Abstract
The aim of this study was to pilot test in a minority cancer patient population a communication workshop to improve doctor-patient communication skills. Thirty-two patients participated. Eighteen evaluated a face-to-face workshop, while 14 completed surveys only. Participants in the workshop group completed the Patient Report of Communication Behavior (PRCB) before and after the workshop and a course evaluation. Participants did not differ on baseline PRCB scores. Post-test scores were significantly higher than pre-test scores (p<.01). All participants agreed or strongly agreed that they would use the communication skills; 93% agreed or strongly agreed that the skills would improve their healthcare.
Keywords: oncology, communication skills training, patient education, minority patients
Introduction
Research has indicated that African-American and other minority patient populations receive differential and suboptimal health care (Smedley, 2003). As noted by Cooper-Patrick and colleagues (Cooper-Patrick et al., 1999), observed racial differences in healthcare are explained only partially by socioeconomic status and health insurance coverage. Differences in interpersonal aspects of care, such as clinician-patient communication, may contribute to such disparities across a wide range of conditions.
Minority patients perceive their visits as less participatory than White patients (Kaplan, Gandek, Greenfield, Rogers, & Ware, 1995) especially when encountering race-discordant consultations (Cooper-Patrick, et al., 1999). Racial and ethnic minorities endorse more negative ratings of the quality of interpersonal care received from healthcare professionals (Collins et al., 2002). Observational studies have shown that physicians are more verbally dominant and engage in less patient-centered communication with African-American patients, and further, that both African-American patients and their physicians display lower levels of positive affect during visits (Johnson, Roter, Powe, & Cooper, 2004). In addition, self-perceived communication skills within medical interactions among minority patient populations are lower than those reported by their ethnic majority counterparts (Bylund, D'Agostino, Ho, & Chewning, 2010).
Clinician-patient communication barriers may culminate from the influence of various factors, including: cultural, racial or linguistic incongruity between the clinician and patient (Cooper-Patrick, et al., 1999; Cooper et al., 2003; Hutching, Lac, & LaBrie, 2008; Saha, Komaromy, Koepsell, & Bindman, 1999), medical mistrust and health fatalism on the part of minority patients (Medicine, 2003), clinician bias (Cooper et al., 2009; Medicine, 2003), racial discrimination and lack of cultural competency (Beach et al., 2005), or possibly a lack of effective communication skills among either patients or physicians.
Efforts proposed to improve health disparities often focus on the clinician, such as improving physicians’ ability to provide culturally competent healthcare (Berlin & Fowkes, 1983; Smith et al., 2007) and results indicate such interventions are beneficial (Beach, et al., 2005). However, clinician-patient communication is a two-person process and attending to clinicians’ skills addresses only half of the clinical interaction.
Question prompt lists for patients have been shown to be useful techniques in improving patients’ question asking abilities and some patient outcomes (Brown, Butow, Boyer, & Tattersall, 1999; Shields et al., 2010). The work of Don Cegala and colleagues has gone beyond question asking to include other types of communication (e.g., giving information). Cegala's work has indicated that training patients to more effectively communicate with physicians significantly improves patient participation and health-related behaviors as well as impacting health care outcomes (Cegala, Marinelli, & Post, 2000; Cegala, McClure, Marinelli, & Post, 2000; Post, Cegala, & Marinelli, 2001). Further, the importance of tailoring communication interventions around patients’ individual needs and characteristics has been noted (Cegala & Lenzmeier Broz, 2003). For example, Post, Cegala, and Marinelli (Post, et al., 2001) explored racial differences in the impact of patient communication training. Across analyses, receipt of a communication skills workbook had a strong and significant effect on White patients, but minimal to no effect on African-American patients. The authors suggest that such findings may be explained by the fact that a workbook intervention involves minimal interpersonal contact, thus failing to address cultural factors.
The purpose of this study was to determine the acceptability and perceived usefulness of a face-to-face (rather than workbook) patient communication training intervention for minority cancer patients. Although patient communication skills training cannot solve many of the systemic problems faced by underserved and minority populations such as denial of or lack of access to care, this form of patient intervention can address ineffective care due to inadequate patient or clinician communication skills.
