Supplemental Digital Content is available in the text.
Key Words: acupuncture, back pain, fear of pain, health knowledge, attitudes, practice, self-efficacy
Abstract
Objectives:
To identify psychological covariates of longitudinal changes in back-related disability in patients undergoing acupuncture.
Materials and Methods:
A longitudinal postal questionnaire study was conducted with data collection at baseline (pretreatment), 2 weeks, 3, and 6 months later. A total of 485 patients were recruited from 83 acupuncturists before commencing acupuncture for back pain. Questionnaires measured variables from 4 theories (fear-avoidance model, common-sense model, expectancy theory, social-cognitive theory), clinical and sociodemographic characteristics, and disability. Longitudinal multilevel models were constructed with disability over time as the outcome.
Results:
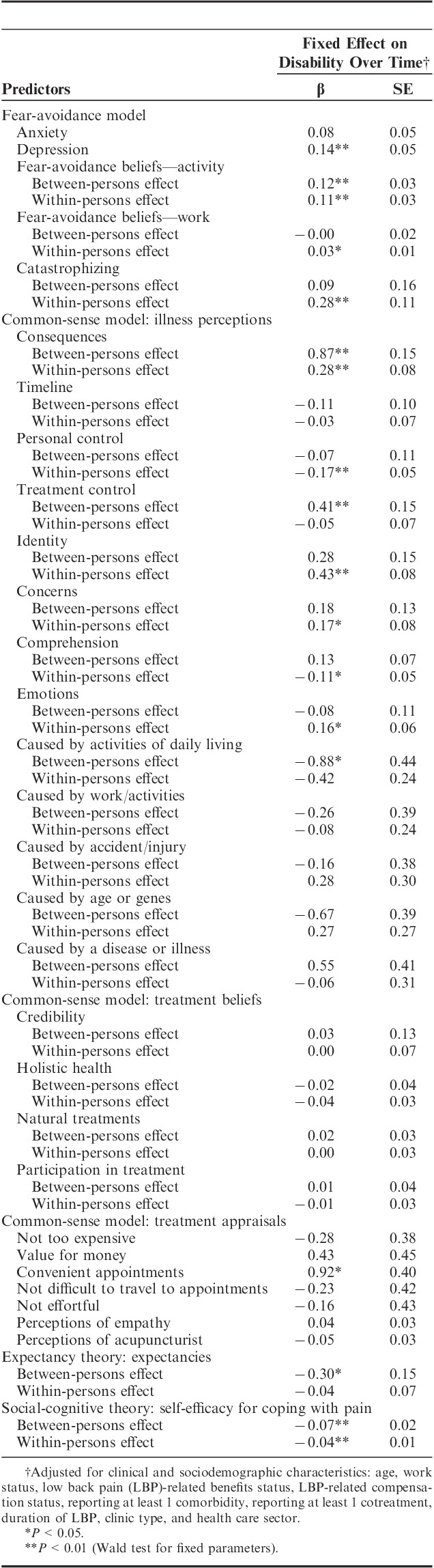
Within individuals, reductions in disability (compared with the person’s individual mean) were associated with reductions in: fear-avoidance beliefs about physical activity (β=0.11, P<0.01) and work (β=0.03, P<0.05), catastrophizing (β=0.28, P<0.05), consequences (β=0.28, P<0.01), concerns (β=0.17, P<0.05), emotions (β=0.16, P<0.05), and pain identity (β=0.43, P<0.01). Within-person reductions in disability were associated with increases in: personal control (β=−0.17, P<0.01), comprehension (β=−0.11, P<0.05) and self-efficacy for coping (β=−0.04, P<0.01). Between individuals, people who were less disabled had weaker fear-avoidance beliefs about physical activity (β=0.12, P<0.01), had more self-efficacy for coping (β=−0.07, P<0.01), perceived less severe consequences of back pain (β=0.87, P<0.01), had more positive outcome expectancies (β=−0.30, P<0.05), and appraised acupuncture appointments as less convenient (β=0.92, P<0.05).
Discussion:
Illness perceptions and, to a lesser extent, self-efficacy and expectancies can usefully supplement variables from the fear-avoidance model in theorizing pain-related disability. Positive changes in patients’ beliefs about back pain might underpin the large nonspecific effects of acupuncture seen in trials and could be targeted clinically.
Personally, economically, and socially, back pain is costly.1 Acupuncture is recommended by UK clinical guidelines for low back pain (LBP)2 and is commonly used for LBP.3 In randomized clinical trials acupuncture has shown large effects on chronic pain compared with usual care or waiting list controls but often only small effects compared with sham acupuncture.4,5 This suggests acupuncture has large nonspecific effects, that is, factors other than needling characteristics contribute to patients’ outcomes.6 Indeed, acupuncture can be conceptualized as a complex intervention in which changes in patients’ health are produced not only by needling but also by more psychosocial factors such as empathic therapeutic relationships and holistic consultations in which discussions of lifestyle and self-care can trigger changes in how patients think and feel about their symptoms and their ability to manage them.7–10 However, little is known about the psychosocial factors and processes that might be involved in acupuncture for LBP: established psychological models have not been applied to understand acupuncture’s effects. Although variables from such models may not be explicitly addressed by acupuncturists, this does not mean they are not involved in patients’ ongoing LBP in this treatment context. Therefore, a comprehensive and theoretically informed investigation of psychological covariates of acupuncture’s effects on LBP was designed, drawing on major theoretical frameworks that have predicted LBP outcomes in patients undergoing other interventions: the fear-avoidance model (FAM), common-sense model (CSM), expectancy theory, and social-cognitive theory (SCT).
According to the FAM of chronic pain, psychological factors are intrinsic to the development and maintenance of chronic pain.11 When patients catastrophize about pain, they come to fear pain and avoid situations/activities that might trigger it. This inactivity (with depression, disability, and anxiety/hypervigilance) prevents recovery and the pain experience continues. Positive outcomes have been associated with less catastrophizing, weaker fear-avoidance beliefs, and less negative effect in LBP patients undergoing conventional and/or explicitly psychological treatments.11–13 If fear-avoidance processes are indeed intrinsic to the maintenance of chronic pain and associated disability then one would expect changes in fear-avoidance variables to predict positive outcomes in patients undergoing acupuncture.
According to the CSM of self-regulation of health and illness,14 people’s perceptions of symptoms such as LBP are organized along 5 core cognitive dimensions (identity, consequences, controllability/cure, causes, timeline) and guide the individual’s choice of treatment; having more positive illness perceptions (eg, seeing LBP as more controllable) leads to better health outcomes.15 The theorized role of illness perceptions in LBP has not yet been tested in patients receiving acupuncture but is supported by studies of LBP patients in other settings, including chronic pain clinics,16 primary care,17 and rehabilitation.18 An extension of the common-sense model19,20 further suggests that, regardless of which treatment is chosen, patients who have positive beliefs about their treatment, practitioner, and therapeutic relationship (eg, believing their treatment is credible and their practitioner cares for them), are more likely to adhere to treatment and experience positive outcomes. Consistent with this, patients’ appraisals of the therapeutic relationship predicted acupuncture outcomes in 1 small study21 and in clinical trials an enhanced therapeutic relationship augmented the effects of acupuncture for patients with irritable bowel syndrome22 but not osteoarthritis.23 Questions therefore remain about the role of acupuncture patients’ illness perceptions, treatment beliefs, and perceptions of their practitioner/therapeutic relationship with respect to treatment outcome.
