Abstract
Chemokines mediate numerous physiological and pathological processes related primarily to cell homing and migration. The chemokine CXCL12, also known as stromal cell-derived factor-1, binds the G-protein-coupled receptor CXCR4, which, through multiple divergent pathways, leads to chemotaxis, enhanced intracellular calcium, cell adhesion, survival, proliferation, and gene transcription. CXCR4, initially discovered for its involvement in HIV entry and leukocytes trafficking, is overexpressed in more than 23 human cancers. Cancer cell CXCR4 overexpression contributes to tumor growth, invasion, angiogenesis, metastasis, relapse, and therapeutic resistance. CXCR4 antagonism has been shown to disrupt tumor–stromal interactions, sensitize cancer cells to cytotoxic drugs, and reduce tumor growth and metastatic burden. As such, CXCR4 is a target not only for therapeutic intervention but also for noninvasive monitoring of disease progression and therapeutic guidance. This review provides a comprehensive overview of the biological involvement of CXCR4 in human cancers, the current status of CXCR4-based therapeutic approaches, as well as recent advances in noninvasive imaging of CXCR4 expression.
1. INTRODUCTION
Chemokines are a family of cytokines defined by their ability to induce gradient-dependent directional chemotaxis and are secreted by a variety of stromal and epithelial cells (Howard, Ben-Baruch, & Oppenheim, 1996; Smith, Whittall, Weksler, & Middleton, 2012). These small proteins (8–10 kDa) possess a common structural feature of conserved cysteine residues at the N-terminus (Baggiolini, 1998). Based on the number and relative spacing of the N-terminal cysteine residues, chemokines are divided into CXC, CX3C, CC, and C subfamilies with CXC chemokines characterized by one amino acid (X) between the two N-terminal cysteine residues (C) and CX3C chemokines with two N-terminal cysteine residues separated by three amino acids, etc. (Le, Zhou, Iribarren, & Wang, 2004). To date, nearly 50 chemokines have been discovered (Balkwill, 2004a; Viola & Luster, 2008). Chemokines exert their biological function through interaction with chemokine receptors, seven transmembrane G-protein-coupled receptors (GPCRs; Gilman, 1987), present on the target cells (Baggiolini, 1998). Chemokine receptors are grouped into four different families as CXC, CX3C, CC, and XC based on the chemokines they primarily interact with for signaling. Thus far, nearly 20 chemokine receptors have been identified (Balkwill, 2004a; Gilman, 1987; Pierce, Premont, & Lefkowitz, 2002; Viola & Luster, 2008). The large number of chemokines, compared to chemokine receptors, implies considerable redundancy in chemokine receptor interactions with multiple ligands binding to the same receptor and vice versa. The chemokine receptor 4 (CXCR4) is unique in that it exclusively interacts with the endogenous ligand CXCL12 (Oberlin et al., 1996).
CXCR4, also known as “fusin,” is one of the most well-studied chemokine receptors due to its earlier found role as a coreceptor for HIV entry (Feng, Broder, Kennedy, & Berger, 1996). The chemokine stromal cell-derived factor-1, now renamed as CXCL12, was established as the specific ligand for CXCR4 (Bleul, Fuhlbrigge, Casasnovas, Aiuti, & Springer, 1996; Oberlin et al., 1996). Although CXCL12 is the only known chemokine that binds CXCR4, recent studies suggest that extracellular ubiquitin also acts as an immune modulator through CXCR4-mediated signaling (Saini, Marchese, & Majetschak, 2010; Tripathi et al., 2013). Although CXCR4 is known to bind only CXCL12, in 2005 another chemokine receptor CXC receptor 7 (CXCR7, ACKR3, RDC1, CMKOR1, or GPR159) was established as a receptor for CXCL12 (Balabanian et al., 2005; Burns et al., 2006). CXCR7 functions to control the CXCL12 gradients through high-affinity binding and rapid degradation (Hoffmann et al., 2012). Thus, the role of the CXCR4–CXCR7–CXCL12 axes has become more intricate in the regulation of numerous biological processes involving cell survival and migration. Comprehensive studies will be required to delineate the exact role of CXCR4–CXCR7–CXCL12 axes in cell migration. Roles of CXCR7 and CXCL12 in biology and disease have been reviewed in detail by others (Hattermann & Mentlein, 2013; Liao et al., 2013; Sun et al., 2010).
2. CXCR4/CXCL12 SIGNALING
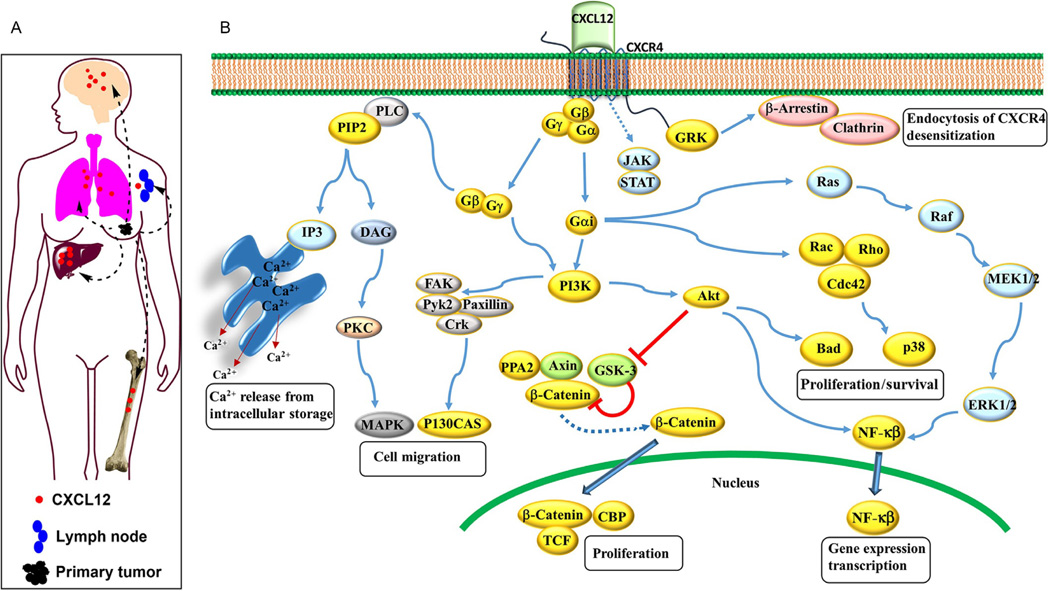
CXCL12 binding to CXCR4 initiates various downstream signaling pathways that result in a plethora of responses (Fig. 2.1) such as increase in intracellular calcium, gene transcription, chemotaxis, cell survival, and proliferation (Ganju et al., 1998), which will be briefly discussed here. Chemokine receptors are pertussis toxin-sensitive GTP-binding proteins of Gi type. After chemokine binding, the heterotrimeric G protein is activated by the exchange of GDP for GTP and dissociates into the GTP-bound α and the βγ subunits (Goldsmith & Dhanasekaran, 2007; Mellado, Rodriguez-Frade, Manes, & Martinez, 2001). The dissociated βγ subunit activates two major signal transduction enzymes, a phospholipase C-β (PLC-β), which is specific for phosphatidylinositol, and a phosphatidylinositol-3-OH kinase (PI3K). The PLC-β cleaves phosphatidylinositol (4,5)-bisphosphate into two secondary messengers, inositol (1,4,5)-trisphosphate (IP3) and diacylglycerol (DAG). Through binding to its specific receptor in the endoplasmic reticulum, IP3 induces the release of Ca2+ from intracellular stores. Acting in conjunction with Ca2+, DAG activates protein kinase C and mitogen-activated protein kinase (MAPK), contributing to cell migration (Bendall, Baraz, Juarez, Shen, & Bradstock, 2005; Mellado et al., 2001).
Figure 2.1.
(A) CXCL12 is highly expressed in tissues like lungs, liver, and bone marrow and is also secreted by tumor and stromal cells. CXCR4/CXCL12 interaction results in increased proliferative, migratory, and invasive properties of tumor cells that enable them to escape from primary tumors. CXCR4-expressing tumor cells migrate toward CXCL12 gradient and home to organs that release CXCL12. (B) Schematic diagram of CXCR4/CXCL12 signaling pathway.
Gβγ or Gα subunits activate PI3K leading to phosphorylation of many focal adhesion components including focal adhesion kinase, proline-rich kinase-2, Crk-associated substrate (p130Cas), cytoskeletal protein paxillin, Crk, Nck, and CrkL (Wang, Park, & Groopman, 2000; Zhang, Wang, Matczak, Proper, & Groopman, 2001) and contribute to reorganization of the actin cytoskeleton and changes necessary for cell migration. The activated PI3K rapidly generates phosphatidylinositol (3,4,5)-trisphosphate and initiates the activation of the AKT pathway (Mellado et al., 2001; Ward, 2006). Activated AKT plays a key role in tumor cell survival through inactivation of BCL-2 antagonist proapoptotic BAD resulting in cell survival. CXCR4 signaling via AKT also leads to inactivation of GSK3β and stabilization of β-catenin. Stabilized β-catenin moves to the nucleus and activates gene transcription and promotes proliferation (Mo et al., 2013).
Signaling through Gαi has been linked to transcription and gene expression through the PI3K-AKT-NF-κB, MEK1/2, and ERK1/2 axes. In addition, Gα subunit also activates the Ras and Rac/Rho pathways, leading to the phosphorylation of ERK and P38 proteins, respectively (Vlahakis et al., 2002). Activated ERK can phosphorylate and regulate other cellular proteins, as well as translocate into the nucleus and phosphorylate and regulate transcription factors, leading to changes in gene expression and cell cycle progression.
Homodimerization of CXCR4 has been suggested to result in G-protein-independent signaling through the JAK/STAT signaling pathway (Mellado et al., 2001; Vila-Coro et al., 1999). JAK/STAT pathway, possibly in conjunction with other signaling pathways, promotes changes in cell morphology, collectively known as polarization, leading to chemotactic responses (Mellado et al., 2001).
In addition to these general signaling cascades, other chemokine-specific signaling mechanisms also exist, making the outcomes of specific targeting of these pathways unpredictable. Even though several chemokine-targeted agents are in use, redundancy in chemokine signaling suggests that receptor-targeted strategies that eliminate redundant functions of chemokine signalingmay have greater effect than agents that solely target the effects of chemokines.
3. EXPRESSION AND PHYSIOLOGICAL FUNCTIONS OF THE CXCR4/CXCL12 AXIS
CXCR4 is commonly expressed on most hematopoietic cell types including macrophages, monocytes, T and B lymphocytes, neutrophils, hematopoietic, endothelial progenitor, and stem cells in the blood or bone marrow, dendritic cells, Langerhans cells (Bleul et al., 1996; Zabel et al., 1999), vascular endothelial cells (Gupta, Lysko, Pillarisetti, Ohlstein, & Stadel, 1998), neurons and neuronal stem cells (Hesselgesser et al., 1997), microglia and astrocytes (He et al., 1997), as well as embryonic stem cells (Kucia et al., 2005; Ratajczak et al., 2003). CXCR4-expressing cells respond to and migrate along CXCL12 gradients and contribute to several physiological functions and organ development (Kucia et al., 2004; Zou, Kottmann, Kuroda, Taniuchi, & Littman, 1998).
The chemokine CXCL12, an effective lymphocyte chemoattractant and hematopoiesis regulator (Aiuti, Webb, Bleul, Springer, & Gutierrez-Ramos, 1997; Bleul, Fuhlbrigge, Casasnovas, Aiuti, & Springer, 1996; Ma et al., 1998; Zou et al., 1998), is a modulator of several biological processes through its interaction with CXCR4. CXCL12 is expressed and secreted in different organs such as the liver, lung, kidney, brain, and bone marrow where it retains or chemoattracts CXCR4-expressing cells (Janowski, 2009; Kucia et al., 2004; Yu et al., 2006). The CXCR4/CXCL12 axis is indispensable for cell migration during embryonic hematopoiesis, organogenesis, vascularization, and organ homeostasis (Petit, Jin, & Rafii, 2007; Ratajczak et al., 2006; Schober & Zernecke, 2007). CXCR4 or CXCL12 knockout mice show significant defects in hematopoiesis, heart, blood vessels, and brain. Ablation of either CXCR4 or CXCL12 gene is lethal at embryonic stage (Lazarini, Tham, Casanova, Arenzana-Seisdedos, & Dubois-Dalcq, 2003; Ma et al., 1998; Nagasawa et al., 1996; Ratajczak et al., 2006; Vagima et al., 2011) underscoring the importance of this axis in organ development and physiological function. The CXCR4/CXCL12 axis also plays an important role in inflammation and immune surveillance of tissues (Viola & Luster, 2008). Different tissue damaging conditions, such as hypoxia, toxins, or irradiation, increase the expression of CXCL12, thereby recruiting CXCR4-positive stem cells to the site that requires tissue repair or regeneration (Gambaryan et al., 2011; Kucia et al., 2004; Ratajczak et al., 2006; Yu & Hales, 2011). Vital roles of the CXCR4/CXCL12 axis in normal biological processes suggest a cautious approach for therapeutic targeting.
CXCR4 and CXCL12 are highly conserved between species such that the amino acid sequence homology between human and murine CXCR4 and CXCL12 is 91% and 99%, respectively (Heesen, Berman, Benson, Gerard, & Dorf, 1996; Schabath et al., 1999). Very few mutations in CXCR4 have been reported. A specific dominant germline mutation in CXCR4 gene causes WHIM syndrome (Warts, Hypogammaglobulinemia, Infections, and Myelokathexis) (Bachelerie, 2010; Hernandez et al., 2003), a immunodeficiency disorder characterized by neutropenia. Following CXCL12 stimulation, the C-terminal mutations (both nonsense and frameshift have been observed) block receptor internalization due to distal truncations of the receptor’s carboxy terminal tail that removes potential phosphorylation sites involved in the receptor attenuation or desensitization processes. This results in persistent CXCR4 activation and failure of mature neutrophils to reach the bloodstream from bone marrow, leading to neutropenia.
First ever somatic mutations in CXCR4 in cancer were recently identified by Hunter et al. (2012) in 27% of Waldenström macroglobulinemia (WM), an indolent B-cell malignancy, patients. While several nonsense and frameshift mutations were identified in the C-terminus, most frequent mutations were observed at S338 of CXCR4. The recent success in treating WHIM patients with very low doses of the CXCR4 inhibitor (AMD3100/plerixafor at 001–0.02 mg/kg) (McDermott et al., 2014) suggests that similar targeted therapy approaches could be used for WM patients.
In addition to cancer, the CXCR4/CXCL12 axis is implicated in the pathology of several diseases due to its role in mediating the immune cell movement. Role of CXCR4 in autoimmune and inflammatory diseases can be found elsewhere (Buckley et al., 2000; Choi, Duggineni, Xu, Huang, & An, 2012; Chong & Mohan, 2009; Chung et al., 2010; Debnath, Xu, Grande, Garofalo, & Neamati, 2013; De Klerck et al., 2005; Gulino, 2003; Hsu, Rosenquist, Ansari, & Gershwin, 2005).
4. ROLE OF CXCR4 IN CANCER
Although initial studies were centered on the participation of CXCR4 in HIV infection of T-cells, its connection to cancer became an intense research topic with the discovery of its involvement in B-cell trafficking and tissue localization in chronic leukemia patients (Burger, Burger, & Kipps, 1999; Mohle, Failenschmid, Bautz, & Kanz, 1999) as well as regulation of organ-specific metastasis in breast cancer models (Muller et al., 2001). CXCR4 is overexpressed in more than 23 different types of human cancers including kidney, lung, brain, prostate, breast, pancreas, ovarian, and melanomas and contributes to the tumor growth, angiogenesis, metastasis, and therapeutic resistance (Balkwill, 2004b; Darash-Yahana et al., 2004; Furusato, Mohamed, Uhlen,& Rhim, 2010; Muller et al., 2001; Vandercappellen, Van Damme, & Struyf, 2008; Zlotnik, 2008).
Cancer cells are thought to hijack the CXCR4/CXCL12 axis to establish distant organ metastasis. Supporting this hypothesis, CXCL12 expression levels are highest in common sites of metastasis such as brain, bone marrow, lungs, and liver (Ho, Shiwen, Abraham, Tsui, & Baker, 2012; Janowski, 2009; Muller et al., 2001; Yu et al., 2006). Further supporting this hypothesis, abrogation of the CXCR4/CXCL12 axis results in reduced metastatic burden in a variety of mouse models of cancer.
Elevated CXCR4 expression observed in several cancers has been identified as a poor prognostic biomarker and will be discussed in detail in the later sections. Several factors contribute to the upregulation of CXCR4 in malignant cells. Notably, the hypoxia-inducible factor (HIF)-1α (Ishikawa et al., 2009; Zagzag et al., 2006), growth factors such as basic fibroblast growth factor, vascular endothelial growth factor (VEGF) (Salcedo et al., 1999), and epidermal growth factor (EGF) (Phillips et al., 2005), and transcription factors like nuclear respiratory factor-1 (Wegner et al., 1998) positively upregulate CXCR4 expression.
The CXCR4/CXCL12 axis plays a critical role in therapeutic resistance by (i) directly promoting cancer cell survival, invasion, and cancer stem (or tumor-initiating) cell phenotype; (ii) recruiting myeloid bone marrow-derived cells to indirectly facilitate tumor recurrence and metastasis; and (iii) promoting angiogenesis directly or in a paracrine manner (Duda et al., 2011; Teicher, 2011). Several studies have also identified increased expression of CXCR4 in cancer-associated fibroblasts (CAFs), which play an important role in tumorigenesis and have been implicated in neoplastic progression, tumor growth, angiogenesis, and metastasis (Eck, Cote, Winkelman, & Brinckerhoff, 2009; Kojima et al., 2010; Orimo et al., 2005). Data from these studies suggest that soluble breast cancer factors initiate the transdifferentiation of normal human mammary fibroblasts to tumor-promoting CAFs through the induction of matrix metalloproteinase-1 (MMP-1) and CXCR4 expression (Kwong, Kulbe, Wong, Chakravarty, & Balkwill, 2009). Similarly, the CXCR4/CXCL12 axis is critical for mesenchymal stem cell recruitment to the tumors (Domanska et al., 2012). In mouse models of human breast cancer (Orimo et al., 2005) and prostate cancer (PCa) (Olumi et al., 1999), high intratumoral CXCL12 levels have been shown to attract CXCR4-positive inflammatory, vascular, and stromal cells into the tumors, where they eventually support tumor growth by secreting growth factors, cytokines, chemokines, and proangiogenic factors.
In addition to contributing to the tumor–stromal interactions, CXCR4 is also expressed on cancer stem-like cells and contributes to cancer recurrence. Recent studies have shown the presence of a small subset of cancer cells, with very similar characteristics to stem cells, known as cancer stem cells (CSCs), which mediate tumor growth, metastasis, recurrence, as well as therapeutic resistance (Baccelli & Trumpp, 2012; Baumann, Krause, & Hill, 2008; Peitzsch, Kurth, Kunz-Schughart, Baumann, & Dubrovska, 2013). CXCR4 expression in CSCs confers increased invasiveness and metastatic potential as well as improved self-renewal and survival capacity (Gatti et al., 2013; Hermann et al., 2007). Hermann et al. (2007) reported that in the invasive front of pancreatic tumor, CD133+ pancreatic CSCs contained a subpopulation, characterized by CXCR4 coexpression, capable of evading the primary tumor and establishing distant metastases. The role of CXCR4 signaling in CSC survival and self-renewal was further demonstrated by Gatti et al. (2013) in human glioblastoma stem-like cells using the CXCR4 antagonist AMD3100, which reduced self-renewal and survival with greater efficacy in the cultures releasing higher levels of CXCL12.
Expression, specific involvement, and therapeutic targeting of CXCR4 in different types of cancers will be discussed in detail in the following sections.
4.1. Leukemia
Leukemia causes approximately 281,500 deaths annually and represents roughly 3% of all cancer deaths in the world (Lozano et al., 2012). Spoo, Lubbert, Wierda, and Burger (2007) reported that CXCR4 expression in acute myeloid leukemia cells in patients varied from low (n = 32), medium (n = 26) to high (n = 32) and that CXCR4 expression is an independent prognostic predictor of disease relapse. Similar observations were made in other hematological cancers such as chronic myeloid leukemia (CML), acute myelogenous leukemia (AML), and multiple myeloma (MM) (Barretina et al., 2003; Ko et al., 2014; Konoplev et al., 2011; Peled & Tavor, 2013), where CXCR4 expression on cancer cells contributed to therapeutic resistance (Chen et al., 2013; Sison, McIntyre, Magoon, & Brown, 2013). In chronic lymphocytic leukemia (CLL), CXCR4-expressing cancerous B-cells are attracted toward bone marrow stromal cells, which secrete high levels of CXCL12 (Burger et al., 1999), resembling the homing of normal hematopoietic stem cells to bone marrow (Burger & Peled, 2009; Konopleva & Jordan, 2011). The CXCR4/CXCL12 interaction within the bone marrow microenvironment protects the cancer cells from chemotherapy-induced apoptosis (Burger, 2010; Nervi et al., 2009). Stromal cells exert the protective effects, at least partially, through phosphorylation of PI3K/AKT, MAPK, and ERK (Zeng et al., 2009). In addition, the CXCR4/CXCL12 axis promotes tumor cell invasion in the stromal layer, thereby facilitating attachment to the stromal cells (Burger & Peled, 2009; Meads, Hazlehurst, & Dalton, 2008). Active adhesion molecules, such as integrins, convey prosurvival signals to the malignant cells, leading to adhesion-mediated drug resistance. Because CXCR4/CXCL12 interactions are crucial for homing of tumor cells to the bone marrow microenvironment and drug resistance, CXCR4 antagonists have been explored as chemosensitizers in leukemia treatment (Dillmann et al., 2009; Nervi et al., 2009). The CXCR4 inhibitor plerixafor is used in combination with other chemotherapy drugs, to disrupt cancer cell adhesion to the stromal cells (Dillmann et al., 2009), leading to mobilization of cancer cells into systemic circulation and subsequent exposure to the cytotoxic chemotherapeutic agents (Nervi et al., 2009). AMD3100 is also the first FDA-approved CXCR4 antagonist used to mobilize hematopoietic stem cells from bone marrow for collection and subsequent autologous transplantation in non-Hodgkin’s lymphoma and MM patients (DiPersio et al., 2009; DiPersio, Uy, Yasothan, & Kirkpatrick, 2009).