The conceptual framework used for this study is based upon the notion of ‘concordance’, or shared understanding, between clinician and patient (Bylund, D'Agostino, & Chewning, 2010; Bylund, D'Agostino, Ho, et al., 2010). The concept of concordance was first introduced in an effort to improve medication adherence and referred to a shared understanding between the patient and health care professional regarding whether, when, and how medications are to be taken (RPSGB, 1997). Rather than a one-way, often top-down transmission, the concordance framework can be viewed within a two-way transactional communication process (Shah & Chewning, 2006) reflecting patient responsibility for observation, self-reflection, and communication (Bylund, D'Agostino, Ho, et al., 2010). Concordance within a medical consultation involves each actor (i.e., patient and physician) sharing and exchanging rationale and expertise to reach mutual agreement and understanding. Our framework for the patient communication training intervention posits that concordance is necessary in six areas: the goals of the visit; the patient's illness experience; the patient's preference for information, involvement, and treatment; the information conveyed by the physician; the patient's values; and the next steps the patients should take. It is necessary for both patients and physicians to participate in achieving this concordance. Physician communication skills to achieve such concordance have been described in the literature (e.g.,(Brown & Bylund, 2008) but there has been less focus on patient communication skills.
As this intervention was focused on patient communication skills, we adapted Cegala and colleagues’ (Cegala, 2000) P.A.C.E. curriculum, which proposes four strategies to achieve effective physician-patient communication: Presenting Detailed Information relates to pre-visit preparation and patient's ability to give a focused and extensive breadth of information about symptoms, history, reasons for visit, needs, expectations, etc. Asking Questions pertains to having a preset list of questions prepared that will deepen or clarify patient understanding of any material (e.g., treatments, test, or diagnoses) that may be presented in the consultation. Checking Understanding refers to a form of information verification, and involves patient skills such as asking the clinician to repeat or clarify information, rehearsing information to improve retention, and summarizing information back to the clinician in order to check understanding. Finally, Expressing Concerns aims to bring forward any conflicts or concerns (e.g., religious or cultural beliefs) that may hinder treatment or the clinician-patient relationship. Through open expression of these concerns, a mutual effort of resolution or accommodation can be reached. With the goal of concordance in mind, we added a fifth component that contributes to the P.A.C.E. curriculum, training patients to State Preferences, if one is held, regarding communication, role in decision making, treatments, etc. (Bylund, D'Agostino, Ho, et al., 2010). This patient communication skill moves beyond noting concerns, allowing the patient to take an active role in shaping the dynamic of the physician-patient relationship and the flow of information.
Using this framework, the aims for this study were to: (1) test the acceptability of a face-to-face communication skills training intervention for patients at a minority-serving hospital; (2) examine differences between patients who agreed to participate in the communication skills training intervention and those who didn't; and (3) collect preliminary data on the perceived usefulness of the intervention.
Methods
Participants
A research study assistant (RSA) approached 140 consecutive cancer patients in the waiting room at Queens Cancer Center on six individual days. In order to be consented to the study, patients had to be 18 years or older, able to sign informed consent, and speak English. Family members could not consent to the study, but could accompany the patient to the workshop if desired. A large sign announcing the training workshop was on display in the waiting room. The research study and its procedures were approved by both the Memorial Sloan-Kettering Cancer Center and the Queens Cancer Center Institutional Review Boards.
Data Collection
The RSA first asked each patient if he or she was interested in participating in the communication training workshop. If the patient declined, the patient was asked if he or she would participate in a survey only version of the study that consisted of completing questionnaires. The rationale for the alternative of the survey only version was to allow for the assessment of differences between patients who consented to the workshop and those who did not. In other words, we wanted to see if patients’ perceptions of their own communication skills and their reported anxiety and depression impacted their decision to participate in the workshop. If the patient declined to participate in any part of the study, his or her reason for refusal was recorded.
Patients who consented to participate in the communication training workshop completed a baseline survey and then were directed to a small conference room, usually following their visit with their doctor. The first author led all of the workshops. Each workshop consisted of a 20-30 minute Power Point presentation, video clips demonstrating the skills taught in the workshop, and discussion about the skills taught. Following the workshop, patients completed a post-training survey. The content of the workshop was based upon the PACE system as discussed above. Patients who consented to participate in the survey only version of the study completed questionnaires at baseline.
Measures
The baseline survey, which both groups completed, consisted of two parts: (1) The Patient Report of Communication Behavior (PRCB). The PRCB is an 11-item Likert type scale that measures patients’ assessment of their competence in communicating with their doctors. There are two items for each of the five skills of the workshop curriculum (Presenting Clear Information, Asking Questions, Checking Understanding, Expressing Concerns, and Stating Preferences). In addition, there is one global item. Respondents are asked to rate the frequency with which they use each of these skills using a 5-point scale, ranging from never to always. This measure has demonstrated good internal reliability, with Cronbach's alpha = .93 and Guttman split-half = .90. (Bylund, D'Agostino, Ho, et al., 2010). The measure has also demonstrated preliminary concurrent validity as lower reports of behavior were more likely to be associated with a preference to participate in the communication skill training workshop (Bylund, D'Agostino, Ho, et al., 2010).
