Abstract
Background:
We aimed to develop and validate the Persian version of Short Form McGill Pain Questionnaire-2 (SF-MPQ-2) in patients with knee osteoarthritis.
Methods:
Translation and back translation was performed using Beaton's guideline. After a consensus has achieved on the Persian version of SF-MPQ-2, it was administered to 30 patients with knee osteoarthritis in a pilot study. Then, we enrolled 100 patients with knee osteoarthritis to fill the final SF-MPQ-2 as well as SF-36 and WOMAC questionnaires. Forty-three patients returned 3 days after the initial visit to fill the Persian SF-MPQ-2 for the second time. Construct validity was tested by Pearson's correlation coefficient between subscales of SF-MPQ-2 and subscales of SF-36 and WOMAC. Internal consistency for total and subscales was calculated by Cronbach's alpha and reliability between test retest was performed using Intraclass correlation coefficient (ICC).
Results:
ICC for subscales of SF-MPQ-2 ranged from 0.73 to 0.90. The ICC for total SF-MPQ-2 was 0.90. Cronbach's alpha for subscales was 0.65-0.74 at the first visit and 0.58-0.81 at the second visit. Cronbach's alpha for the total questionnaire was 0.88 and 0.91 at the first and second visit, respectively. Pearson's correlation coefficient was highly significant when comparing subscales specifically with WOMAC (r=-0.47 to -0.61; P<0.001). Interscale correlation between subscales of SF-MPQ-2 was significant as well (r: 0.43-0.88, P<0.001).
Conclusions:
Persian SF-MPQ-2 showed excellent reliability and good to excellent internal consistency throughout the questionnaire. It is a valid and reliable instrument for measuring the pain intensity and applicable in osteoarthritic pain assessment.
Key words: Persian, Psychometric, Reliability, Short from McGill pain questionnaire, Validity
Introduction
McGill pain Questionnaire (MPQ) was developed in 1975 which was a time consuming tool (1). Thereafter, Short Form McGill Pain Questionnaire (SF-MPQ) was developed in 1987 with 15 descriptors consisting of 11 sensory and 4 affective which are rated from 0= none to 3= severe (2). Dworkin et al expanded the SF-MPQ in 2009 by adding relevant neuropathic symptoms and modification of rating from 0-10 (3). This version was tested on patients with chronic pain syndromes and painful diabetic neuropathy. Excellent validity and reliability was found for this new version, namely SF-MPQ-2 (3).
The assessment of neuropathic pain plays an important role in its measure, treatment and follow-up. MPQ and SF-MPQ were defective in distinguishing neuropathic from non-neuropathic pain which limits their use for whole spectrum of pain. Moreover, SF-MPQ items are rated based on a 4-point scale which limits its ability in contrast to an 11-point numeric rating scale to detect small changes (3).
The primary objective of this study is to adapt and validate the Persian version of SF-MPQ-2 which can be used in studies of neuropathic and non-neuropathic pain conditions, treatment response and follow-up evaluation.
Materials and Methods:
Patients
We enrolled 100 consecutive patients from the Knee Clinic in 2012 [Table 1]. Inclusion criteria were age above 20 years, knee pain due to osteoarthritis for more than 6 month, alert with no cognitive disorder, without underlying systemic disease or dementia and being a native Persian speaker. We confirmed knee osteoarthritis by standing AP radiography of the knees. The Internal Review Board (IRB) of the university has approved the protocol. Patients were asked to fill the consent form prior to enrolling.
Table 1.
Characteristics of patients with knee osteoarthritis (N=100)
| Age, mean (SD) | 53± 11 |
| Sex, no (%) | |
| Male | 20 (20) |
| Female | 80 (80) |
| Education, no (%) | |
| Illiterate | 36 (36) |
| School | 41 (41) |
| Undergraduate | 15 (15) |
| Graduate | 8 (8) |
| Affected side, no. (%) | |
| Right | 24 (24) |
| Left | 33 (33) |
| Bilateral | 43 (43) |
| WOMAC, mean (SD) | 44±18 |
| PCS, mean (SD) | 34±8.5 |
| MCS, mean (SD) | 43±10 |
| SF-MPQ-2, mean (SD) | 4.6±2.0 |
WOMAC=Western Ontario and McMaster Universities Arthritis Index, PCS=Physical Component Summary, MCS=Mental Component Summary, SD=Standard Deviation
At the first visit (T1), we asked patients to fill the Persian version of the SF-MPQ-2 along with the Western Ontario and McMaster Universities Arthritis Index (WOMAC) and Medical Outcome Study 36-Item Short Form Health Survey (SF-36) which has been tested for reliability and validity in Persian speaking population. The second visit (T2) was planned 3 days after the initial visit and patients were asked to fill the Persian version of SF-MPQ-2 as a retest. Patients were convenient with 3-day interval visits. Also, none of the patients received serious or aggressive intervention which alters the disease course during the 3-day interval. Forty-three patients returned and filled the SF-MPQ-2 for the second time after 3 days from the initial visit. Literate patients filled the form individually; however, a literate family member to help fill the questionnaire often accompanied illiterate patients. In case an illiterate patient has presented to the clinic alone, the researcher has taken the responsibility to read.
