Abstract
The present study investigated whether a culturally-tailored problem-solving intervention delivered by a trained depression care specialist (DCS) would improve depressive symptoms over a six month period among Hispanic/Latino patients in a federally-qualified community health center by the California-Mexico border. Participants included 189 low income Hispanic/Latino patients of Mexican heritage. Based on the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) evidence-based treatment, patients received evidence-based problem-solving therapy. The Patient Health Questionnaire-9 (PHQ-9) was administered to assess changes in self-reported depressive symptoms between baseline and monthly for a 6-month follow up period. The majority of participants were female (72.5%) with a mean age of 52.5 (SD=11.7). The mean PHQ-9 at baseline was 16.9 (SD=4.0) and at the 6-month follow-up, the average PHQ-9 decreased to 9.9 (SD=5.7). A linear mixed model analysis showed significant improvement in PHQ-9 scores over a 6 month period (F=124.1; p<0.001) after controlling for age, gender, smoking and diabetes. There was a significant three way interaction between time, gender and smoking (p=0.01) showing that the depressive symptoms among male smokers did not improve as much as non-smoking males and females. Results suggest that a culturally-tailored problem solving approach can significantly reduce depressive symptoms among Hispanic/Latino low-income patients.
Keywords: Hispanic/Latinos, Depression, Integrated Care, IMPACT
Introduction
Depression is a costly and disabling condition, frequently encountered in community health centers (Gilmer TP, Walker C, Johnson ED, Phlis-Tsimikas A, & Unützer J, 2008; Katon W et al., 2003). Depression negatively affects one's ability to adhere to medical health recommendations and to engage in healthy life-changing behaviors such as dietary restrictions, increased exercise and smoking cessation (Gilmer TP, et al., 2008; Katon W, et al., 2003; Lin et al., 2004). Depression is projected to become one of the top leading causes of disability worldwide (González HM, Tarraf W, Whitfield K, & Gallo JJ, 2012; Inagaki et al.; World Health Organization, 2004). In addition, utilization of behavioral health treatment is limited among Hispanic/Latinos due to cultural beliefs about stigma associated with mental illness (González HM et al., 2010). Approximately 40% of individuals with complaints of depressive symptoms are first seen in community health centers (Herrman H et al., 2002) and 25% of patients with a chronic medical conditions tend to experience depression or anxiety (Leon AC et al., 1995). Based on this information, it is a public health necessity to find innovative and practical approaches to deliver behavioral health interventions to diverse ethnic minority populations attending community health centers.
Depression is commonly encountered among Hispanic/Latinos. The prevalence of depression among Hispanic/Latinos has been reported between 8% and 15% compared to 22% encountered in non-Latino white individuals (Alegría M et al., 2008; González HM, Vega WA, et al., 2010). Additionally, access to care continues to be a major public health challenge for Hispanic/Latinos due to cultural and sociodemographic issues (Breslau J & et al., 2011; González HM, Vega WA, et al., 2010). Furthermore, depression is frequently misdiagnosed and often remains untreated among Hispanic/Latinos due to the high presence of associated somatic symptoms (McGuire TG, Alegria M, Cook BL, Wells KB, & Zaslavsky AM, 2006). Hispanic/Latinos attending community health centers tend to have low health literacy (Moreno FA, Chong J, Dumbauld J, Humke M, & Byreddy S, 2012) be less receptive to behavioral health care services because of stigma (Marin H, Escobar JI, & Vega WA, 2006) and have less awareness about services available to address behavioral health concerns (González HM, Tarraf W, Whitfield KE, & Vega WA, 2010; Marin H, et al., 2006; Moreno FA, et al., 2012). Depressive symptoms are frequently accompanied by lack of adherence to treatment plans for other chronic medical conditions (Katon W, et al., 2003). It is known that depressive symptoms such as poor concentration, anhedonia, poor motivation, lack of energy affect the ability of an individual to care for chronic medical conditions (Gilmer TP, et al., 2008). For example, in a recent cross-sectional study, Parada and colleagues (2012) found that high levels of depression among Hispanic/Latinos were significantly correlated with poor adherence to medication and treatment for diabetes (Parada, Horton, Cherrington, Ibarra, & Ayala, 2012).
Another important factor that is frequently ignored is the high prevalence of depressive symptoms and smoking among Hispanic/Latino men. The literature reported that around 16% of Hispanic/Latinos smoke compared to the general population in the United States (Center for Disease Control and Prevention (CDC), 2008; Lorenzo-Blanco EI & Cortina LM, 2013). Even though the literature has reported that depression is higher among Hispanic/Latino women than men (Alegría M, et al., 2008), rates of smoking have been reported to be higher among Hispanic/Latino men than women (Lorenzo-Blanco EI & Cortina LM, 2013). Furthermore, longitudinal analysis have shown that negative emotions identified during young age predict an increase in smoking among Hispanic/Latino men than in women (Lorenzo-Blanco EI & Cortina LM, 2013).