(2) The Hospital Anxiety and Depression Scale (HADS) (Snaith & Zigmond, 2000). The HADS consists of fourteen items, rated on a 4-point scale, with seven items contributing to an anxiety subscale and seven items contributing to a depression subscale. This scale has demonstrated internal reliability (Cronbach's alpha=.89), test-retest reliability (r=.72, p<.001) (Savard, Laberge, Gauthier, Ivers, & Bergeron, 1998), and concurrent validity (Bjelland, Dahl, Haug, & Neckelmann, 2002; Hopwood, Howell, & Maguire, 1991). Those who did not participate in the workshop also completed a demographic sheet at this time.
The post-training survey, completed only by those who participated in the workshop, had three parts: (1) The PRCB-Intention scale, a slightly modified version of the PRCB, focusing on patients’ intent for future use of communication skills; (2) a 7-item course evaluation; and (3) a demographic sheet.
Patients who consented to either portion gave permission for their medical charts to be reviewed by an RSA. Data was collected on the following: age, race/ethnicity, disease stage, disease recurrence, and time since diagnosis.
Analysis
Analyses were completed using descriptive statistics, Pearson's Chi-Square tests and paired t-tests. Immediately following the workshop, patients had not yet had time to demonstrate these behaviors. Thus, in order to obtain post-training comparison data, we compared scores of the baseline PRCB to scores of a behavioral intention version of the PRCB, as noted above, and so this was not a true pre-post test. Instead, we were comparing scores of patients’ reports of their regular behavior before participating in the study (pre-test) and their intentions for behavior after participating in the study (post-test). However, there is a good deal of evidence to support the relationship between behavioral intentions and future behaviors (Ajzen, 1991; Hutching, et al., 2008; Pai & Eddington, 2008) so this seemed to be a reasonable proxy.
There was little missing data. One patient completed only one item on the HADS; this was not used. Three patients had one item missing each. Because of the small sample size, we imputed average values for the two participants that had one item missing each on the PRCB and the one participant that had one item missing on the HADS. This allowed us to have a full set of data on the summed scores of the HADS subscales of anxiety and depression and PRCB and PRCB-I.
Results
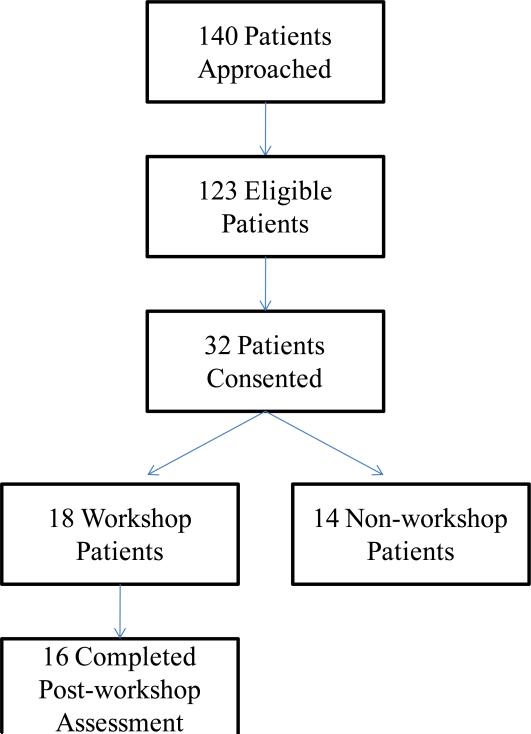
One hundred and forty patients were initially approached, with 123 meeting eligibility criteria, and 32 providing informed consent to participate in the study. This resulted in a 26% recruitment rate. (See Figure 1). The sex of the patient did not impact whether the patient consented to participate. The most frequent reasons given for refusal included: not interested (51%), no time (27%) and too tired (7%).
Figure 1.
Recruitment Diagram.
Study sample
Table 1 displays demographic information of the 32 patients who participated in the study. Participants’ average age was 53.8 years (SD=9.7). Participants were predominantly female and non-Caucasian, with 41% of patients African-American and 41% Asian. Sixty-six percent of participants had a diagnosis of breast cancer, while 19% had a type of gastrointestinal (GI) cancer (e.g., colon cancer, pancreatic cancer). Disease stage was mixed, with 53% of patients at Stage 2 or below, 25% at Stage 3, and 22% at Stage 4. The majority of patients (63%) were diagnosed more than one year before participating in the study. Eighteen patients consented to participate in the workshop and 14 patients consented to participate in the survey-only portion of the study.
