Abstract
Purpose of review
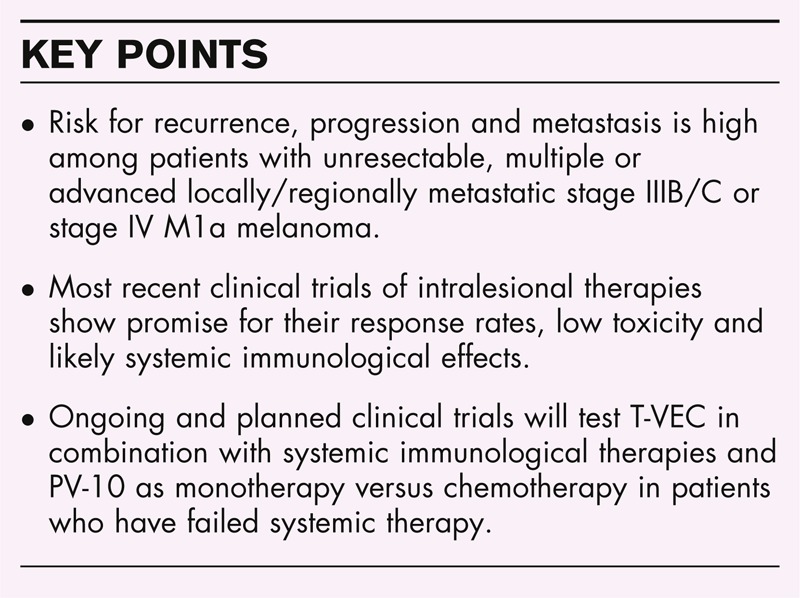
Patients with unresectable, multiple or advanced locally/regionally metastatic stage IIIB/C or stage IV M1a melanoma have a high risk for recurrence, progression and metastasis. The article reviews treatment advances for this population.
Recent findings
After promising phase 2 results with Allovectin-7 (velimogene aliplasmid), overall survival in a phase 3 study was shorter for Allovectin-7 than for dacarbazine/temozolomide (median 18.8 versus 24.1 months).
In a phase 2 trial of intratumoral electroporation of plasmid interleukin-12 among 28 patients with advanced melanoma, the primary endpoint of best overall response rate within 24 weeks of first treatment was 32.2% for objective response and 10.7% for complete response.
In the phase 3 OPTiM trial of talimogene laherparepvec, the intralesional agent that is furthest along in clinical testing, the primary endpoint of durable response rate was 16% for talimogene laherparepvec and 2% for granulocyte macrophage colony-stimulating factor.
In the PV-10 phase 2 trial among 80 patients with stage III–IV melanoma, the overall response rate was 51%, with a 26% complete response rate.
Summary
Despite advances, many patients will need several lines of therapy. Some will not be eligible for systemic therapy. Their low toxicity, easy administration and likely systemic immune effects make intralesional therapies an attractive option.
Keywords: electroporation, immunotherapy, intralesional therapy, oncolytic
INTRODUCTION
The landscape for the treatment of melanoma has changed dramatically in recent years. For decades, dacarbazine chemotherapy and high-dose interleukin (IL)-2 were the only US Food and Drug Administration (FDA)-approved agents for advanced disease, and both drugs are limited in their efficacy and application. Fortunately, with the advent of agents targeting the MAP-kinase pathway and the discovery of more effective immunologic agents, this is changing, and several new drugs have been approved in the past 2 years.
Melanoma has always been a disease with a propensity to cutaneous, subcutaneous and nodal metastases, which has led to investigation of various direct cutaneous interventions [1▪,2▪,3▪▪]. Melanoma also has a unique and close relationship with the immune system, with tumor infiltration by lymphocytes often indicating the attempt of the immune system to eliminate the tumor. These two facts have led to interest in intralesional therapy approaches with agents that may not only shrink the tumor directly but also stimulate a systemic immune response by modifying the tumor's antigenic milieu through intratumoral injection of therapeutic agents.
