Sir,
Cephalosomatic anastomosis (CSA), that is, the surgical transference of a healthy head on a surgically beheaded body under deep hypothermic conditions, as conceived by Robert White,[39] hinges on the reconnection of the severed stumps of two heterologous spinal cords (reviewed in reference).[7]
On the occasion of the first CSA between primates in 1970, Dr White hewed to the view that a severed spinal cord could not be reconnected, thus leaving the animal paralyzed.[7,39]
In 1902, Stewart and Harte reported on CN, aged 26 years, who had her spinal cord severed by a 0.32 caliber gunshot. The distance between the segments of the cord was 0.75 inch, as verified by all five attending physicians: “The ends of the cord were then approximated with 3 chromicized catgut sutures passed by means of a small staphylorraphy needle, one suture being passed anteroposteriorly through the entire thickness of the cord and the other two being passed transversely. This part of the operation was attended with unusual difficulties because of…the wide interval between the fragments, the catgut frequently tearing out before the ends were finally brought together.” Sixteen months later, “the patient slides out of bed into her chair by her own efforts and is able to stand with either hand on the back of a chair, thus supporting much of the weight of the body.”[36]
Importantly, they reviewed several cases of patients with sharp wounds to the cord that spontaneously recovered from initial paraplegia. Their conclusion was that “the operation of myelorrhaphy will be specially indicated in cases in which the cord has been cut by a sharp instrument or severed by a projectile.”[36] Whereas myelorrhaphy was not effective at 15 months in a young paraplegic patient after a self-inflicted 0.38 caliber gunshot,[16,35] nonetheless, a huge body of evidence accrued over the past decades made the first part of Stewart and Harte's prediction highly relevant.[33] In fact, had White attempted to reattach the sharply severed cord stumps in the monkey, the possibility exists that the animal might have recovered at least partial motricity.
In this paper, I will detail the recently proposed GEMINI spinal cord fusion (SCF) protocol in view of the first human CSA,[7] giving new meaning to Stewart and Harte's prediction. The recent study by Estrada et al.,[14] in which rats whose spinal cords were sharply transected recovered ambulation, confirms that CSA (HEAVEN: 7) is feasible.
Two key principles underlie the GEMINI SCF:
A sharp severance of the cords is not as damaging as clinical spinal cord injury
The gray matter “motor highway” is more important than the pyramidal tract in human motor processing.
PRINCIPLE 1: SHARP SEVERANCE
The key to SCF is a sharp severance of the cords themselves, with its attendant minimal damage to both the axons in the white matter and the neurons in the gray laminae. This is a key point: A typical force generated by creating a sharp transection is less than 10 N versus approximately 26000 N experienced during spinal cord injury, a 2600× difference![33]
A specially fashioned diamond microtomic snare-blade is one option (unpublished); a nanoknife made of a thin layer of silicon nitride with a nanometer sharp cutting edge is another alternative.[8,9] Notably, the mechanical strength of silicon is superior to that of steel.[34]
PRINCIPLE 2: GRAY MATTER “MOTOR HIGHWAY” VS PYRAMIDAL TRACT
In man, motricity is only modestly subserved by long axonal systems coursing through the spinal white matter as taught in contemporary anatomical and neurology textbooks (parenthetically, “Subdivision of the (human) white matter…into tracts is…not feasible, because most of the tracts mix with one another and overlap”).[27] Skilled voluntary movements of the hand in man are often considered to be dependent on the direct access of motor neurons (MN) from the primary motor cortex to the cord (monosynaptic Pyramidal Tract). However, indirect pathways from the motor cortex (e.g. corticobulbospinal pathways via, e.g., the reticulospinal tracts) and spinal interneuronal systems by far contribute the majority of inputs to the MNs: In man, the corticospinal tract predominantly terminates in the intermediate layers of the spinal cord where many interneurons are located.[1] Laruelle[24] wrote: L’association plurisegmentaire est réalisée, non seulement par les voies cordonales connues, mais par un système de fibres intrinsèques de la substance grise, pouvait parcourir plusieurs segments successifs: Elles confèrent une fonction conductrice à la substance grise de la moelle (The plurisegmentary association is brought about not only via the known cordonal pathways, but via a gray-matter-based system of intrinsic fibers, which cover up to several cord segments: These confer conductive properties to the cord gray matter)”. This association is further enacted via short fibers lying closest to the spinal gray matter that connect nearby spinal segments over short or very short distances (e.g., the lateral limiting layer of the Ground Bundles).[26] This explains why «in man, recovery of motor function including the distal movement is compatible with …degeneration of 83% of the pyramidal tract fibers»,[20] as occurs for lesions restricted to the human lateral corticospinal tracts.[28] In the words of Bucy et al.,[6] “The pyramidal tract…is not essential to useful control of the skeletal musculature…In the absence of the corticospinal fibers other fiber systems, particularly some…multineuronal mechanism passing through the mesencephalic tegmentum, are capable of producing useful, well-coordinated, strong and delicate movements of the extremities.”