4.2. Multiple myeloma
Although MM is relatively rare, it is the second most prevalent hematological cancer after non-Hodgkin’s lymphoma (Collins, 2005), accounting for 114,251 new cases and 80,015 deaths each year (WHO, 2012). CXCR4 overexpression was detected in 43.2% of MM patients (Bao et al., 2013). CXCL12 and CXCR4 have been shown to be involved in cancer cell homing and migration in MM by attracting and activating plasma cells in bone marrow (Alsayed et al., 2007). The CXCR4/CXCL12 axis plays an important role on the biological behavior of MM cells by mediating the effect of adhesion molecules such as ICAM-1, integrin α4β1 (Li et al., 2003; Parmo-Cabanas et al., 2004). MM patients overexpressing CXCR4 were shown to be more sensitive to therapy with significantly longer median survival time than CXCR4-negative patients (48 months vs. 42 months, respectively, P< 0.05) (Bao et al., 2013; Pei et al., 2011; Stessman et al., 2013). The CXCR4 antagonist 4F-benzoyl-TN14003 (BKT140) was shown to inhibit MM tumor growth (Beider et al., 2011). Taking advantage of the CXCR4 expression in MM cells, Kuhne et al. (2012) demonstrated that MDX-1338, a fully humanized anti-CXCR4 antibody, significantly inhibited proliferation of MM cell lines in vitro and reduced tumor growth of MM xenografts in mouse models. CXCR4 antagonists, AMD3100 and BKT140, are used either alone or in combination with G-CSF to mobilize hematopoietic stem cells for autologous transplantation following high-dose chemotherapy (Lanza et al., 2014; Peled et al., 2014; Steinberg & Silva, 2010).
4.3. Breast cancer
Breast cancer is the most prevalent invasive cancer in women worldwide. It comprises 16% of all female cancers causing approximately half a million deaths every year (WHO, 2014a). The concept of cancer cells hijacking chemokine receptor pathways was first demonstrated in breast cancer models (Muller et al., 2001). It is now well established that the CXCR4/CXCL12 axis plays an important role in regulation of breast tumor growth, invasion, and metastasis (Liang et al., 2005, p. 89; Muller et al., 2001). Most breast tumors express higher levels of CXCR4 with very low expression levels reported in normal breast tissues. While all breast tumor tissues have some level of CXCR4 expression, more than 40% of the tumors have elevated CXCR4 levels (Salvucci et al., 2006). This expression also increases with tumor grade from 20% in normal breast tissue to 43% in ductal carcinoma in situ (DCIS) to 67% in invasive cancer (Salvucci et al., 2006). More importantly, nearly 75% of triple-negative (TN) breast cancer patients express high levels of activated CXCR4 (Chu et al., 2010; Hassan et al., 2009). A meta-analysis by Xu, Shen, Liu, and Shu (2013) showed that overall survival (OS) and disease-free survival (DFS) in breast cancer patients were negatively correlated to CXCR4 expression, with the hazard ratios (HRs) being 1.65 (95% CI: 1.34–2.03; P< 0.00001) and 1.94 (95% CI: 1.42–2.65; P< 0.00001), respectively. CXCR4 is one of the few genes that is highly enriched in metastatic breast cancer subpopulation and significantly overexpressed in bone metastases (Kang et al., 2003; Liang et al., 2005). Overexpression of CXCR4 in primary tumors is directly correlated to the degree of lymph node metastasis and poor survival rates in breast cancer patients (Kang, Watkins, Douglas-Jones, Mansel, & Jiang, 2005; Kato, Kitayama, Kazama, & Nagawa, 2003). The CXCR4/CXCL12 axis transactivation of HER-2 receptor and upregulation of CXCR4 are essential for HER-2-mediated metastasis (Balkwill, 2004a; Cabioglu et al., 2005). A study by Holm et al. demonstrated that CXCR4 overexpression occurs in most breast cancer patients. HER-2-negative breast tumors with higher levels of CXCR4 expression exhibit more aggressive behavior and are more likely to recur compared to tumors with lower CXCR4 expression (Holm et al., 2007). Similarly, CXCR4 has been shown to mediate estrogen-independent tumorigenesis, metastasis, and resistance to endocrine therapy. CXCR4 overexpression is correlated with worse prognosis and decreased patient survival rates, irrespective of the ER status (Rhodes et al., 2011). Involvement of CXCR4 in breast cancer invasion and metastasis was further supported by the findings that blocking the CXCR4/CXCL12 axis by low molecular weight (LMW) agents, peptides, or antibodies inhibited tumor growth and metastasis in breast cancer models (Huang et al., 2009; Muller et al., 2001; Smith et al., 2004). Similar results were also observed with siRNA-based downregulation of CXCR4 in breast cancer cell lines and mouse xenograft models (Liang et al., 2005).
4.4. Prostate cancer
PCa has the highest incidence among men in the United States (CDC, 2013). Although early detection improves prognosis, majority of PCa patients eventually develop bone metastasis. CXCR4 is one of the crucial factors involved in the bone metastasis of PCa (Gladson & Welch, 2008; Wang et al., 2005). Nearly 90% of all PCas exhibit high levels of CXCR4 resulting in poor clinical outcome (Akashi et al., 2008). Increased CXCR4 expression in PCas is associated with an aggressive phenotype and poor patient survival rates (Akashi et al., 2008). High-density prostate tumor tissue microarray analyses have revealed that (a) levels of CXCR4 protein expression in the malignant epithelia is greater than that of benign epithelia; (b) both prostatic intraepithelial neoplasia and some atrophic lesions, thought to be potentially precancerous, demonstrate positive staining for CXCR4; (c) CXCR4 expression increases with increasing tumor aggressiveness; and (d) metastases have elevated CXCR4 expression compared to primary tumors (Sun et al., 2003). In addition, the CXCR4/CXCL12 axis regulates the angiogenic phenotype in PCa (Darash-Yahana et al., 2004). As a result, CXCR4 expression has been proposed as a prognostic factor and considered a therapeutic target in PCa (Darash-Yahana et al., 2004; Wang et al., 2005). The CXCR4/CXCL12 interaction and subsequent downstream signaling pathways elicit multiple responses in PCa cells. CXCL12 treatment of human PCa cell line PC3 results in MEK/ERK signaling and activation of NF-κB, which are important for tumor cell survival (Fernandis, Cherla, Chernock, & Ganju, 2002). CXCR4/CXCL12 interaction, through upregulation of integrins, increases the attachment of PCa cells to the endothelial cell layer or to the stromal collagen, fibronectin, and laminins (Engl et al., 2006; Kukreja, Abdel-Mageed, Mondal, Liu, & Agrawal, 2005). In vivo studies in animal model of PCa metastasis demonstrated that CXCR4 inhibitory antibody reduces the extent of metastases to bones and CXCR4-blocking peptide limits intraosseous growth of PCa (Sun et al., 2005). CXCL12 is highly expressed in prostate tumor-associated blood vessels and basal cell hyperplasia (Darash-Yahana et al., 2004). Overexpression of CXCR4 in subcutaneous PC3 mouse xenografts induced greater vasculature and invasiveness of tumor cells into the adjacent tissues. On the other hand, CXCR4 inhibitory antibody blocked CXCR4-dependent vascularization and tumor growth (Darash-Yahana et al., 2004). In addition, inhibition of CXCR4/CXCL12 signaling by antibodies, peptide analogues, or small molecules has been found to reduce metastatic burden in various orthotopic and metastatic mouse xenograft models of PCa (Porvasnik et al., 2009; Sun et al., 2005; Taichman et al., 2002). The above findings illustrate the importance of CXCR4/CXCL12 interaction in tumor growth and metastasis of PCa.
4.5. Ovarian cancer
Ovarian cancer is the fifth leading cause of cancer deaths in women with <25% 5-year survival rates in the United States alone (ACS, 2014). Ovarian cancers often metastasize to lymph nodes, uterus, fallopian tube, and lungs. Advanced or metastatic ovarian cancers express high levels of CXCR4 and CXCR4/CXCL12 interactions are shown to regulate metastasis of epithelial ovarian cancer (EOC) (Barbolina et al., 2010). Nearly 59% of ovarian tumors are positive for CXCR4 (Jiang, Wu, Shi, Wu, & Yin, 2006). A recent meta-analysis showed that higher CXCR4 expression in ovarian cancer is associated with a poor progression-free survival (HR, 8.48; 95% CI: 2.13–33.70; P = 0.002) and a lower OS (HR, 2.81; 95% CI: 1.16–6.80; P = 0.022) (Liu et al., 2014). The CXCL12/CXCR4 axis together with multiple other factors regulates tumor growth and metastasis in ovarian cancer. Increased CD164 expression is reported to be involved in ovarian cancer progression via the CXCL12/CXCR4 axis (Huang et al., 2009). Concomitant expression of CD40 and CXCR4 in ovarian carcinoma tissues strongly correlates with pelvic metastasis (Qu et al., 2013). Higher expression of CXCL12, seen in 20% of the ovarian tumors, has also been demonstrated to enhance ovarian cancer cell invasion through αvβ6-mediated urokinase-type plasminogen activator expression via the p38 MAPK and PI3K/AKT pathways (Xue et al., 2013). In ascites isolated from ovarian cancer patients, both CXCR4 and CXCL12 were shown to be regulated by the tumor-associated inflammatory mediator prostaglandin E2 (PGE2), which induces chemotaxis of myeloid-derived suppressor cells into the ascites’ microenvironment (Obermajer, Muthuswamy, Odunsi, Edwards, & Kalinski, 2011), contributing to therapeutic resistance.
In vitro knock down of CXCR4 by small interfering RNA reduced cell proliferation while increasing apoptosis and chemosensitivity in EOC cell lines (Chen et al., 2012). Inhibition of CXCR4 by AMD3100 has been shown to delay CXCR4-mediated metastasis and invasion of EOC (Kajiyama et al., 2008). Similarly, the CXCR4 antagonist peptide CTCE-9908 increased the cytotoxicity of paclitaxel by inducing mitotic catastrophe in ovarian cancer cell lines (Kwong et al., 2009).
4.6. Lung cancer
Lung cancer is the most common cancer in the world and the leading cause of cancer-related death in the United States (ACS, 2014). Nonsmall-cell lung cancer (NSCLC) accounts for 85–90% of lung cancer cases with a 5-year survival rate of 15% (Siegel, Naishadham, & Jemal, 2012). Metastatic spread accounts for >70% of NSCLC deaths with the major sites of NSCLC metastasis being brain, bone, adrenal gland, and liver (Hubbard, Fu, Margevicius, Dowlati, & Linden, 2012; Murthy et al., 2010; Saintigny & Burger, 2012; Triano, Deshpande, & Gettinger, 2010). Numerous studies have established a strong correlation between CXCR4 expression and poor prognosis in NSCLC (Burger, Stewart, Wald, & Peled, 2011; Saintigny & Burger, 2012; Spano et al., 2004; Su et al., 2005; Wagner et al., 2009). CXCR4 expression levels are elevated in primary and metastatic tumor tissue compared to normal lung. In NSCLC, disease prognosis correlates with localization of CXCR4 to the nuclear and/or the cytomembranous compartment (Spano et al., 2004; Su et al., 2005; Wagner et al., 2009). Higher CXCR4 expression in cytomembranous compartment is correlated with a higher tendency to locally invade neighboring tissues and with increased propensity of tumor cells to form distant metastases. CXCR4 overexpression in cytomembranous compartment is also linked to greater density of microvasculature in tumors and associated with increased microvessel invasion by tumor cells (Franco et al., 2011; Su et al., 2005). Cytomembranous overexpression of CXCR4 is also associated with poor survival in stage IV NSCLC patients (Otsuka et al., 2011). On the contrary, stronger nuclear CXCR4 expression was linked with better outcomes in early-stage patients (Spano et al., 2004). CXCL12 is also overexpressed in NSCLC in more than 80% of cases (Wald et al., 2006) and elevated CXCL12 expression was correlated with higher recurrence rate and lymph node metastasis (Wagner et al., 2009). Overall, these findings demonstrate the crucial role of the CXCR4/CXCL12 axis in tumor growth and metastasis of NSCLC.
CXCR4 expression in lung cancer is modulated by other tumor microenvironmental factors such as hypoxia or the EGF (Liu et al., 2009). In NSCLC cells, increase in CXCR4 expression due to activation of EGF receptor (EGFR) is remarkably enhanced under hypoxic conditions. Augmented expression of CXCR4 is regulated by the PI3K/PTEN/AKT/mammalian target of rapamycin (mTOR) signal transduction pathway which upregulates HIF-1α and increases CXCR4 gene transcription (Phillips et al., 2005).
The in vitro cisplatin treatment of NSCLC cells results in enrichment of the cell population positive for CD133, a marker for CSCs. Supporting these observations, in vivo cisplatin treatment of NSCLC xenografts derived from primary tumors also demonstrated an enrichment of a subpopulation of CD133+/CXCR4+ cells (Bertolini et al., 2009) suggesting involvement of CXCR4 in chemotherapy resistance and recurrence of lung cancer.
Small-cell lung cancer (SCLC) accounts for nearly 13% of lung cancers. SCLC often presents with extensive spread of the disease. Although investigated in only a few patients, CXCR4 is highly expressed in all the tested cases. CXCR4 is also overexpressed in almost all SCLC cell lines. Activation of the CXCR4/CXCL12 axis induces actin polymerization and activation of MAPK signaling, leading to firm adhesion of SCLC cells to the surrounding extracellular matrix (ECM) of stromal cells (Burger et al., 2003; Sethi et al., 1999). This increased adhesive interaction between SCLC and ECM of stromal cells increases the expression of β1, α3, α6, and αv integrins, as well as increased tyrosine-kinase activity that prevents caspase activation, resulting in decreased chemotherapy-induced cell death (Sethi et al., 1999). Furthermore, integrin activation increases MMP-9 expression and enhances the invasiveness of SCLC cells (Han, Ritzenthaler, Sitaraman, & Roman, 2006). Previously, CXCR4 was known to be involved in the activation of the JAK2/STAT3 pathway (Ahr, Denizot, Robert-Hebmann, Brelot, & Biard-Piechaczyk, 2005). It was found that due to CXCR4/CXCL12 activation, STAT3 always remains phosphorylated in SCLC cells. Blocking JAK2 or CXCR4 reduces cell growth in soft agar, demonstrating the role of CXCR4 and JAK2/STAT3 signaling in adhesion-independent SCLC cell growth (Ahr et al., 2005; Pfeiffer et al., 2009).
CXCR4 antagonists reduce the tumor growth and metastatic burden in lung cancer models (Fahham et al., 2012; Jung et al., 2013). Fahham et al. (2012) reported that targeting the CXCL12/CXCR4 axis with the antagonist BKT140 attenuated NSCLC cell tumor growth and augmented the effects of chemotherapy and radiotherapy. Taken together, CXCR4/CXCL12 plays an important role in tumor growth, invasion, metastasis, chemoresistance, and relapse of lung cancer, and CXCR4 antagonists combined with cytotoxic chemotherapy may improve the therapeutic response.
4.7. Gastrointestinal cancers
CXCR4 is involved in tumor growth and metastasis in various gastrointestinal cancers, in particular colorectal, pancreatic, hepatocellular, gastric, and esophageal cancers.
Each year, more than one million people are diagnosed worldwide with colorectal cancer (CRC), which is the fourth most common cause of cancer-related death (WHO, 2012). In colorectal cancer patients, CXCR4 expression in primary tumor cells correlates with survival, metastasis, and recurrence (Kim et al., 2006). All the CRC samples stained for CXCR4 by IHC were positive with nearly 58% demonstrating strong expression (Schimanski et al., 2005). Similarly, analysis of cell lines, 100 CRC tumors and 39 liver metastases by qRT-PCR demonstrated higher CXCR4 expression in the cell lines and tumors (Kim et al., 2005). Patients with high CXCR4-expressing tumors had increased risk of local recurrence and distant metastases, lymph node involvement, as well as significantly decreased OS (median, 9 months vs 23 months; log-rank P = 0.03) (Kim et al., 2005). Also, CXCR4 expression was higher in the liver metastases compared to primary tumors. In 12 of 14 paired tumors and metastases, CXCR4 expression was higher in the metastases than the primary tumor (Kim et al., 2005; Schimanski et al., 2005). These observations reiterate the role of CXCR4 expression in CRC growth, recurrence, and metastasis. Studies in an animal model using CT-26, a mouse colorectal cancer cell line, revealed that CXCR4 is important for metastasis of colon cancer to liver but not involved in tissue invasion (Zeelenberg, Ruuls-Van Stalle, & Roos, 2003). Interestingly, CXCR4 surface expression levels were found to be low or absent in colon cancer cell lines in vitro while high expression levels were observed in vivo in animal models of liver metastasis (Zeelenberg et al., 2003). These findings suggested that CXCR4 expression on colon cancer cells is regulated by tumor microenvironment and isolated metastatic cells utilize CXCR4 signaling for proliferation.
Pancreatic cancer has a very poor prognosis and limited early detection options with a 5-year survival of less than 5% (ACS, 2014). In pancreatic cancer, the CXCR4/CXCL12 axis plays an important role in tumor cell proliferation, migration, and angiogenesis. Nearly 85% of pancreatic tumor samples tested were positive for CXCR4 expression. Patients with high CXCR4-expressing tumors had a worse outcome than those with low CXCR4 expression with OS: 9.7 months (95% CI: 6.0–13.4) versus 43.2 months (95% CI: 16.3–78.1), P = 0.0006 (Marechal et al., 2009). In another study, high CXCR4 expression in pancreatic adenocarcinoma was observed to be an independent negative prognostic biomarker (HR = 1.74; P<0.0001) and associated with distant relapse (HR = 2.19; P<0.0001) (Bachet et al., 2012, 2012). Also, a subpopulation of CSCs expressing CD133 and CXCR4 in invasive pancreatic tumors was found to be the determinant of metastasis (Hermann et al., 2007). While HIF-1α is known to be a major factor contributing to CXCR4 expression in pancreatic and other cancers, recent studies in pancreatic cancer cells and tumors demonstrated that transcription factors such as SOX9 upregulate CXCR4 expression independently of HIF-1α, which may have consequences not only for pancreatic cancer but also for other cancers such as SCLC where SOX transcription factors are known to be overexpressed (Camaj et al., 2014). CXCR4 antagonist AMD3100 significantly inhibited the proliferation, migration, and invasion of pancreatic cancer cells (Gao, Wang, Wu, Zhao, & Hu, 2010). Mori et al. (2004) reported that CXCR4 antagonist TN14003 inhibited the migration and invasion of pancreatic cancer cells. Singh, Srivastava, Bhardwaj, Owen, and Singh (2010) demonstrated that inhibition of the CXCR4/CXCL12 axis by AMD3100 arrested the pancreatic cancer cell growth and abrogated gemcitabine resistance. Ma, Hwang, Logsdon, and Ullrich, 2013 showed that AMD3100 treatment reduced tumor growth in animal models of pancreatic ductal adenocarcinoma by blocking CXCR4-dependent mast cell migration.
Hepatocellular carcinoma (HCC) is one of the most common cancers and causes 745,000 deaths each year (WHO, 2014b). Roughly, 50% of HCC tumor specimens were identified as CXCR4 positive (Xiang et al., 2009). In HCC, the expression of CXCR4 was found to be correlated with tumor progression, lymphatic metastasis, distant dissemination, and a reduced 3-year survival rate (Schimanski et al., 2006). The CXCR4/CXCL12 axis was reported to regulate angiogenesis, essential for growth and progression of HCC (Li, Gomez, & Zhang, 2007). Li et al. (2007) found a higher expression of the CXCL12 and CXCR4 in sinusoidal endothelial cells in HCC specimens than in normal liver tissues. Findings by Mavier et al. (2004) suggested that CXCR4/CXCL12 axis promotes the proliferation of oval cells and abnormal differentiation of these cells may be associated with HCC. A study by Chu et al. (2007) indicated that the CXCR4/CXCL12 axis mediates active MMP-9 and MMP-2 secretion, thereby facilitating metastasis. CXCR4 inhibition by AMD3100 in combination with sorafenib treatment was reported to inhibit HCC growth (Chen et al., 2014).
In esophageal cancer, CXCR4 expression was found to be correlated with increased lymph node and bone marrow metastases (Sasaki et al., 2008). Approximately 85% of esophageal cancer tumors are CXCR4 positive (Sasaki et al., 2009). A study by Gockel et al. (2006) showed that patients with CXCR4-expressing tumors have a lower median OS of 20 months compared to a median OS of 76 months for patients with CXCR4-negative tumors. Supporting these observations, CXCR4 gene silencing by lentivirus shRNA inhibited proliferation of the EC9706 human esophageal carcinoma cell line and reduced the growth of tumor xenografts in mouse models (Wang, Lou, Qiu, Lin, & Liang, 2013).
Gastric and stomach cancers cause 723,000 deaths every year (WHO, 2014b) and have a poor prognosis with less than 10% 5-year survival rate (Orditura et al., 2014). Positive staining for CXCR4 was identified in 80% of the primary gastric tumor tissues (Han et al., 2014). CXCR4 expression in primary gastric carcinomas is associated with the development of peritoneal carcinomatosis and malignant ascites which contained high levels of CXCL12 (Yasumoto et al., 2006). CXCR4 expression in primary gastric tumors was positively correlated with lymph node metastasis (Ying, Xu, Zhang, Liu, & Zhu, 2012). A meta-analysis by Han et al showed that CXCR4 expression is associated with poor prognosis in gastric cancer patients. In this study, OS was found to significantly correlate with CXCR4 expression, with the HR of 2.63 (95% CI: 1.69–4.09; P<0.0001), and a significant association was also detected between CXCR4 expression and tumor stage (odd ratio (OR): 0.52, 95% CI: 0.32–0.83; P = 0.007), depth of invasion (OR: 0.44, 95% CI: 0.27–0.73; P = 0.001), lymph node metastasis (OR: 2.30, 95% CI: 1.57–3.36; P<0.0001), and vascular invasion (OR: 0.72, 95% CI: 0.53–0.98; P = 0.04) (Han et al., 2014). Fakhari et al. (2014) reported that Helicobacter pylori infection increased CXCL12 secretion by gastric epithelial cell line, upregulated CXCR4 expression in bone marrow-derived-mesenchymal stem cells, and enhanced their migration toward CXCL12 gradient. Findings by Oh et al. (2012) indicate that hypoxia upregulates CXCR4 in gastric cancer cells in a HIF-1α-dependent manner and that upregulation of CXCR4 is involved in gastric cancer cell migration and invasion. Iwanaga et al. showed that CXCR4 blockers AMD3100 and KRH3955 inhibited the growth of gastric cancer xenografts in a mouse model (Iwanaga, Iwasaki, Ohashi, Nunobe, & Iwagami, 2007; Iwanaga et al., 2012).
