Abstract
AIM: To investigate the diagnostic accuracy of the mean platelet volume and platelet distribution width in acute appendicitis.
METHODS: This retrospective, case-controlled study compared 295 patients with acute appendicitis (Group I), 100 patients with other intra-abdominal infections (Group II), and 100 healthy individuals (Group III) between January 2012 and January 2013. The age, gender, and white blood cell count, neutrophil percentage, mean platelet volume, and platelet distribution width values from blood samples were compared among the groups. Statistical analyses were performed using SPSS for Windows 21.0 software. In addition, the sensitivity, specificity, positive and negative predictive values and likelihood ratios, and diagnostic accuracy were calculated.
RESULTS: The mean ages of patients were 29.9 ± 12.0 years for Group I, 31.5 ± 14.0 years for Group II, and 30.4 ± 13.0 years for Group III. Demographic features such as age and gender were not significantly different among the groups. White blood cell count, neutrophil percentage and platelet distribution width were significantly higher in Group I compared to groups II and III (P < 0.05). Diagnostically, the sensitivity, specificity and diagnostic accuracy were 73.1%, 94.0%, and 78% for white blood cell count, 70.0%, 96.0%, and 76.0% for neutrophil percentage, 29.5%, 49.0%, and 34.0% for mean platelet volume, and 97.1%, 93.0%, and 96.0% for platelet distribution width, respectively. The highest diagnostic accuracy detected was for platelet distribution width between Group I and Group III (P < 0.01).
CONCLUSION: Platelet distribution width analysis can be used for diagnosis of acute appendicitis without requiring additional tests, thus reducing the cost and loss of time.
Keywords: Appendicitis, Diagnosis, Platelet function test, Platelet distribution width
Core tip: The diagnosis of acute appendicitis can be difficult and confusing. A rapid and accurate diagnosis is important because of potential complications, therefore, new biomarkers for diagnosis are needed. This study investigated the diagnostic accuracy of indicators of platelet activation, namely mean platelet volume and platelet distribution width, in acute appendicitis patients. Results shows that platelet distribution width analysis can be used for diagnosis of acute appendicitis without requiring additional tests. Therefore, it reduces the cost and loss of time.
INTRODUCTION
Acute appendicitis (AA) is among the most common urgent abdominal surgical conditions worldwide[1,2]. The people in Western society have an approximately 8% possibility of having AA during their lifetime[3]. Whereas the diagnosis of AA is usually established clinically, the symptoms and findings may not always typical, in which case the establishment of diagnosis becomes difficult[4,5]. Rapid and accurate diagnosis is important because extension of the period between the initiation of the symptoms and start of the surgical procedure increases the risk for appendiceal perforation, thereby potentially resulting in sepsis and even death[6]. In addition, the ratio of patients undergoing appendectomy with a normal histopathologic investigation result (negative appendectomy) ranges between 5% and 42%. The morbidity of these patients who are operated on despite the absence of AA is thus increased[7,8]. The rate of clinical diagnosis of AA is approximately 85%[1]. Although current advanced imaging methods such as ultrasonography, computed tomography and magnetic resonance imaging are promising, they are not adequate. Therefore, novel methods that differentiate AA from nonspecific abdominal pain and reduce the rate of negative appendectomy are needed. Such methods should be inexpensive and convenient, with results obtained in a short time.
Recent studies have investigated the diagnostic accuracy of inflammatory markers[9,10]. Mean platelet volume (MPV) and platelet distribution width (PDW) are presented in the complete blood cell count, which is routinely used in emergency departments. They are the indicators of platelet activation. The size of the platelet is correlated with the activity and the function of the platelet; larger platelets are more active than small ones. Thus, MPV may be used as a biomarker in myocardial infarction, diabetes mellitus, inflammatory disorders, sepsis-like conditions, myeloproliferative diseases, massive hemorrhage, leukemia, vasculitis and post-splenectomy conditions[11,12]. Platelet distribution width is an indicator of variation in platelet size, which can be a sign of active platelet release. Studies have demonstrated that in addition to MPV, PDW is also altered compared to healthy subjects in several conditions[13,14].
