10.1300/J069v25n02_10. [DOI] [PubMed] [Google Scholar]
- 57.Hotton T, Haans D. Alcohol and drug use in early adolescence. Health Report. 2004;15(3):9–19. [PubMed] [Google Scholar]
- 58.Hahn-Holbrook J, Holbrook C, Haselton MG. Parental precaution: Neurobiological means and adaptive ends. Neurosci Biobehav Rev. 2011;34(4):1052–1066. doi: 10.1016/j.neubiorev.2010.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Patock-Peckham JA, Morgan-Lopez AA. Direct and meditational links between parental bonds and neglect, antisocial personality, reasons for drinking, alcohol use, and alcohol problems. J Stud Alcohol Drugs. 2010;71(1):95–104. doi: 10.15288/jsad.2010.71.95. [DOI] [PubMed] [Google Scholar]
- 60.Bohlin G, Eninger L, Brocki KC, Thorell LB. Disorganized attachment and inhibitory capacity: Predicting externalizing problem behaviors. J Abnorm Child Psychol. 2012;40(3):449–458. doi: 10.1007/s10802-011-9574-7. [DOI] [PubMed] [Google Scholar]
- 61.Hawes DJ, Dadds MR, Frost AD, Hasking PA. Do childhood callous-unemotional traits drive changes in parenting practices? J Clin Child Adolesc Psychol. 2011;40(4):507–518. doi: 10.1080/15374416.2011.581624. [DOI] [PubMed] [Google Scholar]
- 62.Ridenour TA, Stormshak EA. Introduction and rationale for individualized substance abuse prevention from an ontogenetic perspective. Am J Drug Alcohol Abuse. 2009;35(4):206–208. doi: 10.1080/00952990903005924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ridenour TA. Transitioning from DSM-IV abuse to dependence: The essence of harmful compulsive substance use is ontogenetic and dynamic. Am J Drug Alcohol Abuse. 2013;39(3):139–141. doi: 10.3109/00952990.2013.797988. [DOI] [PMC free article] [PubMed] [Google Scholar]