Abstract
Gastrointestinal duplication is an uncommon congenital abnormality in two-thirds of cases manifesting before the age of 2 years. Ileal duplication is common while colonic duplication, either cystic or tubular, is a rather unusual clinical entity that remains asymptomatic and undiagnosed in most cases. Mostly occurring in pediatric patients, colonic duplication is encountered in adults only in a few cases. This study reports two cases of colonic duplication in adults. Both cases presented with rectal bleeding on admission. The study was focused on clinical, imaging, histological, and therapeutical aspects of the presenting cases. Gastrografin enema established the diagnosis in both cases. The cystic structure and the adjacent part of the colon were excised en-block. The study implies that colonic duplication, though uncommon, should be included in the differential diagnosis of rectal bleeding.
Keywords: Colonic duplication, Gastrointestinal bleeding
INTRODUCTION
Gastrointestinal duplication is an uncommon congenital abnormality[1]. More than 80% of cases present before the age of 2 years as an acute abdomen or bowel obstruction and can occur anywhere throughout the alimentary tract[1,2]. Ileum is the most common site for duplication, accounting for over 60% of cases[4]. On the other hand, duplication of the colon is a rare abnormality, accounting for 4-18% of all gastrointestinal duplications, often located in the cecum[3,4]. A thorough review of the international literature since 1950, has revealed 83 cases of colonic duplications reported up-to-date.
Although intestinal duplications are considered to be benign lesions, mostly asymptomatic, they may result in significant morbidity and mortality, if left untreated[5]. Indications for surgical intervention often arise in an acute setting, in the form of a complication. Specifically, patients with previously undetected duplications may present in the setting of bowel obstruction or severe gastrointestinal hemorrhage (i.e., ulcerating gastric mucosa within a duplication cyst)[3]. If encountered incidentally, these lesions should be surgically addressed to avoid any future complication, including the possibility of malignant degeneration within the duplication cyst[3,5].
The cases mentioned in the present article refer to patients manifesting bleeding of the lower gastrointestinal tract, which was finally proved as originating from the mucosa of a colonic duplication.
CASE REPORTS
Case 1
A 53-year-old male was admitted to our department with rectal bleeding. He claimed of stool mixed with blood, without pain or changes in bowel habits, 5 d prior to admission. The patient had a medical history of constipation, being treated with diet for more than 20 years. On admission, he was in a stable clinical condition, with normal vital signs and blood tests were within normal ranges. Rectal examination confirmed the presence of blood in the stools. Plain X-rays of the abdomen showed no particular findings.
Colonoscopy was performed showing only two small diverticula in the sigmoid colon, but could not reveal the site of bleeding. It was not possible for the right colon to be examined thoroughly, due to imperfect bowel cleansing. As a second step of the diagnostic procedure, radiographic colon imaging after gastrografin enema was performed. It showed a fistula in the middle of the ascending colon, communicating with a cystic formation approximately 2 cm×1 cm in dimension. Furthermore, a computerized tomography of the abdomen was performed, which confirmed the findings and a possible diagnosis of colonic duplication of ascending colon was concluded. A second colonoscopy detected the mucosa of the colonic duplication to be the origin of bleeding.
Excision of the cystic lesion was decided (Figure 1). It was resected en-block to the section of the ascending colon and an end-to-end anastomosis of the colon was performed. Pathological examination of the resected lesion revealed a duplication cyst in the mesenteric border of the ascending colon, with normal intestinal mucosa lining its wall (Figure 2). Within the mucosa of the duplication, a site of angiodysplasia was detected as the origin of bleeding.
Figure 1.

Surgical specimen including the ascending colon together with a duplication cyst attached to the mesenteric border of the colon.
Figure 2.
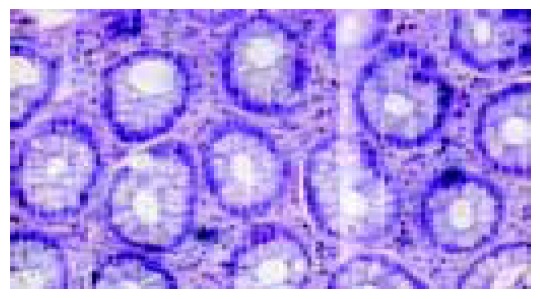
Normal intestinal mucosa of the cyst in the first case (HE ×125).
The patient had an uneventful postoperative course and was discharged on the 6th post-operative day. He remained asymptomatic ever since.
Case 2
A 45-year-old male was referred to our department claiming of fatigue and a 5-d history of bloody stools. Physical examination as well as blood investigations were entirely unremarkable. The patient was submitted to rectal examination as well as colonoscopy, which did not reveal any source of bleeding. The radiological imaging control using gastrografin enema showed a cystic formation of 0.5 cm×5 cm in size, located in the mesenteric border of the descending colon. This finding was confirmed by a second colonoscopy, which established the diagnosis of a colonic duplication.
