Abstract
Background
The Chronic Obstructive Pulmonary Disease Assessment Test (CAT) could play a role in detecting acute deterioration in health status during monitoring visits in routine clinical practice.
Objective
To evaluate the discriminative property of a change in CAT score from a stable baseline visit for detecting acute deterioration in health status visits of chronic obstructive pulmonary disease (COPD) patients.
Methods
The CAT questionnaire was administered to stable COPD patients routinely attending the chest clinic of Chiang Mai University Hospital who were monitored using the CAT score every 1–3 months for 15 months. Acute deterioration in health status was defined as worsening or exacerbation. CAT scores at baseline, and subsequent visits with acute deterioration in health status were analyzed using the t-test. The receiver operating characteristic curve was performed to evaluate the discriminative property of change in CAT score for detecting acute deterioration during a health status visit.
Results
A total of 354 follow-up visits were made by 140 patients, aged 71.1±8.4 years, with a forced expiratory volume in 1 second of 47.49%±18.2% predicted, who were monitored for 15 months. The mean CAT score change between stable baseline visits, by patients’ and physicians’ global assessments, were 0.05 (95% confidence interval [CI], −0.37–0.46) and 0.18 (95% CI, −0.23–0.60), respectively. At worsening visits, as assessed by patients, there was significant increase in CAT score (6.07; 95% CI, 4.95–7.19). There were also significant increases in CAT scores at visits with mild and moderate exacerbation (5.51 [95% CI, 4.39–6.63] and 8.84 [95% CI, 6.29–11.39], respectively), as assessed by physicians. The area under the receiver operating characteristic curve of CAT score change for the detection of acute deterioration in health status was 0.89 (95% CI, 0.84–0.94), and the optimum cut-off point score was at 4, with a sensitivity, specificity, and accuracy of 76.8%, 83.6%, and 82.4%, respectively.
Conclusions
Change in CAT score during monitoring visits is useful for detecting acute deterioration in health status, and a change of 4 units could make a moderate prediction of acute deterioration in health status.
Keywords: chronic obstructive pulmonary disease, health status, questionnaire
Introduction
Chronic obstructive pulmonary disease (COPD), a chronic inflammatory airway condition associated with episodes of acute deterioration, termed exacerbations,1 is a major cause of chronic morbidity and mortality worldwide.2 The natural history of COPD is interrupted by episodes of worsening symptoms and signs of accelerating lung function decline,3,4 leading to decreased health-related quality of life,5,6 increased mortality,7,8 and increased healthcare costs.9,10 Acute exacerbation of COPD is currently defined as a sustained worsening of the patient’s condition from the stable state, and beyond normal day-to-day variations, that is acute in onset and necessitates a change in regular medication.11 Given the importance of early treatment, there is a need for new low-burden strategies to capture symptom-based exacerbations. Disease-specific questionnaires such as the St George’s Respiratory Questionnaire, the Chronic Respiratory Disease Questionnaire, and the Clinical COPD Questionnaire have been developed to quantify the effect of COPD on health-related quality of life. However, their extent and complexity make them unsuitable for use in routine clinical practice.12 The COPD Assessment Test (CAT) is a validated eight-item questionnaire designed to assess and quantify the effect of COPD symptoms on patient health status. It has excellent measurement properties and is short and simple for patients to complete, providing a score out of 40 to indicate disease effect without the need for complex calculation. Initial studies have shown that the CAT correlates closely with health-related quality of life, as measured by the St George’s Respiratory Questionnaire.13 The CAT questionnaire covers a broad range of effects of COPD on patient health, with very good measurement properties, and is applicable to global use.14,15 The CAT score change from stable visits should play a role in detecting acute deterioration in health status during monitoring visits for COPD patients in Thailand.
Materials and methods
Patients
Patients diagnosed as having COPD (Global initiative for chronic Obstructive Lung Disease [GOLD] stages I–IV)16 in a stable clinical condition (no exacerbation during the previous 6 weeks before study inclusion) who were attending the chest clinic of the Chiang Mai University Hospital were enrolled. The inclusion criteria were smokers or ex-smokers with a smoking history of 10 or more pack-years who were aged 40 years or older and who had no exacerbation more than 6 weeks before enrollment. Patients were excluded if they had a history of asthma, chronic chest symptoms in those aged younger than 40 years, or concomitant cardiopulmonary diseases or were unable to complete questionnaires. The study was approved by the ethics committees of the Faculty of Medicine, Chiang Mai University, and written informed consent was obtained from all patients.