4.8. Renal cell carcinoma
Nearly 337,860 new cases of renal cancer are diagnosed and an estimated 143,369 related deaths are reported every year in the world (WHO, 2012). The majority of reported renal cell cancer (RCC) cases are clear cell renal cell carcinoma (ccRCC). Loss of function of the von Hippel–Lindau (VHL) tumor suppressor protein is the genetic hallmark of most ccRCCs (Zagzag et al., 2005). Native VHL targets HIF-1α for degradation under normoxic conditions. In ccRCCs with known VHL mutation, this process is suppressed due to loss of function of VHL or hypoxic conditions, leading to stabilization of HIF-1α and enhanced CXCR4 expression through interaction of HIF-1α with the promoter region of the CXCR4 gene (Staller et al., 2003; Zagzag et al., 2005). As such, CXCR4 is highly overexpressed in ccRCC. In a recent study, CXCR4 expression was found in 65.4% of ccRCC patients with 36.8% demonstrating strong immunoreactivity (Li et al., 2013). High CXCR4 expression was associated with a poor prognosis in ccRCC patients (Li et al., 2013). A significant aspect of VHL mutation is that it does not automatically drive ccRCC into metastasis or correlate with poor clinical outcome, but rather it is the CXCR4 expression that contributes to poor prognosis (Vanharanta et al., 2013). Recent studies demonstrate that genes beneficial for tumor cell survival and metastasis, such as CXCR4 and CYTIP, are selected for and induced through selective epigenetic changes in polycomb repression complex 2 (PRC2), eventually driving the metastatic phenotype of a subpopulation of VHL-mutated ccRCCs (Vanharanta et al., 2013). In essence, CXCR4 expression is an important prognostic factor in ccRCCs (Li et al., 2013). Also, in patients with known metastatic RCC, CXCR4 was shown to be expressed on circulating pan-cytokeratin-positive RCC cells (Reckamp et al., 2009). Several studies in preclinical models also confirmed that the CXCR4/CXCL12 axis regulates invasiveness, angiogenesis, and organ-specific metastasis of RCC (D’Alterio et al., 2010; Gahan et al., 2012; Wang et al., 2012, 2009). CXCR4 expression in RCC is correlated with metastatic potential in orthotopic mouse models of human RCC xenografts (Pan et al., 2006). Abrogation of the CXCR4/CXCL12 axis through CXCR4 inhibition resulted in reduced metastasis to distant organs (Portella et al., 2013).
4.9. Melanoma
Melanoma is the malignant tumor of melanocytes, which mostly occurs on skin (Jerant, Johnson, Sheridan, & Caffrey, 2000). A study by Longo-Imedio, Longo, Trevino, Lazaro, and Sanchez-Mateos (2005) showed that CXCR4 expression by melanoma cells in primary lesions was correlated with increased tumor thickness, ulceration, higher risk of regional and distant metastases, and higher mortality rates. Scala et al. reported CXCR4 expression in 43.6% primary cutaneous melanomas of which the CXCR4 expression levels were low in 21%, moderate in 14%, and high in 8% of cases. Tumor cell CXCR4 expression correlated with an unfavorable prognosis with a median DFS of 22 months and OS of 35 months. CXCR4 expression was able to predict the prognosis for both DFS (P = 0.0154) and OS (P = 0.0009). In patients with CXCR4-positive tumors, the HRs of relapse and death, compared with patients with CXCR4-negative tumors, were 2.5 (95% CI) and 3.1 (95% CI), respectively (Scala et al., 2005).
The role of CXCR4 in lung-specific metastasis of melanoma cells was demonstrated by Murakami et al. The authors reported that murine B16 melanoma cells transduced with CXCR4 showed more than 10-fold increase in lung-specific metastasis, which was completely inhibited by T22, a small peptide CXCR4 antagonist (Murakami, Cardones, & Hwang, 2004; Murakami et al., 2002). CXCR4 and membrane-type 1 matrix metalloproteinase (MT1-MMP) were found to coordinate their activities at different stages during metastasis of melanoma cells to the lungs. CXCR4 was essential at initial phases of melanoma cell migration and homing to lungs. On the contrary, MT1-MMP was not required at the initial stage but helped subsequent dissemination and invasion of CXCR4-positive tumor cells (Bartolome et al., 2009). Similarly, metastasis of chemoresistant CXCR4+/CD133+ stem-like melanoma cells to the target organs is stimulated by secretion of CXCL12 from lymphatic vessels (Kim et al., 2010). Blockade of CXCR4 by AMD3100 coupled with cytotoxic drug dacarbazine significantly inhibited tumor growth and metastasis of melanoma compared to dacarbazine alone (Kim et al., 2010). Recently, another CXCR4 inhibitor AMD11070 was shown to abrogate melanoma cell migration significantly and more effectively than AMD3100 (O’Boyle et al., 2013).
4.10. Brain tumors
Several studies demonstrated that the CXCR4/CXCL12 axis is involved in tumor cell proliferation, angiogenesis, invasion, and metastasis in malignant gliomas as well as in other brain tumors. Brain tumor cell lines, primary tumors, and metastases have high concentrations of CXCR4 receptors compared to normal brain parenchyma (Rempel, Dudas, Ge, & Gutierrez, 2000; Rubin et al., 2003; Sehgal, Keener, Boynton, Warrick, & Murphy, 1998; Woerner, Warrington, Kung, Perry, & Rubin, 2005). Expression analysis using cDNA expression arrays revealed that CXCR4 is overexpressed in 57% of primary glioblastoma multiforme tumor tissues and in 88% of glioblastoma cell lines analyzed (Sehgal et al., 1998). CXCR4 and CXCL12 expression varies in glioma cells with low-grade tumors expressing intermediate level of CXCR4 and CXCL12 and advanced gliomas expressing higher levels of CXCR4 (Gagliardi et al., 2014; Rempel et al., 2000). The invading regions of glioblastomas and satellite tumors, which are the primary reason for recurrence, are also known to express high levels of CXCR4 (Zagzag et al., 2008). As such, CXCR4 expression is considered a prognostic marker in gliomas. In addition, patients with CXCR4-positive glioblastoma multiforme exhibited poorer postoperative life expectancy when compared to patients with CXCR4-negative tumors.
Schuller et al. (2005) showed that 17/18 and 6/7 of desmoplastic and nodular medulloblastomas have elevated CXCR4 expression. In another study, Smith et al. (2007) demonstrated that 80% of malignant B-cells from patients with primary central nervous system lymphoma stained positive for CXCL12 and CXCR4. More than 50% of astrocytomas, regardless of grade, were shown to be positive for CXCR4 expression. More importantly, 100% of expressed CXCR4 was present in the phosphorylated state (pCXCR4/CXCR4 ratio) in grades 2–4 astrocytomas compared with only 76% in grade 1 astrocytomas suggesting that staining for CXCR4 alone may not be sufficient but staining for activated CXCR4 may provide more information regarding the contribution of the CXCR4/CXCL12 axis to the tumor biology (Woerner et al., 2005).
CXCR4 expression in brain tumors is upregulated by factors such as HIF-1α and hepatocyte growth factor (Esencay, Newcomb, & Zagzag, 2010; Zagzag et al., 2008). CD133+/CXCR4+ glioma stem-like cells mediate VEGF production and promote tumor angiogenesis (Ping et al., 2011). Taking advantage of the CXCR4 expression observed in brain tumors, Rubin et al. (2003) demonstrated that systemic administration of the CXCR4 antagonist AMD3100 inhibits intracranial growth of glioblastoma xenografts by inducing apoptosis and reducing tumor cell proliferation. Furthermore, combination treatments, incorporating CXCR4 inhibition, have resulted in a synergistic effect with cytotoxic 1,3-bis(2-chloroethyl)-1-nitrosourea (BCNU)-based chemotherapy in glioblastoma models (Redjal, Chan, Segal, & Kung, 2006).
4.11. Soft tissue sarcomas
Soft tissue sarcomas are relatively rare cancers accounting for approximately 12,000 cases (0.7% of all cancer cases) and 4700 deaths (0.8% all cancer-related deaths) each year in the United States (ACS, 2014). Soft tissue sarcoma is one of the most therapy resistant forms of cancer. The neurofibromatosis type 1 (NF1) disorder, a genetic disorder of the nervous system, results in the development of neurofibrosarcomas called the malignant peripheral nerve sheath tumors (MPNSTs). MPNSTs have limited therapeutic options and a cause of significant mortality in NF1 patients. Tissue microarray analysis of NF1 tumors has indicated that 94% of neurofibromas, 98% of NF1-deficient MPNSTs, and 66% of sporadic MPNST tissues showed CXCR4 immunoreactivity (Mo et al., 2013). CXCR4 expression, in association with CXCL12, forms an autocrine loop and activates the AKT/GSK-3b/β-catenin pathway, resulting in malignant transformation of cells. In addition, CXCR4 downregulation or inhibition results in cyclin D1-mediated cytostatic effects on tumor growth (Mo et al., 2013) suggesting that inhibition of CXCR4 in these patient populations may have therapeutic benefit.
5. CXCR4 ANTAGONISTS AS THERAPEUTIC AND IMAGING AGENTS
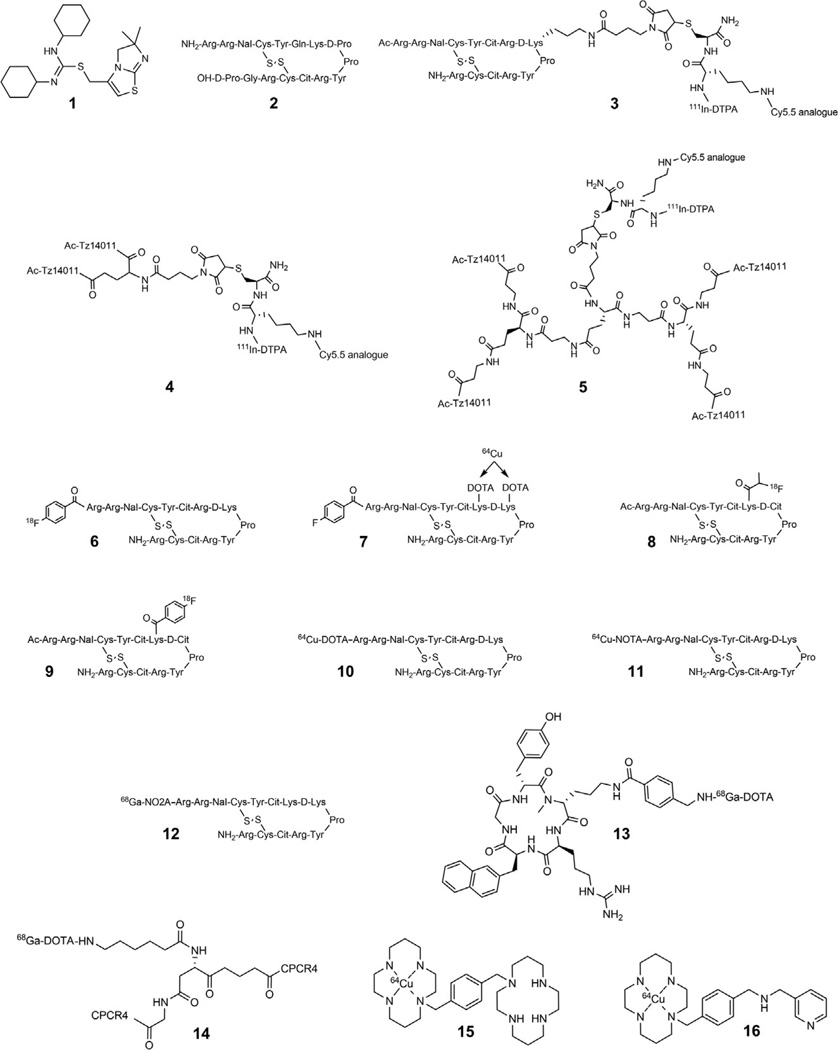
Considering the critical role of the CXCR4/CXCL12 axis in various disease states, there is currently significant interest in the discovery and development of antagonists and imaging probes for therapeutic targeting and noninvasive monitoring of CXCR4 expression. Reports on CXCR4 and CXCL12 NMR and homology models have contributed significantly to our understanding of CXCR4–ligand interactions, thereby facilitating the development of highly specific CXCR4 inhibitors. A recent study by Wu et al. (2010) described the crystal structure of ligand-activated human CXCR4, thereby further illuminating probable receptor-ligand binding modes. This study utilized three stabilized constructs of CXCR4, expressed in baculovirus-infected Spodoptera frugiperda (Sf9) insect cells, for structural evaluation based on thermal stability, monodispersity, and lipid matrix diffusion. The small-molecule isothiourea derivative (IT1t, Fig. 2.2-1) and the 16-amino acid cyclic peptide analogue CVX15 (Fig. 2.2-2), both potent CXCR4 ligands, were selected based on solubility, affinity, and thermostability. IT1t was shown to interact with side chains from helices I, II, III, and VII while making no contact with helices IV, V, and VI. Nitrogen 4, or potentially nitrogen 3 (in the flipped thiourea conformation), of the isothiourea group formed a salt bridge with the Asp97 residue, thus indicating the crucial role of both N4 and N3 as also previously illustrated by the drastic reduction in binding affinity (roughly 100-fold) following methylation of only one nitrogen atom (Thoma et al., 2008). In case of CVX15, the cyclic peptide fills most of the binding cavity volume and forms a disulfide-stabilized (Cys4–Cys13) β-hairpin structure with d-Pro8-Pro9 at the extracellular turn. Hydrogen bonding is observed between the N-terminus of the peptide and residues Asp187 to Tyr190 of the CXCR4 backbone. The NaI3 group is anchored into the hydrophobic region neighboring helix V. Arg14 in particular forms hydrogen bonds with Asp262 and Tyr5. The C-terminus d-proline establishes a water-mediated interaction with Asp288 of CXCR4. Although binding modes of the small-molecule inhibitor and peptidic ligand overlap to some extent, conformational variations in CXCR4 induced by latter are more pronounced. For instance, CVX15 binding induces structural reconfiguration in the base of the receptor N-terminus as well as the extracellular regions of the helices. The binding interaction of CXCL12 to CXCR4 takes place with the RFFESH loop of CXCL12α interacting with the N-terminus of CXCR4, while the N-terminus of CXCL12 simultaneously interacts with the binding pocket comprising the transmembrane helices and the extracellular loops (Zhong et al., 2013). While this study has shed more light on CXCR4–ligand interactions, the observed variability in binding modes has further complicated the rationale design and predictability of essential structural backbones necessary for production of high-affinity CXCR4 binding ligands. Currently, the majority of CXCR4-targeted scaffolds have been derived from optimization of preexisting compounds or library hits known to have sufficient affinity for CXCR4. Numerous agents, including peptide, small-molecule and antibody-based therapeutics, and imaging probes have been developed for the monitoring of CXCR4 expression, each of which will be discussed categorically in more detail in the following sections. Most of these agents have cationic parts that can bind chiefly anionic extracellular domains of CXCR4. Considering the large number of therapeutics and imaging agents reported, only those routinely used as therapeutics or for direct in vivo imaging of CXCR4 expression will be discussed. Existing CXCR4 antagonists can be broadly categorized into (1) peptide-based CXCR4 antagonists, (2) antibodies against CXCR4, and (3) LMW agents.
Figure 2.2.
Representative structures of CXCR4-targeted tracers employed in in vivo imaging applications.
6. PEPTIDES AND PEPTIDOMIMETICS
6.1. CXCL12-based peptides
CXCL12 binds both CXCR4 and CXCR7 receptors and is commonly utilized in in vitro competition binding assays and a natural choice to derive peptides that bind to CXCR4 (Kryczek, Wei, Keller, Liu, & Zou, 2007; Sun et al., 2011). As a result, several CXCL12-derived peptides were developed as therapeutics based on known CXCR4/CXCL12 interactions. CTCE-9908, a 17-amino acid peptide analogue of CXCL12, has been shown to reduce the growth and adhesion of tumor cells as well as metastatic dissemination of cancer cells in a variety of tumor models (Kim et al., 2008; Wong & Korz, 2008). Currently, CTCE-9908 is in phase I/II clinical trial in patients with advanced solid tumors (Wong & Korz, 2008). Spiegelmers are RNA oligonucleotides in l-configuration that can be selectively designed for a protein of choice. NOX-A12 is a PEGylated spiegelmer that binds and neutralizes CXCL12 and inhibits CXCR4/CXCL12 interactions. NOX-A12 was shown to mobilize stem cells in mice and humans and chemosensitize CLL cells through disruption of CXCR4/CXCL12 interactions (Vater et al., 2013). Furthermore, combination of NOX-A12 with bendamustine and rituximab is in phase II clinical trial for the treatment of relapsed CLL (NCI, 2014).
Similarly, CXCL12-based imaging agents are beneficial to both in vitro evaluation as well as in vivo imaging applications of chemokine receptor expression. Meincke, Tiwari, Hattermann, Kalthoff, and Mentlein (2011) reported the development and evaluation of an IRDye 800CW-CXCL12 conjugate, via optical imaging, in nude mice with MCF-7 breast (high expression of CXCR4 and CXCR7) and A764 glioma (high expression of only CXCR7) tumor xenografts. Both tumors were visible from 24 to 96 h post probe injection; however, significant nonspecific uptake was also observed in the liver, brain, and bone marrow. Images obtained 96 h p.i. indicated almost complete clearance of the tracer from nonspecific organs and A764 tumor, while maintaining retention in MCF-7 tumors.
Misra et al. (2008) reported the development and biological analysis of 99mTc-labeled CXCL12 for monitoring changes in CXCR4 expression before and after myocardial infarction (MI). The pharmacokinetics of [99mTc-MAS3]-CXCL12 were evaluated and quantified in Sprague-Dawley rats before and after experimentally induced MI. The tracer exhibited high CXCR4 specificity and affinity (2.7±0.9 nM) on the surface of living rat neonatal cardiomyocytes as well as rapid clearance within 2 h p.i. with less than 26.2±6.1% of injected dose remaining with low nonspecific uptake (<0.1%) in the liver, spleen, lung, and heart. Following MI induction, a 5-fold increase in tracer uptake was observed and correlated with increased CXCR4 expression, as indicated by confocal immunofluorescence, confirming the capability of this tracer to monitor CXCR4 expression prior to and following onset of MI. [99mTc-MAS3]-CXCL12 was not tested in cancer models.
6.2. Synthetic peptide CXCR4 antagonists
The development of current CXCR4-targeted peptide analogues has taken place over the past 23 years, starting with the discovery of the antiviral activity of tachyplesin I and II as well as polyphemusin I and II (isolated from Tachypleus tridentatus and Limulus polyphemus, respectively) against HIV-1 (Masuda et al., 1992; Miyata et al., 1989; Morimoto et al., 1991; Nakamura et al., 1988). Numerous lower molecular weight peptide analogues (e.g., T22, TW70, and T134) have since been developed exhibiting reduced cytotoxicity levels (Nakashima et al., 1992; Tamamura et al., 1998; Waki et al., 1996). Following the discovery of TC134, a high-affinity (IC50 = 4 nM for CXCR4) 14 amino acid cyclic structural analogue, T140, was developed, which has since been the cornerstone for the development of various peptide analogues such as CVX15 (IC50 = 0.6 nM) and Ac-TZ14011 (IC50 = 5.2 nM) (Tamamura et al., 2003, 1998). The latter has also been heavily utilized for molecular imaging applications of CXCR4 expression utilizing optical and nuclear imaging modalities.
Numerous in vitro and in vivo preclinical studies have established the efficacy of T140 and its analogues for blocking CXCR4 thus reducing tumor growth and metastasis in breast cancer, melanoma, chronic leukemia, MM, and pancreatic cancer mouse models (Burger, 2009).
The 14-residue polypeptide 4F-benzoyl-TN14003 (BKT140), derived from a naturally occurring horseshoe crab protein, exemplifies this category of peptides. BKT140 binds CXCR4 with high specificity and affinity (Tamamura et al., 2003). Beider et al. (2011) demonstrated that BKT140 treatment can significantly reduce acute myeloid leukemia and MM xenografts in animal models, while Peled et al. (2014) have shown that BKT140 treatment induces a robust mobilization of CD34+ cells in patients with MM. BKT140 in combination with imatinib, a tyrosine-kinase inhibitor, was shown to overcome the protective effects of stroma in CML models (Fahham et al., 2012). POL6326 is another selective CXCR4 peptidomimetic antagonist developed based on protein epitope mimetics technology (DeMarco et al., 2006; Lederer et al., 2007). POL6326 is in phase II trial in MM patients (Schmitt et al., 2010).
Peptides have been used as imaging agents owing to their relatively faster clearance compared to antibodies and simplified bifunctional chelation chemistry allowing for use of various radiometals. Based on the discussed peptide scaffolds, several peptide-based CXCR4 imaging agents were investigated. The group of van Lueewen has developed both mono and multimodality imaging agents encompassing Ac-TZ14011 analogues for CXCR4 imaging. In one report by Kuil, Buckle, Yuan, et al. (2011), Ac-TZ14011 was conjugated to DTPA for In-111 labeling and SPECT imaging, as well as a Cy5.5-like dye for optical imaging (Fig. 2.2-3). Flow cytometry and confocal microscopy demonstrated the receptor specificity of this dual modality peptide while SPECT–CT imaging in a mouse model bearing CXCR4-positive (MIN-O) and CXCR4-negative (4T1) tumors indicated CXCR4-specific tumor uptake. Although tumor uptake (%ID/g) values were not provided, tumor-to-muscle ratios of 4.55±0.68 and 1.20±0.12 for MIN-O and 4T1 tumors, respectively, were observed indicating enhanced uptake with targeting. Bunschoten et al. (2012) reported a 99mTc-labeled human serum albumin (HSA) nanoparticle coated with Ac-TZ14011 and the NIR dye IR783 for use in CXCR4-specific sentinel lymph node procedures. Tracer uptake in lymph nodes was confirmed by ex vivo detection of 99mTc-HSA and ex vivo fluorescence imaging of excised mouse lymph nodes, thereby illustrating the application of this probe for use in studying lymphatic drainage.
Kuil, Buckle, Oldenburg, et al. (2011) also reported the in vivo evaluation of dimeric and tetrameric Ac-TZ14011 analogues (Figs. 2.2-4 and 2.2-5) using a multifunctional single attachment point (MSAP) label which contained DTPA for In-111 conjugation and a Cy5.5-like fluorophore for optical imaging. Although peptide multimerization was shown to reduce nonspecific muscle uptake from 0.31±0.01 to 0.08±0.02, the tumor uptake (%ID/g) in MIN-O tumor-bearing mice was fairly consistent at 1.10±0.60. Of note was the higher toxicity and lower tumor-to-muscle ratios of the tetrameric compound (7.41±1.87 for the dimer vs. 5.47±0.50 for the tetramer) compared to the dimeric analogue. Buckle et al. (2012) reported the use of the 111In-labeled monomeric analogue to study the extent of CXCR4 expression in MIN-O mouse tumor models, which resemble human DCIS. Utilizing 111In-cDTPA-[RGDfK], the authors aimed to study and correlate CXCR4 expression with tumor angiogenesis. While CXCR4-expression levels were distinguished using 111In-Ac-TZ-14011, angiogenesis in MIN-O lesions and low CXCR4-expressing control tumors was too similar to differentiate.