A surgical intervention was decided in order to detect the site of bleeding, as well as to prevent any further complication of the cyst. The cystic lesion was resected en-block to the adjacent part of the colon (Figure 3) and an end-to-end anastomosis was performed. The cyst was confirmed to be a colonic duplication of normal colonic mucosa according to the pathologic study. Indeed, there was a mucosal ulceration in the cystic cavity, probably representing the origin of bleeding. There was no immediate or delayed post-operative complication.
Figure 3.

Surgical specimen in the second case including the descending colon with a duplication cyst adjacent to the colon.
DISCUSSION
Intestinal duplication is a congenital malformation, that occurs mostly in pediatric patients[2,6]. It could be encountered anywhere throughout the gastrointestinal tract, from the mouth to the anus. Current nomenclature relies on the anatomic location of the duplication in relation to the normal intestinal tract and not on the histological features of the mucosal lining[2]. Intestinal duplications are located in, or attached (share a common wall) to the wall of an adjacent part of the gastrointestinal tract and possess at least one exterior layer of smooth muscle and are lined with various types of gastrointestinal mucosa[1]. Further characterization defines these abnormalities as either spherical or tubular. Rarely, complete duplication of the colon may be encountered[7].
Approximately 75% of duplications have been reported to be located within the abdominal cavity. Jejunal and ileal lesions are the most commonly encountered (53%), while colonic lesions are found in 13% of cases. These lesions may be cystic (75%) or tubular (25%) in appearance and characteristically arise from the mesenteric border of the bowel[5,6]. They may or may not have one or more direct communications with the adjacent part of the bowel across the common septum[3]. Non-communicating duplications typically contain clear alkaline fluid, except in cases in which gastric mucosa is present (25%) and acidic fluid is observed. In addition, non-activated pancreatic enzymes may also be observed in cases of ectopic pancreatic tissue within the duplication lesion[3]. In adults, either cystic or tubular duplication of the colon is a rare entity[8].
Most colonic duplication cysts are asymptomatic and remain undiagnosed for years[9]. If symptomatic, they manifest with obstruction[10,11], bleeding[10-13] or constipation[8]. Cystic duplications have been reported to cause obstruction of the colon as a result of direct compression, volvulus, or intussusception, whereas tubular duplications of the rectum have been described as having direct communication with the perineum[3,13]. Although many duplications are diagnosed incidentally, most patients present with a combination of pain and/or obstructive symptoms[14,15]. These symptoms may be the direct effects of distension of the duplication or caused by compression of adjacent organs (including their associated blood supplies). In addition, abrupt hemorrhage with hemodynamic instability can be encountered in the case of a cyst, lined with mucosa that ulcerates and eventually erodes into adjacent organs and/or vessels[3,13]. There are scattered reports of intestinal carcinomas found within duplication cysts[14,16]. No significant difference in clinical presentation has been detected between communicating and non-communicating cysts[3].
Histological analysis typically reveals at least one outer muscular layer with an inner gastrointestinal mucosal lining. The mucosal lining does not necessarily correspond to that of the adjacent normal intestine and may be comprised several different types of gastrointestinal mucosa[2]. Because of the relative scarcity of such abnormalities, current literature consists mainly of small populations and case reports rather than any large single or multi-institutional series[8-10,13].
The first patient reported in this study, presented with bleeding in the stools and constipation as his major complaints on admission, while the other one claimed of rectal bleeding. Abdominal X-rays in both cases showed no abnormal findings. The use of contrast material in the imaging control was necessary to discover the cysts. Ultrasonography could help in the diagnostic procedure[17,18]. Colonoscopy and CT imaging could establish the diagnosis. Colonoscopic examination revealed a cystic formation, lined by normal intestinal mucosa, communicating with the colon. CT imaging showed a cystic mass attached to the colon.
Preoperative diagnosis of colonic duplication is often difficult. Symptoms usually include abdominal pain, often confusing colonic duplication with other more common diagnoses. Plain X-rays of the chest and abdomen should be routinely performed; however, because of the non-specificity of their results, it is difficult to make a pre-operative diagnosis on the basis of radiographic findings. Computerized tomography of the chest or abdomen is useful in establishing a diagnosis of alimentary tract duplication during the pre-operative workup and may be used to evaluate the synchronous lesions, once a single duplication is identified[2,3]. Ultrasonography is also helpful in establishing a pre-operative diagnosis[17,18].
Treatment is reserved for symptomatic cases and usually includes resection of the cyst and the neighboring part of the intestine[11,13,19]. Complications related to surgical intervention are typically nonspecific and include post-operative bleeding, infection, and bowel obstruction[3]. However, in patients with large tubular duplications, injury to the normal intestine with resultant short bowel syndrome must be considered[3].