According to expectancy theory (which was developed and tested primarily in relation to placebo effects) response expectancies are directly related to nonvolitional responses including pain.24 Applied to a clinical setting, this theory suggests that when patients expect to experience pain relief following a particular treatment they are then more likely to experience pain relief from that treatment. A few acupuncture studies have reported that patients who have more positive expectancies have better outcomes.25–27 However, overall the evidence for expectancy effects in acupuncture is mixed and this inconsistency may be related to small sample sizes and the use of various unvalidated and general questionnaires to measure expectancies.28,29
SCT is a general theory of motivation and action which holds that self-efficacy mechanisms are central to self-regulation processes involved in human behavior: a strong belief in one’s capability to attain a particular goal is causally related to one’s actual ability to attain that goal.30,31 Applied to LBP, belief in one’s ability to cope with pain is causally related to actual coping ability: people with higher self-efficacy for coping are expected to commit to more challenging goals related to coping with LBP, to put more effort into achieving those goals, and to recover more quickly after setbacks.32 The predicted relationship between self-efficacy and coping ability has been demonstrated in LBP but not specifically in patients undergoing acupuncture for LBP. For example, in 1 multivariate analysis, illness perceptions and self-efficacy predicted disability in LBP patients but depression, catastrophizing, and fear-avoidance did not,33 indicating the value of considering self-efficacy alongside other psychological variables.
To summarize, acupuncture has large nonspecific effects that might be underpinned by psychosocial processes. Variables from the FAM, CSM, and SCT have been associated with LBP outcomes in other settings, but there has been an almost exclusive focus on the role of expectancies and the therapeutic relationship in research on psychosocial processes in acupuncture. A prospective longitudinal observational cohort study with patients undergoing acupuncture for LBP was conducted to test the hypotheses that disability is associated with variables derived from (1) FAM; (2) the CSM; (3) expectancy theory; and (4) SCT. The aims were (1) to compare the 4 models; (2) to identify which individual variables across all of these models were independently associated with disability; and (3) to test whether each variable had its effect between or within individuals. If, as the theories suggest, psychological processes have a causal role in maintaining back pain-related disability and mediate changes in disability during the course of acupuncture, then changes in psychological factors within individuals should be directly associated with changes in disability levels also within individuals. If psychological factors predispose patients to respond to acupuncture (ie, moderate changes in disability), then there should be between-person effects of psychological factors on disability levels.
MATERIALS AND METHODS
Design and Measures
Back-related disability (the primary outcome) was assessed 4 times: pretreatment, 2 weeks after first treatment, 3 months (when most courses of acupuncture for LBP have been completed), and 6 months. Clinical (eg, LBP duration) and sociodemographic characteristics (eg, age, work status) previously associated with disability were assessed pretreatment. Depression and anxiety were assessed pretreatment, appraisals were assessed posttreatment, and all other psychological predictors described below were assessed at every measurement occasion. Self-report questionnaires were chosen for their theoretical relevance, psychometric properties, and length (to reduce response burden). They are described briefly here; further details are available in Supplemental Digital Content 1, http://links.lww.com/CJP/A107.
Disability
The primary outcome, back pain-related disability was assessed using the 24-item Roland Morris Disability Questionnaire (RMDQ),34 which asks patients to think about “today” and to indicate whether their back pain interferes with 24 activities, for example “I stay at home most of the time because of my back.” High scores indicate greater back-related disability.
Fear-Avoidance Model Measures
Catastrophizing was assessed using the 6-item catastrophizing subscale of the Coping Strategies Questionnaire.35 Fear-avoidance beliefs about activity and work were assessed using the 4- and 7-item subscales of the Fear-Avoidance Beliefs Questionnaire.36 Anxiety and depression were measured using the two 7-item subscales of the 14-item Hospital Anxiety and Depression Scale.37
Common-Sense Model Measures
Illness perceptions of back pain were measured with the 9-item Brief Illness Perception Questionnaire.38 Responses to the free-response question that asks respondents to name the 3 main causes of their back pain were inductively grouped into categories, resulting in dichotomous variables representing whether or not each participant believed that their back pain was caused by: work, disease, injury, age, and activity.
Treatment beliefs were assessed with the 3 subscales of the Complementary and Alternative Medicine Belief Inventory39 which measure respondents’ beliefs in holistic approaches to health (6 items), natural treatments (6 items), and participation in treatment (5 items). Treatment appraisals were assessed with the Treatment Appraisal Questionnaire,40 using the 10-item subscale measuring appraisals of one’s therapist and 5 single items measuring appraisals of practical aspects of treatment (eg, cost). Appraisals of the credibility of acupuncture were assessed with the 3-item credibility subscale of the Credibility Expectancy Questionnaire.41 Appraisals of the acupuncturist’s empathy were measured using the 10-item CARE.42
Expectancy Theory Measures
Response expectancies were measured using the 3-item expectancy subscale of the Credibility Expectancy Questionnaire (41).
Social-Cognitive Theory Measures
Self-efficacy for coping with back pain was assessed using the 5-item Chronic Pain Self-Efficacy for Pain Management subscale.43
Procedure and Participants
Ethics approval was obtained from Southampton and South West Hampshire Research Ethics Committee (A) (08/H0502/92). In the United Kingdom, many forms of acupuncture are available (eg, western acupuncture, traditional Chinese acupuncture) in different types of clinic (eg, complementary medicine, pain clinics) and different health care sectors (private, National Health Service); acupuncturists were recruited from a range of settings to reflect this diversity (Table 1). Eighty-three acupuncturists were recruited from across Great Britain and Northern Ireland through the Primary Care Research Network, acupuncturist associations, and internet searches for hospital-based services.
