Abstract
Background
Coronary slow flow (CSF) is a special coronary microvascular disorder. The pathogenesis and effective therapeutics of CSF remain unclear. This study aimed to evaluate the global and regional functions of the left ventricle (LV) and investigate the efficacy of nicorandil in patients with CSF.
Patients and methods
Thirty-six patients with CSF in the left anterior descending (LAD) branch and 20 patients with normal coronary arteries were included. Global and regional functions of the LV supplied by LAD were measured using conventional Doppler echocardiography and two-dimensional speckle tracking echocardiography, respectively, within 24 h after coronary angiography. Concentrations of plasma nitric oxide (NO) and endothelin-1 (ET-1) were detected using colorimetry and radioimmunoassay, respectively. The function of the LV and the levels of NO and ET-1 were also investigated before and 90 days after treatment with 15 mg/day of nicorandil.
Results
Compared with the control group, the early diastolic peak velocity (E), E/A ratio, and plasma NO levels were lower, whereas the late diastolic peak flow velocity (A) and plasma ET-1 levels were significantly higher in the CSF group (P<0.05). The longitudinal strain rate peak of the LV was reduced significantly in CSF patients (P<0.001). After treatment, 75% (27/36) of CSF patients were free of chest pain. The values of E peak, E/A ratio, longitudinal strain rate peak, and plasma NO level were increased (P<0.001), whereas the ET-1 level was decreased in CSF patients (P<0.001).
Conclusion
Nicorandil may improve chest pain symptoms and the impaired function of the LV, possibly by increasing plasma NO and reducing ET-1 in CSF.
Keywords: coronary slow flow, echocardiography, endothelin-1, nicorandil, nitric oxide, speckle tracking
Background
Coronary slow flow (CSF) is a special phenomenon of coronary microvascular disorder, characterized by delayed opacification of coronary arteries on angiography without obvious lesions in the coronary artery on coronary arteriography (CAG) analysis 1,2. It has been reported that the incidence of CSF is 7% among patients who undergo coronary angiography suspicious of various cardiovascular diseases 3.
At present, many studies suggest that the diastolic function of CSF patients is impaired but that systolic function shows no significant change 4–6. However, there are also studies indicating, using conventional echocardiography, that the left ventricle (LV) systolic function is damaged 7,8. To our knowledge, whether the systolic function of the LV is impaired in cases of CSF remains controversial at present 8. Two-dimensional speckle tracking echocardiography is a novel imaging technique that analyzes the motion of heart tissues 9. At present, this method is greatly applied in various diseases in cardiology, with the advantage of quantitative assessment of regional myocardial function 10,11.
Regarding the potential molecular mechanism, many studies have shown that endothelial dysfunction, which could be caused by many factors such as inflammation, adiposity, and atherogenesis, may be involved in the pathogenesis of CSF 12–14. It has been reported that increased levels of plasma endothelin-1 (ET-1) and decreased levels of nitric oxide (NO) may be involved in the pathogenesis of CSF 15,16. Besides, recent studies have also demonstrated that CSF is associated with coronary microcirculation dysfunction 12,17,18.
Nicorandil (N-[2-hydroxyethyl] nicotinamide nitrate) is a useful vasodilatory drug for different ischemic cardiac diseases 19. A recent study has shown that nicorandil could prevent endothelial dysfunction through an antioxidative mechanism, resulting in increased plasma NO and decreased plasma ET-1, in a diabetic animal model 20. Furthermore, Tsubokawa et al. 21 showed that nicorandil had a preventive effect on the CSF during rotational atherectomy. The same finding was obtained by Juneja et al. 22, who demonstrated that the CSF phenomenon in primary percutaneous coronary intervention could be prevented by nicorandil. Although current studies have demonstrated that nicorandil may reduce the incidence of CSF, the potential mechanism of nicorandil on CSF, as well as the improvement of myocardial function by nicorandil, remains rarely investigated.
We hypothesized that nicorandil may prevent endothelial dysfunction and improve the myocardial function of the LV in CSF patients, possibly by regulating the levels of circulating NO and ET-1 in cases of CSF. To prove this assumption, we assessed the global myocardial function of the LV using conventional Doppler echocardiography and the segmental functions supplied by the left anterior descending (LAD) in CSF patients using two-dimensional speckle tracking echocardiography. In addition, the plasma levels of NO and ET-1 were investigated before and after treatment in CSF patients.
