Abstract
Background
Loneliness is a contributing factor to various health problems in older adults, including complex chronic illness, functional decline, and increased risk of mortality.
Objectives
A pilot study was conducted to learn more about the prevalence of loneliness in rural older adults with chronic illness and how it affects their quality of life. The purposes of the data analysis reported here were twofold: to describe loneliness, chronic illness diagnoses, chronic illness control measures, prescription medication use, and quality of life in a sample of rural older adults; and to examine the relationships among these elements.
Methods
A convenience sample of 60 chronically ill older adults who were community dwelling and living in Appalachia was assessed during face-to-face interviews for loneliness and quality of life, using the University of California, Los Angeles (UCLA) Loneliness Scale (version 3) and the CASP-12 quality of life scale. Chronic illness diagnoses, chronic illness control measures, and medication use data were collected through review of participants’ electronic medical records.
Results
Overall mean loneliness scores indicated significant loneliness. Participants with a mood disorder such as anxiety or depression had the highest mean loneliness scores, followed by those with lung disease and those with heart disease. Furthermore, participants with mood disorders, lung disease, or heart disease had significantly higher loneliness scores than those without these conditions. Loneliness was significantly related to total number of chronic illnesses and use of benzodiazepines. Use of benzodiazepines, diuretics, nitrates, and bronchodilators were each associated with a lower quality of life.
Conclusions
Nurses should assess for loneliness as part of their comprehensive assessment of patients with chronic illness. Further research is needed to design and test interventions for loneliness.
Keywords: chronic illness, loneliness, older adult, quality of life, rural
The nursing literature has long recognized loneliness as a health priority. In 1955, Hildegard Peplau wrote about loneliness for this journal, calling it an “unbearable” condition and describing it as a psychological problem that results from deprivation of some social or emotional need.1 She also noted that being alone, often a chosen and useful state, isn’t the same as being lonely, which is not a chosen state; a distinction that is now well established. Historically, loneliness was first thought of as primarily a social phenomenon, and many of the instruments developed and used to measure it have been based on its social components. More recently, loneliness has been conceptualized in psychological terms, albeit at first as a construct embedded within depression. Currently the health and social sciences literature recognizes loneliness as a unique phenomenon, separate from depression, with emotional and social components.2, 3 This view of loneliness calls for a transdisciplinary approach, one that acknowledges that loneliness can be a significant biopsychosocial stressor and may adversely affect health.
LONELINESS AND CHRONIC ILLNESS IN OLDER ADULTS
Quantitative studies of loneliness in older adults have consistently reported significant correlations between loneliness and physical health problems. There is evidence that loneliness elicits a neuroimmunological stress response.4–6 It’s believed that through this and other mechanisms, loneliness may be linked to multiple chronic illnesses, including hypertension,7 metabolic syndrome,8 and in women, coronary heart disease.9 Lonely adults are more likely to have central (abdominal) obesity8 and to use tobacco,10 both contributing factors for many chronic illnesses. Moreover, loneliness appears to lower the likelihood of engaging in positive health practices such as exercise and relaxation.11 Psychological problems such as anxiety and depression have also been linked to loneliness in older adults.12
Loneliness has been linked to more frequent use of the health care system. In a study of community-dwelling older adults in Ireland, Molloy and colleagues found that as the frequency of loneliness increased, the odds of unplanned emergency hospitalization also increased.13 This finding held up even when potential confounders of depression, social participation, and social support were controlled for. In a Swedish study of frail elderly people, Jakobsson and colleagues found that high use of inpatient services was correlated with relatively high scores on loneliness and depression measures and relatively low scores on life satisfaction and social network measures.14 And in two recent analyses of data from a nationally representative study of older Americans, loneliness was reported as a significant independent predictor of functional decline and increased mortality, even after controlling for comorbidities and age.15, 16
Rurality and loneliness
Rural older adults experience many of the social, physical, and psychological factors associated with loneliness. Although research findings lack consensus, at least one study of older Chinese adults found that loneliness was significantly higher among rural residents than city dwellers.17 Poverty has also been linked to loneliness,10, 18 and according to the U.S. Department of Agriculture, in 2011 17% of people in nonmetro (rural) areas were living in poverty, compared with 14.6% of people in metro areas.19 Lower educational levels have been reported as predictive of loneliness,10 and there is evidence that people living in rural areas tend to have less education. One recent report found that nearly one-quarter of rural students don’t graduate from high school20; another report noted that the percentage of people who had attained a bachelor’s degree was 13% in rural areas, compared with a national average of 17%.21 In one study of rural older adults, the loss of a spouse was linked to emotional loneliness, while infrequent visits with siblings and impaired hearing were linked to social loneliness.22
Another study, exploring how rural older adults experience chronic illness, found that many do so with a sense of “quiet pride.”23 Participants valued self-reliance; sought support from family and community, especially religious community; and were reluctant to enter the health care system. These findings underscore how important it is for clinicians to address loneliness in this population.
THE PILOT STUDY
To learn more about loneliness and chronic illness in rural older adults, we conducted a pilot study. An earlier data analysis focused on the relationships between loneliness, depression, social support, and quality of life; those results have been published in the Journal of Psychology.24 This article reports on a subsequent data analysis, which had two aims: first, to describe loneliness, chronic illness diagnoses, chronic illness control measures, prescription medication use, and quality of life in chronically ill older adults living in Appalachia; and second, to examine the relationships among these elements.
We started with three hypotheses, as follows:
Hypothesis 1: Loneliness, chronic illness, and prescription medication use will be prevalent in a sample of older adults living in Appalachia.
