Abstract
Attention-deficit/hyperactivity disorder (ADHD) is defined by extreme levels of inattention–disorganization and/or hyperactivity–impulsivity. In DSM-IV, the diagnostic criteria required impairment in social, academic, or occupational functioning. With DSM-5 publication imminent in 2013, further evaluation of impairment in ADHD is timely. This article reviews the current state of knowledge on health-related impairments of ADHD, including smoking, drug abuse, accidental injury, sleep, obesity, hypertension, diabetes, and suicidal behavior. It concludes by suggesting the need for new avenues of research on mechanisms of association and the potential for ADHD to be an early warning sign for secondary prevention of some poor health outcomes.
Keywords: ADHD, Health, Suicide, Injury, Obesity, Sleep
1. Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a developmental disorder characterized by a pattern of severe inattention–disorganization and/or hyperactivity–impulsivity beyond that observed in individuals at a comparable level of development (American Psychiatric Association, 2000). Worldwide, prevalence is estimated at about 5% for children (Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007) and 2.5% for adults (Simon, Czobor, Balint, Meszaros, & Bitter, 2009). For a diagnosis of ADHD, the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) required that symptoms must cause impairment.
It is important to note that impairment is not the same thing as severity, at least conceptually. Severity can be thought of as the intensity or frequency of symptoms, whereas impairment is the consequence of those symptoms. Depending on the degree of support in the environment, even a severe condition might bring very little impairment. That said, untangling severity from impairment in practice is notoriously difficult. Scheduled for released in 2013, DSM-5 will likely reflect an enhanced effort to distinguish disorder (and severity) from impairment to some extent, but impairment must still be evaluated (American Psychiatric Association, 2012a, 2012b). The consideration of physical health outcomes of ADHD may assist in this regard, as these are outcomes that are conceptually quite different from the core symptoms of ADHD. As context, this article briefly comments on key areas of impairment that are already well-documented or else beyond the scope of this review, then explores the relatively new area of ADHD-related physical health impairments and physical health outcomes.
Clinicians are increasingly evaluating ADHD symptoms in adults, but because the DSM-IV criteria were developed primarily for children, ADHD symptoms in adults present additional clinical and conceptual challenges (Adler, Shaw, Sitt, Maya, & Morrill, 2009). Whereas childhood hyperactive behaviors may subside in intensity with age or may be replaced by restlessness, which is difficult to quantify, characteristics such as inattentiveness, organizational (executive) dysfunction, and impulsivity often persist (Adler & Chua, 2002; Barkley, Murphy, & Fischer, 2008; Gallagher & Blader, 2001). Although health issues for children and adults are quite different, the literature is sufficiently small that studies of both children and adults were surveyed here.
Insights about ADHD can include study of the diagnosis of ADHD, or of population patterns of the correlates of inattention, impulsivity, and hyperactivity. Because ADHD appears to be an extreme of a continuously varying trait in the population, studies of symptomatic variation are considered to be informative about etiology and risk/ morbidity even in the absence of formal diagnosis. This is important because establishing formal diagnosis of ADHD by research criteria in large populations is very costly and thus rarely done. However, studies of symptom variation in the population are also limited by the fact that the universe of influences on symptoms of inattention may be broader than the influences on ADHD itself. That is, ADHD diagnosis requires ruling out many of the known health influences on inattention. This review considers studies of both dimensional and categorical diagnosis, highlighting whenever these approaches do not converge.
It also is crucial to recognize that ADHD is often associated with comorbid psychiatric disorders that may be independently associated with impairment. Oppositional defiant disorder and conduct disorder, in particular, are commonly comorbid with ADHD (Barkley, 2002). In adolescents and adults, mood disorders (Baron, 2007) and substance use problems can complicate the picture (Baron, 2007; Goodman, 2007). Relatedly, ADHD's varying severity and comorbidity results in widely varying course of treatment for different individuals; further, many individuals discontinue treatment in adolescence and adulthood just as many health risks take hold. Thus, both clinically and scientifically, it is often difficult to be certain of the specificity of impairment to ADHD, and to foreshadow the conclusions, one important area of research is to try to identify component functional domains of ADHD and other disorders, as well as course and treatment moderators, that mediate and moderate particular health outcomes.
2. Well documented impairments and conditions
Several well documented associated problems and/or impairments warrant brief mention here, both to set the stage for the new domain of health impairments but also because any interpretation of health impairments ultimately has to consider the potential interplay of ADHD and associated problems with outcome.
First, cognitive and emotional problems are well documented in ADHD. ADHD is associated, at least at a group level, with reduced executive functions (e.g., working memory, response inhibition, and organization) (Brown, 2008; Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005). Like the symptoms of inattention, difficulties in these areas may become more apparent as patients age and demands for self-management increase (Brown, 2008). It is also increasingly recognized that ADHD is often associated with problems in emotion regulation, mood, and irritability (Anastopoulos et al., 2010; Barkley & Fischer, 2010; Barkley & Murphy, 2010). Although not part of the formal symptoms of ADHD, they may cause interpersonal problems in addition to adjustment difficulties.
Second, in addition to the comorbid problems noted earlier, some physical problems are already known in ADHD, notably that ADHD is often associated with problems in motor coordination or motor development (Carte, Nigg, & Hinshaw, 1996; Cole, Mostofsky, Larson, Denckla, & Mahone, 2008; Macneil et al., 2011). These also may either index or predispose to secondary health problems as noted later.
Third, the DSM-IV-Text Revision (2000) specification that ADHD should be associated with impairment in “occupational, social, and academic” functioning (American Psychiatric Association, 2000) warrants brief comment.
The association of ADHD with academic underachievement has been documented for some decades and holds over and above comorbid learning disorder (Barbaresi, Katusic, Colligan, Weaver, & Jacobsen, 2007; Faraone et al., 1993; Hinshaw, 1992). Notably, recent prospective data indicate that in population samples, early childhood attention problems prospectively predict adolescent academic failure, even after controlling for intervening IQ and disruptive behavior problems, although ADHD was not formally assessed (Breslau et al., 2010).
By the turn of the 21st century, deficits in occupational functioning were recognized in adults with ADHD. ADHD has been associated with substantially higher rates of job termination, lower performance ratings by supervisors, and reduced productivity (Barkley, 2002; Barkley, Fischer, Smallish, & Fletcher, 2006; De Graaf et al., 2008; for a review see Küpper et al., 2012). More recently, one study reported that these effects were associated cross-sectionally with inattention, rather than hyperactivity–impulsivity, and mediated by problems in executive functioning (Stavro, Ettenhofer, & Nigg, 2007). Further work is needed to develop and identify interventions that can prevent these outcomes, but new interventions to improve academic or occupational outcomes are beyond the scope.
With regard to social impairment and functioning, the association between ADHD and peer rejection and neglect is the most important and well studied to date. This association, first noted decades ago, is increasingly well described (Hoza, 2007; Hoza et al., 2005; Pelham & Milich, 1984). This more recent literature highlights how important peer effects are on overall outcome for ADHD (Hoza et al., 2005; Mikami & Lorenzi, 2011; Mrug et al., 2012) as well as the important interplay across psychosocial domains (e.g., parenting and peer relations; see (Hurt, Hoza, & Pelham, 2007; Mikami, Jack, Emeh, & Stephens, 2010). These effects are present in both boys and girls but girls are understudied, and some indications suggest potential unique patterns of risk and protection in girls (e.g., Blachman & Hinshaw, 2002; Mikami & Lorenzi, 2011).
Although less fully documented, additional social, relational, and psychological impacts of ADHD have continued to emerge and could occupy an entire review in their own right even beyond the area of peer relations. In particular, for both children and adults, ADHD can have a direct negative influence on familial relationships (Escobar et al., 2005) and other family members (Barkley, 2008; Harpin, 2005). These effects may reflect either gene–environment correlations (the parents and child share genes that predispose the child to ADHD and the parent to depression or substance use), or they may also reflect parental inability to cope with the burden of caring for a child with ADHD. This burden may be perceived differently by mothers and fathers, but both appear to experience elevated stress that is only partly attributable to comorbid child defiant/oppositional behavior (Podolski & Nigg, 2001).
Parent–child conflict is well-appreciated as a complication in ADHD and is an important target for behavioral intervention, as it may contribute to continuing ADHD symptoms (Wells et al., 2000). However, children with ADHD have also reported witnessing more interparental conflict than children without ADHD, which was associated with teacher ratings of ADHD severity (Counts, Nigg, Stawicki, Rappley, & von Eye, 2005), an effect that may be modulated by child genotype (Martel et al., 2011; Nikolas, Friderici, Waldman, Jernigan, & Nigg, 2010). Data from twin studies using behavioral genetic methods indicate that these child reports do not merely reflect the child's genotype (e.g., temperament), but also environmental effects, such as conflict in the home (Nikolas, Klump, & Burt, 2011). These reports imply that a recursive loop may occur in which ADHD provokes interparental conflict, which in turn exacerbates emotional load and ADHD symptoms in the child. This possibility, and the potential that a subset of children with ADHD are particularly vulnerable, suggests both avenues for intervention and avenues for understanding the underlying etiological process. Thus, significant work remains to be done on ADHD-related impairment related to psychosocial function. Overall, the interplay of family conflict, attributions of child and parent, and ADHD persistence remains a rich area for research exploration and a reminder for clinicians of the relevance of family assessment in treatment planning for individuals with ADHD.
Furthermore, many secondary consequences of ADHD could serve as mediators of downstream psychological impairments. Of particular note is that individuals with ADHD may suffer reduced self esteem, perhaps secondary to peer rejection or academic or occupational difficulties (Hoza et al., 2004; Barber, Grubbs, & Cottrell, 2005; Rucklidge, Brown, Crawford, & Kaplan, 2007; but for a negative finding see Ek, Westerlund, Holmberg, & Fernell, 2008). This issue of self-esteem intersects with complex findings about the nature of attributions in children with ADHD that are quite interesting but well beyond the scope of the current review (Hoza et al., 2004; Owens et al., 2007; Evangelista, Owens, Golden, & Pelham, 2008; Swanson, Owens, & Hinshaw, 2012). This remains an area ripe for investigation, particularly in regard to attributions about treatment and recovery.
Both self-esteem and attributions intersect with the elusive interpersonal phenomenon of stigma, which may result in individuals with ADHD or their families (e.g., parents of affected children) suffering social rejection over and above that related to their own behavior or that of their child. This is because the public now holds beliefs that ADHD is associated with being lazy, angry, or otherwise unpleasant to have around, whether or not this applies to the individual in question (Canu, Newman, Morrow, & Pope, 2008; Coleman, Walker, Lee, Friesen, & Squire, 2009; Martin, Pescosolido, Olafsdottir, & McLeod, 2007; Norvilitis, Scime, & Lee, 2002; Pescosolido, Fettes, Martin, Monahan, & McLeod, 2007; Walker, Coleman, Lee, Squire, & Friesen, 2008).
For our purposes, the attributional, attitudinal, and social aspects of ADHD set an important context for considering health effects. Because these social consequences, along with impulsivity or inattention, could contribute indirectly to or modulate health outcomes in their own right, failure to note them could risk over-simplifying health patterns and findings.
3. Context for health outcomes in ADHD
Turning to health problems per se, it has been suggested that the early treatment of primary psychiatric conditions may prevent the development of future disorders (Hazell, 2007). Indeed, ADHD is usually the first of the several comorbid psychiatric disorders to emerge during development (Mannuzza, Klein, Abikoff, & Moulton, 2004), suggesting that it may be a risk condition that often can progress to antisocial behavior, substance use disorders and, in some instances, mood disorders and other outcomes (Hazell, 2007; Mannuzza et al., 2004; Martel et al., 2007; Rutter, Kim-Cohen, & Maughan, 2006). For example, in boys, conduct disorder and antisocial personality disorder are generally preceded by ADHD (see Beauchaine, Hinshaw, and Pang (2010) and Loeber and Hay (1997), although many children with ADHD do not develop conduct disorder. Therefore, the possibility is extremely important and has been noted that ADHD may be a target for secondary prevention of complicating mental disorders.
Less appreciated, however, has been the potential for ADHD to be a target for the secondary prevention of other health outcomes. Because of its association with impulsivity and poor decision making, executive functioning, and social functioning, as well as subtle developmental delays, it is beginning to be recognized that ADHD might be expected to convey risk of frank physical health disorders or impairments. This review is intended to provide an introduction and update to this state of knowledge in relation to physical-health related outcomes. Treatment is commented on within each section if it complicates interpretation of health outcomes or if there are notable findings on it; otherwise treatment implications of the findings are noted in the concluding section.
4. Methods
Although this is a selective review intended to illustrate new directions for investigation, the following literature search strategy was undertaken to ensure that the literature was adequately surveyed. Electronic searches were performed in PubMed using the base terms “ADHD” or “attention deficit hyperactivity disorder” and the following limits: “humans, clinical trial, meta-analysis, practice guideline, randomized controlled trial, review, English.” Electronic searches were also performed in Psych Info using “ADHD” or “attention deficit hyperactivity disorder” text words. Additional search terms were added to the base terms for each area of potential impairment assessed. The electronic searches were complemented with reference lists from the identified literature and from prior reviews retrieved by informal search of the literature. When prior formal meta-analyses are available, I emphasize those findings and add context and considerations to them for the reader. When large scale population studies or prospective cohort studies were available, I put most emphasis on those findings. The actual number of similar studies remained far too small for formal meta-analysis in any area that was not already meta-analyzed. The literature was also deemed too limited to justify a formal systematic review on which clinical recommendations would be based. Thus, instead, a qualitative review was undertaken, with literature selectively cited to illustrate the main themes in the current impairment literature. The goal therefore was not a comprehensive or systematic review (which would not be possible at article length while surveying the several areas covered here), but rather to bring readers up-to-date on the current state of knowledge about health impairment in ADHD so as to set the stage for and highlight newly emerging areas of clinical and research interest.