Patients and methods
Ethics
All studies have been approved by the Affiliated Hospital of Qingdao University Ethics Committee and were performed in accordance with ethical standards.
Patients
In the Affiliated Hospital of Qingdao University, a total of 3478 patients underwent CAG from April 2013 to September 2013 because of clinical chest pain suspicious of coronary artery disease. CSF was defined according to the thrombolysis in myocardial infarction (TIMI) flow grade method, and the blood flow of the LAD with or below TIMI grade 2 (i.e. requiring ≥3 cardiac cycles to opacify the distal blood vessels) was defined as CSF 23. Patients with angiographically proven CSF in the LAD were recruited into our study (Fig. 1). Patients with artery stenosis (>40%), congenital heart disease, valvular heart disease, cardiomyopathy, cardiac disease, peripheral vascular disease, hematological system disease, tumor, recent surgical operation, dysfunction of liver, lung, and kidney, and acute and chronic infections were excluded from the study. None of the enrolled patients had prior myocardial infarction. Following CAG, blood testing of high-density lipoprotein cholesterol and low-density lipoprotein cholesterol concentrations was carried out. The clinical data of the selected patients were collected from our hospital database.
Fig. 1.

A typical coronary angiography image of coronary slow flow in the left anterior descending.
Patients with CSF in the LAD were given 5 mg nicorandil (Batch number: B01008970; Chugai Pharmaceutical Co. Ltd, Tokyo, Japan) orally three times a day. The clinical symptoms of the patients were observed 90 days after treatment. Patients were not allowed to take any other drugs that may affect NO and ET-1 levels, such as nitrates, β-blockers, and angiotensin-converting enzyme inhibitors, within 5–7 days before the study and 90 days after using nicorandil.
For investigations involving humans, approval was obtained from the institutional review board of the hospital committee and the study was performed according to the Declaration of Helsinki. Informed consent was provided by each patient.
Coronary arteriongraphy protocols
CAG was performed with a digital subtraction angiography system (Allura Xper FD20; Philips Medical Systems, Best, the Netherlands) using the standard Judkins technique, obtaining images at the rate of 30 frames/s. During CAG, the iopromide (Ultravist 370; Schering AG, Berlin, Germany) contrast and the 6-F diagnostic catheter were used in all patients. The injection speed was 4–5 ml/s for the left coronary artery and 3–4 ml/s for the right coronary artery (RCA). The injection amount was 8–10 ml for the left coronary artery and 6–8 ml for the RCA. We visualized the LAD in a right anterior oblique projection with head angulation of 20–25°, the left circumflex coronary artery (LCX) in a right anterior projection with foot angulation of 20–25°, and the RCA in a normotopia position with head angulation of 30°. All patients were carefully observed in terms of pulse and blood pressure during CAG.
Myocardial function detection
The global functions of the selected patients were assessed with conventional Doppler echocardiography: two-dimensional gray-scale images of the apical two-chamber, apical left ventricular long-axis view, the left ventricular short-axis basal level, and the apical basal level were collected using conventional Doppler echocardiography within 24 h after CAG and 90 days after treatment 10. The left ventricular internal diameter at end-diastole (LVIDd), left ventricular internal end-systolic diameter (LVIDs), left ventricular ejection fraction (LVEF), mitral valve flow spectrum of early diastolic peak velocity (E), and late diastolic peak flow velocity (A) were measured using conventional Doppler echocardiography 24 h after CAG, and E/A ratios were calculated. All of the above data were measured to assess the global function of the LV.
The regional functions of the selected patients were evaluated by means of two-dimensional speckle tracking echocardiography: the peak value of the longitudinal strain rate (LSR) of LV segmental systoles supplied by the LAD was measured with GE Echo PAC software using two-dimensional speckle tracking echocardiography for regional functions of the LV. The segments supplied by the LAD included six parts: the basal anterior wall, the mid-anterior, the apical anterior, the basal anteroseptal, the mid-anteroseptal, and the apical septal 24.
Detection of plasma nitric oxide and endothelin-1
Venous blood of a volume of 4 ml was drawn to measure the plasma levels of NO and ET-1 of all the patients 24 h after CAG and 90 days after treatment with nicorandil in the CSF group. The method of colorimetry was used to detect plasma NO concentration, and plasma ET-1 level was examined by means of radioimmunoassay 25.
