Abstract
The National HIV/AIDS Strategy emphasizes the importance of bringing prevention to the most at-risk populations. Interventions targeting all men who have sex with men (MSM) fail in that respect because only a minority engages in behavior that is likely to lead to HIV infection. Previous studies have shown that MSM who seek male sexual partners in more than one venue type (e.g., bathhouse, cruising area, online) are most likely to engage in unprotected anal intercourse (UAI), compared to men who only meet partners in any one of these setting types or who do not use venues. The present study reports differences in prevalence of UAI among MSM by their use of venue sites to meet sexual partners. A probability sample of 459 bathhouse patrons completed exit surveys. In the three months before the current bathhouse visit, 63.5% visited a bathhouse (not including the visit at which they were recruited), 46.7% visited a cruising area, 46.5% used online cruise sites to find sex partners, and 30.9% reported UAI. While UAI was associated with online cruise site use, prevalence of UAI with men met online was relatively low. The odds of UAI among men who used all three venues was significantly higher compared to men using zero [Odds Ratio (OR)=4.4; 95% Confidence Interval (CI): 1.6, 12.1)] one (OR=5.3; 95% CI: 2.2, 12.8) or two venues (OR=4.3; 95% CI: 1.9, 9.6). The findings suggest that prevention would benefit from screening for venue use to help identify men with the greatest behavioral risk.
Keywords: MSM, Internet, bathhouses, cruising areas, sexual risk behavior
INTRODUCTION
Over the decades following the onset of the AIDS epidemic, studies repeatedly show that only a minority of men who have sex with men (MSM) engage in behavior that is likely to lead to HIV infection, even among men who are recruited from venues long associated with risk behavior, such as gay bathhouses (or saunas, including sex clubs), cruising areas (such as backrooms at bars, adult bookstores, parks, and public toilets) and online cruise sites (such as Craigslist and Adam4Adam) (Bolton, Vincke, & Mak, 1992; Coates et al., 1996; Colfax et al., 2001; Horvath, Bowen, & Williams, 2006; Martin, 1987; McKusick, Horstman, & Coates, 1985). Such consistent results suggest that prevention for MSM should be more narrowly focused toward those who are truly at risk for HIV. Such an approach is called for in the National HIV/AIDS Strategy (Collins & Diallo, 2010; White House Office of National AIDS Policy, 2010), which emphasizes the importance of bringing prevention to the most at risk populations.
A particular challenge has been to find this minority of MSM where they congregate in larger proportions. A study completed in the late 1990s obtained a probability sample of MSM recruited from the four U.S. cities with the highest HIV incidence: Chicago, New York, Los Angeles and San Francisco (Binson et al., 2001). Data from this study showed that MSM who sought male sexual partners both at gay bathhouses and at cruising areas reported more sexual partners and were significantly more likely to engage in UAI with a casual partner or in a public or group setting, compared to men who meet partners only at bathhouses or only in cruising areas. Thus it seemed that the bathhouse was an excellent venue to find a larger proportion of high-risk men than might be found in other settings (e.g., gay bars, social groups).
In addition to bathhouses and cruising areas, MSM historically have used communications media to meet other men for sex (e.g., personal ads in local papers, party phone lines, online bulletin boards) (Bartholome, Tewksbury, & Bruzzone, 2000; Tikkanen & Ross, 2000). However, the advent of the Internet and its online cruise sites (i.e., websites where MSM can arrange one-time sexual encounters) has greatly increased the opportunities for and immediacy of meeting sexual partners. This may raise the potential for engaging in high risk HIV-related behaviors. Research has established that a larger proportion of MSM than women or heterosexual men reported searching for sexual partners online (Kim, Kent, McFarland, & Klausner, 2001). A 2006 meta-analysis found that sexual partners were sought online by approximately 85% of MSM recruited via the Internet for research studies, and by 40% of MSM recruited via means other than the Internet (Liau, Millett, & Marks, 2006).
Physical and online venues differ in several important ways. First, in physical venues, MSM typically have sex where they meet; on the Internet, after making initial contact, men have to agree on a physical location to meet. Second, while many MSM find sexual partners on the Internet (Tikkanen & Ross, 2000), by definition sex must occur elsewhere, most typically in private locations (e.g., at home or at a hotel) where behaviors involving greater risk of HIV transmission are more likely to occur (Grov, 2012; Grov, Hirshfield, Remien, Humberstone, & Chiasson, 2013; Woods et al., 2007). Finally, although its veracity may be uncertain, personal information (e.g., name, HIV status) is available in many Internet cruise sites, as opposed to physical venues where such personal information is rarely exchanged (Hancock, Toma, & Ellison, 2007).
Based on the Binson et al. (2001) findings, one might expect that MSM who use both Internet cruise sites and physical venues to find sexual partners would be more likely to report sexual risk behavior than MSM who use only one type of venue. Two recent studies that used non-probability, opt-in web samples of MSM found that the prevalence of unprotected anal intercourse during the most recent sexual encounter with a new/first-time/casual male sex partner did not vary by whether they met the partner in Internet cruise sites or physical venues (Chiasson et al., 2007; Grov et al., 2013). However, in addition to the potential for self-selection bias inherent in opt-in sampling and limitations in the scope of results based on a single sexual encounter, these studies failed to directly address the apparent connection between venue use, or more specifically the use of multiple venue types, and sexual risk behavior. Another study (Grov, 2012) used time-location sampling, but respondents were categorized based on the venue where they were recruited (bathhouses vs. bars/clubs vs. Craigslist.org) rather than on which venues they used in a specified time period.
