Abstract
Objective
The purpose of this paper is to present a case of a patient with neck pain, tinnitus, and headache in the setting of bilateral elongated styloid processes (ESP) and calcified stylohyoid ligaments (CSL), how knowledge of this anatomical variation and symptomatic presentation affected the rehabilitation management plan for this patient, and to discuss the potential relevance of ESPs and CSLs to carotid artery dissection.
Clinical features
A 29-year-old male military helicopter mechanic presented for chiropractic care for chronic pain in the right side of his neck and upper back, tinnitus, and dizziness with a past history of right side parietal headaches and tonsillitis. Conventional radiographs showed C6 and C7 spinous process fractures, degenerative disc disease at C6/7, and an elongated right styloid process with associated calcification of the left stylohyoid ligament. Volumetric computerized tomography demonstrated calcification of the stylohyoid ligaments bilaterally.
Intervention and outcome
Given the proximity of the calcified stylohyoid apparatus to the carotid arteries, spinal manipulation techniques were modified to minimize rotation of the neck. Rehabilitation also included soft tissue mobilization and stretching, corrective postural exercises, and acupuncture. An otolaryngologist felt that the symptoms were not consistent with Eagle syndrome and the tinnitus was associated with symmetric high frequency hearing loss, likely due to occupational noise exposure. Initially, the patient's symptoms improved but plateaued by the fifth visit.
Conclusion
Neck pain in the presence of ESPs and CSLs can be associated with Eagle syndrome, which can include ipsilateral head and neck pain, odynophagia, dysphagia, and cerebrovascular symptoms. This case, initially thought to be Eagle syndrome, highlights proper diagnostic workup for this condition and presents potential contraindications to consider with regard to cervical spine manipulation in such patients. Manual therapy precautions pertaining to cervical spine manipulation may be appropriate in cases involving ESPs and calcified stylohyoid ligaments.
Key indexing terms: Neck pain; Manipulation, spinal; Elongated styloid process syndrome; Carotid artery, internal
Introduction
Neck pain is a common problem in the general population with a 12-month prevalence between 30% and 50% and a lifetime prevalence exceeding 60%.1 Because of its frequency and often-times associated disability, people seek relief of their neck pain from a variety of health care providers.2 Cervical spine manipulation and mobilization is a common procedure employed by chiropractors, physical therapists, osteopaths, and others to relieve neck pain.2 Anatomical variations in the neck may present relative contraindications for various types of manipulative procedures, such as high velocity, low amplitude thrust manipulation.
Elongated styloid processes (ESP) and calcified stylohyoid ligaments (CSL) may be part of a condition known as Eagle syndrome. Named after prominent otolaryngologist Dr Watt Eagle4 (Fig 1), Eagle syndrome includes a sensation of a foreign body in the throat, odynophagia, and dysphagia and often includes pain in the neck or face,3 as cranial nerves are affected by crowding or compression by the anomalous ESP or CSL. Eagle syndrome may also include symptoms suggestive of cerebrovascular compromise, such as dizziness, headache, syncope, and transient visual loss if the internal carotid artery is affected.4 Symptoms may be more bothersome with head and neck rotation as the structures undergo increased compression or tension from the ESP or CSL.4
Fig 1.

Dr Watt W. Eagle, for whom Eagle syndrome is named. Photograph published with permission of Duke University Medical Center Archives.
There is literature that discusses the relevance of ESPs and CSLs to both traumatic and spontaneous internal carotid artery dissection. However, there are few publications that discuss the relevance of these neighboring anatomical structures as they pertain to manual therapies, such as manipulation or mobilization, of the cervical spine. The purpose of this paper is to present a case of a patient with neck pain, tinnitus, and headache in the setting of bilateral ESPs and CSLs and how knowledge of this anatomical variation and symptomatic presentation affected the rehabilitation management plan for this patient. We also discuss the potential relevance of ESPs and CSLs to carotid artery dissection.