Statistical analysis
Data were analyzed with SPSS 13.0 statistical software (IBM-SPSS Inc., Armonk, New York, USA). The χ2-test was used to enumerate data between groups. Data were expressed as mean±SD. The t-test was used to compare two independent samples of cardiac function and plasma parameters between the CSF and control groups. If differences in cardiac functions and plasma parameters in the groups before and after nicorandil treatment conformed to Gaussian distribution, the paired t-test was used in the analysis. Otherwise, the paired rank-sum test was used. P values less than 0.05 indicated that the difference was significant.
Results
Basic characteristics of the enrolled patients
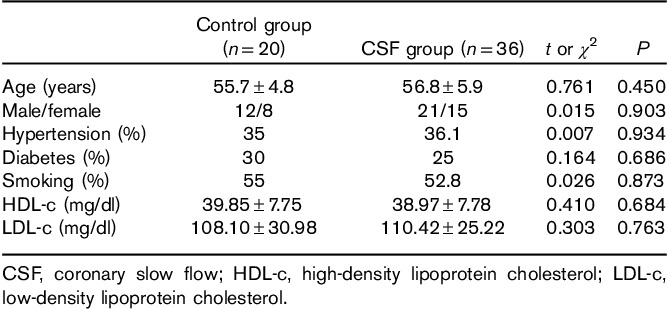
Of the total 3478 patients, 2178 showed coronary artery stenosis above 40%, 1072 cases showed normal coronary blood flow, and 228 showed CSF. The CSF phenomenon was observed in 6.56% (228/3478) of patients. Among the 228 CSF patients, there were 43 for single RCA, 64 for single LAD, 23 for single LCX, 41 for LAD combined with RCA, 28 for LAD combined with LCX, 17 for RCA combined with LCX, and 12 for all three branches. Of the 64 CSF patients with LAD, we selected 36 patients for participation in our study (defined as the CSF group), after excluding eight patients for hypertrophic cardiomyopathy, five for aortic valve insufficiency, four for aortic valve stenosis, six for rheumatic heart disease, three for atrial septal defect, and two for ventricular septal defect. Meanwhile, we selected 20 patients with a normal coronary artery (defined as the control group), which showed no significant difference in terms of age, sex, diabetes, hypertension, smoking, and blood lipids compared with the selected CSF group (P>0.05) (Table 1).
Table 1.
Baseline clinical characteristics of the participants in the coronary slow flow group and the control group
Comparison of echocardiography values and levels of circulating nitric oxide and endothelin-1 between the coronary slow flow group and the control group
To assess the integral functions of the LV, the values of LVIDd, LVIDs, LVEF, E peak, A peak, and E/A ratio were measured within 24 h after CAG using conventional Doppler echocardiography. It was found that there were no statistical differences in LVIDd, LVIDs, and LVEF between the CSF group and the control group (t=0.318–0.545, P>0.05). E peak value and E/A ratio were significantly lower (t=4.817–9.443, P<0.001), whereas the A peak value was significantly higher (t=3.534, P<0.01), in the CSF group compared with the control group (Table 2).
Table 2.
Comparison of echocardiographic parameters, longitudinal strain peak values, and plasma markers between the coronary slow flow and control groups
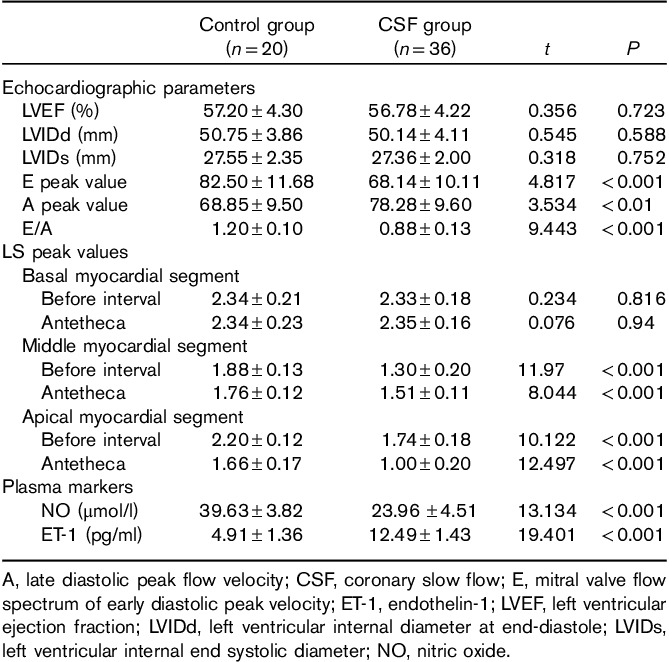
Using the two-dimensional speckle tracking technique, we evaluated the regional functions of the LV within 24 h after CAG. Our results showed that LSR peak values of four myocardial segments supplied by the LAD, including the mid-anterior, the mid-anteroseptal, the apical anterior, and the apical septal, were significantly lower than those of the control group (t=8.044–12.497, P<0.001). There was no difference in LSR peak values of the two segments, including the basal anterior and the basal anteroseptal, between the CSF group and the control group (t=0.076–0.234, P>0.05) (Table 2 and Fig. 2a and b).