There are very few studies investigating the diagnostic accuracy of platelet function parameters in cases of AA. We present the first case-controlled study investigating the diagnostic significance of platelet parameters, including MPV and PDW, in AA.
MATERIALS AND METHODS
Participants
The records of 295 adult patients, aged between 16 and 94 years, who underwent appendectomy (Group I), 100 patients with other intra-abdominal infections (Group II), and 100 healthy individuals (Group III) were retrospectively investigated between January 2012 and January 2013. The groups were compared by age, gender and routine tests of complete blood count. Group I was comprised of patients diagnosed with AA based on the analysis of at least two samples performed by the pathologist.
Patients were excluded from the study for: < 15 years of age, having acute or chronic infectious disease, comorbid conditions (cardiac, respiratory, renal, endocrinal, and vascular disease, cancer, etc.), hematologic disease and blood transfusion within the last year for any reason, using ongoing medication (analgesics, oral contraceptives, antimetabolites, etc.), having a histopathologically normal appendix following appendectomy.
There were two control groups. The first of these, Group II did not have AA but they had intra-abdominal infections that depended on causes such as acute cholecystitis, pelvic inflammatory disease, and mesenteric lymphadenitis. Group III was comprised of healthy individuals, including people who came for health control and they did not have acute or chronic disease. The control groups were selected from among people of similar age and gender to AA patients. There was no history of drug use or blood transfusion in any of the patients.
Test methods
All blood samples were obtained from the venous system and stored in tubes containing EDTA and assayed automatically using internationally certified devices. The reference values were 4.5 × 109/μL-10.8 × 109/μL for white blood cell count (WBC), 40%-70% for neutrophils, 7.2-11.0 fL for MPV and 10%-18% for PDW. All results were approved by an independent biochemistry expert who was blind to the patients’ histories. Extreme results were repeated again. The results of blood samples were approved in < 10 min.
Statistical analysis
Statistical analyses were performed using SPSS for Windows 21.0 software (IBM Corp., Armonk, NY, United States). The demographic and clinical properties of patients are expressed using mean ± SD, median (range), and percentage values. Parametric parameters were investigated with a Student’s t-test and one-way analysis of variance, and non-parametric parameters were investigated using the Mann-Whitney U, χ2 and Kruskal-Wallis tests. The association between the numeric data was compared using a correlation analysis. The parameters in the AA and control groups were described using a receiver operating characteristic (ROC) curve analysis. In addition, the sensitivity, specificity, positive and negative predictive values and likelihood ratios, and diagnostic accuracy were calculated by the area under the ROC curve. Results were evaluated within the 95%CI, and a P < 0.05 was considered as statistically significant.
RESULTS
The mean ages of patients were 29.9 ± 12.0 (range: 16-94 years), 31.5 ± 14.0 (range: 16-85 years) and 30.4 ± 13.0 years (range: 16-70 years) in Group I, Group II and Group III, respectively. Group I was comprised of 60.7% (179/295) men and 39.3% (116/295) women; Group II was comprised of 50.0% (50/100) men and 50.0% (50/100) women; and Group III was comprised of 60.0% (60/100) men and 40.0% (40/100) women. There were no demographic differences among the groups.
The comparisons of the laboratory values among the groups are given in Table 1. For all parameters, there were statistical differences between Group I and the two control groups (Ps < 0.05). MPV was lower in Group I, whereas PDW, WBC (Figures 1 and 2) and neutrophil percentage were higher compared to the control groups.
Table 1.