Study design
The study involved a prospective investigation of patients attending the chest clinic of Chiang Mai University Hospital from October 2010 to December 2011. After orientation by a nurse, the patients completed the validated Thai version of the CAT questionnaire, which is available online at http://www.catestonline.org13. The patients were monitored every 1–3 months during routine or unscheduled visits for detecting worsening and exacerbation of symptoms. A worsening visit was assessed by the patient’s global assessment, and an exacerbation visit was assessed by the physicians. Moderate exacerbation was defined as a worsening of two or more of the following major symptoms for 2 or more consecutive days: dyspnea, sputum volume, or sputum purulence, requiring treatment with systemic corticosteroids and/or antibiotics.1 Mild exacerbation in this study was defined as worsening of COPD symptoms more than the usual daily variations by patient’s global assessment or worsening of symptoms requiring increased dosage, shortened dosage interval, or additional long-acting bronchodilators, but not systemic corticosteroids and/or antibiotics, by physician’s global assessment. Spirometry was performed in accordance with guidelines of the American Thoracic Society and the European Respiratory Society.17 In addition, a modified Medical Research Council dyspnea score,16 as well as exercise capacity determined by the longest distance walked in 6 minutes (6-MWD), tested by a standard 6-minute walk test, were recorded.18 The postbronchodilator forced expiratory volume in 1 second (FEV1), forced vital capacity, FEV1/forced vital capacity ratio, and 6-MWD parameters, if performed within 6 months before enrollment, were acceptable.
Statistical analysis
Calculation of sample size formula proportion in n=Zα2PQ/d2, alpha =0.05, sensitivity =0.8, desired precision =0.2, and prevalence of COPD exacerbation in Thailand in a previous study was 28.7%.19 A sample size of 84 patients was required for this study. CAT scores, categorized into stable, mild, and moderate exacerbation visits, were analyzed by using paired t-test within groups and by independent sample t-tests between groups. Receiver operating characteristic (ROC) curve was performed to predict those with acute deterioration in health status by area under the curve and 95% confidence interval (CI). Contingency tables were made to calculate the following performance parameters: sensitivity, specificity, positive predictive value, negative predictive value, and accuracy from various point changes of CAT score to identify the optimum cut-off point. Statistical significance was set at P<0.05. All analyses were carried out with the SPSS statistical package, version 16, for Windows.
Results
Patient demographics and clinical characteristics are displayed in Table 1. A total of 354 follow-up visits were made for 140 study patients (56.4% male; aged 71.1±8.4 years; FEV1=47.4%±18.2% predicted) with GOLD stages I–IV comprising 10 (7.1%), 51 (36.4%), 51 (36.4%), and 26 (18.6%) patients, respectively. There were 56 exacerbation visits, and 37 and 19 visits were mild and moderate, respectively. The mean CAT score change in stable COPD was not significant (0.05 [95% CI, −0.37–0.46] and 0.18 [95% CI, −0.23–0.60], by patient’s and physician’s global assessment, respectively). The mean CAT score changes at worsening visit were significantly higher than baseline stable visit (6.07; 95% CI, 4.95–7.19; P<0.0001). At the time of physician’s global assessments, the mean CAT score changes were 5.51 (95% CI, 4.39–6.6; P<0.0001) and 8.84 (95% CI, 6.29–11.39; P<0.0001) at mild and moderate exacerbation visits, respectively. The mean CAT score change between mild and moderate exacerbation visits was also significantly different (3.22; 95% CI, 0.46–5.98; P<0.007; Table 2). The area under the ROC curve of CAT score change for detection of acute deterioration in health status was 0.89 (95% CI, 0.84–0.94; Figure 1). Estimates of discriminative performance of the CAT score change were calculated from 1 to 10 points on the ROC curve (Table 3). The cut-off point CAT score change of 4 had acceptable sensitivity, specificity, and accuracy values of 76.8%, 83.6%, and 82.4%, respectively.
Table 1.