Fig. 2.
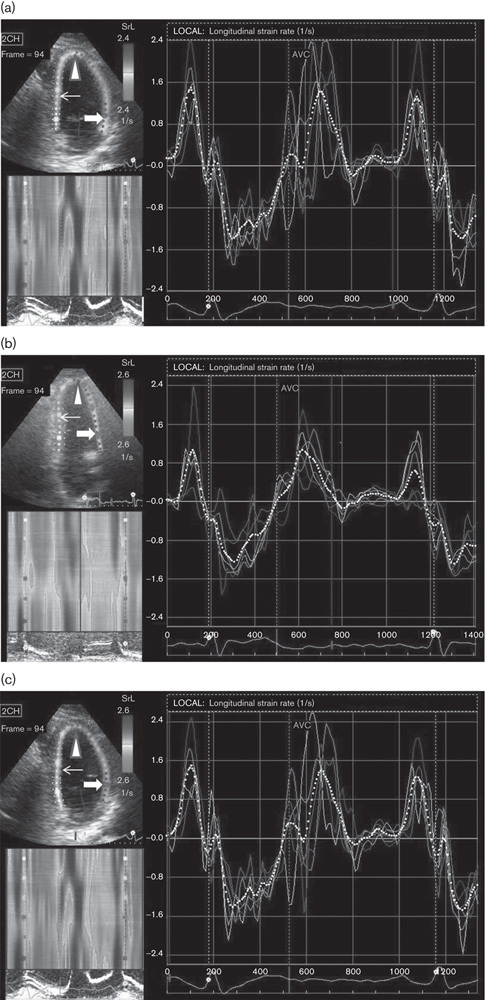
Longitudinal strain rate (LSR) peak images of patients in the control group (a) and coronary slow flow group before (b) and after (c) treatment. (a) An apical two-chamber heart tangent plane is shown in the top left corner of the picture, on which the basal anterior segment (thick arrow), the mid-anterior segment (thin arrow), the apica anterior l segment (triangle), and the LSR curve independent of the present study are shown. The white dotted line represents the overall strain rate curve. (b) Compared with the control group, the LSR peak value of the anterior basal segment (thick arrow) did not change significantly, whereas the LSR peak values of the mid-anterior segment (thin arrow) and the apical anterior segment (triangle) decreased. The overall strain rate (dashed white line) was significantly decreased. (c) Compared with pretreatment values, there were changes in the basal anterior segment (thick arrow) and mid-anterior segment (thin arrow). The peak value of LSR had no change, and the LSR peak values of the apical anterior segment (triangle) and the whole LSR peak value (white dotted line) were significantly increased.
For further investigating the mechanism of CSF, the levels of circulating NO and ET-1 were also examined within 24 h after CAG. Our present study showed that the plasma NO level was downregulated significantly (t=13.134, P<0.001), whereas the level of ET-1 was upregulated significantly (t=19.401, P<0.001), in the CSF group compared with the control group (Table 2).
Comparison of echocardiography values and levels of circulating nitric oxide and endothelin-1 before and after treatment in patients with coronary slow flow
According to the criterion of subjective descriptions of patients with respect to improvement in chest pain symptoms, chest pain symptoms of 27 patients in the CSF group after nicorandil treatment improved and the remission rate was 75%.
Using conventional Doppler echocardiography, we found that the E peak value (t=28.847, P<0.001) and E/A ratio (Z=3.757, P<0.001) had increased significantly in the CSF group after treatment with nicorandil. There was no significant improvement in the A peak value after treatment (Z=0.869, P>0.05) (Table 3).