Two recent studies support the notion that higher risk behavior is associated with visiting multiple types of venues. Downing (2012) characterized men who completed a web-based survey as either high-frequency or low frequency in their use of the Internet to meet men for sex in the past 12 months. High-frequency users were more likely to visit physical sex venues and more likely to report UAI than low-frequency users. A recent study in East and Southeast Asia recruited MSM online and asked whether, in the prior six months, they met their male sex partners online or offline (Wei, Lim, Guadamuz, & Koe, 2013). Men who had met partners both online and offline were more likely to engage in a range of risk behaviors than men who had met partners only online or only offline, suggesting that the association of multiple venue use with HIV risk continues in the Internet age.
Taking the opposite approach, our study recruited from a physical venue and asked about online and offline partnering. Recruiting from a physical setting offered the additional advantage of being able to utilize time-location sampling to obtain a probability sample of bathhouse patrons to investigate differences in the prevalence of UAI among MSM by whether or not they visited each of three types of venues in the three months prior to the current bathhouse visit: bathhouses, cruising areas, and Internet cruise sites. We hypothesized that prevalence of UAI would increase as the number of venue types used increased.
METHODS
Data were collected as part of a larger mixed-methods study (Woods, Pollack, Blair, & Binson, 2012) designed to assess sexual networks among bathhouse patrons including where they meet partners, where they have sex, and what type of sex they have in that venue.
Sampling
The respondents were a probability sample of men (n=459) leaving either of two gay bathhouses operating within the city limits of the same California metropolitan area. A two-stage time probability cluster sample design was used to select bathhouse patrons. To facilitate implementation of this design, the daily operating hours of each bathhouse were divided into 2-hour recruitment shifts. In the first stage of selection, a sample of shifts was selected with probabilities proportional to the expected number of patrons (based on historical data provided by each bathhouse). In the second stage, within each selected shift, a fixed cluster size of x patrons was randomly selected. These two stages taken together produced an equal probability sample of patron visits. It is important to note that the sample is of visits rather than patrons. The probability of selection of an individual patron is proportional to the number of times he visited during the data collection period. Patrons who visited more often had a higher chance of being sampled than those who visited less frequently. As a part of the estimation procedure, the sample of visits was statistically weighted (inversely proportional to each patron’s total visits) to convert it to a sample of individual patrons. To produce unbiased sample estimates of patron behavior, the weights were also adjusted for selecting either more or fewer than x patrons in a sampled shift (i.e., adjusting for nonresponse and noncoverage). All data in this report are weighted.
Recruitment
Data collection occurred from March through August of 2007. This 26-week period consisted of 2,288 2-hour recruitment shifts. From these 2,288 shifts, 138 were randomly selected for data collection. For each selected shift, N men were expected to exit (based on business records of past patronage). The men actually exiting the bathhouse during a shift were counted and every nth exiting patron was selected for inclusion (where n=N/x, x=the number of interviews we aimed to obtain during each shift). Two-man teams were assigned to each randomly selected shift; one man to serve as counter while the other recruited each nth man exiting the club.
Each selected patron was approached to do an interview. A patron was considered eligible unless he said he had been interviewed previously, or was unable to give consent because of insufficient knowledge of either English or Spanish or appeared to the recruiter to be cognitively impaired. Patrons who agreed to participate were taken aside, consented, and completed the survey using audio-computer-assisted self-interview (ACASI). Participation was voluntary, anonymous, and reimbursed $20 after completing the survey. All procedures and measures were reviewed and approved by the Institutional Review Board of the University of California, San Francisco.
Measures
The exit survey first assessed participants’ sexual behavior during the just-completed bathhouse visit and their substance use in the past 24 hours. Respondents were then asked a series of questions about their same-gender sexual behavior in the three months immediately prior to (but not including) the just completed bathhouse visit including number of oral and anal sex partners, with the latter broken down into insertive or receptive anal sex partners, and each of these categories in turn divided into protected and unprotected anal sex partners. Respondents were also asked if they had oral or anal sex in the prior three months in each of seven venues:
Their own home.
Someone else’s home.
A bathhouse (including sex clubs).
Another commercial adult sex venue (like an adult movie theater or bookstore).
A public cruising area (like a beach, alley, or public men’s room).
A hotel room.
A car, truck, bus, train, plane or other public or private means of transit.
Respondents who did not report sexual contact in a bathhouse, commercial adult venue, or public cruising area were asked if they visited such a venue in the prior three months. Finally, respondents were asked, “Have you ever had sexual contact (oral or anal sex) with a man within a few hours of meeting him on an Internet cruise site?” If they had met a male sex partner online, respondents were then asked to indicate the last time it had occurred. For contacts in the prior three months, respondents indicated the type of sex that occurred (i.e., oral/anal, insertive/receptive, protected/unprotected) and the type of venue in which the sex occurred. Respondents who did not report sexual contact with an online partner in the prior three months were asked if they attempted to find a sexual partner by going online in the prior three months. HIV testing history and demographic characteristics including age, education, race/ethnicity, sexual orientation, relationship status, and the first three digits of the respondent’s residential zip code (or the name of his country of residence) were assessed at the end of the survey. Average time to complete the survey was 13 minutes.
Statistical Analysis
It was not possible to weight the data to adjust directly for demographic variables such as age or education because that information was not available for the total patron population. Each respondent was assigned a sample weight that is the multiplicative product of three weighting components:
The probability of a visit (the probability of a 2-hour shift being chosen for data collection multiplied by the probability of selection within the 2-hour shift).
