Supplemental Digital Content is available in the text.
Abstract
Background:
Cross-sectional analyses of national data have found that persons with high baseline body mass index (BMI) gain weight faster than persons at the median and that those whose weight was below the median gain very little weight. However, it is not clear whether these population-level changes reflect patterns at the individual level.
Methods:
We examined longitudinal changes in BMI in initially underweight, normal-weight, overweight, and obese US men and women using individual-level repeat data from the Health and Retirement Study (n = 15,895; age range, 40–69 years at baseline). Linear mixed-effect regression was used to model 6-year change in self-reported BMI during 4 study periods (1992/1994–1998/2000, 1996/1998–2002/2004, 2000/2002–2006/2008, and 2004–2010).
Results:
In the first 6-year period, the mean increase in BMI was greatest among persons who were initially normal weight (0.3 kg/m2 [95% confidence interval = 0.2 to 0.4]) and overweight (0.2 kg/m2 [0.1 to 0.3]). Weight gain accelerated in these groups with each subsequent period. Weight gain was less for initially class-I obese participants, and a net decrease in BMI was observed for class-III obese participants.
Conclusion:
These analyses suggest that the change in mean BMI among middle-aged and older US adults between 1992 and 2010 resulted mainly from accelerated weight gain among persons who were initially normal weight and overweight.
Over the past 4 decades, the United States and many other countries have seen a dramatic increase in the mean level of body mass index (BMI).1 According to the most recent National Health and Nutrition Examination Surveys, more than two thirds of US adults are overweight or obese.2 Previous research based on cross-sectional surveys has shown that at the population level, the patterns of weight gain have differed markedly by initial BMI, with person of higher BMI gaining weight at an increased rate relative to the median and very little weight gain occurring among those whose baseline weight was below the median.3–5 However, changes in the BMI distribution of population may differ from individual-level changes.
In this study, we used individual-level longitudinal data from the US Health and Retirement Study to examine the change in self-reported BMI among initially normal-weight, overweight, and obese middle-aged and older US adults. Our aim was to determine whether there were dissimilarities in weight change depending on the persons’ initial BMI categories.
METHODS
Participants
The target population of the Health and Retirement Study is a representative sample of approximately 26,000 Americans.6 The first cohort was interviewed in 1992. Between 1994 and 2010, 5 additional cohorts were included. Ethical approval was obtained from the University of Michigan Institutional Review Board.
In the present longitudinal analysis, we used data from 1992 to 2010. The following four 6-year study periods were defined: from 1992/1994 to 1998/2000, from 1996/1998 to 2002/2004, from 2000/2002 to 2006/2008, and from 2004 to 2010. We included participants aged 40–69 years at the baseline of each period and with no missing data for BMI during the 6-year period. Thus, participants could contribute to one or more of the 4 study periods. The total study population was 15,895 men and women with 38,760 BMI measurements from an average of 2.5 periods from repeated data collections.
Measurements
The BMI was calculated on the basis of self-reported weight and height. Our outcome was the 6-year change in self-reported BMI calculated across 4 BMI measurements during each 6-year period for each participant. Baseline BMI was defined as the average of the participants’ first and second BMI measurements (rather than the first measurement alone), to reduce bias due to regression to the mean (a tendency of extreme values in the first measurement to be followed by measurements closer to the mean).7 Participants were divided into 6 groups at the baseline of each study period: underweight (BMI, <18.5 kg/m2), normal weight (BMI, 18.5–24.9 kg/m2), overweight (BMI, 25–29.9 kg/m2), class-I obesity (BMI, 30–34.9 kg/m2), class-II obesity (BMI, 35–39.9 kg/m2), and class-III obesity (BMI, ≥40 kg/m2).8 Baseline covariates were age (40–49, 50–59, and 60–69 years), ethnicity (white, black/African American, and other), and education (low, lower than high school; medium, high school or some college; and high, college and higher).
Statistical Analysis
We report the characteristics of the study population at baseline for each period as mean values for continuous variables and as proportions for categorical variables. The outcome measure was the 6-year change in self-reported BMI calculated as a slope from the linear regression analysis obtained from 4 BMI measurements from the participants during each 6-year period. For people who participated in more than 1 study period, the 6-year trend was calculated separately for all the available study periods. To take into account correlation among the repeated observations within an individual, we applied linear mixed-effect regression models in examining the differences in BMI change across the baseline BMI categories and periods with an interaction term of baseline BMI × period and their main effects included in the model.9 We also examined whether there were differences according to age, sex, and race by including BMI × period × age/sex/race interaction terms in the model. Adjusted mean estimates were calculated to represent the average change in BMI in each baseline BMI category and study period. All of the models were adjusted for age, sex, ethnicity, and education. The SAS 9.3 Statistical Package was used for all of the analyses (SAS Institute Inc., Cary, NC).