Demographic and clinical characteristics of COPD patients
| Characteristics | N=140 |
|---|---|
| Number of follow-up visits (n) | 354 |
| Number of visits/case | 3.6±1.5 |
| Age, years | 71.1±8.4 |
| Male sex, n (%) | 79 (56.4) |
| FEV1 percentage predicted | 47.4±18.2 |
| FEV1/FVC, % | 51.8±10.7 |
| SGRQ score | 39.3±21.2 |
| mMRC score | 1.9±1.1 |
| CAT score | 9.9±6.4 |
| 6-MWD, m | 324.0±103.4 |
| GOLD classification, n (%) | |
| I | 10 (7.1) |
| II | 51 (36.4) |
| III | 51 (36.4) |
| IV | 26 (18.6) |
| Missing | 2 (1.5) |
Note: Data are n (%) or mean ± SD.
Abbreviations: COPD, chronic obstructive pulmonary disease; FEV1, percentage predicted, percentage predicted of forced expiratory volume in first second; FEV1/FVC, ratio of FEV1 to forced vital capacity; SGRQ, St George’s Respiratory Questionnaire; mMRC, modified Medical Research Council score; CAT, COPD Assessment Test; 6-MWD, 6-minute walking distance; GOLD, Global initiative for chronic Obstructive Lung Disease.
Table 2.
Mean CAT score difference by COPD status (stable, worsening, and exacerbation visits)
| Assessment of COPD status (n=354) | CAT score, mean difference (95% confidence interval) | P-value |
|---|---|---|
| Patients global assessment | ||
| Stable–stable (n=286) | 0.05 (−0.37–0.46) | 0.817 |
| Stable–worsening (n=68) | 6.07 (4.95–7.19) | <0.0001 |
| Physician global assessment | ||
| Stable–stable (n=298) | 0.18 (−0.23–0.60) | 0.389 |
| Stable–mild exacerbation (n=37) | 5.51 (4.39–6.63) | <0.0001 |
| Stable–moderate exacerbation (n=19) | 8.84 (6.29–11.39) | <0.0001 |
| Mild–moderate exacerbation | 3.22 (0.46–5.98) | 0.007 |
Note: Data are mean difference (95% confidence interval).
Abbreviations: CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease.
Figure 1.
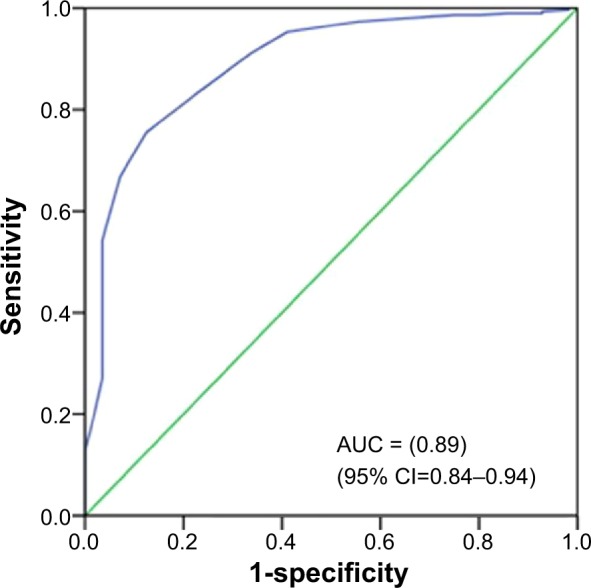
Receiver operating curve of the CAT score for detecting exacerbation in COPD patients.
Abbreviations: AUC, area under the curve; CI, confidence interval; CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease.
Table 3.
Discriminative property change of CAT score cut-off points for acute deterioration in health status detection
| Change of CAT score cut-off points | Sensitivity, % | Specificity, % | Accuracy, % | PPV, % | NPV, % |
|---|---|---|---|---|---|
| 1 | 96.4 | 54.4 | 61.0 | 28.4 | 98.8 |
| 2 | 92.9 | 66.8 | 70.9 | 34.4 | 98.0 |
| 3 | 87.5 | 75.5 | 77.4 | 40.2 | 97.0 |
| 4* | 76.8 | 83.6 | 82.4 | 46.7 | 95.0 |
| 5 | 66.1 | 91.3 | 87.3 | 58.7 | 93.5 |
| 6 | 58.9 | 95.3 | 89.5 | 70.2 | 92.5 |
| 7 | 44.6 | 97.3 | 88.9 | 75.8 | 90.3 |
| 8 | 30.4 | 98.3 | 87.6 | 77.3 | 88.3 |
| 9 | 25.0 | 98.7 | 87.0 | 77.8 | 87.5 |
| 10 | 23.6 | 98.7 | 86.7 | 76.5 | 87.5 |
Note:
The best cut-off point.