Hypothesis 2: Chronic illness control indicators will not be within the recommended guidelines for good control in participants who are lonely.
Hypothesis 3: Participants who are lonely will have higher numbers of chronic illnesses, poorer chronic illness control, higher numbers of prescription medications, and lower quality of life.
Theoretical basis
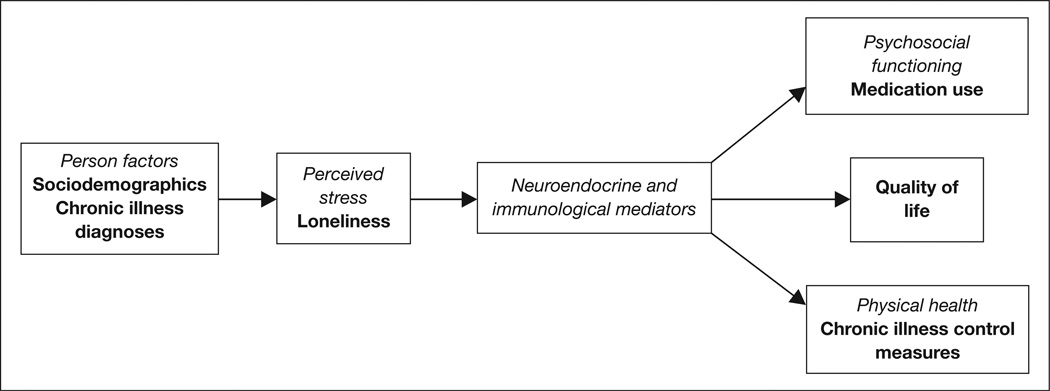
The theoretical framework for this study is the psychoneuroimmunology (PNI) paradigm, which is concerned with “the mechanisms of bidirectional communication between the neuroendocrine and immune systems” and may be used to guide relevant research.25 As Zeller and colleagues have stated, per this paradigm, the experience of a stressor can elicit neurologic and immune system responses that in turn can affect physical health, psychosocial functioning, and quality of life.25 For this study, loneliness was conceptualized as a biopsychosocial stressor that influences mind–body interactions. In accordance with the PNI paradigm, we posited that the stress of loneliness, in combination with socio-demographic and individual health-related factors, elicits a neuroimmunological response pattern that influences chronic illness, chronic illness control, and quality of life. For a model of the PNI framework integrated with the study variables, see Figure 1.
Figure 1.
The study variables integrated into the model of the psychoneuroimmunology (PNI) paradigm. This figure is based on the PNI model in McCain NL, et al. Adv Nursing Sci 2005;28(4):320–322. Bolded text = the variables measured in this study.
METHODS
Setting
The study was conducted in northern West Virginia, which lies entirely within the Appalachian region. Appalachia is geographically rural, and most counties have been designated by the Health Resources and Services Administration as medically underserved.26 For older adults, the rurality of Appalachia may limit opportunities for socialization, self-development, and access to health care, and might contribute to loneliness. The relationships among loneliness, chronic illness, chronic illness control, medication use, and quality of life are understudied in Appalachian samples.
Sample
This descriptive, cross-sectional study took place at a university family medical center (also referred to as “the clinic”). A convenience sample was recruited from a total clinic population of 1,900 older adults. We estimated that we needed a sample size of 60 to ensure that our findings would be reliable. Participants were recruited through advertisements in a local newspaper and through flyers and posters placed in the clinic waiting rooms and hallways. The posters and flyers listed the inclusion and exclusion criteria. Older adults who called about participating in the study were assessed regarding these criteria and were scheduled for an interview with a research team member for data collection. Data collection was completed between January 15 and March 31 of 2009. Adults who were 65 years of age or older, community dwelling, living in Appalachia, and living with chronic illness were eligible for inclusion. Those with dementia or psychotic illness requiring antipsychotic medication, as indicated on medical chart review, were excluded. Those who were grieving the loss of a spouse in the two years before the interviews were also excluded, to avoid the potential confounding of grief and emotional loneliness in this relatively small sample.27
Data collection included written surveys, which participants completed during their scheduled interview. Members of the research team were available to facilitate data collection and answer logistical questions about the surveys. All surveys were completed in full; no data were missing. Chronic illness diagnoses, chronic illness control indicators, and medications were obtained from medical chart reviews. The study was approved by the West Virginia University institutional review board.
Measurements
Sociodemographics
Data on age, gender, marital status, education level (highest attained), annual household income, employment status, and living situation were collected. Age was measured as years at the time of the interview. Gender was self-reported and dichotomous, categorized as male or female. Marital status was categorized as “never married,” “widowed,” “separated/divorced,” “married with spouse absent from home,” or “married with spouse living at home.” (“Widowed” was used to refer to both men and women whose spouses have died.) Education level was assessed categorically for completion of grade school, middle school, high school, some college, associate’s degree, bachelor’s degree, master’s degree, and doctoral degree. Annual household income was measured using $10,000 incremental categories, beginning with “less than or equal to $20,000” and ending with “greater than $100,000.” Employment status was categorized as “retired,” “working part-time,” “working full-time,” “working more than full-time,” or “unemployed.” Living situation was assessed using two variables, the number of people living in the home and their relationship to the participant.