The search for effective intralesional therapies may be particularly relevant among patients with tumors accessible to direct injection, especially the subgroup with unresectable, multiple or advanced locally/regionally metastatic stage IIIB/C or stage IV M1a melanoma. These patients, beyond their significant morbidity, are at a high risk for recurrence, progression and metastasis, despite locoregional therapy such as surgery and radiation. Local/satellite/in-transit melanomas represent 6–10% [4] of primary melanomas and are a source of distant disease with high mortality rates. The population with recurrent locoregional disease, however, has usually formed a small subset of patients in randomized controlled trials of metastatic melanoma, and no standard of care has been established for them.
Box 1.
no caption available
BACILLE CALMETTE-GUÉRIN AND OTHER ‘OLDER’ AGENTS
A dramatic example of the potential for intralesional therapy for metastatic melanoma was a case study published [5] in 1975 of a 77-year-old man with 64 intracutaneous metastases and a pulmonary metastatic deposit. After inoculations with Bacille Calmette-Guérin (BCG) over an 8-month period, all 17 treated lesions resolved and more than 50% regression was observed in the pulmonary metastasis. Importantly, beyond the effective local ablation, the responses suggested that the BCG injections had induced adjuvant systemic host immune antitumor activity in the regional and distant uninjected metastases.
The rationale for BCG use in humans had emerged from animal research [6,7] showing it to induce a heightened host immune response against transplanted murine experimental tumors. Dummer et al.[8] showed BCG to increase Melan A-specific cytotoxic T cells, and Barth and Morton [9] reported regression in injected lesions among five of eight melanoma patients, and regression, as well, in uninjected nodules in two patients.
Interest in BCG waned, however, when subsequent experience included anaphylactic reactions and death due to disseminated BCG [10]. Also, an analysis of the large Eastern Cooperative Oncology Group (ECOG) randomized trial (E1673) [11] showed no significant benefit in disease-free or overall survival for BCG. The phase III trial tested adjuvant use of BCG with or without dacarbazine in 734 American Joint Commission on Cancer (AJCC) stage I–III melanoma patients in the United States at a high risk for recurrence after surgery. The patients had been treated between 1974 and 1978 with outcomes projected out to a median of 30 years. Whereas toxicity was generally mild, punctate abscesses were reported in more than two-thirds of the treated patients. It was concluded that with the lack of benefit and potential for clinically troublesome sequelae, use of BCG as an adjuvant therapy for melanoma could not be recommended at any melanoma stage.
Other small intralesional therapy studies have evaluated interleukin, interferon and granulocyte macrophage colony-stimulating factor (GM-CSF), for example, without demonstrating consistent or durable efficacy.
NEWER AGENTS
Among newer intralesional agents, Allovectin-7 (velimogene aliplasmid), plasmid IL-12, talimogene laherparepvec (T-VEC) and PV-10 have shown particular promise.
Allovectin-7
During cancer progression, alteration of major histocompatibility complex class I (MHC-I) expression occurs frequently and is thought to allow tumor cells to evade the immune system [12]. Allovectin-7 has the DNA sequences encoding human leukocyte antigen (HLA)-B7 and ß2 microglobulin, both components of MHC-I. Velimogene aliplasmid induces a five-fold increase in the frequency of HLA-B27-cytotoxic T cells, up-regulates/restores MHC-I molecules and induces a proinflammatory response. It was proposed that the drug increases the immune system's ability to recognize and target melanoma cells.
In phase 2 results, among 133 patients (127 evaluable) with stage IIIB/C and IV M1a/b injectable cutaneous, subcutaneous or nodal melanoma lesions [13], the overall response rate (ORR) (complete response + partial response) was 11.8% (3.2% + 8.7%), with stable disease in 25%. Time to death was significantly longer from the 24-week landmark in responders than in nonresponders (P = 0.036). Responses were observed in noninjected target lesions among 21% of patients (9/42) with stage IV disease (M1a/b).