5. Results
5.1. Smoking and substance use
Substance use disorders and smoking (cigarette use) are health outcomes that are well recognized to co-occur with ADHD. Based on a recent meta-analysis, about one in four substance dependent patients had or have ADHD (van Emmerik-van Oortmerssen et al., 2012). Two recent meta-analyses (Charach, Yeung, Climans, & Lillie, 2011; Lee, Humphreys, Flory, Liu, & Glass, 2011) focused on prospective cohort studies that directly address the question of future risk posed by having ADHD. I therefore simply note those results and add brief caveats and considerations.
First, as summarized in Table 1, both meta-analyses confirm reliable prospective associations of ADHD with future substance use disorders, with a doubling of risk for nicotine use and risks ranging below and above that figure for different definitions of substance use disorders. While we might expect that sex, in particular, and other moderators, generally, would alter these conclusions, no moderator effects were significant in either meta-analysis.
Table 1.
Odds ratios (and 95% confidence intervals) derived from two meta-analyses of ADHD and future substance use
| Charach et al., 2011 | Lee et al., 2011 | |
|---|---|---|
| Nicotine | 2.36(1.71, 3.27) | 2.82(2.41–3.29) |
| Alcohol | 1.35(1.11–1.64) | 1.74(1.38–2.20) |
| Cannabis | 1.51(1.02–2.24) | 1.58 (1.16–2.14) |
| Cocaine | na | 2.05(1.38–3.04) |
| Non-specific drug use | na | 2.64(1.77–3.94) |
| Non-alcohol drug use disorder | 3.48 (1.80–6.73) | na |
| Psychoactive substances | 1.59(1.12–2.25) | na |
Note to table: odds ratio ranges from 1 (no increased risk) to infinity. An odds ratio of 2.0 indicates a doubling (or a 100% increase) in risk. An odds ratio of 1.5 indicates a 50% increase in risk.
Second, however, the number of studies available for pooling remained small in all instances, resulting in low statistical power to detect moderator effects. This also resulted in some effects, notably those for non-specific substance use disorders, to be difficult to estimate because effects depended heavily on one or two studies. Further, very few outcome studies have extended beyond young adulthood, making it difficult to evaluate the role of age of assessment on these outcomes. A recent follow up of children with ADHD to age 41 showed an elevated rate of substance use disorders and smoking– but not alcoholism, an effect that was weaker than at earlier ages and largely carried by individuals who developed antisocial personality disorder (Klein et al., 2012).
Third, it would be interesting to consider component domains of ADHD that may predict risk (e.g., inattention, impulsivity). Nicotine is a “special case” in regard to drug use that ADHD may predispose to, because nicotine may temporarily reduce the severity of ADHD symptoms, leading patients to attempt to self-medicate (Potter, Bucci, & Newhouse, 2012; Wilens et al., 2007). As pointed out by the meta-analysis authors and others, data to enable such pooled analysis of component domains like inattention remain lacking.
Fourth, those reviews concurred with earlier authors in concluding that it is unclear whether comorbid conduct or antisocial personality disorder accounts for these effects, because there were not enough such studies to meta-analyze the moderator effect or mediator effect. It seems fairly clear, as Lee et al. (2011) concluded, that children with ADHD + conduct disorder are at higher risk than those with ADHD alone. But does ADHD alone still confer risk? Burke, Loeber, and Lahey (2001) followed 177 clinic-referred boys with ADHD to age 15 and examined substance use. ADHD was associated with substance use but this effect was accounted for statistically by conduct disorder. However, symptoms of inattention predicted smoking even after control of conduct disorder and other confounders. Other studies also suggested that the association of ADHD with substance use was accounted for by the group with conduct disorder (e.g., (Barkley, Murphy, & Fisher, 2008).
Population samples, which also looked at dimensional symptom variation, have amplified the findings from Burke et al. (2001), tending to show unique effects of inattention or hyperactivity/impulsivity independently of conduct disorder symptoms or aggression. Elkins, McGue, and Iacono (2007), for example, examined age 18 drug use prospectively in a population sample of just over 1500 twins recruited at age 11 years. Although conduct disorder was a more powerful predictor than ADHD, ADHD independently predicted tobacco and illicit drug use (but not abuse/dependence) and hyperactivity–impulsivity uniquely predicted all outcomes. Lambert (2005) also found similar effects, although in that study effects were only significant for ADHD at age 14 and not by age 18.
Pingault et al. (2012) recently reported on a prospective population cohort examining just over 1800 participants from childhood to early adulthood and looking at nicotine, alcohol, and cannabis dependence. While most of the risk for most substance use disorders was indeed carried by disruptive behavior problems, inattention contributed unique predictive power over and above behavior problems for nicotine dependence.
Similarly, Jester et al. (2008) studied 335 youth and evaluated growth curve trajectories of continuously measured attention problems and conduct problems (rated by parent and teacher beginning at age 5 and continuing until age 17) in a sample at high and low risk of drug abuse problems by family history. They examined alcohol abuse and marijuana use at age 17. Results identified distinct trajectories of attention problems and aggression using parent and teacher ratings. Whereas the greatest risk for onset of problem drug use was in children with elevated attention problems and aggression, the group with elevated attention problems alone was also at increased risk. Further, the group with aggression and attention problems was at higher risk than the group with aggression alone.
Fifth, most evidence suggests that pharmacological treatment of ADHD does not increase the risk for subsequent substance use disorders (i.e., alcohol, tobacco, and drug) and may even have a protective effect (Biederman et al., 2008; Gray & Upadhyaya, 2009; Wilens, Faraone, Biederman, & Gunawardene, 2003; Wilens et al., 2008). However, clinicians are obliged to monitor potential misuse and diversion of psychostimulants for ADHD, including the illicit use of prescription stimulant medications for performance enhancement or diversion for selling, trading, or giving away by adolescents and young adults (Kollins, 2007; McCabe, Teter, & Boyd, 2006; Poulin, 2001).
In short, smoking and substance use disorders may represent both a health risk in ADHD (albeit at least partially mediated by conduct disorder or accounted for by the subset of individuals with co-occurring serious antisocial behavior problems).
Overall, ADHD conveys marked future risk of substance use disorders. In the case of cigarette smoking, ADHD confers unique risk over and above that conveyed by conduct disorder or disruptive behavior problems. In the case of illicit substance use disorders, the main risk is carried by those with ADHD and comorbid conduct disorder, although at a population level both inattention and aggression/conduct problems appear to convey some degree of unique risk. Because smoking and drug abuse mediate a host of subsequent negative social and health outcomes, and because ADHD is often detected earlier than conduct disorder, ADHD is a promising target for prevention of future smoking and substance use disorders.
5.2. Sleep
Sleep difficulties in ADHD have received considerable investigation yet this area continues to lack consensus conclusions. Clinicians too often can overlook the possibility of a sleep disorder in children with inattention, although it is well established that sleep disorders can contribute to inattention (Owens, 2005, 2008). Less clear is how often true sleep disorders, vs. sleep-associated behavior problems, are found in youth or adults with ADHD (Chervin, Dillon, Bassetti, Ganoczy, & Pituch, 1997; Owens, 2005, 2008).
The relationship between sleep and ADHD is quite complex and likely bidirectional due to the extensive interplay of sleep and diurnal rhythm with basic functions of arousal and attention shared neurotransmitter systems, and the interplay of behavior and context with sleep readiness and quality. The observational clinical data on ADHD and sleep problems was reviewed by several authors recently (Nigg 2006; Cortese, Faraone, Konofal, and Lecendreux 2009; Corkum, Tannock, & Moldofsky, 1998; Spruyt & Gozal, 2011; Yoon, Jain, & Shapiro, 2012), An accessible yet detailed outline of basic mechanisms and research hypotheses and question that might productively be pursued in ADHD and sleep was summarized by a special review panel and published by Owens et al. (2012). The clinical reviews concluded that (a) studies of intrinsic sleep disorder in ADHD (e.g., sleep apnea, parasomnias, restless leg syndrome, circadian disorder, etc.) yield numerous but inconsistent findings, and (b) parent ratings data and actigraphy studies provide fairly convincing evidence that ADHD is often (in perhaps 50% of cases) related to impairments in sleep quality due to sleep-related behavior problems, such as bedtime resistance, sleep-onset difficulties, and trouble with waking in the morning, all of which in turn may exacerbate daytime inattention and overactivity at least in children (Dahl, 1996; Spruyt & Gozal, 2011) Adults with ADHD are also at substantially higher risk for experiencing disturbed sleep than are control populations, independent of other psychiatric comorbidities and not accounted for by ADHD pharmacotherapy (Surman et al., 2009).
It is increasingly recognized that these behavior-related sleep problems also appear to be primary downstream health effects of having ADHD and not merely medication side effects. Even so, medications can complicate the clinical picture, since psychostimulants can increase sleep-onset latency (Weiss & Salpekar, 2010). Conversely, α2-adrenoceptor agonists have been used to facilitate sleep, although there are limited data regarding their impact on sleep parameters (Spiegel & DeVos, 1980; Weiss & Salpekar, 2010), and even afternoon doses of traditional stimulants may sometimes improve sleep in children with ADHD (see discussion in Spruyt & Gozal, 2011).
Mixed findings in the sleep domain suggest the need for additional characterization. The most likely state of affairs at the moment is that behavioral-sleep problems (and thus impaired sleep quality) may be quite common and should be examined routinely in clinical assessment of ADHD, whereas intrinsic sleep disorders are certainly possible but not necessarily common in children or adults presenting with ADHD. Thus, it is small clear that sleep problems are a health consequence of ADHD, but perhaps only a fairly minority of the time is sleep disorder a primary etiology for ADHD. That said, however, it will also be helpful to continue to attempt to characterize a subset of children with ADHD who may have an intrinsic sleep regulation disorder. It is also helpful to recognize that sleep-related behavior problems can impair sleep, creating a negative cycle of worsened attention and behavior in children with ADHD. Thus, disturbed sleep may be a target for behavioral intervention for some children to address inability to settle, family conflict around bedtime, excessive energy in the evening, or related behavior inputs. Clinical suggestions along these lines are provided in more detail by Lecendreux and Cortese (2007).
5.3. Physical injuries
Evidence continues to accumulate indicating that ADHD is associated with elevated risk of physical injuries (Badger, Anderson, & Kagan, 2008; Marcus, Wan, Zhang, & Olfson, 2008; Merrill, Lyon, Baker, & Gren, 2009; Pastor & Reuben, 2006). Common physical traumas among individuals with ADHD include superficial injuries and contusions, open wounds, dislocations, strains, sprains, and fractures of the upper limbs (Marcus et al., 2008; Merrill et al., 2009). Many studies examining the association between ADHD and unintentional injury rely on medical records and are, therefore, limited to those diagnoses that have received medical attention. However, using data from the National Health Interview Survey among more than 50,000 children aged 6 to 17 years, Pastor and Reuben (2006) examined parent-reported injuries (excluding poisoning) that required consultation with a medical professional. The annualized injury rate in the general population was 115/ 1000 (11.5%); but, among those ever diagnosed with ADHD, this rate was 204/1000 (20.4%; adjusted odds ratio [OR], 1.83; 95% confidence interval [CI], 1.48–2.26).
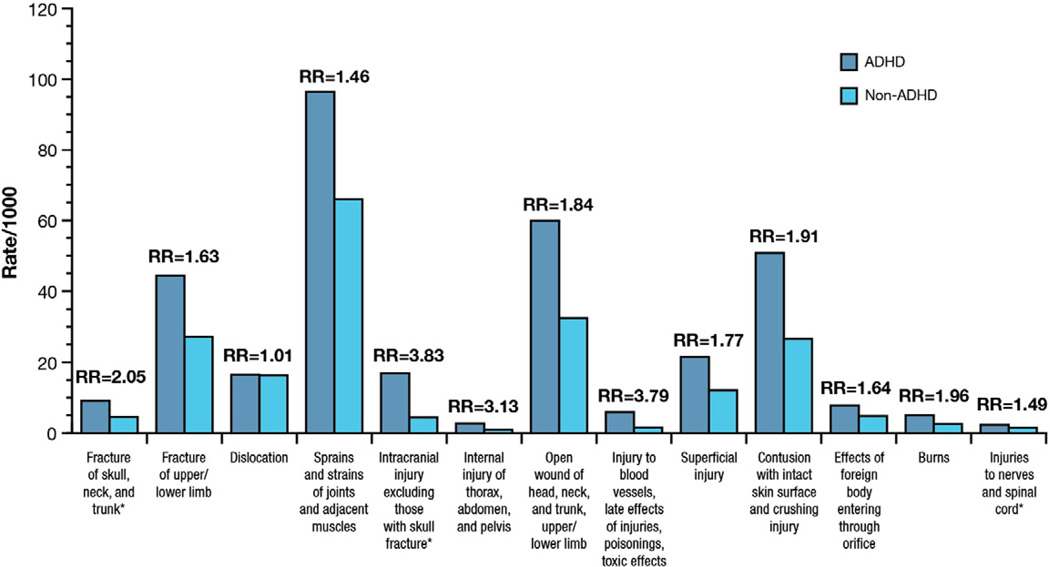
The risk for injuries appears to continue into adulthood. Pulling from a large insurance claims data base of over 100,000 individuals, Swensen et al. (2004) compared 1308 individuals with at least one time point of physician-applied ADHD diagnosis and a matched control group. They identified a doubling of claims for accidental injury or poisoning in ADHD vs. controls (p < 0.05) (Swensen et al., 2004). In a cohort that included nearly 500,000 persons aged 0 to 64 years, Merrill et al. (2009) demonstrated that, after adjustment for age, sex, and socioeconomic status, individuals with ADHD exhibited a 1.55 times greater rate of injury than did individuals without ADHD. In that retrospective study, ADHD appeared most strongly associated with severe injuries. Fig. 1 displays the pattern of injuries observed.
