Abstract
Objective
This study compared the impact of cognitive-behavioral therapy for pain (CBT-P), mindful awareness and acceptance treatment (M), and arthritis education (E) on day-to-day pain- and stress-related changes in cognitions, symptoms, and affect among adults with rheumatoid arthritis (RA).
Method
143 RA patients were randomized to one of the three treatment conditions. CBT-P targeted pain coping skills; M targeted awareness and acceptance of current experience to enhance coping with a range of aversive experiences; and E provided information regarding RA pain and its management. At pre- and post-treatment, participants completed 30 consecutive evening diaries assessing that day's pain, fatigue, pain-related catastrophizing and perceived control, morning disability, and serene and anxious affects.
Results
Multilevel models compared groups in the magnitude of within-person change in daily pain- and stress-reactivity from pre- to post-treatment. M yielded greater reductions than did CBT-P and E in daily pain-related catastrophizing, morning disability, and fatigue, and greater reductions in daily stress-related anxious affect. CBT-P yielded less pronounced declines in daily pain-related perceived control than did M and E.
Conclusions
For individuals with RA, M produces the broadest improvements in daily pain- and stress-reactivity relative to CBT-P and E. These findings also highlight the utility of a diary-based approach to evaluating the treatment-related changes in responses to daily life.
Keywords: cognitive-behavioral, mindfulness, interventions, pain, reactivity, arthritis
Chronic pain is a prevalent health condition that requires individuals to adapt to a daily life that can include episodes of increased pain, functional impairment, and affective disturbance (Banks & Kerns, 1996; Lawrence et al., 2008). Over the past 30 years, a substantial body of empirical evidence has accrued establishing the efficacy of psychosocial treatment of chronic pain beyond the effects of standard medical care (Astin, Beckner, Soeken, Hochberg, & Berman, 2002; Dixon, Keefe, Scipio, L., & Caitlin, 2007; Morley, Eccleston, & Williams, 1999). In particular, cognitive-behavioral therapy (CBT) has emerged as one of the most common and effective forms of psychosocial treatment. From a cognitive-behavioral perspective, an individual's beliefs regarding physical symptoms and the coping responses that stem from those beliefs are central to adaptation to chronic pain. A key facet of CBT is training individuals to apply cognitive reappraisal strategies to address the faulty cognitions that contribute to their poor adjustment. To that end, individuals are encouraged to adopt a more detached or “decentered” view of thoughts, considering their thoughts are not facts but as temporary mental events that can be evaluated to determine their veracity and/or utility and changed if necessary. In addition to cognitive reappraisal, CBT typically incorporates behavioral components, including training in relaxation techniques and activity pacing, with the overarching goal of helping individuals respond to their pain more effectively. Over the long term, CBT aims to improve coping self-efficacy, psychological and physical symptoms, and functional health. A series of meta-analyses summarizing the benefits of CBT has shown that it yields moderate to large effects for cognitive coping responses and small to moderate effects for pain outcomes relative to controls (Astin et al., 2002; Dixon et al., 2007).
More recently, alternative approaches have pointed to the value of fostering both awareness and acceptance of pain and other aversive experiences to help individuals with chronic pain effectively manage the physical and emotional demands of their illness (Hayes & Duckworth, 2006; Kabat-Zinn, 1990). Much like CBT, acceptance-based approaches foster the development of a decentered view that thoughts, emotions, and physical sensations are simply temporary experiences. However, in contrast to the focus in CBT on promoting efforts to challenge and change faulty cognitions to control pain, the focus in acceptance-oriented treatments is on increasing individuals' capacity to be both aware and nonjudgmental of present moment experiences, including pain and their reactions to pain. Acceptance-oriented treatments typically include exercises designed to illustrate the principles of mindfulness; with notable exceptions (e.g., Hayes & Duckworth, 2006), these exercises incorporate the regular practice of mindfulness meditation to build the capacity for increased awareness and acceptance. Mindfulness training helps individuals attend to current experiences without suppressing or elaborating those experiences. Increasing the capacity to sustain awareness without judgment when faced with pain or stress may be key to decreasing automatic, maladaptive responses, including hypervigilance to threats and catastrophizing (Garland et al., 2012; Garland & Howard, 2013). One important aim of an acceptance-oriented approach is to decrease automatic cognitive and emotional reactivity to aversive experiences, thereby increasing the ability to act more intentionally to response to pain and other stressors. A recent meta-analysis of randomized clinical trials of acceptance-based treatments for chronic pain indicated that they yield small improvements in pain and depression, and small to moderate improvements in physical well-being relative to education controls or treatment-as-usual (Veehof, Oskam, Schreurs, & Bohlmeijer, 2011).
Taken together, the evidence to date suggests that both CBT and acceptance-based treatments for chronic pain improve physical and psychological symptoms. Yet most evaluations of the benefits of these treatments have relied on global measures that ask individuals to recall their symptoms, emotional experiences, and coping responses over a period ranging from several days to several weeks. Moreover, some assessments require individuals to recollect not simply the levels of their symptoms and/or coping responses but rather the covariation between the two (i.e., “when-then” relations). For example, a commonly-used measure of functional health, the SF36 (Ware & Sherbourne, 1992), asks individuals to estimate the extent to which their physical or emotional problems have interfered with their social activities or their performance of regular daily activities. A key limitation of retrospective reports is that recall of past experience can be heavily influenced by the enduring beliefs individuals hold about themselves, including how they typically feel or respond, and their implicit theories about the relations between variables (Robinson & Clore, 2002). Although this approach to assessment yields important information about general functioning, it provides relatively little insight into whether treatments actually alter coping and adaptation on a daily basis among people with chronic pain.
An approach that can complement the use of static retrospective reports to evaluate intervention effects involves the intensive assessment of individuals over time and across contexts, and has been termed the daily process method, ecological momentary assessment, and experience sampling (Affleck, Zautra, Tennen, & Armeli, 1999; Csikszentmihalyi & Larson, 1987; Shiffman, Stone, & Hufford, 2008). In contrast to scales that require respondents to recall their symptoms and emotional experiences over periods ranging from days to weeks, daily process methods can focus diary reports on a more limited time frame, from the past few moments to a single day, reducing the time between an experience and the report of that experience and thus the error variance of the measure (Epstein, 1979). The primary advantage, though, is that diary data have the potential to shed light on intervention-related changes in the dynamics of behavior in real-world contexts (Shiffman et al., 2008). Indeed, changes in relations among variables are often at the heart of purported mechanisms of action, and the principal value of daily process data is that such changes can be captured with intensive within-person assessment. In the evaluation of treatments for chronic pain, pre- and post-intervention assessment using the daily diary process method provides the opportunity to assess change in the daily dynamics of responses to pain and other daily stressors as a function of treatment. That is, the covariation between pain/stress and daily functioning can be estimated in the data rather than based on respondents’ retrospective judgments of these covariations.
The use of diary methods to examine the covariation among variables has grown exponentially over the past 20 years. Yet despite clear advantages for the evaluation of intervention effects, this particular application of daily process methods remains in its infancy. To our knowledge, in the arena of behavioral treatments for chronic pain conditions in particular, only a single report has examined diary reports as a means of examining intervention effects on real-time responses to pain (Gil et al., 2001). Gil and colleagues (2001) evaluated post-intervention daily diaries of children with sickle cell disease who had been randomized to brief coping skills training (versus usual care) to probe within-person relations between daily pain, daily coping practice, and functioning during the month following treatment. The findings were enlightening. On days of high pain, if children also reported higher use of coping practice, they were significantly less likely to have contact with health care providers and to decrease school participation. These relations are intriguing, but interpretation of the findings is constrained by the use of post-intervention diary assessments only in the intervention group and not in a comparison condition. Thus, the extent to which the relations between pain, pain coping practice, and daily functioning were the result of the intervention cannot be ascertained.
Overview of the Current Study
The present study is based on diary data obtained from a clinical trial in which 144 individuals with rheumatoid arthritis (RA) were randomized to either CBT for pain (CBT-P), mindful awareness and acceptance therapy (M), or an arthritis education condition (E), which served as a placebo control (Zautra et al., 2008). In CBT-P, training in cognitive reappraisal, relaxation, and activity pacing were used to change faulty cognitions and coping responses to pain episodes to responses that are more adaptive. In M, training in mindfulness skills was used to increase awareness and nonjudgment of aversive experiences, thereby decreasing reactivity and increasing emotional regulation to not only pain but also stress episodes. An earlier report of findings from this trial detailed pre-to-post changes in overall daily levels of coping cognitions, emotions, and symptoms by aggregating scores across the 30 days of pre- and 30 days of post-intervention diaries. Results indicated that CBT-P and E yielded more improvement than did M in overall levels of pain control in the sample as a whole. For the subgroup of individuals with a history of recurrent depression, however, M yielded more improvement than did CBT-P and E in overall levels of pain catastrophizing, coping efficacy, and positive and negative affect (Zautra et al., 2008).