The phase 3 Allovectin Immunotherapy for Metastatic Melanoma (AIMM) trial included 390 patients randomized 2 : 1 to velimogene aliplasmid or intravenous dacarbazine or oral temozolomide (TMZ). Patients had stage IIIB–IVM1a/b melanoma. The primary endpoint of response rate of at least 24 weeks was reported at 4.6% for velimogene aliplasmid and at 12.3% for dacarbazine/TMZ (P = 0.010). Duration of response among velimogene aliplasmid responders was marginally longer (P = 0.066), but overall survival was shorter [median 18.8 months, 95% confidence interval (CI) 16.6, 21.3 versus 24.1, 95% CI 17.1, 27.9, P = 0.491] than with dacarbazine/TMZ. Among responders, median overall survival was improved with velimogene aliplasmid [not applicable (n/a) (19.7, n/a) versus 40.7 months (28.9, n/a) P = 0.018]. The authors concluded that velimogene aliplasmid was not an effective treatment for the selected patient population.
Plasmid interleukin-12
Interleukin-12 enhances the immune capacity of natural killer (NK) cells and T cells, up-regulating interferon γ (IFNγ) and antigen presenting and processing. The first study of beneficial clinical effects of plasmid IL-12 intratumoral injections was by Heinzerling et al.[14] in 2005.
Presentations at the 50th Annual Meeting of the American Society of Clinical Oncology encompassing the most recent research on intralesional therapies for melanoma included one on a phase 2 trial of intratumoral electroporation of plasmid IL-12 [15]. The principle behind electroporation is that a mild current induced in tumor cells via an electrode opens cell pores, allowing a higher influx of a cytokine for a longer time span than would occur with systemic therapy with that same agent. The further benefit is that systemic concentrations are comparatively reduced. Electrochemotherapy is widely available in Europe.
Patients received injections of IL-12 on days 1, 5, and 8 for a maximum of four cycles at 12-week intervals. Among 28 patients with advanced melanoma receiving at least one treatment cycle, the primary endpoint best ORR within 24 weeks of first treatment (according to modified RECIST criteria) was 32.2% for objective response and 10.7% for complete response. Among 85 evaluated treated lesions, the complete response rate was 44.7%, with partial responses at 8.2% and stable disease at 30.6%. Assessment of systemic response revealed regression of untreated distant lesions in 13 (59.1%) of 22 evaluable patients.
Apart from injection site pain (69.0%) and inflammation (20.7%), the treatment produced no toxicity, with only one report of grade 3 pain and no serious adverse events. The findings, the authors concluded, suggest successful induction of a systemic response. An expansion protocol is planned.
Talimogene laherparepvec
Among intralesional therapies, T-VEC is furthest along in clinical testing. T-VEC is a herpes simplex virus (HSV)-1-derived oncolytic immunotherapy that produces both local and systemic effects. The virus selectively replicates within tumors, rupturing them and producing GM-CSF which enhances systemic, specific antitumor immune responses.
In a phase 2 study [16], among 50 advanced melanoma patients, most with treatment-resistant disease, T-VEC response rates were 16% complete, 10% partial, 4% surgical complete and another 20% had stable disease for at least 3 months. Three more patients achieved complete responses on an extension protocol. Overall survival was 54 and 52% at 1 and 2 years, respectively. Systemic immunotherapeutic effects were evidenced by responses in both injected and uninjected lesions.
In the phase 3 OPTiM trial, Kaufman et al.[17▪] compared T-VEC versus subcutaneous GM-CSF in 436 stage IIIB/C and IV melanoma patients who had injectable and unresectable disease. The primary endpoint was durable response rate. Durable responses (complete or partial) were defined as those lasting continuously for at least 6 months and begun within 12 months of initiation of therapy.
