Abstract
The tumour microenvironment, long considered as determining cancer development, still offers research fields to define hallmarks of cancer. An early key-step, the “angiogenic switch”, allows tumour growth. Pathologic angiogenesis is a cancer hallmark as it features results of tumour-specific properties that can be summarised as a response to hypoxia. The hypoxic state occurs when the tumour mass reaches a volume sufficient not to permit oxygen diffusion inside the tumour centre. Thus tumour cells turn on adaptation mechanisms to the low pO2 level, inducing biochemical responses in terms of cytokines/chemokines/receptors and consequently recruitment of specific cell types, as well as cell-selection inside the tumour. Moreover, these changes are orchestrated by the microRNA balance strongly reflecting the hypoxic milieu and mediating the cross-talk between endothelial and tumour cells. MicroRNAs control of the endothelial precursor-vascular settings shapes the niche for selection of cancer stem cells.
Keywords: angiogenesis, cancer stem cell, endothelial precursor cell, hypoxia, microRNA
Introduction
As cancer stem cell (CSC) is a term to describe the most resistant and quiescent subpopulation of cells that, among the growing tumour cells, may be resistant to treatments and are able to aggressively reconstitute the malignant disease, these cells are also called cancer-initiating cells. Deciphering the molecular mechanisms they to use to dedifferentiate and to resist the harsh conditions resulting from the therapies is a challenge for new anticancer approaches. The cancer stem cells are not highly different from other stem cells, which makes their targeting difficult. In this aspect, the place and conditions in which they originate inside the tumour mass as well as their microenvironmental milieu remain a question of controversy. As they often appear to be associated with endothelial cells of the micro-vessels, their niche is described as non-hypoxic while they display resistance to hypoxia [1]. They also are the hypoxia-resistant cells that recruit endothelial cells to form the tumour vasculature both from sprouting preformed vessels as well as from bone marrow and/or vessel wall mobilized endothelial precursors [2]. In that process, cancer stem cells act through the production of factors able to exert a paracrine chemoattractant effect towards responsive endothelial cells and especially precursor endothelial cells. This effect is insured mainly by the production of vascular endothelial growth factors (VEGFs) and their endothelial receptors; it also permits the conditioning of the pre-metastatic niches by activating the endothelial barrier in secondary sites [3].
Vascular endothelial growth factor production illustrates the response to hypoxia by the proangiogenic molecule cascade [4] that develops after hypoxia-inducible factors (HIFs) early production and transcription [5]. As tumour angiogenesis is not efficient, it is unable to restore the cell oxygenation thus maintains the VEGF production, and pathologic angiogenesis is pursued in a vicious circle [3].
The antiangiogenesis strategies for cancer treatment have been successful in destroying the tumour vessels and reducing the tumour size. They have, unfortunately, also resulted in the selection of resistant cancer cells surviving to deep hypoxia and escaping from most conventional treatments because they are not dividing and isolated from systemic access [3]. Consequently, the interactions between the endothelial cells and the cancer stem cells determine the status of the niche [6]. This review focuses on the characteristics of cancer stem cells, pointing out their relation to hypoxia, the hypoxia-mediated participation of endothelial precursor cells to the cancer stem cell niche, and the fine mechanisms of regulation between EPCs and CSCs that the non-coding microRNAs are tuning in the context of hypoxia.
The characteristics of cancer stem cells are linked to hypoxia
Because it was shown that metastatic potential might be attributed to stem cell-like tumour cells (also called cancer stem cells), which are resistant to chemotherapy and induce dormancy in tumours, their detection, isolation, and characterisation is a challenge for cancer-targeted therapeutic strategies. As they are quite similar to normal stem cells, it is critical to find specific markers allowing CSC identification for effective targeted therapy. A number of markers have been used to isolate CSCs from solid tumours of the colon, oesophagus, liver, breast, brain, cervix, and head and neck squamous cell carcinomas (HNSCC). As summarised [7], antigens should be combined in order to type and even isolate the CSCs from a whole tumour population. CD44 and CD133 are commonly expressed in oesophageal stem cell carcinoma, liver, breast, prostate, and colon carcinoma. In addition, Nanog Oct3/4, CD90, CD166, CD34, CD177 (stem cell factor receptor), or CD271 are helping to type CSCs in various head and neck localised cancers [8].