Short form McGill Pain Questionnaire 2 (SF-MPQ-2)
This questionnaire is used to measure the quality as well as the intensity of pain (3). It is not only measuring neuropathic pain, but it is developed to measure both neuropathic and non-neuropathic pain. It consists of 22 different descriptors of pain and each item is rated based on a 0-10 scale with 0 equal to no pain and 10 equal to the worst pain ever during the past week. The total score is calculated by summing 22 individual scores. SF-MPQ-2 comprises of 4 parts including Continuous (throbbing pain, cramping pain, gnawing pain, aching pain, heavy pain, tender), Intermittent (shooting pain, stabbing pain, sharp pain, splitting pain, electric-shock pain, piercing), Neuropathic (hot-burning pain, cold-freezing pain, pain caused by light touch, itching, tingling or "pins and needles", numbness), and Affective (tiring-exhausting, sickening, fearful, punishing-cruel) subscales.
Translation
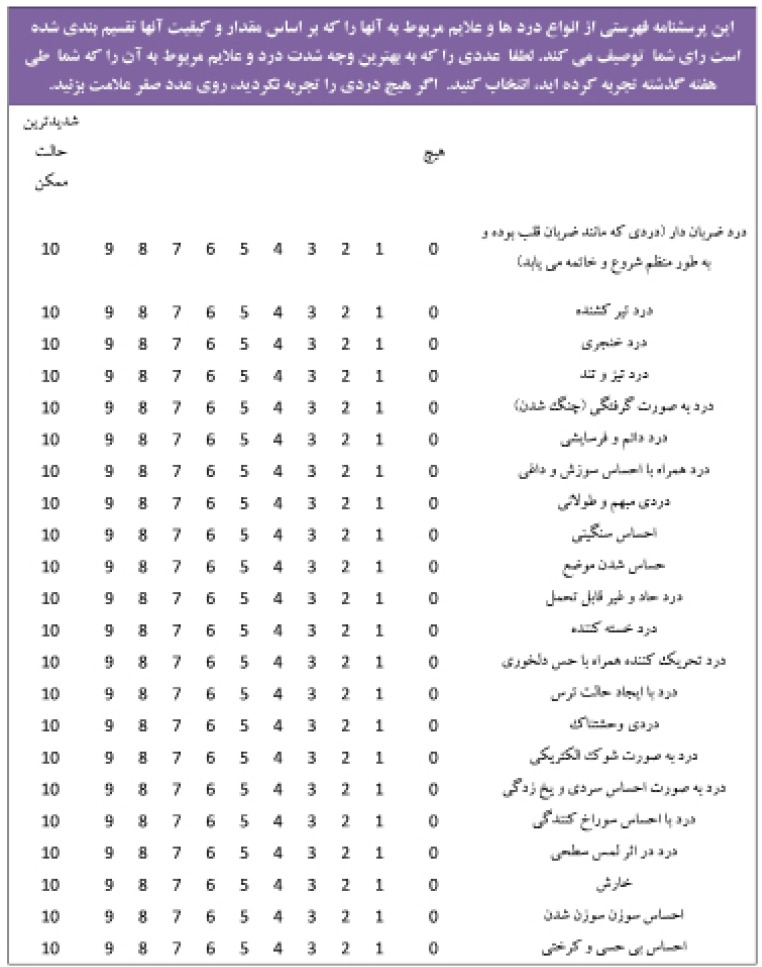
We applied Beaton's Guideline for cultural adaptation of the translated questionnaires (4). Two Iranian orthopedic surgeons and an independent professional interpreter, whose mother tongue is Persian, translated the English version of SF-MPQ-2 into Persian. In a meeting, a uniform version of the Persian translation for the SF-MPQ-2 was produced with an attempt to consider the cultural issues. We sent this Persian translated draft to an English-Persian translator, whose mother tongue is American English, to back translate the Persian version to English. She was not aware of the study details and had not seen the original English transcript of Sf-MPQ-2. In a second meeting, we compared the original English version and backward translated transcript. There was not a remarkable difference between the two. Finally, consensus was reached for the final version of the Persian SF-MPQ-2 [Figure 1].