The probability that a given respondent would visit the club during the data collection period (based on responses to survey questions on number of previous and subsequent planned visits to the venue during the 26-week data collection period).
Nonresponse/noncoverage (based on actual numbers of visits in a shift not matching the anticipated number of visits).
The survey data analysis (i.e., those incorporating the svy: prefix) statistical algorithms in Stata Release 12 (StataCorp LP, College Station, TX) were used in order to obtain standard errors, p-values, and confidence intervals that have been appropriately adjusted for the application of probability weighting.
The focus of the analysis was to determine how venue use in the prior three months is associated with prevalence of UAI in the prior three months. We derived three dichotomous venue use variables: bathhouse use, cruising area use including commercial adult sex venues in order to match the definition used by Binson et al. (2001), and Internet cruise site use. Bathhouse use did not include the current visit in which patrons were recruited into the study. The emphasis was on the “intent” to find sexual partners, so these dichotomous variables assessed whether or not respondents visited a venue to seek partners, regardless of whether they successfully found a partner during the visit. The three dichotomous venue use variables were then used to create two additional variables:
A count variable representing the number of venue types used in the prior three months.
An eight-category variable representing venue use patterns.
Adjusted odds ratios and 95% confidence intervals (95%CIs) were estimated using logistic regression. The initial model regressed UAI (yes vs. no) on number of venues used (0–3), HIV-serostatus (HIV-positive vs. non-positive), sexual orientation (gay/queer/homosexual vs. bisexual/heterosexual/straight), region [reside within the metropolitan area (residents) vs. outside it (non-residents), based on Zip Code], age (categorized as 20–29, 30–39, 40–49, 50+), race/ethnicity (categorized as non-Hispanic white, non-Hispanic other, Hispanic), and education (categorized as < college degree, college degree, advanced degree) as well as possible two-way interactions. In the final model, all non-significant (p>0.05) interaction terms were deleted, and a Hosmer-Lemeshow goodness-of-fit test assessed the logit model fit assumption. In addition, in order to determine if use of specific venue types was differentially associated with UAI, we ran a simple logistic regression, with the eight-category venue use patterns variable as the predictor.
RESULTS
A total of 1,245 men were randomly selected to be approached about participation in the exit survey. Thirty-nine men were not approached because of recruiter unavailability and/or procedural errors. In addition, part-way into the data collection period, bathhouse management requested that we cease recruiting a certain amount of time prior to closing, resulting in another 36 men selected for participation not being approached. Of the 1,170 men we asked to participate in the survey, 634 (54.2%) refused, 54 (4.6%) were ineligible, and 482 (41.2%) accepted. Of those who accepted to do the interview, the completion rate was 98.9% (477); however 18 were determined to be repeat respondents, so the sample for analysis totals 459 respondents.
A majority of respondents were in their 30s and 40s (69.4%, Mean=41.1, SE=0.66), non-Hispanic white, gay self-identified, and not residing within the metropolitan area (Table 1). In the prior three months, almost two-thirds of respondents (63.5%) had patronized a bathhouse; slightly fewer than half visited a cruising area (46.7%) or went online looking for a sex partner (46.5%). Just under a third of the respondents (30.9%) engaged in UAI with 24.5% reporting UAI in a private setting (i.e., private home or hotel) and 12.6% reporting UAI in a public setting. On average, respondents visited 1.6 (SD=0.1) types of venues in the prior three months.
Table 1.
Demographics of 459 study respondents
| Variable | % | |
|---|---|---|
| Bathhouse use in the prior three monthsa | Yes | 63.5% |
| No | 36.5% | |
| Cruising area use in the prior three months | Yes | 46.7% |
| No | 53.3% | |
| Internet cruise site use in the prior three months | Yes | 46.5% |
| No | 53.5% | |
| Age | 20 to 29 | 12.7% |
| 30 to 39 | 31.4% | |
| 40 to 49 | 38.0% | |
| 50 to 83 | 17.9% | |
| Education | < College degree | 29.1% |
| College degree | 38.6% | |
| Advanced degree | 32.3% | |
| Race | White, Non-Hispanic | 64.5% |
| Hispanic | 17.0% | |
| Other, Non-Hispanic | 18.5% | |
| Reside in region | Yes | 45.5% |