Fig. 1.
Incidence of injuries among individuals aged 0 to 64 years by ADHD status. (Merrill et al., 2009). Cohort included 490,378 individuals including 2186 with ADHD. *Considered severe injuries by investigators. ADHD, attention-deficit/hyperactivity disorder; Fx, fracture; RR, rate ratio (obtained by dividing the incidence rate of injuries in the ADHD participants to the non-ADHD participants). Reprinted from Advances in Medical Sciences, 2009, 54, 20–26.
Not surprisingly, the types of injuries associated with ADHD appear to vary with the stage of development of the individual. In very young children, ADHD and hyperactivity in general are associated with an increased risk of nasal and aural foreign body insertions (Perera, Fernando, Yasawardena, & Karunaratne, 2009). Pediatric patients with ADHD are at increased risk for burns (Badger et al., 2008; Fritz & Butz, 2007), and adolescents and adults with ADHD are at risk of auto accidents (Barkley & Cox, 2007) and related injuries (Barkley, 2002; Barkley & Cox, 2007; Barkley, Murphy, & Kwasnik, 1996) due to poorer driving including more traffic violations and license suspension (Barkley, 2002, 2004; Barkley, Guevremont, Anastopoulos, DuPaul, & Shelton, 1993; Jerome, Segal, & Habinski, 2006).
Whether intervention for ADHD prevents secondary accidental injury cannot be concluded with confidence due to methodological limitations. Two studies failed to demonstrate statistically reliable differential rates of injury on and off medication (Marcus et al., 2008; Merrill et al., 2009), but statistical power was low in these studies given the relatively low base rate of injuries. On the other hand, prospective treatment studies, most conducted with methylphenidate, have generally concluded that psychostimulant treatment can improve driving behavior and thus may reduce driving related accidental injury (Barkley & Cox, 2007; Jerome et al., 2006; Kay, Michaels, & Pakull, 2009), although interpretation of these data is also limited by small sample sizes, short study durations, and reliance on simulator assessments that may not generalize to real-world outcomes.
Treatment and prevention of impairments may be improved by a better understanding of the mechanisms linking ADHD to injury, accidents, or proximal behavior like dangerous driving. The component problem could be distractibility (Farmer & Peterson, 1995; Merrill et al., 2009) or risk taking (Badger et al., 2008; Garzon, Huang, & Todd, 2008), though data to address such suppositions are sparse (Garzon et al., 2008). However, with regard to driving problems, Oliver, Nigg, Cassavaugh, and Backs (2011) conducted a small experimental simulation study suggesting that driving errors and accidents in individuals with ADHD were related not to inattention but to negative emotionality and poor frustration tolerance (Oliver et al., 2011).
Furthermore, the reliable association between ADHD and certain types of injuries may permit identification of children who would benefit from ADHD screening. In a sample of 133 children aged 6 to 12 years who were hospitalized for injuries sustained as a result of auto-pedestrian collision, auto-bicycle collision, other bicycle collision, or falling, 28.6% screened positive for ADHD, but only 34% of those were receiving treatment for ADHD (Maxson, Lawson, Pop, Yuma-Guerrero, & Johnson, 2009). In contrast, among children admitted to the hospital for appendicitis, only 12.7% had a positive screen for ADHD (although again, only a minority of them, 40%, was receiving ADHD treatment). After adjusting for sex, age, ethnicity, use of ADHD pharmacotherapy, previous hospital visits, and parental education, children being admitted for injuries were more than three times as likely to have a positive screen for ADHD than were those being admitted for appendicitis (OR, 3.25; 95% CI, 1.57–6.72). Comorbid psychopathology was not assessed.
Overall, elevated risk of accidental injuries sufficient to seek medical attention (assuming no treatment-seeking bias in ADHD) is a marker of impairment and morbidity that is increasingly well established, and mechanisms that might account for this association need more intensive and large scale study.
5.4. Risky sexual activity and sexually transmitted infections
The effect of ADHD on sexual behaviors is understudied, but preliminary data suggest that individuals with ADHD lead higher-risk sexual lifestyles. Barkley et al. (2006) examined sexual activity in young adulthood (aged 19 to 25 years) in their local sample of 149 individuals who had been diagnosed as hyperactive in childhood and 72 community controls. Those with a history of ADHD had intercourse at an earlier age, more prior sexual partners, less use of artificial birth control, higher rates of pregnancy (or getting a female pregnant), and a fourfold increase in history of sexually transmitted disease vs. the non-ADHD group. Similar results were reported by Flory, Molina, Pelham, Gnagy, & Smith (2006) using adult follow up interviews of the Pittsburgh ADHD longitudinal study with 175 men with prior ADHD and 111 community controls. Young men with prior ADHD had earlier onset of sexual activity, more sexual partners, and more partner pregnancies than those without a history of ADHD. Crucially, conduct disorder or symptoms only partially accounted for this effect. Brown et al. (2010) found that adolescents with externalizing disorders (i.e., ADHD, opposi-tional defiant disorder, conduct disorder) were more likely to be sexually active than were adolescents without psychiatric diagnoses, but this effect, unlike in the other studies, was not reliable after adjustment for age, sex, race, alcohol use, and psychiatric hospitalization.
These studies focused on males, leaving it unclear how women's behavior was affected. Hosain, Berenson, Tennen, Bauer, and Wu (2012) began to address that. They reported, in a general community sample of women, that some risky sexual behaviors, but not others, were related to symptoms of inattention or hyperactivity/impulsivity. A second study to address this issue was recently reported by Huggins, Rooney, and Chronis-Tuscano (2012). Although it was also a retrospective survey (42 college age women with ADHD and controls), the women with ADHD reported more unprotected sex not only than non-ADHD women but also more so than men on average. Notably, this effect was moderated by their perception of their parental relationship with their mother. Thus, while preliminary, the evidence at this point suggests that both men and women with ADHD are at elevated risk, but more study of gender differences and particularly of gender-specific moderators of risk will be important. Whereas ADHD is more common in males, risky sex may have more severe consequences for women.
This literature remains limited by small samples, reliance on self report and retrospective recall, and varying control of confounders. Nonetheless, while the role of conduct disorder and substance use need to be more definitively described, the studies provides suggestive evidence that ADHD may independently contribute to risky sexual behavior (and thus to sex-related outcomes like unwanted pregnancy or sexually transmitted disease) over and above the effects of conduct disorder.
These results are potentially quite important and should encourage more study. Areas for future investigation include generalizability across age, sex, race/ethnicity, and sampling type, further clarification of the extent to which conduct problems or substance use mediate risky sexual behaviors, evaluation of the role of impulsivity, negative affect/tension reduction, low self-esteem, and risk taking and sensation seeking as mediators, and whether ADHD treatments influence these behaviors and outcomes.
5.5. Obesity and physical fitness
Perhaps the most striking claim about ADHD-related health effects in the past decade has been the emergence of a possible association between ADHD and obesity, at least in the United States (Chen, Kim, Houtrow, & Newacheck, 2010; Cortese & Penalver, 2010; Cortese et al., 2008; Fuemmeler, Ostbye, Yang, McClernon, & Kollins, 2010; Pagoto et al., 2009; Taurines et al., 2010; Waring & Lapane, 2008). This literature was recently reviewed in detail by Cortese and Vincenzi (2012) and is summarized here with emphasis on the largest studies.
It is consistently reported that, among children presenting for obesity care, rates of ADHD are elevated (Cortese et al., 2008). However, it is less clear how elevated obesity rates are among children with ADHD. In the United States, the most compelling data come from population-based epidemiological surveys. Although these studies all lack a full clinical assessment of ADHD, they avoid the potential inferential biases in clinical samples. Two publications examined data from the 2003 National Survey of Children's Health in the United States (Chen et al., 2010; Waring & Lapane, 2008). The first (Chen et al., 2010) examined over 46,000 participants aged 10 to 17 years. The obesity rate in children this age group overall was 12.2%, but among children who were ever told they had ADHD by a doctor, the rate was nearly 19% (Chen et al., 2010), yielding an unadjusted risk ratio of 1.6. The second study examined both children and adolescents (aged 5 to 17 years, more than 62,000 participants) with similar findings (Waring & Lapane, 2008). Although lack of formal diagnostic evaluation is a limitation, these population results tend to confirm the clinical findings, and also demonstrate that socioeconomic status does not account for the ADHD-obesity association.
To address the lack of formal diagnosis, Pagoto et al. (2009) looked at nationally representative samples of adults (n = 6735) and conducted structured diagnostic interviews in a subset to ascertain the presence of ADHD. Here, with formal diagnostic evaluation, the same picture emerged: 21.6% of adults were obese, but this percentage rose to 29.4% for those with ADHD (an unadjusted ratio of 1.4). Thus, the evidence from population surveys holds up even when more formal evaluation of ADHD is considered.
One important confound is that both ADHD and obesity are related to socio-economic status; this has been controlled in the best studies and does not explain the effect. Another is that both ADHD and obesity are also associated with other psychiatric conditions, particularly depression (Goodman & Whitaker, 2002; Pine, Goldstein, Wolk, & Weissman, 2001). While sex was adjusted in some studies, the relative risk and timing of risk for boys vs. girls remains in need of more investigation.
However, the most important issue is that the direction and mechanism of the association remain unknown. As pointed out by Cortese and Penalver (2010), all studies to date were cross-sectional, such that the causal structure of relations among ADHD, obesity, and associated health characteristics and psychopathology is still uncertain.
Obesity itself is multidetermined, relating to socioeconomic status, mood, family structure, and other factors (Puder & Munsch, 2010); therefore, simple linear effects are unlikely. However, several mechanisms might account for this association [for further elaboration of some of these possibilities, see Cortese and Penalver (2010) and Cortese and Vincenzi (2012)]. First, obesity could create symptoms that mimic ADHD (e.g., via sleep deprivation secondary to sleep-disordered breathing). Because ADHD generally has onset prior to obesity, this possibility seems unlikely to fully account for the observed association, but prospective data, preferably with control of baseline body mass index, are needed. Second, a shared neurobiological or genetic mechanism may be common to ADHD and obesity. For example, there is evidence that microdeletions at chromosome 11p14.1 may link ADHD and obesity (Shinawi et al., 2011). Other potential common mechanisms include immune or inflammatory response. Third, shared intergenerational transmission of ADHD and obesity may occur via fetal-programming mechanisms (Odent, 2010). Finally, the last and perhaps simplest possibility is that ADHD behaviors lead to poor eating and exercise habits, or that ADHD-related motor delays (see introduction to this review) may discourage exercise and participation in physical activity, either directly or indirectly leading to excess weight gain.
Although these possibilities are not mutually exclusive, this last proximal behavioral hypothesis is the easiest to study and, consequently, has been the first to receive support. Initial studies suggest that patients with ADHD eat more impulsively (Dempsey, Dyehouse, & Schafer, 2011), consume foods with less nutrient density and more total fat than non-ADHD individuals (Howard et al., 2011), and receive less exercise than their peers (Barkley, 2002; Harvey et al., 2009; Kim, Mutyala, Agiovlasitis, & Fernhall, 2011), although it is unclear whether this is due to lack of energy, lack of persistence, motor clumsiness, or other factors. Children with ADHD are rated not only as more hyperactive but also as more sluggish and underactive (McBurnett, Pfiffner, & Frick, 2001); hyperactivity and sluggishness are positively correlated. Thus, ADHD may be characterized by poor energy regulation, with bursts of overactivity interspersed with underactivity. The type of sustained activity that promotes fitness and weight loss, which in childhood requires collaboration with peers and cooperation with authorities, in adulthood requires planning, and at all ages requires sustained effort, may be less typical of individuals with ADHD, at least in contemporary, sedentary societies.
A potential association between obesity and ADHD has important clinical implications with regard to health outcomes and prevention. If ADHD contributes to obesity risk, serious downstream health effects are likely. As societal activity and eating patterns continue to evolve and obesity rises both among children and adults in the United States and other Western countries, it will be important to determine with better epidemiological data whether individuals with ADHD are among those vulnerable to the dynamics that cause obesity (whether due to mood regulation, impulsivity, lack of energy, or shared biology vis-à-vis altered metabolism). It may be helpful to screen obese patients for ADHD and, conversely, to ask patients with ADHD about their eating and exercise patterns (Cortese & Penalver, 2010).
With regard to intervention, moderate to vigorous physical activity as a potential intervention for ADHD needs more aggressive investigation. It might both improve primary symptoms of ADHD and prevent obesity, if ADHD is causally related to obesity. In aging adults, aerobic physical activity can improve attention and other cognitive functioning (Kramer et al., 1999). Initial, small studies in children are encouraging. For example, in a study of 18 boys aged 8 to 12 years with ADHD, higher physical activity was associated with improved executive function (Gapin & Etnier, 2010). A study of 25 boys aged 7 to 15 years with ADHD observed that their attention deficits were improved through physical activity independent of methylphenidate treatment (Medina et al., 2010). Finally, a small study of 17 elementary school children (grades K-3) found that an 8-week regimen of daily moderate to vigorous physical activity resulted in moderate improvement in response inhibition and in ADHD symptoms (Smith et al., 2011). Secondary prevention of obesity in this population is unstudied and randomized controlled studies are lacking in general, but have begun to be initiated in some centers.