Figure 1.
Persian version of the Short Form McGill Pain Questionnaire-2 (SF-MPQ-2).
In a pilot study, for face validity, the final version of SF-MPQ-2 was administered to 30 patients with knee osteoarthritis. Items 1 (Throbbing pain) and 5 (Cramping pain) were somewhat vague in meaning for patients. Therefore, we added a brief explanation after the Persian equivalent. This study showed that the applied words and phrases were understandable for patients with no necessity to be described.
Medical Outcome Study 36-Item Short Form Health Survey (SF-36)
The SF-36 is a generic, short-form health survey with only 36 questions that includes an 8-scale profile of functional health and well-being scores as well as psychometrically-based physical and mental health summary measures. The SF-36 has proven useful in surveys of general and specific populations, comparing the relative burden of diseases, and in differentiating the health benefits produced by a wide range of different treatments. Among the most frequently used conditions are chronic musculoskeletal conditions including osteoarthritis, back pain, and knee and shoulder disorders. Moreover, its validity and reliability has been documented in many countries including Iran (5).
Western Ontario and McMaster Universities Arthritis Index (WOMAC)
WOMAC is a self-administered questionnaire developed to evaluate patients with knee osteoarthritis. It consists of five items for pain (score from 0-20), two items for stiffness (score from 0 to 8), and 17 items for functional limitation (score from 0-68). It takes about 12 minutes. Persian version of WOMAC has been developed after testing for reliability and validity (6).
Psychometric analysis
Construct validity
Convergent validity is testing the ratio of correlation between a new measure and other related measures which are supposed to be correlated in a same field (7). In this study, we have used the already approved valid Persian SF-36 survey and WOMAC to test the validity of the SF-MPQ-2. We assessed the convergent validity by calculating the Pearson correlation coefficient between SF-MPQ-2 and SF-36 and WOMAC.
Reliability
Reliability refers to the consistency of a measure; hence, a test is considered reliable if we could get the same result repeatedly (8). Intraclass correlation coefficient (ICC) was measured to show how strongly test and retest resemble each other. This type of reliability assumes that there will be no change in the quality or construct being measured across time. For this purpose we asked 43 participants to fill out the Persian SF-MPQ-2 three days after the first study visit. ICC is confined to the interval between -1 and +1.
Internal consistency
Internal consistency is a part of reliability testing that tests the consistency of the ratings across items in a same measure (9). In other words, we are comparing question items that measure the same construct to determine that the tests are internally consistent. Internal consistency was tested by means of the Cronbach's alpha coefficient that calculates the internal correlations of all the items on the same scale. The Cronbach's alpha coefficient indirectly evaluates the extent to which all of the 22 questions of the SF-MPQ-2 measure the same construct. A high Cronbach's alpha coefficient (range from 0 to 1) indicates more consistency. A commonly accepted values of Cronbach's alpha for description of internal consistency is considered excellent for α ≥ 0.9, good for 0.7≥ α ≥0.9, acceptable for 0.6≥ α ≥0.7, poor for 0.5≥ α ≥0.6 and unacceptable for α <0.5.
Results
Forty-three patients out of 100 returned for the retest [Table 1]. Intraclass correlation coefficient (ICC) for 22 individually tested items was highly correlated between test and retest except item 18 (Piercing) that was not significantly correlated [Table 2]. ICC for subscales of SF-MPQ-2 showed a good to excellent reliability between test and retest [Table 3]. The ICC for total SF-MPQ-2 showed an excellent reliability throughout the questionnaire [Table 3].
Table 2.