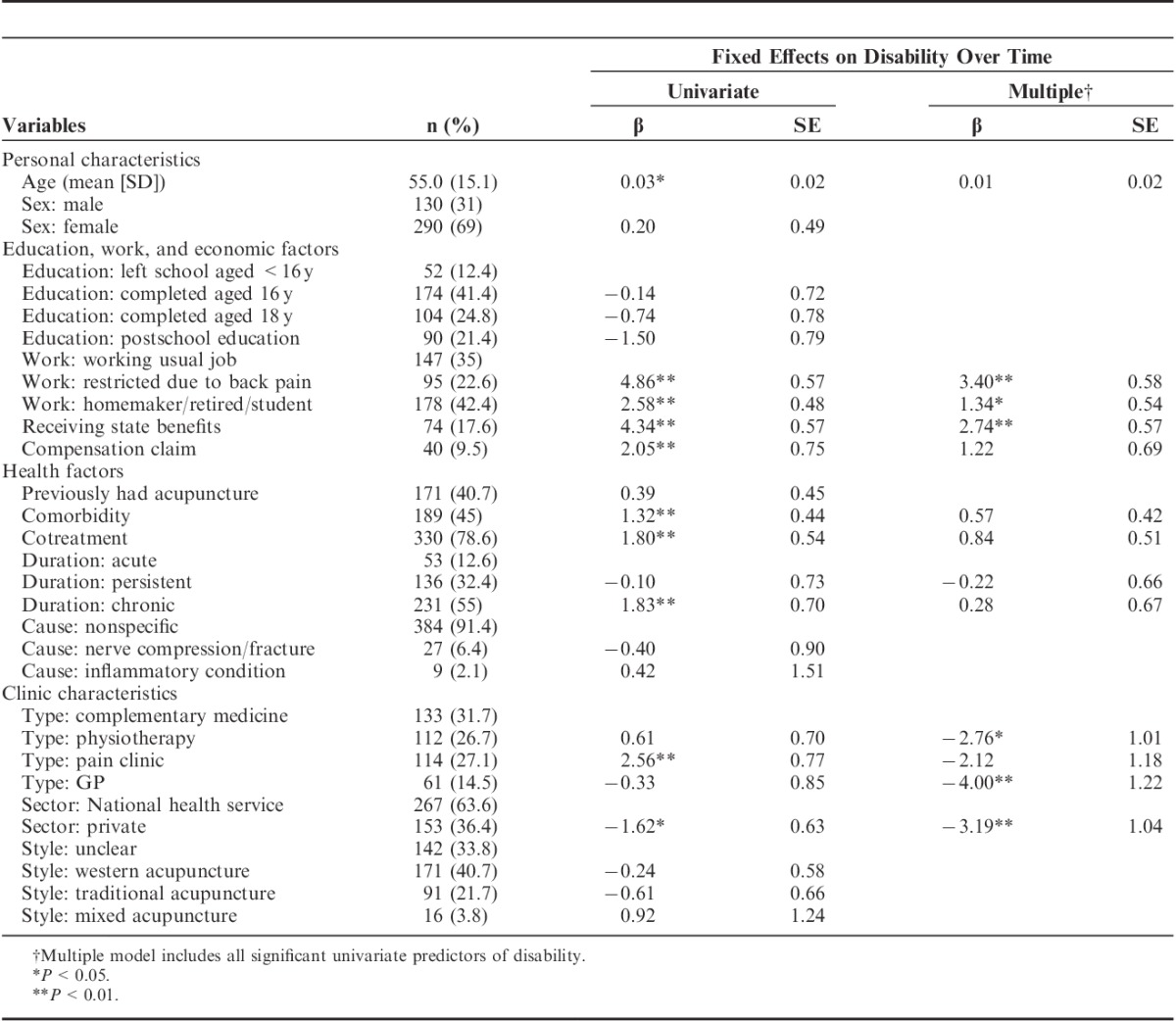
TABLE 1.
Clinical and Sociodemographic Characteristics, and Effects on Disability
Acupuncturists distributed baseline questionnaires (including information and consent documents) to consecutive patients identified from waiting lists or at triage who were: aged over 18 and scored at least 4 on the RMDQ.34 Patients with pain associated with cancer were excluded. Patients returned baseline questionnaires and consent forms by Freepost directly to the researchers, from November 2008 until October 2010. Subsequent questionnaires were posted to participants. Gift vouchers and personalized repeated follow-ups were sent to enhance recruitment and retention.44
Data Analysis
Within each timepoint, the proportion of missing data was low (typically <5% missing values per variable) and Missing at Random (according to Little’s Missing Completely at Random test) and thus missing values were imputed using EM.45 Data were not imputed when a participant provided no data at a particular timepoint.46 IBM SPSS Statistics 19 was used to impute missing data and generate descriptive statistics. There were no very high (>0.9) bivariate correlations among predictors, suggesting absence of problematic multicollinearity.45 LBP duration at baseline was categorized as acute (<6 wk), persistent (6 to 52 wk), or chronic (>52 wk).2
A longitudinal multilevel approach modeled linear trends in disability over time using MLwiN.47 Level 1 units were timepoints, level 2 units were individual patients, and level 3 units were acupuncturists. Intercepts and slopes were allowed to vary between individuals and level 2 residual covariance (between the slope and intercept across all individuals) was estimated. The fixed effects of clinical and sociodemographic variables were assessed by comparison with this 3-level model.
To assess the effects of variables on posttreatment disability, timepoint was centered on 6 months.48 Variables measured at baseline only and measures of treatment appraisals were included as time-invariant predictors. Other psychological variables were included as time-varying predictors, that is, changes in these variables measured over the study period were modeled. Time-varying predictors were person-mean centered at level 1 (time) and level 2 (person) of each model. The level 1 coefficient is the within-person effect of the predictor and the level 2 coefficient is the between-person effect.49 For example, significant positive coefficients of catastrophizing would be interpreted as follows: at level 1, increased catastrophizing in an individual (compared with their own personal average level of catastrophizing) is associated with increases in disability, when controlling for between-person differences in catastrophizing. At level 2, higher levels of catastrophizing overall (compared with the sample average level of catastrophizing) are associated with higher levels of disability compared with other people, when controlling for within-person changes in catastrophizing over time.
A series of multilevel models tested which psychological variables were independently associated with disability over time after controlling for clinical and sociodemographic characteristics that were significant in univariate analyses (Table 1, univariate models). First, a model including clinical and sociodemographic characteristics was specified to provide a nested comparison model for subsequent models (Table 1, multivariate model). Then, 4 separate models were specified to test whether each set of psychological variables (from each theoretical framework) was associated with disability and to identify, within each framework, which variables were independently associated with disability. The difference between the −2 log-likelihoods of nested models was used to test comparative fit.46 Finally, variables from all 4 theoretical frameworks were entered together to identify which psychological factors overall were independently associated with disability. For this model, plots of residuals against normal scores, participant ID, time, and pain confirmed that level 1 and level 2 residuals were approximately normally distributed and met assumptions of heteroscedasticity. These plots identified 4 possible outliers, but removing these participants did not alter the fixed-effects estimates.
Throughout, Wald statistics were used to evaluate the significance of individual variables. Pseudo-R2 statistics were calculated by computing and squaring the sample correlation between observed and predicted values of disability48 and are reported as an approximate indicator of the proportion of variance explained.
RESULTS
Clinical and Sociodemographic Characteristics, Pain, and Well-Being
In total, 1371 baseline questionnaires were distributed to participating acupuncturists, and completed baseline questionnaires were received from 524 patients; 39 were excluded for scoring <4 on the RMDQ, giving a final sample at baseline of 485. The majority of participants provided data at all 4 timepoints (n=326, 67%) and 420 (87%) provided data at baseline and at least 1 follow-up (Fig. 1). In logistic regression analyses, baseline disability levels did not predict dropout (β=0.003, SE=0.02). Age was the only characteristic that predicted dropout (β=0.05, SE=0.01): patients who dropped out were younger (M=48.03, SD=16.48) than those who did not (M=56.37, SD=14.22). Of the psychological variables measured at baseline, only timeline perceptions predicted dropout (β=0.14, SE=0.06): patients who dropped out believed their back pain would last less time (M=7.76, SD=2.13) than those who did not dropout (M=8.23, SD=1.97). To facilitate model comparison, the analyses reported below are conducted on the 420 participants who supplied data at baseline and at least 1 follow-up.