Abbreviations: CAT, COPD Assessment Test; COPD, chronic obstructive pulmonary disease; PPV, positive predictive value; NPV, negative predictive value.
Discussion
The CAT is a short and simple-to-administer patient-completed questionnaire designed for routine use in clinical practice, covering a wide range of effects of COPD.1 This study shows that CAT score was stable between baseline visits with the score change less than 1 point, as determined by patients or physicians, which was similar to the previous study.13 At worsening or exacerbation visits, as assessed by patients or physicians, CAT scores were significantly increased, with the highest changes observed at moderate exacerbation visits. This study revealed that the magnitude of CAT score change correlated well with acute deterioration in health status of the patient, as the change was higher at the moderate than at the mild exacerbation visits. The relatively high CAT score change at moderate exacerbation visit in this study, compared with other studies (mean CAT score changes, 4.1–6.6 points),12–14,20 could be a result of lower baseline CAT scores in our group of patients and possible hesitation in making unscheduled visits by the patients.
In this study, the performance of CAT score change to discriminate between stable and acute deterioration in health status visits was highly acceptable, with area under the ROC =0.89. This exploratory study shows that monitoring CAT score change at routine chest clinic visits is useful for detecting acute deterioration in health status. Exploration of this ROC curve revealed that overall sensitivity and specificity are relatively disappointing and substantially vary between different point changes. The highest point change (CAT score change =10) results in the highest specificity and accuracy, but the lowest sensitivity, whereas the lowest point change (CAT score change =1) is associated with the highest sensitivity, but the lowest specificity and accuracy. The point change of 4 was optimally found to have a good combination of specificity (83.6%) and sensitivity (76.8%) to detect acute deterioration in health status. Therefore, serial monitoring CAT score at monitoring visit is a useful screening tool, and identifying the most optimum trade-off point between sensitivity and specificity for detecting acute deterioration in health status needs to be done with caution.
In addition to providing a standardized assessment and an apparently reliable numerical estimate of disease effect,1,2 CAT also likely describes the overall health-related quality of life of COPD patients more comprehensively by supplementing measurements of lung function, especially in outpatient settings. Because CAT encourages patients to express themselves meaningfully, it is plausible to presume that the test would enable patients and physicians to “speak the same language” to gain a common understanding of the effect that COPD has on a patient’s life. It is well noted that CAT cannot be used to diagnose COPD or to guide healthcare professionals on specific decisions about treatments.15 It could, however, be one part of the clinician’s tool, to be used alongside overall assessment tools, such as medical history, spirometry, modified Medical Research Council score, and 6-MWD. The CAT could be administered to COPD patients while they are waiting for their physicians at the outpatient department. Not only could CAT score be used as an outcome measure in clinical practice but it also has the potential to track changes in patients’ overall health status and to improve communication between patients and healthcare professionals.15
The study has some limitations and points for further consideration. First, the study population was from a single university hospital managed by pulmonologists, resulting in only 56 acute deterioration-in-health status visits (37 mild and 19 moderate exacerbation visits) from a total of 354 visits. A longer follow-up study with more exacerbation events would enable us to better evaluate the cut-off CAT score change with higher sensitivity, specificity, and accuracy. Second, the baseline CAT score of the patients in this study was relatively low (9.9±6.4), which could be facilitating the detection of the CAT score change, rather than the higher baseline CAT score group. Third, the CAT score change at routine monitoring visits might help alert the physician of acute deterioration in health status but cannot entirely replace the physician’s judgment and standard exacerbation criteria.
Conclusion
Determining CAT score change during monitoring visits is a useful screening tool for detecting acute deterioration in health status of COPD patients in routine clinical practice. The appropriate point change of CAT score should be identified for raising awareness of acute deterioration in the health status of COPD patients. However, its implementation for routine use at general practice clinics needs further study.