Case Report
A 29-year-old male United States Marine helicopter mechanic was referred to the primary author for chiropractic care for chronic pain in the right side of his neck and upper back, which started 7 years earlier after sustaining a cervical flexion injury during Marine Corps martial arts training. At that time he fell from a height of approximately 3 ft onto the back of his head. The patient described the chronic, constant pain as an aching sensation and he felt the need to frequently stretch his neck or “crack it”; however, nothing actually provided sustained relief. Prolonged static postures, such as sustained desk work, or vigorous activity tended to aggravate the pain. He had no pain or altered sensation in his upper extremities. His pain was generally moderate in intensity, rating it a 7 out of 10 on a verbal pain scale (VPS). He had received various interventions over the previous several years from his primary care providers, neurologists, physical therapists, and chiropractors without resolution. A review of systems revealed that the patient had concurrent tinnitus and dizziness and a past history of right side parietal headaches and right side tonsillitis. He had no loss of consciousness, no dysphagia, dysphonia, nystagmus, nausea or vomiting.
The patient posture demonstrated anterior head carriage, increased kyphosis and rounded forward shoulders. He had an increase in neck and upper back pain on his right side with flexion and left rotation of his neck. The patient's neck pain was reproduced by pressing down on the top of his head and palpation of the right cervicothoracic extensor and upper trapezius muscles. He showed no signs of cervical nerve root tension or impingement. Cranial nerve, cervical nerve root, and brachial plexus examinations were unremarkable.
Conventional radiographs had been previously obtained by the patient's primary care provider 1 month prior to his chiropractic consultation and demonstrated old C6 and C7 spinous process (“clay shoveler's”) fractures, degenerative disc disease at C6/7 hypolordosis, and a right ESP with left CSL (Fig 2). The radiologist noted that ESPs and CSL can be seen in Eagle syndrome and recommended clinical correlation. Thoracic plain films were normal. The patient was diagnosed with mechanical cervicothoracic pain and myalgia.
Fig 2.
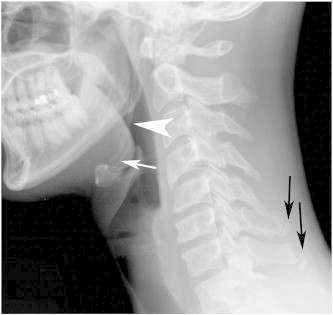
Conventional radiograph of the cervical spine showed an elongated styloid process on the right (white arrowhead) and calcification of the left stylohyoid ligament (white arrow). Old clay shoveler's fractures of C6 and C7 (black arrows) and degenerative disc disease at C6/7 are also visible.
The patient was scheduled for treatment twice a week for 2 weeks. The rehabilitation regimen was created using precautions to avoid end range loading of the cervical spine into rotation, lateral bending, or combinations of the 2 movements due to the ESP/CSL. The upper thoracic spine was manipulated in the prone position while the head of the patient was stabilized to reduce rotation and lateral bending and the head portion of the table was set to maintain spinal neutral. Supine or seated cervical spine manipulation procedures were not used to avoid rotating the cervical spine. Soft tissue mobilization of the right cervical paravertebral and upper trapezius muscles was performed with the patient in a seated position. For these procedures, the patient positioned his head into the contracted muscle position and then slowly moved to the neutral cervical position while digital pressure was applied to tender points in the muscle. The patient was also given a home exercise program of corrective postural exercises that included stretching, strengthening, and proprioceptive exercises. Education on proper computer ergonomics was also provided since part of his job involved prolonged computer use.
At his third office visit he stated that his tinnitus was more predominant in his right ear but denied any alteration in symptoms with changes in head position and no positional dizziness, which are both characteristic of Eagle syndrome. He had no headache on this visit and his neck pain severity was reduced to a VPS of 4/10) from previous visits. A re-examination revealed no significant changes in his exam findings. With Eagle syndrome being a differential diagnosis, specific confirmatory tests were conducted, which were negative, including no reproduction of Eagle syndrome symptoms with palpation of the tonsillar pillars, and no increase in tinnitus or production of dizziness with active or passive head positioning into end range of motion for extension, flexion, side bending, or rotation. Treatment was continued and computed tomography angiography of the neck was ordered after consultation with the radiologist.