Intraclass correlation coefficient between test-retest of Short Form McGill Pain Questionnaire-2
| Item | Domain | Original SF-MPQ-2 | Mean | SD | ICC | 95% CI | P value |
|---|---|---|---|---|---|---|---|
| 1 | Continuous | Throbbing pain | 3.1 | 3.4 | 0.86 | 0.74-0.93 | <0.001 |
| 2 | Intermittent | Shooting pain | 6.8 | 3.2 | 0.67 | 0.39-0.82 | <0.001 |
| 3 | Intermittent | Stabbing pain | 2.4 | 3.8 | 0.75 | 0.54-0.87 | <0.001 |
| 4 | Intermittent | Sharp pain | 5.7 | 3.7 | 0.81 | 0.65-0.90 | <0.001 |
| 5 | Continuous | Cramping pain | 5.0 | 4.0 | 0.74 | 0.56-0.87 | <0.001 |
| 6 | Continuous | Gnawing pain | 6.5 | 3.6 | 0.86 | 0.74-0.92 | <0.001 |
| 7 | Neuropathic | Hot-burning pain | 4.9 | 3.9 | 0.77 | 0.58-0.88 | <0.001 |
| 8 | Continuous | Aching pain | 4.7 | 4.1 | 0.71 | 0.47-0.84 | <0.001 |
| 9 | Continuous | Heavy pain | 4.8 | 4.2 | 0.78 | 0.59-0.88 | <0.001 |
| 10 | Continuous | Tender | 4.2 | 4.1 | 0.88 | 0.77-0.93 | <0.001 |
| 11 | Intermittent | Splitting pain | 6.1 | 3.5 | 0.81 | 0.65-0.90 | <0.001 |
| 12 | Affective | Tiring-exhausting | 7.2 | 3.3 | 0.81 | 0.65-0.90 | <0.001 |
| 13 | Affective | Sickening | 7.2 | 3.3 | 0.67 | 0.39-0.82 | <0.001 |
| 14 | Affective | Fearful | 4.1 | 4.2 | 0.59 | 0.23-0.78 | 0.0030 |
| 15 | Affective | Punishing-cruel | 4.7 | 4.1 | 0.60 | 0.26-0.78 | 0.0020 |
| 16 | Intermittent | Electric-shock pain | 2.4 | 3.4 | 0.55 | 0.17-0.76 | 0.0060 |
| 17 | Neuropathic | Cold-freezing pain | 4.1 | 4.1 | 0.84 | 0.71-0.91 | <0.001 |
| 18 | Intermittent | Piercing | 2.2 | 3.4 | 0.30 | (-0.27)-0.62 | 0.12 |
| 19 | Neuropathic | Pain caused by light touch | 4.4 | 3.8 | 0.65 | 0.36-0.81 | <0.001 |
| 20 | Neuropathic | Itching | 1.9 | 3.1 | 0.75 | 0.54-0.87 | <0.001 |
| 21 | Neuropathic | Tingling or 'pins and needles' | 4.2 | 4.0 | 0.64 | 0.33-0.81 | 0.0010 |
| 22 | Neuropathic | Numbness | 4.4 | 4.0 | 0.86 | 0.73-0.92 | <0.001 |
SD=Standard Deviation, ICC=Intraclass Correlation Coefficient, CI=Confidence Interval
Table 3.
Internal consistency and test-retest reliability of the Persian version of the Short Form McGill Pain Questionnaire-2
| Subscale | Number of Items | Item number | T1 (N=100) mean±SD | T2 (N=43) mean±SD | Cronbach's alpha (T1, T2) | (Intraclass Correlation Coefficient) | ||
|---|---|---|---|---|---|---|---|---|
| ICC | 95% CI | P value | ||||||
| Continuous | 6 | 1, 5, 6, 8, 9, 10 | 4.7±2.4 | 4.5±2.5 | 0.65, 0.75 | 0.90 | 0.82-0.95 | <0.001 |
| Intermittent | 6 | 2, 3, 4, 11, 16, 18 | 4.3±2.3 | 3.3±2.4 | 0.74, 0.81 | 0.87 | 0.75-0.93 | <0.001 |
| Neuropathic | 6 | 7, 17, 19, 20, 21, 22 | 4.0±2.4 | 3.5±2.1 | 0.70, 0.58 | 0.89 | 0.80-0.94 | <0.001 |
| Affective | 4 | 12, 13, 14, 15 | 5.8±2.8 | 5.0±3.0 | 0.73, 0.81 | 0.73 | 0.50-0.85 | <0.001 |
| Total | 22 | 4.6±2.0 | 4.0±2.1 | 0.88, 0.91 | 0.90 | 0.81-0.94 | <0.001 | |
T1=Test, T2=Retest, SD=Standard Deviation, ICC=Intraclass Correlation Coefficient, CI=Confidence Interval
Cronbach's alpha showed good and excellent internal consistency for the total SF-MPQ-2 at the first and second visit, respectively [Table 3].