| No | 54.5% | |
| Sexual orientation | Gay/Queer/Homosexual | 85.1% |
| Bisexual/Heterosexual/Straight | 14.9% | |
| Self-reported HIV-serostatus | HIV-positive | 16.0% |
| HIV-negative | 84.0% | |
| UAI (unprotected anal intercourse over prior three months) | Yes | 30.9% |
| No | 69.1% |
Does not include current bathhouse visit
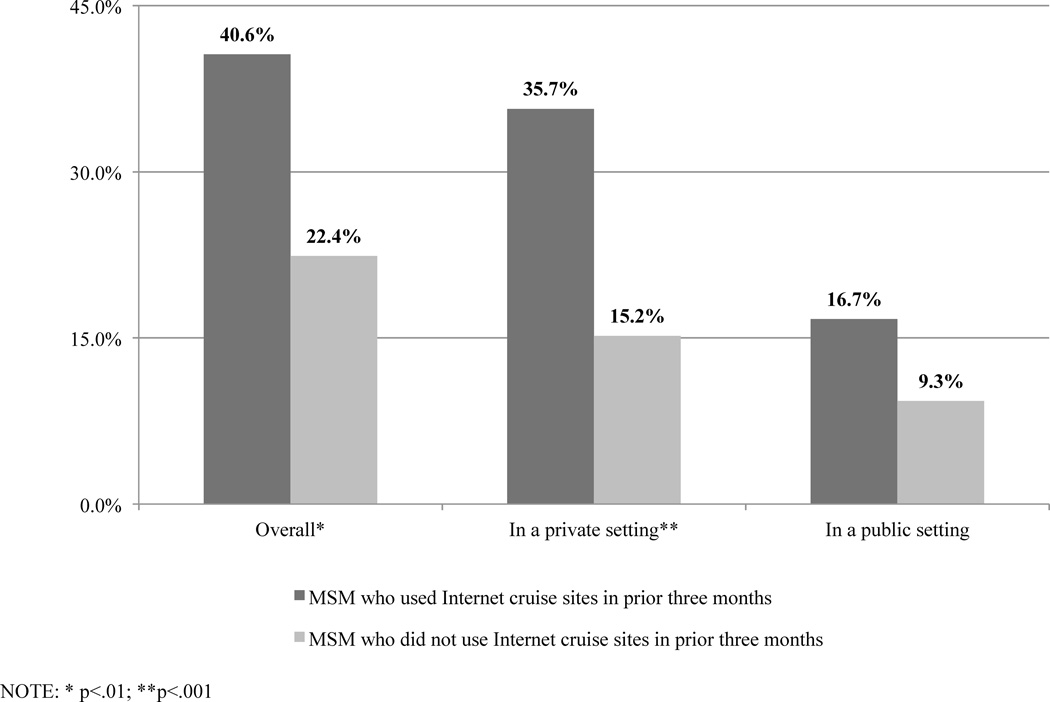
Of the 459 respondents, a larger proportion of those who used Internet cruise sites in the prior three months reported UAI in the prior three months than respondents who did not use Internet cruise sites (p<0.01). This finding held for UAI in a private setting (p<0.001), and in a public setting (p=0.07) (Figure 1). Of those respondents who ever went online looking to meet men, 45.3% did not engage in sex with anyone they met online; 17.9% engaged in oral sex only; 21.5% engaged in anal sex with condoms; and 15.4% engaged in unprotected anal intercourse (7.1% of the overall sample). Respondents who had met someone via Internet cruise sites in the prior three months, on average, met 4.7 partners (SE= 0.8) in that timeframe.
Figure 1.
Proportion of bathhouse patrons reporting unprotected anal intercourse in prior three months, by Internet usage in prior three months
The highest three-month prevalence of UAI occurred among respondents who had visited all three venue types (i.e., bathhouse, cruising area, and Internet cruise sites) in the prior three months (Table 2). In the logistic regression model, the number of venue types used in the prior three months was a significant predictor of the odds of reporting UAI in the prior three months (p<0.001). Men who used all three venue types had 4.4 times (95% CI: 1.62, 12.11) the odds of reporting UAI in the prior three months than men who did not use any venues (UAI prevalence, 57.4% vs. 25.8%). UAI in the prior three months among men who used all three venue types was also 5.3 (95% CI: 2.2, 12.8) and 4.3 (95% CI: 1.9, 9.6) times higher than that of men who used one or two types of venues, respectively. The only other significant covariate was an interaction between region and HIV-serostatus. Among HIV-positive men, local residents had lower odds of reporting UAI than non-residents (OR=0.31, 95%CI: 0.06, 1.52), although the difference was not statistically significant. Among HIV-negative and HIV-unknown men, local residents had significantly higher odds of reporting UAI than men who resided outside the region (OR=2.41, 95%CI: 1.27, 4.58).
Table 2.
Logistic regression results with prevalence of reporting unprotected anal intercourse (UAI) in the prior three months as outcome (n=414)
| Variable | % UAI | Adjusted Odds Ratio (95% CI) |
|
|---|---|---|---|
| Number of venues | Nonea | 25.8 | 1.00 |
| One | 24.4 | 0.83 (0.31, 2.23) | |
| Two | 26.5 | 1.04 (0.41, 2.61) | |
| Three | 57.4 | 4.43 (1.62, 12.11)** | |
| HIV-serostatus by Region | |||
| HIV-positive | Reside outside region | 77.3 | 1.00 |
| Reside in region | 56.2 | 0.31 (0.06, 1.52) | |
| Non-positive | Reside outside region | 19.5 | 1.00 |
| Reside in region | 33.2 | 2.41 (1.27, 4.58)** | |
| Sexual Orientation | Gay-identified | 33.2 | 1.60 (0.56, 4.56) |
| Other-identified | 18.6 | 1.00 | |
| Age | 20–29 | 26.9 | 1.00 |
| 30–39 | 35.1 | 1.62 (0.57, 4.59) | |
| 40–49 | 31.2 | 0.96 (0.36, 2.60) | |
| 50+ | 25.6 | 0.98 (0.33, 2.94) | |
| Race/Ethnicity | Non-Hispanic white | 31.5 | 1.00 |
| Hispanic | 27.0 | 0.63 (0.26, 1.48) | |
| Non-Hispanic other | 32.2 | 1.30 (0.56, 3.04) | |
| Education | < College degree | 36.6 | 1.04 (0.47, 2.30) |
| College degree | 34.3 | 1.35 (0.65, 2.82) | |
| Advanced degree | 22.4 | 1.00 |
p < .05
p < .01
NOTE: Hosmer-Lemeshow goodness-of-fit test p=0.76
Does not include current bathhouse visit
Given the unexpected absence of a linear relationship between number of venue types used and UAI, we performed a simple logistic regression with the eight-category venue use variable as the predictor in order to further examine if the odds of reporting UAI in the prior three months between men who used all three venue types and men who used other combinations of venue types were significant (Table 3). Despite some small group sizes, five of the seven pairwise comparisons with the three-venue group were statistically significant. Prevalence of UAI did appear to be higher among men who visited two types of venues than among men who visited only one venue type or none of the venue types as long as one of the two types visited was Internet cruise sites. However, only the bathhouse-and-Internet cruise site vs. bathhouse-and-cruising area comparison was statistically significant (OR=2.92, 95%CI: 1.05, 8.11).