A fluorine-18-labeled T140 analogue (Fig. 2.2-6) was reported by Jacobson, Weiss, Kiesewetter, Farber, and Chen (2010) and studied in mouse models bearing tumors of CHO cells stably transfected with CXCR4. While this tracer did exhibit some receptor-specific accumulation in the CXCR4-positive tumor, it also significantly bound to red blood cells, requiring the coinjection of cold peptide for direct in vivo tumor visualization. The highest tumor %ID/g obtained following this methodology was 3.03±0.31. Jacobson et al. (2011) later reported the development of a Cu-64-labeled T140 analogue which was substituted with two DOTA molecules at both lysine residues in the peptide backbone (Fig. 2.2-7). This tracer also suffered from the same limitation as the F-18T140 analogue and was administered with a low specific activity to circumvent red blood cell uptake. While the Cu-64-labeled peptide showed similar tumor uptake compared to the F-18 analogue, it also demonstrated higher accumulation in metabolic organs such as liver, kidneys, and intestines most likely owing to the transchelation of Cu-64 in vivo. Following this study, Zhang et al. (2013) reported the synthesis and biological evaluation of two F-18-labeled Ac-TC14012 (a T140 analogue) peptides in mice bearing CHO-CXCR4 and control CHO tumors. The differentiating factor between the two reported analogues was the prosthetic group used for F-18 labeling, namely fluoropropionate (Fig. 2.2-8) and fluorobenzoate (Fig. 2.2-9) groups. Analogue 6 showed superior pharmacokinetics with a tumor %ID/g of 4.30±0.86% and 0.93±0.06% in the CXCR4-positive and negative tumors, respectively. This peptide exhibited lower binding to red blood cells (0.7%), when compared to 4, with hepatic and renal retention of 25% and 15%, respectively. Jacobson et al. also reported two 64Cu-labeled T140 analogues denoted as DOTA-NFB (Fig. 2.2-10) and NOTA-NFB (Fig. 2.2-11) with very similar biodistribution as that of compound 6 (Jacobson et al., 2012).
George et al. (2014) recently reported the synthesis and biological evaluation of a 68Ga-labeled TN14003 (a T140 analogue) peptide (Fig. 2.2-12) in CXCR4-positive and negative U87-CD4 tumor mouse models). Tracer uptake in CXCR4-positive and negative tumors was 5.5% and 1.5%, respectively. High nonspecific retention was observed in liver (35%), kidneys (35%), and gallbladder (55%).
6.3. Small cyclic peptide analogues
LMW cyclic peptides have garnered considerable attention as imaging agents owing to their faster overall clearance rates, in vivo stability, and low nonspecific retention. Fujii et al. (2003) were the first to report small cyclic peptide analogues of T140. Their previous study using T140 analogues indicated the four amino acids Arg2, NaI3, Tyr5, and Arg14 of T140 to be essential for intrinsic bioactivity (Tamamura et al., 2000). Based on those observations, two orthogonal peptide libraries were designed based on sequence and conformation, leading to the discovery of the cyclic pentapeptide FC131 (also known as CPCR4), which exhibited a similar bioactivity to T140. Demmer et al. were first to report the synthesis, structural optimization, and in vivo evaluation of CPCR4 for PET imaging (Fig. 2.2-13; Demmer, Gourni, Schumacher, Kessler, & Wester, 2011). In that report, CPCR4 was optimized for Ga-68 labeling and evaluated in vivo in nude mice harboring OH-1 human small-cell lung tumors. The tracer exhibited a 6.16±1.16% uptake 60 min post-tracer injection in the CXCR4-expressing tumor with a 16.55±3.84 tumor-to-muscle ratio. That uptake was successfully blocked (CXCR4-tumor %ID/g 1.88±0.30) with 50 µg of the cold peptide. After tumor, the highest uptake was observed in kidneys (3.06±0.63), indicating rapid clearance of the tracer from the blood pool and nonspecific organs. Surprisingly, very little uptake was observed in tissues, such as liver and spleen, known to express CXCR4. A plausible explanation for the lack of uptake in other tissues is that CPCR4 may not bind to mouse CXCR4 and may only bind human CXCR4 receptors exclusively expressed on xenografted tumor cells. Although this tracer has thus far produced the “cleanest” PET images of CXCR4 expression, it may be of limited use in evaluating the comprehensive effects of CXCR4 inhibition or expression levels in preclinical models. An additional key finding of this report was that chelation of metals to DOTA significantly enhanced the binding affinity of CPCR4 toward CXCR4 receptors with indium and gallium enhancing the binding affinity by 3.4 and 30-fold, respectively. The gallium complex had a virtually identical binding affinity to the unmodified native CPCR4 peptide.
Demmer et al. (2011) also reported the synthesis and biological evaluation of a 68Ga-labeled CPCR4 dimer (Fig. 2.2-14) in the OH1 tumor model. This tracer exhibited lower tumor uptake (2.08±0.48%) and higher nonspecific hepatic uptake (44.31±5.56%) relative to the monomeric compound reported by Wester et al. Authors attributed the variation in the observed pharmacokinetics to the high lipophilicity of dimeric peptide species.
6.4. Antibodies against CXCR4
Monoclonal antibodies (mAbs) are gaining attention as therapeutics due to their long half-life and antigen specificity and affinity. In animal models, anti-CXCR4 antibodies markedly reduced metastasis and disease progression of breast cancer, lung cancer, lymphoma, and prostate tumors (Bertolini et al., 2002; Engl et al., 2006; Phillips et al., 2003). 12G5 is the most commonly used anti-CXCR4 antibody. Inhibition of CXCR4/CXCL12 interaction by 12G5 showed significant impairment of tumor cell migration in vitro (Engl et al., 2006). Kuhne et al. (2012) developed a fully humanized antibody, MDX1338, against CXCR4 and applied it for therapy in AML, non-Hodgkin lymphoma (NHL), CLL, and MM. These authors showed that MDX1338 antibody alone effectively inhibited cancer cell proliferation and retarded tumor growth in xenograft models by antibody-induced apoptosis. Therapeutic mAb development against CXCR4 may be complicated due to conformational heterogeneity of CXCR4 (Baribaud et al., 2001).CXCR4 exhibits significant conformational heterogeneity on primary and transformed B, T, and other hematopoietic cell types. Although the exact reason behind this conformational heterogeneity is not fully understood, altered glycosylation and glycation patterns in cancer cells may partially contribute to this heterogeneity (Farzan et al., 2002). These factors may create differences or change antibody specificity to CXCR4 in cancer cells.
Optically tagged CXCR4 antibodies are currently commercially available and thus far only utilized in flow cytometry or fluorescence microscopy experiments. The use of 125I-12G5 was reported by Nimmagadda, Pullambhatla, and Pomper (2009) for SPECT–CT imaging of mouse models bearing U87 tumors. Tracer uptake in the tumor was of 7% 48 h p.i. relative to the 3% uptake observed for the isotype antibody, suggesting the application of this tracer for in vivo SPECT imaging of CXCR4 expression.
6.5. LMW CXCR4 antagonists
In the early 1990s, a series of bicyclam analogues were developed to screen for anti-HIV activity. Among those compounds, AMD3100 was found to be a specific antagonist of CXCR4, binding to CXCR4 and inhibiting CXCR4/CXCL12 interactions with no cross-reactivity with other chemokine receptors (De Clercq, 2003; Fricker et al., 2006;Hatse, Princen, Bridger, De Clercq, & Schols, 2002). Although the initial focus of this drug development was on anti-HIV activity, soon it was found in clinical trials that AMD3100 induced leukocytosis caused by the mobilization of hematopoietic cells to the peripheral blood (Hendrix et al., 2004, 2000). Further preclinical studies and clinical trials demonstrated that AMD3100 alone and in combination with granulocyte colony-stimulating factor (G-CSF) can effectively mobilize hematopoietic cells from bone marrow (De Clercq, 2010; Devine et al., 2008; Liles et al., 2003). Therapeutic use of AMD3100 to inhibit CXCR4/CXCL12 axis in different cancer types has been mentioned in previous sections. An extensive array of CXCR4 binding LMW agents has been developed and discussed in detail by others (Mosley, Wilson, Wiseman, Skudlarek, & Liotta, 2009), and a few have been extensively validated. Ling et al. (2013) reported that the CXCR4 antagonist AMD3465 inhibited breast cancer growth and metastases by acting on tumor cells as well as immune cells that constitute the tumor microenvironment. AMD11070, an orally bioavailable CXCR4 inhibitor, was demonstrated to be more effective than AMD3100 in inhibiting melanoma tumor cell migration (O’Boyle et al., 2013). Liang et al. (2012) showed that MSX-122, a partial CXCR4 antagonist without mobilizing stem cells, blocked breast cancer and melanoma metastasis in animal models. KRH3955, a nonpeptide CXCR4 inhibitor, was shown to reduce the growth of gastric tumor xenograft in animal models (Iwanaga et al., 2012). TG-0054, a small-molecule CXCR4 antagonist, is in phase II trial for MM, non-Hodgkin lymphoma, and Hodgkin disease (Chung et al., 2009).
LMW compounds are a primary choice as imaging agents due to their high affinity and superior pharmacokinetics. LMW imaging probes for CXCR4 expression have mainly focused on the bicyclam compound AMD3100. The first report of radiolabeling (Fig. 2.2-15) and in vivo PET imaging of AMD3100 was carried out by Jacobson, Weiss, Szajek, Farber, and Kiesewetter (2009) in C57Bl/6 mice. High accumulation of the tracer was noted in the liver (41%), kidneys (10%), as well as in the immune-related organs such as spleen (13%), bone marrow (14%), and lymph nodes (10%), 1 h post tracer injection. Blocking with unlabeled AMD3100 resulted in significant reduction of signal in the spleen, liver, lymph nodes, and bone marrow implying CXCR4-specific uptake. The remaining uptake in liver tracer retention post blocking (12%) was attributed to nonspecific tracer uptake. The exact mechanism of action for this uptake still remains to be elucidated.
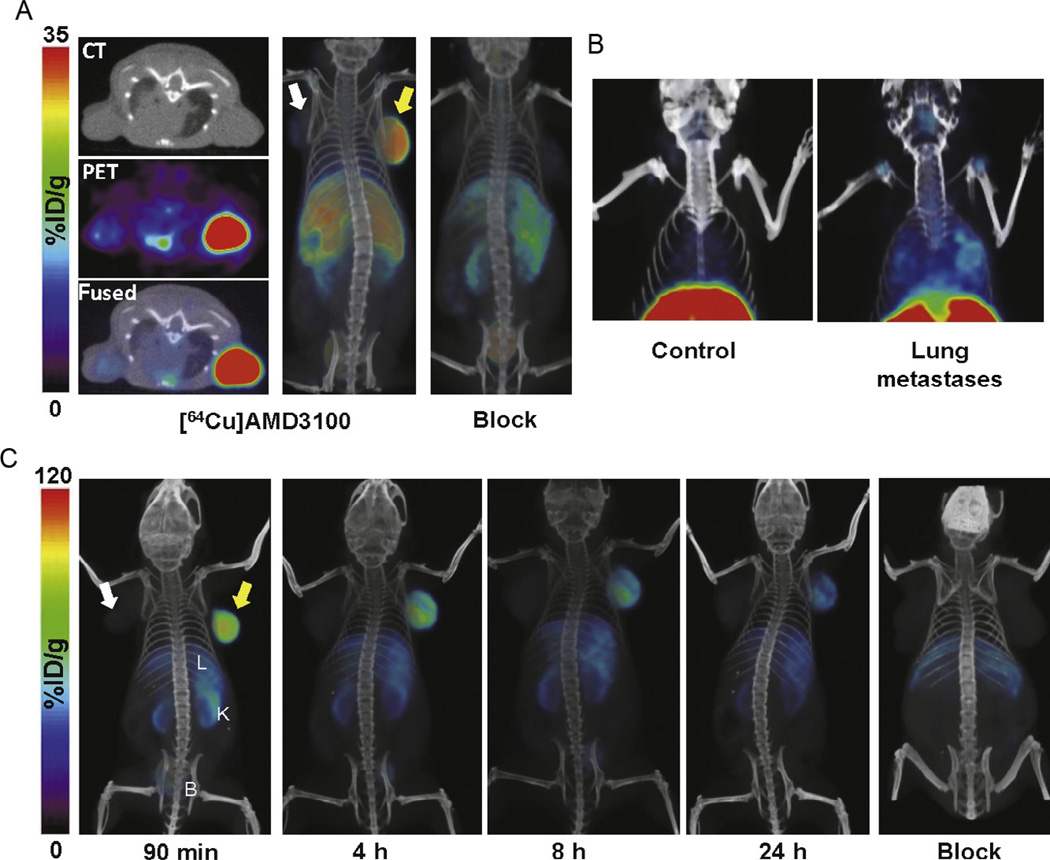
Nimmagadda et al. (2010) have established the utility of 64Cu-AMD3100 in imaging graded levels of CXCR4 expression in human tumor xenografts preselected for CXCR4 expression. Proof-of-principle imaging and biodistribution studies were carried out in NOD/SCID mice bearing (1) U87-stb-CXCR4 and U87 control tumors, (2) orthotopic breast MDA-MB-231 (low CXCR4) and DU4475 (high CXCR4) tumors, or (3) MDA-MB-231-derived lung metastases. In the U87 mouse model, tumor uptake was shown to be CXCR4 specific reaching 35% at 60 min p.i. in the U87-stb-CXCR4 tumors (Fig. 2.3A). Specificity for CXCR4 was confirmed using in vivo blocking studies with unlabeled AMD3100. Similar results were obtained in breast cancer models, indicating a tumor uptake of 6% in the DU4475 tumors compared to 2% in MDA-MB-231 tumors. In mice bearing lung metastases, 64Cu-AMD3100 was able to identify metastatic nodules in the lung (Fig. 2.3B), which was further validated by flow cytometry and immunohistochemistry. This report clearly illustrated the utility of 64Cu-AMD3100 for imaging of graded levels of CXCR4 expression.
Figure 2.3.
Volume rendered whole body PET/CT images of CXCR4 expression in subcutaneous NOD–SCID mice bearing U87-stb-CXCR4 (yellow arrow) and U87 control (white arrow) tumors (A) and MDA-MB-231-derived lung metastases (B) following injection of 300 µCi of 64Cu-AMD3100; U87-stb-CXCR4 (yellow arrow) and U87 control (white arrow) tumors following administration of 250 µCi of 64Cu-AMD3465 or a 25-mg/kg AMD3465 blocking dose followed by 250 µCi of 64Cu-AMD3465 (C). Images (A,B) were recreated from Nimmagadda et al. (2010) and (C) from De Silva et al. (2011).
A 99mTc-labeled AMD3100 analogue was reported and evaluated in mouse models bearing the human hepatocyte carcinoma cell line, Hep-G2 (Zhang, Tian, Li, Guo, & Shen, 2010). While biodistribution studies were not carried out, SPECT images indicated tumor uptake. Significant uptake was also observed in the liver, spleen, and kidneys at 60 min postinjection. More recently, Hartimath, Domanska, Walenkamp, Dierckx, and de Vries (2013) reported the evaluation of [99mTc]O2-AMD3100 in mice bearing PC3 tumors. Tumor uptake was reported at 1.7% at 5 min post injection decreasing to 0.7% over 60 min post-tracer injection. This uptake, though low, was blocked with excess unlabeled AMD3100 confirming CXCR4-mediated uptake.
De Silva et al. (2011) reported the in vivo evaluation of CXCR4 expression using the AMD3100 analogue AMD3465 (Fig. 2.2-16) in NOD/SCID mice harboring U87-stb-CXCR4 and U87 control tumors (Fig. 2.3C). TheU87-stb-CXCR4 tumor uptake was 96.29±13.98%at 90 min p.i. compared to 4.15±0.94% in U87 control tumors at the same time point. In addition, tumor-to-muscle and tumor-to-blood ratios were 362.56±153.51 and 138.78±30.87, respectively. These values are much higher than those previously reported for 64Cu-AMD3100 (tumor to muscle: 47.36±6.93; tumor to blood: 16.93±3.40). This tracer was further validated in mice with CXCR4 expressing colorectal adenocarcinoma HT-29 tumors. The HT-29 tumor uptake was 5.62±0.90% 90 min p.i. correlating with the lower CXCR4 expression (roughly 10-fold) when compared to that in U87-stb-CXCR4. This study validated the use of 64Cu-AMD3465 for in vivo imaging of graded levels of CXCR4 expression while showing higher tumor accumulation and tumor-to-muscle and tumor-to-blood ratios when compared to 64Cu-AMD3100 in the same mouse xenografts.
7. CONCLUSION
Diverse roles of CXCR4 in different types of cancers as well as in HIV infection and other pathological states have established CXCR4 as an important target for therapeutic intervention. Interaction of cancer cells with the tumor microenvironment, which protects the malignant cells from cytotoxic chemotherapy, is becoming an attractive target for improved anticancer treatment. CXCR4 antagonists through disruption of tumor–stromal cell interactions could play a significant role in sensitizing tumor cells to chemotherapy. Existing CXCR4-targeted imaging agents can detect graded levels of CXCR4 expression and have potential for therapeutic guidance and monitoring of cancer treatment. In spite of our improved understanding of CXCR4 biology, multiple challenges still remain such as delineating the role of CXCR7–CXCL12 axis contribution to these observations, identifying chemotherapeutics that modulate CXCR4 expression and developing suitable combination treatments with existing therapies.
ACKNOWLEDGMENTS
This work was supported by R01CA166131 (S. N.), The Alexander and Margaret Stewart Trust (S. N.), DOD W81XWH-12-BCRP-IDEA (S. N.), and DOD W81XWH-13-BCRP-POSTDOCTORAL FELLOWSHIP (B. B. A.).
