Abstract
Background and Aims:
Continuous arterial pressure monitoring is essential in cardiac surgical patients during induction of general anaesthesia (GA). Continuous non-invasive arterial pressure (CNAP) monitoring is fast gaining importance due to complications associated with the invasive arterial monitoring. Recently, a new continuous non-invasive arterial pressure device (CNAP™) has been validated perioperatively in non-cardiac surgeries. The aim of our study is to compare and assess the performance of CNAP during GA with invasive arterial pressure (IAP) in patients undergoing cardiac surgeries.
Methods:
Sixty patients undergoing cardiac surgery were included. Systolic, diastolic, and mean arterial pressure (MAP) data were recorded every minute for 20 min simultaneously for both IAP and CNAP™. Statistical analysis was performed using mountain plot and Bland Altman plots for assessing limits of agreement and bias (accuracy) calculation. Totally 1200 pairs of data were analysed.
Results:
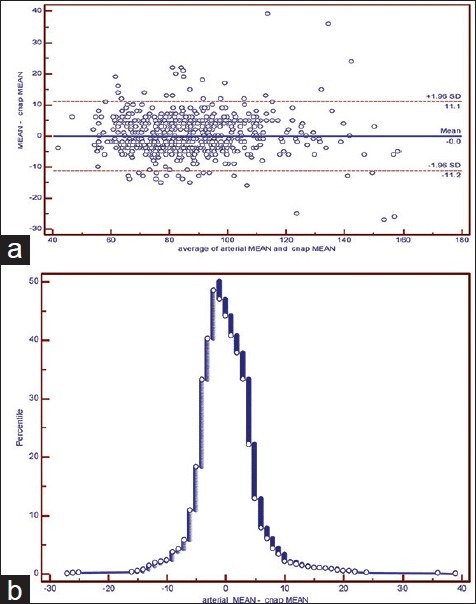
The CNAP™ systolic, diastolic and MAP bias was 5.98 mm Hg, −3.72 mm Hg, and − 0.02 mm Hg respectively. Percentage within limits of agreement was 96.0%, 95.2% and 95.7% for systolic, diastolic and MAP. The mountain plot showed similar results as the Bland Altman plots.
Conclusion:
We conclude CNAP™ provides real-time estimates of arterial pressure comparable to IAP during induction of GA for cardiac surgery. We recommend CNAP can be used as an alternative to IAP in situations such as cardiac patients coming for non-cardiac surgeries, cardiac catheterization procedures, positive Allen's test, inability to cannulate radial artery and vascular diseases, where continuous blood pressure monitoring is required.
Keywords: Continuous non-invasive arterial pressure, general anaesthesia, invasive arterial pressure
INTRODUCTION
Blood pressure (BP) is one of the most important cardiovascular parameters in clinical practice. Standard non-invasive BP (NIBP) monitoring is an intermittent, non-continuous procedure. Accurate measurement of arterial blood pressure (ABP) is essential for the rational management of adult cardiac surgical patients. This requirement is most commonly met by the placement of an intra-arterial catheter, which is considered the “gold standard” of ABP measurement in patients who may experience rapid changes in haemodynamic status.
Invasive arterial pressure (IAP) monitoring is essential in cardiac surgical patients during induction of general anaesthesia. Insertion of a radial artery cannula can lead to injury of the radial artery, requires skill[1] and there are situations especially in vascular surgery where there is no availability of arteries to cannulate. The post-procedural complications of radial artery cannulation include thrombosis, occlusion of the vessel with limb ischemia, haemorrhage and infection. In view of these problems, investigators have been evaluating non-invasive monitoring systems based on oscillometry, arterial tonometry and finapress principle but, data have been inconsistent.
Recent studies showed that continuous non-invasive arterial pressure (CNAP) measurements generated by a new device, called Infinity® continuous non-invasive arterial pressure device (CNAP™) SmartPod® (Draeger Medical Systems Inc., Telford, PA, USA), have been superior to intermittent oscillometric measurements during sedation for interventional endoscopy,[2] spinal anaesthesia for caesarean section[3] and during general anaesthesia (GA).[4] The basic principle of CNAP™ is the vascular unloading technique described by Penaz.
This new technology has not been yet validated in the operating room for cardiac surgical patients though it has been validated in the post-operative cardiac surgical setting.[5] The present study was designed to compare systolic, diastolic and mean arterial pressure (MAP) values between CNAP and IAP during induction of general anaesthesia for different cardiac surgical procedures.