FIGURE 1.
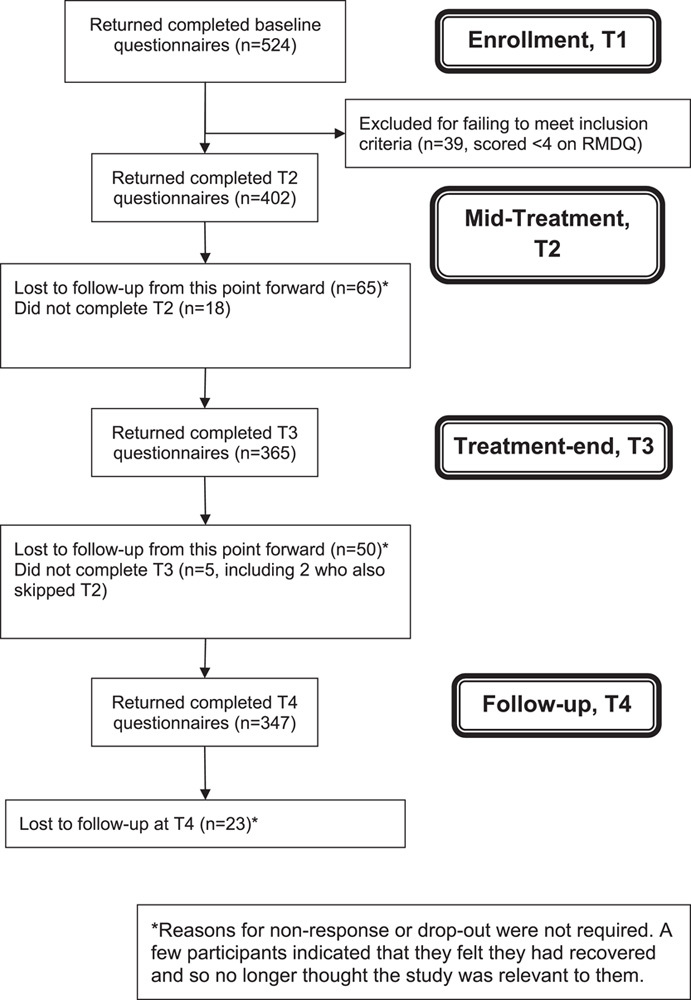
Flow diagram of participants through study. RMDQ indicates Roland Morris Disability Questionnaire.
Table 1 shows participants’ clinical and sociodemographic characteristics and the effects of these factors on disability. Characteristics that were significant univariate predictors of disability and were thus included as covariates in all subsequent models were: age, work status, LBP-related benefits status, LBP-related compensation status, reporting at least 1 comorbidity, reporting at least 1 cotreatment, duration of LBP, clinic type, and health care sector.
Fear-Avoidance Model
Participants had moderate levels of catastrophizing and fear-avoidance beliefs at baseline (Table 2). Mean levels of psychological symptoms fell just below (for depression) and just above (for anxiety) clinical cut-off points for medical patients.50
TABLE 2.
Fear-Avoidance Model: Baseline Values and Fixed Effects on Disability Over Time
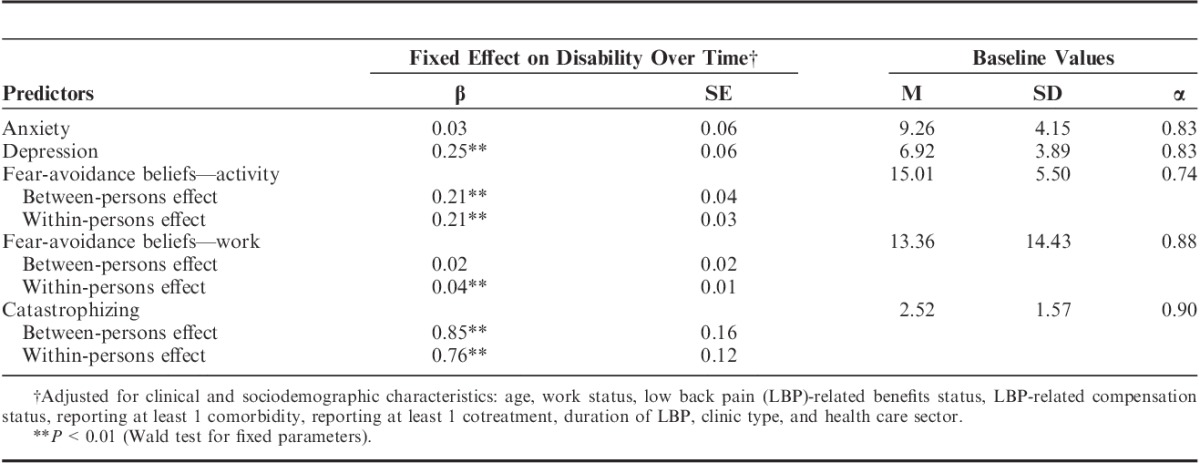
As a set, these variables significantly improved model fit χ2(8)=305.85, P<0.001, and explained an additional 20.93% of the variance in disability beyond that accounted for by clinical and sociodemographic characteristics. Within individuals over time, reductions in disability were associated with decreasing fear-avoidance beliefs about work and/or activity and decreasing catastrophizing. Between individuals, people who had lower levels of disability had lower levels of depression, catastrophizing, and fear-avoidance beliefs about activity.
Common-Sense Model
Participants had particularly strong concerns about their pain, thought it would last a long time, and appraised their acupuncturist positively (Table 3). Most commonly, participants attributed their back pain to work or other activities.
TABLE 3.