Table 3.
Comparisons of echocardiographic parameters, longitudinal strain peak values and plasma markers in the coronary slow flow group before and after treatment
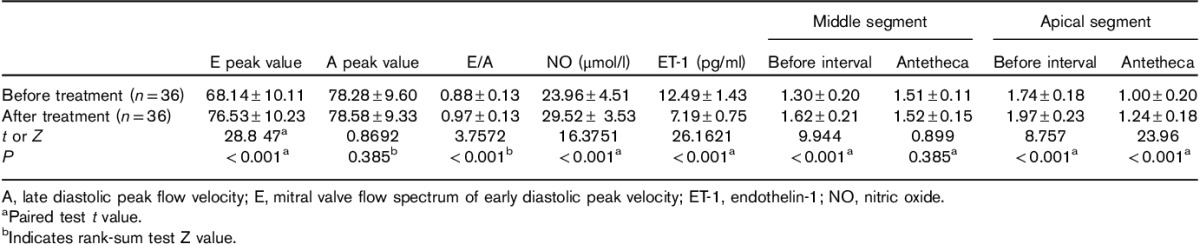
After treatment with nicorandil, the LSR peak values of three myocardial segments including the mid-anteroseptal, the apical anterior, and the apical septal increased (t=8.757–23.96, P<0.001). There was no difference in LSR peak value of the mid-anterior before and after treatment (t=0.899, P>0.05) (Table 3 and Fig. 2b and c).
In addition, our results found that the concentration of circulating NO increased (t=16.375, P<0.001), whereas the ET-1 level decreased significantly, after treatment with nicorandil in the CSF group (t=26.162, P<0.001) (Table 4).
Table 4.
Comparisons of echocardiographic parameters, longitudinal strain peak values, and plasma markers between the coronary slow flow group after treatment and the control group
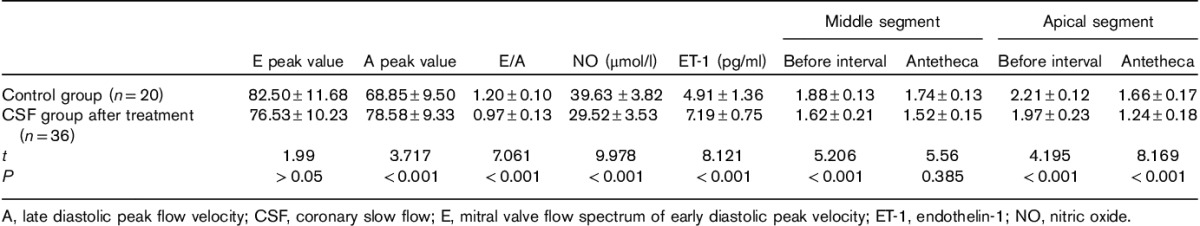
Comparison of post-treatment echocardiography values and levels of circulating nitric oxide and endothelin-1 with those in the control group
For assessing the extent of improvement in CSF patients as a result of treatment with nicorandil, we compared the post-treatment echocardiography values and levels of plasma NO and ET-1 with those in the control group. It was found that the E peak value had become normal in the CSF group after treatment (t=1.990, P>0.05), whereas the E/A ratio A peak value was still higher than that in the control group (t=3.717–7.061, P<0.001) (Table 4). The E/A ratio was lower than that in the control group (t=7.061, P<0.001) (Table 4).
In terms of regional function assessment of the LV, the results showed that the LSR peak values of four segments, including the mid-anterior, the apical anterior, and the apical septal, in the CSF group after treatment were still lower than those of the control group (t=4.195–8.169, P<0.001) (Table 4).
In addition, the plasma concentrations of NO in the CSF group with nicorandil treatment increased greatly but did not reach normal levels as in the control group (t=8.121–9.978, P<0.001) (Table 4).