In a recent case report, a subject with tetraplegia (ASIA A) recovered 15 months later to ASIA D, despite a 62% atrophy of the white matter tissue at the injury epicenter,[12] including the pyramidal tracts. Even in multiple sclerosis, long regarded as the prototypical white matter (long axons) disease, it is the damage to the gray matter that accounts for most of the related motor disability – even in cases without white matter loss![30] Similar anatomical arguments – propriospinal transmission versus spinothalamic tract in the case of nociception – could be made for the sensory return.[18]
In GEMINI, the gray matter neuropil will be restored by spontaneous regrowth of the severed axons/dendrites over very short distances at the point of contact between the apposed cords.
FUSOGEN-ASSISTED NEURAL RECONSTITUTION
GEMINI exploits special substances (fusogens/sealants: Poly-ethylene glycol [PEG], Chitosan) that have the power to literally fuse together severed axons or seal injured leaky neurons.[7,11,29] It is based on the concept of biological fusion, which occurs both naturally (e.g., in myoblasts) and artificially (e.g. hybridoma cells): Up to 10% of severed axons in some invertebrates can undergo spontaneous fusion with their separate distal segments.[10] Different technologies can induce axonal fusion: Chemical, laser, and electrofusion.[10,34,40] Chemical fusion is likely mediated by a dehydration effect and volume-exclusion aggregation of membrane lipids bringing adjacent lipids into physical contact.[11] Two scenarios are particularly attractive: (i) A PEG containing solution is flowed for 2 min (more than 3’ is actually deleterious) over the lesion site, and then flushed out, as outlined by Bittner et al.;[5] or (ii) a semi-interpenetrating network of PEG and photo-cross-linkable chitosan can be employed as an in situ-forming nerve adhesive/fusogen.[2] Chitosan nanoparticles or PEG can also be injected IV for several hours to enhance the effect.[7] Interestingly, there may be a body temperature effect on PEG's viscosity and efficacy (Kouhzaei et al.).[21] In contrast, chitosan in an injectable solution that moves throughout the systemic circulation – apparently regardless of viscosity: Thus the route of administration does not appear to matter in a manner similar to PEG.[11] Animal experiments on transected cords have already given proof-of-principle of the feasibility of fusogen-assisted SCF.[7,11,21,22,32] Anyway, PEG-mediated functional reconnection between closely apposed proximal and distal segments of severed axons takes many minutes of absolute immobility of the axon segments and an untested period of immobilization of the tissue for the repair to become permanent.[11] The question is whether this is actually required for successful reconstitution of motor (and sensory) transmission, also considering how perfect one-on-one axonal alignment is impossible. As proven by Bittner et al.[5,31] in peripheral nerves in vivo, behavioral recovery is excellent and improves over time after PEG fusion. This means that a sufficient number of axonal proximal stumps get fused with the distal counterparts in such a way to ensure appropriate electrophysio-logical conduction, likely the result of tight axonal packing. This number is likely low (10–15%), and yet enough for recovery, reflecting the potential for substantial plasticity in the injured CNS.[34] A similar figure applies to the damaged spinal cord in man,[4] where the number of axons in the spinal white matter is estimated at over 20 million, with about 1 million pyramidal fibers. Also, reconnection with an adjacent axon, as long as it is not an extreme mismatch, may restore acceptable function.[34] Dense axonal packing would ensure that a number of fibers would get fused.