Loneliness
The 20-item University of California, Los Angeles (UCLA) Loneliness Scale (version 3) was used to assess loneliness.28 It reflects a conceptualization of loneliness as a complex phenomenon with both emotional and social components. The original scale was developed by Russell and colleagues in 1978 and consisted of 20 items that were all worded in a negative way.29 A second, revised version was published in 1980, with 10 positively and 10 negatively worded items; but there were still problems with wording.30 The current version, version 3, appeared in 1996 and includes 11 positively worded and nine negatively worded items.28 All items can be answered using a Likert scale, with potential answers of “never,” “rarely,” “sometimes,” and “often”; each answer is assigned a point value ranging from 1 (never) to 4 (often). Possible total scores range from 20 to 80, with 20 indicating no loneliness and higher scores indicating greater loneliness. Scores over 40 are generally considered to indicate loneliness. The scale has high internal consistency (a Cronbach α of 0.89 to 0.94) and positive test-retest reliability (r = 0.73).28 For our study sample, the Cronbach α was 0.825.
Quality of life
The CASP-12 scale was used to assess quality of life. The CASP-12, which is derived from a longer version known as the CASP-19, conceptualizes quality of life in older adults under three domains: control and autonomy, self-realization, and pleasure (the acronym derives from the first letters of these domains).31 The scale consists of 12 questions that can be answered using a Likert scale, with potential answers of “never,” “rarely,” “sometimes,” and “often”; each answer is assigned a point value ranging from 0 (never) to 3 (often). Possible total scores range from 0 to 36, with higher scores indicating a higher quality of life. The CASP-12 had a Cronbach α reported as 0.67 during instrument development with older adults.31 For our study sample, the Cronbach α was 0.606.
Chronic illness
Diagnoses of hypertension, hyper-lipidemia, heart disease, arthritis, diabetes, lung disease, mood disorders, stroke, cancer (excluding skin cancer), and obesity (defined as a body mass index [BMI] equal to or greater than 30 kg/m2) were obtained through both patient self-report and medical chart review. The number of chronic illnesses was measured as a simple sum of the chronic illness diagnoses.
Chronic illness control
Laboratory test results were gathered from the electronic medical records. Laboratory studies that had been performed in the preceding 12 months were included in the data collection. For participants with diabetes, fasting glucose and glycated hemoglobin (HbA1c) levels were collected, when available, as a measure of diabetes control. The lipid profile was collected as a measure of hyperlipidemia control. Creatinine and glomerular filtration rate (GFR) were collected as measures of renal disease control. Blood pressure was taken during the interview as a measure of hypertension control. Resting heart rate was assessed during the interview as a measure of heart function. Kapoor and Heidenreich found that elevated resting heart rates were associated with increased mortality in people with both heart failure and preserved left ventricular function; they concluded that resting heart rate should be considered when assessing cardiovascular risk.32 BMI was calculated as a measure of obesity; this was felt to be important since obesity is a factor in many chronic illnesses.
Medications listed in the medical records were recorded by their medication classification as given in the 63rd edition of the Physicians’ Desk Reference.33
Data analysis
SPSS software version 20 was used for the data analysis. For all statistical analyses, significance was set at 0.05. To address the first of our two aims, univariate descriptive analysis was completed for sociodemographics, loneliness, chronic illness diagnoses, chronic illness control measures, prescription medication use, and quality of life. To address the second aim, initial comparisons were conducted to assess relationships among loneliness, chronic illness diagnoses, chronic illness control measures, prescription medication use, and quality of life. For significant correlations, mean comparisons of loneliness, chronic illness control measures, and quality of life were conducted for each diagnosis and medication classification.
RESULTS
Description of the sample
Sixty-four people volunteered to participate in the study during the three-month data collection period. Four were excluded because of a diagnosis of dementia. The final sample of 60 white older adults had a high mean UCLA Loneliness Scale score (mean, 49.05; SD, 4.77; range, 38–59). Fifty-eight of the 60 participants had scores of 41 or higher. This means that the prevalence rate of loneliness in our sample was 97%, as compared with a national prevalence rate of about 17%.10 Table 1 reports additional sociodemographic characteristics of the sample.
Table 1.
Description of the Sample (N = 60)a
| Variable | Category | n (%) |
|---|---|---|
| Gender | Female | 39 (65) |
| Male | 21 (35) | |
| Marital status | Married | 39 (65) |
| Married, spouse absent | 1 (2) | |
| Separated/divorced | 2 (3) | |
| Widowed | 17 (28) | |
| Never married | 1 (2) | |
| Education | Less than high school | 4 (7) |
| High school diploma | 26 (43) | |
| Some college | 12 (20) | |
| College degree and higher | 18 (30) | |
| Household income ($/year) |
1st quartile ($0–$20,000) | 14 (23) |
| 2nd quartile ($20,001–$30,000) | 16 (27) | |
| 3rd quartile ($30,001–$50,000) | 16 (27) | |
| 4th quartile ($50,001 and up) | 14 (23) | |
| Others in the home | Spouse | 39 (65) |
| Nobody, lives alone | 15 (25) | |
| Sibling, children, or grandchildren | 6 (10) | |
| Employment status | Retired | 52 (87) |
| Working part-time | 4 (7) | |
| Working full-time | 3 (5) | |
| Working more than full-time | 1 (2) | |
Mean age of the sample was 75.2 years (SD, 6.42).
Note: Some values may not sum to 100 because of rounding.
Adapted from Theeke LA, et al. Loneliness, depression, social support, and quality of life in older chronically ill Appalachians. J Psychol 2012;146(1–2):155-71. Adapted by permission of Taylor and Francis.