Discussion
In the present study, myocardial global function was assessed by conventional echocardiography, and segmental functions of the LV supplied by the LAD were evaluated by means of two-dimensional speckle tracking echocardiography in the present study. The results of the conventional echocardiography showed that the E peak value and E/A ratio in the CSF group were lower than that in the control group (Table 2), suggesting that the diastolic function was impaired in CSF patients. Meanwhile, we also found that there was no significant difference in LVEF between the two groups (Table 2), suggesting that the overall systolic function of the LV was not damaged in the CSF group compared with the normal values. This may be explained by the fact that LV diastolic function is more susceptible to ischemia than is systolic function 26. Gunes et al. 8 reported that patients with CSF had impaired diastolic and regional LV systolic functions on the basis of myocardial tissue Doppler velocities. In accordance with the above finding, our results from two-dimensional speckle tracking echocardiography showed that the LSR peak values of four myocardial segments supplied by the LAD were significantly lower compared with that of the control group (Table 2 and Fig. 2a and b). These results suggested that CSF patients had segmental systolic dysfunctions of the LV, although LV global systolic function was normal.
Vascular endothelial dysfunction has been demonstrated to be involved in the pathogenesis of CSF 12. Valeriani et al. 27 reported that endothelial NO synthase activity, as well as NO concentration, was decreased in patients with microcirculation disorder. Another study by Celebi et al. 28 showed that ET-1 concentration was increased in CSF patients. In accordance with the above findings, our results also showed that the plasma NO concentration was decreased and the concentration of ET-1 was increased in the CSF group compared with the control group (Table 2), suggesting that the combination of decreased level of plasma NO and increased level of ET-1 may be involved in the formation and development of CSF. Chen et al. 29 reported that nicorandil had vasodilatory effects on the coronary artery with a diameter of 100–200 μm. Besides its direct vasodilatory effect, the fact that nicorandil could improve vascular endothelial dysfunction has been demonstrated 30. Another report by Serizawa et al. 20 has reported that nicorandil could prevent endothelial dysfunction by regulating NO and ET-1. In our study, nicorandil was applied in 36 CSF patients with LAD, and the results showed that 27 patients with chest pain symptoms had recovered. Functional analysis showed that diastolic function had improved after treatment (Table 3). LSR peak values of three myocardial segments increased after treatment (Table 3 and Fig. 2b and c). Besides, we also found that the concentration of plasma NO had increased in patients with CSF after treatment with nicorandil, whereas the plasma ET-1 concentration had decreased (Table 4). These results suggest that nicorandil could improve chest pain symptoms and the cardiac functions of the LV, possibly by regulating the plasma levels of NO and ET-1 in CSF.
Besides, our study further compared the post-treatment echocardiographic values and levels of circulating NO and ET-1 with those in the control group to assess the extent of improvement in CSF patients by treatment with nicorandil (Table 4). Our results suggested that nicorandil could not improve the hemodynamic disorder and LV function to the normal state, although it could improve the symptoms of CSF and the impaired myocardial function of the LV greatly, as well as increasing plasma NO and decreasing plasma ET-1. Our finding suggested that nicorandil combined with other effective drugs is of considerable value in the treatment of CSF 31. Further studies are needed to cure CSF completely.
We must point out that the TIMI method is an important index for evaluating the effect of coronary blood flow 32. It is more direct and accurate to assess the treatment effects of nicorandil by using the TIMI method than by echocardiographic evaluation of LV myocardial function. However, because most CSF patients refused to accept the second CAG, echocardiographic myocardial function was used as the evaluation index in this study. In addition, our study was limited by a small number of cases. A randomized optimal group and parallel controls were not used in the treatment of CSF with nicorandil. Thus, a large population of CSF patients and more accurate methods of assessing CSF should be further studied.
Conclusion
CSF patients presented with both diastolic and regional systolic dysfunctions of the LV. The combination of decreased level of circulating NO and increased level of plasma ET-1 may be involved in the pathophysiological mechanism of CSF. Nicorandil shows beneficial efficacy in CSF by improving chest pain symptoms and cardiac function, possibly by upregulating the level of plasma NO and downregulating the level of ET-1.
Acknowledgements
This work was supported by a grant from the National Natural Science Foundation of China.