Among 141 patients receiving GM-CSF, the ORR was 5.7% (95% CI 1.9, 9.5) as compared with 26.4% for the 295 patients receiving T-VEC (95% CI 21.4, 31.5) (P < 0.0001). Complete responses were reported in 0.7% of GM-CSF patients and in 10.8% of T-VEC patients. The treatment difference of 14.1% (95% CI 8.2, 19.2) was highly significant (P < 0.0001). The durable response rate for T-VEC was 16% (95% CI 12%, 21%) and 2% for GM-CSF (95% CI 0%, 5%, P < 0.0001). Median overall survival was 18.9 months (95% CI 16.0, 23.7) in the GM-CSF group and 23.3 months (95% CI 19.5, 29.6) in the T-VEC group (P = 0.051). An exploratory subgroup analysis showed an overall survival hazard ratio of 0.57 among patients with stage IIIB/C, IVM1a disease as compared with 1.07 in patients with stage IVM1b/c disease.
In uninjected nonvisceral lesions (N = 981), tumor area reductions were at least 50% in 34% of patients and 100% in 22% with T-VEC. Among uninjected visceral lesions (N = 177), the rates were 15 and 9%, respectively. T-VEC was tolerable, with cellulitis as the only grade 3–4 adverse event occurring in more than 2% of the patients. The authors concluded that T-VEC monotherapy provides a novel potential therapeutic approach for metastatic melanoma.
Some melanoma researchers have surmised that the likely ultimate application of intralesional therapies will be in combination with one of the systemic immunotherapies in use or in development. Preliminary data from the phase 1b/2 study [18] of T-VEC combined with ipilimumab suggest much higher complete and ORRs with the combination than have been seen with either agent alone. Investigators enrolled 18 patients with stage IIIB–IV M1c melanoma. All received T-VEC and ipilimumab. The investigator assessed ORR was 56% (95% CI 31–79%), with complete responses in 33%, partial responses in 22% and stable disease in 17%. In responders, mean/median time to investigator-assessed response was 18.8/22.9 weeks (range 11.1–25.0). Flow cytometry showed a higher increase in the number of activated CD8 T cells in patients with disease control, which may indicate T-VEC responses. No dose-limiting toxicities were observed, and most reported toxicities were apparently related to ipilimumab. The randomized phase 2 portion of the trial is currently ongoing. A trial in combination with the anti-programmed death-1 (PD1) antibody, pembrolizumab, is also being initiated.
PV-10
PV-10 is derived from Rose Bengal disodium, a water-soluble xanthene dye used currently as an ophthalmological topical diagnostic aid, and previously used as an intravenous liver function diagnostic agent. As an intralesional injection, the 10% sterile, nonpyrogenic saline solution (PV-10) induces chemical tumor ablation and has ‘bystander’ effects in uninjected lesions. This latter observation suggests that tumor ablation elicits a systemic immune response [19].
While PV-10 is excluded from normal cells, it transits the plasmalemma of cancer cells, accumulating in lysosomes [20] and stimulating lysosomal release. Complete autolysis occurs within 30–60 min. A bystander effect, it is hypothesized, is the result of acute exposure of antigenic tumor fragments to antigen-presenting cells. The consequence, combined with autolysis, is rapid reduction in tumor burden and immunologic activation.
A phase 2 trial, which followed promising phase 1 results [21], included 80 patients with measurable stage III–IV melanoma. In this multicenter, international investigation [22▪], patients with a median of six prior interventions received PV-10 into up to 20 cutaneous and subcutaneous lesions up to four times over a 16-week period. Best ORR (BORR) assessed by RECIST in up to 10 injected target lesions at 52 weeks was the primary endpoint.
In the intention-to-treat population, the ORR was 51% (95% CI 40–63%), with a 26% complete response rate (95% CI 17–37%). Among the 54 patients of 62 with cutaneous disease only in whom all melanoma was followed, all lesions were treated with PV-10 in 28 patients. In this subgroup, the ORR was 71% (95% CI 51–87%), with complete responses in 50% (95% CI 31–70%). In the other 26 patients with ‘all melanoma followed’ who had untreated bystander lesions, the ORR was 54% (95% CI 33–73%) with a complete response rate of 23% (95% CI 9–44%) (see Table 1).