REFERENCES
- ACS. Cancer facts and figures 2014. Atlanta, GA: American Cancer Society; 2014. [Google Scholar]
- Ahr B, Denizot M, Robert-Hebmann V, Brelot A, Biard-Piechaczyk M. Identification of the cytoplasmic domains of CXCR4 involved in Jak2 and STAT3 phosphorylation. Journal of Biological Chemistry. 2005;280(8):6692–6700. doi: 10.1074/jbc.M408481200. [DOI] [PubMed] [Google Scholar]
- Aiuti A, Webb IJ, Bleul C, Springer T, Gutierrez-Ramos JC. The chemokine SDF-1 is a chemoattractant for human CD34+ hematopoietic progenitor cells and provides a new mechanism to explain the mobilization of CD34+ progenitors to peripheral blood. Journal of Experimental Medicine. 1997;185(1):111–120. doi: 10.1084/jem.185.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akashi T, Koizumi K, Tsuneyama K, Saiki I, Takano Y, Fuse H. Chemokine receptor CXCR4 expression and prognosis in patients with metastatic prostate cancer. Cancer Science. 2008;99(3):539–542. doi: 10.1111/j.1349-7006.2007.00712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsayed Y, Ngo H, Runnels J, Leleu X, Singha UK, Pitsillides CM, et al. Mechanisms of regulation of CXCR4/SDF-1 (CXCL12)-dependent migration and homing in multiple myeloma. Blood. 2007;109(7):2708–2717. doi: 10.1182/blood-2006-07-035857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baccelli I, Trumpp A. The evolving concept of cancer and metastasis stem cells. Journal of Cell Biology. 2012;198(3):281–293. doi: 10.1083/jcb.201202014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachelerie F. CXCL12/CXCR4-axis dysfunctions: Markers of the rare immunodeficiency disorder WHIM syndrome. Disease Markers. 2010;29(3–4):189–198. doi: 10.3233/DMA-2010-0736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachet JB, Marechal R, Demetter P, Bonnetain F, Couvelard A, Svrcek M, et al. Contribution of CXCR4 and SMAD4 in predicting disease progression pattern and benefit from adjuvant chemotherapy in resected pancreatic adenocarcinoma. Annals of Oncology. 2012;23(9):2327–2335. doi: 10.1093/annonc/mdr617. [DOI] [PubMed] [Google Scholar]
- Baggiolini M. Chemokines and leukocyte traffic. Nature. 1998;392(6676):565–568. doi: 10.1038/33340. [DOI] [PubMed] [Google Scholar]
- Balabanian K, Lagane B, Infantino S, Chow KY, Harriague J, Moepps B, et al. The chemokine SDF-1/CXCL12 binds to and signals through the orphan receptor RDC1 in T lymphocytes. Journal of Biological Chemistry. 2005;280(42):35760–35766. doi: 10.1074/jbc.M508234200. [DOI] [PubMed] [Google Scholar]
- Balkwill F. Cancer and the chemokine network. Nature Reviews. Cancer. 2004a;4(7):540–550. doi: 10.1038/nrc1388. [DOI] [PubMed] [Google Scholar]
- Balkwill F. The significance of cancer cell expression of the chemokine receptor CXCR4. Seminars in Cancer Biology. 2004b;14(3):171–179. doi: 10.1016/j.semcancer.2003.10.003. [DOI] [PubMed] [Google Scholar]
- Bao L, Lai Y, Liu Y, Qin Y, Zhao X, Lu X, et al. CXCR4 is a good survival prognostic indicator in multiple myeloma patients. Leukemia Research. 2013;37(9):1083–1088. doi: 10.1016/j.leukres.2013.06.002. [DOI] [PubMed] [Google Scholar]
- Barbolina MV, Kim M, Liu Y, Shepard J, Belmadani A, Miller RJ, et al. Microenvironmental regulation of chemokine (C-X-C-motif) receptor 4 in ovarian carcinoma. Molecular Cancer Research. 2010;8(5):653–664. doi: 10.1158/1541-7786.MCR-09-0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baribaud F, Edwards TG, Sharron M, Brelot A, Heveker N, Price K, et al. Antigenically distinct conformations of CXCR4. Journal of Virology. 2001;75(19):8957–8967. doi: 10.1128/JVI.75.19.8957-8967.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barretina J, Junca J, Llano A, Gutierrez A, Flores A, Blanco J, et al. CXCR4 and SDF-1 expression in B-cell chronic lymphocytic leukemia and stage of the disease. Annals of Hematology. 2003;82(8):500–505. doi: 10.1007/s00277-003-0679-0. [DOI] [PubMed] [Google Scholar]
- Bartolome RA, Ferreiro S, Miquilena-Colina ME, Martinez-Prats L, Soto-Montenegro ML, Garcia-Bernal D, et al. The chemokine receptor CXCR4 and the metalloproteinase MT1-MMP are mutually required during melanoma metastasis to lungs. American Journal of Pathology. 2009;174(2):602–612. doi: 10.2353/ajpath.2009.080636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann M, Krause M, Hill R. Exploring the role of cancer stem cells in radioresistance. Nature Reviews. Cancer. 2008;8(7):545–554. doi: 10.1038/nrc2419. [DOI] [PubMed] [Google Scholar]
- Beider K, Begin M, Abraham M, Wald H, Weiss ID, Wald O, et al. CXCR4 antagonist 4 F-benzoyl-TN14003 inhibits leukemia and multiple myeloma tumor growth. Experimental Hematology. 2011;39(3):282–292. doi: 10.1016/j.exphem.2010.11.010. [DOI] [PubMed] [Google Scholar]
- Bendall LJ, Baraz R, Juarez J, Shen W, Bradstock KF. Defective p38 mitogen-activated protein kinase signaling impairs chemotaxic but not proliferative responses to stromal-derived factor-1alpha in acute lymphoblastic leukemia. Cancer Research. 2005;65(8):3290–3298. doi: 10.1158/0008-5472.CAN-04-3402. [DOI] [PubMed] [Google Scholar]
- Bertolini F, Dell’Agnola C, Mancuso P, Rabascio C, Burlini A, Monestiroli S, et al. CXCR4 neutralization, a novel therapeutic approach for non-Hodgkin’s lymphoma. Cancer Research. 2002;62(11):3106–3112. [PubMed] [Google Scholar]
- Bertolini G, Roz L, Perego P, Tortoreto M, Fontanella E, Gatti L, et al. Highly tumorigenic lung cancer CD133+ cells display stem-like features and are spared by cisplatin treatment. Proceedings of the National Academy of Sciences of the United States of America. 2009;106(38):16281–16286. doi: 10.1073/pnas.0905653106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleul CC, Farzan M, Choe H, Parolin C, Clark-Lewis I, Sodroski J, et al. The lymphocyte chemoattractant SDF-1 is a ligand for LESTR/fusin and blocks HIV-1 entry. Nature. 1996;382(6594):829–833. doi: 10.1038/382829a0. [DOI] [PubMed] [Google Scholar]
- Bleul CC, Fuhlbrigge RC, Casasnovas JM, Aiuti, A.,&Springer TA. A highly efficacious lymphocyte chemoattractant, stromal cell-derived factor 1 (SDF-1) Journal of Experimental Medicine. 1996;184(3):1101–1109. doi: 10.1084/jem.184.3.1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckle T, van den Berg NS, Kuil J, Bunschoten A, Oldenburg J, Borowsky AD, et al. Non-invasive longitudinal imaging of tumor progression using an 111Indium labeled CXCR4 peptide antagonist. European Journal of Nuclear Medicine and Molecular Imaging. 2012;38:S145. [PMC free article] [PubMed] [Google Scholar]
- Buckley CD, Amft N, Bradfield PF, Pilling D, Ross E, Arenzana-Seisdedos F, et al. Persistent induction of the chemokine receptor CXCR4 by TGF-beta 1 on synovial T cells contributes to their accumulation within the rheumatoid synovium. Journal of Immunology. 2000;165(6):3423–3429. doi: 10.4049/jimmunol.165.6.3423. [DOI] [PubMed] [Google Scholar]
- Bunschoten A, Buckle T, Kuil J, Luker GD, Luker KE, Nieweg OE, et al. Targeted non-covalent self-assembled nanoparticles based on human serum albumin. Biomaterials. 2012;33(3):867–875. doi: 10.1016/j.biomaterials.2011.10.005. http://dx.doi.org/10.1016/j.biomaterials.2011.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burger JA. Targeting the microenvironment in chronic lymphocytic leukemia is changing the therapeutic landscape. Current Opinion in Oncology. 2009;24(6):643–649. doi: 10.1097/CCO.0b013e3283589950. [DOI] [PubMed] [Google Scholar]
- Burger JA. Chemokines and chemokine receptors in chronic lymphocytic leukemia (CLL): From understanding the basics towards therapeutic targeting. Seminars in Cancer Biology. 2010;20(6):424–430. doi: 10.1016/j.semcancer.2010.09.005. [DOI] [PubMed] [Google Scholar]
- Burger JA, Burger M, Kipps TJ. Chronic lymphocytic leukemia B cells express functional CXCR4 chemokine receptors that mediate spontaneous migration beneath bone marrow stromal cells. Blood. 1999;94(11):3658–3667. [PubMed] [Google Scholar]
- Burger M, Glodek A, Hartmann T, Schmitt-Graff A, Silberstein LE, Fujii N, et al. Functional expression ofCXCR4 (CD184) on small-cell lung cancer cells mediates migration, integrin activation, and adhesion to stromal cells. Oncogene. 2003;22(50):8093–8101. doi: 10.1038/sj.onc.1207097. [DOI] [PubMed] [Google Scholar]
- Burger JA, Peled A. CXCR4 antagonists: Targeting the microenvironment in leukemia and other cancers. Leukemia. 2009;23(1):43–52. doi: 10.1038/leu.2008.299. [DOI] [PubMed] [Google Scholar]
- Burger JA, Stewart DJ, Wald O, Peled A. Potential of CXCR4 antagonists for the treatment of metastatic lung cancer. Expert Review of Anticancer Therapy. 2011;11(4):621–630. doi: 10.1586/era.11.11. [DOI] [PubMed] [Google Scholar]
- Burns JM, Summers BC, Wang Y, Melikian A, Berahovich R, Miao Z, et al. A novel chemokine receptor for SDF-1 and I-TAC involved in cell survival, cell adhesion, and tumor development. Journal of Experimental Medicine. 2006;203(9):2201–2213. doi: 10.1084/jem.20052144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabioglu N, Summy J, Miller C, Parikh NU, Sahin AA, Tuzlali S, et al. CXCL-12/stromal cell-derived factor-1alpha transactivates HER2-neu in breast cancer cells by a novel pathway involving Src kinase activation. Cancer Research. 2005;15:6493–6497. doi: 10.1158/0008-5472.CAN-04-1303. http://dx.doi.org/10.1158/0008-5472.CAN-04-1303. [DOI] [PubMed] [Google Scholar]
- Camaj P, Jackel C, Krebs S, Detoni EN, Blum H, Jauch KW, et al. Hypoxia-independent gene expression mediated by SOX9 promotes aggressive pancreatic tumor biology. Molecular Cancer Research. 2014;12(3):421–432. doi: 10.1158/1541-7786.MCR-13-0351. [DOI] [PubMed] [Google Scholar]
- CDC. Cancer among men. 2013 [Google Scholar]
- Chen Y, Huang Y, Reiberger T, Duyverman AM, Huang P, Samuel R, et al. Differential effects of sorafenib on liver versus tumor fibrosis mediated by stromal-derived factor 1 alpha/C-X-C receptor type 4 axis and myeloid differentiation antigen-positive myeloid cell infiltration in mice. Hepatology. 2014;59(4):1435–1447. doi: 10.1002/hep.26790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y, Jacamo R, Konopleva M, Garzon R, Croce C, Andreeff M. CXCR4 downregulation of let-7a drives chemoresistance in acute myeloid leukemia. Journal of Clinical Investigation. 2013;123(6):2395–2407. doi: 10.1172/JCI66553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HY, Wang JM, Wang HY, Zhang YX, Liu W, Pan L, et al. Effect of short hairpin RNA-induced CXCR4 silence on ovarian cancer cell. Biomedicine & Pharmacotherapy. 2012;66(7):549–553. doi: 10.1016/j.biopha.2012.04.007. [DOI] [PubMed] [Google Scholar]
- Choi WT, Duggineni S, Xu Y, Huang Z, An J. Drug discovery research targeting the CXC chemokine receptor 4 (CXCR4) Journal of Medicinal Chemistry. 2012;55(3):977–994. doi: 10.1021/jm200568c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong BF, Mohan C. Targeting the CXCR4/CXCL12 axis in systemic lupus erythematosus. Expert Opinion on Therapeutic Targets. 2009;13(10):1147–1153. doi: 10.1517/14728220903196761. [DOI] [PubMed] [Google Scholar]
- Chu QD, Panu L, Holm NT, Li BD, Johnson LW, Zhang S. High chemokine receptor CXCR4 level in triple negative breast cancer specimens predicts poor clinical outcome. Journal of Surgical Research. 2010;159(2):689–695. doi: 10.1016/j.jss.2008.09.020. [DOI] [PubMed] [Google Scholar]
- Chu H, Zhou H, Liu Y, Liu X, Hu Y, Zhang J. Functional expression of CXC chemokine receptor-4 mediates the secretion of matrix metalloproteinases from mouse hepatocarcinoma cell lines with different lymphatic metastasis ability. International Journal of Biochemistry & Cell Biology. 2007;39(1):197–205. doi: 10.1016/j.biocel.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Chung DT, Chang L-W, Huang Y-H, Tsai C-Y, Hsu C-H, King C-HR, et al. TG-0054, a novel and potent stem cell mobilizer, displays excellent PK/PD and safety profile in phase I trial. Blood. 2009;114(22):357. [Google Scholar]
- Chung SH, Seki K, Choi BI, Kimura KB, Ito A, Fujikado N, et al. CXC chemokine receptor 4 expressed in T cells plays an important role in the development of collagen-induced arthritis. Arthritis Research & Therapy. 2010;12((5):R188. doi: 10.1186/ar3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins CD. Problems monitoring response in multiple myeloma. Cancer Imaging. 2005;5(Spec No A):S119–S126. doi: 10.1102/1470-7330.2005.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Alterio C, Consales C, Polimeno M, Franco R, Cindolo L, Portella L, et al. Concomitant CXCR4 and CXCR7 expression predicts poor prognosis in renal cancer. Current Cancer Drug Targets. 2010;10(7):772–781. doi: 10.2174/156800910793605839. [DOI] [PubMed] [Google Scholar]
- Darash-Yahana M, Pikarsky E, Abramovitch R, Zeira E, Pal B, Karplus R, et al. Role of high expression levels of CXCR4 in tumor growth, vascularization, and metastasis. FASEB Journal. 2004;18(11):1240–1242. doi: 10.1096/fj.03-0935fje. [DOI] [PubMed] [Google Scholar]
- Debnath B, Xu S, Grande F, Garofalo A, Neamati N. Small molecule inhibitors of CXCR4. Theranostics. 2013;3(1):47–75. doi: 10.7150/thno.5376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Clercq E. The bicyclam AMD3100 story. Nature Reviews. Drug Discovery. 2003;2(7):581–587. doi: 10.1038/nrd1134. [DOI] [PubMed] [Google Scholar]
- De Clercq E. Recent advances on the use of the CXCR4 antagonist plerixafor (AMD3100, Mozobil) and potential of other CXCR4 antagonists as stem cell mobilizers. Pharmacology & Therapeutics. 2010;128(3):509–518. doi: 10.1016/j.pharmthera.2010.08.009. [DOI] [PubMed] [Google Scholar]
- De Klerck B, Geboes L, Hatse S, Kelchtermans H, Meyvis Y, Vermeire K, et al. Pro-inflammatory properties of stromal cell-derived factor-1 (CXCL12) in collagen-induced arthritis. Arthritis Research & Therapy. 2005;7(6):R1208–R1220. doi: 10.1186/ar1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMarco SJ, Henze H, Lederer A, Moehle K, Mukherjee R, Romagnoli B, et al. Discovery of novel, highly potent and selective beta-hairpin mimetic CXCR4 inhibitors with excellent anti-HIV activity and pharmacokinetic profiles. Bioorganic & Medicinal Chemistry. 2006;14(24):8396–8404. doi: 10.1016/j.bmc.2006.09.003. [DOI] [PubMed] [Google Scholar]
- Demmer O, Dijkgraaf I, Schumacher U, Marinelli L, Cosconati S, Gourni E, et al. Design, synthesis, and functionalization of dimeric peptides targeting chemokine receptor CXCR4. Journal of Medicinal Chemistry. 2011;54(21):7648–7662. doi: 10.1021/jm2009716. http://dx.doi.org/10.1021/jm2009716. [DOI] [PubMed] [Google Scholar]
- Demmer O, Gourni E, Schumacher U, Kessler H, Wester H-J. PET imaging of CXCR4 receptors in cancer by a new optimized ligand. Chem Med Chem. 2011;6(10):1789–1791. doi: 10.1002/cmdc.201100320. http://dx.doi.org/10.1002/cmdc.201100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Silva RA, Peyre K, Pullambhatla M, Fox JJ, Pomper MG, Nimmagadda S. Imaging CXCR4 expression in human cancer xenografts: Evaluation of monocyclam Cu-64-AMD3465. Journal of Nuclear Medicine. 2011;52(6):986–993. doi: 10.2967/jnumed.110.085613. http://dx.doi.org/10.2967/jnumed.110.085613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devine SM, Vij R, Rettig M, Todt L, McGlauchlen K, Fisher N, et al. Rapid mobilization of functional donor hematopoietic cells without G-CSF using AMD3100, an antagonist of the CXCR4/SDF-1 interaction. Blood. 2008;112(4):990–998. doi: 10.1182/blood-2007-12-130179. [DOI] [PubMed] [Google Scholar]
- Dillmann F, Veldwijk MR, Laufs S, Sperandio M, Calandra G, Wenz F, et al. Plerixafor inhibits chemotaxis toward SDF-1 and CXCR4-mediated stroma contact in a dose-dependent manner resulting in increased susceptibility of BCR-ABL+ cell to Imatinib and Nilotinib. Leukemia & Lymphoma. 2009;50(10):1676–1686. doi: 10.1080/10428190903150847. [DOI] [PubMed] [Google Scholar]
- DiPersio JF, Stadtmauer EA, Nademanee A, Micallef IN, Stiff PJ, Kaufman JL, et al. Plerixafor and G-CSF versus placebo and G-CSF to mobilize hematopoietic stem cells for autologous stem cell transplantation in patients with multiple myeloma. Blood. 2009;113(23):5720–5726. doi: 10.1182/blood-2008-08-174946. [DOI] [PubMed] [Google Scholar]
- DiPersio JF, Uy GL, Yasothan U, Kirkpatrick P. Plerixafor. Nature Reviews. Drug Discovery. 2009;8(2):105–106. doi: 10.1038/nrd2819. [DOI] [PubMed] [Google Scholar]
- Domanska UM, Kruizinga RC, Nagengast WB, Timmer-Bosscha H, Huls G, de Vries EG, et al. A review on CXCR4/CXCL12 axis in oncology: No place to hide. European Journal of Cancer. 2012;49(1):219–230. doi: 10.1016/j.ejca.2012.05.005. [DOI] [PubMed] [Google Scholar]
- Duda DG, Kozin SV, Kirkpatrick ND, Xu L, Fukumura D, Jain RK. CXCL12 (SDF1alpha)-CXCR4/CXCR7 pathway inhibition: An emerging sensitizer for anticancer therapies? Clinical Cancer Research. 2011;17(8):2074–2080. doi: 10.1158/1078-0432.CCR-10-2636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eck SM, Cote AL, Winkelman WD, Brinckerhoff CE. CXCR4 and matrix metalloproteinase-1 are elevated in breast carcinoma-associated fibroblasts and in normal mammary fibroblasts exposed to factors secreted by breast cancer cells. Molecular Cancer Research. 2009;7(7):1033–1044. doi: 10.1158/1541-7786.MCR-09-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engl T, Relja B, Marian D, Blumenberg C, Muller I, Beecken WD, et al. CXCR4 chemokine receptor mediates prostate tumor cell adhesion through alpha5 and beta3 integrins. Neoplasia. 2006;8(4):290–301. doi: 10.1593/neo.05694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esencay M, Newcomb EW, Zagzag D. HGF upregulates CXCR4 expression in gliomas via NF-kappaB: Implications for glioma cell migration. Journal of Neuro-Oncology. 2010;99(1):33–40. doi: 10.1007/s11060-010-0111-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fahham D, Weiss ID, Abraham M, Beider K, Hanna W, Shlomai Z, et al. In vitro and in vivo therapeutic efficacy of CXCR4 antagonist BKT140 against human non-small cell lung cancer. Journal of Thoracic and Cardiovascular Surgery. 2012;144(5):1167–1175. e1161. doi: 10.1016/j.jtcvs.2012.07.031. [DOI] [PubMed] [Google Scholar]
- Fakhari S, Kalantar E, Nikzaban M, Hakhamneshi MS, Fathi F, Nikkhoo B, et al. Effect of Helicobacter pylori infection on stromal-derived factor-1/CXCR4 axis in bone marrow-derived mesenchymal stem cells. Advanced Biomedical Research. 2014;3:19. doi: 10.4103/2277-9175.124650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farzan M, Babcock GJ, Vasilieva N, Wright PL, Kiprilov E, Mirzabekov T, et al. The role of post-translational modifications of the CXCR4 amino terminus in stromal-derived factor 1 alpha association and HIV-1 entry. Journal of Biological Chemistry. 2002;277(33):29484–29489. doi: 10.1074/jbc.M203361200. [DOI] [PubMed] [Google Scholar]
- Feng Y, Broder CC, Kennedy PE, Berger EA. HIV-1 entry cofactor: Functional cDNA cloning of a seven-transmembrane, G protein-coupled receptor. Science. 1996;272(5263):872–877. doi: 10.1126/science.272.5263.872. [DOI] [PubMed] [Google Scholar]
- Fernandis AZ, Cherla RP, Chernock RD, Ganju RK. CXCR4/CCR5 down-modulation and chemotaxis are regulated by the proteasome pathway. Journal of Biological Chemistry. 2002;277(20):18111–18117. doi: 10.1074/jbc.M200750200. [DOI] [PubMed] [Google Scholar]
- Franco R, Pirozzi G, Scala S, Cantile M, Scognamiglio G, Camerlingo R, et al. CXCL12-binding receptors expression in non-small cell lung cancer relates to tumoral microvascular density and CXCR4 positive circulating tumoral cells in lung draining venous blood. European Journal of Cardio-Thoracic Surgery. 2011;41(2):368–375. doi: 10.1016/j.ejcts.2011.05.009. [DOI] [PubMed] [Google Scholar]
- Fricker SP, Anastassov V, Cox J, Darkes MC, Grujic O, Idzan SR, et al. Characterization of the molecular pharmacology of AMD3100: A specific antagonist of the G-protein coupled chemokine receptor, CXCR4. Biochemical Pharmacology. 2006;72(5):588–596. doi: 10.1016/j.bcp.2006.05.010. [DOI] [PubMed] [Google Scholar]
- Fujii N, Oishi S, Hiramatsu K, Araki T, Ueda S, Tamamura H, et al. Molecular-size reduction of a potent CXCR4-chemokine antagonist using orthogonal combination of conformation- and sequence-based libraries. Angewandte Chemie International Edition. 2003;42(28):3251–3253. doi: 10.1002/anie.200351024. http://dx.doi.org/10.1002/anie.200351024. [DOI] [PubMed] [Google Scholar]