Studies have shown that using the Improving Mood-Promoting Access to Collaborative Treatment (IMPACT) evidence-based approach is a feasible method to address behavioral health needs for patients with chronic diseases attending community health clinics (Gilmer TP, et al., 2008; Unützer et al., 2002). Similar to other integrated care studies (Katon W et al., 1995)(Katon W et al., 1999), the IMPACT model that includes co-location of behavioral health workers and primary care providers, is an ideal treatment approach for patients attending community health centers and is a potentially effective approach to reduce disparities in the treatment of depressive symptoms(Unützer, et al., 2002). However, the feasibility of implementing IMPACT varied according to the need, health literacy, resources and cultural background of a given community (Grazier, Smith, Song, & Smiley, 2013; Unützer, et al., 2002).
The purpose of this study was to evaluate changes in depressive symptoms among Hispanics/Latinos attending a community health center near the US-Mexico border of an ongoing program to reduce depression in primary care community health centers implemented by San Diego County Mental Health Services. Depressive symptoms were measured over a 6 month-period where participants took part in a culturally-tailored IMPACT model delivered by trained paraprofessional mental health workers that were defined as Depression Care Specialists (DCS). Given that culturally tailored supportive treatment has proven to improve symptoms of chronic diseases, such as diabetes, (Ell K; Ell et al., 2011), a culturally modified IMPACT model was used to meet the needs and characteristics of the patient population in the targeted community health center. Based on this rationale, we hypothesized that individuals receiving a culturally tailored IMPACT intervention delivered by a DCS would demonstrate a sustained improvement in their depressive symptoms over a 6 month period as measured by the PHQ-9.
Methods
Sample
Participants were registered patients of San Ysidro Health Center (SYHC). SYHC is a large federally-qualified community health center located along the California-Mexico border region of San Diego County with approximately 80,000 registered patients and served by 10 clinical facilities. Participants were recruited through their primary care provider and eligible for the study if they self-identified as Mexican or Mexican-American and were at least 18 years old, capable of providing informed consent. The sample included the first 189 patients who were referred to receive the culturally tailored IMPACT. Results reported here reflect data on participants with complete data for at least 2 measurement time-points from baseline to 6-month follow-up.
Implementation of the Culturally Tailored IMPACT Program
The implementation of the IMPACT program was part of an integrated care program funded by San Diego County Mental Health Services. The program followed the IMPACT evidence-based approach in which the co-location of behavioral health workers among primary care providers reduces disparities and improves depressive symptoms (Unützer, et al., 2002). The program's aim was to familiarize primary care providers at SYHC with the screening and treatment of depression with the assistance of a DCS.
Depression Care Specialists (DCS)
In our program, the DCS were physicians trained in Mexico but not licensed to practice medicine in the United States. They had background as research coordinators as well as knowledge in prevention and management of chronic diseases but not in mental health treatment. The DCS were trained and received a certificate in the evidence-based manualized problem solving therapy (Arean, Hegel, Vannoy, Fan, & Unuzter, 2008; Hegel MT, Dietrich AJ, Seville JL, & Jordan CB, 2004). This training was provided and sponsored by San Diego County Mental Health Services and the Council of Community Clinics. In order to facilitate recruitment and communication between the primary care provider and the DCS, a warm hand-off approach was used. The rationale behind the warm and-off approach is that a face to face introduction of the patient from the primary care provider to the DCS will confer the trust that the patient has established with the provider and helps ensure that the next appointment with the DCS will be kept to improve compliance (California Mental Health Services Authority; Little V, 2010).
Implementation of Problem Solving Therapy(PST) within the IMPACT model
As described by the Health Resources and Service Administration (HRSA), the population served by the San Ysidro Health Center has low-health literacy and is economically disadvantaged (US Department of Health and Human Services). As part of the IMPACT model, DCS were trained by a certified licensed trainer sponsored by San Diego County Behavioral Health Services and the Council of Community Clinics to deliver the evidence based problem solving therapy (PST) to the patients identified or referred by the primary care provider. Problem solving therapy has been shown to improve symptoms of depression and maintain improvement and remission of symptoms post-treatment(Arean PA et al., 1993). As described in the literature, PST is a cognitive behavioral therapy intervention that is composed of seven steps that patients learn in treatment: 1) how to define problems; 2) how to set goals; 3) brainstorming solutions; 4) solution selection; 5) solution implementation; 6) review of the implemented plan, and 7) activity scheduling (Arean, et al., 2008; Arean PA, et al., 1993; Hegel MT, et al., 2004).
Cultural Adaption of the Problem Solving Therapy Intervention
Pilot work and debriefing with program participants revealed that the content and delivery of the manualized PST was not possible due to patients’ beliefs and expectations and had to be modified to their cultural perspectives. For example, out of the seven manualized steps, patients were not receptive to the implementation of plans and solutions or to review the schedule of activities to improve the identified problems (Arean, et al., 2008; Hegel MT, et al., 2004). In other words, adherence to the PST provider checklist was not possible due to the patient's needs (Hegel MT, et al., 2004). Instead, PST was culturally-tailored to this population by receiving at least 15-30 minutes of receptive listening and support based on the two first steps of PST: 1) definition of the problem and 2) brainstorming to build problem skills but without any review of homework or check list as defined in the literature (Arean, et al., 2008; Arean PA, et al., 1993; Hegel MT, et al., 2004). Another culturally-tailored approach is that the intervention was delivered in Spanish. The problems that were focus of attention were family conflicts, financial stressors and dealing with ongoing chronic medical conditions. Patients were followed for 6 months to monitor changes in their depressive symptoms as measured by the Patient Health Questionnaire (PHQ-9). The study was approved by San Diego State University, SYHC's, and the San Diego County Health and Human Services respective Institutional Review Boards.