The appropriate role of pharmacotherapy in obese patients with ADHD has yet to be determined. In a cross-sectional study of children and adolescents with ADHD, subjects receiving pharmacotherapy were no more likely to be overweight than were children without ADHD (Waring & Lapane, 2008), but rather were more likely to be underweight. This is consistent with data indicating that psychostimulant use during childhood may slow growth in both height and weight (Faraone, Biederman, Morley, & Spencer, 2008; Swanson et al., 2007), although these effects may not be enduring (Biederman, Spencer, Monuteaux, & Faraone, 2010; Faraone et al., 2008; Spencer et al., 2007).
Overall, the role of weight and obesity in ADHD is increasingly important in societies that are experiencing rapid increases in rates of obesity. Individuals with ADHD may be particularly susceptible to various causes of obesity, whether via prenatal programming, biology, or behavioral habits, and the relationship between ADHD and obesity may be changing as obesity rates increase worldwide. Further study of this relationship will be extremely important. Most needed at this juncture are prospective studies that can establish temporal precedence, i.e., whether when baseline body mass is taken into account, ADHD symptoms predict excessive weight gain going forward.
5.6. Diabetes
Whereas an association between ADHD and obesity is beginning to be documented, there is a paucity of data examining whether ADHD is directly associated with obesity-related medical complications including type 2 diabetes mellitus (T2DM) and hypertension (Krause, Cleper, Kovalski, Sinai, & Davidovits, 2009; Levitt Katz et al., 2005). A retrospective chart review that examined the incidence of neuropsychiatric disorders in children with T2DM found that 46 of the 237 subjects (19.4%) had a neuropsychiatric disorder and 10 (4.2%) had a diagnosis of ADHD (Levitt Katz et al., 2005). Although the overall rate of neuropsychiatric disorders observed in this population was notable, the prevalence of ADHD per se was not elevated. The current review thus identified no data supporting an association of ADHD with diabetes. However, as obesity rates increase and the possibility exists that individuals with ADHD are overrepresented for obesity risk, ADHD as a risk factor for diabetes will need to be monitored.
5.7. Hypertension
The possible relationship between ADHD and hypertension is nuanced and is one area where the dynamics are very different for adults vs. children. Both obesity and smoking are recognized risk factors for hypertension and could mediate an association between hypertension and ADHD in adults (Biederman et al., 2006; Cortese & Penalver, 2010). Additionally, psychosocial factors may mediate the risk of developing hypertension (Fuemmeler et al., 2010). In the largest study to date, Fuemmeler et al. recently examined the relationship between ADHD symptoms and hypertension among adults in a large cohort from the National Longitudinal Study on Adolescent Health. They observed a significant association (p ≤ 0.05) between three or more hyperactive–impulsive symptoms and hypertension. Following adjustment for body mass index, the association was no longer significant, suggesting that obesity was mediating this effect. The authors did not report on psychoactive medications in their sample, which could affect cardiovascular findings (Fuemmeler et al., 2010; Resnick et al., 1997) and did not formally diagnose ADHD.
In the pediatric population, however, the picture is different because smoking and other health related behaviors are rarely at issue. Here, the relationship between hypertension and inattentive and hyperactive– impulsive behaviors is essentially unstudied. In contrast to adults, in whom hypertension is generally primary, in children it is usually secondary (i.e., a medical cause can typically be identified). However, in those cases hypertension may cause inattentive symptoms–a virtually unstudied possibility due to the rarity of hypertension in children. However, in a small, pilot chart review study, 11 children with renovascular hypertension were reviewed; 5 of them exhibited elevated restlessness, sleep disturbances, temper tantrums, hyperactivity, aggressive behavior, and attention deficit (Krause et al., 2009). Upon successful treatment with percutaneous angioplasty (1 patient continued to require antihypertensive therapy with amlodipine), all 5 showed behavioral improvement, including complete resolution in 3 of them. Further studies employing standardized behavioral ratings and comparisons to a reference cohort may allow for better evaluation of this possibility.
Psychostimulant medications are, of course, an important factor to consider with regard to ADHD and hypertension. Amphetamine- and methylphenidate-based medications approved for the treatment of ADHD can increase heart rate and blood pressure as a result of sympathetic activation (Elia & Vetter, 2010), although the mean increases in heart rate and blood pressure observed in healthy ADHD patients without a history of cardiovascular disease have been relatively small and are rarely clinically significant (Elia & Vetter, 2010; Stiefel & Besag, 2010). The use of these medications in patients with underlying cardiovascular disease is generally contraindicated, and caution should be exercised when treating patients with preexisting hypertension (Adderall XR [package insert], 2011; Ritalin LA [package insert], 2010; Vyvanse [package insert], 2011; Wigal, 2009).
In all, a link between ADHD and hypertension has not been studied to any extent in children, but evidence suggestive of an association has emerged for adults in the only major population survey conducted to date, but mediated by obesity. The possibility of this association should be monitored as population health trends continue. Hypertension may become a secondary health outcome of ADHD, via smoking and obesity, and a more significant risk in adults than children. Prospective studies that can establish direction (or sequence) of effects will be extremely helpful.
5.8. Early mortality
5.8.1. Impulsivity and mortality
The life expectancy of individuals with ADHD either alone or compared with individuals without ADHD has not been characterized. An increase in mortality associated with ADHD is quite plausible, however, since impulsivity has been linked to earlier mortality in the general population (Barkley, 2002; Friedman et al., 1995). Overall, mortality risk is expected to be somewhat increased in patients with ADHD because of elevated smoking, drug use, accidents, and impulsivity. However, the magnitude of this risk is not well characterized. Klein et al. (2012) reported that children with ADHD were more likely than non-ADHD children to have died by the age 41 follow up (p < .05) although the numbers were small. The presence of coexisting disorders may also significantly affect the mortality of patients with ADHD such that it has been suggested that health insurance providers consider the mortality risk of individuals with ADHD comparable to that of the general population, except when conduct or substance abuse disorders are present (Cotlar, 2003).
Instead, studies addressing ADHD-related mortality issues have focused largely on the potential contributions of (a) treatment-related sudden death and (b) suicide (James, Lai, & Dahl, 2004; McCarthy, Cranswick, Potts, Taylor, & Wong, 2009).
5.8.2. Treatment risk
Considerable research has examined the risk of sudden cardiac death among individuals with ADHD, particularly among those taking psychostimulants. A matched case–control study examining sudden unexplained death in children and adolescents found a significant association between psychostimulant use and sudden death (p = 0.02) (Gould et al., 2009). However, the appropriateness of using patients who died in motor vehicle accidents as a comparator group in that study has been questioned, given evidence that psychostimulant use may improve driving performance in those with ADHD (Blume & Rostain, 2010). Furthermore, a large retrospective cohort study from the United Kingdom failed to demonstrate an increased rate of sudden death associated with methylphenidate- or amphetamine-based psychostimulants or atomoxetine (McCarthy et al., 2009). A large survey of health records in the United States similarly failed to find evidence of an association, although small effects could not be ruled out (Cooper et al., 2011). Clinical guidelines now advise caution in relation to cardiac abnormalities when treating with psychostimulants, albeit with some disagreement about specifics of how this should be done (Adderall XR [package insert], 2011; American Academy of Child and Adolescent Psychiatry, 2007; Ritalin LA [package insert], 2010; Vyvanse [package insert], 2011).
5.8.3. Suicide
Recent evidence has clarified that ADHD is associated with a small but reliable increase in suicide risk. Suicide is the third leading cause of death in teenagers in the United States (American Academy of Child and Adolescent Psychiatry, 2001), particularly among boys. In general, girls and women are more likely than boys and men to attempt suicide, but males are more likely than females to complete suicide. Suicide risk is difficult to quantify because it is a rare event, so even large samples have very few cases to evaluate. However, a handful of key reviews and epidemiological studies provide the most relevant evidence.
First, in a classic review, James et al. (2004) concluded that the annualized risk of completed suicide in individuals with ADHD was about 32/100,000. This represented approximately a threefold risk increase when compared with about 11/100,000 among males aged 5 to 24 years at that time. However, the authors concluded that the effect was primarily due to individuals with comorbid psychiatric conditions, particularly mood and substance use disorders. They nonetheless considered ADHD an amplifier of risk in individuals with these disorders.
In a more recent review, Impey and Heun (2012) concluded that ADHD was associated with elevated rates of suicide attempts. Similarly, using nationally representative data from the National Comorbidity Survey, Agosti, Chen, and Levin (2011) found that 16% of adults with ADHD had attempted suicide compared with approximately 11% of adults without ADHD (OR=1.5). However, again, this effect was largely due to individuals with ADHD who had comorbid psychiatric disorders.
In one of the largest prospective studies, Haavisto et al. (2005) examined an all-male sample from a large birth cohort follow-up in Finland. Subjects were assessed for psychopathology by adult ratings scales at age 8 years and for suicidal behavior in the last 6 months at age 18 years. Numerous age-8 predictors of age-18 suicide attempts were identified. The rate of suicide attempts by age 18 in those with ADHD at age 8 (defined as a clinical range score on the rating scale) was 13% vs. 1% in the non-ADHD group (OR=13.6). However, other domains of psychopathology, particularly aggression and withdrawal, accounted for this effect statistically.
With regard to lethally serious and completed attempts, another analysis examined the same all male cohort to age 24 years (n = 5302, with 54 attempts that resulted in either hospitalization or death) (Sourander et al., 2009). Hyperactive behaviors (OR>4), as well as conduct and emotional problems, were among the age-8 predictors of life-threatening or lethal suicide attempts. However, once again hyperactive and inattentive behaviors at age 8 did not predict serious suicide outcome independently of conduct and emotional problems. The strongest overall age-8 predictor in the psychopathology domain was the presence of clinical-range conduct and emotional problems together.
However, in studies of clinical populations (i.e., either formally diagnosed and followed up in case–control design or identified via psychiatric inpatients or incarcerated individuals), the presence of ADHD may become an additional predictor of suicidal behavior (such studies are inevitably too small to inform completed suicide or lethality with adequate statistical power). In a prospective case–control study of 125 children diagnosed with ADHD at age 4 to 6 years and subsequently assessed for depression and suicidal behavior during the span of age 9 to 18 years, ADHD was associated with elevated risk for both single and recurrent episodes of adolescent depression and suicidal behavior (Chronis-Tuscano et al., 2010). Consistent with population base rates, girls with ADHD were at a greater risk for depression and suicide attempts than were boys with ADHD (Chronis-Tuscano et al., 2010).
The confirmation of risks of suicide attempts in girls and women with ADHD was also reported by Hinshaw et al. (2012). This ten-year follow up of girls who were 6–12 years old at baseline and 17–24 years old at follow up (140 with ADHD and 88 typically developing) revealed higher rates of suicide attempts in the girls with ADHD, despite failing to show increases in several other domains of poor outcome.
A similar pattern seems to hold in clinical, inpatient as opposed to community samples. In a study of 178 subjects with depression, impairments in attention, as assessed by the Stroop task, were linked to more frequent and more lethal suicide attempts (Keilp, Gorlyn, Oquendo, Burke, & Mann, 2008). In a cross-sectional study of 43 children admitted to a psychiatric inpatient unit (N = 43), Goodman, Gerstadt, Pfeffer, Stroh, and Valdez (2008) reported that assaultive/ suicidal patients were approximately 6 times more likely to be diagnosed with ADHD than were patients who displayed only assaultive behaviors (29.2% vs. 5.3%; p < 0.05). The presence of ADHD, suicidal behavior, and aggression were all intercorrelated.
It is unclear whether treatment of ADHD in itself may reduce suicide or suicide-attempt risk in these high-risk comorbid cases. However, one study found that boys treated with methylphenidate were less likely to attempt suicide by the time they reached young adulthood (Paternite, Loney, Salisbury, & Whaley, 1999).
Overall, whereas ADHD is associated with elevated risk of suicide attempts (particularly in girls) and lethal suicide attempts (particularly in boys), to a substantial extent this risk is mediated by co-occurring psychiatric conditions, which may vary for males (conduct and emotional problems) and females (depression). The coexistence of impulsivity (or ADHD), depression, and substance use, specifically when severe enough to warrant hospitalization, is of particular concern. However, it is important to recognize that because suicide attempts are rare, even with a slight elevation of risk in ADHD, the risk of suicide attempt in ADHD alone remains relatively small. Risk is more notable, however, when ADHD co-occurs with depression or antisocial behavior.
5.9. Increased health system costs/use
Examining health care use is not equivalent to attempting to quantify the overall societal economic impact of a disorder, which would include health care costs, increased rates of incarceration, occupational impairment, and other costs. However, ADHD is associated with a doubling of direct medical costs (Guevara, Lozano, Wickizer, Mell, & Gephart, 2001; Leibson & Long, 2003). The mean total out-of-pocket health care costs for children with ADHD in 1996 was $386 compared with $202 for the general population (p = 0.001), and, during a given year, children with ADHD used more outpatient visits (6.0 vs. 2.4) and prescriptions (9.9 vs. 2.3) than did the general pediatric population (Chan, Zhan, & Homer, 2002).
Guevara and colleagues found that children with ADHD were 2.1 times (adjusted OR, 2.08; 95% CI, 1.78–2.42) more likely to be hospitalized than were children without ADHD, although the number of inpatient days between the 2 groups was not significantly different (Guevara et al., 2001). Children with ADHD treated with psycho-stimulants have substantially higher health care costs (both inpatient and outpatient) than do those with ADHD not receiving such therapy, with the exception of emergency department visits (Chan et al., 2002). Increases in inpatient and outpatient health care costs as well as prescription drug costs have also been documented in adults with ADHD (Secnik, Swensen, & Lage, 2005). In addition, these use rates and associated costs escalate if ADHD co-occurs with comorbid disorders. Using claims data from a large health maintenance organization, adjusted incremental health care costs for children with ADHD alone were $375 compared with $812 when ADHD occurred with a comorbid mental health disorder (Guevara et al., 2001).