METHODS
This study was approved by the Ethics Committee of our hospital and performed during February 2013-July 2013. Written informed consent was obtained from patients during the pre-operative visit. Patients above the age of 16 years undergoing cardiac surgery were recruited. Patients with body mass index > 40 kg/m2 or < 15 kg/m2 , low ejection fraction < 45%, absence of bilateral radial pulses, >5 mm Hg difference in ABP between the upper extremities, systemic vasculopathies, arterio-venous shunt, propensity to hand ischemia in the presence of radial arterial obstruction as evidenced by a positive Allen's test, hypothermia, Raynaud syndrome and related diseases, arrhythmias, were excluded from study.
Baseline demographics was recorded. All patients were pre-medicated with 0.5 mg of alprazolam in the previous night and 2 h before surgery. Standard monitoring with electrocardiography and pulse oximetry were attached and connected to a monitor. In the induction room, a 16G cannula was inserted into a peripheral vein for infusion of fluids and drugs. A 20G arterial line was inserted into the left radial artery after skin infiltration with 0.5–1 ml of 2% lignocaine and connected to transducer after calibration. The tubing and transducer were inspected to ensure that there were no technical issues or air bubbles that could cause erroneous recordings.
The basic principle of the CNAP™ is that the blood volume in a suitable artery is measured and kept constant by applying corresponding external pressure (i.e., volume clamping).The continuously changing external pressure that is needed to keep the arterial blood volume constant, directly corresponds to the arterial pressure and, therefore, is an instantaneous ABP. Inside the sensor cuff, the blood volume in the finger arteries is measured using an infrared light source and a light detector. During systole, with more blood in the artery, the absorption is stronger, and less light reaches the detector. During diastole, the absorption is weaker, and more light reaches the detector. The sensor cuff pressure is equal to the pressure in the artery under the sensor cuff and is, therefore, a direct real-time measure of ABP. Since the CNAP™ is measured on a small finger artery, it may not be representative of the systemic BP in large arteries. Thus, CNAP™ values are automatically and continuously corrected to absolute BP values obtained by the built-in monitor oscillometric NIBP device. The oscillometric BP readings are measured on the brachial artery and are triggered automatically every 15 min (calibration). In order to provide optimal patient comfort and measurement reliability, the sensor cuff alternates between the two fingers every 30 min. Only one sensor cuff is inflated at any given time.
The CNAP™ monitoring system consists of reusable finger cuffs, the cuff controller, and the CNAP™ pod, which interfaces into the patient monitor. The finger cuffs are available in three sizes (i.e. small, medium, and large) and consist of two semi-rigid cylinders containing inflatable cuffs, sensors and electronics inside, covering two adjacent fingers between digits 2nd and 4th . The adequately sized finger cuff was connected to the cuff controller that contains the pneumatic control unit of the inflatable parts of the finger cuff. The finger cuff was applied contralateral to the radial artery catheter. A 2.5 m long cable leads from the cuff controller to the CNAP™ pod that evaluates the CNAP curve. The NIBP measurements were performed on the same arm with the CNAP™ finger cuff.
During the study, all patients were supine and their arms were kept at the level of the heart. After 5 min of stabilisation, simultaneous measurements of IAP and CNAP were recorded every minute.
After pre-oxygenation with 100% oxygen, injection midazolam 0.05 mg/kg intravenous (i.v.), injection fentanyl 5 mcg/kg i.v. injection propofol 0.25 mg/kg i.v. injection vecuronium 0.1 mg/kg i.v. injection xylocard 1 mg/kg. i.v. were administered. The patient's trachea was intubated with appropriate size endotracheal tube and mechanical ventilation was started using volume-controlled ventilation. Oxygen-air mixture and ventilation parameters were adjusted to maintain SpO2 above 96% and end tidal carbon dioxide partial pressure between 33 and 38 mm Hg. A total of 20 pairs of readings between CNAP and IAP were recorded each minute for 20 min from induction.
Measurements of ABP from CNAP™ and invasive arterial line were analysed for correlation. Between-technique variability of two different methods of measuring the same parameter was evaluated by bias as recommended by Bland and Altman. Bias is the mean difference between CNAP and IAP, where by differences were calculated by subtracting CNAP and IAP values.