Comparison of the laboratory values between the groups
| Variable | Group I | Group II | Group III |
P values |
|||
| (n = 295) | (n = 100) | (n = 100) | I vs II | I vs III | II vs III | Overall | |
| White blood cell count, × 109/μL | 12.9 (3.1-25.7) | 11.5 (5.2-20.0) | 7.5 (3.5-13.6) | 0.032 | < 0.001 | < 0.001 | < 0.001 |
| Neutrophil, % | 73.9 (18.0-93.0) | 67.9 (45.0-87.9) | 57.6 (21.0-76.0) | 0.031 | < 0.001 | < 0.001 | < 0.001 |
| Mean platelet volume, fL | 8.5 (6.1-14.2) | 8.9 (6.0-13.0) | 8.9 (6.9-14.5) | NS | 0.001 | NS | 0.003 |
| Platelet distribution width, % | 49.0 (10.6-86.5) | 40.8 (12.8-87.9) | 18.4 (10.3-62.5) | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Data are presented as mean (range). NS: Not significant.
Figure 1.
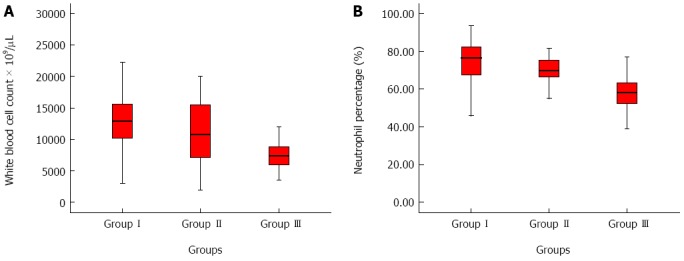
Blood cell counts. A: White blood cell count; B: Neutrophil percentage count variation.
Figure 2.
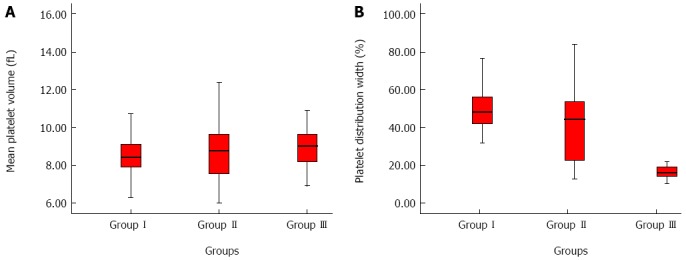
Platelet analyses. A: Mean platelet volume; B: Platelet distribution width variation.
The diagnostic comparisons of the blood value evaluations are given in Table 2. PDW was the most important diagnostic parameter, followed by WBC, neutrophil percentage and MPV. PDW showed high positive and low negative likelihood ratios. As a result, the diagnostic accuracy for PDW is higher than WBC and neutrophil percentage. In contrast, MPV has the lowest diagnostic accuracy, with a significant difference between Group I and Group III. The ROC curves for these parameters are shown in Figure 3. The high positive accuracy of PDW can also be seen here. As the MPV accuracy shows a reduction in Group I, it is located on the negative side of the reference line as a weak positive. The ROC curve analysis is presented for MPV without correction; smaller test results used in SPSS indicate a more positive test.
Table 2.
Diagnostic comparison of blood parameters
| Parameter | Cutoff | AUC | Sensitivity | Specificity | PPV | NPV | PLR | NLR | DA |
| (95%CI) | (%) | (%) | (%) | (%) | (%) | ||||
| White blood cell count | 10.6 × 109/μL | 0.87 (0.84-0.91) | 73.1 | 94 | 97.1 | 56.0 | 12.1 | 0.3 | 78 |
| Neutrophil | 69.85% | 0.87 (0.84-0.91) | 70.0 | 96 | 97.9 | 54.2 | 23.0 | 0.3 | 76 |
| Mean platelet volume | 8.98 fL | 0.62 (0.55-0.68) | 29.5 | 49 | 61.1 | 20.1 | 0.5 | 4.5 | 34 |
| Platelet distribution width | 32.15% | 0.95 (0.92-0.98) | 97.1 | 93 | 97.4 | 92.1 | 13.8 | 0.0 | 96 |
AUC: Area under the receiver operating characteristic curve; DA: Diagnostic accuracy; NLR: Negative likelihood ratio; NPV: Negative predictive value; PLR: Positive likelihood ratio; PPV: Positive predictive value.