5.10. Summary and discussion
Whereas it has been well known that many kinds of psychiatric, academic, occupational, and social impairments are associated with ADHD in children and adults, the association of ADHD with frank health risks has been less often noted. This review considered several such health risks, highlighting positive findings in some and not in others. These findings suggest new directions for treatment and prevention research. Such research can both attempt to ameliorate secondary complications and test causal theories of the association between ADHD and health outcomes.
There are several limitations to this literature, and consequently this review, that must be noted before drawing conclusions. First, with a few exceptions noted, and although most major studies covaried sex, it remains unclear to what extent risks vary by sex. This is of obvious importance given that ADHD itself differs in prevalence by sex. This question is relatively well studied in the case of substance use disorders, but less so in most of the other health domains. For example, this review did not include eating disorders, which may be a health outcome more likely in girls with ADHD, while noting briefly that influences on suicidality vary by sex due to differential comorbidity profile and differential base rates. Likewise, effects of race and ethnicity, though covaried in key studies, are largely unstudied in regard to differential health outcomes in ADHD, despite evidence that many important health effects discussed herein (e.g., obesity, hypertension) carry crucial race or ethnicity-related moderators and specific risk factors. Both sex and age could interact with age effects, which were noted when relevant throughout.
Another important limitation is that, although prospective data are in hand for some important domains (notably substance and nicotine use, suicidality, and risky sexual behavior), other domains such as obesity rely on cross-sectional data. Thus, health effects and ADHD remains a new area that needs a fully mature literature including prospective outcome studies, in some areas.
Finally, a crucial limitation as well as a future direction concerns the extent to which existing treatments vs. new, yet-to-be developed treatments are sufficient to address or prevent the outcomes noted here. Only hints in this regard exist as noted. In general, the findings suggest the potential for follow up of existing prospective cohorts to examine health outcomes related to interventions. They also suggest a potentially broader scope for novel pharmacological, behavioral, or psychoeducational interventions that can take the best of what is known about preventing obesity, accidental injury, and other risks and combine this with what is known about how to treat ADHD in children and adults.
Table 2 summarizes the main take home messages from this review. Several points can be made from this summary. First, ADHD is clearly associated with worse physical health outcomes across multiple domains. These include unhealthy behaviors and outcomes like smoking, illicit substance use disorders, accidental injuries, obesity, and even suicide attempts and completed suicides.
Table 2.
Summary of main health related findings.
| Health domain | Conclusion | Comment and caveats |
|---|---|---|
| Smoking | OR = 2.3–2.8 | Not accounted for by conduct disorder |
| Substance use disorders | OR = 1.5–2.5 | Conduct disorder explains many effects |
| Impaired sleep | Associated | Bedtime related behavior problems |
| Intrinsic sleep disorder | Unclear | Mixed, small sample studies |
| Injury | OR = 1.5–1.8 | Mediators, role of comorbidity not clear |
| Risky sexual behavior | Preliminary | Prospective case control data only |
| Obesity | OR = 1.5 | Cross sectional data only |
| Diabetes | No effect | Essentially unstudied |
| Hypertension | Population effect | Adults, mediated by obesity/body mass |
| Suicide attempt | Associated | Girls, mediated by mood disorder |
| Lethal or completed Attempt | OR>4 | Boys, mediated by conduct, substance |
Second, however, the quality of evidence for these associations varies. Population based surveys are still lacking for risky sexual behavior, diabetes, or hypertension. Prospective data are lacking for obesity and reduced fitness, while comorbid or associated conditions mediates much of the association with drug abuse and suicide risk.
Third, following on this, the health effects are best understood from a developmental perspective. ADHD is widely understood as a developmental condition with onset in childhood. Nearly all of the health effects seen here emerge in adolescence or adulthood. In the intervening years, children with ADHD can develop additional problems, particularly conduct disorder and mood problems. When these occur, they tend to statistically account for many (though certainly not all) of the health effects seen. Thus, two interpretations can be made. One interpretation is that ADHD provides an amplification of risk in the presence of conduct or mood problems for risks such as suicide. Another, complementary interpretation is that ADHD risk on health outcomes operate via a meditational pathway or a kind of developmental cascade, in which symptoms or disorder of ADHD can develop into conduct problems and then serious health outcomes.
In either scenario, ADHD is best seen not as an isolated risk factor but as part of a constellation of psychopathological and perhaps personality-related risk factors for poor health outcomes. Nonetheless, it appears likely that ADHD does provide a unique contribution, in varying degrees, to key outcomes including smoking, accidental injury, and potentially obesity. Crucially, by virtue of its early onset prior to many of the complicating conditions that ultimately “carry” the individual all the way into disease, ADHD may be one of the earliest reliable predictors of long term poor health outcomes, making it a powerful potential target for secondary prevention early in life before other risk conditions have emerged. Thus, ADHD becomes an important target in its own right for prevention of future smoking, substance use disorders, risky sexual behavior, accidental injury, suicide risk, and perhaps obesity. While some of those risks are addressed by preventing conduct disorder and antisocial behavior from emerging in youth with ADHD, others are not.
5.11. Clinical and treatment implications
In addition to the prevention implications just noted, these findings reinforce the conclusion that evaluation of fundamental health behaviors and outcomes is important in individuals with ADHD. Further, the findings suggest that more consideration be given to viewing children with ADHD as being at elevated risk for multiple poor health outcomes, and that this risk should be monitored routinely. Clinical treatments that might preventsuch outcomes, either by preventing mediating conditions like conduct disorder or by rem oving the ADHD component of combined risk, warrant further examination.
6. Conclusion
By virtue of its standing as an early onset, developmental condition that is often persistent, ADHD may be understood as an important gateway not only to psychiatric comorbidity and poor life outcome but to at least some poor health outcomes as well. As trends in health change, risks associated with ADHD may also evolve further. In particular, the findings for obesity, although still in need of causal evaluation, may open new questions about etiology and early developmental influences. In aggregate, the emerging data on impairment in ADHD underscore the importance of identifying opportunities for secondary prevention of the worst outcomes when children present with ADHD.
HIGHLIGHTS.
-
►
Health-related outcomes of ADHD are not well understood.
-
►
ADHD is associated with elevated morbidity and mortality.
-
►
ADHD is related to obesity but prospective data are lacking.
-
►
ADHD is associated with elevated risk of accidental injury.
-
►
Research on interventions targeting secondary health correlates of ADHD is necessary.
References
- Adderall XR. [package insert] Wayne, PA: Shire US Inc.; 2011. [Google Scholar]
- Adler L, Shaw D, Sitt D, Maya E, Morrill MI. Issues in the diagnosis and treatment of adult ADHD by primary care physicians. Primary Psychiatry. 2009;16:57–63. [Google Scholar]
- Adler LA, Chua HC. Management of ADHD in adults. The Journal of Clinical Psychiatry. 2002;63(Suppl. 12):29–35. [PubMed] [Google Scholar]
- Agosti V, Chen Y, Levin FR. Does attention deficit hyperactivity disorder increase the risk of suicide attempts? Journal of Affective Disorders. 2011;133:595–599. doi: 10.1016/j.jad.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry. Summary of the practice parameters for the assessment and treatment of children and adolescents with suicidal behavior. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40:495–499. doi: 10.1097/00004583-200104000-00024. [DOI] [PubMed] [Google Scholar]
- American Academy of Child and Adolescent Psychiatry. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/ hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:894–921. doi: 10.1097/chi.0b013e318054e724. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. 4th Edition. Washington, DC: American Psychiatric Association; 2000. Attention-deficit and disruptive behavior disorders; pp. 85–93. (Text Revision). [Google Scholar]
- American Psychiatric Association. [Accessed February 29];The impairment and disability subgroup. 2012a www.dsm5.org/meetus/pages/impairmentanddisability.aspx.
- American Psychiatric Association. [Accessed February 29];DSM-5: The Future of Psychiatric Diagnosis. 2012b http://www.dsm5.org/Pages/Default.aspx.
- Anastopoulos AD, Smith TF, Garrett ME, Morrissey-Kane E, Schatz NK, Sommer JL, et al. Self-regulation of emotion, functional impairment, and comorbidity among children with ADHD. Journal of Attention Disorders. 2010;15:583–592. doi: 10.1177/1087054710370567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badger K, Anderson L, Kagan RJ. Attention deficit-hyperactivity disorder in children with burn injuries. Journal of Burn Care & Research. 2008;29:724–729. doi: 10.1097/BCR.0b013e31818480e1. [DOI] [PubMed] [Google Scholar]
- Barbaresi WJ, Katusic SK, Colligan RC, Weaver AL, Jacobsen SJ. Long-term school outcomes for children with attention-deficit/hyperactivity disorder: a population-based perspective. Journal of Developmental and Behavioral Pediatrics. 2007;28:265–273. doi: 10.1097/DBP.0b013e31811ff87d. [DOI] [PubMed] [Google Scholar]
- Barber S, Grubbs L, Cottrell B. Self-perception in children with attention deficit/hyperactivity disorder. Journal of Pediatric Nursing. 2005;20:235–245. doi: 10.1016/j.pedn.2005.02.012. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Driving impairments in teens and adults with attention-deficit/ hyperactivity disorder. The Psychiatric Clinics of North America. 2004;27:233–260. doi: 10.1016/S0193-953X(03)00091-1. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Major life activity and health outcomes associated with attention-deficit/hyperactivity disorder. The Journal of Clinical Psychiatry. 2002;63(Suppl. 12):10–15. [PubMed] [Google Scholar]
- Barkley RA. Global issues related to the impact of untreated attention-deficit/ hyperactivity disorder from childhood to young adulthood. Postgraduate Medicine. 2008;120:48–59. doi: 10.3810/pgm.2008.09.1907. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Cox D. A review of driving risks and impairments associated with attention-deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. Journal of Safety Research. 2007;38:113–128. doi: 10.1016/j.jsr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:503–513. doi: 10.1097/00004583-201005000-00011. [DOI] [PubMed] [Google Scholar]
- Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: adaptive functioning in major life activities. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- Barkley R, Murphy K, Fisher M. ADHD in Adults. New York: Guilford Press; 2008. [Google Scholar]
- Barkley RA, Guevremont DC, Anastopoulos AD, DuPaul GJ, Shelton TL. Driving-related risks and outcomes of attention deficit hyperactivity disorder in adolescents and young adults: a 3- to 5-year follow-up survey. Pediatrics. 1993;92:212–218. [PubMed] [Google Scholar]
- Barkley RA, Murphy KR. Deficient emotional self-regulation in adults with attention-deficit/hyperactivity disorder (ADHD): the relative contributions of emotional impulsiveness and ADHD symptoms to adaptive impairments in major life activities. Journal of ADHD & Related Disorders. 2010;1:5–28. [Google Scholar]
- Barkley RA, Murphy KR, Fischer M. Impairment in major life activities. ADHD in Adults: What the Science Tells Us. New York, NY: Guilford Press; 2008. [Google Scholar]
- Barkley RA, Murphy KR, Kwasnik D. Motor vehicle driving competencies and risks in teens and young adults with attention deficit hyperactivity disorder. Pediatrics. 1996;98:1089–1095. [PubMed] [Google Scholar]
- Baron D. The impact of comorbid disorders on adults with ADHD. Psychiatric Times. 2007:7–10. [Google Scholar]
- Beauchaine TP, Hinshaw SP, Pang K. Comorbidity of attention-deficit/ hyperactivity disorder and early onset conduct disorder: Biological, environmental, and developmental mechanisms. Clinical Psychology: Science and Practice. 2010;17:327–336. [Google Scholar]