In the current study, we re-examined the pre- and post-intervention diary data to evaluate the effects of the CBT-P, M, and E conditions on day-to-day pain- and stress-reactivity via the 30 daily diary reports obtained at pre- and post-intervention. We use the term “reactivity” to refer to daily within-person changes in cognitions, fatigue and morning disability, and affect associated with daily changes in pain and stress (Hamilton et al., 2008; Suls & Martin, 2005). Improvement in reactivity would be manifested by weakened relations between daily changes in pain or stress and daily cognitions, symptoms, and affect from pre- to post-treatment. As a specific example, if individuals reacted to days of high pain with smaller increases in catastrophizing at post-treatment relative to pre-treatment, they would be demonstrating an enhanced ability to limit the negative effects of pain flares (i.e., improved pain reactivity). In line with its focus on teaching skills to manage and control pain, we expected the CBT-P group to show improvement on pain-related changes in pain catastrophizing and control, fatigue, and morning disability compared with the E group, and on pain-related changes pain control compared with the M group. In contrast, because M targets the development of broader emotion regulation skills to dampen the impact of pain and stress flares, we expected the M group to show improvement in pain-related changes in pain cognitions, fatigue, and morning disability relative to the E group, and in pain-related and stress-related changes in affect relative to both the E and CBT-P groups.
Method
Participants
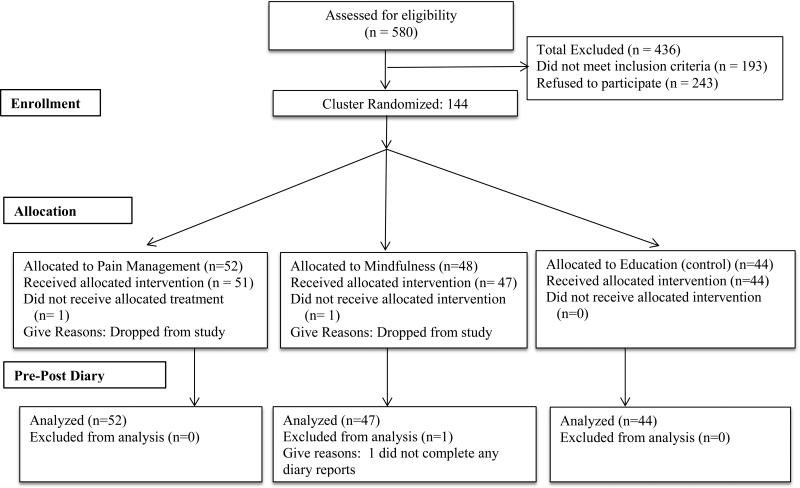
One hundred and forty four participants from the Phoenix, AZ metropolitan area were recruited from physician's offices, referrals from VA hospital rheumatologists, senior citizen groups, advertisements, and mailings to members of the Arthritis Foundation. To be eligible for the study, participants were required to (a) be between 21 and 86 years old, (b) have a physician-confirmed diagnosis of rheumatoid arthritis (RA), and (c) exhibit bilateral tenderness or swelling as determined by an examination conducted by a rheumatologist as part of the study procedures. In addition, participants were excluded if they had a diagnosis of Lupus Erythematosus or if they were receiving a cyclical estrogen-replacement therapy. The 144 participants were randomly allocated to one of three conditions: CBT-P (n=52), M (n=48), or E (n=44). Of the 144 individuals who were randomized, 1 participant in the M condition was dropped from the pre-post diary analyses because she did not complete any diary reports. (See Figure 1 for participant flow throughout the study.) The analyses for the current study were based on data from 143 participants.
Figure 1.
Participant flow throughout the study.
Procedure
This study was conducted in compliance with the Institutional Review Boards of Arizona State University and the PhoenixVA Healthcare System in Phoenix, AZ. Participants were screened by phone to determine initial eligibility, and eligible individuals received a full description of the study by phone and by mail via a written consent form. Interested individuals returned a signed consent form by mail, together with a release of information allowing study personnel to contact their physicians. Participants became enrolled in the study once their physicians confirmed their RA diagnosis. Participants then received a set of 30 daily diary booklets assessing interpersonal stress, pain and fatigue, affect, pain-related cognitions, and morning disability. One half the participants were selected at random to undergo a pre-intervention laboratory pain and stress assessment and a blood draw.
For each of eight intervention waves, cohorts of 20-28 individuals provided a schedule of their availability and were assigned to one of three group meeting days. The project manager, under the supervision of the study's principal investigator, randomly assigned these day clusters to one of three treatment conditions using a random numbers table. A post-intervention questionnaire, diary assessment, and laboratory visit followed completion of the eight-week intervention for all participants. Data collection began January 2003 and ended June 2005.
The current study draws on data from the pre- and post-intervention diaries. An extensive description of all study components is available in Zautra et al. (2008).
Intervention Plan
The M, CBT-P, and E groups followed a parallel format: Each treatment included eight modules that were delivered in weekly 2-hour group meetings and addressed themes that defined the content of that intervention. The CBT-P and M treatments included experiential activities designed to enhance targeted skills, whereas the E group received information regarding pain and stress management but did not practice skills to manage pain or emotional difficulties.
The CBT-P treatment focused explicitly on increasing pain management skills to enhance cognitive coping and functional health and limit fatigue symptoms in response to pain, following a standard cognitive-behavioral format. Included among the topics covered to provide cognitive and behavioral strategies to manage daily pain were: 1) relaxation training; 2) autogenic training; 3) cognitive coping with pain; 4) activity pacing and managing daily activities; and 4) managing intense pain episodes. The M treatment focused on developing two distinct sets of skills, one to reduce the negative impact of pain and stress episodes on mood, symptoms, and functioning, and the other to enhance positive affective engagement. The inclusion of training to boost positive engagement, a focus not included in many mindfulness programs, is based on research pointing to the value of drawing on positive resources to interrupt automatic responding to pain and other stressors (e.g., Strand et al., 2006). The ultimate purpose of targeting emotion regulation was to position individuals to make more intentional (versus reflexive) choices both day-to-day and in the long term. Specific targeted skills included: 1) use of mindful techniques (e.g., breathing meditation) to increase present-moment awareness and acceptance/nonjudgment of difficult experiences; and 2) identification of strategies (e.g., savoring positive events) to develop positive emotional resources, including more satisfying social relations. The E group provided didactic information regarding the etiology, pathophysiology, and treatment of RA, and healthy lifestyles and physician-patient communication. The E condition intentionally omitted information on coping practices and did not engage participants in any experiential activities or skill rehearsal exercises.
Groups were co-facilitated by a doctoral-level clinical health psychologist and an advanced doctoral student in clinical psychology. Clinicians had prior training in CBT and mindfulness methods, particularly with regard to the treatment of chronic pain. Each intervention was manualized; manuals included information regarding the rationale for the intervention, and material regarding specific objectives, didactic instructions, learning activities, and homework assignments for each session. Prior to delivering the interventions, clinicians reviewed the treatment manuals with the treatment team to maximize treatment fidelity across the eight waves of groups. During treatment waves, the treatment supervisor conducted weekly review sessions to foster adherence and address clinical issues arising in treatment groups.
Diary Assessment
After enrollment and completion of the initial clinical interview, participants received 30 paper diaries and pre-addressed, stamped envelopes by mail, and were contacted by a staff member who provided diary instructions by phone. Participants were asked to complete a diary each night approximately 30 minutes prior to going to bed, and to place the completed diary in the mail the next day. Postmark verification was monitored to substantiate compliance with instructions. Participants were compensated up to $90 for their completion of the diaries: $2/day for each completed diary and a bonus of $1/day if they completed more than 25 diaries. Immediately following the eight-week intervention, participants received and completed a second set of 30 diaries, and received compensation according to the same criteria. Aggregating across participants, 95% of the pre diaries and 92.5% of the post diaries were completed, and of those completed diaries, 97.3% were received with a verified postmark. Of the diaries with a verified postmark, 80% were postmarked within 2 days of diary completion (allowing for weekend and holiday constraints on mail service). Among other questions, the daily diary assessed the following variables targeted in the current study: pain and interpersonal stress, fatigue, morning disability, pain-related cognitions, and serene and anxious affects.