Figure 3.
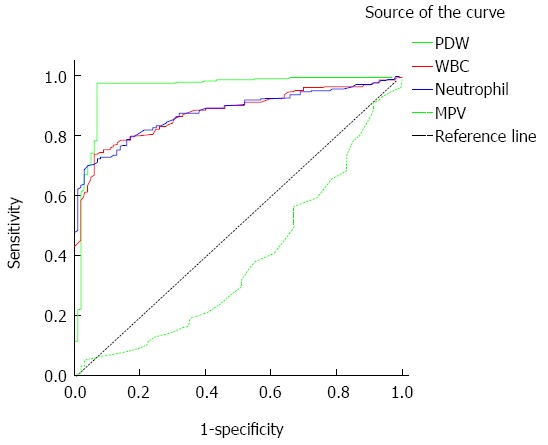
Receiver operating characteristic curves. MPV: Mean platelet volume; PDW: Platelet distribution width count; WBC: White blood cell count.
DISCUSSION
AA is the most common cause of “acute abdomen” in all age groups. Although the classical symptomatology and the examination findings of AA are well known, the diagnosis remains quite difficult to make among the causes of abdominal pain[15]. It is important to make a rapid and accurate diagnosis before the complications develop[1]. As AA is an inflammatory process, many authors consider using biomarkers for diagnosis. Among these, WBC is the one most commonly used. Many studies support that WBC is the first indicator to be elevated in appendix inflammation[16]. Among patients with AA, the sensitivity and specificity of WBC is 60%-87% and 53%-100%, respectively[15], with cut-off values of 11 × 109/L in the study by Bilic et al[9], and 10.4 × 103/mm3 in the study by Narci et al[6], which are consistent with our findings. In addition, the 78% diagnostic accuracy enhances the significance of WBC diagnostically.
There are several studies investigating the diagnostic accuracy of neutrophils in AA. Al-Gaithy[17] reported a sensitivity and a specificity of 70.9% and 65.5%, respectively, for neutrophil detection in patients undergoing surgery for suspected appendicitis that were classified according to pathology as AA or normal. In a case-controlled study by Bilici et al[9] in children, the sensitivity was 77% and the specificity was 91%. In the current study, we found a sensitivity of 70% and a specificity of 96%, which is similar to the literature. The differences in ratios were potentially attributed to the variability of the individuals (adult, child, etc.) and the type of the designed study.
Platelet activation is related to pathophysiology of disorders with a tendency for inflammation and thrombosis. MPV, a marker of platelet activation, is being investigated for its correlation with both inflammation and thrombosis. High MPV values are associated with cardio- and cerebrovascular disorders, and low-grade inflammatory conditions prone to arterial and venous thrombosis. Low MPV values may occur in high-grade inflammatory diseases, such as active rheumatoid arthritis or attacks of familial Mediterranean fever. These results are from anti-inflammatory treatment. As a result, a decrease in MPV occurs in acute cases, whereas an increase occurs with chronic events[18].
The proinflammatory activities of platelets are maintained by bioactive molecules stored within their alpha and dense granules[19,20]. After activation, these molecules are rapidly secreted. However, the exact organelle activity that controls the thrombocyte volume has not yet been clearly identified[19]. Danese et al[20] speculated that the reduced MPV could be due to the consumption or sequestration of the large activated platelets in the intestinal vasculature.