The Bias represents the systemic error between the two techniques, and standard deviation (SD) of bias represents the random error or variability between the two techniques. Bland Altman plots were constructed of systolic, diastolic and MAPs to enable visual observation of data for agreement between the two methods and to determine the 95% confidence limits (limits of agreement). In addition, folded empirical cumulative distribution plot (mountain plot) were also plotted. The advantage of the mountain plot is that it is easier to find the central 95% of the data and it is easier to estimate percentiles for large differences. If two monitors are unbiased with respect to each other, the mountain will be centered over zero. Long tails in the plot reflect large differences between the methods. All statistical analysis was conducted with the SPSS statistical programme (version 18.0) and MedCalc software version 12.2.1.
RESULTS
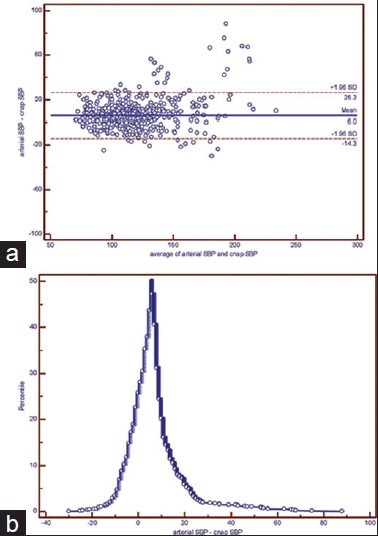
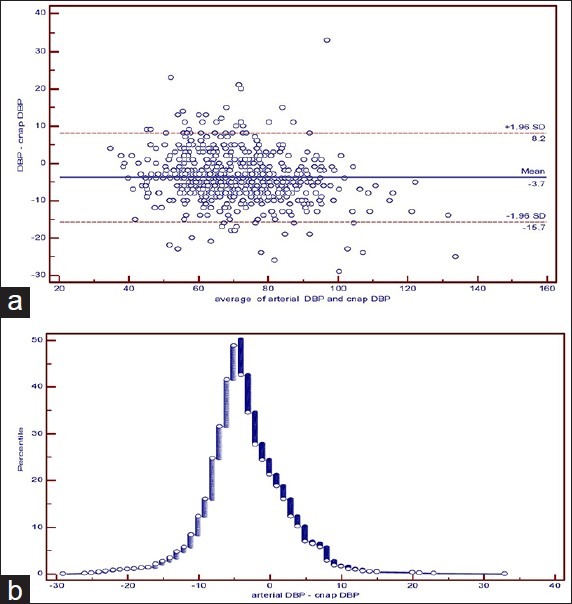
Sixty patients were enrolled in the study. Data from 36 males and 24 females were available for analysis. Twenty-four patients underwent coronary artery bypass grafting, 13 patients had mitral valve repair or replacement, eight patients had atrial septal defect closure, five patients had aortic valve replacement, four patients had double-valve replacement, three patients had Tetralogy of fallot repair, and three patients had ventricular septal defect closure. A total of 1200 paired data were obtained. 2.5% of the patients received a small finger cuff, while 81% received medium and 16.5% received large cuffs, respectively. The system set-up time of CNAP™ is defined as the time between the start of the CNAP™ device and the occurrence of the first valid CNAP™ beat took on an average of 5 min. The systolic ABP by CNAP™ was consistently lower than systolic IAP, and the CNAP™ diastolic ABP was consistently higher than diastolic IAP, yielding a systolic bias of 5.98 mm Hg and a diastolic bias of − 3.72 mm Hg. CNAP™ MAP values were almost close to the IAP mean ABP value, yielding a bias of − 0.02 mm Hg [Table 1]. Frequency of ABP pairs within the limits of agreement was 96.0%, 95.2% and 95.7% for systolic, diastolic, and MAP, respectively. Calculated limits of agreement were − 14.33 to 26.29, −15.68 to 8.23 and − 11.17 to 11.12 for systolic, diastolic and MAP, respectively [Table 1]. Bland Altman plot [Figures 1a, 2a and 3a] showed uniform distribution of the variances over all measured ABP values and a good agreement of ABP between CNAP™ and IAP values. Mountain plot that is generally used as complimentary to Bland Altman plot, also showed similar results [Figures 1b, 2b and 3b]. The median (bias, centre of the plot) between IAP and CNAP™ for systolic ABP was 6.000, for diastolic ABP was − 4.000 and for MAP was − 1.000. No significant differences in performance were present between measurements with different-sized finger cuffs.