Measures
Sociodemographic variables included in the analyses were age and gender. Smoking (Y/N) and diagnosis of diabetes (Y/N) verified by medical record were collected since these are frequent comorbidities observed in depressed patients attending community clinics (Parada, et al., 2012; Patton et al., 1998). No additional biological or behavioral data was analyzed.
Main Outcome
The change PHQ-9 scores over time was the main outcome variable. The PHQ-9 is a self-administered nine-item validated instrument for screening and monitoring depressive symptoms. It has been widely used among different ethnic groups, including Hispanic/Latinos and is available both in English and Spanish (Huang FY, Chung H, Kroenke K, Delucchi KL, & Spitzer RL, 2006). A score of ≥10 was considered a positive screen for mild to moderate symptoms of depression.
Statistical Analyses
Continuous variables were described by means/standard deviations (SD) and categorical variables as frequencies/percentages. A linear mixed model was used to examine changes in levels of depressive symptomatology over time controlling for age, gender, smoking and diabetes. This approach was also used to measure the variability of the PHQ-9 changes across time points. A random intercept and slope approach was used since it provides a better fit for the variables in the model. A three way interaction was explored to analyze the effect modification of time, gender and smoking with depressive symptoms since smoking and depression have been reported to be strongly associated among Hispanic/Latinos (Lorenzo-Blanco EI & Cortina LM, 2013). Data was analyzed using IBM-SPSS Statistics Premium V.21 (SPSS Inc. Chicago,IL) and R version 2.15.1.
Results
Table 1 summarizes the characteristics of this sample population. Participants were assessed over a 6-month period to examine changes in their depressive symptoms as measured by the PHQ-9. The mean age was 52.5 (SD=11.7) and 137 (72.5%) participants were female. The mean PHQ-9 at a baseline was 15.0 (SD=5.4).
Table 1.
Participant characteristics
| N=189 | Male n=52 | Female n=137 | p |
|---|---|---|---|
| Age (SD) | 52.3 (11.3) | 52.5 (11.9) | 0.99 |
| Smoking (%) | 9 (17.3%) | 6 (4.4%) | 0.003* |
| Diabetes (%) | 20 (38.5%) | 45 (32.8%) | 0.46 |
| PHQ-9 Baseline (SD) | 16.8 (3.7) | 16.9 (4.1) | 0.92 |
p<0.05
There were no significant mean differences for gender at the baseline PHQ-9 scores (p=0.93). Linear mixed effects analyses showed a significant improvement of PHQ-9 changes on a monthly basis over a 6-month period (F=124.1; p=<0.001) after controlling for age, gender, diabetes and smoking. Throughout the different time points, the total sample size varied; although linear mixed effects analyses is sufficiently robust to correct for this sample variation issue. Table 2 summarizes the changes of PHQ-9 over the 6-month period and table 3 illustrates the different participants per session over the 6 month period.
Table 2.
Association of time by PHQ-9 by gender and smoking over a 6 month period
| DF | F-value | P | |
|---|---|---|---|
| Age | 1 | 0.039 | 0.842 |
| Diabetes | 1 | 0.001 | 0.965 |
| Time | 1 | 124.168 | <.000** |
| Smoking | 1 | 27.748 | <.000** |
| Gender | 1 | 1.178 | 0.278 |
| Time*smoke | 1 | 12.720 | <0.000** |
| Time*Gender | 1 | 0.079 | 0.778 |
| Smoke*Gender | 1 | 0.033 | 0.856 |
| Time*smoke*Gender | 1 | 5.956 | 0.015* |
Significant at the .01 level
Association of PHQ-9 scores adjusting for gender, smoking and looking at the interaction of time by gender and time by gender and smoking
Table 3.
Number of participants per visit over a 6 month period.