Acknowledgments
The authors would like to thank the patients who kindly took part in this study and acknowledge the staff members of the Division of Pulmonary, Critical Care and Allergy, Department of Internal Medicine, Faculty of Medicine, Chiang Mai University, for their contribution to this trial. The COPD Assessment Test is a trademark of the GlaxoSmithKline group of companies.
Author contributions
CP (pulmonologist) developed study design and carried out acquisition and interpretation of data, statistical analysis, manuscript preparation, and critical revision of intellectual contents. The other authors contributed to acquisition and interpretation of data, revised the article for important intellectual content and final approval of the version to be published.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Rabe KF, Hurd S, Anzueto A, et al. Global Initiative for Chronic Obstructive Lung Disease Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2007;176(6):532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 2.Wedzicha JA, Seemungal TA. COPD exacerbations: defining their cause and prevention. Lancet. 2007;370(9589):786–796. doi: 10.1016/S0140-6736(07)61382-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852. doi: 10.1136/thorax.57.10.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kanner RE, Anthonisen NR, Connett JE, Lung Health Study Research Group Lower respiratory illnesses promote FEV(1) decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease: results from the lung health study. Am J Respir Crit Care Med. 2001;164(3):358–364. doi: 10.1164/ajrccm.164.3.2010017. [DOI] [PubMed] [Google Scholar]
- 5.Seemungal TA, Donaldson GC, Paul EA, Bestall JC, Jeffries DJ, Wedzicha JA. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;157(5 Pt 1):1418–1422. doi: 10.1164/ajrccm.157.5.9709032. [DOI] [PubMed] [Google Scholar]
- 6.Miravitlles M, Ferrer M, Pont A, et al. IMPAC Study Group Effect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up study. Thorax. 2004;59(5):387–395. doi: 10.1136/thx.2003.008730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. doi: 10.1136/thx.2005.040527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Connors AF, Jr, Dawson NV, Thomas C, et al. Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments) Am J Respir Crit Care Med. 1996;154(4 Pt 1):959–967. doi: 10.1164/ajrccm.154.4.8887592. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest. 2000;117(2(suppl)):5S–9S. doi: 10.1378/chest.117.2_suppl.5s. [DOI] [PubMed] [Google Scholar]
- 10.Britton M. The burden of COPD in the UK: results from the Confronting COPD survey. Respir Med. 2003;97(suppl C):S71–S79. doi: 10.1016/s0954-6111(03)80027-6. [DOI] [PubMed] [Google Scholar]
- 11.Rodriguez-Roisin R. Toward a consensus definition for COPD exacerbations. Chest. 2000;117(5(suppl 2)):398S–401S. doi: 10.1378/chest.117.5_suppl_2.398s. [DOI] [PubMed] [Google Scholar]
- 12.Agustí A, Soler JJ, Molina J, et al. Is the CAT questionnaire sensitive to changes in health status in patients with severe COPD exacerbations? COPD. 2012;9(5):492–498. doi: 10.3109/15412555.2012.692409. [DOI] [PubMed] [Google Scholar]
- 13.Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. doi: 10.1183/09031936.00102509. [DOI] [PubMed] [Google Scholar]
- 14.Jones PW, Brusselle G, Dal Negro RW, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29–35. doi: 10.1183/09031936.00177210. [DOI] [PubMed] [Google Scholar]
- 15.Kelly JL, Bamsey O, Smith C, et al. Health status assessment in routine clinical practice: the chronic obstructive pulmonary disease assessment test score in outpatients. Respiration. 2012;84(3):193–199. doi: 10.1159/000336549. [DOI] [PubMed] [Google Scholar]
- 16.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi: 10.1136/thx.54.7.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 18.Statement ATS. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 19.Pothirat C, Phetsuk N, Deesomchok A, et al. Clinical characteristics, management in real world practice and long-term survival among COPD patients of Northern Thailand COPD club members. J Med Assoc Thai. 2007;90(4):653–662. [PubMed] [Google Scholar]
- 20.Feliz-Rodriguez D, Zudaire S, Carpio C, et al. Evolution of the COPD Assessment Test score during chronic obstructive pulmonary disease exacerbations: determinants and prognostic value. Can Respir J. 2013;20(5):e92–e97. doi: 10.1155/2013/398120. [DOI] [PMC free article] [PubMed] [Google Scholar]