Notice that during CSA no gap is expected between the cord stumps. Should have this not been the case, transplantable miniature neurono-axonal constructs internalized within engineered tubes could have been used to fill the gap (e.g.[13]). Actually, PEG appears to be more than sufficient even in this context. Estrada et al.[14] have fully transected rats’ spinal cords and filled the gap with PEG 600: They reported massive elongation of axons from all fiber populations (including interneurons) that grew into the PEG bridge and became remyelinated upon entering the CNS tissue. The axon growth effect was already visible at 1 week posttreatment, grew in time steadily and was long-lasting. Rats could recover physiologic locomotion.
Tangentially, collagen conduits containing autologous platelet-rich plasma have allowed successful axonal regeneration and neurological recovery in clinical peripheral nerve injury with gaps up to 12 cm (16 cm along with an added sensory nerve graft).[23]
ELECTRICITY-ACCELERATED RECOVERY
In GEMINI, local sprouting between neurons in the gray matter (see above) will reestablish a functional bridge over days to weeks. This process is accelerated by electrical stimulation via application of a spinal cord stimulator (SCS) straddling the fusion point. For instance, 1 h of continuous electrical stimulation at 20 Hz applied right after suturing together the stumps of a transected peripheral nerve cut the regeneration time from 8–10 to 3 weeks; similar accelerations are seen in man.[17]
The role of electrical stimulation goes well beyond acceleration of axonal and dendritic regrowth. The spinal cord has the capacity to execute complex stereotyped motor tasks in response to rather unspecific stimuli even after chronic separation from supraspinal structures. However, being deprived of sufficient supraspinal drive, neural processing, and pattern generating networks caudal to a spinal cord lesion lose an adequate, sustainable state of excitability to be fully operational: SCS (15–60 Hz, 5–9 V) provides a multi-segmental tonic neural drive to these circuitries and “tune” their physiological state to a more functional level.[25] Thus, “loss of voluntary control of movement may be attributed to not only a physical disruption of descending connections, but also to a physiological alteration of the central state of excitability of the spinal circuitry…(spinal cord) stimulation may facilitate excitation of propriospinal neurons which support propagation of the voluntary command to the lumbosacral spinal cord…after repetitive epidural stimulation and training…multiple, novel neuronal pathways and synapses (are established).”[3] The result is recovery of intentional movement in the setting of complete paralysis of the legs.[3,25] Similar arguments and results apply to the cervical spinal cord.[37] Of course, useful plasticity will not only occur in the cord, but also at higher levels, including the motor cortex.[12,19]
CONCLUSION
In sum, the GEMINI SCF protocol hinges on the following steps [Figure 1]:
Figure 1.
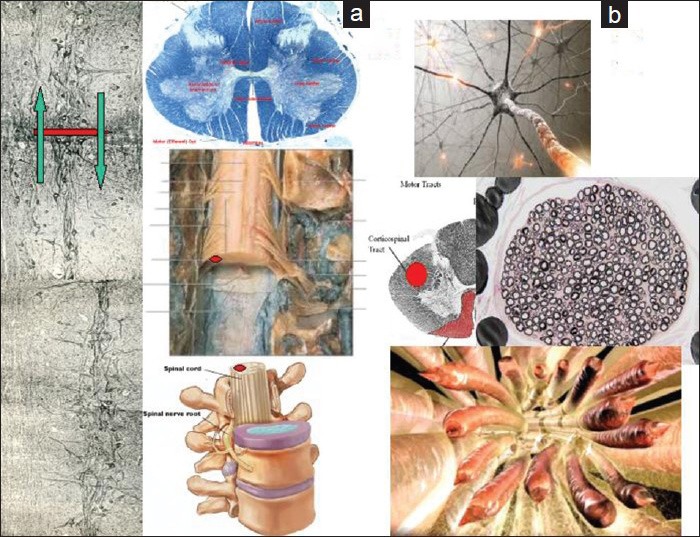
(a) Longitudinal cut along a primate spinal cord depicting the internuncial system (gray matter motor highway) and the nano-size of the proposed severance (left). The red circle on the right side of this panel is the pyramidal tract, shown in two exploded views of a sharply transected cord (middle right) and of the cord in the vertebral canal (lower middle right). (b)Visualization of the severed pyramidal tract. The uppermost image depicts a motor neuron in the cortex sending forth the axonal prolongation. Middle panel: The pyramidal tract (red) and a portion of its severed axons. Lower panel: The sharply severed axonal extensions (adapted from Laruelle 1937 and several images in the public domain)
The sharp severance of the cervical cords (donor's and recipient's), with its attendant minimal tissue damage
The exploitation of the gray matter internuncial sensori-motor “highway” rebridged by sprouting connections between the two reapposed cord stumps. This could also explain the partial motor recovery in a paraplegic patient submitted to implantation of olfactory ensheathing glia and peripheral nerve bridges: A 2-mm bridge of remaining cord matter might have allowed gray matter axons to reconnect the two ends[38]
The bridging as per point 2 above is accelerated by electrical SCS straddling the fusion point
The application of “fusogens/sealants”: Sealants “seal” the thin layer of injured cells in the gray matter, both neuronal, glial and vascular, with little expected scarring; simultaneously they fuse a certain number of axons in the white matter.