Table 1.
Bias and limits of agreement between IAP and CNAP™ BP measurements
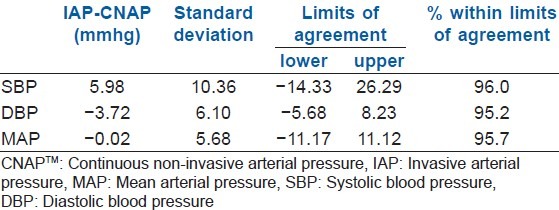
Figure 1.
(a) Bland Altman method and (b) Mountain plot method analysis of agreement between the continuous non-invasive arterial pressure device and invasive arterial pressure measurement of systolic blood pressure
Figure 2.
(a) Bland Altman method and (b) Mountain plot method analysis of agreement between the continuous non-invasive arterial pressure device and invasive arterial pressure measurement of diastolic blood pressure
Figure 3.
(a) Bland Altman method and (b) Mountain plot method analysis of agreement between the continuous non-invasive arterial pressure device and invasive arterial pressure measurement of mean arterial pressure
DISCUSSION
We investigated whether CNAP values were comparable with IAP readings during induction of general anaesthesia for different types of cardiac surgical procedures. The time for obtaining the first valid CNAP measurement was comparable with the time for obtaining the first IAP measurement.
In clinical practice, a new monitoring technique is acceptable for clinical use if both the applicability and the performance are comparable with those of an established method. The intraarterial measurement of ABP from radial or femoral artery has been the method of choice when continuous ABP monitoring during predictable haemodynamic instability is required. Nevertheless, given the fact that CNAP™ is a reliable device to assess the ABP continuously, there is a wide range of possible clinical applications.
The currently available recommendations for evaluation of the accuracy of non-invasive ABP monitoring devices consider the mean difference and the SD of differences between the test and the reference method,[6] or express agreement in terms of percentage of differences that decrease within certain thresholds. Because CNAP™ provides reconstructed brachial ABP, and the invasive ABP measurements were performed in the radial artery, the observed bias may be explained by the inherent physiological difference between brachial and radial artery ABP. The systolic ABP in the radial artery increases as a result of wave reflection, whereas the diastolic ABP decreases due to resistance to flow, which is reflected by the systolic and diastolic bias of our study [Table 1]. This systematic bias is also considered by the Food and Drug Administration-standard for intermittent oscillometric sphygmomanometers in a metaanalysis that reported absolute differences of 0.68–13.4 and 0.8–18 mm Hg for systolic and diastolic ABP, respectively.[6] The observed bias of 5.98 and − 3.72 mm Hg for systolic and diastolic ABP with this investigation lie within these ranges. Median values of 6.00 mm Hg of systolic ABP and − 4 mm Hg of diastolic ABP obtained from mountain plot also lie within the above-mentioned ranges. Furthermore, the observed bias for diastolic and mean ABP lies within the range of ± 5 mm Hg with a SD < 8 mm Hg for clinically acceptable agreement as recommended by the Association for the Advancement of Medical Instrumentation ANSI/AAMI SP10.
We observed that in 4 cases with severe aortic regurgitation (AR), wide pulse pressure and uncontrolled hypertension (HTN) pre-operatively, CNAP values did not correlate well with IAP values. Some values outside the limits of agreement could be due to some of the values of these patients. Based on such clinically acceptable bias between mean ABP values seen between CNAP™ and invasive ABP, we can advocate the use of CNAP™ during induction of GA in cardiac surgical patients.
Currently, commercially available devices for continuous non-invasive ABP measurement are based on arterial tonometry and on the volume clamp method (Finapres®). To obtain accurate pressure values by tonometry, it is important to find the optimal position over the artery to apply the sensor.[7,8] Finapress was shown in many studies as unreliable reflection of invasive ABP in anaesthetized adults that may have been caused by an increase in venous blood volume distal to the finger cuff and by rapid contractions and dilatations of finger arteries in relation to psychological, physical, and chemical stress. In order to reduce these limitations, the CNAP™ device switches repeatedly between two adjacent finger cuffs that are controlled by concentrically interlocking loops for rapid detection of blood flow oscillation.[9]
From clinically acceptable bias between CNAP and IAP, we can recommend use of CNAP monitor for induction of GA or in regional anaesthesia of cardiac patients coming for non cardiac surgeries, in cardiac catheterisation procedures, difficult radial artery cannulation, radial artery harvesting, patients with positive Allen's test, patients with radial artery grafts used for coronary revascularisation in the past coming for procedures where continuous BP monitoring is required.
