Abstract
Spitz nevus is a benign melanocytic lesion and also one of the main differential diagnosis of melanoma. A descriptive and retrospective study of surgical specimens from patients with a diagnosis of Spitz nevus was conducted at two institutions in Niterói - RJ. 32 cases were analyzed. The most frequent histological subtype was compound (60 %), with a predominance of epithelioid cells (17 cases - 53%). Pagetoid spread was observed in 21 cases (68%). Maturation of melanocytes was present in 13 cases (81%). Kamino bodies were found in eight cases (25%). Atypical melanocytes were present in 18 cases (56%). Mitoses were present in 11 cases (34%). Detailed knowledge of the classical form of Spitz nevi is essential for the differential diagnosis with melanoma. However, no single criterium is definitive in the differential diagnosis between Spitz nevus and melanoma.
Keywords: Nevi and melanomas; Nevus, epithelioid and spindle cell; Pathology
INTRODUCTION
Spitz nevus, also known as Spitz tumor or spindle and epithelioid cell nevus, is an usually acquired, benign melanocytic lesion and one of the main differential diagnosis of melanoma. Ever since it has been first described, it has been more frequently reported in children and young people, but recent studies show that its occurrence is not rare in adults.1,2
From a histopathological point of view, Spitz nevus is classified into numerous subtypes. These subtypes have, in most cases, architectural and cytological features which help distinguish them from other melanocytic lesions: a) symmetry; b) circumscription; c) orthokeratosis, hypergranulosis and hyperplasia of the spinous layer, which develop with the progression of the lesion; d) uniform melanocyte aggregates perpendicular to the epidermis; e) clefts between melanocyte aggregates and adjacent keratinocytes; f) absence of pagetoid melanocytes in most cases or, when present, located in the center of the lesion; g) mitotic figures in the dermis located, when existant, on the surface component, and scarce mitoses at the base of the lesion; h) Kamino bodies (rounded, eosinophilic proteinaceous aggregates stained by hematoxylin-eosin, PAS-positive and diastase resistant, of little-known meaning); i) absence of regression; j) maturation of melanocytes; k) perivascular lymphocytic infiltrate in the periphery of the lesion.3-6
However, all of these criteria may also be present in melanomas. The aim of this study was to describe the histopathologic features of classic Spitz nevi, especially highlighting those features which may erroneously induce a diagnosis of melanoma. In parallel, clinical and demographic data were recorded and checked.
MATERIALS AND METHODS
This is a descriptive and retrospective study of the surgical specimens from patients with a diagnosis of Spitz nevus. The study was conducted at the Pathological Anatomy Service of the Antonio Pedro University Hospital, Fluminense Federal University, and the 'Consultoria em Dermatopatologia' ('Consultancy in Dermatopathology') Laboratory, Niterói. Thirty-two cases were analyzed.
Slides with 5μm sections stained with hematoxylin and eosin (HE) were selected. These were evaluated using a detailed protocol of histopathological features, and considering the following aspects: symmetry and circumscription, alterations of the epidermis (orthokeratosis, parakeratosis, hypergranulosis and acanthosis), histopathological type (junctional, intradermal and compound), melanocytes´predominant cell type (spindle or epithelioid), the predominant distribution of melanocytes (nests or single cells), orientation of junctional nests of melanocytes in relation to the epidermis, confluence of nests, clefts between the nests of melanocytes in the epidermis and the keratinocytes, pagetoid spread, maturation of melanocytes, loss of cohesion between melanocytes, involvement of skin appendages, Kamino bodies, presence of melanin pigment, desmoplasia, inflammatory infiltrate, presence of atypical melanocytes in the epidermis and dermis.
RESULTS
We evaluated the clinical data of 29 patients. Mean age was 18 years (range 2-42 years). There was no difference in gender distribution, with 52% (15) of men and 48% (14) of women.