Zhang et al. (2009) first suggested, that Hoechst 33342 dye by the ATP-binding cassette transporter (ABC, multi-drug resistance receptors) can also be used to identify the side-population of cells that possess stem-like properties [9].
Aldehyde dehydrogenase enzymatic activity is used to type, isolate, and study the cancer stem cells. In many tumour types the cells that display a high aldehyde dehydrogenase (ALDH) activity have stem-like properties in terms of spheroid formation and tumourigenicity [10], but it is not a general feature [11].
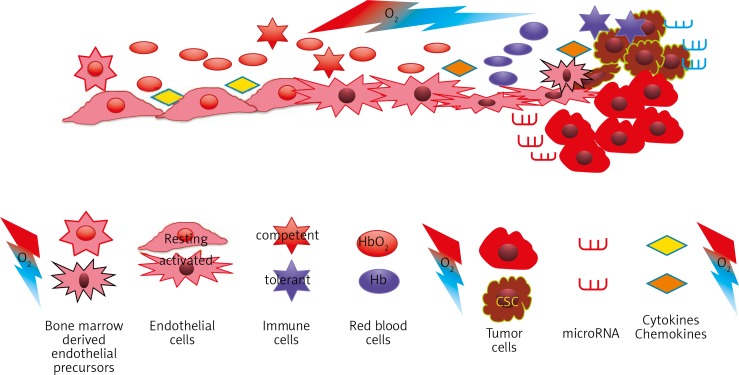
Consequently, a variety of cell surface markers are used to define CSCs from primary tumours and lines, commonly CD133, CD44, CD24, and CD166 [12], but no study has allowed definition of the CSC identity, since the CSC-phenotype may vary substantially across different tumours, as in the case of melanoma metastatic process [13].Figure 1
Fig. 1.
Schematic representation of the cellular and molecular modulation of the tumour microenvironment due to oxygen tension modification
An interesting feature that is usually not taken into account along with characterization and functional studies is the influence of hypoxia vs. physioxia [14]. Most of the cited antigens and putative markers assessed are regulated by the pO2 conditions. Indeed, CD133 promoter is activated by hypoxia-inducible factors (HIFs) [15] and its glycosylation is also hypoxia-dependent, which explains the variable results obtained by antibody detection [16]. CD44 was also shown to be regulated by hypoxia in expressing its variant isoforms in triple negative breast cancer [17], as similarly shown for CD271 in melanoma [18]. This hypoxia-mediated effect was clearly demonstrated on CD34+ chronic myeloid precursor cells operating differentiation [19] and on CD24 as an effector of HIF-1α-driven primary tumour growth and metastasis [20]. Although in the melanoma, ALDH was not correlated with aggressiveness [21], we showed that its expression is stabilized in hypoxia-selected cells and it was shown to regulate stemness in breast cancer by activating HIF-2α [22].
Consequently, considering hypoxia effects on antigen expression it might help to precisely identify the stem cell characteristics in tumours.