Common-Sense Model: Baseline Values and Effects on Disability Over Time
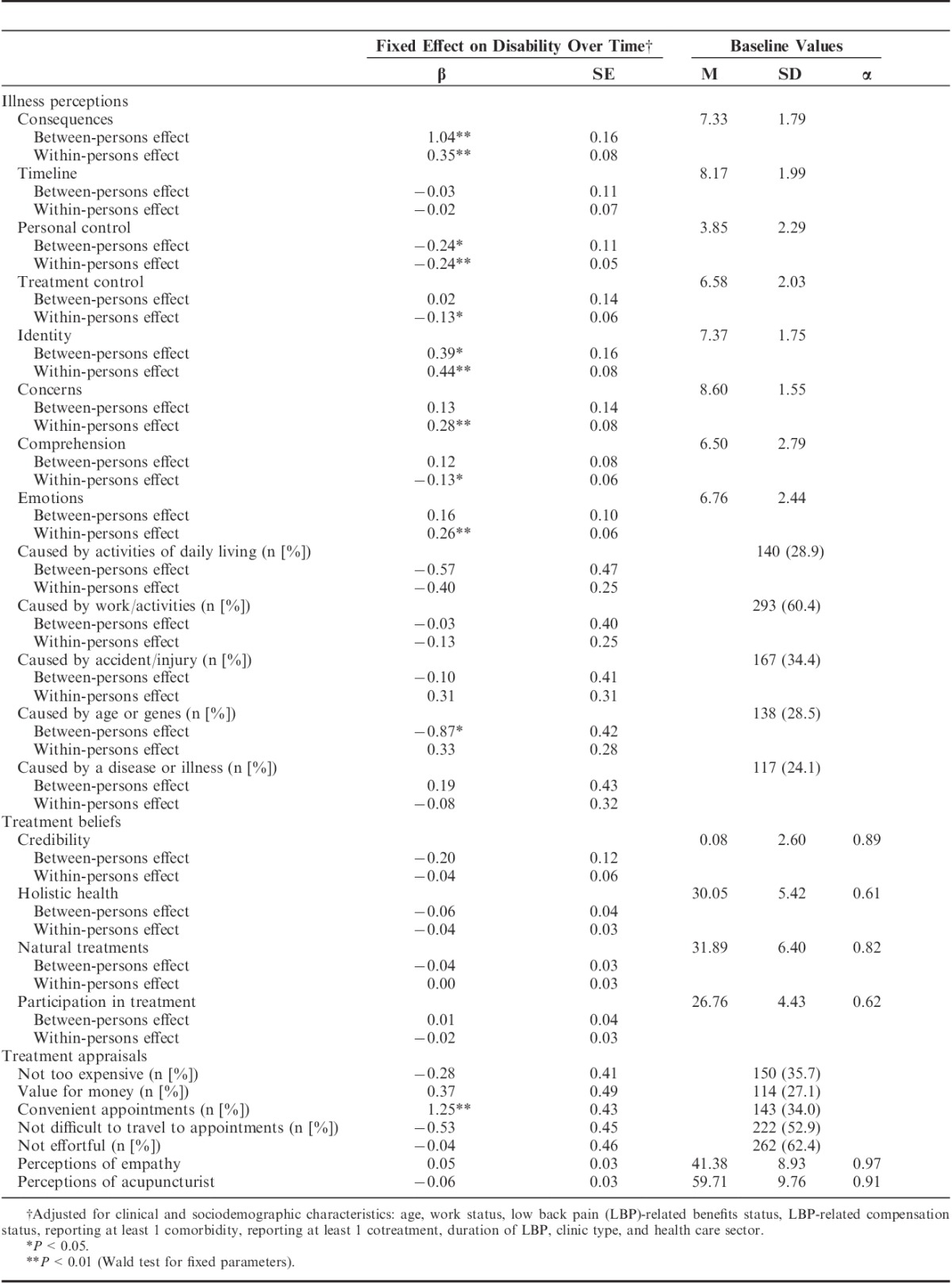
As a set, variables from the CSM significantly improved model fit χ2(41)=665.18, P<0.001, and explained an additional 33.76% of the variance in disability beyond that accounted for by clinical and sociodemographic characteristics. Within individuals, reductions in disability were associated with adaptive changes in illness perceptions: increasing perceptions of control over back pain (both personal control and treatment control); improving sense of understanding back pain; associating fewer symptoms with back pain; being less concerned about back pain; perceiving fewer severe consequences of back pain; and associating fewer emotions with back pain. Between individuals, people who had lower levels of disability: attributed back pain to aging or hereditary factors, perceived LBP as less threatening (less severe consequences, more personal control, fewer associated symptoms), and appraised appointments as inconvenient.
Expectancy Theory
When added to the model with clinical and sociodemographic characteristics, expectancies significantly improved model fit χ2(2)=59.21, P<0.001, and explained an additional 5.12% of the variance in disability. Within individuals, reductions in disability were associated with increasingly positive expectancies (β=−0.38, SE=0.06, P<0.01). Between individuals, people who had lower levels of disability had more positive expectancies (β=−0.43, SE=0.09, P<0.01).
Social-Cognitive Theory
At baseline, participants had moderate levels of self-efficacy for coping (M=52.23, SD=18.78). Adding self-efficacy significantly improved model fit χ2(2)=275.88, P<0.01, and explained an additional 18.90% of the variance in disability beyond that explained by clinical and sociodemographic characteristics. Within individuals, reductions in disability were associated with increasing self-efficacy (β=−0.10, SE=0.01, P<0.01). Between individuals, people with lower levels of disability had higher self-efficacy (β=−0.15, SE=0.01, P<0.01).
Combined Model
When predictors from all the theoretical frameworks were modeled simultaneously, variables from the FAM, CSM, expectancy theory, and SCT were independently associated with disability after controlling for clinical and sociodemographic characteristics (Table 4). Within individuals, reductions in disability were associated with: decreasing catastrophizing and fear-avoidance beliefs about activity and work; increasing personal control over and understanding of back pain and perceiving fewer symptoms, concerns, consequences, and emotions associated with back pain; and increasing self-efficacy. Between individuals, people with lower levels of disability had lower levels of depression and fear-avoidance beliefs about activity; perceived less severe consequences of back pain and greater treatment control over back pain, perceived their back pain was caused by activities of daily living, and appraised appointments as inconvenient; had higher expectancies; and had higher levels of self-efficacy. Overall, adding these psychological variables significantly improved model fit χ2(53)=793.47, P<0.01, and explained an additional 38.16% of the variance in disability beyond that explained by clinical and sociodemographic characteristics. This final multilevel model incorporating variables from all 4 theoretical frameworks accounted for approximately 64% of the variance in disability.
TABLE 4.