The location of the lesions was reported in 27 patients. Lesions were predominantly located in the lower limbs (13 cases - 48%), the trunk (7 cases - 26%), the upper limbs (5 cases - 18.5%) and the oral mucosa, the head and neck (1 case - 3.25% each). The color of the lesion in the 24 patients was mostly blackened (15 cases - 62.5%), followed by a brown (seven cases 29%) and an erythematous coloration (two cases 8.5%). The average size of these lesions was 0.5 cm (range 0.2-1.5 cm).
The main clinical hypothesis was melanoma (13 cases), followed by melanocytic nevus (11 cases), atypical melanocytic nevus (nine cases) and Spitz nevus (only five cases).
The evolution time of the lesions was reported in nine cases, with a mean of 12 months (range three months to five years). The latter was congenital. There were reports of recent growth in the last few months in 12 patients (34.5%).
The histopathological features evaluated in 32 cases (1) showed that symmetry was present in 25 cases (78%) and circumscription was present in 26 cases (81%) (Figures 1 and 2).
FIGURE 1.
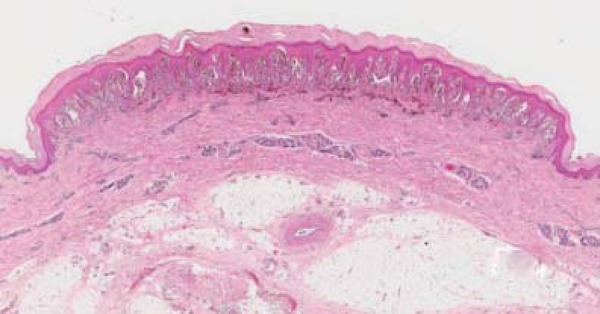
Panoramic photo shows marked symmetry and circumscription, prominent skin alterations (orthokeratosis, hypergranulosis and acanthosis), nests of melanocytes perpendicular to the epidermis, artifactual cleft between the nests of melanocytes and the keratinocytes, and pigmentary incontinence (HE, original magnification - 15x)
FIGURE 2.
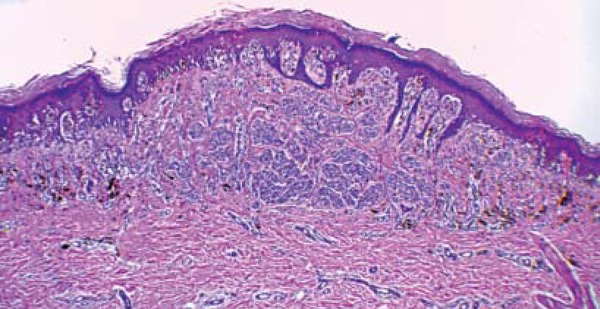
Asymmetry and imperfect circumscription; orthokeratosis, hypergranulosis and acanthosis (HE, original magnification - 40x)
The most common histopathological subtype, according to the location of melanocytes, was compound (19 cases -60%), followed by junctional (11 cases - 34%) and intradermal (one case - 3.0%). Regarding the cytological aspect, lesions with predominant epithelioid cells were more frequent (17 cases -53%), followed by spindle cells (8 cases - 25%) and mixed epithelioid and spindle cells (7 cases - 22%). The orientation of the nests of melanocytes in relation to the epidermis was found to be perpendicular in 65.5% of cases. There were some clefts between the nests of melanocytes in the epidermis and the keratinocytes in 17 cases (55% of cases with intraepidermal component). Multinucleation was present in nine cases (28%) and nuclear pseudoinclusion was found in seven cases (22%), especially in epithelioid cells. Loss of cohesion between melanocytes was present in 19% of cases (Figures 1 and 3).
FIGURE 3.