In the current trial, we detected a lower MPV in patients with AA. The cause of this remains unclear. A small number of studies failed to clearly demonstrate the correlation between MPV and AA. In the studies by Albayrak et al[21], Bilici et al[9] and Aydogan et al[11], MPV was significantly lower in the AA group, and with a sensitivity and specificity of 73%-84% and 54%-84%, respectively. Uyanik et al[15] failed to detect a correlation between AA and MPV in their study in children. However, we detected a statistical difference between the groups, and MPV was lower in the infected group. While the pathophysiology of this decrease is not known, it may be similar to the mechanism suggested by Danese et al[20]. The values of sensitivity and specificity of MPV in our study, 25.9% and 49.0%, respectively, are low compared to the literature. This result may stem from the emergency surgery after the clinical history and physical examination.
Both MPV and PDW are markers of platelet immaturity, and an increase in both as compared to controls suggests that young platelets are entering peripheral circulation. PDW is a function of standard deviation of log volume and is also known as the volume change coefficient. PDW is an index of thrombocyte volume heterogeneity, similar to erythrocyte distribution. The heterogeneity of thrombocyte volume occurs due to heterogenic demarcation of megakaryocytes rather than the aging of circulating thrombocytes[11].
There are a small number of studies that evaluate PDW. In a trial by Liang et al[22] investigating vascular dementia and Alzheimer’s disease, PDW was significantly lower in the patient group compared to the control group. In contrast, Mete Ural et al[23] detected high PDW values in patients with recurrent miscarriages. Cetin et al[24] reported a higher PDW value in patients with acute ST-segment elevation myocardial infarction compared to those with stable coronary artery disease. Yang et al[25] detected higher PDW values in patients with severe preeclampsia relative to those with mild preeclampsia. In the literature, there exists only one study that investigates the correlation between PDW and AA. In a 202-case study by Aydogan et al[11], patients were divided into groups as perforated and non-perforated. In this study with no control group, PDW values were significantly higher in the perforated group. In conclusion, PDW was considered as a marker that could be used in early detection of the perforation risk in AA. In the current study, we detected high PDW values in patients with AA, for which the sensitivity, specificity and diagnostic accuracy suggest that it could help in early diagnosis of AA.
This is the first study in the literature to present the correlation between AA and PDW as a case-controlled clinical trial. Detection of higher PDW values in the AA group relative to the control groups, and the high values of sensitivity, specificity, and diagnostic accuracy detected for AA are promising for future studies in diagnosis and early prediction of potential complications. This may provide an opportunity for making a diagnosis of AA without requiring additional analysis, increased cost, or loss of time, and is practically applicable in the emergency department. Nevertheless, diagnosis of AA should always be combined with clinical, laboratory and radiologic evaluations. PDW could be an important laboratory evaluation, but should always be associated with additional signs (right lower quadrant tenderness, elevated temperature, rebound tenderness), symptoms (migration of pain, vomiting) and other laboratory tests (leukocytosis, C-reactive protein). Additional multi-center, prospective studies are needed involving a larger sample size to confirm the results of this study.
COMMENTS
Background
The diagnosis of acute appendicitis (AA) can be difficult and confusing. While the diagnosis of AA is usually established clinically, the symptoms and findings may not always be typical. Rapid and accurate diagnosis is important because of potential complications. Novel methods that differentiate AA from non-specific abdominal pain and reduce the rate of negative appendectomy are needed. Such methods should be inexpensive and convenient, with results obtained in a short time. Therefore, recent studies have been investigating the diagnostic accuracy of inflammatory markers.
Research frontiers
Mean platelet volume (MPV) and platelet distribution width (PDW) are presented in the complete blood cell count, which is routinely used in emergency departments. They are the indicators of platelet activation.
Innovations and breakthroughs
There are very few studies investigating the diagnostic accuracy of platelet function parameters in cases of AA. A diagnostic comparison of these blood values was conducted in this study. The most important parameter identified was PDW, followed by white blood cell count, neutrophil percentage and MPV. Among the laboratory evaluations for AA, PDW could be an important one, but it should always be in association with the signs (right lower quadrant tenderness, elevated temperature, rebound tenderness), symptoms (migration of pain, vomiting) and other laboratory tests (leukocytosis, C-reactive protein).