Effects of Variables From 4 Theoretical Frameworks on Disability Over Time
Exploring Causality
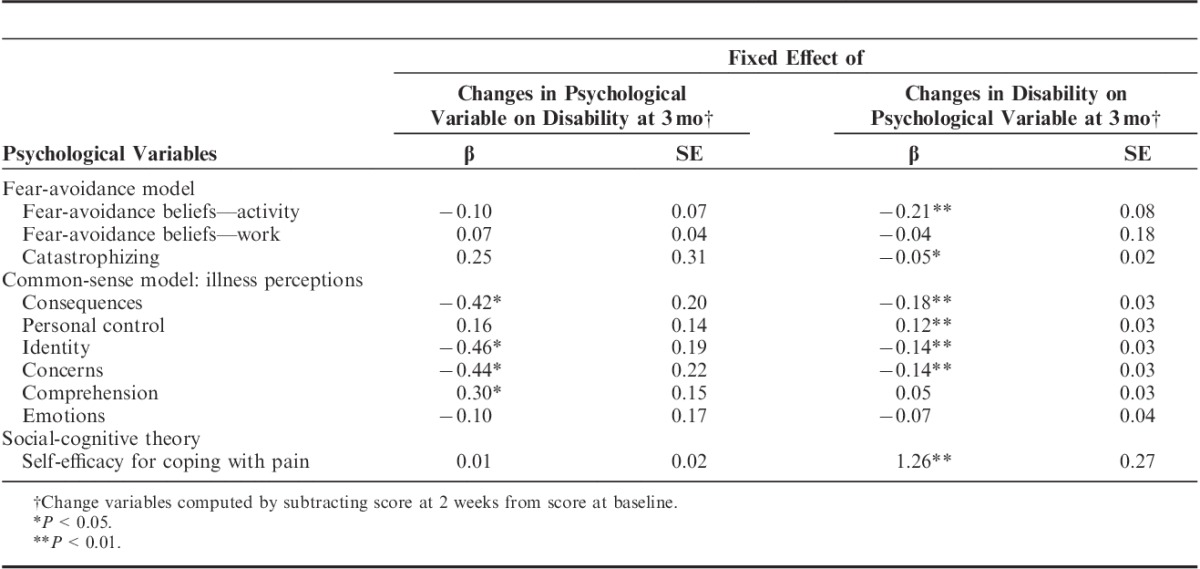
For each psychological variable that had a significant within-person effect on disability in the combined model, the direction of causality was explored. Table 5 shows the β-coefficients of models in which (1) disability scores at 3 months were regressed on changes in psychological variables from baseline to 2 weeks; and (2) scores on psychological variables at 3 months were regressed on changes in disability from baseline to 2 weeks. Changes in disability early in treatment predicted fear-avoidance, catastrophizing, self-efficacy, and perceptions of personal control at 3 months but not vice versa. Increased understanding of back pain early in treatment predicted disability at 3 months but not vice versa. Other illness perceptions (consequences, identity, and concerns) had reciprocal relationships with disability: early changes in illness perceptions predicted disability at 3 months and early changes in disability predicted illness perceptions at 3 months.
TABLE 5.
Exploring Causality Between Psychological Variables and Disability
DISCUSSION
As hypothesized, variables derived from expectancy theory, FAM, CSM, and SCT were associated with changes in disability among back pain patients receiving acupuncture. The final model showed that variables from these theoretical frameworks had independent effects and, together with clinical and socio-demographic characteristics, accounted for two thirds of the variance in disability.
Within-individual reductions in disability were consistently associated with decreases in: fear-avoidance beliefs about physical activity and work; catastrophizing; perceived symptoms associated with LBP; concerns about LBP; perceived consequences of LBP; and emotions associated with LBP. Within-individual reductions in disability were consistently associated with increases in: perceived personal control over LBP; perceived comprehension of LBP; and self-efficacy for coping with LBP. Further analysis suggested that changes in fear-avoidance beliefs and self-efficacy for coping may be epiphenomenal and occur after changes in disability, although it is possible that our measurement points were too far apart in time to capture what might be a very close reciprocal relationship between changes in fear-avoidance beliefs, self-efficacy, and disability. Changes in illness perceptions appeared to both lead to and result from changes in disability, which is consistent with the idea that illness perceptions evolve over time and patients’ perceptions of their symptoms influence their concrete experiences of therapy which in turn can feedback and modify their illness perceptions.19,51 The results of this study suggest that illness perceptions appear to be mediators of changes in disability over the course of acupuncture treatment and they could be deliberately targeted clinically to enhance acupuncture’s effectiveness.
Variables that only had a between-person effect are possible moderators of changes in disability over the course of acupuncture treatment. People who had lower levels of disability appraised appointments as inconvenient and had higher outcome expectancies. Appraisals were measured after 2 weeks of treatment and so it might be that people who were less disabled early in treatment were less motivated to attend appointments and so appraised them as inconvenient. Having low expectations of benefit might be a marker for acupuncture patients at high risk of relatively poor outcome.
The findings have implications for how we theorize disability in patients with LBP undergoing treatment. Each of our models explained some of the variance in changes in disability over time; conceptually, the theories provide somewhat complementary but at times overlapping insights. The fear-avoidance model11 focuses on emotional representations, whereas the common-sense model14 better elaborates cognitive illness representations. Self-efficacy for coping overlaps conceptually with perceptions of personal control from the common-sense model. Both the extended CSM19,20 and expectancy theory24 emphasize treatment cognitions, which in this study distinguished between people who also reported different levels of disability but were rarely associated with individual changes in disability. Although no single theoretical framework provided a complete account of the psychological factors involved in disability, we found that changes in illness perceptions were the most likely to be causally related to improvements in LBP-related disability over time, at least during acupuncture treatment. Given that psychological theories implicitly focus on within-person processes, analytic techniques to distinguish within and between-person effects (such as those used here) could inform further theoretical development.
Other studies have looked at smaller subsets of the variables we investigated in different settings. In 1 RCT of physical therapy and CBT for chronic back pain, expectancy predicted disability and satisfaction with treatment, whereas credibility predicted symptoms and satisfaction.52 In a mixed cohort of patients with neck and/or back pain, fear-avoidance beliefs, negative affect, and expecting pain to persist (similar to timeline beliefs) all independently predicted disability.53 Cross-sectional studies show that self-efficacy is a stronger mediator between pain and disability and a stronger correlate of disability than fear-avoidance variables in chronic and acute pain.54,55 A longitudinal study in primary care reported that changes in self-efficacy, but not fear-avoidance beliefs, mediated the relationship between pain and disability.56 Fewer studies have investigated the common-sense model. Foster et al,33 investigated fear-avoidance variables, self-efficacy, and illness perceptions (but not other components, ie, treatment beliefs and appraisals) in a primary care LBP cohort. The significant independent predictors of disability were identity beliefs (perceived symptoms), personal control beliefs, timeline beliefs, and pain self-efficacy; fear-avoidance variables tended to be weaker predictors.33 The present study contributes to this evidence that self-efficacy and illness perceptions in particular can usefully supplement variables from the fear-avoidance model in advancing our understanding of back pain-related disability and suggests that these variables are relevant in acupuncture as well as conventional treatment settings. A single study of people receiving different LBP therapies is needed to compare the relative importance of psychological variables across various therapeutic modalities and clinical settings.
The findings also have implications for understanding acupuncture’s large nonspecific effects6 and, more generally, for understanding the processes whereby acupuncture may result in decreased disability. Given that similar variables predict disability in other settings, patients’ perceptions of pain and self-efficacy could be influencing disability outcomes in patients receiving both real and sham acupuncture in clinical trials. These psychological variables offer one means by which major components of acupuncture as a complex intervention, such as ritual,57 the therapeutic relationship,22 and lifestyle advice,58 could trigger positive clinical outcomes. In the context of a warm relationship and therapeutic ritual, providing positive self-help advice encouraging physical activity could help patients to develop more positive illness perceptions, confront their fear of activities and become more active, breaking the negative cycle proposed in the fear-avoidance model11 and triggering a more positive perception of back pain as controllable and enabling an increasing sense of self-efficacy for coping. According to social-cognitive theory, enhanced self-efficacy for coping could then trigger a positive feedback loop increasing actual coping ability30 and reducing disability.
Expectancies were associated with disability between-persons but not within-persons. Previous acupuncture studies are inconsistent28,29 but the placebo literature strongly suggests that enhancing expectancies can generate placebo analgesia.24 Perhaps, and consistent with the present results, expectancy might have an indirect effect mediated by pain perceptions: positive response expectancy might help to reduce perceptions of pain as threatening and thus facilitate the development of more adaptive pain perceptions and coping behaviors.