Measures
Pain and fatigue
Daily pain and daily fatigue were each day with the standard instruction for a numerical rating scale (Jensen, Karoly, & Braver, 1986): “Please choose a number between 0 and 100 that best describes the average level of pain (fatigue) you have experienced today due to your RA. A zero (0) would mean ‘no pain (fatigue)’ and a one hundred (100) would mean ‘pain (fatigue) as bad as it can be’ (Jensen et al., 1986). The estimated intraclass correlations in the current sample were assessed for the diary reports by evaluating unconditional means models (described below). The intraclass correlation estimates were .58 for pain and .54 for fatigue.
Morning disability
Morning disability was assessed with the item “After you woke up this morning, how long did it take you to reach your maximum physical ability for the day?” (Yazici, Pincus, Kautiainen, & Sokka, 2004). Ratings ranged from 1 (less than 15 minutes) to 5 (more than an hour). This assessment of morning stiffness is a widely used marker of functional disability in RA and reflects disease activity more than do traditional markers of inflammation like joint counts (Westhoff, Buttgereit, Gromnica-Ihle, & Zink, 2008). The estimated intraclass correlation was .66 in the current sample.
Interpersonal stress
Perceived interpersonal stress in social relationships was assessed by asking participants to respond to four items regarding the stressfulness of their relations within four domains: Spouse, friends, family, and work. Ratings for each item were made on a scale of 1 (not at all) to 4 (extremely), and responses to the statements were averaged to yield a daily score for interpersonal stress (Watson, 1988). The estimated intraclass correlation for interpersonal stress in the present sample was .25.
Pain-related cognitions
Two common pain-related cognitions were assessed in the diaries: pain catastrophizing and pain control. Existing evidence points to these particular pain cognitions as key mediators of treatment-related improvements in functional and psychological health among individuals in chronic pain (e.g., Smeets, Vlaeyen, Kester, & Knottnerus, 2006; Spinhoven et al., 2004; Turner, Holtzman, & Mancl, 2007). Pain catastrophizing was assessed with two statements: “I worried about whether my pain would ever end” and “I felt my pain was so bad I couldn't stand it anymore,” derived from the Coping Strategies Questionnaire (Rosenstiel & Keefe, 1983). Ratings for each statement were made on a scale of 1 (strongly disagree) to 5 (strongly agree), and responses to the statements were averaged within day to yield a daily score for catastrophizing. Pain control was assessed with the statement “What number between 0 and 10 best describes how much personal control you were able to exert over the amount of pain you experienced today?”, with anchors of 0 (no control at all) and 10 (complete control). This item was a modified version of an item drawn from the Arthritis Self-Efficacy Scale (Lorig, Chastain, Ung, Shoor, & Holman, 1989). Estimated intraclass correlations were .53 for catastrophizing and .56 for pain control in the current sample.
Serene and anxious affects
Serene and anxious affects were assessed via items drawn from lower order subscales of the Positive and Negative Affect Scale-Expanded Form (PANAS-X; Watson & Clark, 1994). Participants rated three adjectives describing serene affect (i.e., relaxed, at ease, calm) and four items describing anxious affect (i.e., nervous, afraid, scared, jittery) on a 5-point scale ranging from 1 (very slightly or not at all) to 5 (extremely). The lower order, empirically-derived subscales of the PANAS-X reflect specific dimensions of positive and negative affect, consistent with existing models of emotion, and show good psychometric properties (Watson & Clark, 1994). Limiting the impact of pain on serenity and anxiety was a target of CBT-P and M, and decreased pain-related anxiety has been linked to improved outcomes among individuals with chronic pain (McCracken & Gross, 1998). Mean serenity and anxiety scores were calculated for each day by averaging across items. Within-person reliabilities were .61 for serenity and .42 for anxiety.
Analytic approach
To examine the proportion of total variance in daily outcomes that was between-person, unconditional means models were computed for each outcome, yielding estimates of the intraclass correlations (Singer, 1998). Multilevel analyses were then conducted to evaluate intervention group differences in daily pain- and stress-reactivity, modeling up to 60 daily measurement occasions (30 pre- and 30 post-intervention diaries) nested within each of the 143 participants. Thus, multilevel modeling partitions the variance into two components: daily reports (Level 1) are clustered within individuals (Level 2). For each person within each set of diaries (pre and post), we first computed an average score across the 30 days for pain and stress measures. We then subtracted each person's average score from each of his/her daily scores within a diary set, resulting in a set of up to 60 deviation scores for pain and stress (30 pre and 30 post) (Singer, 1998). These deviation scores, also termed person-centered scores, index day-to-day within-person change relative to an individual's average level on the variable of interest. Deviation scores are denoted in this article by the Greek letter Δ. A day of positive deviation indicates a pain or stress episode for that individual. The Level 2 variable in the current analyses was group assignment (CBT-P, M, or E).
Pain reactivity was assessed for all outcomes whereas stress reactivity was assessed for affective outcomes. We first determined whether groups were comparable prior to the intervention by examining group differences at pre-treatment in pain- and/or stress-related changes (i.e., reactivity); these models included Group, ΔPain/ΔStress, and Group × ΔPain/ΔStress interactions as predictors of each outcome. We next asked whether pain- and/or stress reactivity changed significantly from pre to post for each intervention group separately by including Time, ΔPain/ΔStress, and Time × ΔPain/Stress interactions as predictors in each model. Finally, we compared groups in the magnitude of change from pre to post by including Group main effects and interaction terms in the models. To illustrate this final set of analyses, the basic equation evaluating differences between interventions in their effects on pain- and/or stress-related changes in anxious affect was as follows:
Anxious affect = b0 + b1 (Group) + b2 (ΔPain) + b3 (ΔStress) + b4 (Group × ΔPain) + b5
(Group × ΔStress) + b6 (Time: Pre vs. Post) +b7 (Group × Time) + b8 (Time × ΔPain) + b9
(Time × ΔStress) + b10 (Group × Time × ΔPain) + b11 (Group × Time × ΔStress) + r.
b0 yields an estimate of the intercept for anxiety. Coefficients b1-11 provide slope estimates of predictor variables, with slopes b10 and b11 testing for differences between groups in pre-post changes in pain- and stress-reactivity, respectively. The r stands for the within-person residual. This approach mirrors the one taken by Geschwind and colleagues (2011) to evaluate group differences in pre- to post-treatment effects on affective reactivity in recurrent depression. Repeating the analyses using a three-level approach (i.e., diary days, pre-post assessment, and individuals as levels) retained the pattern of findings for pain- and stress-reactivity.
All multilevel analyses were conducted using the SAS (version 9.3) PROC MIXED software, which furnished parameters in the form of unstandardized restricted maximum likelihood estimates (β coefficients). These are partial correlations, adjusted for between-unit differences, which serve as useful effect size estimations of magnitude and direction of changes in dependent variables associated with changes in independent variables. For all analyses, we allowed intercepts to vary randomly, thus enabling us to generalize the findings to the population of persons from which the sample was drawn and the populations of observations from which their daily reports were sampled. We also allowed the slopes reflecting changes in pain to vary randomly because doing so improved the fit of the models. Autocorrelated residuals are a common consequence of equally spaced observations and can bias standard errors and significance levels; thus, a first order autoregressive term [i.e., AR(1)] was included in all models. To illustrate significant Time × Group × ΔPain/Stress interaction effects, which were derived from continuous ΔPain and ΔStress variables, we followed the guidelines of Aiken and West (1991) to plot the interactions. Specifically, we used values for ΔPain/ΔStress that were one standard deviation above the mean (i.e., high pain/stress days) and one standard deviation below the mean (i.e., low pain/stress days) to generate plots of the average within-person pre- and post-intervention slopes for each intervention group.
Results
Participants
The sample was primarily female (68.5%) and Caucasian (85%), with an average age of 54.28 years (SD = 13.80, range 21 to 81). Although some participants did not complete high school (6%), the vast majority of participants graduated from high school (10%), attended trade school (13%) or college (29%), or graduated from college (42%). The average annual family income of the sample was between $30,000 and $39,000. The three intervention groups were comparable in age, income, and education (Fs < 1.58, ps > .21), and in proportions of females and Caucasians (χ2 (2) < 3.32, ps > .19).