Table 1.
Primary endpoints for Allovectin-7, talimogene laherparepvec and PV-10
| Agent, trial (N) | Phase | Comparator | Response at ≥24 weeks | P value | Comment |
| Allovectin-7, AIMM (N = 390) | 3 | DTIC or TMZ | 4.6 vs. 12.3%a | NS | Trial did not meet primary endpoint |
| Agent, trial (N) | Phase | Comparator | Durable response | P value | Comment |
| T-VEC, OPTiM (N = 436) | 3 | GM-CSF | 16% (95% CI 12%, 21%) vs. 2.0% (95% CI 0%, 5%) | <0.0001 | Trial met primary endpoint |
| Agent (N) | Phase | Comparator | Overall response | P value | Comment |
| PV-10 (N = 80) | 2 | NA | 51% (95% CI 40%-63%) | NA | Phase 3 trial to be initiated |
AIMM, Allovectin Immunotherapy for Metastatic Melanoma; CI, confidence interval; DTIC, dacarbazine; GM-CSF, granulocyte macrophage colony-stimulating factor; NS, not significant; TMZ, temozolomide; T-VEC, talimogene laherparepvec.
aIn favor of DTIC or TMZ.
While pain at the injection site was the most frequently reported adverse event immediately following PV-10 injection, median lesion pain score improvements for patients in the ‘all melanoma followed’ cohort reporting pain at baseline coincided with tumor burden reductions.
Sarnaik et al.[23], in a small recently presented trial, provided corroboration of not just the potential clinical benefit of intralesional PV-10 in metastatic melanoma, but of a concomitant immune response. Six of the eight patients included in the pilot study had metastatic disease refractory to previous ipilimumab, anti-PD-1 and/or vemurafenib (BRAF) therapy. Investigators biopsied two study lesions in each of the eight patients, all with dermal and/or subcutaneous metastatic melanoma. One of the two lesions was injected with PV-10, and then 1–2 weeks later, both residual sites were completely excised and compared to determine pathologic complete response (pCR). In four of the eight patients, PV-10 led to pCR in the post-treatment biopsies of both PV-10-injected and uninjected study lesions. Partial regression was observed in all eight injected lesions. Four of the patients refractory to prior ipilimumab, anti-PD-1 and/or vemurafenib (BRAF) therapy had pCRs in both the injected and uninjected lesions.
Investigators also found a significant increase in immune cells in peripheral blood after PV-10 therapy, with augmentation of CD3+ (P = 0.03), CD4+ (P = 0.06), CD8+ (P = 0.03) T cells and NK cells (P = 0.05). All eight patients evaluable to date had at least partial regression of injected lesions, and four had pathological complete responses.
A phase 3 trial of PV-10 as a single agent among patients who have locoregional disease and have failed or are ineligible for systemic therapy will compare the agent to chemotherapy consisting of dacarbazine or TMZ.
DISCUSSION
In an era of effective and promising systemic agents, one must ask the question: is there still a role and rationale for intralesional and regional therapy for what is usually a systemic disease?
As noted above, melanoma tends to have lesions accessible to intralesional therapy in a high percentage of cases. Despite the new advances seen in melanoma therapy, cure for most is still elusive and patients are probably going to need several lines of therapy alone or in combination to maximize their chances of survival. Furthermore, given the advanced age and comorbidities of many patients with melanoma, systemic therapy may not be an option for all patients. The relative lack of toxicity and ease of administration of intralesional treatments, coupled with their potential for a systemic immune effect, makes them an attractive prospect particularly in those situations.