RESULTS
The Table shows the baseline characteristics of the study population at the beginning of each study period. The mean 6-year change in BMI, adjusted for age, sex, ethnicity, and education, for each baseline BMI category according to study period is shown in the Figure. The weight gain in the normal-weight, overweight, and class-I obese groups accelerated with each subsequent period (test for trend, P < 0.001). The mean increase in BMI was greatest among the initially normal-weight participants (0.3 kg/m2 [95% confidence interval (CI) = 0.2 to 0.4] in the first 6-year period and 0.5 kg/m2 [0.4 to 0.6] in the last 6-year period) and among the initially overweight (0.2 kg/m2 [0.1 to 0.3] in the first and 0.6 kg/m2 [0.5 to 0.7] in the last period). Weight gain was less for initially class-I obese participants (0.00 kg/m2 [−0.2 to 0.2] in the first and 0.4 kg/m2 [0.2 to 0.5] in the last period). A net decrease in BMI was observed for initially class-III obese participants. Mean BMI change across study periods confirms this general pattern and is in contrast to cross-sectional population-level analyses, which shows a relative small increase in BMI among persons in the lower segments of the baseline BMI distribution but a large increase in the upper segments (eFigure 1B, http://links.lww.com/EDE/A863). There were no appreciable differences in how weight changed by initial BMI status across age, sex, or race groups (eTable 1, http://links.lww.com/EDE/A863).
TABLE.
Baseline Characteristics of the Study Participants According to the Study Periods—The Health and Retirement Study
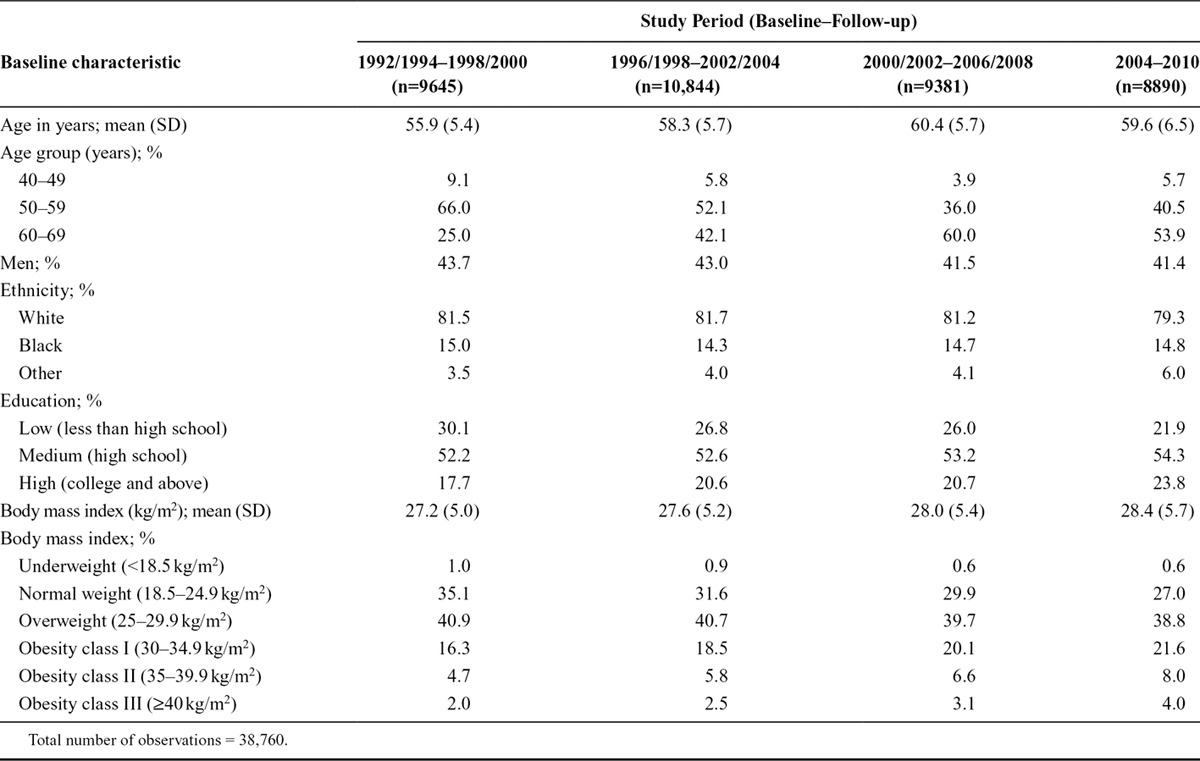
FIGURE.