Pre-Treatment Group Comparisons of Diary Reports
The first sets of models tested whether daily increases in pain and/or stress above an individual's average were related to same-day changes in cognitive, symptom, and affective outcomes in the pre-treatment diaries within each treatment group, and then whether groups differed in their pre-treatment reactivity to daily pain and/or stress. Table 1 summarizes findings from the series of multilevel models 1) examining daily reactivity within each group separately, and 2) comparing daily reactivity between groups at pre-treatment.
Table 1.
Parameter Estimates (Standard Errors) from Multilevel Models of Pre-treatment Daily Pain- and Stress-reactivity for the Mindfulness (M; n=47), CBT-Pain (P; n=52), and Education (E; n=44) Groups
| Effects within groupa |
Group comparisonsb |
||||
|---|---|---|---|---|---|
| Daily Outcome | Mindfulness Estimate (SE) | CBT-Pain Estimate (SE) | Education Estimate (SE) | Main Effect of Group | Interaction Effect with Group |
| Catastrophizing (1-5) | |||||
| Intercept | 2.014 (0.100) | 2.075 (0.092) | 2.045 (0.109) | F (2,140) = 0.10 | |
| Δ Pain | 0.015 (0.002)**** | 0.017 (0.002)**** | 0.011 (0.002)**** | F (2,4044) = 2.17 | |
| Control (0-10) | |||||
| Intercept | 7.082 (0.280) | 5.853 (0.294) | 5.990 (0.369) | F (2,140) = 4.65* | |
| Δ Pain | −0.026 (0.010)** | −0.043 (0.006)**** | −0.039 (0.007)**** | F (2,4026) = 0.28 | |
| Fatigue (0-100) | |||||
| Intercept | 27.076 (2.562) | 35.248 (2.590) | 30.145 (2.391) | F (2,140) = 2.78 | |
| Δ Pain | 0.484 (0.047)**** | 0.439 (0.049)**** | 0.443 (0.044)**** | F (2,4067) = 0.78 | |
| Morning Disability (1-5) | |||||
| Intercept | 2.861 (0.165) | 3.324 (0.182) | 3.088 (0.161) | F (2,140) = 1.90 | |
| Δ Pain | 0.023 (0.003)**** | 0.019 (0.003)**** | 0.021 (0.003)**** | F (2,4063) = 0.49 | |
| Serene affect (1-5) | |||||
| Intercept | 2.926 (0.124) | 2.767 (0.111) | 2.945 (0.103) | F (2,139) = 0.76 | |
| Δ Pain | −0.005 (0.001)**** | −0.012 (0.001)**** | −0.011 (0.001)**** | F (2,3958) = 2.47 | |
| Δ Stress | −0.271 (0.060)**** | −0.246 (0.049)**** | −0.281 (0.042)**** | F (2,3958) = 0.08 | |
| Anxious affect (1-5) | |||||
| Intercept | 1.214 (0.051) | 1.288 (0.067) | 1.227 (0.046) | F (2,139) = 0.52 | |
| Δ Pain | 0.001 (0.001) | 0.002 (0.001)** | 0.002 (0.001)* | F (2,3941) = 2.00 | |
| Δ Stress | 0.162 (0.043)**** | 0.109 (0.034)*** | 0.155 (0.042)*** | F (2,3941) = 1.00 | |
Note. Δ Pain = person-centered pain; Δ Stress = person-centered stress. All models included Δ Pain as a random effect and an AR(1) error structure to model significant daily covariation.
Models were estimated for each group separately.
Models compared groups by including the following predictors: Group, Δ Pain (Δ Stress), and Group X Δ Pain (Δ Stress) interactions.
p < .05.
p < .01.
p < .001.
p < .0001
Findings from within-group models were generally consistent with prediction. Daily pain episodes were strongly related to same-day decreases in perceived pain control and serene affect, and increases in catastrophizing, disability, and fatigue in all groups, and to increases in anxious affect in the CBT-P and E groups (ps < .05). In a similar vein, daily stress episodes were related to same-day decreases in serene affect and increases in anxious affect in all groups (ps < .05). Of note, between-group comparisons at pre-treatment revealed that groups were comparable in pain and stress reactivity across all outcomes (ps > .05). With regard to overall levels of outcomes aggregated across the 30 days of pre-treatment diaries, groups were comparable in their levels of catastrophizing, disability, fatigue, and serene and anxious affects (Group main effect ps > .05). However, the M group reported higher overall levels of pain control than did the CBT-P (t (97) = 3.01, p < .01) and E groups (t (89) = 2.40, p < .02).
Thus, pain and stress episodes predicted same-day changes in cognitions, physical symptoms, and affects, and the magnitude and direction of these changes were comparable across groups at pre-treatment. Taken together, these findings suggest that random assignment by cluster to intervention condition yielded groups that were comparable in pain- and stress-reactivity at pre-treatment.
Intervention Effects on Pain and Stress Reactivity for E, P, and M Groups
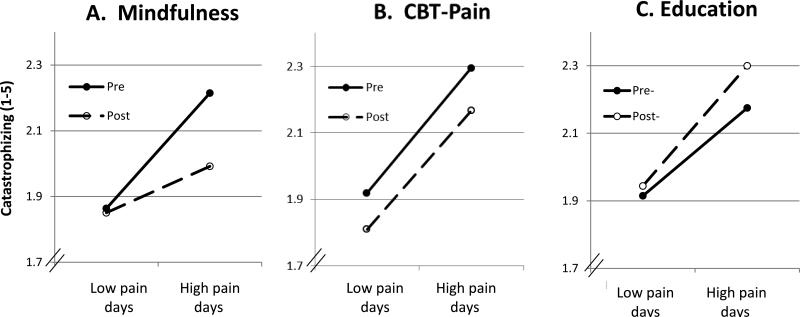
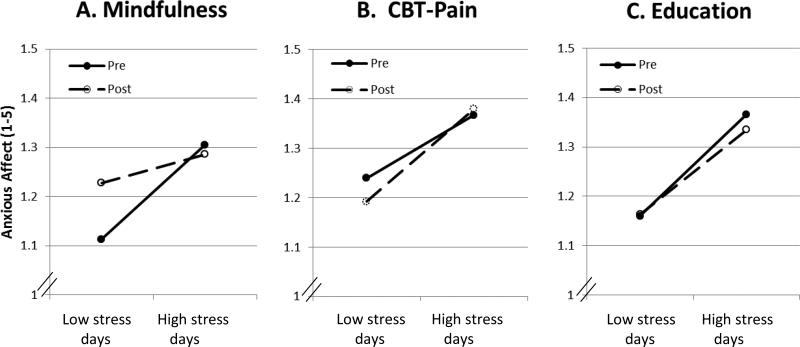
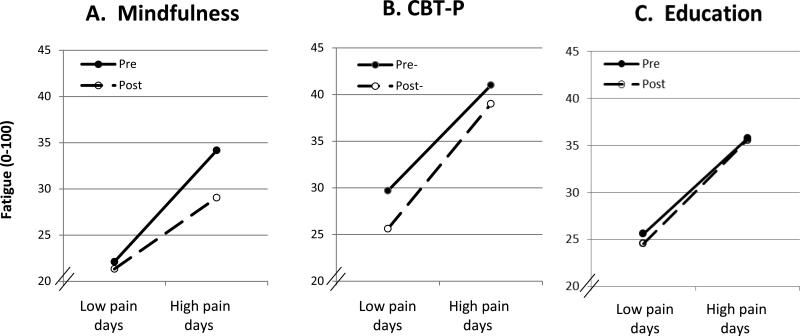
Evaluation of intervention effects began with the examination of changes in pain- and stress-reactivity within each group separately. Although not the focus of the current study, we also report changes from pre- to post-intervention in aggregated levels of each daily outcome, two of which were reported in a previous paper (i.e., pain catastrophizing and control; Zautra et al., 2008). The results of the analyses are summarized in Table 2 and illustrated in Figures 2-4.
Table 2.