Challenges remain and are numerous. What is the correct endpoint for clinical trials with intralesional agents? How should we assess true benefit? The true test of these therapies may not necessarily lie in their ability to improve survival, but rather in the degree to which they afford durable control of predominantly or exclusively locoregional disease that is difficult or impossible to resect. While patients would very likely perceive this as a positive treatment goal, it would not be easy to test as an endpoint in clinical trials.
Intralesional therapies may have their most promise and potential when used in combination with the new systemic therapies, particularly immunotherapies. Preliminary evidence showing augmented response rates when T-VEC is combined with ipilimumab provides a hypothesis to build upon. Another interesting but as yet untested approach would be to consider this as a ‘neo-adjuvant’ approach in patients who are destined for surgical cure. Can we instigate a potentially useful systemic immune response prior to removal of the tumor? In other words, can we make the tumor our ‘ally’ and allow it to benefit the host's immune system with an enhanced systemic response by using an intralesional agent in this setting? These and other questions must await the conduct of well designed clinical trials.
CONCLUSION
While the development of systemic immunotherapies has brought significant improvements in outcomes for patients with metastatic melanoma, interest in emerging intralesional therapies is justified by their strong ablative effects, lack of toxicity and their stimulation of local and systemic immunological responses. What remains unclear at this early stage of experience with the agents in current development is how clinically significant the evoked systemic effects will be, and further, what combinations of intralesional therapy and systemic immune therapy will reap the greatest benefits for patients. Future clinical trials, it is hoped, will help answer these questions and provide yet another potentially effective approach to treat our patients with melanoma.
Acknowledgements
None.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1▪.John HE, Mahafffey PJ. Ablation and cryotherapy of melanoma metastases. J Surg Oncol 2014; 109:296–300. [DOI] [PubMed] [Google Scholar]; Comprehensive and recent review of ablative therapy and cryotherapy for cutaneous melanoma metastases.
- 2▪.Campana LG, Testori A, Mozzillo N, Rossi CR. Treatment of metastatic melanoma with electrochemotherapy. J Surg Oncol 2014; 109:301–307. [DOI] [PubMed] [Google Scholar]; Recent review on technique of electrochemotherapy, a modality more widely used in Europe than North America.
- 3▪▪.Temple-Oberle CF, Byers BA, Hurdle V, et al. Intra-lesional interleukin-2 therapy for in transit melanoma. J Surg Oncol 2014; 109:327–331. [DOI] [PubMed] [Google Scholar]; Intralesional IL-2 has been a treatment that has been available for many years. This is the most recent and complete review of the subject.
- 4.Thompson JF. Local and regional therapies for melanoma: many arrows in the quiver. J Surg Oncol 2014; 109:29. [DOI] [PubMed] [Google Scholar]
- 5.Mastrangelo MJ, Bellet RE, Berkelhammer J, Clark WH., Jr Regression of pulmonary metastatic disease associated with intralesional BCG therapy of intracutaneous melanoma metastases. Cancer 1975; 36:1305–1308. [DOI] [PubMed] [Google Scholar]
- 6.Goldie JH. Scientific basis for adjuvant and primary (neoadjuvant) chemotherapy. Semin Oncol 1987; 14:1–7. [PubMed] [Google Scholar]
- 7.Weiss DW. MER and other mycobacterial fractions in the immunotherapy of cancer. Med Clin North Am 1976; 60:473–497. [DOI] [PubMed] [Google Scholar]