The patient's pain plateaued by the fifth office visit. He reported mild reduction in his pain after each treatment but the pain would return to moderate levels of severity within 24 to 48 hours. The patient's tinnitus also plateaued. Treatment focusing on a home based exercise program for postural correction continued while awaiting the computed tomography examination and results. The volumetric helical computed tomography demonstrated calcification of the stylohyoid ligaments and imaging of the spatial relationship between the ESPs and carotid arteries (Figs 3-4). At the report of imaging findings the patient reported no improvements in his symptoms and an elevated level of concern regarding his tinnitus. A consultation with an otolaryngologist was made for a definitive evaluation for Eagle syndrome or other pathology and the patient was also referred to a physical therapist for acupuncture treatment while he continued with chiropractic care.
Fig 3.
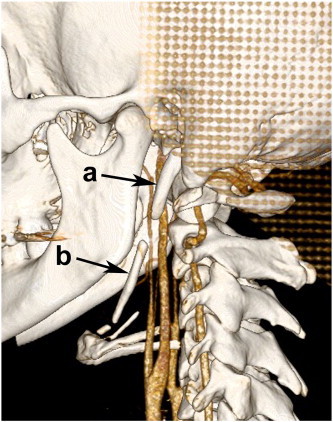
Volumetric helical CT data set reformatted for 3D bone surface shadow rendering as viewed from the left oblique clearly showing the elongated styloid process (A) on the left and ossification of the stylohyoid ligament (B). The elongated styloid process traverses immediately lateral to the internal jugular vein and to the cervical internal carotid artery but does not have significant mass effect on the cervical internal carotid artery. The branches of the external carotid artery are immediately lateral to the ossified stylohyoid ligament between the cervical segments of the internal and external carotid arteries, also exhibiting no significant mass effect on these vessels in neutral position.
Fig 4.
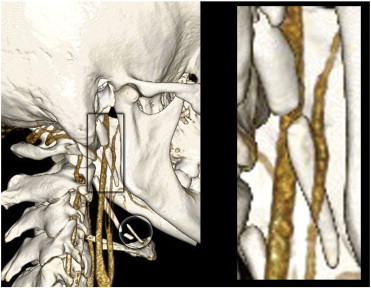
Three-dimensional rendering as viewed from the patient's right oblique shows the elongated styloid process on the right in the boxed area. The boxed area is presented on the right side of the figure in magnified form for better viewing of the elongated styloid process. This view more clearly demonstrates the close proximity of the styloid process to the sensitive vasculature of the neck, as it marginates both the internal and external carotid arteries. The lesser degree of ossification of the right stylohyoid ligament is seen in the circled area.
Acupuncture treatment consisted of electroacupuncture for 20 minutes at 2 Hz with needles placed at the right BL11, TH15, BL42, and BL44 as well as GB20 and GV20 without electrical stimulation. The patient received 4 acupuncture treatments with needles placed as indicated by clinical exam but usually in the above locations. On 1 visit he was treated with additional needle placement without electrical stimulation of the right Shen Men point and point zero. The patient's numerical pain scale usually was a 4/10 before acupuncture treatment and either the same or 1 point lower after treatment.
The patient was thoroughly evaluated by the otolaryngologist to include a comprehensive series of hearing tests. His physical examination was normal and he had normal tympanograms. His hearing tests showed mild high frequency bilateral hearing reduction that was symmetrical and consistent with occupational exposure to loud noises. The otolaryngologist reported that the patient did not have Eagle syndrome.
The patient had a total of 8 chiropractic treatments and 5 physical therapy (acupuncture) treatments. He reported decreased neck stiffness but his pain remained at a level of approximately VPS of 4/10. He continued to have tinnitus. No adverse effects were reported during treatment. Due to military commitments and a lack of further improvement in his symptoms, care was discontinued.
Discussion
Calcified stylohyoid ligaments are thought to be the result of post-tonsillectomy or traumatic scarring.4,6 Elongated styloid processes develop from variations in embryological development.7 A styloid process is typically considered to be long when it is more than 30 mm.4,7 Most anatomical variants pose little risk in manual therapy but this case is a potential example of an exception to this rule. Fusco and colleagues state that a styloid process longer than 30 mm is considered to be an increased risk for Eagle syndrome.4 Both ESPs and CSLs can be associated with Eagle syndrome; mechanisms for the production of symptoms include compressive cranial neuropathy and compression of the carotid artery and/or jugular vein by the ESP and or CSL.4,6,7
When encountered in clinical practice, one may wonder if ESPs and CSLs should be considered contraindications for manipulation of the cervical spine. Two primary issues should be considered with regard to complications. The first is the potential of fracturing the ESP or CSL. Fractures of ESPs have been reported with traumatic8 and spontaneous6 mechanisms of injury. Thus, a manipulative contact on the styloid process area could feasibly induce iatrogenic fracture, resulting in pain and symptoms of Eagle syndrome. Echoing what Cagnie and colleagues9 have discussed previously, we feel that care should be taken when applying manual procedures.