The contribution of endothelial precursor cells to tumour angiogenesis as a response to hypoxia
Similarly to cancer stem cells, normal stem cells are very reactive to hypoxia and hypoxia-mediated signalling, as shown in embryonic development and particularly for haemangioblast specification [23]. This “good” aspect of angiogenesis becomes “bad” as it occurs in tumours through the early ‘angiogenic switch’ due to hypoxia (Hanahan and Folkman, 1996). It allows tumour development [24] and sets the tumour microenvironment in terms of cytokines, enzymes, extracellular matrix, and cells [14, 25]. Tumour angiogenesis promotes tumour growth and facilitates metastasis. In response to pro-angiogenic signals, as vascular endothelial growth factor (VEGF)-A or interleukin (IL)-8 released mainly from neoplastic cells and stromal cells, such as Tie-2 expressing monocytes (TEMs) [26] and fibroblasts [25], endothelial cells are further actively recruited to participate to the pathologic angiogenesis into the tumour mass [25]. Similarly, the infiltrating immune cell subpopulations that are recruited, apart from tumour-antagonising CD8 cytotoxic T lymphocytes (CTLs) and natural killer (NK) cells, i.e. macrophages, mast cells, neutrophils, and T and B lymphocytes, act as tumour-promoting cells [2]. Defining the type and differentiation characteristics of the endothelial precursors that are specifically recruited into the developing tumour is an important aspect in the design of new angiogenesis-based treatments [27, 28] that are able to take over antiangiogenic treatments and avoid selection of cancer stem cells. The normalization of tumour vessels, first suggested by Jain [29], represents an adjuvant strategy which not only permits a strong increase of the efficacy of chemotherapy and radiotherapy, but also reduces the tumour growth and allows eradication of metastases [30]. Moreover, it clearly reduces the number of stem-like cells in the treated tumours where the remaining markers are CD133+ and CD34+ cells, attributable to EPCs [31], while Oct3,4+, CD24+, and CD271+ cells totally disappeared together with the expression of their mRNA [30]. Stable normalization may thus be the alternative to antiangiogenic treatments [32, 33].
MicroRNA contribution to the vascular cancer stem cell niche
MicroRNAs mediate an important aspect of the endothelial cell-to-cancer stem like cell cross-talk. They have various means to act on cells and regulate their gene expression. They are largely documented for their expression in response to hypoxia. The so-called hypoxia miRs are regularly induced in hypoxia, and some of them act on angiogenesis (angiomiRs). In tumours, miR-210, the most typical hypoxia miR, is HIF-1α-dependent and also stabilises HIF-1α, thus controlling the hypoxic phenotype [34]. This process is of fundamental interest for further therapeutic applications involving radiosensitisation. As miR-210 is proangiogenic, it promotes endothelial cell migration [35]. It operates through endosome transport to endothelial cells [36], which appears to be a common means of interaction [37]. Besides this classical example, the huge role played by miRs in tuning the tumour microenvironment is documented for immune cells [38, 39], the extracellular matrix and, enzymatic regulation, as well as angiogenesis [2, 38, 40]. In this instance HO-1 activity in angiogenesis and compensation by miR-378 expression was shown to occur through exosomes produced by tumour cells [38]. MiRs that normally regulate stem cell biology act on cancer stem cells as well. MiR-34a was found to be a key negative regulator of CD44+ prostate cancer cells, thus offering a therapeutic agent against prostate CSCs [41]. Similarly, the endothelial precursors recruited and responding to the hypoxic milieu of the CSCs niche are submitted to the identical miR regulation. Tumour endothelial cells were found to share the same abnormalities as found in cancer cells [42], which could be due to a common cancer/endothelial cell progenitor [43], to cancer-to-endothelial cell transdifferentiation [44], to fusion between cancer and ECs [45], or to cancer stem-like cells undergoing vascular mimicry. In contrast, tumour endothelial cells have unique properties [46] suggesting that oncogene-bearing circulating endothelial cell precursors might be one of the possible identities of cancer stem cells. As such, miRs that potentially normalize angiogenesis by regulating PTEN activity [2, 30] like miR-21 vs. mir-29b, might provide powerful targets for therapies linking vessel stable normalization to tumour growth control [47].
Discussion
As CSCs and endothelial precursor cells cooperate closely in the achievement of vascular/cancer stem niche, they operate through very close mechanisms and responses. The notch signalling protein is a mediator exemplifying the convergence of hypoxic responses to promote signals that lead cancer stem cells via the epithelial-mesenchymal transition [48]. Although the HIF-1α-mediated EMT pathway still remains undefined as to the precise mechanisms of the molecular expression cascade, the similar pathways used by the CSC and EPC responses to hypoxia offer new insights. The endothelial cells perform angiogenesis through the tips cells/stalk cell notch signalling, and the concordance of the mechanisms led to the observation of the CSCs transdifferentiation into endothelial cells, thus achieving vascular mimicry [49].