| Visits | n (%) Participants Completed |
|---|---|
| Baseline Visit | 189 (96.9) |
| Visit 2 | 99 (51.8) |
| Visit 3 | 57 (29.8) |
| Visit 4 | 79 (41.4) |
| Visit 5 | 42 (22.0) |
| Visit 6 | 32 (16.8) |
| Visit 7 | 36 (18.8) |
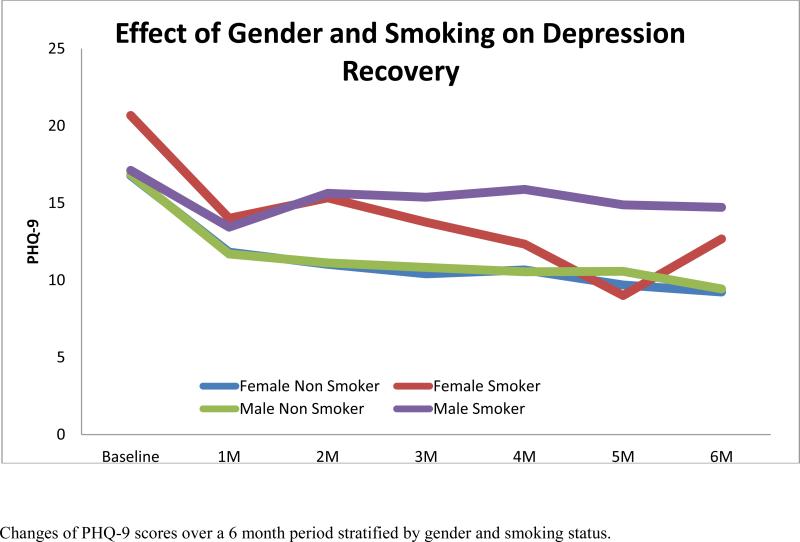
There was a significant three-way interaction between time, gender and smoking showing that depressive symptoms among male smokers did not improve compared to male and female non-smokers. Figure 1 illustrates these interactions. We also compared PHQ-9 scores using the commonly used cutoff of 10 described in the literature (Kroenke K, Spitzer RL, & Williams JB, 2001) at baseline and at the 6-month period using a logistic regression approach, controlling for age, gender, smoking and diabetes. Compared to the baseline PHQ-9, we found a significant improvement in depressive symptoms when using the cut-off of 10 (p<0.001; 95%CI:0.001-0.039) among patients receiving problem solving therapy from a DCS at 6 months after treatment.
Figure 1.
Changes of PHQ-9 scores over a 6 month period stratified by gender and smoking status.
Discussion
This study shows the value of using a co-located trained DCS to deliver a culturally sensitive and tailored brief problem solving therapeutical intervention to improve depressive symptoms among indigent Hispanic/Latinos attending a community health center by the US-Mexico border. The vast majority of patients (75%) had severe depressive symptoms upon entry into the program as measured by the PHQ-9 (mean=15.0) which suggested that patients were highly symptomatic during their initial consultation with the primary care provider.
Several studies have described the importance of overcoming barriers to deliver culturally appropriate interventions for Hispanic/Latino patients attending community health centers to improve symptoms of depression (González-Prendes AA, Hindo C, & Pardo Y, 2011; Grazier, et al., 2013). This is particularly relevant due to the strong familism or strong family bonds described in this ethnic group and the importance of adapting interventions to provide support and deliver treatment for different psychosocial stressors (Duarté-Vélez, Bernal, & Bonilla, 2010). Additionally, since this culturally adapted IMPACT and PST intervention is an ongoing program in the health center, our positive results show that this treatment approach does require replication as a randomized clinical trial.
The use of DCS has not been extensively studied among Hispanic/Latinos of low socioeconomic status. To our knowledge, few studies have reported the use of trained DCS to address symptoms of depression in community health clinic especially among Hispanic/Latinos living by the US-Mexico border. The uniqueness of our DCS is that they were trained physicians from Mexico. This could be an issue for replication in other community health centers. In order to overcome this aspect, we expect to train DCS that have the same socioeconomic background as the patient population served. This will be based on the theory that DCS could be considered as community mental health worker that will delivered culturally appropriate mental health interventions for patients attending community health centers (Balcazar H et al., 2006). Future studies will evaluate the use of DCS as trained community mental health worker to deliver interventions as educators or counselors. This will be consistent with previous work that has used community health workers for cardiac rehabilitation and management of diabetes among Hispanic/Latinos (Balcázar H, Alvarado M, Cantu F, Pedregon V, & Fulwood R, 2009; Balcázar H et al., 2012; Philis-Tsimikas, Fortmann, Lleva-Ocana, Walker, & Gallo, 2011; Ryabov I, 2010).
Issues with compliance were also observed in our sample, even though we did not measure this directly. As reported in the literature, Hispanic/Latinos have a 60% rate of non-compliance to medical treatment plans; this is further complicated by the presence of depressive symptoms (Parada, et al., 2012). This shows the importance of building a strong and culturally sensitive program where DCS serve as pivotal providers to address issues of poor compliance, lack of trust or other psychosocial aspects that interfere with the patient's ability to comply with recommended medical and psychiatric treatment. Also future studies need to validate the reliability of delivering our culturally-modified problem solving-therapy in Spanish among low-health literacy individuals living by the US-Mexico border.
We considered our DCS as one alternative to developing a trained workforce of community mental health workers. Previous research reviews have addressed that community mental health workers are crucial in reducing health disparities among Hispanic/Latinos from different acculturation and socio-cultural immigration backgrounds (Elder JP, Ayala GX, Parra-Medina D, & Talavera GA, 2009). Future studies will examine the feasibility and outcomes of training community mental health workers to deliver our described culturally sensitive problem solving intervention. This could be complemented by using the communication-persuasion model. This model suggests how various forms of public communication and engagement can change attitudes and behaviors(Elder JP, et al., 2009). This same model has been successful in reducing signs and symptoms of diabetes by improving awareness and importance of treatment (Elder JP, et al., 2009; Teufel-Shone NI, Drummond R, & Rawiel U, 2005). This same theoretical model could be applied to behavioral health to improve different symptoms of depression and anxiety. Our study is an important stepping stone in that direction.