The possible limitations of our study could be the choice of radial artery as a reference for IAP measurement. At our institution, continuous ABP monitoring during induction of general anaesthesia for cardiac surgical patients is usually performed by an intra-arterial catheter inserted into the left or right radial artery. CNAP measurements represent ABP at the brachial artery because of the calibration with upper-arm oscillometric measurements. Although the comparison between CNAP and IAP in the brachial artery would have been more close to an ideal study design, we decided not to perform the IAP measurements at this site because of the complications associated with brachial artery puncture. We did not continue CNAP and IAP comparison intra-operatively. Further studies are required to compare the accuracy between them intra-operatively and on cardiopulmonary bypass. In some cases with severe AR and uncontrolled HTN, CNAP values could not correlate with IAP values. The probable reasons could be wide pulse pressure and technical problems in the CNAP monitor in severe AR and significant pressure variation in uncontrolled HTN cases. Since we did not conduct adequate AR cases, we were not able to conclude on the difference between IAP and CNAP values and we recommend further studies in these severe AR cases.
CONCLUSION
The systolic, diastolic, and mean CNAP measurements were not statistically equivalent to simultaneous IAP values. The observed ABP differences between methods could be explained by physiological differences between radial and brachial measurements.
DISCUSSION
The bias for mean ABP and diastolic ABP between CNAP and IAP fall within the recommended, clinically acceptable range. Hence, we recommend CNAP monitor for induction of GA in patients undergoing different types of cardiac surgeries.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Scheer B, Perel A, Pfeiffer UJ. Clinical review: Complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002;6:199–204. doi: 10.1186/cc1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Siebig S, Rockmann F, Sabel K, Zuber-Jerger I, Dierkes C, Brünnler T, et al. Continuous non-invasive arterial pressure technique improves patient monitoring during interventional endoscopy. Int J Med Sci. 2009;6:37–42. doi: 10.7150/ijms.6.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanss R, Ilies C, Missala H, Steinfath M, Bein B. Continuous noninvasive blood pressure monitoring during spinal anesthesia for caesarean section. Eur J Anaesthesiol. 2010;27:166–7. [Google Scholar]
- 4.Jeleazcov C, Krajinovic L, Münster T, Birkholz T, Fried R, Schüttler J, et al. Precision and accuracy of a new device (CNAPTM) for continuous non-invasive arterial pressure monitoring: Assessment during general anaesthesia. Br J Anaesth. 2010;105:264–72. doi: 10.1093/bja/aeq143. [DOI] [PubMed] [Google Scholar]
- 5.Jagadeesh AM, Singh NG, Mahankali S. A comparison of a continuous noninvasive arterial pressure (CNAP™) monitor with an invasive arterial blood pressure monitor in the cardiac surgical ICU. Ann Card Anaesth. 2012;15:180–4. doi: 10.4103/0971-9784.97973. [DOI] [PubMed] [Google Scholar]
- 6.ANSI/AAMI. American National Standard for Manual, Electronic, or Automated Sphygmomanometers. Arlington, VA: Association for the Advancement of Medical Instrumentation; 2002. [Google Scholar]
- 7.Szmuk P, Pivalizza E, Warters RD, Ezri T, Gebhard R. An evaluation of the T-Line Tensymeter continuous noninvasive blood pressure device during induced hypotension. Anaesthesia. 2008;63:307–12. doi: 10.1111/j.1365-2044.2007.05369.x. [DOI] [PubMed] [Google Scholar]
- 8.Janelle GM, Gravenstein N. An accuracy evaluation of the T-Line Tensymeter (continuous noninvasive blood pressure management device) versus conventional invasive radial artery monitoring in surgical patients. Anesth Analg. 2006;102:484–90. doi: 10.1213/01.ane.0000194873.52453.bd. [DOI] [PubMed] [Google Scholar]
- 9.Fortin J, Marte W, Grüllenberger R, Hacker A, Habenbacher W, Heller A, et al. Continuous non-invasive blood pressure monitoring using concentrically interlocking control loops. Comput Biol Med. 2006;36:941–57. doi: 10.1016/j.compbiomed.2005.04.003. [DOI] [PubMed] [Google Scholar]