In most instances, cystic duplications can be completely excised. Resection of normal intestine must often accompany removal of the lesion, because of the intimate attachment of the common wall or because isolated resection of the cyst would compromise blood flow to the adjacent intestinal segment[3,11,13,19]. An alternative approach involving marsupialization of the cystic structure consists of a partial cystectomy combined with mucosal stripping of the remaining cyst wall to preserve normal anatomy[3]. Although current literature does not specifically address the prognosis and outcome related to the diagnosis of alimentary tract duplications, the overall outcome is generally favorable[2,3].
Footnotes
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
References
- 1.Macpherson RI. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13:1063–1080. doi: 10.1148/radiographics.13.5.8210590. [DOI] [PubMed] [Google Scholar]
- 2.O'Neil J, Rowe M. Duplications of the gastrointestinal tract. In: Essentials of Pediatric Surgery. St. Louis, Mo. Mosby Yearbook; 1995. pp. 520–525. [Google Scholar]
- 3.Holcomb GW, Gheissari A, O'Neill JA, Shorter NA, Bishop HC. Surgical management of alimentary tract duplications. Ann Surg. 1989;209:167–174. doi: 10.1097/00000658-198902000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Puligandla PS, Nguyen LT, St-Vil D, Flageole H, Bensoussan AL, Nguyen VH, Laberge JM. Gastrointestinal duplications. J Pediatr Surg. 2003;38:740–744. doi: 10.1016/jpsu.2003.50197. [DOI] [PubMed] [Google Scholar]
- 5.Chen CC, Yeh DC, Wu CC, Li MC, Kwan PC. Huge cystic duplication of the ascending colon in adult. Zhonghua YiXue ZaZhi (Taipei) 2001;64:174–178. [PubMed] [Google Scholar]
- 6.Keramidas DC, Demetriades DM. Total tubular duplication of the colon and distal ileum combined with transmesenteric hernia: surgical management and long-term-results. Eur J Pediatr Surg. 1996;6:243–244. doi: 10.1055/s-2008-1066520. [DOI] [PubMed] [Google Scholar]
- 7.Li L, Zhang J, Wang Y, Chen R, Qin H. Complete duplication of the colon: definitive management by resection of the duplication without the normal bowel. Chin Med J (Engl) 2002;115:779–781. [PubMed] [Google Scholar]
- 8.Pennehouat G, Houry S, Huguier M. Sigmoid duplication in an adult. J Chir (Paris) 1986;123:169–170. [PubMed] [Google Scholar]
- 9.Favara BE, Franciosi RA, Akers DR. Enteric duplications. Thirty-seven cases: a vascular theory of pathogenesis. Am J Dis Child. 1971;122:501–506. [PubMed] [Google Scholar]
- 10.Otter MI, Marks CG, Cook MG. An unusual presentation of intestinal duplication with a literature review. Dig Dis Sci. 1996;41:627–629. doi: 10.1007/BF02282353. [DOI] [PubMed] [Google Scholar]
- 11.Van Elst F, Hubens A. Duplication of the colon in the adult (author's transl) Acta Chir Belg. 1978;77:335–342. [PubMed] [Google Scholar]
- 12.Bremer JL. Diverticula and duplications of the intestinal tract. Arch Pathol. 1944;38:132–140. [Google Scholar]
- 13.Frittelli P, Costa G, Zanella L, Sguazzini G, Rossi FS. Intestinal duplication in the adult. A case report of colonic duplication and a review of the literature. Chir Ital. 2002;54:721–728. [PubMed] [Google Scholar]
- 14.Choong CK, Frizelle FA. Giant colonic diverticulum: report of four cases and review of the literature. Dis Colon Rectum. 1998;41:1178–185; discussion 1178-1185;. doi: 10.1007/BF02239441. [DOI] [PubMed] [Google Scholar]
- 15.Salvador II, Modelli ME, Pereira CR. Tubular duplication of the colon: a case report and review of the literature. J Pediatr (Rio J) 1996;72:254–257. doi: 10.2223/jped.628. [DOI] [PubMed] [Google Scholar]
- 16.Horie H, Iwasaki I, Takahashi H. Carcinoid in a gastrointestinal duplication. J Pediatr Surg. 1986;21:902–904. doi: 10.1016/s0022-3468(86)80021-5. [DOI] [PubMed] [Google Scholar]
- 17.Kangarloo H, Sample WF, Hansen G, Robinson JS, Sarti D. Ultrasonic evaluation of abdominal gastrointestinal tract duplication in children. Radiology. 1979;131:191–194. doi: 10.1148/131.1.191. [DOI] [PubMed] [Google Scholar]
- 18.Hayden CK. Ultrasonography of the gastrointestinal tract in infants and children. Abdom Imaging. 1996;21:9–20. doi: 10.1007/s002619900002. [DOI] [PubMed] [Google Scholar]
- 19.Robert J, Ambrosetti P, Widgren S, Rohner A. Perforated tubular duplication of the sigmoid colon in adults. Gastroenterol Clin Biol. 1990;14:776–779. [PubMed] [Google Scholar]