Treatment beliefs and appraisals of the acupuncturist were consistently weakly associated with disability. Previous studies found treatment beliefs and perceived empathy were related to adherence40 and enablement.21 Treatment beliefs and appraisals might be more important for such proximal outcomes than for distal outcomes like disability. The measure of treatment beliefs used in this study may have been too general as it assessed beliefs about complementary therapies rather than acupuncture in particular.
The generalizability of the findings is enhanced by the large cohort of back pain patients receiving acupuncture in usual care and the limited exclusion criteria. However, the representativeness of the sample is difficult to assess. Compared with a national (UK) survey of acupuncture users with various conditions,3 participants were similar in age (51 y) and sex (68% vs. 74% females) but fewer had previous acupuncture experience (42% vs. 87%) and more used acupuncture in the National Health Servic (63% vs. 5%). Compared with a large cohort of primary care LBP patients,17 participants were older (51 vs. 44 y), more disabled at baseline (mean RMDQ 13.4 vs. 8.6), and more were female (68% vs. 59%). Although some participants were lost to follow-up, attrition was not associated with disability. Compared with other acupuncture studies, a large and theoretically grounded set of confounders and predictors were measured. A smaller selection of predictors could be used in future but should include illness perceptions (most likely to prospectively predict within-person changes), self-efficacy, and expectancy (for between-person differences).
In conclusion, cognitive and emotional pain perceptions and self-efficacy for coping with pain are associated with changes in disability over the course of acupuncture for LBP. Changes in illness perceptions may predict subsequent disability, whereas changes in disability appear to predict subsequent self-efficacy and fear-avoidance beliefs. Self-efficacy and, in particular, illness perceptions can usefully supplement variables from the fear-avoidance model in advancing our understanding of back pain-related disability. Acupuncture patients experience less back-related disability when they are less afraid and avoidant of physical activity and work, perceive fewer symptoms emotions and consequences of LBP, perceive their LBP as less threatening, and when they feel greater control over, understanding of, and ability to cope with their back pain. Future studies should test whether integrating acupuncture and psychological interventions targeting these constructs can enhance patient outcomes.
Supplementary Material
ACKNOWLEDGMENTS
The authors are grateful to the Primary Care Research Network, the Acupuncture Association of Chartered Physiotherapists, and British Acupuncture Council, and the British Medical Acupuncture Society for help recruiting acupuncturists. They are grateful to the acupuncturists for recruiting our participants and to the participants for completing the questionnaires. They thank Jane Cousins, Naomi Guppy, and Gemma Fitzsimmons; (School of Medicine, University of Southampton, Southampton, UK) for administrative support.
Footnotes
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Website, www.clinicalpain.com.
Supported by Arthritis Research UK (Career Development Fellowship 18099), Chesterfield, UK. G.T.L.’s post is supported by a grant from the Rufford Maurice Laing Foundation. The remaining authors declare no conflict of interest.
REFERENCES
- 1.Breivik H, Collett B, Ventafridda V, et al. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287–333. [DOI] [PubMed] [Google Scholar]
- 2.Savigny P, Kuntze S, Watson P, et al. Low Back Pain. Early Management of Persistent Non-Specific Low Back Pain. NICE Clinical Guideline. 2009:88 edLondon: National Collaborating Centre for Primary Care and Royal College of General Practitioners; Available at: http://www.nice.org.uk/CG88. [PubMed] [Google Scholar]
- 3.MacPherson H, Sinclair-Lian N, Thomas K. Patients seeking care from acupuncture practitioners in the UK: a national survey. Complement Ther Med. 2006;14:20–30. [DOI] [PubMed] [Google Scholar]
- 4.Brinkhaus B, Witt CM, Jena S, et al. Acupuncture in patients with chronic low back pain—a randomized controlled trial. Arch Intern Med. 2006;166:450–457. [DOI] [PubMed] [Google Scholar]
- 5.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med. 2012;172:1444–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Linde K, Niemann K, Schneider A, et al. How large are the nonspecific effects of acupuncture? A meta-analysis of randomized controlled trials. BMC Med. 2010;8:75.doi:10.1186/1741-7015-8-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ. 2005;330:1202–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacPherson H, Thorpe L, Thomas K. Beyond needling—therapeutic processes in acupuncture care: a qualitative study nested within a low-back pain trial. J Altern Complement Med. 2006;12:873–880. [DOI] [PubMed] [Google Scholar]
- 9.Paterson C, Evans M, Bertschlinger R, et al. Communication about self-care in traditional acupuncture consultations: the co-construction of individualised support and advice. Patient Educ Couns. 2012;89:467–475. [DOI] [PubMed] [Google Scholar]
- 10.Rugg S, Paterson C, Britten N, et al. Traditional acupuncture for people with medically unexplained symptoms: a longitudinal qualitative study of patients’ experiences. Br J Gen Pract. 2011;61:e306–e315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vlaeyen JWS, Linton SJ. Fear-avoidance and its consequences in chronic musculoskeletal pain: a state of the art. Pain. 2000;85:317–332. [DOI] [PubMed] [Google Scholar]
- 12.Leeuw M, Goossens MEJB, Linton SJ, et al. The fear-avoidance model of musculoskeletal pain: current state of scientific evidence. J Behav Med. 2007;30:77–94. [DOI] [PubMed] [Google Scholar]
- 13.Bailey KM, Carleton RN, Vlaeyen JWS, et al. Treatments addressing pain-related fear and anxiety in patients with chronic musculoskeletal pain: a preliminary review. Cogn Behav Ther. 2009;39:46–63. [DOI] [PubMed] [Google Scholar]
- 14.Leventhal HA, Brissette I, Leventhal EA.Cameron LD, Leventhal H. The common-sense model of self-regulation of health and illness. The Self-Regulation of Health and Illness Behaviour. 2003London: Routledge;42–65. [Google Scholar]
- 15.Hagger MS, Orbell S. A meta-analytic review of the common-sense model of illness representations. Psychol Health. 2003;18:141–184. [Google Scholar]
- 16.Nicklas LB, Dunbar M, Wild M. Adherence to pharmacological treatment of non-malignant chronic pain: the role of illness perceptions and medication beliefs. Psychol Health. 2009;25:601–615. [DOI] [PubMed] [Google Scholar]
- 17.Foster NE, Bishop A, Thomas E, et al. Illness perceptions of low back pain patients in primary care: what are they, do they change and are they associated with outcome? Pain. 2008;136:177–187. [DOI] [PubMed] [Google Scholar]