Another interesting finding was the effect modification observed with smoking among men with depressive symptoms. Studies have recently described that comorbid smoking among Hispanic/Latinos is a major contributor to the development of depression from early age and is a poor predictor for recovery (Escobedo, Kirch, & Anda, 1996). Additionally, data showed that a history of major depression is significantly associated with progression of smoking (OR:3.0;95%CI:1.1-8.2) and a history of smoking is also significantly associated with the progression of major depressive symptoms (OR:1.9;95%CI:1.1,3.4). It has been demonstrated that emotional factors are one of the main reasons that prevent individuals from engaging in smoking cessation programs delivered by community health workers (Dawson AP, Cargo M, Stewart H, Chong A, & Daniel M, 2012).
Studies have shown that daily stressors such as acculturation, family conflict and perceived sense of discrimination are significantly associated with depression and smoking among Hispanic/Latinos (Lorenzo-Blanco EI & Cortina LM, 2013) and might be gender specific (Bethel JW & Schenker MB, 2005). A cross-sectional study of 2,554 Hispanic/Latinos from different backgrounds found that individuals with perceived discrimination and family conflict had a significant association with depression and smoking. Interestingly the association was stronger for women than for men (Lorenzo-Blanco EI & Cortina LM, 2013). In a similar study among Hispanic/Latino youth, Lorenzo-Blanco et al. showed that young women tend to have higher levels of depression and smoking compared to men when facing specific stressors such as perceived discrimination with acculturation (Lorenzo-Blanco EI, Unger JB, Ritt-Olson A, Soto D, & Baezconde-Garbanati L, 2011). Our results showed that men have higher levels of depression and smoking compared to females. Due to program limitations, we did not measure acculturation, perceived discrimination, family conflict and other life stressors in our sample. Based on the characteristics of our sample (low-SES patients living by the US-Mexico border) we speculate that stressors including acculturation, perceived family, social and economic problems could explain the higher levels of depressive symptoms and smoking among men than women. Another hypothesis is that lack of family cohesion or familism might affect men in higher proportion that women in our sample, being reflected in higher depressive symptoms and smoking. This hypothesis needs to be further tested since the literature has reported that high family conflict and low family cohesion affects more women than men and is associated with depression and smoking among Hispanic/Latinos (Lorenzo-Blanco EI & Cortina LM, 2013). Future studies will also examine the use of community mental health workers to deliver treatments for patients living by the US-Mexico border to reduce symptoms of depression, improve family conflict, life stressors and reduce risk factors for cardiovascular disease (smoking) using culturally-modified evidence based psychosocial interventions.
Experts in community based participatory research have implemented a curriculum toolbox for trained community mental health workers to address comorbid depression among Hispanic/Latinos suffering from diabetes (Reinschmidt KM & Chong J, 2007). The authors addressed the fact that Hispanic/Latinos tend to confuse their emotional afflictions with somatic complaints, making it difficult for primary care providers to identify and refer for behavioral health treatment. Another important factor that precludes Hispanics/Latinos from receiving behavioral health treatment is the high degree of stigma associated with mental health illnesses. The stigma is associated with lack of awareness/knowledge about symptoms of depression, stress and anxiety and lack of access to behavioral health treatment, especially in rural areas by the US-Mexico border (Cherrington, Ayala, Sleath, & Corbie-Smith, 2006; Schraufnagel TJ, Wagner AW, Miranda J, & Roy-Byrne PP, 2006). These factors also contribute to increase the already reported higher prevalence of depression among Hispanic/Latinos compared to other US ethnic groups (Reinschmidt KM & Chong J, 2007).
Although there is a paucity of research addressing the use of DCS to address chronic mental health issues, our findings show the value and feasibility of using trained DCS to deliver a culturally modified intervention to improve symptoms of depression among Hispanic/Latinos. Additionally, this study shows the improvement of depressive symptoms over time by delivering the culturally tailored problem solving therapeutic intervention. The use of behavioral interventions has been advocated to improve mental health in underserved communities (Bocker E, Glasser M, Nielsen K, & Weidenbacher-Hoper V, 2012). Additionally, studies have previously reported that supportive therapeutic interventions by non-medical workers adequately address symptoms of depression, especially around the post-partum period (McComish JF, Groh CJ, & Moldenhauer JA, 2013). This period is marked by an increased risk of developing major depression and similar serious mood disorders (Di Florio A et al., 2013; Tavares D et al., 2012; Topiwala A, Hothi G, & Ebmeier KP, 2012).