Table 1.
Patient Demographics.
| n | % | |
|---|---|---|
| Age 53.8 (26-72) | ||
| 25-34 | 2 | 6.2 |
| 35-44 | 2 | 6.2 |
| 45-54 | 13 | 40.6 |
| 55-64 | 11 | 34.4 |
| ≥65 | 4 | 12.5 |
| Gender | ||
| Female | 28 | 87.5 |
| Male | 4 | 12.5 |
| Race | ||
| African American | 13 | 40.6 |
| Asian | 13 | 40.6 |
| Hispanic | 4 | 12.5 |
| Caucasian | 2 | 6.2 |
| Cancer Type | ||
| Breast | 21 | 65.6 |
| Gastrointestinal | 6 | 18.7 |
| Gynecological | 2 | 6.2 |
| Lymphoma | 1 | 3.1 |
| Prostate | 1 | 3.1 |
| Melanoma | 1 | 3.1 |
| Disease Stage | ||
| 0 | 3 | 9.3 |
| Stage I | 8 | 25 |
| Stage II | 6 | 18.7 |
| Stage III | 8 | 25 |
| Stage IV | 7 | 21.9 |
| Disease Recurrence | 1 | 3.1 |
| Time since diagnosis | ||
| <6 mos | 10 | 31.2 |
| 6 mos-1 yr. | 2 | 6.2 |
| 1-3 yrs. | 13 | 40.6 |
| 3-5 yrs. | 4 | 12.5 |
| >5 yrs. | 3 | 9.3 |
| Marital Status | ||
| Single | 12 | 37.5 |
| Married/Living with partner | 12 | 37.5 |
| Divorced/Separated | 4 | 12.5 |
| Widowed | 1 | 3.1 |
| Missing | 3 | 9.3 |
| Education | ||
| Junior high (8th grade) | 7 | 21.9 |
| Senior high (12th grade) | 9 | 28.1 |
| Technical degree | 4 | 12.5 |
| Undergraduate | 8 | 25 |
| Higher degree (post grad) | 2 | 6.2 |
| Missing | 2 | 6.2 |
To address the second aim, we examined differences between patients who participated in the workshop and patients who did not. There were no significant differences in terms of participant gender, race, time since diagnosis, cancer type or disease stage. However, patients who agreed to participate in the workshop were significantly older (x̄ =57.7 years) than those who did not (x̄=48.9 years). We also compared the two groups based upon their self-reported communication behaviors (using the PRCB) and their anxiety and depression (using the HADS). There were no significant differences between the two groups on their self-reported communication behaviors or on their depression or anxiety.
Workshop Results
Sixteen of the 18 study participants who consented to the workshop completed the workshop. The two who did not were unable to because of scheduling (both started the workshop, but then were called out by a clinic nurse for their appointment). Workshops were constructed as either one-on-one (n=9) or in small groups, with either two patients (n=6), or three patients (n=3).
Paired t-tests demonstrated significant increases in scores on the PRCB-I from the baseline PRCB (p<.01). The average score on the PRCB was 42.4 and the average score on the PRCB-I was 50.4, a difference of 8 points.
Participant evaluations of the course were generally positive. All participants agreed or strongly agreed that they would use the skills taught, and 93% agreed or strongly agreed that using the skills would improve their healthcare. Furthermore, 93% of participants agreed or strongly agreed that they would recommend the workshop to friends and family. Participants evaluated individual portions of the workshop. They were asked to rate the didactic portion, the videos, and the small group experience using an ordinal scale of “did not help me to learn,” “helped me to learn somewhat,” and “helped me to learn a lot.” Eighty-seven percent reported that the didactic and the videos helped them to learn a lot. Of those that did participate in a small group version of the workshop, 88% said that the small group experience helped them to learn a lot.
Discussion, Limitations and Future Work
One of the key issues for this study was if we could adequately recruit patients from clinic waiting rooms to participate in the study. Our recruitment rate of 26% was lower than that of other studies on patient communication training. However, in our experience, this was a reasonable recruitment rate for this patient population for several reasons. First, our recruitment rate is almost identical to a large, ongoing study at a primary care clinic at the same hospital using a similar approach to recruitment. Second, many of the patients do not speak English well and may have found the approach and recruitment process too difficult. Third, some of the patients who attend this center are non U.S. citizens and may be fearful of providing personal information. Finally, our recruitment approach may not have been ideal. Being approached by a new and unfamiliar research assistant may have not been comfortable for some patients. Future studies with this patient population may benefit from an initial approach about the study coming from the patient's doctor or other trusted health care worker.