- Biederman J, Faraone SV, Spencer TJ, Mick E, Monuteaux MC, Aleardi M. Functional impairments in adults with self-reports of diagnosed ADHD: a controlled study of 1001 adults in the community. The Journal of Clinical Psychiatry. 2006;67:524–540. doi: 10.4088/jcp.v67n0403. [DOI] [PubMed] [Google Scholar]
- Biederman J, Monuteaux MC, Spencer T, Wilens TE, Macpherson HA, Faraone SV. Stimulant therapy and risk for subsequent substance use disorders in male adults with ADHD: a naturalistic controlled 10-year follow-up study. The American Journal of Psychiatry. 2008;165:597–603. doi: 10.1176/appi.ajp.2007.07091486. [DOI] [PubMed] [Google Scholar]
- Biederman J, Spencer TJ, Monuteaux MC, Faraone SV. A naturalistic 10-year prospective study of height and weight in children with attention-deficit hyperactivity disorder grown up: sex and treatment effects. Journal of Pediatrics. 2010;157(635–640):640. doi: 10.1016/j.jpeds.2010.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blachman DR, Hinshaw SP. Patterns of friendship among girls with and without attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2002;30(6):625–640. doi: 10.1023/a:1020815814973. [DOI] [PubMed] [Google Scholar]
- Blume J, Rostain AL. Increased cardiac death or decreased motor vehicle accidents? The American Journal of Psychiatry. 2010;167:213–215. doi: 10.1176/appi.ajp.2009.09101388. [DOI] [PubMed] [Google Scholar]
- Breslau N, Breslau J, Peterson E, Miller E, Lucia VC, Bohnert K, et al. Change in teachers' ratings of attention problems and subsequent change in academic achievement: a prospective analysis. Psychological Medicine. 2010;40:159–166. doi: 10.1017/S0033291709005960. [DOI] [PubMed] [Google Scholar]
- Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G, et al. Psychiatric disorders and sexual risk among adolescents in mental health treatment. Journal of Consulting and Clinical Psychology. 2010;78:590–597. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TE. ADD/ADHD and impaired executive function in clinical practice. Current Psychiatry Reports. 2008;10:407–411. doi: 10.1007/s11920-008-0065-7. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB. Which aspects of ADHD are associated with tobacco use in early adolescence? Journal of Child Psychology and Psychiatry. 2001;42(4):493–502. [PubMed] [Google Scholar]
- Canu WH, Newman ML, Morrow TL, Pope DL. Social appraisal of adult ADHD: stigma and influences of the beholder's Big Five personality traits. Journal of Attention Disorders. 2008;11:700–710. doi: 10.1177/1087054707305090. [DOI] [PubMed] [Google Scholar]
- Carte ET, Nigg JT, Hinshaw SP. Neuropsychological functioning, motor speed, and language processing in boys with and without ADHD. Journal of Abnormal Child Psychology. 1996;24(4):481–498. doi: 10.1007/BF01441570. [DOI] [PubMed] [Google Scholar]
- Chan E, Zhan C, Homer CJ. Health care use and costs for children with attention-deficit/hyperactivity disorder: national estimates from the medical expenditure panel survey. Archives of Pediatrics & Adolescent Medicine. 2002;156:504–511. doi: 10.1001/archpedi.156.5.504. [DOI] [PubMed] [Google Scholar]
- Charach A, Yeung E, Climans T, Lillie E. Childhood attention-deficit/ hyperactivity disorder and future substance use disorders: comparative meta-analyses. Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(1):9–21. doi: 10.1016/j.jaac.2010.09.019. http://dx.doi.org/10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- Chen AY, Kim SE, Houtrow AJ, Newacheck PW. Prevalence of obesity among children with chronic conditions. Obesity. 2010;18:210–213. doi: 10.1038/oby.2009.185. (Silver.Spring). [DOI] [PubMed] [Google Scholar]
- Chervin RD, Dillon JE, Bassetti C, Ganoczy DA, Pituch KJ. Symptoms of sleep disorders, inattention, and hyperactivity in children. Sleep. 1997;20:1185–1192. doi: 10.1093/sleep/20.12.1185. [DOI] [PubMed] [Google Scholar]
- Chronis-Tuscano A, Molina BS, Pelham WE, Applegate B, Dahlke A, Overmyer M, et al. Very early predictors of adolescent depression and suicide attempts in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry. 2010;67:1044–1051. doi: 10.1001/archgenpsychiatry.2010.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corkum P, Tannock R, Moldofsky H. Sleep disturbances in children with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(6):637–646. doi: 10.1097/00004583-199806000-00014. http://dx.doi.org/10.1097/00004583-199806000-00014. [DOI] [PubMed] [Google Scholar]
- Cole WR, Mostofsky SH, Larson JC, Denckla MB, Mahone EM. Age-related changes in motor subtle signs among girls and boys with ADHD. Neurology. 2008;71(19):1514–1520. doi: 10.1212/01.wnl.0000334275.57734.5f. http://dx.doi.org/10.1212/01.wnl.0000334275.57734.5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman D, Walker JS, Lee J, Friesen BJ, Squire PN. Children's beliefs about causes of childhood depression and ADHD: a study of stigmatization. Psychiatric Services. 2009;60:950–957. doi: 10.1176/ps.2009.60.7.950. [DOI] [PubMed] [Google Scholar]
- Cooper WO, Habel LA, Sox CM, Chan KA, Arbogast PG, Cheetham TC, et al. ADHD drugs and serious cardiovascular events in children and young adults. The New England Journal of Medicine. 2011;365:1896–1904. doi: 10.1056/NEJMoa1110212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cortese S, Angriman M, Maffeis C, Isnard P, Konofal E, Lecendreux M, et al. Attention-deficit/hyperactivity disorder (ADHD) and obesity: a systematic review of the literature. Critical Reviews in Food Science and Nutrition. 2008;48:524–537. doi: 10.1080/10408390701540124. [DOI] [PubMed] [Google Scholar]
- Cortese S, Faraone SV, Konofal E, Lecendreux M. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:894–908. doi: 10.1097/CHI.0b013e3181ac09c9. [DOI] [PubMed] [Google Scholar]
- Cortese S, Penalver CM. Comorbidity between ADHD and obesity: exploring shared mechanisms and clinical implications. Postgraduate Medicine. 2010;122:88–96. doi: 10.3810/pgm.2010.09.2205. [DOI] [PubMed] [Google Scholar]
- Cortese S, Vincenzi B. Obesity and ADHD: clinical and neurobiological implications. Current Topics in Behavioral Neurosciences. 2012;9:199–218. doi: 10.1007/7854_2011_154. [DOI] [PubMed] [Google Scholar]
- Cotlar MJ. Attention deficit hyperactivity disorder (ADHD)-life insurance implications. Journal of Insurance Medicine. 2003;35:51–56. [PubMed] [Google Scholar]
- Counts CA, Nigg JT, Stawicki JA, Rappley MD, von Eye A. Family adversity in DSM-IV ADHD combined and inattentive subtypes and associated disruptive behavior problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:690–698. doi: 10.1097/01.chi.0000162582.87710.66. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The impact of inadequate sleep on children's daytime cognitive function. Seminars in Pediatric Neurology. 1996;3(1):44–50. doi: 10.1016/s1071-9091(96)80028-3. [DOI] [PubMed] [Google Scholar]
- De Graaf R, Kessler RC, Fayyad J, Ten, Have M, Alonso J, Angermeyer M, et al. The prevalence and effects of adult attention-deficit/hyperactivity disorder (ADHD) on the performance of workers: Results from the WHO World Mental Health Survey Initiative. Occupational and Environmental Medicine. 2008;65:835–842. doi: 10.1136/oem.2007.038448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dempsey A, Dyehouse J, Schafer J. The relationship between executive function, AD/HD, overeating, and obesity. Western Journal of Nursing Research. 2011;33:609–629. doi: 10.1177/0193945910382533. [DOI] [PubMed] [Google Scholar]
- Ek U, Westerlund J, Holmberg K, Fernell E. Self-esteem in children with attention and/or learning deficits: the importance of gender. Acta Paediatrica. 2008;97:1125–1130. doi: 10.1111/j.1651-2227.2008.00894.x. [DOI] [PubMed] [Google Scholar]
- Elia J, Vetter VL. Cardiovascular effects of medications for the treatment of attention-deficit hyperactivity disorder: what is known and how should it influence prescribing in children? Paediatr Drugs. 2010;12:165–175. doi: 10.2165/11532570-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/ hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of General Psychiatry. 2007;64(10):1145–1152. doi: 10.1001/archpsyc.64.10.1145. http://dx.doi.org/10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Escobar R, Soutullo CA, Hervas A, Gastaminza X, Polavieja P, Gilaberte I. Worse quality of life for children with newly diagnosed attention-deficit/ hyperactivity disorder, compared with asthmatic and healthy children. Pediatrics. 2005;116:e364–e369. doi: 10.1542/peds.2005-0386. [DOI] [PubMed] [Google Scholar]
- Evangelista NM, Owens JS, Golden CM, Pelham WE., Jr The positive illusory bias: do inflated self-perceptions in children with ADHD generalize to perceptions of others? J Abnorm Child Psychol. 2008 Jul 36;(5):779–791. doi: 10.1007/s10802-007-9210-8. http://dx.doi.org/10.1007/s10802-007-9210-8 Epub 2008 Jan 10. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Lehman BK, Spencer T, Norman D, Seidman LJ, et al. Intellectual performance and school failure in children with attention deficit hyperactivity disorder and in their siblings. Journal of Abnormal Psychology. 1993;102:616–623. doi: 10.1037/0021-843X.102.4.616. [DOI] [PubMed] [Google Scholar]
- Faraone SV, Biederman J, Morley CP, Spencer TJ. Effect of stimulants on height and weight: A review of the literature. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:994–1009. doi: 10.1097/CHI.ObO13e31817eOea7. [DOI] [PubMed] [Google Scholar]
- Farmer JE, Peterson L. Injury risk factors in children with attention deficit hyperactivity disorder. Health Psychology. 1995;14:325–332. doi: 10.1037/0278-6133.14.4.325. [DOI] [PubMed] [Google Scholar]
- Flory K, Molina BS, Pelham WE, Jr, Gnagy E, Smith B. Childhood ADHD predicts risky sexual behavior in young adulthood. Journal of Clinical Child and Adolescent Psychology. 2006;35(4):571–577. doi: 10.1207/s15374424jccp3504_8. http://dx.doi.org/10.1207/s15374424jccp3504_8. [DOI] [PubMed] [Google Scholar]
- Friedman HS, Tucker JS, Schwartz JE, Tomlinson-Keasey C, Martin LR, Wingard DL, et al. Psychosocial and behavioral predictors of longevity. The aging and death of the "termites". American Psychologist. 1995;50:69–78. doi: 10.1037//0003-066x.50.2.69. (Ref ID: 3049) [DOI] [PubMed] [Google Scholar]
- Fritz KM, Butz C. Attention deficit/hyperactivity disorder and pediatric burn injury: important considerations regarding premorbid risk. Current Opinion in Pediatrics. 2007;19:565–569. doi: 10.1097/MOP.0b013e3282ef498c. [DOI] [PubMed] [Google Scholar]
- Fuemmeler BF, Ostbye T, Yang C, McClernon FJ, Kollins SH. Association between attention-deficit/hyperactivity disorder symptoms and obesity and hypertension in early adulthood: A population-based study. International Journal of Obesity. 2010;35:852–862. doi: 10.1038/ijo.2010.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher R, Blader J. The diagnosis and neuropsychological assessment of adult attention deficit/hyperactivity disorder. Scientific study and practical guidelines. Annals of the New York Academy of Sciences. 2001;931:148–171. doi: 10.1111/j.1749-6632.2001.tb05778.x. [DOI] [PubMed] [Google Scholar]
- Gapin J, Etnier JL. The relationship between physical activity and executive function performance in children with attention-deficit hyperactivity disorder. Journal of Sport & Exercise Psychology. 2010;32:753–763. doi: 10.1123/jsep.32.6.753. [DOI] [PubMed] [Google Scholar]
- Garzon DL, Huang H, Todd RD. Do attention deficit/hyperactivity disorder and oppositional defiant disorder influence preschool unintentional injury risk? Archives of Psychiatric Nursing. 2008;22:288–296. doi: 10.1016/j.apnu.2007.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman DW. The consequences of attention-deficit/hyperactivity disorder in adults. J Psychiatr Pract. 2007 Sep 13;(5):318–327. doi: 10.1097/01.pra.0000290670.87236.18. Review. [DOI] [PubMed] [Google Scholar]
- Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- Goodman G, Gerstadt C, Pfeffer CR, Stroh M, Valdez A. ADHD and aggression as correlates of suicidal behavior in assaultive prepubertal psychiatric inpatients. Suicide & Life-Threatening Behavior. 2008;38:46–59. doi: 10.1521/suli.2008.38.1.46. [DOI] [PubMed] [Google Scholar]
- Gould MS, Walsh BT, Munfakh JL, Kleinman M, Duan N, Olfson M, et al. Sudden death and use of stimulant medications in youths. The American Journal of Psychiatry. 2009;166:992–1001. doi: 10.1176/appi.ajp.2009.09040472. [DOI] [PubMed] [Google Scholar]
- Gray KM, Upadhyaya HP. Tobacco smoking in individuals with attention-deficit hyperactivity disorder: Epidemiology and pharmacological approaches to cessation. CNS Drugs. 2009;23:661–668. doi: 10.2165/00023210-200923080-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guevara J, Lozano P, Wickizer T, Mell L, Gephart H. Utilization and cost of health care services for children with attention-deficit/hyperactivity disorder. Pediatrics. 2001;108:71–78. doi: 10.1542/peds.108.1.71. [DOI] [PubMed] [Google Scholar]
- Haavisto A, Sourander A, Multimaki P, Parkkola K, Santalahti P, Helenius H, et al. Factors associated with ideation and acts of deliberate self-harm among 18-year-old boys. A prospective 10-year follow-up study. Social Psychiatry and Psychiatric Epidemiology. 2005;40:912–921. doi: 10.1007/s00127-005-0966-2. [DOI] [PubMed] [Google Scholar]