Our study has several limitations related to the fact that it was a service-oriented program designed by the County of San Diego but adapted by the community health center. The small sample size reflects the preliminary results presented in this manuscript. Other covariates such as lipids, blood pressure, glucose and body mass index and use of antidepressants that could explain improvement of depressive symptoms were not available. The service-oriented nature of the program prevented us from having a comparison group, so caution should be used when interpreting the effectiveness of the culturally-tailored approach. Furthermore, due to the design of the study and effect size, caution should be used when generalizing our findings to similar groups of Hispanic/Latinos living in other communities or from other backgrounds. Conversely, our study has considerable strengths. First is the longitudinal examination in the trend of symptoms over a 6 month period. Furthermore, to the best of our knowledge this is one of the few studies that examined a culturally tailored IMPACT and PST model targeting depressed Hispanic/Latino patients living in a low-health literally community by the US-Mexico border. Additionally, the strength of using co-located trained DCS denoted the feasibility of delivering culturally tailored evidence based psychosocial approach to improve symptoms of depression.
In conclusion, our manuscript shows that depression care specialists delivering a culturally tailored problem solving therapy are valuable providers that could be co-located in community health centers to improve symptoms of depression. Randomized-controlled trials are needed to assess the effectiveness of trained depression care specialists to deliver the described culturally tailored intervention compared to usual care. These trials will validate if our intervention improves symptoms of depression, anxiety and comorbid cardiovascular risk factors for patients attending community health centers in urban and rural settings.
Table 4.
Proportions of PHQ-9 by categories at baseline and 6 months post-treatment
| PHQ-9 Categories | ||
|---|---|---|
| Depressive Symptoms | Baseline, n (%) | Post-Test, n (%) |
| Mild (5-9) | 1 (5.3) | 18 (94.7) |
| Moderate (10-14) | 50 (68.5) | 23 (31.5) |
| Severe (>15) | 138 (90.8) | 14 (9.2) |
Acknowledgements
Special thanks to staff and administration of San Ysidro Health Center in San Diego County, CA. The study was supported by Grant Number P20MD002293-01, from the San Diego EXPORT Center, National Center of Minority Health and Health Disparities and grant number T32HL079891 from the National Heart Lung and Blood Institute, National Institutes of Health. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
References
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165(3):359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arean P, Hegel M, Vannoy S, Fan M-Y, Unuzter J. Effectiveness of Problem-Solving Therapy for Older, Primary Care Patients With Depression: Results From the IMPACT Project. The Gerontologist. 2008;48(3):311–323. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- Arean PA, Perri MG, Nezu AM, Schein RL, Christopher F, Joseph TX. Comparative effectiveness of social problem-solving therapy and reminiscence therapy as treatment for depression in older adults. J Consult Clin Psychol. 1993;61(6):1003–1010. doi: 10.1037//0022-006x.61.6.1003. [DOI] [PubMed] [Google Scholar]
- Balcázar H, Alvarado M, Cantu F, Pedregon V, Fulwood R. A promotora de salud model for addressing cardiovascular disease risk factors in the US-Mexico border region. Prev Chronic Dis. 2009;6:1, A02. [PMC free article] [PubMed] [Google Scholar]
- Balcazar H, Alvarado M, Hollen ML, Gonzalez-Cruz Y, Hughes O, Vazquez E, et al. Salud Para Su Corazon-NCLR: a comprehensive Promotora outreach program to promote heart-healthy behaviors among hispanics. Health Promot Pract. 2006;7(1):68–77. doi: 10.1177/1524839904266799. [DOI] [PubMed] [Google Scholar]
- Balcázar H, Wise S, Rosenthal EL, Ochoa C, Rodriguez J, Hastings D, et al. An ecological model using promotores de salud to prevent cardiovascular disease on the US-Mexico border: the HEART project. Prev Chronic Dis. 2012;9:E35. doi: 10.5888/pcd9.110100. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med. 2005;29(2):143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Bocker E, Glasser M, Nielsen K, Weidenbacher-Hoper V. Rural older adults' mental health: status and challenges in care delivery. Rural Remote Health. 2012;12:2199. Epub. [PubMed] [Google Scholar]
- Breslau J BGTD, et al. Migration from mexico to the united states and subsequent risk for depressive and anxiety disorders: A cross-national study. Archives of General Psychiatry. 2011;68(4):428–433. doi: 10.1001/archgenpsychiatry.2011.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- California Mental Health Services Authority [Nov 2013];Integrated Behavioral Health Project. Warm Hand-Off Referrals By the Primary Care Provider To the Behavioralist. Available at http://www.ibhp.org/?section=pages&cid=122. 2007.