Hypoxia and HIF-1α overexpression have been reported to promote the expression of EMT activators [50]. Notch signalling pathway is required to convert the hypoxic stimulus into EMT [51]. As recently shown [52], hypoxia upregulates c-Myc and OCT3/4, contributing to vascular mimicry formation. Hypoxia is also a regulator of CSCs and EMT through NFκB, PI3K/Akt/mTOR, NOTCH, Wnt/β-catenin, and Hedgehog signalling pathways [48].
Thus, the hypoxic microenvironment seems to rule the vascular mimicry mechanism of angiogenesis formation, which is a convergence of the diverse angiogenesis mechanisms through stemness maintenance and cooperation of endothelial precursor cells with cancer stem cells. At this level, the regulation operated by microRNAs [53] offers an opportunity to control and possibly transform the tumour microenvironment at the CSC/EPC niche.
The authors declare no conflict of interest.
Guillaume Collet was a doctoral fellow sponsored by the French Ministry of Research; fellowship N 32852-2008, the Malopolska Marshal's Office, and the LNCC (National League Against Cancer). Anna Tejchman and Krzysztof Klimkiewicz are co-tutorial doctoral fellows, MNiSW and French MAE. BEHR is a postdoctoral fellow from Normoxys Inc.
This work was partly supported by the French-Polish Grant INCa/CNRS/MNiSW (347/N-INCA/2008) for cooperation and ANR “triple sens project”, the LNCC and the Institut National de la Santé et de la Recherche Médicale (INSERM) and LIA CNRS/UJ MiRTANGO.
References
- 1.Borovski T, De Sousa EMF, Vermeulen L, Medema JP. Cancer stem cell niche: the place to be. Cancer Res. 2011;71:634–9. doi: 10.1158/0008-5472.CAN-10-3220. [DOI] [PubMed] [Google Scholar]
- 2.Collet G, Skrzypek K, Grillon C, Matejuk A, El Hafni-Rahbi B, Lamerant-Fayel N, Kieda C. Hypoxia control to normalize pathologic angiogenesis: potential role for endothelial precursor cells and miRNAs regulation. Vascul Pharmacol. 2012;56:252–61. doi: 10.1016/j.vph.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Goel S, Duda DG, Xu L, Munn LL, Boucher Y, Fukumura D, Jain RK. Normalization of the vasculature for treatment of cancer and other diseases. Physiol Rev. 2011;91:1071–121. doi: 10.1152/physrev.00038.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285:1182–6. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 5.Zhong H, Chiles K, Feldser D, Laughner E, Hanrahan C, Georgescu MM, Simons JW, Semenza GL. Modulation of hypoxia-inducible factor 1alpha expression by the epidermal growth factor/phosphatidylinositol 3-kinase/PTEN/AKT/FRAP pathway in human prostate cancer cells: implications for tumor angiogenesis and therapeutics. Cancer Res. 2000;60:1541–5. [PubMed] [Google Scholar]
- 6.Gao D, Nolan DJ, Mellick AS, Bambino K, McDonnell K, Mittal V. Endothelial progenitor cells control the angiogenic switch in mouse lung metastasis. Science. 2008;319:195–8. doi: 10.1126/science.1150224. [DOI] [PubMed] [Google Scholar]
- 7.Moghbeli M, Moghbeli F, Forghanifard MM, Abbaszadegan MR. Cancer stem cell detection and isolation. Med Oncol. 2014;31:69. doi: 10.1007/s12032-014-0069-6. [DOI] [PubMed] [Google Scholar]