- Furusato B, Mohamed A, Uhlen M, Rhim JS. CXCR4 and cancer. Pathology International. 2010;60(7):497–505. doi: 10.1111/j.1440-1827.2010.02548.x. [DOI] [PubMed] [Google Scholar]
- Gagliardi F, Narayanan A, Reni M, Franzin A, Mazza E, Boari N, et al. The role of CXCR4 in highly malignant human gliomas biology: Current knowledge and future directions. Glia. 2014;62(7):1015–1023. doi: 10.1002/glia.22669. http://dx.doi.org/10.1002/glia.22669. [DOI] [PubMed] [Google Scholar]
- Gahan JC, Gosalbez M, Yates T, Young EE, Escudero DO, Chi A, et al. Chemokine and chemokine receptor expression in kidney tumors: Molecular profiling of histological subtypes and association with metastasis. Journal of Urology. 2012;187(3):827–833. doi: 10.1016/j.juro.2011.10.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambaryan N, Perros F, Montani D, Cohen-Kaminsky S, Mazmanian M, Renaud JF, et al. Targeting of c-kit+haematopoietic progenitor cells prevents hypoxic pulmonary hypertension. European Respiratory Journal. 2011;37(6):1392–1399. doi: 10.1183/09031936.00045710. [DOI] [PubMed] [Google Scholar]
- Ganju RK, Brubaker SA, Meyer J, Dutt P, Yang Y, Qin S, et al. The alpha-chemokine, stromal cell-derived factor-1alpha, binds to the transmembrane G-protein-coupled CXCR-4 receptor and activates multiple signal transduction pathways. Journal of Biological Chemistry. 1998;273(36):23169–23175. doi: 10.1074/jbc.273.36.23169. [DOI] [PubMed] [Google Scholar]
- Gao Z, Wang X, Wu K, Zhao Y, Hu G. Pancreatic stellate cells increase the invasion of human pancreatic cancer cells through the stromal cell-derived factor-1/CXCR4 axis. Pancreatology. 2010;10(2–3):186–193. doi: 10.1159/000236012. [DOI] [PubMed] [Google Scholar]
- Gatti M, Pattarozzi A, Bajetto A, Wurth R, Daga A, Fiaschi P, et al. Inhibition of CXCL12/CXCR4 autocrine/paracrine loop reduces viability of human glioblastoma stem-like cells affecting self-renewal activity. Toxicology. 2013;314(2–3):209–220. doi: 10.1016/j.tox.2013.10.003. [DOI] [PubMed] [Google Scholar]
- George GPC, Stevens E, Aberg O, Quang-De N, Pisaneschi F, Spivey AC, et al. Preclinical evaluation of a CXCR4-specific Ga-68-labelled TN14003 derivative for cancer PET imaging. Bioorganic & Medicinal Chemistry. 2014;22(2):796–803. doi: 10.1016/j.bmc.2013.12.012. http://dx.doi.org/10.1016/j.bmc.2013.12.012. [DOI] [PubMed] [Google Scholar]
- Gilman AG. G proteins: Transducers of receptor-generated signals. Annual Review of Biochemistry. 1987;56:615–649. doi: 10.1146/annurev.bi.56.070187.003151. [DOI] [PubMed] [Google Scholar]
- Gladson CL, Welch DR. New insights into the role of CXCR4 in prostate cancer metastasis. Cancer Biology & Therapy. 2008;7(11):1849–1851. doi: 10.4161/cbt.7.11.7218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gockel I, Schimanski CC, Heinrich C, Wehler T, Frerichs K, Drescher D, et al. Expression of chemokine receptor CXCR4 in esophageal squamous cell and adenocarcinoma. BMC Cancer. 2006;6:290. doi: 10.1186/1471-2407-6-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldsmith ZG, Dhanasekaran DN. G protein regulation of MAPK networks. Oncogene. 2007;26(22):3122–3142. doi: 10.1038/sj.onc.1210407. [DOI] [PubMed] [Google Scholar]
- Gulino AV. WHIM syndrome: A genetic disorder of leukocyte trafficking. Current Opinion in Allergy and Clinical Immunology. 2003;3(6):443–450. doi: 10.1097/00130832-200312000-00005. [DOI] [PubMed] [Google Scholar]
- Gupta SK, Lysko PG, Pillarisetti K, Ohlstein E, Stadel JM. Chemokine receptors in human endothelial cells. Functional expression of CXCR4 and its transcriptional regulation by inflammatory cytokines. Journal of Biological Chemistry. 1998;273(7):4282–4287. doi: 10.1074/jbc.273.7.4282. [DOI] [PubMed] [Google Scholar]
- Han M, Lv S, Zhang Y, Yi R, Huang B, Fu H, et al. The prognosis and clinicopathology of CXCR4 in gastric cancer patients: A meta-analysis. Tumour Biology. 2014;35(5):4589–4597. doi: 10.1007/s13277-013-1603-4. [DOI] [PubMed] [Google Scholar]
- Han S, Ritzenthaler JD, Sitaraman SV, Roman J. Fibronectin increases matrix metalloproteinase 9 expression through activation of c-Fos via extracellular-regulated kinase and phosphatidylinositol 3-kinase pathways in human lung carcinoma cells. Journal of Biological Chemistry. 2006;281(40):29614–29624. doi: 10.1074/jbc.M604013200. [DOI] [PubMed] [Google Scholar]
- Hartimath SV, Domanska UM, Walenkamp AME, Dierckx RAJO, de Vries EFJ. [Tc-99 m]O-2-AMD3100 as a SPECT tracer for CXCR4 receptor imaging. Nuclear Medicine and Biology. 2013;40(4):507–517. doi: 10.1016/j.nucmedbio.2013.02.003. http://dx.doi.org/10.1016/j.nucmedbio.2013.02.003. [DOI] [PubMed] [Google Scholar]
- Hassan S, Ferrario C, Saragovi U, Quenneville L, Gaboury L, Baccarelli A, et al. The influence of tumor-host interactions in the stromal cell-derived factor-1/CXCR4 ligand/receptor axis in determining metastatic risk in breast cancer. The American Journal of Pathology. 2009;175(1):66–73. doi: 10.2353/ajpath.2009.080948. http://dx.doi.org/10.2353/ajpath.2009.080948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatse S, Princen K, Bridger G, De Clercq E, Schols D. Chemokine receptor inhibition by AMD3100 is strictly confined to CXCR4. FEBS Letters. 2002;527(1–3):255–262. doi: 10.1016/s0014-5793(02)03143-5. [DOI] [PubMed] [Google Scholar]
- Hattermann K, Mentlein R. An infernal trio: The chemokine CXCL12 and its receptors CXCR4 and CXCR7 in tumor biology. Annals of Anatomy. 2013;195(2):103–110. doi: 10.1016/j.aanat.2012.10.013. [DOI] [PubMed] [Google Scholar]
- He J, Chen Y, Farzan M, Choe H, Ohagen A, Gartner S, et al. CCR3 and CCR5 are co-receptors for HIV-1 infection of microglia. Nature. 1997;385(6617):645–649. doi: 10.1038/385645a0. [DOI] [PubMed] [Google Scholar]
- Heesen M, Berman MA, Benson JD, Gerard C, Dorf ME. Cloning of the mouse fusin gene, homologue to a human HIV-1 co-factor. Journal of Immunology. 1996;157(12):5455–5460. [PubMed] [Google Scholar]
- Hendrix CW, Collier AC, Lederman MM, Schols D, Pollard RB, Brown S, et al. Safety, pharmacokinetics, and antiviral activity of AMD3100, a selective CXCR4 receptor inhibitor, in HIV-1 infection. Journal of Acquired Immune Deficiency Syndromes. 2004;37(2):1253–1262. doi: 10.1097/01.qai.0000137371.80695.ef. [DOI] [PubMed] [Google Scholar]
- Hendrix CW, Flexner C, MacFarland RT, Giandomenico C, Fuchs EJ, Redpath E, et al. Pharmacokinetics and safety of AMD-3100, a novel antagonist of the CXCR-4 chemokine receptor, in human volunteers. Antimicrobial Agents and Chemotherapy. 2000;44(6):1667–1673. doi: 10.1128/aac.44.6.1667-1673.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, et al. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1(3):313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- Hernandez PA, Gorlin RJ, Lukens JN, Taniuchi S, Bohinjec J, Francois F, et al. Mutations in the chemokine receptor gene CXCR4 are associated with WHIM syndrome, a combined immunodeficiency disease. Nature Genetics. 2003;34(1):70–74. doi: 10.1038/ng1149. [DOI] [PubMed] [Google Scholar]
- Hesselgesser J, Halks-Miller M, DelVecchio V, Peiper SC, Hoxie J, Kolson DL, et al. CD4-independent association between HIV-1 gp120 and CXCR4: Functional chemokine receptors are expressed in human neurons. Current Biology. 1997;7(2):112–121. doi: 10.1016/s0960-9822(06)00055-8. [DOI] [PubMed] [Google Scholar]
- Ho TK, Shiwen X, Abraham D, Tsui J, Baker D. Stromal-cell-derived factor-1 (SDF-1)/CXCL12 as potential target of therapeutic angiogenesis in critical leg ischaemia. Cardiology Research and Practice, 2012. 2012;2012:143209. doi: 10.1155/2012/143209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann F, Muller W, Schutz D, Penfold ME, Wong YH, Schulz S, et al. Rapid uptake and degradation of CXCL12 depend on CXCR7 carboxyl-terminal serine/threonine residues. Journal of Biological Chemistry. 2012;287(34):28362–28377. doi: 10.1074/jbc.M111.335679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holm NT, Byrnes K, Li BD, Turnage RH, Abreo F, Mathis JM, et al. Elevated levels of chemokine receptor CXCR4 in HER-2 negative breast cancer specimens predict recurrence. Journal of Surgical Research. 2007;141(1):53–59. doi: 10.1016/j.jss.2007.03.015. [DOI] [PubMed] [Google Scholar]
- Howard OM, Ben-Baruch A, Oppenheim JJ. Chemokines: Progress toward identifying molecular targets for therapeutic agents. Trends in Biotechnology. 1996;14(2):46–51. doi: 10.1016/0167-7799(96)80920-6. [DOI] [PubMed] [Google Scholar]
- Hsu W, Rosenquist GL, Ansari AA, Gershwin ME. Autoimmunity and tyrosine sulfation. Autoimmunity Reviews. 2005;4(7):429–435. doi: 10.1016/j.autrev.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Huang EH, Singh B, Cristofanilli M, Gelovani J, Wei C, Vincent L, et al. A CXCR4 antagonist CTCE-9908 inhibits primary tumor growth and metastasis of breast cancer. Journal of Surgical Research. 2009;155(2):231–236. doi: 10.1016/j.jss.2008.06.044. [DOI] [PubMed] [Google Scholar]
- Hubbard MO, Fu P, Margevicius S, Dowlati A, Linden PA. Five-year survival does not equal cure in non-small cell lung cancer: A surveillance, epidemiology, and end results-based analysis of variables affecting 10- to 18-year survival. Journal of Thoracic and Cardiovascular Surgery. 2012;143(6):1307–1313. doi: 10.1016/j.jtcvs.2012.01.078. [DOI] [PubMed] [Google Scholar]
- Hunter ZR, Xu L, Yang G, Zhou Y, Liu X, Cao Y, et al. The genomic landscape of Waldenstrom macroglobulinemia is characterized by highly recurring MYD88 and WHIM-like CXCR4 mutations, and small somatic deletions associated with B-cell lymphomagenesis. Blood. 2012;123(11):1637–1646. doi: 10.1182/blood-2013-09-525808. [DOI] [PubMed] [Google Scholar]
- Ishikawa T, Nakashiro K, Klosek SK, Goda H, Hara S, Uchida D, et al. Hypoxia enhances CXCR4 expression by activating HIF-1 in oral squamous cell carcinoma. Oncology Reports. 2009;21(3):707–712. [PubMed] [Google Scholar]
- Iwanaga T, Iwasaki Y, Ohashi M, Nunobe S, Iwagami S. Establishment of a CXCR4-expressing gastric cancer cell line in nude mice and the effect of AMD 3100 on tumor regression. Gan to Kagaku Ryoho. 2007;34(12):1917–1919. [PubMed] [Google Scholar]
- Iwanaga T, Iwasaki Y, Ohashi M, Ohinata R, Takahashi K, Yamaguchi T, et al. Inhibitory effect of CXCR4 blockers on a CXCR4-expressing gastric cancer cell line in nude mice. Gan to Kagaku Ryoho. 2012;39(12):1788–1790. [PubMed] [Google Scholar]
- Jacobson O, Weiss ID, Kiesewetter DO, Farber JM, Chen X. PET of tumor CXCR4 expression with 4-F-18-T140. Journal of Nuclear Medicine. 2010;51(11):1796–1804. doi: 10.2967/jnumed.110.079418. http://dx.doi.org/10.2967/jnumed.110.079418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson O, Weiss ID, Szajek L, Farber JM, Kiesewetter DO. Cu-64-AMD3100—A novel imaging agent for targeting chemokine receptor CXCR4. Bioorganic & Medicinal Chemistry. 2009;17(4):1486–1493. doi: 10.1016/j.bmc.2009.01.014. http://dx.doi.org/10.1016/j.bmc.2009.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson O, Weiss ID, Szajek LP, Niu G, Ma Y, Kiesewetter DO, et al. PET imaging of CXCR4 using copper-64 labeled peptide antagonist. Theranostics. 2011;1:251–262. doi: 10.7150/thno/v01p0251. http://dx.doi.org/10.7150/thno/v01p0251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson O, Weiss ID, Szajek LP, Niu G, Ma Y, Kiesewetter DO, et al. Improvement of CXCR4 tracer specificity for PET imaging. Journal of Controlled Release. 2012;157(2):216–223. doi: 10.1016/j.jconrel.2011.09.076. http://dx.doi.org/10.1016/j.jconrel.2011.09.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janowski M. Functional diversity of SDF-1 splicing variants. Cell Adhesion &Migration. 2009;3(3):243–249. doi: 10.4161/cam.3.3.8260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jerant AF, Johnson JT, Sheridan CD, Caffrey TJ. Early detection and treatment of skin cancer. American Family Physician. 2000;62(2):357–368. 375–356, 381–352. [PubMed] [Google Scholar]
- Jiang YP, Wu XH, Shi B, Wu WX, Yin GR. Expression of chemokine CXCL12 and its receptor CXCR4 in human epithelial ovarian cancer: An independent prognostic factor for tumor progression. Gynecologic Oncology. 2006;103(1):226–233. doi: 10.1016/j.ygyno.2006.02.036. [DOI] [PubMed] [Google Scholar]
- Jung MJ, Rho JK, Kim YM, Jung JE, Jin YB, Ko YG, et al. Upregulation of CXCR4 is functionally crucial for maintenance of stemness in drugresistant non-small cell lung cancer cells. Oncogene. 2013;32(2):209–221. doi: 10.1038/onc.2012.37. [DOI] [PubMed] [Google Scholar]
- Kajiyama H, Shibata K, Terauchi M, Ino K, Nawa A, Kikkawa F. Involvement of SDF-1alpha/CXCR4 axis in the enhanced peritoneal metastasis of epithelial ovarian carcinoma. International Journal of Cancer. 2008;122(1):91–99. doi: 10.1002/ijc.23083. [DOI] [PubMed] [Google Scholar]
- Kang Y, Siegel PM, Shu W, Drobnjak M, Kakonen SM, Cordon-Cardo C, et al. A multigenic program mediating breast cancer metastasis to bone. Cancer Cell. 2003;3(6):537–549. doi: 10.1016/s1535-6108(03)00132-6. [DOI] [PubMed] [Google Scholar]
- Kang H, Watkins G, Douglas-Jones A, Mansel RE, Jiang WG. The elevated level of CXCR4 is correlated with nodal metastasis of human breast cancer. Breast. 2005;14(5):360–367. doi: 10.1016/j.breast.2004.12.007. [DOI] [PubMed] [Google Scholar]
- Kato M, Kitayama J, Kazama S, Nagawa H. Expression pattern of CXC chemokine receptor-4 is correlated with lymph node metastasis in human invasive ductal carcinoma. Breast Cancer Research. 2003;5(5):R144–R150. doi: 10.1186/bcr627. http://dx.doi.org/10.1186/bcr627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim M, Koh YJ, Kim KE, Koh BI, Nam DH, Alitalo K, et al. CXCR4 signaling regulates metastasis of chemoresistant melanoma cells by a lymphatic metastatic niche. Cancer Research. 2010;70(24):10411–10421. doi: 10.1158/0008-5472.CAN-10-2591. [DOI] [PubMed] [Google Scholar]
- Kim SY, Lee CH, Midura BV, Yeung C, Mendoza A, Hong SH, et al. Inhibition of the CXCR4/CXCL12 chemokine pathway reduces the development of murine pulmonary metastases. Clinical & Experimental Metastasis. 2008;25(3):201–211. doi: 10.1007/s10585-007-9133-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Mori T, Chen SL, Amersi FF, Martinez SR, Kuo C, et al. Chemokine receptor CXCR4 expression in patients with melanoma and colorectal cancer liver metastases and the association with disease outcome. Annals of Surgery. 2006;244(1):113–120. doi: 10.1097/01.sla.0000217690.65909.9c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Takeuchi H, Lam ST, Turner RR, Wang HJ, Kuo C, et al. Chemokine receptor CXCR4 expression in colorectal cancer patients increases the risk for recurrence and for poor survival. Journal of Clinical Oncology. 2005;23(12):2744–2753. doi: 10.1200/JCO.2005.07.078. [DOI] [PubMed] [Google Scholar]
- Ko SY, Park CJ, Park SH, Cho YU, Jang S, Seo E, et al. High CXCR4 and low VLA-4 expression predicts poor survival in adults with acute lymphoblastic leukemia. Leukemia Research. 2014;38(1):65–70. doi: 10.1016/j.leukres.2013.10.016. [DOI] [PubMed] [Google Scholar]
- Kojima Y, Acar A, Eaton EN, Mellody KT, Scheel C, Ben-Porath I, et al. Autocrine TGF-beta and stromal cell-derived factor-1 (SDF-1) signaling drives the evolution of tumor-promoting mammary stromal myofibroblasts. Proceedings of the National Academy of Sciences of the United States of America. 2010;107(46):20009–20014. doi: 10.1073/pnas.1013805107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konoplev S, Jorgensen JL, Thomas DA, Lin E, Burger J, Kantarjian HM, et al. Phosphorylated CXCR4 is associated with poor survival in adults with B-acute lymphoblastic leukemia. Cancer. 2011;117(20):4689–4695. doi: 10.1002/cncr.26113. [DOI] [PubMed] [Google Scholar]
- Konopleva MY, Jordan CT. Leukemia stem cells and microenvironment: Biology and therapeutic targeting. Journal of Clinical Oncology. 2011;29(5):591–599. doi: 10.1200/JCO.2010.31.0904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kryczek I, Wei S, Keller E, Liu R, Zou W. Stroma-derived factor (SDF-1/CXCL12) and human tumor pathogenesis. American Journal of Physiology. Cell Physiology. 2007;292(3):C987–C995. doi: 10.1152/ajpcell.00406.2006. http://dx.doi.org/10.1152/ajpcell.00406.2006. [DOI] [PubMed] [Google Scholar]
- Kucia M, Jankowski K, Reca R, Wysoczynski M, Bandura L, Allendorf DJ, et al. CXCR4-SDF-1 signalling, locomotion, chemotaxis and adhesion. Journal of Molecular Histology. 2004;35(3):233–245. doi: 10.1023/b:hijo.0000032355.66152.b8. [DOI] [PubMed] [Google Scholar]
- Kucia M, Reca R, Miekus K, Wanzeck J, Wojakowski W, Janowska-Wieczorek A, et al. Trafficking of normal stem cells and metastasis of cancer stem cells involve similar mechanisms: Pivotal role of the SDF-1-CXCR4 axis. Stem Cells. 2005;23(7):879–894. doi: 10.1634/stemcells.2004-0342. [DOI] [PubMed] [Google Scholar]
- Kuhne MR, Mulvey T, Belanger B, Chen S, Pan C, Chong C, et al. BMS-936564/MDX-1338: A fully human anti-CXCR4 antibody induces apoptosis in vitro and shows antitumor activity in vivo in hematologic malignancies. Clinical Cancer Research. 2012;19(2):357–366. doi: 10.1158/1078-0432.CCR-12-2333. [DOI] [PubMed] [Google Scholar]
- Kuil J, Buckle T, Oldenburg J, Yuan H, Borowsky AD, Josephson L, et al. Hybrid peptide dendrimers for imaging of chemokine receptor 4 (CXCR4) expression. Molecular Pharmaceutics. 2011;8(6):2444–2453. doi: 10.1021/mp200401p. http://dx.doi.org/10.1021/mp200401p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuil J, Buckle T, Yuan H, van den Berg NS, Oishi S, Fujii N, et al. Synthesis and evaluation of a bimodal CXCR4 antagonistic peptide. Bioconjugate Chemistry. 2011;22(5):859–864. doi: 10.1021/bc2000947. http://dx.doi.org/10.1021/bc2000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kukreja P, Abdel-Mageed AB, Mondal D, Liu K, Agrawal KC. Up-regulation of CXCR4 expression in PC-3 cells by stromal-derived factor-1alpha (CXCL12) increases endothelial adhesion and transendothelial migration: Role of MEK/ERK signaling pathway-dependent NF-kappaB activation. Cancer Research. 2005;65(21):9891–9898. doi: 10.1158/0008-5472.CAN-05-1293. [DOI] [PubMed] [Google Scholar]
- Kwong J, Kulbe H, Wong D, Chakravarty P, Balkwill F. An antagonist of the chemokine receptor CXCR4 induces mitotic catastrophe in ovarian cancer cells. Molecular Cancer Therapeutics. 2009;8(7):1893–1905. doi: 10.1158/1535-7163.MCT-08-0966. [DOI] [PubMed] [Google Scholar]
- Lanza F, Lemoli RM, Olivieri A, Laszlo D, Martino M, Specchia G, et al. Factors affecting successful mobilization with plerixafor: An Italian prospective survey in 215 patients with multiple myeloma and lymphoma. Transfusion. 2014;54(2):331–339. doi: 10.1111/trf.12265. [DOI] [PubMed] [Google Scholar]
- Lazarini F, Tham TN, Casanova P, Arenzana-Seisdedos F, Dubois-Dalcq M. Role of the alpha-chemokine stromal cell-derived factor (SDF-1) in the developing and mature central nervous system. Glia. 2003;42(2):139–148. doi: 10.1002/glia.10139. [DOI] [PubMed] [Google Scholar]
- Le Y, Zhou Y, Iribarren P, Wang J. Chemokines and chemokine receptors: Their manifold roles in homeostasis and disease. Cellular and Molecular Immunology. 2004;1(2):95–104. [PubMed] [Google Scholar]
- Lederer A, DeMarco SJ, Henze H, Romagnoli B, Mukherjee R, Zumbrunn J, et al. Discovery of highly potent and selective CXCR4 inhibitors using protein epitope mimetics (PEM) technology. Chimia. 2007;61(4):147–150. [Google Scholar]
- Li G, Badin G, Zhao A, Gentil-Perret A, Tostain J, Peoc’h M, et al. Prognostic value of CXCR4 expression in patients with clear cell renal cell carcinoma. Histology and Histopathology. 2013;28(9):1217–1222. doi: 10.14670/HH-28.1217. [DOI] [PubMed] [Google Scholar]
- Li W, Gomez E, Zhang Z. Immunohistochemical expression of stromal cell-derived factor-1 (SDF-1) and CXCR4 ligand receptor system in hepatocellular carcinoma. Journal of Experimental & Clinical Cancer Research. 2007;26(4):527–533. [PubMed] [Google Scholar]
- Li CX, Wu DP, Wang YD, Yu GH, Liu JM, Zhuang YM, et al. Expression of CXCR4 and its effect on the biological behavior of multiple myeloma cells. Zhonghua Xue Ye Xue Za Zhi. 2003;24(3):122–125. [PubMed] [Google Scholar]
- Liang Z, Yoon Y, Votaw J, Goodman MM, Williams L, Shim H. Silencing of CXCR4 blocks breast cancer metastasis. Cancer Research. 2005;65(3):967–971. [PMC free article] [PubMed] [Google Scholar]