Applications
In the literature, there is no case-controlled study investigating MPV or PDW in cases with AA. This is the first study in the literature to investigate the diagnostic significance of platelet function parameters in AA.
Terminology
MPV and PDW are indicators of platelet activation and are inflammatory markers.
Peer-review
This manuscript is a well-designed, interesting, retrospective, case-controlled study. It defines a new parameter for diagnosis of AA, which is a universal problem. PDW can be an important test in the diagnosis of AA.
Footnotes
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 10, 2014
First decision: August 15, 2014
Article in press: October 15, 2014
P- Reviewer: Augustin G, Ince V, Sartelli M S- Editor: Ma YJ L- Editor: AmEditor E- Editor: Liu XM
References
- 1.Yüksel Y, Dinç B, Yüksel D, Dinç SE, Mesci A. How reliable is the Alvarado score in acute appendicitis? Ulus Travma Acil Cerrahi Derg. 2014;20:12–18. doi: 10.5505/tjtes.2014.60569. [DOI] [PubMed] [Google Scholar]
- 2.Sammalkorpi HE, Mentula P, Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis--a prospective study. BMC Gastroenterol. 2014;14:114. doi: 10.1186/1471-230X-14-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nshuti R, Kruger D, Luvhengo TE. Clinical presentation of acute appendicitis in adults at the Chris Hani Baragwanath academic hospital. Int J Emerg Med. 2014;7:12. doi: 10.1186/1865-1380-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Doherty GM. Current Diagnosis and Treatment. 3rd ed. Doherty GM, editor. New York: McGraw Hill; 2010. pp. 615–620. [Google Scholar]
- 5.Tamanna MZ, Eram U, Al Harbi TM, Alrashdi SA, Khateeb SU, Aladhrai SA, Hussain AM. Clinical value of leukocyte counts in evaluation of patients with suspected appendicitis in emergency department. Ulus Travma Acil Cerrahi Derg. 2012;18:474–478. doi: 10.5505/tjtes.2012.83652. [DOI] [PubMed] [Google Scholar]
- 6.Narci H, Turk E, Karagulle E, Togan T, Karabulut K. The role of red cell distribution width in the diagnosis of acute appendicitis: a retrospective case-controlled study. World J Emerg Surg. 2013;8:46. doi: 10.1186/1749-7922-8-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ashdown HF, D’Souza N, Karim D, Stevens RJ, Huang A, Harnden A. Pain over speed bumps in diagnosis of acute appendicitis: diagnostic accuracy study. BMJ. 2012;345:e8012. doi: 10.1136/bmj.e8012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seetahal SA, Bolorunduro OB, Sookdeo TC, Oyetunji TA, Greene WR, Frederick W, Cornwell EE, Chang DC, Siram SM. Negative appendectomy: a 10-year review of a nationally representative sample. Am J Surg. 2011;201:433–437. doi: 10.1016/j.amjsurg.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Bilici S, Sekmenli T, Göksu M, Melek M, Avci V. Mean platelet volume in diagnosis of acute appendicitis in children. Afr Health Sci. 2011;11:427–432. [PMC free article] [PubMed] [Google Scholar]
- 10.Andersson M, Rubér M, Ekerfelt C, Hallgren HB, Olaison G, Andersson RE. Can new inflammatory markers improve the diagnosis of acute appendicitis? World J Surg. 2014;38:2777–2783. doi: 10.1007/s00268-014-2708-7. [DOI] [PubMed] [Google Scholar]