Zuoyuan Chen and Xiuhua Chen have made substantial contributions to conception and design. Shan Li and Xuezhen Huo have been involved in drafting the manuscript. Xiuxiu Fu and Xiaonan Dong have given final approval of the version to be published.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Camsari A, Ozcan T, Ozer C, Akcay B. Carotid artery intima-media thickness correlates with intravascular ultrasound parameters in patients with slow coronary flow. Atherosclerosis 2008; 200:310–314. [DOI] [PubMed] [Google Scholar]
- 2.Gökçe M, Kaplan S, Tekelioğlu Y, Erdoğan T, Küçükosmanoğlu M. Platelet function disorder in patients with coronary slow flow. Clin Cardiol 2005; 28:145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beltrame JF, Turner SP, Leslie SL, Solomon P, Freedman SB, Horowitz JD. The angiographic and clinical benefits of mibefradil in the coronary slow flow phenomenon. J Am Coll Cardiol 2004; 44:57–62. [DOI] [PubMed] [Google Scholar]
- 4.Aksakal E, Gürlertop Y, Ateflal S. Left ventricular function in patients with coronary slow flow: a tissue Doppler study. Türk Kardiyol Dern Arfl – Arch Turk Soc Cardiol 2007; 35:360–365. [Google Scholar]
- 5.Sezgin AT, Topal E, Barutcu I, Ozdemir R, Gullu H, Bariskaner E, et al. Impaired left ventricle filling in slow coronary flow phenomenon: an echo-Doppler study. Angiology 2005; 56:397–401. [DOI] [PubMed] [Google Scholar]
- 6.Aksakal E, Islamoğlu Y, Simşek Z, Elbey M, Sevimli S, Arslan S, et al. The association of coronary slow flow with time to peak systolic strain. Turk Kardiyol Dern Ars 2011; 39:29–34. [PubMed] [Google Scholar]
- 7.Nurkalem Z, Gorgulu S, Uslu N, Orhan AL, Alper AT, Erer B, et al. Longitudinal left ventricular systolic function is impaired in patients with coronary slow flow. Int J Cardiovasc Imaging 2009; 25:25–32. [DOI] [PubMed] [Google Scholar]
- 8.Gunes Y, Tuncer M, Guntekin U, Ceylan Y, Sahin M, Simsek H. Regional functions of the left ventricle in patients with coronary slow flow and the effects of nebivolol. Ther Adv Cardiovasc Dis 2009; 3:441–446. [DOI] [PubMed] [Google Scholar]
- 9.Mondillo S, Galderisi M, Mele D, Cameli M, Lomoriello VS, Zacà V, et al. Echocardiography Study Group of the Italian Society of Cardiology (Rome, Italy). Speckle-tracking echocardiography: a new technique for assessing myocardial function. J Ultrasound Med 2011; 30:71–83. [DOI] [PubMed] [Google Scholar]
- 10.Leitman M, Lysyansky P, Sidenko S, Shir V, Peleg E, Binenbaum M, et al. Two-dimensional strain – a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 2004; 17:1021–1029. [DOI] [PubMed] [Google Scholar]
- 11.Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, et al. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 2010; 23:351–369quiz 453–455. [DOI] [PubMed] [Google Scholar]
- 12.Sezgin AT, Sigirci A, Barutcu I, Topal E, Sezgin N, Ozdemir R, et al. Vascular endothelial function in patients with slow coronary flow. Coron Artery Dis 2003; 14:155–161. [DOI] [PubMed] [Google Scholar]
- 13.Asanuma H, Sanada S, Asakura M, Asano Y, Kim J, Shinozaki Y, et al. Carperitide induces coronary vasodilation and limits infarct size in canine ischemic hearts: role of NO. Hypertens Res 2014; 37:716–723. [DOI] [PubMed] [Google Scholar]
- 14.Lyon CJ, Law RE, Hsueh WA. Minireview: adiposity, inflammation, and atherogenesis. Endocrinology 2003; 144:2195–2200. [DOI] [PubMed] [Google Scholar]
- 15.Sezgin N, Barutcu I, Sezgin AT, Gullu H, Turkmen M, Esen AM, Karakaya O. Plasma nitric oxide level and its role in slow coronary flow phenomenon. Int Heart J 2005; 46:373–382. [DOI] [PubMed] [Google Scholar]
- 16.Pekdemir H, Cicek D, Camsari A, Akkus MN, Cin VG, Doven O, et al. The relationship between plasma endothelin-1, nitric oxide levels, and heart rate variability in patients with coronary slow flow. Ann Noninvasive Electrocardiol 2004; 9:24–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Beltrame JF, Limaye SB, Horowitz JD. The coronary slow flow phenomenon – a new coronary microvascular disorder. Cardiology 2002; 97:197–202. [DOI] [PubMed] [Google Scholar]