- Liang Z, Zhan W, Zhu A, Yoon Y, Lin S, Sasaki M, et al. Development of a unique small molecule modulator of CXCR4. PLoS One. 2012;7(4):e34038. doi: 10.1371/journal.pone.0034038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao YX, Zhou CH, Zeng H, Zuo DQ, Wang ZY, Yin F, et al. The role of the CXCR4/CXCL12/CXCR7 axis in the progression and metastasis of bone sarcomas (Review) International Journal of Molecular Medicine. 2013;32(6):1239–1246. doi: 10.3892/ijmm.2013.1521. [DOI] [PubMed] [Google Scholar]
- Liles WC, Broxmeyer HE, Rodger E, Wood B, Hubel K, Cooper S, et al. Mobilization of hematopoietic progenitor cells in healthy volunteers by AMD3100, a CXCR4 antagonist. Blood. 2003;102(8):2728–2730. doi: 10.1182/blood-2003-02-0663. [DOI] [PubMed] [Google Scholar]
- Ling X, Spaeth E, Chen Y, Shi Y, Zhang W, Schober W, et al. The CXCR4 antagonist AMD3465 regulates oncogenic signaling and invasiveness in vitro and prevents breast cancer growth and metastasis in vivo. PLoS One. 2013;8(3):e58426. doi: 10.1371/journal.pone.0058426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu CF, Liu SY, Min XY, Ji YY, Wang N, Liu D, et al. The prognostic value of CXCR4 in ovarian cancer: A meta-analysis. PLoS One. 2014;9(3):e92629. doi: 10.1371/journal.pone.0092629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y, Wang B, Wang J, Wan W, Sun R, Zhao Y, et al. Down-regulation of PKCzeta expression inhibits chemotaxis signal transduction in human lung cancer cells. Lung Cancer. 2009;63(2):210–218. doi: 10.1016/j.lungcan.2008.05.010. [DOI] [PubMed] [Google Scholar]
- Longo-Imedio MI, Longo N, Trevino I, Lazaro P, Sanchez-Mateos P. Clinical significance of CXCR3 and CXCR4 expression in primary melanoma. International Journal of Cancer. 2005;117(5):861–865. doi: 10.1002/ijc.21269. [DOI] [PubMed] [Google Scholar]
- Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Y, Hwang RF, Logsdon CD, Ullrich SE. Dynamic mast cell-stromal cell interactions promote growth of pancreatic cancer. Cancer Research. 2013;73(13):3927–3937. doi: 10.1158/0008-5472.CAN-12-4479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma Q, Jones D, Borghesani PR, Segal RA, Nagasawa T, Kishimoto T, et al. Impaired B-lymphopoiesis, myelopoiesis, and derailed cerebellar neuron migration in CXCR4- and SDF-1-deficient mice. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(16):9448–9453. doi: 10.1073/pnas.95.16.9448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marechal R, Demetter P, Nagy N, Berton A, Decaestecker C, Polus M, et al. High expression of CXCR4 may predict poor survival in resected pancreatic adenocarcinoma. British Journal of Cancer. 2009;100(9):1444–1451. doi: 10.1038/sj.bjc.6605020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masuda M, Nakashima H, Ueda T, Naba H, Ikoma R, Otaka A, et al. A novel anti-hiv synthetic peptide, T-22 ([Tyr5,12, Lys7]-polyphemusin-II) Biochemical and Biophysical Research Communications. 1992;189(2):845–850. doi: 10.1016/0006-291x(92)92280-b. http://dx.doi.org/10.1016/0006-291x(92)92280-b. [DOI] [PubMed] [Google Scholar]
- Mavier P, Martin N, Couchie D, Preaux AM, Laperche Y, Zafrani ES. Expression of stromal cell-derived factor-1 and of its receptor CXCR4 in liver regeneration from oval cells in rat. American Journal of Pathology. 2004;165(6):1969–1977. doi: 10.1016/S0002-9440(10)63248-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDermott DH, Liu Q, Velez D, Lopez L, Anaya-O’Brien S, Ulrick J, et al. A phase 1 clinical trial of long-term, low-dose treatment of WHIM syndrome with the CXCR4 antagonist plerixafor. Blood. 2014;123(15):2308–2316. doi: 10.1182/blood-2013-09-527226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meads MB, Hazlehurst LA, Dalton WS. The bone marrow microenvironment as a tumor sanctuary and contributor to drug resistance. Clinical Cancer Research. 2008;14(9):2519–2526. doi: 10.1158/1078-0432.CCR-07-2223. [DOI] [PubMed] [Google Scholar]
- Meincke M, Tiwari S, Hattermann K, Kalthoff H, Mentlein R. Near-infrared molecular imaging of tumors via chemokine receptors CXCR4 and CXCR7. Clinical & Experimental Metastasis. 2011;28(8):713–720. doi: 10.1007/s10585-011-9403-y. http://dx.doi.org/10.1007/s10585-011-9403-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellado M, Rodriguez-Frade JM, Manes S, Martinez AC. Chemokine signaling and functional responses: The role of receptor dimerization and TK pathway activation. Annual Review of Immunology. 2001;19:397–421. doi: 10.1146/annurev.immunol.19.1.397. [DOI] [PubMed] [Google Scholar]
- Misra P, Lebeche D, Ly H, Schwarzkopf M, Diaz G, Hajjar RJ, et al. Quantitation of CXCR4 expression in myocardial infarction using Tc-99 m-labeled SDF-1 alpha. Journal of Nuclear Medicine. 2008;49(6):963–969. doi: 10.2967/jnumed.107.050054. http://dx.doi.org/10.2967/jnumed.107.050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyata T, Tokunaga F, Yoneya T, Yoshikawa K, Iwanaga S, Niwa M, et al. Antimicrobial peptides, isolated from horseshoe-crab hemocytes, tachyplesin-II, and polyphemusin-I and polyphemusin-II—Chemical structures and biological-activity. Journal of Biochemistry. 1989;106(4):663–668. doi: 10.1093/oxfordjournals.jbchem.a122913. [DOI] [PubMed] [Google Scholar]
- Mo W, Chen J, Patel A, Zhang L, Chau V, Li Y, et al. CXCR4/CXCL12 mediate autocrine cell-cycle progression in NF1-associated malignant peripheral nerve sheath tumors. Cell. 2013;152(5):1077–1090. doi: 10.1016/j.cell.2013.01.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohle R, Failenschmid C, Bautz F, Kanz L. Overexpression of the chemokine receptor CXCR4 in B cell chronic lymphocytic leukemia is associated with increased functional response to stromal cell-derived factor-1 (SDF-1) Leukemia. 1999;13(12):1954–1959. doi: 10.1038/sj.leu.2401602. [DOI] [PubMed] [Google Scholar]
- Mori T, Doi R, Koizumi M, Toyoda E, Ito D, Kami K, et al. CXCR4 antagonist inhibits stromal cell-derived factor 1-induced migration and invasion of human pancreatic cancer. Molecular Cancer Therapeutics. 2004;3(1):29–37. [PubMed] [Google Scholar]
- Morimoto M, Mori H, Otake T, Ueba N, Kunita N, Niwa M, et al. Inhibitory effect of tachyplesin-I on the proliferation of human-immunodeficiency-virus in vitro. Chemotherapy. 1991;37(3):206–211. doi: 10.1159/000238855. [DOI] [PubMed] [Google Scholar]
- Mosley CA, Wilson LJ, Wiseman JM, Skudlarek JW, Liotta DC. Recent patents regarding the discovery of small molecule CXCR4 antagonists. Expert Opinion on Therapeutic Patents. 2009;19(1):23–38. doi: 10.1517/13543770802553483. [DOI] [PubMed] [Google Scholar]
- Muller A, Homey B, Soto H, Ge N, Catron D, Buchanan ME, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001;410(6824):50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- Murakami T, Cardones AR, Hwang ST. Chemokine receptors and melanoma metastasis. Journal of Dermatological Science. 2004;36(2):71–78. doi: 10.1016/j.jdermsci.2004.03.002. [DOI] [PubMed] [Google Scholar]
- Murakami T, Maki W, Cardones AR, Fang H, Tun Kyi A, Nestle FO, et al. Expression of CXC chemokine receptor-4 enhances the pulmonary metastatic potential of murine B16 melanoma cells. Cancer Research. 2002;62(24):7328–7334. [PubMed] [Google Scholar]
- Murthy SC, Reznik SI, Ogwudu UC, Farver CF, Arrossi A, Batizy LH, et al. Winning the battle, losing the war: The noncurative “curative” resection for stage I adenocarcinoma of the lung. Annals of Thoracic Surgery. 2010;90(4):1067–1074. doi: 10.1016/j.athoracsur.2010.04.108. [DOI] [PubMed] [Google Scholar]
- Nagasawa T, Hirota S, Tachibana K, Takakura N, Nishikawa S, Kitamura Y, et al. Defects of B-cell lymphopoiesis and bone-marrow myelopoiesis in mice lacking the CXC chemokine PBSF/SDF-1. Nature. 1996;382(6592):635–638. doi: 10.1038/382635a0. [DOI] [PubMed] [Google Scholar]
- Nakamura T, Furunaka H, Miyata T, Tokunaga F, Muta T, Iwanaga S, et al. Tachyplesin, a class of antimicrobial peptide from the hemocytes of the horseshoe-crab (Tachypleus tridentatus)—Isolation and chemical-structure. Journal of Biological Chemistry. 1988;263(32):16709–16713. [PubMed] [Google Scholar]
- Nakashima H, Masuda M, Murakami T, Koyanagi Y, Matsumoto A, Fujii N, et al. Anti-human-immunodeficiency-virus activity of a novel synthetic peptide, T22 ([Tyr-5,12, Lys-7]polyphemusin II)—A possible inhibitor of virus-cell fusion. Antimicrobial Agents and Chemotherapy. 1992;36(6):1249–1255. doi: 10.1128/aac.36.6.1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCI. Clinical trials (PDQ®) 2014 [Google Scholar]
- Nervi B, Ramirez P, Rettig MP, Uy GL, Holt MS, Ritchey JK, et al. Chemosensitization of acute myeloid leukemia (AML) following mobilization by the CXCR4 antagonist AMD3100. Blood. 2009;113(24):6206–6214. doi: 10.1182/blood-2008-06-162123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimmagadda S, Pullambhatla M, Pomper MG. Immunoimaging of CXCR4 expression in brain tumor xenografts using SPECT/CT. Journal of Nuclear Medicine. 2009;50(7):1124–1130. doi: 10.2967/jnumed.108.061325. http://dx.doi.org/10.2967/jnumed.108.061325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimmagadda S, Pullambhatla M, Stone K, Green G, Bhujwalla ZM, Pomper MG. Molecular imaging of CXCR4 receptor expression in human cancer xenografts with [Cu-64]AMD3100 positron emission tomography. Cancer Research. 2010;70(10):3935–3944. doi: 10.1158/0008-5472.CAN-09-4396. http://dx.doi.org/10.1158/0008-5472.can-09-4396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberlin E, Amara A, Bachelerie F, Bessia C, Virelizier JL, Arenzana-Seisdedos F, et al. The CXC chemokine SDF-1 is the ligand for LESTR/fusin and prevents infection by T-cell-line-adapted HIV-1. Nature. 1996;382(6594):833–835. doi: 10.1038/382833a0. [DOI] [PubMed] [Google Scholar]
- Obermajer N, Muthuswamy R, Odunsi K, Edwards RP, Kalinski P. PGE(2)-induced CXCL12 production and CXCR4 expression controls the accumulation of human MDSCs in ovarian cancer environment. Cancer Research. 2011;71(24):7463–7470. doi: 10.1158/0008-5472.CAN-11-2449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Boyle G, Swidenbank I, Marshall H, Barker CE, Armstrong J, White SA, et al. Inhibition of CXCR4/CXCL12 chemotaxis in melanoma by AMD11070. British Journal of Cancer. 2013;108(8):1634–1640. doi: 10.1038/bjc.2013.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oh YS, Kim HY, Song IC, Yun HJ, Jo DY, Kim S, et al. Hypoxia induces CXCR4 expression and biological activity in gastric cancer cells through activation of hypoxia-inducible factor-1alpha. Oncology Reports. 2012;28(6):2239–2246. doi: 10.3892/or.2012.2063. [DOI] [PubMed] [Google Scholar]
- Olumi AF, Grossfeld GD, Hayward SW, Carroll PR, Tlsty TD, Cunha GR. Carcinoma-associated fibroblasts direct tumor progression of initiated human prostatic epithelium. Cancer Research. 1999;59(19):5002–5011. doi: 10.1186/bcr138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orditura M, Galizia G, Sforza V, Gambardella V, Fabozzi A, Laterza MM, et al. Treatment of gastric cancer. World Journal of Gastroenterology. 2014;20(7):1635–1649. doi: 10.3748/wjg.v20.i7.1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orimo A, Gupta PB, Sgroi DC, Arenzana-Seisdedos F, Delaunay T, Naeem R, et al. Stromal fibroblasts present in invasive human breast carcinomas promote tumor growth and angiogenesis through elevated SDF-1/CXCL12 secretion. Cell. 2005;121(3):335–348. doi: 10.1016/j.cell.2005.02.034. [DOI] [PubMed] [Google Scholar]
- Otsuka S, Klimowicz AC, Kopciuk K, Petrillo SK, Konno M, Hao D, et al. CXCR4 overexpression is associated with poor outcome in females diagnosed with stage IV non-small cell lung cancer. Journal of Thoracic Oncology. 2011;6(7):1169–1178. doi: 10.1097/JTO.0b013e3182199a99. [DOI] [PubMed] [Google Scholar]
- Pan J, Mestas J, Burdick MD, Phillips RJ, Thomas GV, Reckamp K, et al. Stromal derived factor-1 (SDF-1/CXCL12) and CXCR4 in renal cell carcinoma metastasis. Molecular Cancer. 2006;5:56. doi: 10.1186/1476-4598-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parmo-Cabanas M, Bartolome RA, Wright N, Hidalgo A, Drager AM, Teixido J. Integrin alpha4beta1 involvement in stromal cell-derived factor-1alpha-promoted myeloma cell transendothelial migration and adhesion: Role of cAMP and the actin cytoskeleton in adhesion. Experimental Cell Research. 2004;294(2):571–580. doi: 10.1016/j.yexcr.2003.12.003. [DOI] [PubMed] [Google Scholar]
- Pei RZ, Tang SH, Ma JX, Zhang PS, Liu XH, Du XH, et al. Relationship between expression of chemokine receptor and curative effect of multiple myeloma. Zhongguo Shi Yan Xue Ye Xue Za Zhi. 2011;19(1):73–75. [PubMed] [Google Scholar]
- Peitzsch C, Kurth I, Kunz-Schughart L, Baumann M, Dubrovska A. Discovery of the cancer stem cell related determinants of radioresistance. Radiotherapy and Oncology. 2013;108(3):378–387. doi: 10.1016/j.radonc.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Peled A, Abraham M, Avivi I, Rowe JM, Beider K, Wald H, et al. The high-affinity CXCR4 antagonist BKT140 is safe and induces a robust mobilization of human CD34+ cells in patients with multiple myeloma. Clinical Cancer Research. 2014;20(2):469–479. doi: 10.1158/1078-0432.CCR-13-1302. [DOI] [PubMed] [Google Scholar]
- Peled A, Tavor S. Role of CXCR4 in the pathogenesis of acute myeloid leukemia. Theranostics. 2013;3(1):34–39. doi: 10.7150/thno.5150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petit I, Jin D, Rafii S. The SDF-1-CXCR4 signaling pathway: A molecular hub modulating neo-angiogenesis. Trends in Immunology. 2007;28(7):299–307. doi: 10.1016/j.it.2007.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer M, Hartmann TN, Leick M, Catusse J, Schmitt-Graeff A, Burger M. Alternative implication of CXCR4 in JAK2/STAT3 activation in small cell lung cancer. British Journal of Cancer. 2009;100(12):1949–1956. doi: 10.1038/sj.bjc.6605068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips RJ, Burdick MD, Lutz M, Belperio JA, Keane MP, Strieter RM. The stromal derived factor-1/CXCL12-CXC chemokine receptor 4 biological axis in non-small cell lung cancer metastases. American Journal of Respiratory and Critical Care Medicine. 2003;167(12):1676–1686. doi: 10.1164/rccm.200301-071OC. [DOI] [PubMed] [Google Scholar]
- Phillips RJ, Mestas J, Gharaee-Kermani M, Burdick MD, Sica A, Belperio JA, et al. Epidermal growth factor and hypoxia-induced expression of CXC chemokine receptor 4 on non-small cell lung cancer cells is regulated by the phosphatidylinositol 3-kinase/PTEN/AKT/mammalian target of rapamycin signaling pathway and activation of hypoxia inducible factor-1alpha. Journal of Biological Chemistry. 2005;280(23):22473–22481. doi: 10.1074/jbc.M500963200. [DOI] [PubMed] [Google Scholar]
- Pierce KL, Premont RT, Lefkowitz RJ. Seven-transmembrane receptors. Nature Reviews. Molecular Cell Biology. 2002;3(9):639–650. doi: 10.1038/nrm908. [DOI] [PubMed] [Google Scholar]
- Ping YF, Yao XH, Jiang JY, Zhao LT, Yu SC, Jiang T, et al. The chemokine CXCL12 and its receptor CXCR4 promote glioma stem cell-mediated VEGF production and tumour angiogenesis via PI3K/AKT signalling. Journal of Pathology. 2011;224(3):344–354. doi: 10.1002/path.2908. [DOI] [PubMed] [Google Scholar]
- Portella L, Vitale R, De Luca S, D’Alterio C, Ierano C, Napolitano M, et al. Preclinical development of a novel class of CXCR4 antagonist impairing solid tumors growth and metastases. PLoS One. 2013;8(9):e74548. doi: 10.1371/journal.pone.0074548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porvasnik S, Sakamoto N, Kusmartsev S, Eruslanov E, Kim WJ, Cao W, et al. Effects of CXCR4 antagonist CTCE-9908 on prostate tumor growth. Prostate. 2009;69(13):1460–1469. doi: 10.1002/pros.21008. [DOI] [PubMed] [Google Scholar]
- Qu QX, Huang Q, Xu J, Duan LT, Zhu YB, Zhang XG. CD40 signal regulates CXCR4 mediating ovarian carcinoma cell migration: Implications for extrapelvic metastastic factors. Oncology Research. 2013;20(9):383–392. doi: 10.3727/096504013X13657689382653. [DOI] [PubMed] [Google Scholar]
- Ratajczak MZ, Majka M, Kucia M, Drukala J, Pietrzkowski Z, Peiper S, et al. Expression of functional CXCR4 by muscle satellite cells and secretion of SDF-1 by muscle-derived fibroblasts is associated with the presence of both muscle progenitors in bone marrow and hematopoietic stem/progenitor cells in muscles. Stem Cells. 2003;21(3):363–371. doi: 10.1634/stemcells.21-3-363. [DOI] [PubMed] [Google Scholar]
- Ratajczak MZ, Zuba-Surma E, Kucia M, Reca R, Wojakowski W, Ratajczak J. The pleiotropic effects of the SDF-1-CXCR4 axis in organogenesis, regeneration and tumorigenesis. Leukemia. 2006;20(11):1915–1924. doi: 10.1038/sj.leu.2404357. [DOI] [PubMed] [Google Scholar]
- Reckamp KL, Figlin RA, Burdick MD, Dubinett SM, Elashoff RM, Strieter RM. CXCR4 expression on circulating pan-cytokeratin positive cells is associated with survival in patients with advanced non-small cell lung cancer. BMC Cancer. 2009;9:213. doi: 10.1186/1471-2407-9-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redjal N, Chan JA, Segal RA, Kung AL. CXCR4 inhibition synergizes with cytotoxic chemotherapy in gliomas. Clinical Cancer Research. 2006;12(22):6765–6771. doi: 10.1158/1078-0432.CCR-06-1372. [DOI] [PubMed] [Google Scholar]
- Rempel SA, Dudas S, Ge S, Gutierrez JA. Identification and localization of the cytokine SDF1 and its receptor, CXC chemokine receptor 4, to regions of necrosis and angiogenesis in human glioblastoma. Clinical Cancer Research. 2000;6(1):102–111. [PubMed] [Google Scholar]
- Rhodes LV, Short SP, Neel NF, Salvo VA, Zhu Y, Elliott S, et al. Cytokine receptor CXCR4 mediates estrogen-independent tumorigenesis, metastasis, and resistance to endocrine therapy in human breast cancer. Cancer Research. 2011;71(2):603–613. doi: 10.1158/0008-5472.CAN-10-3185. http://dx.doi.org/10.1158/0008-5472.CAN-10-3185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin JB, Kung AL, Klein RS, Chan JA, Sun Y, Schmidt K, et al. A small-molecule antagonist of CXCR4 inhibits intracranial growth of primary brain tumors. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(23):13513–13518. doi: 10.1073/pnas.2235846100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini V, Marchese A, Majetschak M. CXC chemokine receptor 4 is a cell surface receptor for extracellular ubiquitin. Journal of Biological Chemistry. 2010;285(20):15566–15576. doi: 10.1074/jbc.M110.103408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saintigny P, Burger JA. Recent advances in non-small cell lung cancer biology and clinical management. Discovery Medicine. 2012;13(71):287–297. [PubMed] [Google Scholar]
- Salcedo R, Wasserman K, Young HA, Grimm MC, Howard OM, Anver MR, et al. Vascular endothelial growth factor and basic fibroblast growth factor induce expression of CXCR4 on human endothelial cells: In vivo neovascularization induced by stromal-derived factor-1alpha. American Journal of Pathology. 1999;154(4):1125–1135. doi: 10.1016/s0002-9440(10)65365-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvucci O, Bouchard A, Baccarelli A, Deschenes J, Sauter G, Simon R, et al. The role of CXCR4 receptor expression in breast cancer: A large tissue microarray study. Breast Cancer Research and Treatment. 2006;97(3):275–283. doi: 10.1007/s10549-005-9121-8. [DOI] [PubMed] [Google Scholar]
- Sasaki K, Natsugoe S, Ishigami S, Matsumoto M, Okumura H, Setoyama T, et al. Expression of CXCL12 and its receptor CXCR4 correlates with lymph node metastasis in submucosal esophageal cancer. Journal of Surgical Oncology. 2008;97(5):433–438. doi: 10.1002/jso.20976. [DOI] [PubMed] [Google Scholar]
- Sasaki K, Natsugoe S, Ishigami S, Matsumoto M, Okumura H, Setoyama T, et al. Expression of CXCL12 and its receptor CXCR4 in esophageal squamous cell carcinoma. Oncology Reports. 2009;21(1):65–71. [PubMed] [Google Scholar]
- Scala S, Ottaiano A, Ascierto PA, Cavalli M, Simeone E, Giuliano P, et al. Expression of CXCR4 predicts poor prognosis in patients with malignant melanoma. Clinical Cancer Research. 2005;11(5):1835–1841. doi: 10.1158/1078-0432.CCR-04-1887. [DOI] [PubMed] [Google Scholar]
- Schabath R, Muller G, Schubel A, Kremmer E, Lipp M, Forster R. The murine chemokine receptor CXCR4 is tightly regulated during T cell development and activation. Journal of Leukocyte Biology. 1999;66(6):996–1004. doi: 10.1002/jlb.66.6.996. [DOI] [PubMed] [Google Scholar]