During CSA, microsutures (mini-myelorrhaphy) will be applied along the outer rim of the apposed stumps. A cephalosomatic anastomosee will thus be kept in induced coma for 3–4 weeks following CSA to give time to the stumps to refuse (and avoid movements of the neck) and will then undergo appropriate rehabilitation in the months following the procedure.
In addition, the immunosuppressant regime that will be instituted after CSA is expected to be pro-regenerative.[15]
ACKNOWLEDGMENT
The author wishes to thank the thousands of scientists and patients from around the world who benefited him with their encouragement and suggestions.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2015/6/1/18/150674
NOTE: The interested reader is referred to the author's TEDx talk for further details on HEAVEN/GEMINI: http://www.ustream.tv/recorded/52890140 (minutes 32–50), and to the author's book: Head Transplantation And The Quest For Immortality (CS/ AMAZON 2014).
REFERENCES
- 1.Alstermark B, Isa T. Circuits for skilled reaching and grasping. Annu Rev Neurosci. 2012;35:559–78. doi: 10.1146/annurev-neuro-062111-150527. [DOI] [PubMed] [Google Scholar]
- 2.Amoozgar Z, Rickett T, Park J, Tuchek C, Shi R, Yeo Y. Semi-interpenetrating network of polyethylene glycol and photocrosslinkable chitosan as an in-situ-forming nerve adhesive. Acta Biomater. 2012;8:1849–58. doi: 10.1016/j.actbio.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 3.Angeli CA, Edgerton VR, Gerasimenko YP, Harkema SJ. Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain. 2014;137:1394–409. doi: 10.1093/brain/awu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basso DM. Neuroanatomical substrates of functional recovery after experimental spinal cord injury: Implications of basic science research for human spinal cord injury. Phys Ther. 2000;80:808–17. [PubMed] [Google Scholar]
- 5.Bittner GD, Keating CP, Kane JR, Britt JM, Spaeth CS, Fan JD, et al. Rapid, effective, and long-lasting behavioral recovery produced by microsutures, methylene blue, and polyethylene glycol after completely cutting rat sciatic nerves. J Neurosci Res. 2012;90:967–80. doi: 10.1002/jnr.23023. [DOI] [PubMed] [Google Scholar]
- 6.Bucy PC, Keplinger JE, Siqueira EB. Destruction of the “pyramidal tract” in man. J Neurosurg. 1964;21:285–98. [PubMed] [Google Scholar]
- 7.Canavero S. HEAVEN: The head anastomosis venture Project outline for the first human head transplantation with spinal linkage (GEMINI) Surg Neurol Int. 2013;4(Suppl 1):S335–42. doi: 10.4103/2152-7806.113444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chang WC, Hawkes EA, Kliot M, Sretavan DW. In vivo use of a nanoknife for axon microsurgery. Neurosurgery. 2007;61:683–92. doi: 10.1227/01.NEU.0000298896.31355.80. [DOI] [PubMed] [Google Scholar]
- 9.Chang WC, Kliot M, Sretavan DW. Microtechnology and nanotechnology in nerve repair. Neurol Res. 2008;30:1053–62. doi: 10.1179/174313208X362532. [DOI] [PubMed] [Google Scholar]