Construct validity was confirmed by showing convergent validity between subscales of SF-MPQ-2 and WOMAC and SF-36. Pearson correlation coefficient was above 0.4 when comparing subscales with WOMAC which is a specific measure for knee osteoarthritis rather than the general health measure of SF-36 [Table 4]. Given the direction of WOMAC and SF-36 are reverse in relation with SF-MPQ-2, correlation coefficients are mostly negative. Interscale correlation between subscales of SF-MPQ-2 was highly significant as well, which further confirmed the construct validity [Table 5].
Table 4.
Convergent validity expressed by Spearman's correlation (r) between subscales of Persian SF-MPQ-2 and WOMAC and SF-36 (N=100)
| WOMAC | PF | RP | BP | GH | VT | SF | RE | MH | PCS | MCS | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Continuous pain | (-0.52)** | (-0.30)** | (-0.23)* | (-0.49)** | (-0.33)** | (-0.26)** | 0.12 | (-0.35)** | (-0.39)** | (-0.30)** | (-0.33)** |
| Intermittent pain | (-0.52)** | (-0.31)** | -0.093 | (-0.46)** | (-0.32)** | (-0.30)** | 0.12 | (-0.31)** | (-0.44)** | (-0.21)* | (-0.38)** |
| Neuropathic pain | (-0.47)** | (-0.42)** | (-0.21)* | (-0.43)** | (-0.29)** | (-0.27)** | 0.28** | (-0.27)** | (-0.29)** | (-0.38)** | -0.16 |
| Affective | (-0.52)** | (-0.35)** | (-0.27)** | (-0.49)** | (-0.23)* | (-0.37)** | 0.21* | (-0.41)** | (-0.48)** | (-0.26)* | (-0.42)** |
| Total SF-MPQ-2 | (-0.61)** | (-0.42)** | (-0.24)* | (-0.56)** | (-0.36)** | (-0.35)** | 0.22* | (-0.40)** | (-0.47)** | (-0.35)** | (-0.38)** |
PF=Physical Functioning, RP=Role-Physical, BP=Bodily Pain, GH=General Health, VT=Vitality, SF=Social Functioning, RE=Role Emotional, MH=Mental Health, PCS=Physical Component Summary, MCS=Mental Component Summary
Correlation is significant at the 0.05 level (2-tailed)
Correlation is significant at the 0.01 level (2-tailed)
Table 5.
The SF-MPQ-2 interscale correlation
| Continuous | Intermittent | Neuropathic | |
|---|---|---|---|
| Intermittent | 0.66* | - | |
| Neuropathic | 0.61* | 0.56* | - |
| Affective | 0.64* | 0.60* | 0.43* |
Correlation is significant at the 0.01 level (two-tailed)
Discussion
In this study, we aimed to develop and validate the Persian version of SF-MPQ-2 that can be used in studies of neuropathic and non-neuropathic pain conditions.
During the study, we enrolled many illiterate patients with which we managed this problem by asking the accompanying family member or the available researcher to help them reading the questions. The taken time for filling the questionnaire was more than anticipated because knee osteoarthritis is more common in older population besides more illiteracy in this patient cohort.
The thorough questionnaire showed excellent reliability and good to excellent internal consistency. In patients with knee osteoarthritis (OA), neuropathic pain and affective subscale had the lowest and highest average scores, respectively, confirming more pain of non-neuropathic nature in OA. Higher scores in SF-36 and WOMAC represent better self-perceived health. The direction in SF-MPQ-2 is reverse in which the higher scores represent more severe pain. Therefore, the correlation between these forms demonstrated a negative correlation. There was a positive correlation only between social functioning (SF) and subscales of pain. SF domain comprise of 2 questions regarding the extent and frequency of emotional problem interfering with social activities. We can assume that patients with knee OA accepted this phenomenon as aging and adapted to the wax and wane pain over the time. On the other hand they may not see this problem as an emotional distress to interfere with their activities.
In individual item ICC calculation, Piercing pain, as a neuropathic pain descriptor, was not significantly correlated between test and retest in spite of 30% correlation. Furthermore, given ICC to neuropathic subscale was the lowest among all. We can assume that because OA is majorly presenting with non-neuropathic pain, patients may be confused and not sure about the nature of neuropathic pain descriptors. Thus, their answers may not be reliable because of uncertainty.