- Harpin VA. The effect of ADHD on the life of an individual, their family, and community from preschool to adult life. Archives of Disease in Childhood. 2005;90(Suppl. 1) doi: 10.1136/adc.2004.059006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey WJ, Reid G, Bloom GA, Staples K, Grizenko N, Mbekou V, et al. Physical activity experiences of boys with and without ADHD. Adapted Physical Activity Quarterly. 2009;26:131–150. doi: 10.1123/apaq.26.2.131. [DOI] [PubMed] [Google Scholar]
- Hazell P. Does the treatment of mental disorders in childhood lead to a healthier adulthood? Current Opinion in Psychiatry. 2007;20:315–318. doi: 10.1097/YCO.0b013e3281a7368d. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP. Academic underachievement, attention deficits, and aggression: Comorbidity and implications for intervention. Journal of Consulting and Clinical Psychology. 1992;60:893–903. doi: 10.1037//0022-006x.60.6.893. [DOI] [PubMed] [Google Scholar]
- Hinshaw SP, Owens EB, Zalecki C, Huggins SP, Montenegro-Nevado AJ, Schrodek E, et al. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: Continuing impairment includes elevated risk for suicide attempts and self-injury. Journal of Consulting and Clinical Psychology. 2012;80:1041–1051. doi: 10.1037/a0029451. http://dx.doi.org/10.1037/a0029451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosain GM, Berenson AB, Tennen H, Bauer LO, Wu ZH. Attention deficit hyperactivity symptoms and risky sexual behavior in young adult women. Journal of Women's Health (Larchmt) 2012;21(4):463–468. doi: 10.1089/jwh.2011.2825. http://dx.doi.org/10.1089/jwh.2011.2825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard AL, Robinson M, Smith GJ, Ambrosini GL, Piek JP, Oddy WH. ADHD is associated with a “Western” dietary pattern in adolescents. Journal of Attention Disorders. 2011;15:403–411. doi: 10.1177/1087054710365990. [DOI] [PubMed] [Google Scholar]
- Hoza B. Peer functioning in children with ADHD. Journal of Pediatric Psychology. 2007;32:655–663. doi: 10.1093/jpepsy/jsm024. [DOI] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Hinshaw SP, Arnold LE, Pelham WE, Jr, Molina BS, et al. Self-perceptions of competence in children with ADHD and comparison children. Journal of Consulting and Clinical Psychology. 2004;72:382–391. doi: 10.1037/0022-006X.72.3.382. [DOI] [PubMed] [Google Scholar]
- Hoza B, Mrug S, Gerdes AC, Hinshaw SP, Bukowski WM, Gold JA, et al. What aspects of peer relationships are impaired in children with attention-deficit/ hyperactivity disorder? Journal of Consulting and Clinical Psychology. 2005;73:411–423. doi: 10.1037/0022-006X.73.3.411. [DOI] [PubMed] [Google Scholar]
- Hoza B, Gerdes AC, Mrug S, Hinshaw SP, Bukowski WM, Gold JA, et al. Peer-assessed outcomes in the multimodal treatment study of children with attention deficit hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2005;34(1):74–86. doi: 10.1207/s15374424jccp3401_7. http://dx.doi.org/10.1207/s15374424jccp3401_7. [DOI] [PubMed] [Google Scholar]
- Huggins SP, Rooney ME, Chronis-Tuscano A. Risky sexual behavior among college students with ADHD: Is the mother-child relationship protective? Journal of Attention Disorders. 2012;20:1–11. doi: 10.1177/1087054712459560. http://dx.doi.org/10.1177/1087054712459560. [DOI] [PubMed] [Google Scholar]
- Hurt EA, Hoza B, Pelham WE., Jr Parenting, family loneliness, and peer functioning in boys with attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2007;35(4):543–555. doi: 10.1007/s10802-007-9111-x. http://dx.doi.org/10.1007/s10802-007-9111-x. [DOI] [PubMed] [Google Scholar]
- Klein RG, Mannuzza S, Olazagasti MA, Roizen E, Hutchison JA, Lashua EC, et al. Clinical and functional outcome of childhood attention-deficit/ hyperactivity disorder 33 years later. Archives of General Psychiatry. 2012:1–9. doi: 10.1001/archgenpsychiatry.2012.271. http://dx.doi.org/10.1001/archgenpsychiatry.2012.2711378851 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Impey M, Heun R. Completed suicide, ideation and attempt in attention deficit hyperactivity disorder. Acta Psychiatrica Scandinavica. 2012;125:93–102. doi: 10.1111/j.1600-0447.2011.01798.x. [DOI] [PubMed] [Google Scholar]
- James A, Lai FH, Dahl C. Attention deficit hyperactivity disorder and suicide: A review of possible associations. Acta Psychiatrica Scandinavica. 2004;110:408–415. doi: 10.1111/j.1600-0447.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- Jerome L, Segal A, Habinski L. What we know about ADHD and driving risk: A literature review, meta-analysis and critique. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2006;15:105–125. [PMC free article] [PubMed] [Google Scholar]
- Jester JM, Nigg JT, Buu A, Puttler LI, Glass JM, Heitzeg MM, et al. Trajectories of childhood aggression and inattention/hyperactivity: Differential effects on substance abuse in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:1158–1165. doi: 10.1097/CHI.0b013e3181825a4e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay GG, Michaels MA, Pakull B. Simulated driving changes in young adults with ADHD receiving mixed amphetamine salts extended release and atomoxetine. Journal of Attention Disorders. 2009;12:316–329. doi: 10.1177/1087054708322986. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Gorlyn M, Oquendo MA, Burke AK, Mann JJ. Attention deficit in depressed suicide attempters. Psychiatry Research. 2008;159:7–17. doi: 10.1016/j.psychres.2007.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Mutyala B, Agiovlasitis S, Fernhall B. Health behaviors and obesity among US children with attention deficit hyperactivity disorder by gender and medication use. Preventive Medicine. 2011;52:218–222. doi: 10.1016/j.ypmed.2011.01.003. [DOI] [PubMed] [Google Scholar]
- Kollins SH. Abuse liability of medications used to treat attention-deficit/ hyperactivity disorder (ADHD) The American Journal on Addictions. 2007;16(Suppl. 1):35–44. doi: 10.1080/10550490601082775. [DOI] [PubMed] [Google Scholar]
- Kramer AF, Hahn S, Cohen NJ, Banich MT, McAuley E, Harrison CR, et al. Ageing, fitness and neurocognitive function. Nature. 1999;400:418–419. doi: 10.1038/22682. [DOI] [PubMed] [Google Scholar]
- Krause I, Cleper R, Kovalski Y, Sinai L, Davidovits M. Changes in behavior as an early symptom of renovascular hypertension in children. Pediatric Nephrolo-gy. 2009;24:2271–2274. doi: 10.1007/s00467-009-1205-y. [DOI] [PubMed] [Google Scholar]
- Küpper T, Haavik J, Drexler H, Ramos-Quiroga JA, Wermelskirchen D, Prutz C, Schauble B. The negative impact of attention-deficit/hyperactivity disorder on occupational health in adults and adolescents. Int Arch Occup Environ Health. 2012 Nov 85;(8):837–847. doi: 10.1007/s00420-012-0794-0. Epub 2012 Jul 3. [DOI] [PubMed] [Google Scholar]
- Lambert N. The contribution of childhood ADHD, conduct problems, and stimulant treatment to adolescent and adult tobacco and psychoactive substance abuse. Ethical Human Psychology and Psychiatry. 2005;7:197–221. [Google Scholar]
- Lecendreux M, Cortese S. Sleep problems associated with ADHD: A review of current therapeutic options and recommendations for the future. Expert Review of Neurotherapeutics. 2007;7(12):1799–1806. doi: 10.1586/14737175.7.12.1799. http://dx.doi.org/10.1586/14737175.7.12.1799. [DOI] [PubMed] [Google Scholar]
- Lee SS, Humphreys KL, Flory K, Liu R, Glass K. Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: A meta-analytic review. Clinical Psychology Review. 2011;31(3):328–341. doi: 10.1016/j.cpr.2011.01.006. http://dx.doi.org/10.1016/j.cpr.2011.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leibson CL, Long KH. Economic implications of attention-deficit hyperac-tivity disorder for healthcare systems. PharmacoEconomics. 2003;21:1239–1262. doi: 10.2165/00019053-200321170-00002. [DOI] [PubMed] [Google Scholar]
- Levitt Katz LE, Swami S, Abraham M, Murphy KM, Jawad AF, Knight-Menci H, et al. Neuropsychiatric disorders at the presentation of type 2 diabetes mellitus in children. Pediatric Diabetes. 2005;6:84–89. doi: 10.1111/j.1399-543X.2005.00105.x. [DOI] [PubMed] [Google Scholar]
- Loeber R, Hay D. Key issues in the development of aggression and violence from childhood to early adulthood. Annual Review of Psychology. 1997;48:371–410. doi: 10.1146/annurev.psych.48.1.371. http://dx.doi.org/10.1146/annurev.psych.48.1.371. [DOI] [PubMed] [Google Scholar]
- Macneil LK, Xavier P, Garvey MA, Gilbert DL, Ranta ME, Denckla MB, et al. Quantifying excessive mirror overflow in children with attention-deficit/ hyperactivity disorder. Neurology. 2011;76(7):622–628. doi: 10.1212/WNL.0b013e31820c3052. http://dx.doi.org/10.1212/WNL.0b013e31820c3052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Abikoff H, Moulton JL., III Significance of childhood conduct problems to later development of conduct disorder among children with ADHD: A prospective follow-up study. Journal of Abnormal Child Psychology. 2004;32:565–573. doi: 10.1023/b:jacp.0000037784.80885.1a. [DOI] [PubMed] [Google Scholar]
- Marcus SC, Wan GJ, Zhang HF, Olfson M. Injury among stimulant-treated youth with ADHD. Journal of Attention Disorders. 2008;12:64–69. doi: 10.1177/1087054707305168. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nigg JT, Wong MM, Fitzgerald HE, Jester JM, Puttler LI, et al. Childhood and adolescent resiliency, regulation, and executive functioning in relation to adolescent problems and competence in a high-risk sample. Development and Psychopathology. 2007;19:541–563. doi: 10.1017/S0954579407070265. [DOI] [PubMed] [Google Scholar]
- Martel MM, Nikolas M, Jernigan K, Friderici K, Waldman I, Nigg JT. The dopamine receptor D4 gene (DRD4) moderates family environmental effects on ADHD. Journal of Abnormal Child Psychology. 2011;39:1–10. doi: 10.1007/s10802-010-9439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JK, Pescosolido BA, Olafsdottir S, McLeod JD. The construction of fear: Americans' preferences for social distance from children and adolescents with mental health problems. Journal of Health and Social Behavior. 2007;48:50–67. doi: 10.1177/002214650704800104. [DOI] [PubMed] [Google Scholar]
- Maxson RT, Lawson KA, Pop R, Yuma-Guerrero P, Johnson KM. Screening for attention-deficit/hyperactivity disorder in a select sample of injured and uninjured pediatric patients. Journal of Pediatric Surgery. 2009;44:743–748. doi: 10.1016/j.jpedsurg.2008.08.003. [DOI] [PubMed] [Google Scholar]
- McBurnett K, Pfiffner LJ, Frick PJ. Symptom properties as a function of ADHD type: An argument for continued study of sluggish cognitive tempo. Journal of Abnormal Child Psychology. 2001;29:207–213. doi: 10.1023/a:1010377530749. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use and diversion of prescription stimulant medication. Journal of Psychoactive Drugs. 2006;38:43–56. doi: 10.1080/02791072.2006.10399827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy S, Cranswick N, Potts L, Taylor E, Wong IC. Mortality associated with attention-deficit hyperactivity disorder (ADHD) drug treatment: A retrospective cohort study of children, adolescents and young adults using the general practice research database. Drug Safety. 2009;32:1089–1096. doi: 10.2165/11317630-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Medina JA, Netto TL, Muszkat M, Medina AC, Botter D, Orbetelli R, et al. Exercise impact on sustained attention of ADHD children, methylpheni-date effects. Attention Deficit and Hyperactivity Disorders. 2010;2:49–58. doi: 10.1007/s12402-009-0018-y. [DOI] [PubMed] [Google Scholar]
- Merrill RM, Lyon JL, Baker RK, Gren LH. Attention deficit hyperactivity disorder and increased risk of injury. Advances in Medical Sciences. 2009;54:20–26. doi: 10.2478/v10039-009-0022-7. [DOI] [PubMed] [Google Scholar]
- Mikami AY, Jack A, Emeh CC, Stephens HF. Parental influence on children with attention-deficit/hyperactivity disorder: I. Relationships between parent behaviors and child peer status. Journal of Abnormal Child Psychology. 2010;38(6):721–736. doi: 10.1007/s10802-010-9393-2. http://dx.doi.org/10.1007/s10802-010-9393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikami AY, Lorenzi J. Gender and conduct problems predict peer functioning among children with attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2011;40(5):777–786. doi: 10.1080/15374416.2011.597089. http://dx.doi.org/10.1080/15374416.2011.597089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mrug S, Molina BS, Hoza B, Gerdes AC, Hinshaw SP, Hechtman L, et al. Peer rejection and friendships in children with attention-deficit/hyperactivity disorder: Contributions to long-term outcomes. Journal of Abnormal Child Psychology. 2012;40(6):1013–1026. doi: 10.1007/s10802-012-9610-2. http://dx.doi.org/10.1007/s10802-012-9610-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nigg JT. What causes ADHD?: Understanding what goes wrong and why. New York, NY: The Guilford Press; 2006. [Google Scholar]
- Nikolas M, Friderici K, Waldman I, Jernigan K, Nigg JT. Gene×environment interactions for ADHD: synergistic effect of 5HTTLPR genotype and youth appraisals of inter-parental conflict. Behavioral and Brain Functions. 2010;6:23. doi: 10.1186/1744-9081-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolas M, Klump KL, Burt SA. Youth appraisals of inter-parental conflict and genetic and environmental contributions to attention-deficit hyperactivity disorder: Examination of G×E effects in a twin sample. Journal of Abnormal Child Psychology. 2011;40:543–554. doi: 10.1007/s10802-011-9583-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norvilitis JM, Scime M, Lee JS. Courtesy stigma in mothers of children with attention-deficit/hyperactivity disorder: A preliminary investigation. Journal of Attention Disorders. 2002;6:61–68. doi: 10.1177/108705470200600202. [DOI] [PubMed] [Google Scholar]