- 10.Chang WC, Hawkes E, Keller CG, Sretavan DW. Axon repair: Surgical application at a subcellular scale. Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2010;2:151–61. doi: 10.1002/wnan.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chen B, Bohnert D, Borgens RB, Cho Y. Pushing the science forward: Chitosan nanoparticles and functional repair of CNS tissue after spinal cord injury. J Biol Eng. 2013;7:15. doi: 10.1186/1754-1611-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Choe AS, Belegu V, Yoshida S, Joel S, Sadowsky CL, Smith SA, et al. Extensive neurological recovery from a complete spinal cord injury: A case report and hypothesis on the role of cortical plasticity. Front Hum Neurosci. 2013;7:290. doi: 10.3389/fnhum.2013.00290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cullen DK, Tang-Schomer MD, Struzyna LA, Joel S, Sadowsky CL, Smith SA, et al. Microtissue engineered constructs with living axons for targeted nervous system reconstruction. Tissue Eng Part A. 2012;18:2280–9. doi: 10.1089/ten.tea.2011.0534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Estrada V, Brazda N, Schmitz C, Heller S, Blazyca H, Martini R, et al. Long-lasting significant functional improvement in chronic severe spinal cord injury following scar resection and polyethylene glycol implantation. Neurobiol Dis. 2014;67C:165–79. doi: 10.1016/j.nbd.2014.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Feringa ER, Johnson RD, Wendt JS. Spinal cord regeneration in rats after immunosuppressive treatment. Theoretic considerations and histologic results. Arch Neurol. 1975;32:676–83. doi: 10.1001/archneur.1975.00490520046007. [DOI] [PubMed] [Google Scholar]
- 16.Goodkin R, Budzilovich GN, Campbell JB. Myelorrhaphy: Part II. Spine. 1976;1:193–5. [Google Scholar]
- 17.Gordon T, Chan KM, Sulaiman OA, Udina E, Amirjani N, Brushart TM. Accelerating axon growth to overcome limitations in functional recovery after peripheral nerve injury. Neurosurgery. 2009;65(4 Suppl):A132–44. doi: 10.1227/01.NEU.0000335650.09473.D3. [DOI] [PubMed] [Google Scholar]
- 18.Gybels JM, Sweet WH. Basel: Karger; 1989. Neurosurgical treatment of persistent pain. [PubMed] [Google Scholar]
- 19.Isa T, Nishimura Y. Plasticity for recovery after partial spinal cord injury – hierarchical organization. Neurosci Res. 2014;78:3–8. doi: 10.1016/j.neures.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 20.Jane JA, Yashon D, Becker DP, Beatty R, Sugar O. The effect of destruction of the corticospinal tract in the human cerebral peduncle upon motor function and involuntary movements. Report of 11 cases. J Neurosurg. 1968;29:581–5. doi: 10.3171/jns.1968.29.6.0581. [DOI] [PubMed] [Google Scholar]
- 21.Kouhzaei S, Rad I, Khodayari K, Mobasheri H. The neuroprotective ability of polyethylene glycol is affected by temperature in ex vivo spinal cord injury model. J Membr Biol. 2013;246:613–9. doi: 10.1007/s00232-013-9574-3. [DOI] [PubMed] [Google Scholar]
- 22.Kouhzaei S, Rad I, Mousavidoust S, Mobasheri H. Protective effect of low molecular weight polyethylene glycol on the repair of experimentally damaged neural membranes in rat's spinal cord. Neurol Res. 2013;35:415–23. doi: 10.1179/1743132812Y.0000000133. [DOI] [PubMed] [Google Scholar]
- 23.Kuffler DP. An assessment of current techniques for inducing axon regeneration and neurological recovery following peripheral nerve trauma. Prog Neurobiol. 2014;116C:1–12. doi: 10.1016/j.pneurobio.2013.12.004. [DOI] [PubMed] [Google Scholar]
- 24.Laruelle L. La structure d la moelle epinière en coupes longitudinales. Rev Neurol. 1937;67:697–711. [Google Scholar]