Parameter Estimates (Standard Errors) from Multilevel Models of Pre-to-post Intervention Change in Daily Pain- and Stress-reactivity for Mindfulness (M; n=47), CBT-Pain (P; n=52) and Education (E; n=44) Groups
| Daily Outcome | Effects within groupa |
Group differencesb | ||
|---|---|---|---|---|
| Mindfulness Estimate (SE) | CBT-Pain Estimate (SE) | Education Estimate (SE) | ||
| Catastrophizing (1-5) | ||||
| Intercept | 2.025 (0.097) | 2.081 (0.090) | 2.045 (0.113) | |
| Time: Pre-post | −0.085 (0.033)* | −0.103 (0.027)*** | 0.081 (0.033)* | M, P > E |
| Δ Pain | 0.015 (0.002)**** | 0.017 (0.002)**** | 0.010 (0.002)**** | |
| Time X Δ Pain | −0.006 (0.002)** | 0.001 (0.002) | 0.004 (0.002)* | M > P, E |
| Control (0-10) | ||||
| Intercept | 7.091 (0.307) | 5.844 (0.294) | 5.983 (0.337) | |
| Time: Pre-post | −0.040 (0.086) | 0.291 (0.087)** | 0.269 (0.109)* | P, E > M |
| Δ Pain | −0.031 (0.010)** | −0.043 (0.006)**** | −0.039 (0.008)**** | |
| Time X Δ Pain | −0.008 (0.007) | 0.015 (0.005)** | −0.002 (0.006) | P > M, E |
| Fatigue (0-100) | ||||
| Intercept | 27.031 (2.609) | 35.343 (2.437) | 30.044 (2.431) | |
| Time: Pre-post | −1.579 (0.843) | −3.049 (0.760)*** | −1.665 (0.869) | |
| Δ Pain | 0.506 (0.047)**** | 0.434 (0.044)**** | 0.470 (0.044)**** | |
| Time X Δ Pain | −0.152 (0.052)** | 0.079 (0.040)* | 0.013 (0.047) | M > P, E |
| Morning Disability (1-5) | ||||
| Intercept | 2.850 (0.153) | 3.328 (0.174) | 3.072 (0.157) | |
| Time: Pre-post | −0.460 (0.045)**** | −0.313 (0.041)**** | −0.327 (0.049)**** | |
| Δ Pain | 0.023 (0.003)**** | 0.018 (0.002)**** | 0.021 (0.003)**** | |
| Time X Δ Pain | −0.007 (0.003)** | 0.004 (0.002)* | 0.001 (0.002) | M > P, E |
| Serene affect (1-5) | ||||
| Intercept | 2.924 (0.122) | 2.758 (0.109) | 2.944 (0.108) | |
| Time: Pre-post | 0.184 (0.034)**** | 0.025 (0.029) | −0.003 (0.036) | M > P,E |
| Δ Pain | −0.005 (0.001)**** | −0.012 (0.001)**** | −0.011 (0.001)**** | |
| Δ Stress | −0.258 (0.054)**** | −0.237 (0.043)**** | −0.268 (0.043)**** | |
| Time X Δ Pain | −0.004 (0.002) | 0.003 (0.002) | 0.003 (0.002) | |
| Time X Δ Stress | 0.111 (0.051)* | 0.028 (0.046) | 0.034 (0.053) | |
| Anxious affect (1-5) | ||||
| Intercept | 1.212 (0.054) | 1.301 (0.063) | 1.223 (0.044) | |
| Time: Pre-post | 0.035 (0.020) | −0.001 (0.023) | −0.007 (0.023) | |
| Δ Pain | 0.000 (0.001) | 0.002 (0.001) | 0.003 (0.001)* | |
| Δ Stress | 0.156 (0.022)**** | 0.134 (0.023)**** | 0.165 (0.025)**** | |
| Time X Δ Pain | 0.003 (0.002) | −0.001 (0.001) | −0.002 (0.001) | |
| Time X Δ Stress | −0.072 (0.033)* | 0.040 (0.035) | 0.036 (0.037) | M > P, E |
Note. Δ Pain = person-centered pain; Δ Stress = person-centered stress. Time is coded Pre=0, Post = 1. All models included Δ Pain as a random effect and an AR(1) error structure to model significant daily covariation.
Models were estimated for each group separately.
Contrasts are from models that included Group, Time, Δ Pain (Δ Stress), and their interactions.
p < .05.
p < .01.
p < .001.
p < .0001.
Figure 2.
Pre- and post-intervention within-person relations between low (− 1 SD) and high (+ 1 SD) pain days and catastrophizing for mindfulness (Panel A), cognitive-behavioral treatment for pain (CBT-P; Panel B), and arthritis education (Panel C) groups. (A flatter slope indicates less daily reactivity to pain.)
Figure 4.
Pre- and post-intervention within-person relations between low (− 1 SD) and high (+ 1 SD) stress days and anxious affect for mindfulness (Panel A), cognitive-behavioral treatment for pain (CBT-P; Panel B), and arthritis education (Panel C) groups. (A flatter slope indicates less daily reactivity to stress.)
The M group showed the broadest changes from pre- to post-treatment in pain- and stress-reactivity of the three groups. The M group showed less pronounced increases from pre- to post-treatment in the catastrophizing associated with a daily pain episode (Time × Δ Pain t = −2.91, p < .004). Figure 2, Panel A, depicts the pre- and post-intervention relations between daily pain and catastrophizing in the M group, and highlights that the strength of the association weakened over time. The M group also showed pre-to-post improvement in relations between pain episodes and changes in disability and fatigue (Time ts < −2.69, ps < .008), and between stress episodes and changes in serene affect (Time × Δ Stress t = 2.18, p < .03), and anxious affect (Time × Δ Stress t = −2.17, p < .03). Figure 3, Panel A, depicts the pre- and post-intervention relations between daily pain and fatigue, and Figure 4, Panel A the pre- and post-intervention relations between daily stress and anxious affect in the M group. With regard to changes in overall levels of each outcome, the M group showed pre-to-post improvement in levels of catastrophizing (Time t = −2.54, p < .02), disability (Time t = −10.17, p < .0001), and serene affect (Time t = 5.48, p < .0001).
Figure 3.
Pre- and post-intervention within-person relations between low (− 1 SD) and high (+ 1 SD) pain days and fatigue for mindfulness (Panel A), cognitive-behavioral treatment for pain (CBT-P; Panel B), and arthritis education (Panel C) groups. (A flatter slope indicates less daily reactivity to pain.)
The CBT-P group showed less pronounced decreases from pre- to post-intervention in perceived pain control on days of high pain (Time × Δ Pain t = 2.89, p < .004). However, the CBT-P group evidenced no change in the relations between daily pain and stress episodes and catastrophizing, serene affect, or anxious affect (Figures 2-4, Panel B). Moreover, the CBT-P group actually showed greater pain-reactivity from pre- to post-treatment, reflected in strengthened associations between daily pain episodes and same-day fatigue and disability (Time × Δ Pain ts > 1.97, ps < .05; see Figure 3, Panel B). With regard to changes in overall levels of each outcome, the CBT-P group showed improvement from pre- to post-treatment in levels of catastrophizing (Time t = −3.85, p < .0003), as well as pain control (Time t = 3.35, p < .002), disability (Time t = −7.55, p < .0001), and fatigue (Time t = −4.01, p < .0002).
The E group showed no pre- to post-intervention change in the relations between pain and stress episodes and any outcome (see Figures 2-4, Panel C). Moreover, the E group showed greater pain-reactivity from pre to post, reflected in strengthened associations between daily pain episodes and same-day catastrophizing from pre-to-post treatment (Time × Δ Pain t = 2.15, p < .05; see Figure 3, Panel C). With regard to changes in overall levels of outcomes, the E group showed improvement in levels of perceived pain control (Time t = 2.47, p < .02) and disability (Time t = −6.73, p < .0001), but worsening in levels of catastrophizing (Time t = 2.49, p < .02).