Chronic illness diagnoses were prevalent: 92% of participants had hypertension, 75% had hyperlipidemia, 68% had heart disease, 53% had arthritis, 37% had diabetes, 35% had lung disease, 33% had mood disorders, 18% had a diagnosis of stroke, 17% had a diagnosis of cancer (excluding skin cancer), and 40% were obese. Participants averaged about four chronic illness diagnoses (SD, 1.75; range, 1–8) and took an average of 7.3 prescription medications (SD, 3.88; range, 0–17). Yet the sample’s mean quality of life score was 25.3 (SD, 4.77; range, 0–36), indicating that participants ranked themselves as having a moderate quality of life. These results support hypothesis 1: loneliness, chronic illness, and prescription medication use were prevalent.
Mean values for the chronic illness control measures are reported in Table 2. Means for HbA1c, fasting glucose, systolic blood pressure, GFR, and BMI were not within the normal ranges for these measures. Even when correcting for age for each individual, GFR values remained below the normal range; indeed, not one GFR value was over 60 mL/min/1.73 m2. These results partially support hypothesis 2: chronic illness control indicators often were not within the recommended guidelines for good control.
Table 2.
Mean Values of Chronic Illness Control Indicators in the Sample
| Control Measure | Mean (SD) | Sample Range | Normal Range | Conclusion |
|---|---|---|---|---|
| HbA1c, % | 7.2 (2.18) | 5.7–16 | ≤ 7 | Elevated |
| Fasting glucose, mg/dL | 111.4 (15.65) | 88–171 | < 100 | Elevated |
| Creatinine, mg/dL | 0.9 (0.27) | 0.54–2.32 | 0.60–1 | Normal |
| GFR, mL/min/1.73 m2 | 56 (6.58) | 27–60 | ≥ 60 | Decreased |
| SBP, mmHg | 134 (17.19) | 102–201 | ≤ 120 | Elevated |
| DBP, mmHg | 74 (11.6) | 44–98 | ≤ 80 | Normal |
| BMI, kg/m2 | 30.5 (8.64) | 14–78 | 18.5–24.9 | Elevated |
| Total cholesterol, mg/dL | 181 (47.3) | 108–333 | ≤ 200 | Normal |
| Triglycerides, mg/dL | 136 (81.56) | 34–568 | ≤ 170 | Normal |
| LDL, mg/dL | 100 (46.4) | 80–279 | ≤ 130 | Normal |
| HDL, mg/dL | 48 (13.5) | 28–100 | 30–75 | Normal |
BMI = body mass index; DBP = diastolic blood pressure; GFR = glomerular filtration rate; HDL = high-density lipoprotein cholesterol; HbA1c = glycated hemoglobin; LDL = low-density lipoprotein cholesterol; SBP = systolic blood pressure; SD = standard deviation.
Note: HbA1c analysis included only 20 participants; the other 40 participants did not have these data available in their medical records.
Relationships among loneliness, quality of life, and chronic illness
Mean differences in loneliness and quality of life scores based on chronic illness diagnosis are reported in Table 3. Participants with a diagnosed mood disorder such as anxiety or depression had the highest loneliness scores (mean, 51.15; SD, 4.13) followed by participants with lung disease (mean, 51.05; SD, 4.27) and those with heart disease (mean, 50.15; SD, 4.10). Participants with a diagnosis of stroke had the lowest overall quality of life scores (mean, 22.68; SD, 6.06). Participants who were obese had significantly lower quality of life scores than those who were not obese. Those with mood disorders, lung disease, or heart disease had significantly higher loneliness scores than those without these illnesses.
Table 3.
Mean Comparisons of Loneliness and Quality of Life Scores Based on Chronic Illness Diagnosis
| Variable | n | UCLA, mean |
SD | t | P | QOL, mean |
SD | t | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Hypertension | Yes | 55 | 49.00 | 4.44 | 0.267 | 0.79 | 25.14 | 4.83 | 1.01 | 0.31 |
| No | 5 | 49.60 | 8.26 | 27.40 | 3.78 | |||||
| Hyperlipidemia | Yes | 45 | 49.64 | 4.11 | 1.69 | 0.1 | 26.73 | 5.03 | 1.33 | 0.19 |
| No | 15 | 47.26 | 6.17 | 24.86 | 3.71 | |||||
| Heart disease | Yes | 41 | 50.15 | 4.10 | 2.75 | 0.01a | 25.55 | 4.99 | 0.25 | 0.8 |
| No | 19 | 46.68 | 5.34 | 25.22 | 4.38 | |||||
| Arthritis | Yes | 32 | 48.79 | 4.12 | 0.46 | 0.65 | 24.31 | 5.42 | 1.79 | 0.08 |
| No | 28 | 49.36 | 5.47 | 26.48 | 3.67 | |||||
| Diabetes | Yes | 22 | 49.90 | 4.38 | 1.06 | 0.29 | 25.57 | 4.43 | 0.51 | 0.61 |
| No | 38 | 48.55 | 4.96 | 24.91 | 5.39 | |||||
| Lung disease | Yes | 21 | 51.05 | 4.27 | 2.48 | 0.02b | 26.17 | 3.99 | 1.90 | 0.06 |
| No | 39 | 47.97 | 4.72 | 23.76 | 5.74 | |||||
| Mood disorder | Yes | 20 | 51.15 | 4.13 | 2.52 | 0.02b | 23.90 | 5.82 | 1.67 | 0.1 |
| No | 40 | 50.05 | 4.78 | 26.04 | 4.05 | |||||
| Stroke | Yes | 11 | 49.90 | 5.20 | 0.66 | 0.51 | 22.68 | 6.06 | 2.09 | 0.04b |
| No | 49 | 51.00 | 4.57 | 25.92 | 4.29 | |||||
| Cancer (excluding skin) | Yes | 10 | 49.80 | 5.26 | 0.54 | 0.59 | 23.65 | 4.89 | 1.22 | 0.23 |
| No | 50 | 48.90 | 5.58 | 25.66 | 4.72 | |||||
| Obesity (BMI ≥ 30) | Yes | 24 | 49.21 | 5.53 | 0.21 | 0.83 | 23.89 | 5.98 | 1.93 | <0.01a |
| No | 36 | 48.94 | 4.27 | 26.27 | 3.54 | |||||
BMI = body mass index; QOL = quality of life; SD = standard deviation; t = t-test values; UCLA = University of California, Los Angeles Loneliness Scale (version 3).