- Center for Disease Control and Prevention (CDC) Smoking attributable mortality, years of potential life lost, and productivity losses–united states, 2000–2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226–1228. [PubMed] [Google Scholar]
- Cherrington A, Ayala GX, Sleath B, Corbie-Smith G. Examining Knowledge, Attitudes, and Beliefs About Depression Among Latino Adults With Type 2 Diabetes. The Diabetes Educator. 2006;32(4):603–613. doi: 10.1177/0145721706290836. [DOI] [PubMed] [Google Scholar]
- Dawson AP, Cargo M, Stewart H, Chong A, Daniel M. Aboriginal health workers experience multilevel barriers to quitting smoking: a qualitative study. Int J Equity Health. 2012 2012 May 23;11:27, 11, 27. doi: 10.1186/1475-9276-11-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Florio A, Forty L, Gordon-Smith K, Heron J, Jones L, Craddock N, et al. Perinatal episodes across the mood disorder spectrum. JAMA Psychiatry. 2013;70(2):168–175. doi: 10.1001/jamapsychiatry.2013.279. [DOI] [PubMed] [Google Scholar]
- Duarté-Vélez Y, Bernal G, Bonilla K. Culturally adapted cognitive-behavior therapy: integrating sexual, spiritual, and family identities in an evidence-based treatment of a depressed Latino adolescent. Journal of Clinical Psychology. 2010;66(8):895–906. doi: 10.1002/jclp.20710. [DOI] [PubMed] [Google Scholar]
- Elder JP, Ayala GX, Parra-Medina D, Talavera GA. Health communication in the Latino community: issues and approaches. Annu Rev Public Health. 2009;30(227-51) doi: 10.1146/annurev.publhealth.031308.100300. [DOI] [PubMed] [Google Scholar]
- Ell K. [April 2013];Social Worker-Led, Culturally Tailored Therapy and Support Improve Treatment Adherence, Depression-Related Symptoms, and Patient Satisfaction in Low-Income Hispanics With Diabetes. Available at http://www.innovations.ahrq.gov/content.aspx?id=3318.
- Ell K, Katon W, Xie B, Lee P-J, Kapetanovic S, Guterman J, et al. One-year postcollaborative depression care trial outcomes among predominantly Hispanic diabetes safety net patients. General Hospital Psychiatry. 2011;33(5):436–442. doi: 10.1016/j.genhosppsych.2011.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobedo LG, Kirch DG, Anda RF. Depression and smoking initiation among US Latinos. Addiction. 1996;91(1):113–119. [PubMed] [Google Scholar]
- Gilmer TP, Walker C, Johnson ED, Phlis-Tsimikas A, Unützer J. Improving Treatment of Depression Among Latinos With Diabetes Using Project Dulce and IMPACT. Diabetes Care. 2008;31:1324–1326. doi: 10.2337/dc08-0307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Prendes AA, Hindo C, Pardo Y. Cultural Values Integration in Cognitive-Behavioral Therapy for a Latino With Depression. Clin Case Studies. 2011;10(5):376–394. [Google Scholar]
- González HM, Tarraf W, Whitfield K, Gallo JJ. Vascular depression prevalence and epidemiology in the United States. J Psychiatr Res. 2012;(46):4. doi: 10.1016/j.jpsychires.2012.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González HM, Tarraf W, Whitfield KE, Vega WA. The epidemiology of major depression and ethnicity in the United States. J Psychiatr Res. 2010;44(15):1043–1045. doi: 10.1016/j.jpsychires.2010.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: too little for too few. Arch Gen Psychiatry. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grazier KL, Smith JE, Song J, Smiley ML. Integration of Depression and Primary Care: Barriers to Adoption. Journal of Primary Care & Community Health. 2013 doi: 10.1177/2150131913491290. [DOI] [PubMed] [Google Scholar]
- Hegel MT, Dietrich AJ, Seville JL, Jordan CB. Training residents in problem-solving treatment of depression: a pilot feasibility and impact study. Fam Med. 2004;36(3):204–208. [PubMed] [Google Scholar]
- Herrman H, Patrick DL, Diehr P, Martin ML, Fleck M, Simon GE, et al. Longitudinal investigation of depression outcomes in primary care in six countries: the LIDO study. Functional status, health service use and treatment of people with depressive symptoms. Psychol Med. 2002;32(5):889–902. doi: 10.1017/s003329170200586x. [DOI] [PubMed] [Google Scholar]
- Huang FY, Chung H, Kroenke K, Delucchi KL, Spitzer RL. Using the patient health questionnaire-9 to measure depression among racially and ethnically diverse primary care patients. Journal of General Internal Medicine. 2006;21:547–552. doi: 10.1111/j.1525-1497.2006.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inagaki M, Ohtsuki T, Yonemoto N, Oikawa Y, Kurosawa M, Muramatsu K, et al. Prevalence of depression among outpatients visiting a general internal medicine polyclinic in rural Japan. General Hospital Psychiatry. (0) doi: 10.1016/j.genhosppsych.2012.11.013. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, Simon G, Ludman E, Bush T, et al. Improving primary care treatment of depression among patients with diabetes mellitus: the design of the pathways study. Gen Hosp Psychiatry. 2003;25:158–168. doi: 10.1016/s0163-8343(03)00013-6. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, Simon G, Walker E, Unützer J, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56(12):1109–1115. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, Walker E, Simon GE, Bush T, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA. 1995;273(13):1026–1031. [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Olfson M, Broadhead WE, Barrett JE, Blacklow RS, Keller MB, et al. Prevalence of mental disorders in primary care. Implications for screening. Arch Fam Med. 1995;4(10):857–861. doi: 10.1001/archfami.4.10.857. [DOI] [PubMed] [Google Scholar]