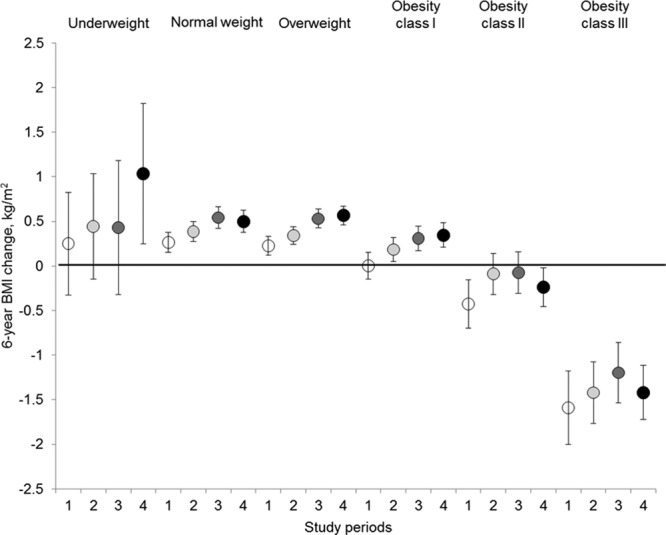
Six-year change in BMI according to baseline BMI category and study period. Results shown as mean estimates adjusted for age, sex, ethnicity, and education. Baseline BMI category was defined as an average of the participants’ first and second BMI measurements. The 6-year change in BMI was calculated as a 6-year slope from the linear regression analysis including all 4 BMI measurements from the participants during the 6-year period. Period 1: 1992/1994–1998/2000; Period 2: 1996/1998–2002/2004; Period 3: 2000/2002–2006/2008; Period 4: 2004–2010.
DISCUSSION
Our analysis of individual-level data from the US Health and Retirement Study extends previous research on BMI trends at the population and individual levels.3–5,10–13 The longitudinal within-participant analyses showed that weight gain increased the most among the underweight, normal weight, overweight, and class-I obese and that these groups accelerated with each subsequent period. By contrast, the proportion of participants losing weight was the highest in the obese categories, leading to a net reduction in BMI among persons in the baseline class-III obese category.
The accelerated weight gain among normal-weight and overweight persons has also been reported in previous study examining long-term trajectories of BMI,11,14 but those studies have not focused on differences between initial BMI categories. It is possible that the observed increase in body weight reflects secular changes in obesogenic environments, which affect certain groups disproportionally.11,12 These could include changes in the food environment, physically inactive lifestyles, and the rise in environmental endocrine disrupting chemicals.10,15,16 As the effects of environmental factors on body weight may take time to accumulate, the current results may not reflect the impacts of the most recent environment or obesity policies.
The reasons for the observed weight loss among severely obese participants are unknown. Interventions of conservative weight management by means of diet and physical exercise may have contributed to this weight loss, although they have shown disappointing outcomes in the long run.17,18 Unintentional weight loss is another plausible explanation as several chronic diseases, including those particularly common among the obese (eg, type-2 diabetes, cardiovascular diseases, and cancer), can lead to weight loss.19,20 Supporting this possibility, the greatest weight losses were observed among those with the most severe forms of obesity and the highest prevalence of chronic diseases. Bariatric surgery is increasingly used to promote weight loss and manage obesity-related comorbidities among morbidly obese patients; thus, it may partly explain our findings.
The statistical phenomenon of regression to the mean operates in repeated measurement data. We sought to overcome this issue by using the participants’ first and second BMI measurements (instead of the first measurement only) to define the baseline BMI category.15 Furthermore, the use of all 4 BMI measurements per period to calculate the 6-year change with linear regression analyses is less affected by regression to the mean than the use of only the first and last measurements. Previous studies suggest that overweight persons tend to underreport, and underweight persons to overreport, their weight21–24; this underestimation of self-reported weight may have increased over time, leading to an increase in underestimation of BMI. Thus, the observed mean weight loss in obese persons may be partially attributable to changes in self-reporting in addition to real weight changes.25
The results of this study suggest that, in addition to paying attention to obese people who are already at a high risk of developing chronic diseases, programs to prevent weight gain among normal-weight and overweight people are needed.
Footnotes
Supported by the European Union’s Era-Age 2 program (Academy of Finland [264944] and the Swedish Research Council for Health, Working Life and Welfare [Forte, 2012-1661]).
Sari Stenholm is supported by the Academy of Finland (273850). Mika Kivimäki is supported by the UK Medical Research Council (K013351), the National Heart, Lung and Blood Institute (HL36310), the National Institute of Aging (AG034454), and a professorial fellowship from the Economic and Social Research Council. The other authors have no conflicts to report.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com). This content is not peer-reviewed or copy-edited; it is the sole responsibility of the author.