Table 3.
Prevalence of reporting unprotected anal intercourse (UAI) in the prior three months, by venue use (n=433)
| Venue(s) | N | % UAI (95% CI) | Odds Ratio (95% CI) |
|---|---|---|---|
| Bathhouse and cruising area and Interneta | 74 | 57.4% (43.4%, 70.2%) | 1.00 |
| Bathhouse and Interneta | 62 | 36.1% (22.6%, 52.3%) | 0.42 (0.18, 1.00) |
| Cruising area and Interneta | 29 | 33.0% (14.1%, 59.6%) | 0.37 (0.11, 1.25) |
| Bathhouse only | 64 | 28.2% (16.7%, 43.4%) | 0.29 (0.12, 0.70)** |
| None | 67 | 25.8% (12.8%, 45.1%) | 0.26 (0.09, 0.72)* |
| Internet onlya | 37 | 22.2% (10.0%, 42.2%) | 0.21 (0.07, 0.63)** |
| Cruising area only | 25 | 18.3% (5.3%, 46.9%) | 0.17 (0.04, 0.73)* |
| Bathhouse and cruising area | 76 | 16.2% (8.2%, 29.6%) | 0.14 (0.06, 0.38)*** |
| Total | 433b | 31.0% (25.5%, 37.1%) |
p < .05
p < .01
p < .001
Internet = Internet cruise sites
Due to rounding of weighted counts, the row Ns will not sum exactly to the total.
DISCUSSION
Previous research had found that use of multiple types of physical venues to meet men for sex (i.e., both bathhouses and cruising areas) was associated with higher prevalence of sexual risk behavior (Binson et al., 2001). However, those data were collected before the advent of widespread access to the Internet and the virtual sex venues that reside there. The current study sought to determine if usage of Internet sex venues in addition to physical sex venues to meet casual sexual partners would also be associated with elevated risk. In this time-location probability sample of bathhouse patrons, men who used all three types of venues (bathhouses, cruising areas, and online cruise sites) to meet men for sex in the prior three months were significantly more likely to report UAI than men who visited two, one, or none of the venue types. In addition, the data also indicated that MSM who visited either bathhouses or cruising areas as well as used online cruise sites to meet men for sex tended to have a higher prevalence of UAI than men who only used one venue type. This is consistent with results reported by Wei et al. (2013).
These findings would appear to have significant implications for sampling very high risk men. Clearly, MSM do not uniformly engage in high risk sexual behavior. Even in this cohort obtained at a venue type known to attract men who engage in high risk sexual behavior, only about three out of every 10 men reported UAI in the prior three months (comparable to results of other bathhouse exit surveys, e.g., Woods et al., 2007; Bingham et al., 2008; Reidy et al., 2009). Thus, regardless of sampling approach, simply targeting MSM is unlikely to result in the recruitment of large numbers of men behaviorally at risk for transmission of HIV. Recruiting in physical or virtual sex venues will be equally inefficient unless men are asked about the types of venue they use. Recruiting at such venues while using multi-venue use as a screener may significantly increase the chances of identifying the highest-risk group of MSM who are more likely to impact overall public health and be in need of prevention services.
These results also raise the issue of considering bathhouses as not just an optimal venue for recruiting high risk MSM, but also as a venue at which to implement a wider array of HIV prevention interventions. The bathhouse not only can provide a point of access to the group of multi-venue users that have the highest prevalence of UAI, but also is the only physically-bounded sex venue in which private space can be appropriated to intervention activities. Although most men did not engage in UAI on premises (only one in eight men reported UAI in a public setting in the prior three months), many of the co-factors of HIV transmission were present including: sex with multiple sexual partners; sex with casual sexual partners; and the accompanying lack of knowledge regarding partner serostatus, sexual history, and exposure to sexually transmitted infections. It is possible that the immediacy of these issues in the bathhouse venue can provide the context for extracting or creating a “teachable moment” that could form the basis of an intervention (Eaton, Cherry, Cain, & Pope, 2011; Lawson & Flocke, 2009). Bathhouses already serve as sites for some individual-level interventions primarily in the form of education and condom distribution (Woods, Euren, Pollack, & Binson, 2010) as well as voluntary counseling and testing (Daskalakis et al., 2009; Huebner et al., 2006). However, greater consideration of the social climate of bathhouses (Binson & Woods, 2003) suggests that larger scale group-level or facility-wide interventions are also possible (see, for example, Pollack, Woods, Blair, & Binson, in press).
It is also worth noting that fewer than half of all respondents went online looking for a sex partner in the prior three months. Consequently, prevention programs should be careful about assuming that online prevention actually reaches a high proportion of the highest risk men (Chiasson et al., 2007; Grov et al., 2013; Smith et al., 2006). Moreover, the rarity of UAI reported with men met online only reinforces the fact that the virtual environment lacks the behavioral immediacy (inherent in most physical sex venues) that may be necessary to help motivate men to change their perceptions and behavior.