- Schimanski CC, Bahre R, Gockel I, Muller A, Frerichs K, Horner V, et al. Dissemination of hepatocellular carcinoma is mediated via chemokine receptor CXCR4. British Journal of Cancer. 2006;95(2):210–217. doi: 10.1038/sj.bjc.6603251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimanski CC, Schwald S, Simiantonaki N, Jayasinghe C, Gonner U, Wilsberg V, et al. Effect of chemokine receptors CXCR4 and CCR7 on the metastatic behavior of human colorectal cancer. Clinical Cancer Research. 2005;11(5):1743–1750. doi: 10.1158/1078-0432.CCR-04-1195. [DOI] [PubMed] [Google Scholar]
- Schmitt S, Weinhold N, Dembowsky K, Neben K, Witzens-Harig M, Braun M, et al. First results of a phase-II study with the new CXCR4 antagonist POL6326 to mobilize hematopoietic stem cells (HSC) in multiple myeloma (MM) Blood. 2010;116(21):359–360. [Google Scholar]
- Schober A, Zernecke A. Chemokines in vascular remodeling. Thrombosis & Haemostasis. 2007;97(5):730–737. [PubMed] [Google Scholar]
- Schuller U, Koch A, Hartmann W, Garre ML, Goodyer CG, Cama A, et al. Subtype-specific expression and genetic alterations of the chemokinereceptor gene CXCR4 in medulloblastomas. International Journal of Cancer. 2005;117(1):82–89. doi: 10.1002/ijc.21116. [DOI] [PubMed] [Google Scholar]
- Sehgal A, Keener C, Boynton AL, Warrick J, Murphy GP. CXCR-4, a chemokine receptor, is overexpressed in and required for proliferation of glioblastoma tumor cells. Journal of Surgical Oncology. 1998;69(2):99–104. doi: 10.1002/(sici)1096-9098(199810)69:2<99::aid-jso10>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- Sethi T, Rintoul RC, Moore SM, MacKinnon AC, Salter D, Choo C, et al. Extracellular matrix proteins protect small cell lung cancer cells against apoptosis: A mechanism for small cell lung cancer growth and drug resistance in vivo. Nature Medicine. 1999;5(6):662–668. doi: 10.1038/9511. [DOI] [PubMed] [Google Scholar]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA: A Cancer Journal for Clinicians. 2012;62(1):10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- Singh S, Srivastava SK, Bhardwaj A, Owen LB, Singh AP. CXCR4/CXCL12 signalling axis confers gemcitabine resistance to pancreatic cancer cells: A novel target for therapy. British Journal of Cancer. 2010;103(11):1671–1679. doi: 10.1038/sj.bjc.6605968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sison EA, McIntyre E, Magoon D, Brown P. Dynamic chemotherapy-induced upregulation of CXCR4 expression: A mechanism of therapeutic resistance in pediatric AML. Molecular Cancer Research. 2013;11(9):1004–1016. doi: 10.1158/1541-7786.MCR-13-0114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JR, Falkenhagen KM, Coupland SE, Chipps TJ, Rosenbaum JT, Braziel RM. Malignant B cells from patients with primary central nervous system lymphoma express stromal cell-derived factor-1. American Journal of Clinical Pathology. 2007;127(4):633–641. doi: 10.1309/NUQHJ79BHWYD9TAF. [DOI] [PubMed] [Google Scholar]
- Smith MC, Luker KE, Garbow JR, Prior JL, Jackson E, Piwnica-Worms D, et al. CXCR4 regulates growth of both primary and metastatic breast cancer. Cancer Research. 2004;64(23):8604–8612. doi: 10.1158/0008-5472.CAN-04-1844. [DOI] [PubMed] [Google Scholar]
- Smith H, Whittall C, Weksler B, Middleton J. Chemokines stimulate bidirectional migration of human mesenchymal stem cells across bone marrow endothelial cells. Stem Cells and Development. 2012;21(3):476–486. doi: 10.1089/scd.2011.0025. [DOI] [PubMed] [Google Scholar]
- Spano JP, Andre F, Morat L, Sabatier L, Besse B, Combadiere C, et al. Chemokine receptor CXCR4 and early-stage non-small cell lung cancer: Pattern of expression and correlation with outcome. Annals of Oncology. 2004;15(4):613–617. doi: 10.1093/annonc/mdh136. [DOI] [PubMed] [Google Scholar]
- Spoo AC, Lubbert M, Wierda WG, Burger JA. CXCR4 is a prognostic marker in acute myelogenous leukemia. Blood. 2007;109(2):786–791. doi: 10.1182/blood-2006-05-024844. [DOI] [PubMed] [Google Scholar]
- Staller P, Sulitkova J, Lisztwan J, Moch H, Oakeley EJ, Krek W. Chemokine receptor CXCR4 downregulated by von Hippel-Lindau tumour suppressor pVHL. Nature. 2003;425(6955):307–311. doi: 10.1038/nature01874. [DOI] [PubMed] [Google Scholar]
- Steinberg M, Silva M. Plerixafor: A chemokine receptor-4 antagonist for mobilization of hematopoietic stem cells for transplantation after high-dose chemotherapy for non-Hodgkin’s lymphoma or multiple myeloma. Clinical Therapeutics. 2010;32(5):821–843. doi: 10.1016/j.clinthera.2010.05.007. [DOI] [PubMed] [Google Scholar]
- Stessman HA, Mansoor A, Zhan F, Janz S, Linden MA, Baughn LB, et al. Reduced CXCR4 expression is associated with extramedullary disease in a mouse model of myeloma and predicts poor survival in multiple myeloma patients treated with bortezomib. Leukemia. 2013;27(10):2075–2077. doi: 10.1038/leu.2013.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su L, Zhang J, Xu H, Wang Y, Chu Y, Liu R, et al. Differential expression of CXCR4 is associated with the metastatic potential of human non-small cell lung cancer cells. Clinical Cancer Research. 2005;11(23):8273–8280. doi: 10.1158/1078-0432.CCR-05-0537. [DOI] [PubMed] [Google Scholar]
- Sun X, Cheng G, Hao M, Zheng J, Zhou X, Zhang J, et al. CXCL12/CXCR4/CXCR7 chemokine axis and cancer progression. Cancer and Metastasis Reviews. 2010;29(4):709–722. doi: 10.1007/s10555-010-9256-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun X, Cheng G, Hao M, Zheng J, Zhou X, Zhang J, et al. CXCL12/CXCR4/CXCR7 chemokine axis and cancer progression (vol 29, pg 709, 2010) Cancer and Metastasis Reviews. 2011;30(2):269–270. doi: 10.1007/s10555-010-9256-x. http://dx.doi.org/10.1007/s10555-010-9266-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun YX, Schneider A, Jung Y, Wang J, Dai J, Wang J, et al. Skeletal localization and neutralization of the SDF-1(CXCL12)/CXCR4 axis blocks prostate cancer metastasis and growth in osseous sites in vivo. Journal of Bone and Mineral Research. 2005;20(2):318–329. doi: 10.1359/JBMR.041109. [DOI] [PubMed] [Google Scholar]
- Sun YX, Wang J, Shelburne CE, Lopatin DE, Chinnaiyan AM, Rubin MA, et al. Expression of CXCR4 and CXCL12 (SDF-1) in human prostate cancers (PCa) in vivo. Journal of Cellular Biochemistry. 2003;89(3):462–473. doi: 10.1002/jcb.10522. [DOI] [PubMed] [Google Scholar]
- Taichman RS, Cooper C, Keller ET, Pienta KJ, Taichman NS, McCauley LK. Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastasis to bone. Cancer Research. 2002;62(6):1832–1837. [PubMed] [Google Scholar]
- Tamamura H, Arakaki R, Funakoshi H, Imai M, Otaka A, Ibuka T, et al. Effective lowly cytotoxic analogs of an HIV-cell fusion inhibitor, T22 ([TyR5,12), Lys(7)]-polyphemusin II) Bioorganic & Medicinal Chemistry. 1998;6(2):231–238. doi: 10.1016/s0968-0896(97)10037-2. http://dx.doi.org/10.1016/s0968-0896(97)10037-2. [DOI] [PubMed] [Google Scholar]
- Tamamura H, Hiramatsu K, Mizumoto M, Ueda S, Kusano S, Terakubo S, et al. Enhancement of the T140-based pharmacophores leads to the development of more potent and bio-stable CXCR4 antagonists. Organic & Biomolecular Chemistry. 2003;1(21):3663–3669. doi: 10.1039/b306613b. [DOI] [PubMed] [Google Scholar]
- Tamamura H, Hori A, Kanzaki N, Hiramatsu K, Mizumoto M, Nakashima H, et al. T140 analogs as CXCR4 antagonists identified as anti-metastatic agents in the treatment of breast cancer. FEBS Letters. 2003;550(1–3):79–83. doi: 10.1016/s0014-5793(03)00824-x. http://dx.doi.org/10.1016/s0014-5793(03)00824-x. [DOI] [PubMed] [Google Scholar]
- Tamamura H, Omagari A, Oishi S, Kanamoto T, Yamamoto N, Peiper SC, et al. Pharmacophore identification of a specific CXCR4 inhibitor, T140, leads to development of effective anti-HIV agents with very high selectivity indexes. Bioorganic & Medicinal Chemistry Letters. 2000;10(23):2633–2637. doi: 10.1016/s0960-894x(00)00535-7. http://dx.doi.org/10.1016/s0960-894x(00)00535-7. [DOI] [PubMed] [Google Scholar]
- Tamamura H, Xu YO, Hattori T, Zhang XY, Arakaki R, Kanbara K, et al. A low-molecular-weight inhibitor against the chemokine receptor CXCR4: A strong anti-HIV peptide T140. Biochemical and Biophysical Research Communications. 1998;253(3):877–882. doi: 10.1006/bbrc.1998.9871. http://dx.doi.org/10.1006/bbrc.1998.9871. [DOI] [PubMed] [Google Scholar]
- Teicher BA. Antiangiogenic agents and targets: A perspective. Biochemical Pharmacology. 2011;81(1):6–12. doi: 10.1016/j.bcp.2010.09.023. [DOI] [PubMed] [Google Scholar]
- Thoma G, Streiff MB, Kovarik J, Glickman F, Wagner T, Beerli C, et al. Orally bioavailable isothioureas block function of the chemokine receptor CXCR4 in vitro and in vivo. Journal of Medicinal Chemistry. 2008;51(24):7915–7920. doi: 10.1021/jm801065q. http://dx.doi.org/10.1021/jm801065q. [DOI] [PubMed] [Google Scholar]
- Triano LR, Deshpande H, Gettinger SN. Management of patients with advanced non-small cell lung cancer: Current and emerging options. Drugs. 2010;70(2):167–179. doi: 10.2165/11532200-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Tripathi A, Saini V, Marchese A, Volkman BF, Tang WJ, Majetschak M. Modulation of the CXC chemokine receptor 4 agonist activity of ubiquitin through C-terminal protein modification. Biochemistry. 2013;52(24):4184–4192. doi: 10.1021/bi400254f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vagima Y, Lapid K, Kollet O, Goichberg P, Alon R, Lapidot T. Pathways implicated in stem cell migration: The SDF-1/CXCR4 axis. Methods in Molecular Biology. 2011;750:277–289. doi: 10.1007/978-1-61779-145-1_19. [DOI] [PubMed] [Google Scholar]
- Vandercappellen J, Van Damme J, Struyf S. The role of CXC chemokines and their receptors in cancer. Cancer Letters. 2008;267(2):226–244. doi: 10.1016/j.canlet.2008.04.050. [DOI] [PubMed] [Google Scholar]
- Vanharanta S, Shu W, Brenet F, Hakimi AA, Heguy A, Viale A, et al. Epigenetic expansion of VHL-HIF signal output drives multiorgan metastasis in renal cancer. Nature Medicine. 2013;19(1):50–56. doi: 10.1038/nm.3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vater A, Sahlmann J, Kroger N, Zollner S, Lioznov M, Maasch C, et al. Hematopoietic stem and progenitor cell mobilization in mice and humans by a first-in-class mirror-image oligonucleotide inhibitor of CXCL12. Clinical Pharmacology and Therapeutics. 2013;94(1):150–157. doi: 10.1038/clpt.2013.58. [DOI] [PubMed] [Google Scholar]
- Vila-Coro AJ, Rodriguez-Frade JM, Martin De Ana A, Moreno-Ortiz MC, Martinez AC, Mellado M. The chemokine SDF-1alpha triggers CXCR4 receptor dimerization and activates the JAK/STAT pathway. FASEB Journal. 1999;13(13):1699–1710. [PubMed] [Google Scholar]
- Viola A, Luster AD. Chemokines and their receptors: Drug targets in immunity and inflammation. Annual Review of Pharmacology and Toxicology. 2008;48:171–197. doi: 10.1146/annurev.pharmtox.48.121806.154841. [DOI] [PubMed] [Google Scholar]
- Vlahakis SR, Villasis-Keever A, Gomez T, Vanegas M, Vlahakis N, Paya CV. G protein-coupled chemokine receptors induce both survival and apoptotic signaling pathways. Journal of Immunology. 2002;169(10):5546–5554. doi: 10.4049/jimmunol.169.10.5546. [DOI] [PubMed] [Google Scholar]
- Wagner PL, Hyjek E, Vazquez MF, Meherally D, Liu YF, Chadwick PA, et al. CXCL12 and CXCR4 in adenocarcinoma of the lung: Association with metastasis and survival. Journal of Thoracic and Cardiovascular Surgery. 2009;137(3):615–621. doi: 10.1016/j.jtcvs.2008.07.039. [DOI] [PubMed] [Google Scholar]
- Waki M, Waki K, Miyamoto K, Matsumoto A, Tamamura H, Fujii N, et al. Molecular size of an anti-HIV peptide, T22, can be reduced without loss of the activity. Chemistry Letters. 1996;25(7):571–572. http://dx.doi.org/10.1246/cl.1996.571. [Google Scholar]
- Wald O, Izhar U, Amir G, Avniel S, Bar-Shavit Y, Wald H, et al. CD4+CXCR4highCD69+ T cells accumulate in lung adenocarcinoma. Journal of Immunology. 2006;177(10):6983–6990. doi: 10.4049/jimmunol.177.10.6983. [DOI] [PubMed] [Google Scholar]
- Wang L, Huang T, Chen W, Gao X, Zhou T, Wu Z, et al. Silencing of CXCR4 by RNA interference inhibits cell growth and metastasis in human renal cancer cells. Oncology Reports. 2012;28(6):2043–2048. doi: 10.3892/or.2012.2028. [DOI] [PubMed] [Google Scholar]
- Wang DF, Lou N, Qiu MZ, Lin YB, Liang Y. Effects of CXCR4 gene silencing by lentivirus shRNA on proliferation of the EC9706 human esophageal carcinoma cell line. Tumour Biology. 2013;34(5):2951–2959. doi: 10.1007/s13277-013-0858-0. [DOI] [PubMed] [Google Scholar]
- Wang JF, Park IW, Groopman JE. Stromal cell-derived factor-1alpha stimulates tyrosine phosphorylation of multiple focal adhesion proteins and induces migration of hematopoietic progenitor cells: Roles of phosphoinositide-3 kinase and protein kinase C. Blood. 2000;95(8):2505–2513. [PubMed] [Google Scholar]
- Wang J, Wang J, Sun Y, Song W, Nor JE, Wang CY, et al. Diverse signaling pathways through the SDF-1/CXCR4 chemokine axis in prostate cancer cell lines leads to altered patterns of cytokine secretion and angiogenesis. Cellular Signalling. 2005;17(12):1578–1592. doi: 10.1016/j.cellsig.2005.03.022. [DOI] [PubMed] [Google Scholar]
- Wang L, Wang L, Yang B, Yang Q, Qiao S, Wang Y, et al. Strong expression of chemokine receptor CXCR4 by renal cell carcinoma cells correlates with metastasis. Clinical & Experimental Metastasis. 2009;26(8):1049–1054. doi: 10.1007/s10585-009-9294-3. [DOI] [PubMed] [Google Scholar]
- Ward SG. T lymphocytes on the move: Chemokines, PI 3-kinase and beyond. Trends in Immunology. 2006;27(2):80–87. doi: 10.1016/j.it.2005.12.004. [DOI] [PubMed] [Google Scholar]
- Wegner SA, Ehrenberg PK, Chang G, Dayhoff DE, Sleeker AL, Michael NL. Genomic organization and functional characterization of the chemokine receptor CXCR4, a major entry co-receptor for human immunodeficiency virus type 1. Journal of Biological Chemistry. 1998;273(8):4754–4760. doi: 10.1074/jbc.273.8.4754. [DOI] [PubMed] [Google Scholar]
- WHO. Globocan 2012: Estimated cancer incidence, mortality and prevalence worldwide in 2012. 2012
- WHO. Breast cancer: Prevention and control. 2014a
- WHO. Cancer (Fact sheet No. 297) 2014b
- Woerner BM, Warrington NM, Kung AL, Perry A, Rubin JB. Widespread CXCR4 activation in astrocytomas revealed by phospho-CXCR4-specific antibodies. Cancer Research. 2005;65(24):11392–11399. doi: 10.1158/0008-5472.CAN-05-0847. [DOI] [PubMed] [Google Scholar]
- Wong D, Korz W. Translating an antagonist of chemokine receptor CXCR4: From bench to bedside. Clinical Cancer Research. 2008;14(24):7975–7980. doi: 10.1158/1078-0432.CCR-07-4846. [DOI] [PubMed] [Google Scholar]
- Wu B, Chien EYT, Mol CD, Fenalti G, Liu W, Katritch V, et al. Structures of the CXCR4 chemokine GPCR with small-molecule and cyclic peptide antagonists. Science. 2010;330(6007):1066–1071. doi: 10.1126/science.1194396. http://dx.doi.org/10.1126/science.1194396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiang ZL, Zeng ZC, Tang ZY, Fan J, Zhuang PY, Liang Y, et al. Chemokine receptor CXCR4 expression in hepatocellular carcinoma patients increases the risk of bone metastases and poor survival. BMC Cancer. 2009;9:176. doi: 10.1186/1471-2407-9-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu TP, Shen H, Liu LX, Shu YQ. The impact of chemokine receptor CXCR4 on breast cancer prognosis: A meta-analysis. Cancer Epidemiology. 2013;37(5):725–731. doi: 10.1016/j.canep.2013.04.017. [DOI] [PubMed] [Google Scholar]
- Xue B, Wu W, Huang K, Xie T, Xu X, Zhang H, et al. Stromal cell-derived factor-1 (SDF-1) enhances cells invasion by alphavbeta6 integrin-mediated signaling in ovarian cancer. Molecular and Cellular Biochemistry. 2013;380(1–2):177–184. doi: 10.1007/s11010-013-1671-1. [DOI] [PubMed] [Google Scholar]
- Yasumoto K, Koizumi K, Kawashima A, Saitoh Y, Arita Y, Shinohara K, et al. Role of the CXCL12/CXCR4 axis in peritoneal carcinomatosis of gastric cancer. Cancer Research. 2006;66(4):2181–2187. doi: 10.1158/0008-5472.CAN-05-3393. [DOI] [PubMed] [Google Scholar]
- Ying J, Xu Q, Zhang G, Liu B, Zhu L. The expression of CXCL12 and CXCR4 in gastric cancer and their correlation to lymph node metastasis. Medical Oncology. 2012;29(3):1716–1722. doi: 10.1007/s12032-011-9990-0. [DOI] [PubMed] [Google Scholar]
- Yu L, Cecil J, Peng SB, Schrementi J, Kovacevic S, Paul D, et al. Identification and expression of novel isoforms of human stromal cell-derived factor 1. Gene. 2006;374:174–179. doi: 10.1016/j.gene.2006.02.001. [DOI] [PubMed] [Google Scholar]
- Yu L, Hales CA. Effect of chemokine receptor CXCR4 on hypoxia-induced pulmonary hypertension and vascular remodeling in rats. Respiratory Research. 2011;12:21. doi: 10.1186/1465-9921-12-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabel BA, Agace WW, Campbell JJ, Heath HM, Parent D, Roberts AI, et al. Human G protein-coupled receptor GPR-9-6/CC chemokine receptor 9 is selectively expressed on intestinal homing T lymphocytes, mucosal lymphocytes, and thymocytes and is required for thymus-expressed chemokine-mediated chemotaxis. Journal of Experimental Medicine. 1999;190(9):1241–1256. doi: 10.1084/jem.190.9.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagzag D, Esencay M, Mendez O, Yee H, Smirnova I, Huang Y, et al. Hypoxia- and vascular endothelial growth factor-induced stromal cell-derived factor- 1alpha/CXCR4 expression in glioblastomas: One plausible explanation of Scherer’s structures. American Journal of Pathology. 2008;173(2):545–560. doi: 10.2353/ajpath.2008.071197. http://dx.doi.org/10.2353/ajpath.2008.071197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zagzag D, Krishnamachary B, Yee H, Okuyama H, Chiriboga L, Ali MA, et al. Stromal cell-derived factor-1alpha and CXCR4 expression in hemangioblastoma and clear cell-renal cell carcinoma: vonHippel-Lindau loss-of-function induces expression of a ligand and its receptor. Cancer Research. 2005;65(14):6178–6188. doi: 10.1158/0008-5472.CAN-04-4406. [DOI] [PubMed] [Google Scholar]
- Zagzag D, Lukyanov Y, Lan L, Ali MA, Esencay M, Mendez O, et al. Hypoxia-inducible factor 1 and VEGF upregulate CXCR4 in glioblastoma: Implications for angiogenesis and glioma cell invasion. Laboratory Investigation. 2006;86(12):1221–1232. doi: 10.1038/labinvest.3700482. [DOI] [PubMed] [Google Scholar]
- Zeelenberg IS, Ruuls-Van Stalle L, Roos E. The chemokine receptor CXCR4 is required for outgrowth of colon carcinoma micrometastases. Cancer Research. 2003;63(13):3833–3839. [PubMed] [Google Scholar]
- Zeng Z, Shi YX, Samudio IJ, Wang RY, Ling X, Frolova O, et al. Targeting the leukemia microenvironment by CXCR4 inhibition overcomes resistance to kinase inhibitors and chemotherapy in AML. Blood. 2009;113(24):6215–6224. doi: 10.1182/blood-2008-05-158311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X-X, Sun Z, Guo J, Wang Z, Wu C, Niu G, et al. Comparison of F-18-labeled CXCR4 antagonist peptides for PET imaging of CXCR4 expression. Molecular Imaging and Biology. 2013;15(6):758–767. doi: 10.1007/s11307-013-0640-0. http://dx.doi.org/10.1007/s11307-013-0640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang JM, Tian JH, Li TR, Guo HY, Shen L. Tc-99 m-AMD3100: A novel potential receptor-targeting radiopharmaceutical for tumor imaging. Chinese Chemical Letters. 2010;21(4):461–463. http://dx.doi.org/10.1016/j.cclet.2009.12.018. [Google Scholar]
- Zhang XF, Wang JF, Matczak E, Proper JA, Groopman JE. Janus kinase 2 is involved in stromal cell-derived factor-1alpha-induced tyrosine phosphorylation of focal adhesion proteins and migration of hematopoietic progenitor cells. Blood. 2001;97(11):3342–3348. doi: 10.1182/blood.v97.11.3342. [DOI] [PubMed] [Google Scholar]
- Zhong C, Wang J, Li B, Xiang H, Ultsch M, Coons M, et al. Development and preclinical characterization of a humanized antibody targeting CXCL12. Clinical Cancer Research. 2013;19(16):4433–4445. doi: 10.1158/1078-0432.CCR-13-0943. http://dx.doi.org/10.1158/1078-0432.ccr-13-0943. [DOI] [PubMed] [Google Scholar]
- Zlotnik A. New insights on the role ofCXCR4 in cancer metastasis. Journal of Pathology. 2008;215(3):211–213. doi: 10.1002/path.2350. [DOI] [PubMed] [Google Scholar]
- Zou YR, Kottmann AH, Kuroda M, Taniuchi I, Littman DR. Function of the chemokine receptor CXCR4 in haematopoiesis and in cerebellar development. Nature. 1998;393(6685):595–599. doi: 10.1038/31269. [DOI] [PubMed] [Google Scholar]