REFERENCES
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Razak F, Corsi DJ, Subramanian SV. Change in the body mass index distribution for women: analysis of surveys from 37 low- and middle-income countries. PLoS Med. 2013;10:e1001367. doi: 10.1371/journal.pmed.1001367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wardle J, Boniface D. Changes in the distributions of body mass index and waist circumference in English adults, 1993/1994 to 2002/2003. Int J Obes (Lond) 2008;32:527–532. doi: 10.1038/sj.ijo.0803740. [DOI] [PubMed] [Google Scholar]
- 5.Beydoun MA, Wang Y. Gender-ethnic disparity in BMI and waist circumference distribution shifts in US adults. Obesity (Silver Spring) 2009;17:169–176. doi: 10.1038/oby.2008.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Growing Older in America: The Health and Retirement Study. 2014. Available at http://hrsonline.isr.umich.edu/index.php?p=dbook. September 10. [Google Scholar]
- 7.Barnett AG, van der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol. 2005;34:215–220. doi: 10.1093/ije/dyh299. [DOI] [PubMed] [Google Scholar]
- 8.National Institutes of Health, National Heart Lung, and Blood Institute. The Practical Guide: Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. NIH Publication No. 00-4084. Bethesda, Md.: National Institutes of Health, National Heart Lung, and Blood Institute; 2000. [Google Scholar]
- 9.Goldstein H. Multilevel Statistical Models. 3rd ed. London: Edward Arnold; 2003. [Google Scholar]
- 10.Botoseneanu A, Liang J. The effect of stability and change in health behaviors on trajectories of body mass index in older Americans: a 14-year longitudinal study. J Gerontol A Biol Sci Med Sci. 2012;67:1075–1084. doi: 10.1093/gerona/gls073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Botoseneanu A, Liang J. Latent heterogeneity in long-term trajectories of body mass index in older adults. J Aging Health. 2013;25:342–363. doi: 10.1177/0898264312468593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clarke P, O’Malley PM, Johnston LD, Schulenberg JE. Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986-2004. Int J Epidemiol. 2009;38:499–509. doi: 10.1093/ije/dyn214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dugravot A, Sabia S, Stringhini S, et al. Do socioeconomic factors shape weight and obesity trajectories over the transition from midlife to old age? Results from the French GAZEL cohort study. Am J Clin Nutr. 2010;92:16–23. doi: 10.3945/ajcn.2010.29223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zheng H, Tumin D, Qian Z. Obesity and mortality risk: new findings from body mass index trajectories. Am J Epidemiol. 2013;178:1591–1599. doi: 10.1093/aje/kwt179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newbold RR. Impact of environmental endocrine disrupting chemicals on the development of obesity. Hormones (Athens) 2010;9:206–217. doi: 10.14310/horm.2002.1271. [DOI] [PubMed] [Google Scholar]
- 16.He XZ, Baker DW. Changes in weight among a nationally representative cohort of adults aged 51 to 61, 1992 to 2000. Am J Prev Med. 2004;27:8–15. doi: 10.1016/j.amepre.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 17.Wing RR, Bolin P, Brancati FL, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med. 2013;369:145–154. doi: 10.1056/NEJMoa1212914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Locher JL, Roth DL, Ritchie CS, et al. Body mass index, weight loss, and mortality in community-dwelling older adults. J Gerontol A Biol Sci Med Sci. 2007;62:1389–1392. doi: 10.1093/gerona/62.12.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Newman AB, Yanez D, Harris T, Duxbury A, Enright PL, Fried LP Cardiovascular Study Research Group. Weight change in old age and its association with mortality. J Am Geriatr Soc. 2001;49:1309–1318. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- 21.Connor Gorber S, Tremblay M, Moher D, Gorber B. A comparison of direct vs. self-report measures for assessing height, weight and body mass index: a systematic review. Obes Rev. 2007;8:307–326. doi: 10.1111/j.1467-789X.2007.00347.x. [DOI] [PubMed] [Google Scholar]
- 22.Villanueva EV. The validity of self-reported weight in US adults: a population based cross-sectional study. BMC Public Health. 2001;1:11. doi: 10.1186/1471-2458-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nyholm M, Gullberg B, Merlo J, Lundqvist-Persson C, Råstam L, Lindblad U. The validity of obesity based on self-reported weight and height: implications for population studies. Obesity (Silver Spring) 2007;15:197–208. doi: 10.1038/oby.2007.536. [DOI] [PubMed] [Google Scholar]
- 24.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 25.Shiely F, Hayes K, Perry IJ, Kelleher CC. Height and weight bias: the influence of time. PLoS One. 2013;8:e54386. doi: 10.1371/journal.pone.0054386. [DOI] [PMC free article] [PubMed] [Google Scholar]