Significant at the 0.01 level.
Significant at the 0.05 level.
Note: Equal variances are assumed.
Table 4 reports the correlation coefficients for loneliness, quality of life, chronic illness control measures, and total numbers of chronic illnesses and prescription medications (go to http://links.lww.com/AJN/A48). The total number of chronic illnesses correlated positively with loneliness (r = 0.273, P = 0.04) and negatively with quality of life (r = −0.376, P = 0.01). Loneliness did not correlate with poorer chronic illness control, total numbers of prescription medications, or quality of life in this sample. Although being widowed has been linked to loneliness,34 we found no significant differences in loneliness or chronic illness control measures based on marital status.
Mean comparisons of loneliness and quality of life scores associated with the use of specific medications are reported in Table 5. Benzodiazepine use correlated significantly with higher loneliness scores (r = 0.272; P = 0.04) and lower quality of life scores (r = −0.445; P < 0.01). Participants with lung disease that required bronchodilator use also reported significantly lower quality of life scores. Use of diuretics and nitrates were also associated with a lower quality of life. These results provide partial support for hypothesis 3: participants with loneliness had higher numbers of chronic illnesses, higher numbers of prescription medications, and lower quality of life, although they did not have poorer chronic illness control.
Table 5.
Mean Comparisons of Loneliness and Quality of Life Scores Based on Medication Use
| Variable | n | UCLA, mean |
SD | t | P | QOL, mean |
SD | t | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Lipid-lowering agent | Yes | 28 | 52.64 | 4.31 | 2.58 | 0.01a | 24.80 | 4.64 | 0.69 | 0.49 |
| No | 29 | 49.62 | 4.45 | 25.68 | 5.04 | |||||
| Narcotic | Yes | 15 | 51.80 | 4.92 | 0.65 | 0.52 | 24.60 | 4.62 | 0.60 | 0.55 |
| No | 44 | 50.89 | 3.98 | 25.46 | 4.85 | |||||
| Benzodiazepine | Yes | 5 | 54.40 | 3.36 | 1.68 | 0.09 | 20.60 | 7.43 | 2.65 | 0.01 a |
| No | 53 | 50.90 | 4.51 | 26.02 | 4.04 | |||||
| Diuretic | Yes | 9 | 52.67 | 3.77 | 0.97 | 0.33 | 22.22 | 6.20 | 2.20 | 0.03 b |
| No | 50 | 51.06 | 4.65 | 25.93 | 4.34 | |||||
| Nitrate | Yes | 11 | 50.81 | 3.89 | 0.39 | 0.67 | 22.59 | 3.98 | 2.19 | 0.03 b |
| No | 48 | 51.41 | 4.70 | 26.00 | 6.98 | |||||
| Anticoagulant | Yes | 13 | 54.07 | 3.22 | 2.89 | < 0.01a | 26.57 | 4.99 | 1.10 | 0.27 |
| No | 46 | 50.15 | 4.56 | 24.91 | 3.93 | |||||
| Calcium supplement | Yes | 7 | 47.71 | 3.40 | 2.14 | 0.04 b | 26.14 | 1.58 | 0.48 | 0.63 |
| No | 53 | 51.60 | 4.63 | 25.21 | 0.67 | |||||
| Bronchodilator MDI | Yes | 7 | 53.86 | 3.62 | 1.66 | 0.1 | 20.28 | 7.01 | 3.19 | < 0.01 a |
| No | 53 | 50.79 | 4.68 | 25.99 | 4.03 | |||||
MDI = multidose inhaler; QOL = quality of life; SD = standard deviation; t = t-test values; UCLA = University of California, Los Angeles Loneliness Scale (version 3).
Significant at the 0.01 level.
Significant at the 0.05 level.
Note: The number of participants does not sum to 60 in some cases because of missing data.
DISCUSSION
These findings demonstrate that loneliness is a significant problem for chronically ill rural older adults. The descriptive analysis indicates that 97% of the sample participants were experiencing significant loneliness, a prevalence rate much higher than that reported by other studies. For example, in a study conducted in Great Britain, Victor and Bowling found that 9% of older adults reported severe loneliness and 30% reported sometimes being lonely.35 In another British study, Shankar and colleagues found that only 2% of older adults reported “feeling lonely all the time,” and only 7% of older adults reported maximum scores for social isolation.36 It appears that older adults in Appalachia experience many of the psychosocial and behavioral factors associated with loneliness (such as widowhood, numerous comorbidities, and self-reported poorer health37), and therefore may be at increased risk for loneliness. The Appalachian region is known to have marked disparities in health care resources, costs, and access compared with other U.S. regions.38 Having a better understanding of how loneliness interacts with the culture of Appalachia, as well as with health behaviors and the development of chronic illness, could make a significant contribution to improving health in this region.