Previous to this pilot study, we conducted a needs assessment of patients at this clinic using the PRCB. That PRCB scores in the needs assessment were lower than the baseline PRCB scores of the consented patients in the current study. This suggests that the refusers may have a greater need for the workshop than acceptors. The anonymous needs assessment had been deemed an exempt study, and did not require a lengthy consenting process thus, those who were willing to consent to the study reported here may have had already had better skills than those who were not willing to consent.
Comparing those who participated in the workshop with those who did not participate demonstrated that the groups were similar across disease characteristics, anxiety, depression, and reported communication behaviors. The only difference was that patients willing to participate in the workshop were older. It is important that workshop and survey-only participants did not differ significantly on their baseline PRCB scores, suggesting that perceived communication competence did not impact the decision to participate in the workshop.
One limitation of this work is that we had to rely on a measure of behavioral intentions (PRCB-I) in order to measure the effect of the workshop. Future studies should collect post-training data from patients to see if they implement these communication skills in their appointments with their doctors. In addition, we limited data collection for this study to patients (rather than family members) for simplicity and clarity in collecting pilot data. While family members were invited to attend each workshop, data was collected from patients only. Finally, time since diagnosis varied widely among our patient population. Future work may focus on cancer patients who have been recently diagnosed.
The results of this study provide preliminary evidence that training cancer patients to communicate better with their doctors is acceptable and perceived as useful, demonstrating a positive impact on behavioral intentions.
Contributor Information
Carma L. Bylund, Memorial Sloan-Kettering Cancer Center Department of Psychiatry and Behavioral Sciences 641 Lexington Ave., 7th floor New York, NY 10022 Telephone: (646) 888-0210 Fax: (212) 888-2356 bylundlc@mskcc.org
Elliott J. Goytia, Queens Cancer Center
Thomas A. D'Agostino, Memorial Sloan-Kettering Cancer Center
Linda Bulone, Queens Cancer Center
Jennifer Horner, Memorial Sloan-Kettering Cancer Center
Yuelin Li, Memorial Sloan-Kettering Cancer Center
Margaret Kemeny, Queens Cancer Center
Jamie S. Ostroff, Memorial Sloan-Kettering Cancer Center
REFERENCES
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processess. 1991;50:179–211. [Google Scholar]
- Beach MC, Price EG, Gary TL, Robinson KA, Gozu A, Palacio A, Cooper LA. Cultural competence: A systematic review of health care provider educational interventions. Medical Care. 2005;43(4):356–373. doi: 10.1097/01.mlr.0000156861.58905.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berlin EA, Fowkes WC. A teaching framework for cross-cultural health-care application in family practice. Western Journal of Medicine. 1983;139(6):934–938. [PMC free article] [PubMed] [Google Scholar]
- Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. Journal of Psychosomatic Research. 2002;52:69–77. doi: 10.1016/s0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- Brown RF, Butow PN, Boyer MJ, Tattersall MHN. Promoting patient participation in the cancer consultation; evaluation of a prompt sheet and coaching in question asking. British Journal of Cancer. 1999;80(1/2):242–248. doi: 10.1038/sj.bjc.6690346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RF, Bylund CL. Communication skills training: Describing a new conceptual model. Academic Medicine. 2008;83:37–44. doi: 10.1097/ACM.0b013e31815c631e. [DOI] [PubMed] [Google Scholar]
- Bylund CL, D'Agostino TA, Chewning BA. Training patients to reach their communication goals: A concordance perspective. In: Kissane D, Bultz B, Butow P, Finaly I, editors. Handbook of Communication in Oncology and Palliative Care. Oxford University Press; 2010. [Google Scholar]
- Bylund CL, D'Agostino TA, Ho EY, Chewning BA. Improving clinical communication and promoting health through concordance-based patient education. Communication Education. 2010;59(3):295–311. [Google Scholar]
- Cegala DJ. Communicating with your doctor: the PACE system. 2000 from http://patcom.jcomm.ohio-state.edu/index.htm.