- 18.Glattacker M, Heyduck K, Meffert C. Illness beliefs, treatment beliefs and information needs as starting points for patient information—evaluation of an intervention for patients with chronic back pain. Patient Educ Couns. 2012;86:378–389. [DOI] [PubMed] [Google Scholar]
- 19.Yardley L, Sharples K, Beech S, et al. Developing a dynamic model of treatment perceptions. J Health Psychol. 2001;6:269–282. [DOI] [PubMed] [Google Scholar]
- 20.Horne R, Weinman J. Self-regulation and self-management in asthma: exploring the role of illness perceptions and treatment beliefs in explaining non-adherence to preventer medication. Psychol Health. 2002;17:17–32. [Google Scholar]
- 21.Price S, Mercer SW, MacPherson H. Practitioner empathy, patient enablement and health outcomes: a prospective study of acupuncture patients. Patient Educ Couns. 2006;63:239–245. [DOI] [PubMed] [Google Scholar]
- 22.Kaptchuk TJ, Kelley JM, Conboy LA, et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ. 2008;336:999–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White P, Bishop FL, Prescott P, et al. Practice, practitioner or placebo? A multifactorial, mixed methods randomized controlled trial of acupuncture. Pain. 2012;153:455–462. [DOI] [PubMed] [Google Scholar]
- 24.Kirsch I. Response expectancy theory and application: a decennial review. Appl Prev Psychol. 1997;6:69–79. [Google Scholar]
- 25.Kalauokalani D, Cherkin DC, Sherman KJ, et al. Lessons from a trial of acupuncture and massage for low back pain. Spine. 2001;26:1418–1424. [DOI] [PubMed] [Google Scholar]
- 26.Linde K, Witt CM, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128:264–271. [DOI] [PubMed] [Google Scholar]
- 27.Suarez-Almazor ME, Looney C, Liu Y, et al. A randomized controlled trial of acupuncture for osteoarthritis of the knee: effects of patient-provider communication. Arthritis Care Res. 2010;62:1229–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sherman KJ, Cherkin DC, Ichikawa L, et al. Treatment expectations and preferences as predictors of outcome of acupuncture for chronic back pain. Spine. 2010;35:1471–1477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Colagiuri B, Smith CA. A systematic review of the effect of expectancy on treatment responses to acupuncture. eCAM. 2012doi:10.1155/2012/857804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bandura A. Self-Efficacy. The Exercise of Control. 1997New York: W.H. Freeman and Company. [Google Scholar]
- 31.Bandura A. Social cognitive theory of self-regulation. Organ Behav Hum Dec. 1991;50:248–287. [Google Scholar]
- 32.Schwarzer R, Fuchs R.Conner M, Norman P. Self-efficacy and health behaviours. Predicting Health Behaviour: Research and Practice With Social Cognition Models. 1995Buckingham: Open University Press;163–196. [Google Scholar]
- 33.Foster NE, Thomas E, Bishop A, et al. Distinctiveness of psychological obstacles to recovery in low back pain patients in primary care. Pain. 2010;148:398–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–144. [DOI] [PubMed] [Google Scholar]
- 35.Rosentiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. [DOI] [PubMed] [Google Scholar]
- 36.Waddell G, Newton M, Henderson I, et al. A fear-avoidance beliefs questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993;52:157–168. [DOI] [PubMed] [Google Scholar]
- 37.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–370. [DOI] [PubMed] [Google Scholar]
- 38.Broadbent E, Petrie KJ, Main J, et al. The Brief Illness Perception Questionnaire. J Psychosom Res. 2006;60:631–637. [DOI] [PubMed] [Google Scholar]
- 39.Bishop FL, Yardley L, Lewith G. Developing a measure of treatment beliefs: the Complementary and Alternative Medicine Beliefs Inventory. Complement Ther Med. 2005;13:144–149. [DOI] [PubMed] [Google Scholar]
- 40.Bishop FL, Yardley L, Lewith GT. Treatment appraisals and beliefs predict adherence to complementary therapies: a prospective study using a dynamic extended self-regulation model. Br J Health Psychol. 2008;13:701–718. [DOI] [PubMed] [Google Scholar]
- 41.Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. J Behav Ther Exp Psychiatry. 2000;31:73–86. [DOI] [PubMed] [Google Scholar]
- 42.Mercer SW, Maxwell M, Heaney D, et al. The development and preliminary validation of the Consultation and Relational Empathy (CARE) measure: an empathy-based consultation process measure. Fam Pract. 2004;21:699–705. [DOI] [PubMed] [Google Scholar]
- 43.Anderson KO, Dowds BN, Pelletz RE, et al. Development and initial validation of a scale to measure self-efficacy beliefs in patients with chronic pain. Pain. 1995;63:77–83. [DOI] [PubMed] [Google Scholar]
- 44.Edwards P, Roberts I, Clarke M, et al. Increasing response rates to postal questionnaires: systematic review. BMJ. 2002;324:1183–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 2001Boston: Allyn and Bacon. [Google Scholar]
- 46.Twisk JWR. Applied Longitudinal Data Analysis for Epidemiology. 2003Cambridge: Cambridge University Press. [Google Scholar]
- 47.Rasbash J, Charlton C, Browne WJ, et al. MLwiN Version 2.1. 2009University of Bristol: Centre for Multilevel Modelling. [Google Scholar]
- 48.Singer JD, Willett JB. Applied Longitudinal Data Analysis. 2003Oxford: Oxford University Press. [Google Scholar]
- 49.Hoffman L, Stawski RS. Persons as contexts: evaluating between-person and within-person effects in longitudinal analysis. Res Hum Dev. 2009;6:97–120. [Google Scholar]
- 50.Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52:69–77. [DOI] [PubMed] [Google Scholar]
- 51.Leventhal H, Leventhal EA, Contrada RJ. Self-regulation, health, and behavior: a perceptual-cognitive approach. Psychol Health. 1998;13:717–733. [Google Scholar]
- 52.Smeets RJEM, Beelen S, Goossens MEJB, et al. Treatment expectancy and credibility are associated with the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. Clin J Pain. 2008;24:305–315. [DOI] [PubMed] [Google Scholar]
- 53.Boersma K, Linton SJ. Expectancy, fear and pain in the prediction of chronic pain and disability: a prospective analysis. Eur J Pain. 2006;10:551–557. [DOI] [PubMed] [Google Scholar]
- 54.Woby SR, Urmston M, Watson PJ. Self-efficacy mediates the relation between pain-related fear and outcome in chronic low back pain patients. Eur J Pain. 2007;11:711–718. [DOI] [PubMed] [Google Scholar]
- 55.Söderlund A, Åsenlöf P. The mediating role of self-efficacy expectations and fear of movement and (re)injury beliefs in two samples of acute pain. Disabil Rehabil. 2010;32:2118–2126. [DOI] [PubMed] [Google Scholar]
- 56.Costa Ld, Maher CG, McAuley JH, et al. Self-efficacy is more important than fear of movement in mediating the relationship between pain and disability in chronic low back pain. Eur J Pain. 2011;15:213–219. [DOI] [PubMed] [Google Scholar]
- 57.Kaptchuk TJ. The placebo effect in alternative medicine: can the performance of a healing ritual have clinical significance? Ann Intern Med. 2002;136:817–825. [DOI] [PubMed] [Google Scholar]
- 58.MacPherson H, Thomas K. Self-help advice as a process integral to traditional acupuncture care: implications for trial design. Complement Ther Med. 2008;16:101–106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