Although we did not find that loneliness correlated with higher blood pressure, BMI, or HbA1c levels, the literature reports associations between loneliness and hypertension39 and metabolic syndrome8 in older adult populations. Furthermore, loneliness has been associated with higher total peripheral resistance in young adults,40 and it may be through this mechanism that loneliness contributes to the development of hypertension. There is also evidence of a link between loneliness and higher food consumption,41 which might partially explain the association one study found between loneliness and central obesity.8
We found that higher loneliness scores were associated with higher numbers of chronic illnesses and lower quality of life scores, and this finding is similar to those from data analyses of larger samples of older adults.10, 37,42,43 Hypothesis 3 was only partially supported, because in our sample loneliness did not correlate with poorer chronic illness control.
Nursing implications
This study identified a population that is at risk for poor health outcomes associated with loneliness: rural older adults who take several medications and have multiple comorbidities, including heart disease, lung disease, mood disorders, stroke, and obesity. Assessment of loneliness in this and other high-risk populations is vital. Assessing and addressing loneliness—especially in older adults with these specific conditions—may lead to changes in health practices that facilitate improved outcomes.
Studies of loneliness and physical health outcomes in other geographic areas would enhance our understanding of how older adults experience loneliness in urban versus rural settings, and might help identify new populations in need of intervention. Studies of how nurses might use mobile technologies to identify and diminish loneliness could expand the capabilities of nursing, particularly in rural and other areas with access disparities. And the advent of patient-centered medical homes might mean that nurse case managers have more frequent contact with chronically ill older adults, yielding more assessment opportunities.
It’s important for all nurses to be proactive about assessing for loneliness. One simple tool, the Three-Item Loneliness Scale—which is derived from the second, revised version of the 20-item UCLA Loneliness Scale—can be readily used in routine patient assessments.44 The three-item scale asks, “How often do you feel that you lack companionship?” “How often do you feel left out?” and “How often do you feel isolated from others?” Each item can be answered with “hardly ever,” “some of the time,” or “often”; each answer is assigned a point value ranging from 1(hardly ever) to 3 (often). Possible total scores range from 3 to 9, with higher scores indicating greater loneliness. This scale reports a Cronbach α of 0.72,44 comparable to values reported for the 20-item version; and it can be administered in far less time, making it useful in busy clinical settings.
Nurses also need to think innovatively and help to develop interventions for loneliness that can be used in clinical practice in various settings, including home care. Recent intervention studies indicate that it’s important to address both emotional and social components of loneliness. Interventions that have demonstrated effectiveness in diminishing loneliness in older adults include programs such as community-based group meetings aimed at social integration.45 A recent meta-analysis of intervention studies indicated that interventions aimed at maladaptive social cognition processes related to loneliness may be the most successful.46
With colleagues, we have recently completed a study that evaluates the effectiveness of an innovative intervention designed specifically to address loneliness. The intervention is based on principles of cognitive restructuring and story theory,47 and is delivered in a group setting. (Story theory offers a structure for using story in nursing research and practice. It emphasizes the use of intentional nurse–patient dialogue to help the patient find meaning in a health challenge and move toward resolution.) The preliminary results indicate that, compared with controls, participants assigned to the story-sharing group demonstrated significant decreases in loneliness and systolic blood pressure.48
In another meta-analysis, Yarcheski and colleagues found that loneliness had “a powerful negative influence on the practice of positive health behaviors,”11 which could have adverse long-term consequences. It stands to reason that by decreasing loneliness, nurses can help older adults to improve their practice of positive health behaviors, which in turn could improve chronic illness outcomes. Social determinants of health, such as rurality, poverty, low educational level, widowhood, and social isolation, compound loneliness and may relate to poor health outcomes in patients with chronic illness.49 It’s important for nurses to plan interventions that increase patients’ opportunities for socialization, self-development, and access to health care. An enhanced understanding of loneliness among nurses, followed by collaborative and interdisciplinary measures aimed at helping older adults address their loneliness, could lead to improved emotional and physical health outcomes.
Loneliness is treatable. There are many opportunities for nurses to be involved in developing multifaceted interventions to target loneliness. As this occurs, it’s more likely that loneliness will become a reimbursable diagnosis, prompting more providers to assess for loneliness and pursue treatment plans. Future longitudinal studies should evaluate the efficacy of interventions for loneliness. Further investigation into the association between loneliness and chronic illnesses and their outcomes, as well as the effects on the health care system, is also warranted.
Limitations
The cross-sectional design of this study eliminates the possibility of establishing causal relationships between variables. The generalizability of the study findings is limited by the relative demographic homogeneity of our sample. Since recent widows and widowers were excluded, the results cannot be generalized to people whose spouses recently died. Because data were gathered on a small convenience sample using self-report methods for psychosocial variables, there is the possibility of sample bias or self-report errors.
The method of data collection was also a limitation. First, a measure of pain control as an indicator of arthritis control was not readily available in the medical record. This was a limitation because there is evidence that people with rheumatic diseases, particularly fibromyalgia, may experience more loneliness.50 The use of chart reviews for clinical laboratory data also meant that HbA1c values were only available for 20 of the 60 participants; this may have influenced the significance of some findings. Prospective studies with larger samples and employing primary data collection of biophysical measures of chronic illness are needed.
CONCLUSIONS
Our findings demonstrate that loneliness is a significant problem for chronically ill rural older adults, particularly those with mood disorders or with heart or lung disease. Currently there are no clinical practice guidelines for loneliness, and clinicians don’t routinely assess for loneliness using validated and reliable instruments. Loneliness has been strongly associated with depression and anxiety12; and more than 50 years of evidence indicates significant relationships between loneliness and various measures of physical health. It’s time for national organizations to consider recommending routine screening for loneliness in all older adults. This would increase awareness of loneliness as a clinical problem, and prompt intervention and practice guideline development.