- 8.Routray S, Mohanty N. Cancer stem cells accountability in progression of head and neck squamous cell carcinoma: the most recent trends! Mol Biol Int. 2014;2014:375325. doi: 10.1155/2014/375325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang P, Zhang Y, Mao L, Zhang Z, Chen W. Side population in oral squamous cell carcinoma possesses tumor stem cell phenotypes. Cancer Lett. 2009;277:227–34. doi: 10.1016/j.canlet.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Lohberger B, Rinner B, Stuendl N, Absenger M, Liegl-Atzwanger B, Walzer SM, Windhager R, Leithner A. Aldehyde dehydrogenase 1, a potential marker for cancer stem cells in human sarcoma. PLoS One. 2012;7:e43664. doi: 10.1371/journal.pone.0043664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yu C, Yao Z, Dai J, Zhang H, Escara-Wilke J, Zhang X, Keller ET. ALDH activity indicates increased tumorigenic cells, but not cancer stem cells, in prostate cancer cell lines. In Vivo. 2011;25:69–76. [PubMed] [Google Scholar]
- 12.Curley MD, Therrien VA, Cummings CL, et al. CD133 expression defines a tumor initiating cell population in primary human ovarian cancer. Stem Cells. 2009;27:2875–83. doi: 10.1002/stem.236. [DOI] [PubMed] [Google Scholar]
- 13.Shiozawa Y, Nie B, Pienta KJ, Morgan TM, Taichman RS. Cancer stem cells and their role in metastasis. Pharmacol Ther. 2013;138:285–93. doi: 10.1016/j.pharmthera.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carreau A, El Hafny-Rahbi B, Matejuk A, Grillon C, Kieda C. Why is the partial oxygen pressure of human tissues a crucial parameter? Small molecules and hypoxia. J Cell Mol Med. 2011;15:1239–53. doi: 10.1111/j.1582-4934.2011.01258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ohnishi S, Maehara O, Nakagawa K, et al. Hypoxia-inducible factors activate CD133 promoter through ETS family transcription factors. PLoS One. 2013;8:e66255. doi: 10.1371/journal.pone.0066255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lehnus KS, Donovan LK, Huang X, Zhao N, Warr TJ, Pilkington GJ, An Q. CD133 glycosylation is enhanced by hypoxia in cultured glioma stem cells. Int J Oncol. 2013;42:1011–7. doi: 10.3892/ijo.2013.1787. [DOI] [PubMed] [Google Scholar]
- 17.Krishnamachary B, Penet MF, Nimmagadda S, et al. Hypoxia regulates CD44 and its variant isoforms through HIF-1alpha in triple negative breast cancer. PLoS One. 2012;7:e44078. doi: 10.1371/journal.pone.0044078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boiko AD, Razorenova OV, van de Rijn M, et al. Human melanoma-initiating cells express neural crest nerve growth factor receptor CD271. Nature. 2010;466:133–7. doi: 10.1038/nature09161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Desplat V, Faucher JL, Mahon FX, Dello Sbarba P, Praloran V, Ivanovic Z. Hypoxia modifies proliferation and differentiation of CD34(+) CML cells. Stem Cells. 2002;20:347–54. doi: 10.1634/stemcells.20-4-347. [DOI] [PubMed] [Google Scholar]
- 20.Thomas S, Harding MA, Smith SC, et al. CD24 is an effector of HIF-1-driven primary tumor growth and metastasis. Cancer Res. 2012;72:5600–12. doi: 10.1158/0008-5472.CAN-11-3666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Prasmickaite L, Engesaeter BØ, Skrbo N, Hellenes T, Kristian A, Oliver NK, Suo Z, Maelandsmo GM. Aldehyde dehydrogenase (ALDH) activity does not select for cells with enhanced aggressive properties in malignant melanoma. PLoS One. 2010;5:e10731. doi: 10.1371/journal.pone.0010731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kim RJ, Park JR, Roh KJ, et al. High aldehyde dehydrogenase activity enhances stem cell features in breast cancer cells by activating hypoxia-inducible factor-2alpha. Cancer Lett. 2013;333:18–31. doi: 10.1016/j.canlet.2012.11.026. [DOI] [PubMed] [Google Scholar]
- 23.Ramírez-Bergeron DL, Runge A, Dahl KD, Fehling HJ, Keller G, Simon MC. Hypoxia affects mesoderm and enhances hemangioblast specification during early development. Development. 2004;131:4623–34. doi: 10.1242/dev.01310. [DOI] [PubMed] [Google Scholar]