Although exit surveys at other bathhouses found high proportions of local residents (Reidy et al., 2009; Woods et al., 2007), half of the current sample reported living outside the region. This makes clear that the population of MSM at the two bathhouses sampled may be quite different from populations at other bathhouses, and that some of the venue use patterns, and their associations with UAI, may be influenced by the fact that many of the men were reporting behavior that occurred while traveling, rather than behavior that occurred at home. It is possible that HIV-positive men residing outside the region found travel to the area liberating in a way that their non-positive counterparts did not (Benotsch et al., 2011). Alternatively, the reported risk behavior could have occurred prior to travel. Combined with the higher prevalence of sexual risk behavior among HIV-negative men from within the region (denoted by the significant two-way interaction between region and HIV-serostatus), there may be an increased likelihood of HIV transmission to local MSM. However, local MSM may also be more comfortable using other methods to reduce their risk of HIV, such as withdrawal prior to ejaculation, serosorting, or strategic positioning (Binson, Pollack, Blair, & Woods, 2010), although they may be perceived as less than ideal risk reduction approaches for non-positive men (Berry, Raymond, Kellogg, & McFarland, 2008; van den Boom et al., 2014).
The weighted sample estimation used for our analyses is the standard procedure for time-location sampling (Karon & Wejnert, 2012). Random selection of men approached to participate in the exit survey combined with careful adherence to the sampling protocol and weighting data by probability of selection allows us to generalize our findings to the population of patrons that visited the two bathhouses during the data collection period. However, that is the extent to which generalization can occur, and caution must be taken in extrapolating our findings to patrons of other bathhouses, let alone MSM in general. The effects of different kinds of bathhouse environments on risk behavior are unknown, but may differentially affect patron risk behavior or draw a safer or riskier group of men (Binson & Woods, 2003). Moreover, men who visit sex venues are demographically and behaviorally distinct from men who do not visit such venues (Binson et al., 2001).
The 41% response rate is lower than what we obtained at a different bathhouse at the beginning of the decade (Woods et al., 2007; Pollack et al., in press), but it is similar to the 45% rate reported by Grov (2012) for a recent time-location sample survey of New York City bathhouses. It is important to remember that response rate is only a weak indicator of response bias, i.e., a low response rate does not guarantee high levels of bias and a high response rate does not obviate response bias (Groves, 2006; Reidy et al., 2009). For example, Reidy et al. (2009) achieved a 30% response rate for a 30–45 minute survey of Seattle bathhouse patrons in 2004 and a 61% response rate for a much briefer version of the same survey at the same bathhouse in 2006; yet the two samples were indistinguishable in terms of demographic characteristics and sexual risk behavior. Overall, despite falling response rates, probability samples are likely to provide less biased estimates than opt-in volunteer samples (i.e., convenience samples, the method most often used in online and venue-based surveys) because probability sample respondents are randomly selected, actively recruited, and have to opt out of participation (Brick, 2011).
Survey fatigue may also have increased refusal rate; in the period before our study, a local community-based organization conducted health surveys of patrons on a regular basis as an introduction to their prevention programming. However, it should be noted that we provided respondents with a private physical setting, used ACASI administration of the survey, and limited the recall timeframe to the prior three months in order to minimize response and recall biases in self-reported sexual behavior (Catania, Gibson, Chitwood, & Coates, 1990; Kauth, St. Lawrence, & Kelly, 1991).
The advent of Internet cruise sites demonstrably changed the phenomena of where and how men meet for sex, and it is changing again as sexually-oriented social networking applications for mobile devices (smart phone “apps”) increase in popularity (Landovitz et al., 2012; Rendina, Jimenez, Grov, Ventuneac, & Parsons, 2013). Future research into venue use and sexual risk behavior will have to take this development into account. Nevertheless, despite the proliferation in ways to “hook up,” only a minority of the men surveyed engaged in high-risk sex in the prior three months and even smaller percentages reported UAI in a public setting or with a man they met online. This supports the contention that the venues themselves (whether they be physical or on the Internet) do not necessarily lead to high-risk behavior, but rather attract MSM who engage in that behavior (Woods et al., 2007). Thus, sampling across all venue types (e.g., Internet cruise sites and related apps, bathhouses, cruising areas) and inquiring about use of other venues to meet men will identify and reach a greater proportion of the population of MSM who engage in very high risk behavior, i.e., men who have UAI with multiple sex partners about whom they may know little if anything regarding their sexual history and HIV status.
ACKNOWLEDGEMENTS
We want to express our deepest thanks to our project directors, Paul Cotten and Bob Siedle-Khan; our study team members, Justin Bailey, Scott Carroll, Louis Cullen, Jason Euren, Trevor Hoppe, James Moser, Gabriel Ortiz, Mateo Rutherford, Ted Tallase; and the club managers, staff and patrons, in particular all the survey respondents. This work was funded by the National Institute of Mental Health: R01 MH071159. The content is solely the responsibility of the authors and does not necessarily represent the official views of NIMH.
Footnotes
Some of the data contained in this manuscript have been presented previously in a poster presented at the 2011 National HIV Prevention Conference, Atlanta, GA, USA, 14–17 August 2011.