- 11.Aydogan A, Akkucuk S, Arica S, Motor S, Karakus A, Ozkan OV, Yetim I, Temiz M. The Analysis of Mean Platelet Volume and Platelet Distribution Width Levels in Appendicitis. Indian J Surg. 2013:1–6. doi: 10.1007/s12262-013-0891-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Catal F, Tayman C, Tonbul A, Akça H, Kara S, Tatli MM, Oztekin O, Bilici M. Mean platelet volume (MPV) may simply predict the severity of sepsis in preterm infants. Clin Lab. 2014;60:1193–1200. doi: 10.7754/clin.lab.2013.130501. [DOI] [PubMed] [Google Scholar]
- 13.Karagöz B, Alacacıoğlu A, Bilgi O, Demirci H, Özgün A, Erikçi AA, Sayan Ö, Yılmaz B, Kandemir EG. Platelet count and platelet distribution width increase in lung cancer patients. Anatol J Clin Investig. 2009;3:32–34. [Google Scholar]
- 14.Artunc Ulkumen B, Pala HG, Calik E, Oruc Koltan S. Platelet distribution width (PDW): A putative marker for threatened preterm labour. Pak J Med Sci. 2014;30:745–748. doi: 10.12669/pjms.304.4991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Uyanik B, Kavalci C, Arslan ED, Yilmaz F, Aslan O, Dede S, Bakir F. Role of mean platelet volume in diagnosis of childhood acute appendicitis. Emerg Med Int. 2012;2012:823095. doi: 10.1155/2012/823095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Birchley D. Patients with clinical acute appendicitis should have pre-operative full blood count and C-reactive protein assays. Ann R Coll Surg Engl. 2006;88:27–32. doi: 10.1308/003588406X83041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Al-Gaithy ZK. Clinical value of total white blood cells and neutrophil counts in patients with suspected appendicitis: retrospective study. World J Emerg Surg. 2012;7:32. doi: 10.1186/1749-7922-7-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011;17:47–58. doi: 10.2174/138161211795049804. [DOI] [PubMed] [Google Scholar]
- 19.Kayahan H, Akarsu M, Ozcan MA, Demir S, Ates H, Unsal B, Akpinar H. Reticulated platelet levels in patients with ulcerative colitis. Int J Colorectal Dis. 2007;22:1429–1435. doi: 10.1007/s00384-007-0330-y. [DOI] [PubMed] [Google Scholar]
- 20.Danese S, Motte Cd Cde L, Fiocchi C. Platelets in inflammatory bowel disease: clinical, pathogenic, and therapeutic implications. Am J Gastroenterol. 2004;99:938–945. doi: 10.1111/j.1572-0241.2004.04129.x. [DOI] [PubMed] [Google Scholar]
- 21.Albayrak Y, Albayrak A, Albayrak F, Yildirim R, Aylu B, Uyanik A, Kabalar E, Güzel IC. Mean platelet volume: a new predictor in confirming acute appendicitis diagnosis. Clin Appl Thromb Hemost. 2011;17:362–366. doi: 10.1177/1076029610364520. [DOI] [PubMed] [Google Scholar]
- 22.Liang QC, Jin D, Li Y, Wang RT. Mean platelet volume and platelet distribution width in vascular dementia and Alzheimer’s disease. Platelets. 2014;25:433–438. doi: 10.3109/09537104.2013.831064. [DOI] [PubMed] [Google Scholar]
- 23.Mete Ural U, Bayoğlu Tekin Y, Balik G, Kir Şahin F, Colak S. Could platelet distribution width be a predictive marker for unexplained recurrent miscarriage? Arch Gynecol Obstet. 2014;290:233–236. doi: 10.1007/s00404-014-3192-x. [DOI] [PubMed] [Google Scholar]
- 24.Cetin M, Bakirci EM, Baysal E, Tasolar H, Balli M, Cakici M, Abus S, Akturk E, Ozgul S. Increased platelet distribution width is associated with ST-segment elevation myocardial infarction and thrombolysis failure. Angiology. 2014;65:737–743. doi: 10.1177/0003319713520068. [DOI] [PubMed] [Google Scholar]
- 25.Yang SW, Cho SH, Kwon HS, Sohn IS, Hwang HS. Significance of the platelet distribution width as a severity marker for the development of preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2014;175:107–111. doi: 10.1016/j.ejogrb.2013.12.036. [DOI] [PubMed] [Google Scholar]