Assessing loneliness in older adults may be particularly important for those with known mood disorders. Since participants of this study reported relatively high quality of life scores in the face of loneliness, poverty, and prevalent chronic illness, it may be that quality of life measures alone can give providers a false sense that “things are OK,” resulting in a missed opportunity for intervention for loneliness. Nurses who understand the health effects of loneliness and address loneliness in care planning may be able to prevent significant adverse physical and psychological outcomes for patients.
Acknowledgments
This study was funded by unrestricted educational grants from the West Virginia University School of Nursing Research Fund and the Robert Wood Johnson Foundation Scholars Program.
Footnotes
The authors and planners have disclosed no potential conflicts of interest, financial or otherwise.
For 66 additional continuing nursing education articles on research topics, go to www.nursingcenter.com/ce
REFERENCES
- 1.Peplau HE. Loneliness. Am J Nurs. 1955;55(12):1476–1481. [PubMed] [Google Scholar]
- 2.Cacioppo JT, et al. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25(2):453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.van Baarsen B, et al. Lonely but not alone: emotional isolation and social isolation as two distinct dimensions of loneliness in older people. Educ Psychol Meas. 2001;61(1):119–135. [Google Scholar]
- 4.Cacioppo JT, et al. Loneliness and health: potential mechanisms. Psychosom Med. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Cole SW, et al. Social regulation of gene expression in human leukocytes. Genome Biol. 2007;8(9):R189. doi: 10.1186/gb-2007-8-9-r189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doane LD, Adam EK. Loneliness and cortisol: momentary, day-to-day, and trait associations. Psychoneuroendocrinology. 2010;35(3):430–441. doi: 10.1016/j.psyneuen.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawkley LC, et al. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21(1):152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- 8.Whisman MA. Loneliness and the metabolic syndrome in a population-based sample of middle-aged and older adults. Health Psychol. 2010;29(5):550–554. doi: 10.1037/a0020760. [DOI] [PubMed] [Google Scholar]
- 9.Thurston RC, Kubzansky LD. Women, loneliness, and incident coronary heart disease. Psychosom Med. 2009;71(8):836–842. doi: 10.1097/PSY.0b013e3181b40efc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Theeke LA. Sociodemographic and health-related risks for loneliness and outcome differences by loneliness status in a sample of U.S. older adults. Res Gerontol Nurs. 2010;3(2):113–125. doi: 10.3928/19404921-20091103-99. [DOI] [PubMed] [Google Scholar]
- 11.Yarcheski A, et al. A meta-analysis of predictors of positive health practices. J Nurs Scholarsh. 2004;36(2):102–108. doi: 10.1111/j.1547-5069.2004.04021.x. [DOI] [PubMed] [Google Scholar]
- 12.Barg FK, et al. A mixed-methods approach to understanding loneliness and depression in older adults. J Gerontol B Psychol Sci Soc Sci. 2006;61(6):S329–S339. doi: 10.1093/geronb/61.6.s329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Molloy GJ, et al. Loneliness and emergency and planned hospitalizations in a community sample of older adults. J Am Geriatr Soc. 2010;58(8):1538–1541. doi: 10.1111/j.1532-5415.2010.02960.x. [DOI] [PubMed] [Google Scholar]
- 14.Jakobsson U, et al. Psychosocial perspectives on health care utilization among frail elderly people: an explorative study. Arch Gerontol Geriatr. 2011;52(3):290–294. doi: 10.1016/j.archger.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 15.Luo Y, et al. Loneliness, health, and mortality in old age: a national longitudinal study. Soc Sci Med. 2012;74(6):907–914. doi: 10.1016/j.socscimed.2011.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perissinotto CM, et al. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang K, Victor CR. The prevalence of and risk factors for loneliness among older people in China. Ageing Soc. 2008;28(3):305–327. [Google Scholar]
- 18.Mullins LC, et al. Social determinants of loneliness among older Americans. Genet Soc Gen Psychol Monogr. 1996;122(4):453–473. [PubMed] [Google Scholar]
- 19.Kusmin L. Rural America at a glance, 2012 edition. Washington, DC: United States Department of Agriculture, Economic Research Service; 2012. Dec, Economic brief no. 21; http://www.ers.usda.gov/publications/eb-economic-brief/eb21.aspx#.UbD2HUDVA8V. [Google Scholar]
- 20.Strange M, et al. Why rural matters 2011-12: the condition of rural education in the 50 states. A report of the Rural School and Community Trust policy program. Washington, DC: Rural School and Community Trust; 2012. Jan, http://files.ruraledu.org/wrm2011-12/WRM2011-12.pdf. [Google Scholar]
- 21.Provasnik S, et al. Status of education in rural America. Washington, DC: U.S. Department of Education, Institute of Education Sciences, National Center for Education Statistics; 2007. Jul, NCES 2007-040. http://nces.ed.gov/pubs2007/2007040.pdf. [Google Scholar]
- 22.Dugan E, Kivett VR. The importance of emotional and social isolation to loneliness among very old rural adults. Gerontologist. 1994;34(3):340–346. doi: 10.1093/geront/34.3.340. [DOI] [PubMed] [Google Scholar]
- 23.Davis R, Magilvy JK. Quiet pride: the experience of chronic illness by rural older adults. J Nurs Scholarsh. 2000;32(4):385–390. doi: 10.1111/j.1547-5069.2000.00385.x. [DOI] [PubMed] [Google Scholar]