- Cegala DJ, Lenzmeier Broz S. Provider and patient communication skills training. In: Thompson TL, Dorsey AM, Miller KI, Parrot R, editors. Handbook of Health Communication. Erlbaum; Mahwah, NJ: 2003. [Google Scholar]
- Cegala DJ, Marinelli T, Post D. The effects of patient communication skills training on compliance. Arch Fam Med. 2000;9(1):57–64. doi: 10.1001/archfami.9.1.57. [DOI] [PubMed] [Google Scholar]
- Cegala DJ, McClure L, Marinelli TM, Post DM. The effects of communication skills training on patients' participation during medical interviews. Patient Educ Couns. 2000;41(2):209–222. doi: 10.1016/s0738-3991(00)00093-8. doi: S0738-3991(00)00093-8 [pii] [DOI] [PubMed] [Google Scholar]
- Collins KS, Hughes DL, Doty MM, Ives BL, Edwards JN, Tenney K. Findings from the Commonwealth Fund 2001 Health Care Quality Survey. The Commonwealth Fund; New York, NY: 2002. Diverse communities, common concerns: Assessing health care quality for minority Americans. [Google Scholar]
- Cooper-Patrick L, Gallo JJ, Gonzales JJ, Vu HT, Powe NR, Nelson C, D.E., F Race, gender and partnership in the patient-physician relationship. Journal of the American Medical Association. 1999;282(6):583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Roter D, Beach MC, Sabin J, Carson KA, Greenwald AG, Inui TS. Implict racial bias among clinicans, communication behaviors, and patient and clinician ratings of interpersonal care. Journal of General Internal Medicine. 2009;24:S101. [Google Scholar]
- Cooper LA, Roter DL, Johson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Hopwood P, Howell A, Maguire P. Screening for psychiatric morbidity in patients with advanced breast cancer: validation of two self-report questionnaires. British Journal of Cancer. 1991;64:353–356. doi: 10.1038/bjc.1991.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutching K, Lac A, LaBrie JW. An application of the theory of planned behavior to sorority alcohol consumption. Addictive Behaviors. 2008;33(4):538–551. doi: 10.1016/j.addbeh.2007.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. American Journal of Public Health. 2004;94(12):2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style. Medical Care. 1995;33(12):1176–1187. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- Medicine I. Unequal treatment: confrontin racial and ethnic disparities in healthcare. Washington, DC.: 2003. [Google Scholar]
- Pai CW, Eddington DW. Association between behavioral intention and actual change for physical activity, smoking, and body weight among an employed population. Journal of Occupational and Envionmental Medicine. 2008;50(9):1077–1083. doi: 10.1097/JOM.0b013e31817d0795. [DOI] [PubMed] [Google Scholar]
- Post DM, Cegala DJ, Marinelli TM. Teaching patients to communicate with physicians: The impact of race. Journal of the National Medical Association. 2001;93:6–12. [PMC free article] [PubMed] [Google Scholar]
- RPSGB [08.15.08];From Compliance to Concordance: achieving shared goals in medicine taking. 1997 from http://www.concordance.org.
- Saha S, Komaromy M, Koepsell TD, Bindman AB. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159:997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Savard J, Laberge B, Gauthier JG, Ivers H, Bergeron MG. Evaluating anxiety and depression in HIV-infected patients. Journal of Personality Assessment. 1998;7:349–367. doi: 10.1207/s15327752jpa7103_5. [DOI] [PubMed] [Google Scholar]
- Shah B, Chewning B. Conceptualizing and measuring pharmacist-patient communication: a review of published studies. Res Social Adm Pharm. 2006;2(2):153–185. doi: 10.1016/j.sapharm.2006.05.001. doi: S1551-7411(06)00032-5 [pii]10.1016/j.sapharm.2006.05.001. [DOI] [PubMed] [Google Scholar]
- Shields CG, Ziner KW, Bourff SA, Schilling K, Zhao Q, Monahan P, Champion V. An intervention to improve communication between breast cancer survivors and their physicians. Journal of Psychosocial Oncology. 2010;28(6):610–629. doi: 10.1080/07347332.2010.516811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. National Academy Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- Smith WR, Betancourt JR, Wynia MK, Bussey-Jones J, Stone VE, Phillips CO, Bowles J. Recommendations for teaching about racial and ethnic disparities in health and health care. Annals of Internal Medicine. 2007;147:654–665. doi: 10.7326/0003-4819-147-9-200711060-00010. [DOI] [PubMed] [Google Scholar]
- Snaith RP, Zigmond AS. Handbook of Psychiatric Measures. American Psychiatric Association; Washington, D.C.: 2000. [Google Scholar]