- 24.Krock BL, Skuli N, Simon MC. Hypoxia-induced angiogenesis: good and evil. Genes Cancer. 2011;2:1117–33. doi: 10.1177/1947601911423654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chouaib S, Kieda C, Benlalam H, Noman MZ, Mami-Chouaib F, Rüegg C. Endothelial cells as key determinants of the tumor microenvironment: interaction with tumor cells, extracellular matrix and immune killer cells. Crit Rev Immunol. 2010;30:529–45. doi: 10.1615/critrevimmunol.v30.i6.30. [DOI] [PubMed] [Google Scholar]
- 26.De Palma M, Venneri MA, Galli R, Sergi Sergi L, Politi LS, Sampaolesi M, Naldini L. Tie2 identifies a hematopoietic lineage of proangiogenic monocytes required for tumor vessel formation and a mesenchymal population of pericyte progenitors. Cancer Cell. 2005;8:211–26. doi: 10.1016/j.ccr.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 27.Asahara T. Cell therapy and gene therapy using endothelial progenitor cells for vascular regeneration. Handb Exp Pharmacol. 2007;180:181–94. doi: 10.1007/978-3-540-68976-8_8. [DOI] [PubMed] [Google Scholar]
- 28.Kieda C. Heterogeneity of endothelial cells – role in vessel specialization and cooperation in vasculogenic mimicry. Postepy Biochem. 2013;59:372–8. [PubMed] [Google Scholar]
- 29.Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 30.Kieda C, El Hafny-Rahbi B, Collet G, et al. Stable tumor vessel normalization with pO2 increase and endothelial PTEN activation by inositol trispyrophosphate brings novel tumor treatment. J Mol Med (Berl) 2013;91:883–99. doi: 10.1007/s00109-013-0992-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Paprocka M, Krawczenko A, Dus D, Kantor A, Carreau A, Grillon C, Kieda C. CD133 positive progenitor endothelial cell lines from human cord blood. Cytometry A. 2011;79:594–602. doi: 10.1002/cyto.a.21092. [DOI] [PubMed] [Google Scholar]
- 32.Collet G, Lamerant-Fayel N, Tertil M, et al. Hypoxia-regulated overexpression of soluble VEGFR2 controls angiogenesis and inhibits tumor growth. Mol Cancer Ther. 2014;13:165–78. doi: 10.1158/1535-7163.MCT-13-0637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sato Y. Persistent vascular normalization as an alternative goal of anti-angiogenic cancer therapy. Cancer Sci. 2011;102:1253–6. doi: 10.1111/j.1349-7006.2011.01929.x. [DOI] [PubMed] [Google Scholar]
- 34.Grosso S, Doyen J, Parks SK, et al. MiR-210 promotes a hypoxic phenotype and increases radioresistance in human lung cancer cell lines. Cell Death Dis. 2013;4:e544. doi: 10.1038/cddis.2013.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zeng L, He X, Wang Y, et al. MicroRNA-210 overexpression induces angiogenesis and neurogenesis in the normal adult mouse brain. Gene Ther. 2014;21:37–43. doi: 10.1038/gt.2013.55. [DOI] [PubMed] [Google Scholar]
- 36.Kosaka N, Iguchi H, Hagiwara K, Yoshioka Y, Takeshita F, Ochiya T. Neutral sphingomyelinase 2 (nSMase2)-dependent exosomal transfer of angiogenic microRNAs regulate cancer cell metastasis. J Biol Chem. 2013;288:10849–59. doi: 10.1074/jbc.M112.446831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kucharzewska P, Christianson HC, Welch JE, et al. Exosomes reflect the hypoxic status of glioma cells and mediate hypoxia-dependent activation of vascular cells during tumor development. Proc Natl Acad Sci U S A. 2013;110:7312–7. doi: 10.1073/pnas.1220998110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Skrzypek K, Tertil M, Golda S, et al. Interplay between heme oxygenase-1 and miR-378 affects non-small cell lung carcinoma growth, vascularization, and metastasis. Antioxid Redox Signal. 2013;19:644–60. doi: 10.1089/ars.2013.5184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matejuk A, Collet G, Nadim M, Grillon C, Kieda C. MicroRNAs and tumor vasculature normalization: impact on anti-tumor immune response. Arch Immunol Ther Exp (Warsz) 2013;61:285–99. doi: 10.1007/s00005-013-0231-4. [DOI] [PubMed] [Google Scholar]