Group Differences in Magnitude of Pre-post Changes in Reactivity
Findings of analyses comparing the magnitude of change in daily pain- and stress-reactivity from pre- to post-treatment across groups indicated that groups showed pronounced differences in response to treatment. On the whole, the M group yielded more substantial benefits than the other two groups. M yielded greater improvements than did CBT-P and E in pain-related changes in catastrophizing (Group × Time × Δ Pain ts < − 2.68, ps < .006; see Figure 2), morning disability (Group × Time × Δ Pain ts < − 2.37, ps < .02), and fatigue (Group × Time × Δ Pain ts < − 2.35, ps < .02; see Figure 3). The M group also showed greater improvement in stress-related changes in anxious affect than did CBT-P and E (Group × Time × Δ Pain ts <− 2.07, ps < .04; see Figure 4). In contrast, CBT-P exhibited greater pre-to-post improvements in pain-related changes in perceived control than did M and E (Group × Time × Δ Pain ts > 2.25, ps < .03). No other group differences in reactivity achieved significance. Comparisons of the magnitude of pre-post-change on levels of outcomes between groups revealed the both M and CBT-P showed greater decreases in levels of pain catastrophizing relative to the E group (Group × Time ts < −3.44, ps < .001), whereas the CBT-P and E groups showed greater increases in levels of pain control compared to the M group (Group × Time ts > 2.30, ps < .03), as reported in Zautra et al. (2008). Finally, the M group improved in levels of serene affect more than did CBT-P and E (Group × Time ts > 3.58, ps < .0001), and in levels of disability more than the CBT-P group (Group × Time t = − 2.25, p < .03).
The original report of this trial examined whether intervention effects on aggregated levels of daily outcomes depended on whether individuals reported a history of recurrent depression (for details of depression assessment, see Zautra et al., 2008). Those findings indicated that the M treatment generally was more beneficial than CBT-P or E for the patients with a recurrent depression history. Here we explored whether a history of recurrent depression (RD; coded 0, 1) moderated treatment effects on daily pain- and/or stress-reactivity by repeating all analyses that compared treatment groups and including the RD main effect and its interaction terms in the models. Findings revealed that RD moderated pre- to post-treatment changes in pain reactivity for a single daily outcome, fatigue (RD × Group × Time × Δ Pain F = 6.56, p < .0002). Follow-up analyses within each RD group revealed that for individuals with a history of recurrent depression, M yielded greater improvements than did CBT-P and E in pain-related changes in fatigue (Group × Time × Δ Pain ts < − 3.59, ps < .0003). In contrast, for individuals without a depression history, improvements from pre- to post-treatment were comparable across groups (Group × Time × Δ Pain ts < 1.95, ps > .06).
Discussion
Our primary aim in this study was to evaluate the differential effects of distinct interventions for RA on cognitive, symptom, and affective responses to daily episodes of pain and stress. Because CBT-P targeted the development of pain coping skills, we expected it to dampen reactivity to daily pain episodes. In contrast, because M targeted skills to cope with a range of aversive experiences, we expected it to dampen not only pain but also stress reactivity day-to-day. The results suggested that on the whole, the mindful awareness and acceptance treatment was more successful in reducing daily reactivity to both pain and stress than either cognitive-behavioral treatment or arthritis education. Specifically, mindful awareness and acceptance was the most effective approach in dampening pain-contingent increases in catastrophizing, fatigue, and disability, and stress-contingent increases in anxious affect. The CBT and education treatments outperformed mindful awareness and acceptance in one domain: limiting pain-contingent decreases in perceived control. Of note, none of the treatments altered the magnitude of pain- or stress-contingent declines in serene affect, including the mindful awareness and acceptance treatment. From a therapeutic perspective, these findings suggest that a mindful awareness and acceptance approach in the treatment of individuals with RA alters how they respond to daily exacerbations of pain and interpersonal stress, limiting effects on fatigue, disability, and anxious affect. These results add to a growing body of evidence regarding the utility of mindful awareness and acceptance-based approaches to decrease reactivity to aversive experiences (Garland et al., 2012).
What can account for the unique benefits of the mindfulness-oriented intervention in real-world contexts relative to CBT, a widely-used, evidence-based treatment for chronic pain? A plausible possibility is that training individuals to simply notice and label aspects of current aversive experiences can make them more adept at detecting even subtle affective cues, allowing them to begin to regulate their responses to pain and stress episodes before emotions become too intense (Teper, Segal, & Inzlicht, 2013). In fact, some evidence suggests that mindfulness-based treatment promotes adaptive changes in fundamental attentional processes. In particular, mindfulness helps to shift attention away from affect-laden appraisals (e.g., catastrophizing) toward the sensory aspects of experience, reducing reactivity to aversive events in individuals with somatic symptoms (Garland et al., 2012). Among pain patients, those exposed to mindfulness training versus a control condition showed decreases in attentional bias to and increases in disengagement from pain-related cues, assessed through use of the dot probe technique (Garland & Howard, 2013; Vago & Nakamura, 2011). A similar pattern of findings is evident in comparisons of long-term meditators and nonmeditators; for example, experienced meditators and non-meditators are similar in the threshold of stimulation required to induce pain, but meditators show less neural activation in anticipation of the painful stimulus and a less negative appraisal of their pain compared to nonmeditators (Brown & Jones, 2010). Thus, mindfulness-based treatment may yield benefits in part because it refocuses attention, thereby diminishing hypervigilance toward and cognitive elaboration of threatening experiences.
CBT, on the other hand, involves reinterpreting the meaning of an experience to change one's emotional response to it. Although cognitive reappraisal is effective, it is often deployed after emotions have intensified, and thus its success hinges on the availability of sufficient cognitive resources to implement it. Yet existing evidence suggests that the demands imposed by intense pain and stress may deplete the reservoir of self-regulatory resources needed to cope effectively (Baumeister & Heatherton, 1996). In fact, individuals choose to engage in reappraisal to regulate their emotions only when negative emotional intensity is low, but prefer to use distraction when negative emotional intensity is high (Sheppes, Scheibe, Suri, & Gross, 2011). Moreover, even when individuals are well-trained in the use of cognitive reappraisal strategies to manage fear responses to an aversive stimulus, they use those strategies effectively only in low but not high stress conditions (Raio, Orederu, Palazzolo, Shurick, & Phelps, 2013).
Nevertheless, acceptance is not always more effective than reappraisal in reducing reactivity to provocation. Investigations employing brief laboratory inductions of acceptance versus reappraisal strategies to regulate responses to aversive experiences in the immediate term have yielded mixed results. Some findings have favored reappraisal (Hofmann, Heering, Sawyer, & Asnaani, 2009; Szasz, Szentagotai, & Hofmann, 2011), others acceptance (Gutiérrez, Luciano, Rodríguez, & Fink, 2004), and still others, neither approach (Low, Stanton, & Bower, 2008; Wolgast, Lundh, & Viborg, 2011). In their meta-analysis of experiments that compared brief inductions of acceptance with other emotion regulation strategies, Kohl et al. (2012) found some areas of superiority for acceptance. Acceptance was more effective in increasing pain tolerance across samples, and in limiting acute distress in clinical but not healthy samples. Thus, the relative benefits of acceptance, reappraisal, or other strategies are likely to hinge on a host of factors, including the nature of the stressor, the characteristics of the individual (e.g., health status), and the time frames of both the intervention and the outcome assessment.
Interventions for chronic pain strive to build both coping resources and the skill needed to apply those resources when circumstances require it. To what extent do they succeed? One means of addressing this question is to consider the findings regarding intervention effects on daily pain reactivity side-by-side with those for pre-post changes in overall levels for pain cognitions. With regard to catastrophizing, although both the mindfulness and CBT conditions improved overall levels, only mindfulness also improved individuals’ ability to limit catastrophizing when confronting periods of high daily pain. For pain control, CBT improved not only overall levels of perceived control, but also individuals’ capacity to sustain a sense of control during pain episodes to a greater extent than did mindfulness. Taken together, this pattern of results underscores the fact that bolstering coping resources in general does not necessarily enhance the capacity of individuals to draw on those resources when they are most needed. Maximizing intervention effects, then, is likely to entail ensuring that individuals are developing not only a repertoire of coping strategies, but also the proficiency to use them effectively.
The study has a number of noteworthy strengths. To our knowledge, this is the first study to capitalize on the richness of pre- and post-intervention diary data to examine changes in the dynamics of daily coping with pain and stress in a large randomized clinical trial. The design compared two distinct treatments (i.e., mindfulness and CBT) with an active control condition (i.e., arthritis education), providing the opportunity to test for differential intervention effects on daily pain and stress reactivity beyond the effects of group support, therapist contact, the passage of time, and other nonspecific factors. Finally, the low level of attrition from intervention groups and of missing diary data strengthens confidence in the validity of the findings.