- 25.Minassian K, Hofstoetter US, Danner SM, Mayr W, McKay WB, Tansey K, et al. Mechanisms of rhythm generation of the human lumbar spinal cord in response to tonic stimulation without and with step-related sensory feedback. Biomed Tech. 2013;58(Suppl.1) doi: 10.1515/bmt-2013-4013. DOI: 10.1515/bmt-2013-4013. [DOI] [PubMed] [Google Scholar]
- 26.Nathan PW, Smith MC. Fasciculi proprii of the spinal cord in man. Brain. 1959;82:610–68. doi: 10.1093/brain/82.4.610. [DOI] [PubMed] [Google Scholar]
- 27.Nathan PW, Smith M, Deacon P. Vestibulospinal, reticulospinal and descending propriospinal nerve fibres in man. Brain. 1996;119:1809–33. doi: 10.1093/brain/119.6.1809. [DOI] [PubMed] [Google Scholar]
- 28.Putnam TJ. Treatment of unilateral paralysis agitans by section of the lateral pyramidal tract. Arch Neurol Psychiatry. 1940;44:950–76. [Google Scholar]
- 29.Rad I, Khodayari K, Hadi Alijanvand S, Mobasheri H. Interaction of polyethylene glycol (PEG) with the membrane-binding domains following spinal cord injury (SCI): Introduction of a mechanism for SCI repair. J Drug Target. 2014:1–10. doi: 10.3109/1061186X.2014.956668. [DOI] [PubMed] [Google Scholar]
- 30.Schlaeger R, Papinutto N, Panara V. Spinal cord gray matter atrophy correlates with multiple sclerosis disability. Ann Neurol. 2014;76:568–80. doi: 10.1002/ana.24241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sexton KW, Pollins AC, Cardwell NL, Del Corral GA, Bittner GD, Shack RB, et al. Hydrophilic polymers enhance early functional outcomes after nerve autografting. J Surg Res. 2012;177:392–400. doi: 10.1016/j.jss.2012.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shi R. Polyethylene glycol repairs membrane damage and enhances functional recovery: A tissue engineering approach to spinal cord injury. Neurosci Bull. 2013;29:460–6. doi: 10.1007/s12264-013-1364-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sledge J, Graham WA, Westmoreland S, Sejdic E, Miller A, Hoggatt A, et al. Spinal cord injury models in non human primates: Are lesions created by sharp instruments relevant to human injuries? Med Hypotheses. 2013;81:747–8. doi: 10.1016/j.mehy.2013.07.040. [DOI] [PubMed] [Google Scholar]
- 34.Sretavan DW, Chang W, Hawkes E, Keller C, Kliot M. Microscale surgery on single axons. Neurosurgery. 2005;57:635–46. [PubMed] [Google Scholar]
- 35.Stauffer ES, Goodman FG, Nickel VL. Myelorrhaphy: Part I. Spine. 1976;1:189–92. [Google Scholar]
- 36.Stewart FT, Harte RH. A case of severed spinal cord in which myelorrhaphy was followed by partial return of function. Philadelphia Med J. 1902;9:1016–20. [Google Scholar]
- 37.Sunshine MD, Cho FS, Lockwood DR, Fechko AS, Kasten MR, Moritz CT. Cervical intraspinal microstimulation evokes robust forelimb movements before and after injury. J Neural Eng. 2013;10:036001. doi: 10.1088/1741-2560/10/3/036001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tabakow P, Raisman G, Fortuna W, Czyz M, Huber J, Li D, et al. Functional regeneration of supraspinal connections in a patient with transected spinal cord following transplantation of bulbar olfactory ensheathing cells with peripheral nerve bridging. Cell Transplant. 2014 doi: 10.3727/096368914X685131. [In Press] [DOI] [PubMed] [Google Scholar]
- 39.White RJ. Head transplants. Sci Am. 1999:24–6. [Google Scholar]
- 40.Zhang J, Sheng L, Jin C, Liu J. Liquid metal as connecting or functional recovery channel for the transected sciatic nerve. 2014 ArXiv: 1404.5931. [Google Scholar]