REFERENCES
- Bartholome A, Tewksbury R, Bruzzone A. "I want a man": Patterns of attraction in all-male personal ads. The Journal of Men's Studies. 2000;8(3):309–321. [Google Scholar]
- Benotsch EG, Martin AM, Espil FM, Nettles CD, Seal DW, Pinkerton SD. Internet use, recreational travel, and HIV risk behaviors in men who have sex with men. Journal of Community Health. 2011;36(3):398–405. doi: 10.1007/s10900-010-9321-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry M, Raymond HF, Kellogg T, McFarland W. The Internet, HIV serosorting and transmission risk among men who have sex with men, San Francisco. AIDS. 2008;22(6):787–789. doi: 10.1097/QAD.0b013e3282f55559. [DOI] [PubMed] [Google Scholar]
- Bingham TA, Secura GM, Behel SK, Bunch JG, Simon PA, MacKellar DA. HIV risk factors reported by two samples of male bathhouse attendees in Los Angeles, California, 2001–2002. Sexually transmitted diseases. 2008;35(6):631–636. doi: 10.1097/OLQ.0b013e31816b475a. [DOI] [PubMed] [Google Scholar]
- Binson D, Pollack LM, Blair J, Woods WJ. HIV transmission risk at a gay bathhouse. Journal of Sex Research. 2010;47(6):580–588. doi: 10.1080/00224490903216755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Binson D, Woods WJ. A theoretical approach to bathhouse environments. Journal of Homosexuality. 2003;44(3–4):23–31. doi: 10.1300/J082v44n03_02. [DOI] [PubMed] [Google Scholar]
- Binson D, Woods WJ, Pollack L, Paul J, Stall R, Catania JA. Differential HIV risk in bathhouses and public cruising areas. American Journal of Public Health. 2001;91(9):1482–1486. doi: 10.2105/ajph.91.9.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton R, Vincke J, Mak R. Gay saunas: Venues on HIV transmission or AIDS prevention. National AIDS Bulletin. 1992;9:22–26. [Google Scholar]
- Brick JM. The future of survey sampling. Public Opinion Quarterly. 2011;75(5):872–888. doi: 10.1093/poq/nfr048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catania JA, Gibson DR, Chitwood DD, Coates TJ. Methodological problems in AIDS behavioral research: influences on measurement error and participation bias in studies of sexual behavior. Psychological Bulletin. 1990;108(3):339–362. doi: 10.1037/0033-2909.108.3.339. [DOI] [PubMed] [Google Scholar]
- Chiasson MA, Hirshfield S, Remien RH, Humberstone M, Wong T, Wolitski RJ. A comparison of on-line and off-line sexual risk in men who have sex with men: an event-based on-line survey. Journal of Acquired Immune Deficiency Syndromes. 2007;44(2):235–243. doi: 10.1097/QAI.0b013e31802e298c. [DOI] [PubMed] [Google Scholar]
- Coates T, Acree M, Stall R, Hoff C, Kegeles S, Ekstrand M, Jinich S. Men who have sex with men in public places are more likely to have unprotected anal intercourse. Presented at: XI International Conference on AIDS; Vancover; British Columbia. 1996. [Google Scholar]
- Colfax GN, Mansergh G, Guzman R, Vittinghoff E, Marks G, Rader M, Buchbinder S. Drug Use and sexual risk behavior among gay and bisexual men who attend circuit parties: a venue-based comparison. Journal of Acquired Immune Deficiency Syndromes. 2001;28(4):373–379. doi: 10.1097/00126334-200112010-00011. [DOI] [PubMed] [Google Scholar]
- Collins C, Diallo DD. A prevention response that fits America’s epidemic: Community perspectives on the status of HIV prevention in the United States. Journal of Acquired Immune Deficiency Syndromes. 2010;55:S148–S150. doi: 10.1097/QAI.0b013e3181fbcb22. [DOI] [PubMed] [Google Scholar]
- Daskalakis D, Silvera R, Bernstein K, Stein D, Hagerty R, Hutt R, Marmor M. Implementation of HIV testing at 2 New York City bathhouses: from pilot to clinical service. Clinical Infectious Diseases. 2009;48(11):1609–1616. doi: 10.1086/598979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downing M. Using the Internet in pursuit of public sexual encounters: Is frequency of use associated with risk behavior among MSM. American Journal of Men’s Health. 2012;6(1):18–27. doi: 10.1177/1557988311407906. [DOI] [PubMed] [Google Scholar]
- Eaton LA, Cherry C, Cain D, Pope H. A novel approach to prevention for at-risk HIV-negative men who have sex with men: Creating a teachable moment to promote informed sexual decision-making. Journal Information. 2011;101(3):539–545. doi: 10.2105/AJPH.2010.191791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C. HIV risk and substance use in men who have sex with men surveyed in bathhouses, bars/clubs, and on Craigslist.org: venue of recruitment matters. AIDS Behav. 2012;16(4):807–817. doi: 10.1007/s10461-011-9999-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Hirshfield S, Remien RH, Humberstone M, Chiasson MA. Exploring the venue's role in risky sexual behavior among gay and bisexual men: an event-level analysis from a national online survey in the U.S. Archives of Sexual Behavior. 2013;42(2):291–302. doi: 10.1007/s10508-011-9854-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groves R. Nonresponse rates and nonresponse bias in household surveys. Public Opinion Quarterly. 2006;70(5):646–675. [Google Scholar]
- Hancock JT, Toma C, Ellison N. The truth about lying in online dating profiles. Presented at: Computer/Human Interaction 2007 Conference; 2007; San Jose, CA. 2007. [Google Scholar]
- Horvath KJ, Bowen AM, Williams ML. Virtual and physical venues as contexts for HIV risk among rural men who have sex with men. Health Psychology. 2006;25(2):237. doi: 10.1037/0278-6133.25.2.237. [DOI] [PubMed] [Google Scholar]