The study also has several limitations that deserve comment. First, the sample was comprised primarily of Caucasian women with RA, constraining generalizability of the findings to individuals with a similar background and pain condition. Second, although our treatments were manualized and clinicians supervised throughout treatment delivery, the clinicians’ training regarding treatment delivery did not include extensive opportunities for role-playing, rehearsal, or booster sessions. Moreover, we did not include obtain and evaluate recordings of sessions to verify clinicians’ competence and compliance with the treatment manuals, verification that is strongly recommended and would enhance the internal validity of the trial (Perepletchikova, Treat, & Kazdin, 2007). Third, the daily assessment involved paper-and-pencil diaries. Although diaries were mailed back to the research team on a daily basis, and evaluation of postmarks assured compliance with mailing instructions, we cannot assure that the diaries were completed in the evening. Fourth, the differences we observed were statistically significant but very small in magnitude. For example, a 30-point increase in daily pain above a person's average daily pain predicted an increase in same-day fatigue at pre- and post-intervention for the M group of 15.2 and 10.6 points, respectively; for the CBT-P group of 13.0 and 15.4 points, respectively; and for the E group of 14.1 and 14.5 points, respectively. The clinical impact of changes of this magnitude remains to be determined. Fifth, the models we evaluated tested same-day relations between pain and stress and study outcomes, but did not test for carryover effects from one day to the next. Future investigations that include within-day assessments may be better positioned to capture the temporal ordering of the processes of interest, which likely occur during a time frame ranging from minutes to hours. Sixth, the study demonstrated that CBT and mindfulness-based treatment impacted daily reactivity, but it did not address how these reductions were accomplished. Although from a theoretical perspective, reappraisal and acceptance are central components of CBT and M approaches, respectively, we did not explicitly measure changes in the capacity for decentering, awareness, reappraisal, or acceptance from pre- to post-treatment. As a result, we cannot be certain that either reappraisal or acceptance were the “active” ingredients driving the changes we observed in reactivity. Moreover, because the interventions were complex, it is possible that differences between groups are due to different “doses” of the active ingredients delivered in each treatment. For example, the less robust effects of CBT versus M may have been due to the inclusion of components that may be less effective in reducing reactivity than is reappraisal, such as relaxation. As a result, the “doses” of training in reappraisal offered in the CBT condition may have been smaller than the “doses” of training in awareness and acceptance offered in the M condition, and may account for the relative inferiority of CBT in comparison with M.
In summary, the present study suggests that mindful awareness and acceptance treatment targeting regulation of emotion yields benefits in the management of daily pain and stress that are broader than those offered by a cognitive-behavioral approach or arthritis education. Mindfulness limited the effects of pain flares on catastrophizing, fatigue, and disability, and of stress on anxious affect. However, despite its emphasis on boosting positive engagement, it did not help individuals sustain serene affect in the face of pain and stress episodes. On the other hand, CBT limited the effects of pain flares on perceived control. Although small in magnitude, the effects demonstrated here reflect changes in day-to-day processes, and the benefits to overall functioning may increase as small daily changes are compounded over time. These findings serve as a reminder that therapeutic change can be effected in subtler ways than can be assessed by static measurement of primary outcomes. Indeed, psychological treatments in general attempt to help people change their habitual responses to ongoing challenges, and success of therapies over the long term depends on the application of skills learned in treatment to problems in daily life. Even with the advent of technological advances, diary assessments impose a larger burden on research participants than do more global types of assessment. Yet when they can shed light on important aspects of how treatments work, diary reports can be worth the additional burden. A daily process approach is one promising avenue toward identifying specific, dynamic mechanisms of change and refining interventions.
Acknowledgments
This study was the National Institutes of Health Clinical Trial NCT00475111, and was supported by grant R01 AR41687 from the National Institute of Musculoskeletal, Immune, and Skin Disease.
Contributor Information
Mary C. Davis, Department of Psychology, Arizona State University
Alex J. Zautra, Department of Psychology, Arizona State University
Laurie D. Wolf, Department of Psychology, Arizona State University
Howard Tennen, Department of Community Medicine and Health Care, University of Connecticut Health Center..
Ellen W. Yeung, Department of Psychology, Arizona State University
References
- Affleck G, Zautra A, Tennen H, Armeli S. Multilevel daily process designs for consulting and clinical psychology: A preface for the perplexed. Journal of Consulting and Clinical Psychology. 1999;67:746–754. doi: 10.1037//0022-006x.67.5.746. doi: http://dx.doi.org.ezproxy1.lib.asu.edu/10.1037/0022-006X.67.5.746. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and intrepreting interactions. Sage; Thousand Oaks, CA: 1991. [Google Scholar]
- Astin JA, Beckner W, Soeken K, Hochberg MC, Berman B. Psychological interventions for rheumatoid arthritis: A meta-analysis of randomized controlled trials. Arthritis Care & Research. 2002;47:291–302. doi: 10.1002/art.10416. doi: http://dx.doi.org/10.1002/art.10416. [DOI] [PubMed] [Google Scholar]
- Banks SM, Kerns RD. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychological Bulletin. 1996;119:95–110. doi: http://dx.doi.org/10.1037/0033-2909.119.1.95. [Google Scholar]
- Baumeister RF, Heatherton TF. Self-regulation failure: An overview. Psychological Inquiry. 1996;7:1–15. doi: 10.1207/s15327965pli0701_1. [Google Scholar]
- Brown CA, Jones AKP. Meditation experience predicts less negative appraisal of pain: Electrophysiological evidence for the involvement of anticipatory neural responses. Pain. 2010;150:428–438. doi: 10.1016/j.pain.2010.04.017. doi: http://dx.doi.org/10.1016/j.pain.2010.04.017. [DOI] [PubMed] [Google Scholar]
- Csikszentmihalyi M, Larson R. Validity and reliability of the experience sampling method. Journal of Nervous and Mental Disease. 1987;175:526–536. doi: 10.1097/00005053-198709000-00004. [DOI] [PubMed] [Google Scholar]
- Dixon KE, Keefe FJ, Scipio CD, L. P, Caitlin M. Psychological interventions for arthritis pain management in adults: A meta-analysis. Health Psychology. 2007;26:241–250. doi: 10.1037/0278-6133.26.3.241. doi: 10.1037/0278-6133.26.3.241. [DOI] [PubMed] [Google Scholar]
- Epstein S. The stability of behavior: I. On predicting most of the people much of the time. Journal of Personality and Social Psychology. 1979;37:1097. [Google Scholar]
- Garland EL, Gaylord SA, Palsson O, Faurot K, Mann JD, Whitehead WE. Therapeutic mechanisms of a mindfulness-based treatment for IBS: Effects on visceral sensitivity, catastrophizing, and affective processing of pain sensations. Journal of Behavioral Medicine. 2012;35:591–602. doi: 10.1007/s10865-011-9391-z. doi: 10.1007/s10865-011-9391-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Howard MO. Mindfulness-oriented recovery enhancement reduces pain attentional bias in chronic pain patients. Psychotherapy and Psychosomatics. 2013;82:311–318. doi: 10.1159/000348868. doi: 10.1159/000348868. [DOI] [PubMed] [Google Scholar]
- Geschwind N, Peeters F, Drukker M, van Os J, Wichers M. Mindfulness training increases momentary positive emotions and reward experience in adults vulnerable to depression: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2011;79:618. doi: 10.1037/a0024595. doi: 10.1037/a0024595. [DOI] [PubMed] [Google Scholar]
- Gil KM, Anthony KK, Carson JW, Redding-Lallinger R, Daeschner CW, Ware RE. Daily coping practice predicts treatment effects in children with sickle cell disease. Journal of Pediatric Psychology. 2001;26:163–173. doi: 10.1093/jpepsy/26.3.163. doi: 10.1093/jpepsy/26.3.163. [DOI] [PubMed] [Google Scholar]