- 18.Fineschi M, Bravi A, Gori T. The ‘slow coronary flow’ phenomenon: evidence of preserved coronary flow reserve despite increased resting microvascular resistances. Int J Cardiol 2008; 127:358–361. [DOI] [PubMed] [Google Scholar]
- 19.Kinoshita M, Sakai K. Pharmacology and therapeutic effects of nicorandil. Cardiovasc Drugs Ther 1990; 4:1075–1088. [DOI] [PubMed] [Google Scholar]
- 20.Serizawa K, Yogo K, Aizawa K, Tashiro Y, Ishizuka N. Nicorandil prevents endothelial dysfunction due to antioxidative effects via normalisation of NADPH oxidase and nitric oxide synthase in streptozotocin diabetic rats. Cardiovasc Diabetol 2011; 10:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tsubokawa A, Ueda K, Sakamoto H, Iwase T, Tamaki S. Effect of intracoronary nicorandil administration on preventing no-reflow/slow flow phenomenon during rotational atherectomy. Circ J 2002; 66:1119–1123. [DOI] [PubMed] [Google Scholar]
- 22.J E, Juneja MS, George T, Sr R, V V, Ak B, et al. Prevention of no flow/slow reflow phenomenon in primary PCI by Nicorandil. Indian Heart J 2007; 59:246–249. [PubMed] [Google Scholar]
- 23.Chesebro JH, Knatterud G, Roberts R, Borer J, Cohen LS, Dalen J, et al. Thrombolysis in Myocardial Infarction (TIMI) Trial, Phase I: a comparison between intravenous tissue plasminogen activator and intravenous streptokinase. Clinical findings through hospital discharge. Circulation 1987; 76:142–154. [DOI] [PubMed] [Google Scholar]
- 24.Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. American Heart Association Writing Group on Myocardial Segmentation and Registration for Cardiac Imaging. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart a statement for healthcare professionals from the cardiac imaging committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 2002; 105:539–542. [DOI] [PubMed] [Google Scholar]
- 25.Camsarl A, Pekdemir H, Cicek D, Polat G, Akkus MN, Döven O, et al. Endothelin-1 and nitric oxide concentrations and their response to exercise in patients with slow coronary flow. Circ J 2003; 67:1022–1028. [DOI] [PubMed] [Google Scholar]
- 26.Labovitz AJ, Lewen MK, Kern M, Vandormael M, Deligonal U, Kennedy HL. Evaluation of left ventricular systolic and diastolic dysfunction during transient myocardial ischemia produced by angioplasty. J Am Coll Cardiol 1987; 10:748–755. [DOI] [PubMed] [Google Scholar]
- 27.Valeriani M, Sestito A, Le Pera D, De Armas L, Infusino F, Maiese T, et al. Abnormal cortical pain processing in patients with cardiac syndrome X. Eur Heart J 2005; 26:975–982. [DOI] [PubMed] [Google Scholar]
- 28.Celebi H, Catakoglu AB, Kurtoglu H, Sener M, Hanavdelogullari R, Demiroglu C, et al. The relation between coronary flow rate, plasma endothelin-1 concentrations, and clinical characteristics in patients with normal coronary arteries. Cardiovasc Revasc Med 2008; 9:144–148. [DOI] [PubMed] [Google Scholar]
- 29.Chen JW, Lee WL, Hsu NW, Lin SJ, Ting CT, Wang SP, Chang MS. Effects of short-term treatment of nicorandil on exercise-induced myocardial ischemia and abnormal cardiac autonomic activity in microvascular angina. Am J Cardiol 1997; 80:32–38. [DOI] [PubMed] [Google Scholar]
- 30.Sekiya M, Sato M, Funada J, Ohtani T, Akutsu H, Watanabe K. Effects of the long-term administration of nicorandil on vascular endothelial function and the progression of arteriosclerosis. J Cardiovasc Pharmacol 2005; 46:63–67. [DOI] [PubMed] [Google Scholar]
- 31.Sadamatsu K, Tashiro H, Yoshida K, Shikada T, Iwamoto K, Morishige K, et al. Acute effects of isosorbide dinitrate and nicorandil on the coronary slow flow phenomenon. Am J Cardiovasc Drugs 2010; 10:203–208. [DOI] [PubMed] [Google Scholar]
- 32.Gibson CM, Cannon CP, Daley WL, Dodge JT, Jr, Alexander B, Jr, Marble SJ, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation 1996; 93:879–888. [DOI] [PubMed] [Google Scholar]