The second potential complication of an ESP or CSL relates to how these structures may affect the arteries they juxtapose in the neck. Radiology authorities Yochum and Rowe state in their third edition (published in 2005), “Stylohyoid ligament ossification does not appear to be a contraindication to cervical spine manipulation, although careful technique selection is required to reduce rotation and avoid a possibly painful direct contact over the ligament.”10 They further state that there were no published cases that demonstrate that CSLs should be considered risk factors for dissection of the carotid artery.10
Yochum and Rowe do not discuss the potential of an ESP to damage the carotid arteries. Several cases of internal carotid artery dissection have been reported where an ESP was the cited cause.5,11–14 In these cases, the presentation of symptoms did not always follow forces to the neck, suggesting that spontaneous dissection occurs.13 Higher level evidence is found in a recent case-control study that investigated the lengths of styloid processes in 38 cervical carotid artery dissection cases and matched controls.15 Raser and colleagues found that people who had dissection had slightly elevated odds of having a longer styloid process on the side of dissection compared to controls (OR, 1.08/mm; 95% CI, 1.00-1.17). However, when looking at the highest quartile of styloid process length, compared with the lower 3 quartiles, the odds of cervical carotid artery dissection were significantly greater (OR, 4.0; 95% CI 1.3-14.2).15 These findings led the research team to hypothesize that it may be possible for a long styloid process to injure a cervical carotid artery. Given the previous discussion and after reviewing the imaging contained in this report and others, it seems reasonable to assume in the interest of patient safety that because of the proximity of ESPs to sensitive neurovascular structures, this anatomic anomaly may pose a relative contraindication for thrust manipulation of the cervical spine.
In searching the literature, we were only able to find 1 other study that discusses the potential clinical relevance, as it pertains to mobilization of the cervical spine, to ESPs or CSLs. In the case report by Cagnie et al,7 the authors discuss the relevance of ESPs and CSLs to the vertebral artery and do not discuss the carotid artery. As far as we are aware, this is the first case to discuss ESPs as a reason to use precautions when applying manual therapy to the cervical spine and neck tissues, as ESPs are associated with increased odds of carotid artery dissection in 1 study and cited as a cause of carotid artery dissection in several case reports.
Conclusion
This study describes a patient with neck pain and other symptoms in the presence of ESPs and CSLs that initially suggested Eagle syndrome as a diagnosis. This diagnosis was later ruled out by an otolaryngologist, however the patient's clinical findings and anatomic features prompted the use of precautions pertaining to the use of cervical spine manipulation. This case highlights proper diagnostic workup for this condition and presents potential contraindications to consider with regard to cervical spine manipulation in such patients. We therefore propose that because of the proximity of ESPs to sensitive neurovascular structures, this anatomic anomaly may pose a relative contraindication for thrust manipulation of the cervical spine.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Footnotes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
Refereeing Editor: Jerrilyn Cambron, DC, PhD (jcambron@nuhs.edu), was the Refereeing Editor for this manuscript. She was solely responsible for managing the peer review process, revision process, and the acceptance of this manuscript. The Editor and Associate Editor declare that they were not involved in the peer review process or acceptance decision for this paper.