- Gutiérrez O, Luciano C, Rodríguez M, Fink BC. Comparison between an acceptance-based and a cognitive-control-based protocol for coping with pain. Behavior Therapy. 2004;35:767–783. doi: 10.1016/S0005-7894(04)80019-4. [Google Scholar]
- Hamilton NA, Affleck G, Tennen H, Karlson C, Luxton D, Preacher KJ, Templin JL. Fibromyalgia: The role of sleep in affect and in negative event reactivity and recovery. Health Psychology. 2008;27:490–497. doi: 10.1037/0278-6133.27.4.490. doi: 10.1037/0278-6133.27.4.490. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Duckworth MP. Acceptance and commitment therapy and traditional cognitive behavior therapy approaches to pain. Cognitive and Behavioral Practice. 2006;13:185–187. doi: 10.1016/j.cbpra.2006.04.002. [Google Scholar]
- Hofmann SG, Heering S, Sawyer AT, Asnaani A. How to handle anxiety: The effects of reappraisal, acceptance, and suppression strategies on anxious arousal. Behaviour Research and Therapy. 2009;47:389–394. doi: 10.1016/j.brat.2009.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: A comparison of six methods. Pain. 1986;27:117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delacorte; New York: 1990. [Google Scholar]
- Kohl A, Rief W, Glombiewski JA. How effective are acceptance strategies? A meta-analytic review of experimental results. Journal of Behavior Therapy and Experimental Psychiatry. 2012;43:988–1001. doi: 10.1016/j.jbtep.2012.03.004. doi: 10.1016/j.jbtep.2012.03.004. [DOI] [PubMed] [Google Scholar]
- Lawrence RC, Felson DT, Helmick CG, Arnold LM, Choi H, Deyo RA, Wolfe F. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis & Rheumatism. 2008;58:26–35. doi: 10.1002/art.23176. doi: 10.1002/art.23176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis & Rheumatism. 1989;32:37–44. doi: 10.1002/anr.1780320107. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- Low CA, Stanton AL, Bower JE. Effects of acceptance-oriented versus evaluative emotional processing on heart rate recovery and habituation. Emotion. 2008;8:419. doi: 10.1037/1528-3542.8.3.419. doi: 10.1037/1528-3542.8.3.419. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Gross RT. The role of pain-related anxiety reduction in the outcome of multidisciplinary treatment for chronic low back pain: Preliminary results. Journal of Occupational Rehabilitation. 1998;8:179–189. doi: 10.1023/A:1021374322673. [Google Scholar]
- Morley S, Eccleston C, Williams A. Systematic review and meta-analysis of randomized controlled trials of cognitive behaviour therapy and behaviour therapy for chronic pain in adults, excluding headache. Pain. 1999;80:1–13. doi: 10.1016/s0304-3959(98)00255-3. doi: 10.1016/S0304-3959(98)00255-3. [DOI] [PubMed] [Google Scholar]
- Perepletchikova F, Treat TA, Kazdin AE. Treatment integrity in psychotherapy research: Analysis of the studies and examination of the associated factors. Journal of Consulting and Clinical Psychology. 2007;75:829–841. doi: 10.1037/0022-006X.75.6.829. doi: 10.1037/0022-006X.75.6.829. [DOI] [PubMed] [Google Scholar]
- Raio CM, Orederu TA, Palazzolo L, Shurick AA, Phelps EA. Cognitive emotion regulation fails the test. Proceedings of the National Academy of Sciences. 2013;110:15139–15144. doi: 10.1073/pnas.1305706110. doi: 10.1073/pnas.1305706110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson MD, Clore GL. Belief and feeling: Evidence for an accessibility model of emotional self-report. Psychological Bulletin. 2002;128:934–960. doi: 10.1037/0033-2909.128.6.934. doi: 10.1037/0033-2909.128.6.934. [DOI] [PubMed] [Google Scholar]
- Rosenstiel AK, Keefe FJ. The use of coping strategies in chronic low back pain patients: Relationship to patient characteristics and current adjustment. Pain. 1983;17:33–44. doi: 10.1016/0304-3959(83)90125-2. doi: 10.1016/0304-3959(83)90125-2. [DOI] [PubMed] [Google Scholar]
- Sheppes G, Scheibe S, Suri G, Gross JJ. Emotion-regulation choice. Psychological Science. 2011;22:1391–1396. doi: 10.1177/0956797611418350. doi: 10.1177/0956797611418350. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annual Review of Clinical Psychology. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Singer JD. Using SAS PROC MIXED to fit multilevel models, hierarchical models and individual growth models. Journal of Educational and Behavioral Statistics. 1998;24:323–355. doi: 10.3102/10769986023004323. [Google Scholar]
- Smeets RJEM, Vlaeyen JWS, Kester ADM, Knottnerus JA. Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral Tteatment in chronic low back pain. The Journal of Pain. 2006;7:261–271. doi: 10.1016/j.jpain.2005.10.011. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Ter Kuile M, Kole-Snijders AM, Hutten Mansfeld M, Den Ouden D-J, Vlaeyen JW. Catastrophizing and internal pain control as mediators of outcome in the multidisciplinary treatment of chronic low back pain. European Journal of Pain. 2004;8:211–219. doi: 10.1016/j.ejpain.2003.08.003. doi: 10.1016/j.ejpain.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Strand EB, Zautra AJ, Thoresen M, Ødegård S, Uhlig T, Finset A. Positive affect as a factor of resilience in the pain—negative affect relationship in patients with rheumatoid arthritis. Journal of Psychosomatic Research. 2006;60:477–484. doi: 10.1016/j.jpsychores.2005.08.010. doi: 10.1016/j.jpsychores.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Suls J, Martin R. The daily life of the garden-variety neurotic: Reactivity, stressor exposure, mood spillover, and maladaptive coping. Journal of Personality. 2005;73:1485–1510. doi: 10.1111/j.1467-6494.2005.00356.x. doi: 10.1111/j.1467-6494.2005.00356.x. [DOI] [PubMed] [Google Scholar]
- Szasz PL, Szentagotai A, Hofmann SG. The effect of emotion regulation strategies on anger. Behaviour Research and Therapy. 2011;49:114–119. doi: 10.1016/j.brat.2010.11.011. doi: 10.1016/j.brat.2010.11.011. [DOI] [PubMed] [Google Scholar]
- Teper R, Segal ZV, Inzlicht M. Inside the mindful mind: How mindfulness enhances emotion regulation through improvements in executive control. Current Directions in Psychological Science. 2013;22:449–454. doi: 10.1177/0963721413495869. [Google Scholar]
- Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain. 2007;127:276–286. doi: 10.1016/j.pain.2006.09.005. doi: 10.1016/j.pain.2006.09.005. [DOI] [PubMed] [Google Scholar]
- Vago DR, Nakamura Y. Selective attentional bias towards pain-related threat in fibromyalgia: Preliminary evidence for effects of mindfulness meditation training. Cognitive Therapy and Research. 2011;35:581–594. doi: 10.1007/s10608-011-9391-x. [Google Scholar]
- Veehof MM, Oskam M-J, Schreurs KM, Bohlmeijer ET. Acceptance-based interventions for the treatment of chronic pain: A systematic review and meta-analysis. Pain. 2011;152:533–542. doi: 10.1016/j.pain.2010.11.002. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Watson D. Intraindividual and interindividual analyses of positive and negative affect: Their relation to health complaints, perceived stress, and daily activities. Journal of Personality and Social Psychology. 1988;54:1020–1030. doi: 10.1037//0022-3514.54.6.1020. doi: http://dx.doi.org/10.1037/0022-3514.54.6.1020. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA. Manual for the Positive and Negative Affect Schedule - Expanded Form. University of Iowa. 1994 Retrieved from http://ir.uiowa.edu/psychology_pubs/11.
- Westhoff G, Buttgereit F, Gromnica-Ihle E, Zink A. Morning stiffness and its influence on early retirement in patients with recent onset rheumatoid arthritis. Rheumatology. 2008;47:980–984. doi: 10.1093/rheumatology/ken137. doi: 10.1093/rheumatology/ken137. [DOI] [PubMed] [Google Scholar]
- Wolgast M, Lundh L-G, Viborg G. Cognitive reappraisal and acceptance: An experimental comparison of two emotion regulation strategies. Behaviour Research and Therapy. 2011;49:858–866. doi: 10.1016/j.brat.2011.09.011. doi: 10.1016/j.brat.2011.09.011. [DOI] [PubMed] [Google Scholar]
- Yazici Y, Pincus T, Kautiainen H, Sokka T. Morning stiffness in patients with early rheumatoid arthritis is associated more strongly with functional disability than with joint swelling and erythrocyte sedimentation rate. Journal of Rheumatology. 2004;31:1723–1726. [PubMed] [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Nicassio P, Tennen H, Finan P, Irwin MR. Comparison of cognitive behavioral and mindfulness meditation interventions on adaptation to rheumatoid arthritis for patients with and without history of recurrent depression. Journal of Consulting and Clinical Psychology. 2008;76:408–421. doi: 10.1037/0022-006X.76.3.408. doi: 10.1037/0022-006X.76.3.408. [DOI] [PubMed] [Google Scholar]