- 8.Dummer R, Rochlitz C, Thierry V, et al. Adenoviral interleukin-2 gene transfer into P815 tumor cells abrogates tumorigenicity and induces antitumoral immunity in mice. Mol Ther 2008; 16:985–994. [DOI] [PubMed] [Google Scholar]
- 9.Barth A, Morton DL. The role of adjuvant therapy in melanoma management. Cancer 1995; 75:726–734. [DOI] [PubMed] [Google Scholar]
- 10.de la Monte SM, Hutchins GM. Fatal disseminated bacillus Calmette-Guerin infection and arrested growth of cutaneous malignant melanoma following intralesional immunotherapy. Am J Dermatopathol 1986; 8:331–335. [DOI] [PubMed] [Google Scholar]
- 11.Agarwala SS, Neuberg D, Park Y, Kirkwood JM. Mature results of a phase III randomized trial of Bacillus Calmette-Guerin (BCG) versus observation and BCG plus dacarbazine versus BCG in the adjuvant therapy of American Joint Committee on Cancer Stage I-III Melanoma (E1673). Cancer 2004; 100:1692–1698. [DOI] [PubMed] [Google Scholar]
- 12.Garrido C, Paco L, Romero I, et al. MHC class I molecules act as tumor suppressor genes regulating the cell cycle gene expression, invasion and intrinsic tumorigenicity of melanoma cells. Carcinogenesis 2012; 33:687–693. [DOI] [PubMed] [Google Scholar]
- 13.Bedikian AY, Richards J, Kharkevitch D, et al. A phase 2 study of high-dose allovectin-7 in patients with advanced metastatic melanoma. Melanoma Res 2010; 20:218–226. [DOI] [PubMed] [Google Scholar]
- 14.Heinzerling L, Burg G, Dummer R, et al. Intratumoral injection of DNA encoding human interleukin 12 into patients with metastatic melanoma: clinical efficacy. Hum Gene Ther 2005; 16:35–48. [DOI] [PubMed] [Google Scholar]
- 15.Daud A, Algazi P, Ashworth MT, et al. Systemic antitumor effect and clinical response in a phase 2 trial of intratumoral electroporation of plasmid interleukin-12 in patients with advanced melanoma. ASCO 2014; abstract. 9025. [Google Scholar]
- 16.Senzer NN, Kaufman HL, Amatruda T, et al. Phase II clinical trial of a granulocyte-macrophage colony-stimulating factor-encoding, second-generation oncolytic herpes virus in patients with unresectable metastatic melanoma. J Clin Oncol 2009; 27:5763–5771. [DOI] [PubMed] [Google Scholar]
- 17▪.Kaufman, Andtbacka RI, Collichio FA, et al. Primary overall survival from OPTiM, a randomized phase III trial of talimogene laherparepvec (T-VEC) versus subcutaneous GM-CSF for the treatment of unresected stage IIIB/Cand IV melanoma. ASCO 2014; abstract 9008a. [Google Scholar]; Important data of a recently evaluated agent, T-VEC, for mostly stage III melanoma only available currently in abstract form.
- 18.Puzanov, Milhem MM, Andtbacka RI, et al. Primary analysis of a phase 1b multicenter trial to evaluate safety and efficacy of talimogene laherparepvec (T-VEC) and ipilimumab (ipi) in previously untreated, unresected stage IIIB-IV melanoma. ASCO 2014; abstract 9029. [Google Scholar]
- 19.Ross MI. Intralesional therapy with PV-10 (Rose Bengal) for in-transit melanoma. J Surg Oncol 2014; 109:314–319. [DOI] [PubMed] [Google Scholar]
- 20.Wachter E. SPIE (International Society for Optics and Photonics) Proceedings, 4611. 2002; 112–118. [Google Scholar]
- 21.Thompson JF, Hersey P, Wachter E. Chemoablation of metastatic melanoma using intralesional Rose Bengal. Melanoma Res 2008; 18:405–411. [DOI] [PubMed] [Google Scholar]
- 22▪.Agarwala SS, Thompson JF, Smithers BM, et al. Mature data on PV-10 as chemoablation for unresectable stage III melanoma and plans for a randomized trial. ASCO 2014; abstract 9027. [Google Scholar]; Mature data on PV-10 as chemoablation for unresectable stage III melanoma and plans for a randomized trial.
- 23.Sarnaik A, Crago G, Liu H, et al. Assessment of immune and clinical efficacy after intralesional PV-10 in injected and uninjected metastatic melanoma lesions. ASCO 2014; abstract 9028. [Google Scholar]