- Odent M. Attention deficit hyperactivity disorder (ADHD) and obesity: Two facets of the same disease? Med Hypotheses. 2010;74:139–141. doi: 10.1016/j.mehy.2009.07.020. [DOI] [PubMed] [Google Scholar]
- Oliver ML, Nigg JT, Cassavaugh ND, Backs RW. Behavioral and cardiovascular responses to frustration during simulated driving tasks in young adults with and without attention disorder symptoms. Journal of Attention Disorders. 2011;16:478–490. doi: 10.1177/1087054710397132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JA. The ADHD and sleep conundrum: A review. Journal of Developmental and Behavioral Pediatrics. 2005;26:312–322. doi: 10.1097/00004703-200508000-00011. [DOI] [PubMed] [Google Scholar]
- Owens JA. Sleep disorders and attention-deficit/hyperactivity disorder. Current Psychiatry Reports. 2008;10:439–444. doi: 10.1007/s11920-008-0070-x. [DOI] [PubMed] [Google Scholar]
- Owens J, Gruber R, Brown T, Corkum P, Cortese S, O'Brien L, et al. Future research directions in sleep and ADHD: Report of a Consensus Working Group. Journal of Attention Disorders. 2012;20:1–15. doi: 10.1177/1087054712457992. http://dx.doi.org/10.1177/1087054712457992. [DOI] [PubMed] [Google Scholar]
- Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM. A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clin Child Fam Psychol Rev. 2007 Dec 10;(4):335–351. doi: 10.1007/s10567-007-0027-3. Review. [DOI] [PubMed] [Google Scholar]
- Pagoto SL, Curtin C, Lemon SC, Bandini LG, Schneider KL, Bodenlos JS, et al. Association between adult attention deficit/hyperactivity disorder and obesity in the US population. Obesity. 2009;17:539–544. doi: 10.1038/oby.2008.587. (Silver.Spring) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pastor PN, Reuben CA. Identified attention-deficit/hyperactivity disorder and medically attended, nonfatal injuries: US school-age children, 1997–2002. Ambulatory Pediatrics. 2006;6:38–44. doi: 10.1016/j.ambp.2005.07.002. [DOI] [PubMed] [Google Scholar]
- Paternite CE, Loney J, Salisbury H, Whaley MA. Childhood inattention-overactivity, aggression, and stimulant medication history as predictors of young adult outcomes. Journal of Child and Adolescent Psychopharmacology. 1999;9:169–184. doi: 10.1089/cap.1999.9.169. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Milich R. Peer relations in children with hyperactivity/attention deficit disorder. Journal of Learning Disabilities. 1984;17:560–567. doi: 10.1177/002221948401700911. [DOI] [PubMed] [Google Scholar]
- Perera H, Fernando SM, Yasawardena AD, Karunaratne I. Prevalence of attention deficit hyperactivity disorder (ADHD) in children presenting with self-inserted nasal and aural foreign bodies. International Journal of Pediatric Oto-rhinolaryngology. 2009;73:1362–1364. doi: 10.1016/j.ijporl.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Pescosolido BA, Fettes DL, Martin JK, Monahan J, McLeod JD. Perceived dangerousness of children with mental health problems and support for coerced treatment. Psychiatric Services. 2007;58:619–625. doi: 10.1176/ps.2007.58.5.619. [DOI] [PubMed] [Google Scholar]
- Pine DS, Goldstein RB, Wolk S, Weissman MM. The association between childhood depression and adulthood body mass index. Pediatrics. 2001;107:1049–1056. doi: 10.1542/peds.107.5.1049. [DOI] [PubMed] [Google Scholar]
- Pingault JB, Cote SM, Galera C, Genolini C, Falissard B, Vitaro F, et al. Childhood trajectories of inattention, hyperactivity and oppositional behaviors and prediction of substance abuse/dependence: A 15-year longitudinal population-based study. Molecular Psychiatry. 2012 doi: 10.1038/mp.2012.87. http://dx.doi.org/10.1038/mp.2012.87mp201287 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podolski C-L, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. Journal of Clinical Child Psychology. 2001;30:503–513. doi: 10.1207/S15374424JCCP3004_07. [DOI] [PubMed] [Google Scholar]
- Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: A systematic review and metaregression analysis. The American Journal of Psychiatry. 2007;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942. http://dx.doi.org/10.1176/appi.ajp.164.6.942. [DOI] [PubMed] [Google Scholar]
- Potter AS, Bucci DJ, Newhouse PA. Manipulation of nicotinic acetylcho-line receptors differentially affects behavioral inhibition in human subjects with and without disordered baseline impulsivity. Psychopharmacology. 2012;220(2):331–340. doi: 10.1007/s00213-011-2476-0. http://dx.doi.org/10.1007/s00213-011-2476-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin C. Medical and nonmedical stimulant use among adolescents: From sanctioned to unsanctioned use. CMAJ. 2001;165:1039–1044. [PMC free article] [PubMed] [Google Scholar]
- Puder JJ, Munsch S. Psychological correlates of childhood obesity. International Journal of Obesity. 2010;34(Suppl. 2):S37–S43. doi: 10.1038/ijo.2010.238. [DOI] [PubMed] [Google Scholar]
- Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm. Findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278:823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- Ritalin LA. [package insert] East Hanover, NJ: Novartis Pharmaceuticals Corporation; 2010. [Google Scholar]
- Rucklidge J, Brown D, Crawford S, Kaplan B. Attributional styles and psy-chosocial functioning of adults with ADHD: Practice issues and gender differences. Journal of Attention Disorders. 2007;10:288–298. doi: 10.1177/1087054706289942. [DOI] [PubMed] [Google Scholar]
- Rutter M, Kim-Cohen J, Maughan B. Continuities and discontinuities in psychopathology between childhood and adult life. Journal of Child Psychology and Psychiatry. 2006;47:276–295. doi: 10.1111/j.1469-7610.2006.01614.x. [DOI] [PubMed] [Google Scholar]
- Secnik K, Swensen A, Lage MJ. Comorbidities and costs of adult patients diagnosed with attention-deficit hyperactivity disorder. PharmacoEconomics. 2005;23:93–102. doi: 10.2165/00019053-200523010-00008. [DOI] [PubMed] [Google Scholar]
- Shinawi M, Sahoo T, Maranda B, Skinner SA, Skinner C, Chinault C, et al. 11p14.1 microdeletions associated with ADHD, autism, developmental delay, and obesity. American Journal of Medical Genetics. Part A. 2011;155A:1272–1280. doi: 10.1002/ajmg.a.33878. [DOI] [PubMed] [Google Scholar]
- Simon V, Czobor P, Balint S, Meszaros A, Bitter I. Prevalence and correlates of adult attention-deficit hyperactivity disorder: Meta-analysis. The British Journal of Psychiatry. 2009;194(3):204–211. doi: 10.1192/bjp.bp.107.048827. http://dx.doi.org/10.1192/bjp.bp.107.048827. [DOI] [PubMed] [Google Scholar]
- Smith AL, Hoza B, Linnea K, McQuade JD, Tomb M, Vaughn AJ, et al. Pilot physical activity intervention reduces severity of ADHD symptoms in young children [Epub] Journal of Attention Disorders. 2011;17:70–82. doi: 10.1177/1087054711417395. [DOI] [PubMed] [Google Scholar]
- Sourander A, Klomek AB, Niemela S, Haavisto A, Gyllenberg D, Helenius H, et al. Childhood predictors of completed and severe suicide attempts: Findings from the Finnish 1981 Birth Cohort Study. Archives of General Psychiatry. 2009;66:398–406. doi: 10.1001/archgenpsychiatry.2009.21. [DOI] [PubMed] [Google Scholar]
- Spencer TJ, Kratochvil CJ, Sangal RB, Saylor KE, Bailey CE, Dunn DW, et al. Effects of atomoxetine on growth in children with attention-deficit/ hyperactivity disorder following up to five years of treatment. Journal of Child and Adolescent Psychopharmacology. 2007;17:689–700. doi: 10.1089/cap.2006.0100. [DOI] [PubMed] [Google Scholar]
- Spiegel R, DeVos JE. Central effects of guanfacine and clonidine during wakefulness and sleep in healthy subjects. British Journal of Clinical Pharmacology. 1980;10(Suppl. 1):165S–168S. doi: 10.1111/j.1365-2125.1980.tb04925.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruyt K, Gozal D. Sleep disturbances in children with attention-deficit/ hyperactivity disorder. Expert Review of Neurotherapeutics. 2011;11(4):565–577. doi: 10.1586/ern.11.7. http://dx.doi.org/10.1586/ern.11.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stavro GM, Ettenhofer ML, Nigg JT. Executive functions and adaptive functioning in young adult attention-deficit/hyperactivity disorder. Journal of the International Neuropsychological Society. 2007;13:324–334. doi: 10.1017/S1355617707070348. [DOI] [PubMed] [Google Scholar]
- Stiefel G, Besag FM. Cardiovascular effects of methylphenidate, amphetamines and atomoxetine in the treatment of attention-deficit hyperactivity disorder. Drug Safety. 2010;33:821–842. doi: 10.2165/11536380-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Surman CB, Adamson JJ, Petty C, Biederman J, Kenealy DC, Levine M, et al. Association between attention-deficit/hyperactivity disorder and sleep impairment in adulthood: Evidence from a large controlled study. The Journal of Clinical Psychiatry. 2009;70:1523–1529. doi: 10.4088/JCP.08m04514. [DOI] [PubMed] [Google Scholar]
- Swanson JM, Elliott GR, Greenhill LL, Wigal T, Arnold LE, Vitiello B, et al. Effects of stimulant medication on growth rates across 3 years in the MTA follow-up. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46:1014–1026. doi: 10.1097/chi.0b013e3180686d7e. [DOI] [PubMed] [Google Scholar]
- Swanson EN, Owens EB, Hinshaw SP. Is the positive illusory bias illusory? Examining discrepant self-perceptions of competence in girls with ADHD. J Abnorm Child Psychol. 2012 Aug;40(6):987–998. doi: 10.1007/s10802-012-9615-x. http://dx.doi.org/10.1007/s10802-012-9615-x. [DOI] [PubMed] [Google Scholar]
- Swensen A, Birnbaum HG, Ben, Hamadi R, Greenberg P, Cremieux PY, Secnik K. Incidence and costs of accidents among attention-deficit/hyperactivity disorder patients. The Journal of Adolescent Health. 2004;35:346–349. [PubMed] [Google Scholar]
- Taurines R, Schmitt J, Renner T, Conner AC, Warnke A, Romanos M. Developmental comorbidity in attention-deficit/hyperactivity disorder. Attention Deficit and Hyperactivity Disorders. 2010;2:267–289. doi: 10.1007/s12402-010-0040-0. [DOI] [PubMed] [Google Scholar]
- van Emmerik-van Oortmerssen K, van de Glind G, van den Brink W, Smit F, Crunelle CL, Swets M, et al. Prevalence of attention-deficit hyperactivity disorder in substance use disorder patients: a meta-analysis and meta-regression analysis. Drug and Alcohol Dependence. 2012;122(1–2):11–19. doi: 10.1016/j.drugalcdep.2011.12.007. http://dx.doi.org/10.1016/j.drugalcdep.2011.12.007. [DOI] [PubMed] [Google Scholar]
- Vyvanse. [package insert] Wayne, PA: Shire US Inc.; 2011. [Google Scholar]
- Walker JS, Coleman D, Lee J, Squire PN, Friesen BJ. Children's stigma-tization of childhood depression and ADHD: Magnitude and demographic variation in a national sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:912–920. doi: 10.1097/CHI.0b013e318179961a. [DOI] [PubMed] [Google Scholar]
- Waring ME, Lapane KL. Overweight in children and adolescents in relation to attention-deficit/hyperactivity disorder: Results from a national sample. Pediatrics. 2008;122:e1–e6. doi: 10.1542/peds.2007-1955. [DOI] [PubMed] [Google Scholar]
- Weiss MD, Salpekar J. Sleep problems in the child with attention-deficit hyperactivity disorder: Defining aetiology and appropriate treatments. CNS Drugs. 2010;24:811–828. doi: 10.2165/11538990-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Wells KC, Epstein JN, Hinshaw SP, Conners CK, Klaric J, Abikoff HB, et al. Parenting and family stress treatment outcomes in attention deficit hyperac-tivity disorder (ADHD): An empirical analysis in the MTA study. Journal of Abnormal Child Psychology. 2000;28:543–553. doi: 10.1023/a:1005131131159. [DOI] [PubMed] [Google Scholar]
- Wigal SB. Efficacy and safety limitations of attention deficit hyperactivity disorder pharmacotherapy in pediatric patients. Journal of Pediatrics. 2009;154:S13–S21. doi: 10.2165/00023210-200923000-00004. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Adamson J, Monuteaux MC, Faraone SV, Schillinger M, Westerberg D, et al. Effect of prior stimulant treatment for attention-deficit/hyperactivity disorder on subsequent risk for cigarette smoking and alcohol and drug use disorders in adolescents. Archives of Pediatrics & Adolescent Medicine. 2008;162:916–921. doi: 10.1001/archpedi.162.10.916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilens TE, Adamson J, Sgambati S, Whitley J, Santry A, Monuteaux MC, et al. Do individuals with ADHD self-medicate with cigarettes and substances of abuse? Results from a controlled family study of ADHD. The American Journal on Addictions. 2007;16(Suppl. 1):14–21. doi: 10.1080/10550490601082742. http://dx.doi.org/10.1080/10550490601082742 quiz 22–13. [DOI] [PubMed] [Google Scholar]
- Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;111:179–185. doi: 10.1542/peds.111.1.179. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry. 2005;57(11):1336–1346. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Yoon SY, Jain U, Shapiro C. Sleep in attention-deficit/hyperactivity disorder in children and adults: Past, present, and future. Sleep Medicine Reviews. 2012;16(4):371–388. doi: 10.1016/j.smrv.2011.07.001. http://dx.doi.org/10.1016/j.smrv.2011.07.001S1087-0792(11)00071-2 (pii) [DOI] [PubMed] [Google Scholar]