- 24.Theeke LA, et al. Loneliness, depression, social support, and quality of life in older chronically ill Appalachians. J Psychol. 2012;146(1–2):155–171. doi: 10.1080/00223980.2011.609571. [DOI] [PubMed] [Google Scholar]
- 25.Zeller JM, et al. Psychoneuroimmunology: an emerging framework for nursing research. J Adv Nurs. 1996;23(4):657–664. doi: 10.1111/j.1365-2648.1996.tb00034.x. [DOI] [PubMed] [Google Scholar]
- 26.Health Resources and Services Administration. Medically underserved areas/populations: guidelines for MUA and MUP designation; U.S. Department of Health and Human Services; http://www.hrsa.gov/shortage/mua. [Google Scholar]
- 27.Stroebe W, et al. The role of loneliness and social support in adjustment to loss: a test of attachment versus stress theory. J Pers Soc Psychol. 1996;70(6):1241–1249. doi: 10.1037//0022-3514.70.6.1241. [DOI] [PubMed] [Google Scholar]
- 28.Russell DW. UCLA Loneliness Scale (Version 3): reliability, validity, and factor structure. J Pers Assess. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- 29.Russell D, et al. Developing a measure of loneliness. J Pers Assess. 1978;42(3):290–294. doi: 10.1207/s15327752jpa4203_11. [DOI] [PubMed] [Google Scholar]
- 30.Russell D, et al. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. J Pers Soc Psychol. 1980;39(3):472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- 31.Wiggins RD, et al. The evaluation of a self-enumerated scale of quality of life (CASP-19) in the context of research on ageing: a combination of exploratory and confirmatory approaches. Soc Indic Res. 2008;89(1):61–77. [Google Scholar]
- 32.Kapoor JR, Heidenreich PA. Heart rate predicts mortality in patients with heart failure and preserved systolic function. J Card Fail. 2010;16(10):806–811. doi: 10.1016/j.cardfail.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 33.PDR Staff (COR), editor. Physicians’ desk reference: PDR. 63rd ed. New York: Thomson Reuters; 2008. [Google Scholar]
- 34.Ben-Zur H. Loneliness, optimism, and well-being among married, divorced, and widowed individuals. J Psychol. 2012;146(1–2):23–36. doi: 10.1080/00223980.2010.548414. [DOI] [PubMed] [Google Scholar]
- 35.Victor CR, Bowling A. A longitudinal analysis of loneliness among older people in Great Britain. J Psychol. 2012;146(3):313–331. doi: 10.1080/00223980.2011.609572. [DOI] [PubMed] [Google Scholar]
- 36.Shankar A, et al. Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol. 2011;30(4):377–385. doi: 10.1037/a0022826. [DOI] [PubMed] [Google Scholar]
- 37.Theeke LA. Predictors of loneliness in U.S. adults over age sixty-five. Arch Psychiatr Nurs. 2009;23(5):387–396. doi: 10.1016/j.apnu.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 38.Lane NM, et al. Health care costs and access disparities in Appalachia [executive summary] Chapel Hill, NC: PDA, Inc: Cecil B. Sheps Center for Health Services Research, University of North Carolina—Chapel Hill; 2012. http://www.arc.gov/assets/research_reports/HealthCareDisparitiesTableof-ContentsandExecutiveSummary.pdf. [Google Scholar]
- 39.Momtaz YA, et al. Loneliness as a risk factor for hypertension in later life. J Aging Health. 2012;24(4):696–710. doi: 10.1177/0898264311431305. [DOI] [PubMed] [Google Scholar]
- 40.Hawkley LC, et al. Loneliness in everyday life: cardiovascular activity, psychosocial context, and health behaviors. J Pers Soc Psychol. 2003;85(1):105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- 41.Rotenberg KJ, Flood D. Loneliness, dysphoria, dietary restraint, and eating behavior. Int J Eat Disord. 1999;25(1):55–64. doi: 10.1002/(sici)1098-108x(199901)25:1<55::aid-eat7>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 42.Chalise HN, et al. Correlates of loneliness among older Newar adults in Nepal. Nippon Koshu Eisei Zasshi (Japanese Journal of Public Health) 2007;54(7):427–433. [PubMed] [Google Scholar]
- 43.Ekwall AK, et al. Loneliness as a predictor of quality of life among older caregivers. J Adv Nurs. 2005;49(1):23–32. doi: 10.1111/j.1365-2648.2004.03260.x. [DOI] [PubMed] [Google Scholar]
- 44.Hughes ME, et al. A short scale for measuring loneliness in large surveys: results from two population-based studies. Res Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saito T, et al. Effects of a program to prevent social isolation on loneliness, depression, and subjective well-being of older adults: a randomized trial among older migrants in Japan. Arch Gerontol Geriatr. 2012;55(3):539–547. doi: 10.1016/j.archger.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 46.Masi CM, et al. A meta-analysis of interventions to reduce loneliness. Pers Soc Psychol Rev. 2011;15(3):219–266. doi: 10.1177/1088868310377394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liehr PR, Smith MJ. Story theory. In: Smith MJ, Liehr PR, editors. Middle range theory for nursing. 2nd ed. New York: Springer Publishing Company; 2008. pp. 205–224. [Google Scholar]
- 48.Theeke LA. Story-sharing to diminish loneliness and its sequelae in chronically ill older adults [poster] Washington, DC: 2011. [Google Scholar]
- 49.Fokkema T, et al. Cross-national differences in older adult loneliness. J Psychol. 2012;146(1–2):201–228. doi: 10.1080/00223980.2011.631612. [DOI] [PubMed] [Google Scholar]
- 50.Kool MB, Geenen R. Loneliness in patients with rheumatic diseases: the significance of invalidation and lack of social support. J Psychol. 2012;146(1–2):229–241. doi: 10.1080/00223980.2011.606434. [DOI] [PubMed] [Google Scholar]