Validation and culturally adaptation of the SF-MPQ-2 has been rarely attempted in the other languages. Adelmanesh et al have developed and validated the Persian version of I-SF-MPQ in 2011on patients with chronic pain (10). The calculated Cronbach's alpha and ICC for total pain score was 0.84 and 0.91, respectively. Thereafter, they validated the Persian version of SF-MPQ-2 in 2012 in patients with neuropathic and non-neuropathic pain (11). They showed high reliability with Cronbach's alpha equal to 0.90 and ICC of 0.94. Other studies have extended the application of the original SF-MPQ-2 in which they further supported the reliability and validity of this instrument (12). In a study to validate SF-MPQ-2 in young and old patients with cancer pain, Cronbach's alpha was equal to 0.89 and 0.93 in young and old patients' cohorts, respectively, which confirmed its appropriateness throughout the life span (13).
Validity and reliability of SF-MPQ-2 has been tested in neuropathic and non-neuropathic pain so far (11, 13). However, there are more to be evaluated and validated in term of chronicity, type of disease, and involvement pattern as well as pre- and post-treatment follow-up investigations.
The Persian version of SF-MPQ-2 proved to be acceptable in face validity among Persian speaking population.
References
- 1. Melzack R. The McGill Pain Questionnaire: major properties and scoring methods. Pain. 1975;1:277–99. doi: 10.1016/0304-3959(75)90044-5. [DOI] [PubMed] [Google Scholar]
- 2. Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 3. Dworkin RH, Turk DC, Revicki DA, Harding G, Coyne KS, Peirce-Sandner S, et al. Development and initial validation of an expanded and revised version of the Short-form McGill Pain Questionnaire (SF-MPQ-2) Pain. 2009;144:35–42. doi: 10.1016/j.pain.2009.02.007. [DOI] [PubMed] [Google Scholar]
- 4. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–32. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 5. Motamed N, Ayatollahi AR, Zare N, Sadeghi-Hassanabadi A. Validity and reliability of the Persian translation of the SF-36 version 2 questionnaire. East Mediterr Health J. 2005;11:349–57. [PubMed] [Google Scholar]
- 6. Nadrian H, Moghimi N, Nadrian E, Moradzadeh R, Bahmanpour K, Iranpour A, et al. Validity and reliability of the Persian versions of WOMAC Osteoarthritis Index and Lequesne Algofunctional Index. Clin Rheumatol. 2012;31:1097–102. doi: 10.1007/s10067-012-1983-7. [DOI] [PubMed] [Google Scholar]
- 7. Smith EV. Evidence for the reliability of measures and validity of measure interpretation: a Rasch measurement perspective. J Appl Meas. 2001;2:281–311. [PubMed] [Google Scholar]
- 8. Koch GG. Intraclass correlation coefficient. In: Kotz S, Johnson NL, editors. Encyclopedia of Statistical Sciences. 4th ed. New York: John Wiley & Sons; 1982. pp. 213–7. [Google Scholar]
- 9. Kline P. The handbook of psychological testing. 2nd ed. London: Routledge; 2000. 13 pp. [Google Scholar]
- 10. Adelmanesh F, Arvantaj A, Rashki H, Ketabchi S, Montazeri A, Raissi G. Results from the translation and adaptation of the Iranian Short-Form McGill Pain Questionnaire (I-SF-MPQ): preliminary evidence of its reliability, construct validity and sensitivity in an Iranian pain population. Sports Med Arthrosc Rehabil Ther Technol. 2011;3:27. doi: 10.1186/1758-2555-3-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adelmanesh F, Jalali A, Attarian H, Farahani B, Ketabchi SM, Arvantaj A, et al. Reliability validity, and sensitivity measures of expanded and revised version of the short-form McGill Pain Questionnaire (SF-MPQ-2) in Iranian patients with neuropathic and non-neuropathic pain. Pain Med. 2012;13:1631–6. doi: 10.1111/j.1526-4637.2012.01517.x. [DOI] [PubMed] [Google Scholar]
- 12. Lovejoy TI, Turk DC, Morasco BJ. Evaluation of the psychometric properties of the revised short-form McGill Pain Questionnaire. J Pain. 2012;13:1250–7. doi: 10.1016/j.jpain.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gauthier LR, Young A, Dworkin RH, Rodin G, Zimmermann C, Warr D, et al. Validation of the Short-Form McGill Pain Questionnaire-2 in Younger and Older People with Cancer Pain. J Pain. 2014;15(7):756–70. doi: 10.1016/j.jpain.2014.04.004. [DOI] [PubMed] [Google Scholar]