- Huebner DM, Binson D, Woods WJ, Dilworth SE, Neilands TB, Grinstead O. Bathhouse-based voluntary counseling and testing is feasible and shows preliminary evidence of effectiveness. Journal of Acquired Immune Deficiency Syndromes. 2006;43(2):239–246. doi: 10.1097/01.qai.0000242464.50947.16. [DOI] [PubMed] [Google Scholar]
- Karon JM, Wejnert C. Statistical methods for the analysis of time-location sampling data. Journal of Urban Health. 2012;89(3):565–586. doi: 10.1007/s11524-012-9676-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauth MR, St. Lawrence JS, Kelly JA. Reliability of retrospective assessments of sexual HIV risk behavior: a comparison of biweekly, three-month, and twelve-month self-reports. AIDS Education and Prevention. 1991;3(3):207–214. [PubMed] [Google Scholar]
- Kim AA, Kent C, McFarland W, Klausner JD. Cruising on the Internet highway. Journal of Acquired Immune Deficiency Syndromes. 2001;28(1):89–93. doi: 10.1097/00042560-200109010-00013. [DOI] [PubMed] [Google Scholar]
- Landovitz RJ, Tseng CH, Weissman M, Haymer M, Mendenhall B, Rogers K, Shoptaw S. Epidemiology, sexual risk behavior, and HIV prevention practices of men who have sex with men using GRINDR in Los Angeles, California. Journal of Urban Health. 2013;90(4):729–739. doi: 10.1007/s11524-012-9766-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson PJ, Flocke SA. Teachable moments for health behavior change: A concept analysis. Patient Education and Counseling. 2009;76(1):25–30. doi: 10.1016/j.pec.2008.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sexually Transmitted Diseases. 2006;33(9):576–584. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- Martin JL. The impact of AIDS on gay male sexual behavior patterns in New York City. American Journal of Public Health. 1987;77(5):578–581. doi: 10.2105/ajph.77.5.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKusick L, Horstman W, Coates TJ. AIDS and sexual behavior reported by gay men in San Francisco. American Journal of Public Health. 1985;75(5):493–496. doi: 10.2105/ajph.75.5.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollack LM, Woods WJ, Blair J, Binson D. Presence of an HIV testing program lowers the prevalence of unprotected insertive anal intercourse inside a gay bathhouse among HIV-negative and HIV-unknown patrons. Journal of HIV/AIDS & Social Services. In press doi: 10.1080/15381501.2013.864175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reidy WJ, Spielberg F, Wood R, Binson D, Woods WJ, Goldbaum GM. HIV risk associated with gay bathhouses and sex clubs: Findings from 2 Seattle surveys of factors related to HIV and sexually transmitted infections. American Journal of Public Health. 2009;99(S1):S165–S172. doi: 10.2105/AJPH.2007.130773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendina HJ, Jimenez RH, Grov C, Ventuneac A, Parsons JT. Patterns of lifetime and recent HIV testing among men who have sex with men in New York City who use Grindr. AIDS and Behavior. 2014;18:41–49. doi: 10.1007/s10461-013-0573-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DM, Drumright LN, Frost SD, Cheng WS, Espitia S, Daar ES, Gorbach PM. Characteristics of recently HIV-infected men who use the Internet to find male sex partners and sexual practices with those partners. Journal of Acquired Immune Deficiency Syndromes. 2006;43(5):582–587. doi: 10.1097/01.qai.0000243100.49899.2a. [DOI] [PubMed] [Google Scholar]
- Tikkanen R, Ross MW. Looking for sexual compatibility: Experiences among Swedish men in visiting Internet gay chat rooms. CyberPsychology & Behavior. 2000;3(4):605–616. [Google Scholar]
- van den Boom W, Konings R, Davidovich U, Sandfort T, Prins M, Stolte IG. Is serosorting effective in reducing the risk of HIV-infection among men who have sex with men with casual sex partners? Journal of Acquired Immune Deficiency Syndromes. 2014;65:375–379. doi: 10.1097/QAI.0000000000000051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei C, Lim SH, Guadamuz TE, Koe S. Virtual versus physical spaces: Which facilitates greater HIV risk taking among men who have sex with men in East and South-East Asia? [Published online: 29 September 2013];AIDS and Behavior. 2013 doi: 10.1007/s10461-013-0628-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White House Office of National AIDS Polic. National HIV/AIDS Strategy for the United States. 2010 from http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
- Woods WJ, Binson D, Blair J, Han L, Spielberg F, Pollack LM. Probability sample estimates of bathhouse sexual risk behavior. Journal of Acquired Immune Deficiency Syndromes. 2007;45(2):231–238. doi: 10.1097/QAI.0b013e318055601e. [DOI] [PubMed] [Google Scholar]
- Woods WJ, Euren J, Pollack LM, Binson D. HIV prevention in gay bathhouses and sex clubs across the United States. Journal of Acquired Immune Deficiency Syndromes. 2010;55:S88–S90. doi: 10.1097/QAI.0b013e3181fbca1b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods WJ, Pollack LM, Blair J, Binson D. JSM Proceedings, Statistical Computing Section. Alexandria, VA: American Statistical Association; 2012. Harder to reach population: Highrisk MSM. Proceedings paper retrieved from http://www.amstat.org/meetings/h2r/2012/AbstractDetails.cfm?AbstractID=301425. [Google Scholar]