- 40.Li X, Wu Z, Fu X, Han W. A microRNA component of the neoplastic microenvironment: microregulators with far-reaching impact. Biomed Res Int. 2013;2013:762183. doi: 10.1155/2013/762183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu C, Kelnar K, Liu B, et al. The microRNA miR-34a inhibits prostate cancer stem cells and metastasis by directly repressing CD44. Nat Med. 2011;17:211–5. doi: 10.1038/nm.2284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Della Porta MG, Malcovati L, Rigolin GM, et al. Immunophenotypic, cytogenetic and functional characterization of circulating endothelial cells in myelodysplastic syndromes. Leukemia. 2008;22:530–7. doi: 10.1038/sj.leu.2405069. [DOI] [PubMed] [Google Scholar]
- 43.Ergun S, Hohn HP, Kilic N, Singer BB, Tilki D. Endothelial and hematopoietic progenitor cells (EPCs and HPCs): hand in hand fate determining partners for cancer cells. Stem Cell Rev. 2008;4:169–77. doi: 10.1007/s12015-008-9028-y. [DOI] [PubMed] [Google Scholar]
- 44.Verfaillie CM. Bony endothelium: tumor-mediated transdifferentiation? Cancer Cell. 2008;14:193–4. doi: 10.1016/j.ccr.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 45.Bertolini F, Shaked Y, Mancuso P, Kerbel RS. The multifaceted circulating endothelial cell in cancer: towards marker and target identification. Nat Rev Cancer. 2006;6:835–45. doi: 10.1038/nrc1971. [DOI] [PubMed] [Google Scholar]
- 46.Weis SM, Cheresh DA. Tumor angiogenesis: molecular pathways and therapeutic targets. Nat Med. 2011;17:1359–70. doi: 10.1038/nm.2537. [DOI] [PubMed] [Google Scholar]
- 47.Xiong B, Cheng Y, Ma L, Zhang C. MiR-21 regulates biological behavior through the PTEN/PI-3 K/Akt signaling pathway in human colorectal cancer cells. Int J Oncol. 2013;42:219–28. doi: 10.3892/ijo.2012.1707. [DOI] [PubMed] [Google Scholar]
- 48.Jiang J, Tang YL, Liang XH. EMT: a new vision of hypoxia promoting cancer progression. Cancer Biol Ther. 2011;11:714–23. doi: 10.4161/cbt.11.8.15274. [DOI] [PubMed] [Google Scholar]
- 49.Fan YL, Zheng M, Tang YL, Liang XH. A new perspective of vasculogenic mimicry: EMT and cancer stem cells (Review) Oncol Lett. 2013;6:1174–80. doi: 10.3892/ol.2013.1555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Majmundar AJ, Wong WJ, Simon MC. Hypoxia-inducible factors and the response to hypoxic stress. Mol Cell. 2010;40:294–309. doi: 10.1016/j.molcel.2010.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sahlgren C, Gustafsson MV, Jin S, Poellinger L, Lendahl U. Notch signaling mediates hypoxia-induced tumor cell migration and invasion. Proc Natl Acad Sci U S A. 2008;105:6392–7. doi: 10.1073/pnas.0802047105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Misra RM, Bajaj MS, Kale VP. Vasculogenic mimicry of HT1080 tumour cells in vivo: critical role of HIF-1alpha-neuropilin-1 axis. PLoS One. 2012;7:e50153. doi: 10.1371/journal.pone.0050153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peter ME. Let-7 and miR-200 microRNAs: guardians against pluripotency and cancer progression. Cell Cycle. 2009;8:843–52. doi: 10.4161/cc.8.6.7907. [DOI] [PMC free article] [PubMed] [Google Scholar]