- Lin EHB, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of Depression and Diabetes Self-Care, Medication Adherence, and Preventive Care. Diabetes Care. 2004;27(9):2154–2160. doi: 10.2337/diacare.27.9.2154. [DOI] [PubMed] [Google Scholar]
- Little V. Transdisciplinary care: opportunities and challenges for behavioral health providers. J Health Care Poor Underserved. 2010;21(4):1103–1107. doi: 10.1353/hpu.2010.0930. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Blanco EI, Cortina LM. Latino/a depression and smoking: an analysis through the lenses of culture, gender, and ethnicity. Am J Community Psychol. 2013;51(3-4):332–346. doi: 10.1007/s10464-012-9553-3. [DOI] [PubMed] [Google Scholar]
- Lorenzo-Blanco EI, Unger JB, Ritt-Olson A, Soto D, Baezconde-Garbanati L. Acculturation, gender, depression, and cigarette smoking among U.S. Hispanic youth: the mediating role of perceived discrimination. J Youth Adolesc. 2011;40(11):1519–1533. doi: 10.1007/s10964-011-9633-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin H, Escobar JI, Vega WA. Mental illness in Hispanics: a review of the literature. Focus. 2006;4:23–37. Focus 4:23–37, 2006. [Google Scholar]
- McComish JF, Groh CJ, Moldenhauer JA. Development of a doula intervention for postpartum depressive symptoms: participants’ recommendations. J Child Adolesc Psychiatr Nurs. 2013;26(1):3–15. doi: 10.1111/jcap.12019. [DOI] [PubMed] [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine definition of disparities: An application to mental health care. Health Serv Res. 2006;5:1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno FA, Chong J, Dumbauld J, Humke M, Byreddy S. Use of standard Webcam and Internet equipment for telepsychiatry treatment of depression among underserved Hispanics. Psychiatr Serv. 2012;63(12):1213–1217. doi: 10.1176/appi.ps.201100274. [DOI] [PubMed] [Google Scholar]
- Parada H, Horton LA, Cherrington A, Ibarra L, Ayala GX. Correlates of Medication Nonadherence Among Latinos With Type 2 Diabetes. The Diabetes Educator. 2012;38(4):552–561. doi: 10.1177/0145721712445215. [DOI] [PubMed] [Google Scholar]
- Patton GC, Carlin JB, Coffey C, Wolfe R, Hibbert M, Bowes G. Depression, anxiety, and smoking initiation: a prospective study over 3 years. American Journal of Public Health. 1998;88(10):1518–1522. doi: 10.2105/ajph.88.10.1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philis-Tsimikas A, Fortmann A, Lleva-Ocana L, Walker C, Gallo LC. Peer-Led Diabetes Education Programs in High-Risk Mexican Americans Improve Glycemic Control Compared With Standard Approaches: A Project Dulce promotora randomized trial. Diabetes Care. 2011;34(9):1926–1931. doi: 10.2337/dc10-2081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reinschmidt KM, Chong J. SONRISA: a curriculum toolbox for promotores to address mental health and diabetes. Prev Chronic Dis. 2007;4(4):A101. Epub. [PMC free article] [PubMed] [Google Scholar]
- Ryabov I. The impact of community health workers on behavioral outcomes and glycemic control of diabetes patients on the U.S.-Mexico border. Int Q Community Health Educ. 2010;31(4):387–399. doi: 10.2190/IQ.31.4.f. [DOI] [PubMed] [Google Scholar]
- Schraufnagel TJ, Wagner AW, Miranda J, Roy-Byrne PP. Treating minority patients with depression and anxiety: what does the evidence tell us? Gen Hosp Psychiatry. 2006;28(1):26–36. doi: 10.1016/j.genhosppsych.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Tavares D, Quevedo L, Jansen K, Souza L, Pinheiro R, Silva R. Prevalence of suicide risk and comorbidities in postpartum women in Pelotas. Rev Bras Psiquiatr. 2012;34(3):270–276. doi: 10.1016/j.rbp.2011.12.001. [DOI] [PubMed] [Google Scholar]
- Teufel-Shone NI, Drummond R, Rawiel U. Developing and adapting a family-based diabetes program at the U.S.-Mexico border. Prev Chronic Dis. 2005;2(1):1–9. [PMC free article] [PubMed] [Google Scholar]
- Topiwala A, Hothi G, Ebmeier KP. Identifying patients at risk of perinatal mood disorders. Practitioner. 2012;256(1751):15–28. [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, Williams JW, Hunkeler E, Harpole L, et al. Collaborative Care Management of Late-Life Depression in the Primary Care Setting. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. Health Resources and Service Administration (HRSA) [Jan 2014];Primary Care: The Health Center Program. Centro de Salud de la Comunidad San Ysidro. Available at: http://bphc.hrsa.gov/uds/datacenter.aspx?q=d&bid=091080&state=CA.
- World Health Organization . The World Health report 2004: Changing history, annex table 3: Burden of disease in DALYs by cause, sex, and mortality stratum in WHO regions, estimates for 2002. Geneva: 2004. [Oct 2012]. Available at: http://www.emro.who.int/health-topics/depression/. [Google Scholar]