References
- 1.Hogg-Johnson S., van der Velde G., Carroll L.J. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl.):S39–S51. doi: 10.1097/BRS.0b013e31816454c8. [Epub 2008/02/07. 00007632-200802151-00009 [pii]. PubMed PMID: 18204398] [DOI] [PubMed] [Google Scholar]
- 2.Hurwitz E.L., Carragee E.J., van der Velde G. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976) 2008;33(4 Suppl.):S123–S152. doi: 10.1097/BRS.0b013e3181644b1d. [Epub 2008/02/07, 00007632-200802151-00016 [pii]. PubMed PMID: 18204386] [DOI] [PubMed] [Google Scholar]
- 3.Haynes M.J., Vincent K., Fischhoff C., Bremner A.P., Lanlo O., Hankey G.J. Assessing the risk of stroke from neck manipulation: a systematic review. Int J Clin Pract. 2012;66(10):940–947. doi: 10.1111/j.1742-1241.2012.03004.x. [PubMed PMID: 22994328; PubMed Central PMCID: PMC3506737] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fusco D.J., Asteraki S., Spetzler R.F. Eagle's syndrome: embryology, anatomy, and clinical management. Acta Neurochir (Wien) 2012;154(7):1119–1126. doi: 10.1007/s00701-012-1385-2. [PubMed PMID: 22638594] [DOI] [PubMed] [Google Scholar]
- 5.Todo T., Alexander M., Stokol C., Lyden P., Braunstein G., Gewertz B. Eagle syndrome revisited: cerebrovascular complications. Ann Vasc Surg. 2012;26(5):729.e1–729.e5. doi: 10.1016/j.avsg.2011.12.005. [Epub 2012/06/06, PubMed PMID: 22664285] [DOI] [PubMed] [Google Scholar]
- 6.Blythe J.N., Matthews N.S., Connor S. Eagle's syndrome after fracture of the elongated styloid process. Br J Oral Maxillofac Surg. 2009;47(3):233–235. doi: 10.1016/j.bjoms.2008.08.009. [PubMed PMID: 18823683] [DOI] [PubMed] [Google Scholar]
- 7.Rechtweg J.S., Wax M.K. Eagle's syndrome: a review. Am J Otolaryngol. 1998;19(5):316–321. doi: 10.1016/s0196-0709(98)90005-9. [PubMed PMID: 9758180] [DOI] [PubMed] [Google Scholar]
- 8.Babad M.S. Eagle's syndrome caused by traumatic fracture of a mineralized stylohyoid ligament—literature review and a case report. Cranio. 1995;13(3):188–192. doi: 10.1080/08869634.1995.11678067. [PubMed PMID: 8949860] [DOI] [PubMed] [Google Scholar]
- 9.Cagnie B., Barbaix E., Vinck E., D'Herde K., Cambier D. A case of abnormal findings in the course of the vertebral artery associated with an ossified hyoid apparatus. A contraindication for manipulation of the cervical spine? J Manip Physiol Ther. 2005;28(5):346–351. doi: 10.1016/j.jmpt.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 10.Yochum T.R., Rowe L.J. 3rd ed. Lippincott Williams & Wilkins; Baltimore, MD: 2005. Yochum and Rowe's essentials of skeletal radiology. [Google Scholar]
- 11.Sveinsson O., Kostulas N., Herrman L. Internal carotid dissection caused by an elongated styloid process (Eagle syndrome) BMJ Case Rep. 2013 Jun;11:1–4. doi: 10.1136/bcr-2013-009878. [PubMed PMID: 23761567] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Razak A., Short J.L., Hussain S.I. Carotid artery dissection due to elongated styloid process: a self-stabbing phenomenon. J Neuroimaging. 2012 doi: 10.1111/j.1552-6569.2012.00759.x. [PubMed PMID: 23163559] [DOI] [PubMed] [Google Scholar]
- 13.Ohara N., Sakaguchi M., Okazaki S., Nagano K., Kitagawa K. Internal carotid artery dissection caused by an elongated styloid process: usefulness of transoral ultrasonography. J Stroke Cerebrovasc Dis. 2012;21(8):918.e7–918.e8. doi: 10.1016/j.jstrokecerebrovasdis.2012.05.014. [PubMed PMID: 22748713] [DOI] [PubMed] [Google Scholar]
- 14.Yamamoto S., Todo K., Kawamoto M., Kohara N. Carotid artery dissection associated with an elongated styloid process. Intern Med. 2013;52(9):1005–1006. doi: 10.2169/internalmedicine.52.0024. [PubMed PMID: 23648723] [DOI] [PubMed] [Google Scholar]
- 15.Raser J.M., Mullen M.T., Kasner S.E., Cucchiara B.L., Messe S.R. Cervical carotid artery dissection is associated with styloid process length. Neurology. 2011;77(23):2061–2066. doi: 10.1212/WNL.0b013e31823b4729. [PubMed PMID: 22116948] [DOI] [PubMed] [Google Scholar]