Numerous Kamino bodies associated with orthokeratosis, hypergranulosis, acanthosis and artifactual clefts between the nests of melanocytes and the keratinocytes (nest extrusion) (HE, original magnification - 100x)
Pagetoid spread was only assessed in cases with intraepidermal component (31 cases). It was present in 21 cases (68%), and ranged from scarce cells (less than five cells per slide) in eight cases (38%) to more than five cells per slide in 13 cases (62%). It was found to be at the center of the lesion in 18 cases (86%), peripheral in two cases (9.0%) and central and peripheral in one case (5.0%). It was also registered that this rise predominated in the form of isolated cells (15 cases - 71.5%) in relation to nests of melanocytes (Figure 4).
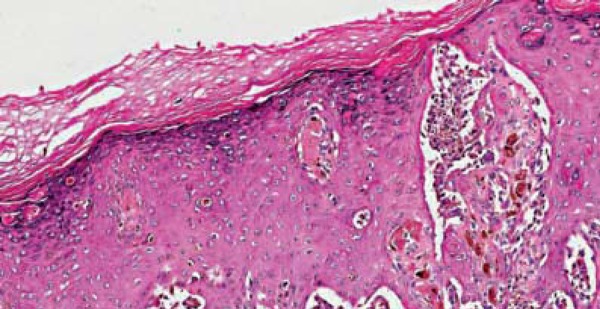
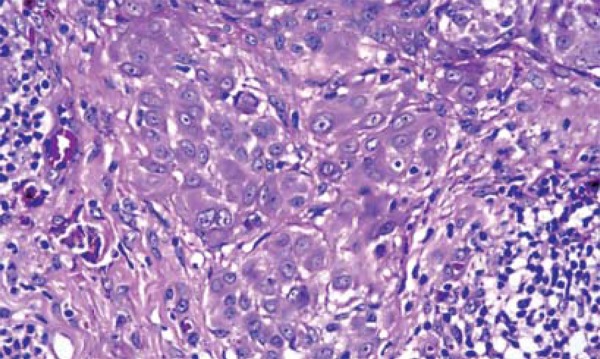
FIGURE 4.
Area of pagetoid spread, with irregular distribution of pigmentation and irregular maturation of melanocytes (HE, original magnification - 100x)
The maturation of melanocytes - described as the reduction in size of melanocytes in deeper portions of the lesion - was evaluated in nevi with dermal component (20 cases) and was observed in 13 cases (81%). It was classified into regular (31%) and irregular (50%) (Figures 4 and 5).
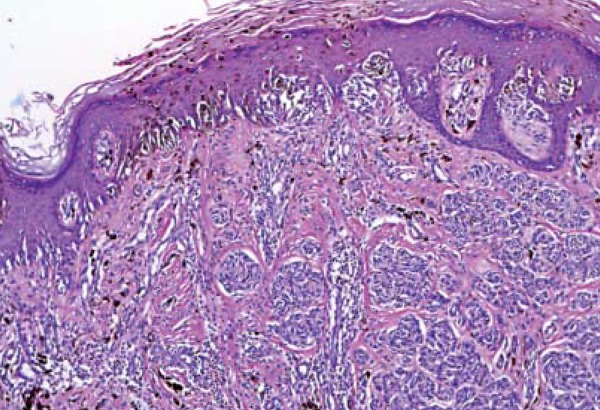
FIGURE 5.
Lack of maturation. Atypical melanocytes with pleomorphism, anisocoria, cariomegaly and eosinophilic nucleoli (HE, original magnification - 400x)
Among the epidermal changes analyzed, orthokeratosis and acanthosis were observed in all lesions (100%). The first was predominantly mild (50%) to moderate (28%). The latter was evaluated as mild (34%), moderate (47%) and severe (19%). Hypergranulosis was found in 28 lesions (87.5%) and considered mild (50%), moderate (46.5%) and severe (3.5%). Parakeratosis was observed in only one case (3.0%) (Figures 1, 2 and 3).
Kamino bodies were found in eight cases (25%) (Figures 3 and 6).
FIGURE 6.
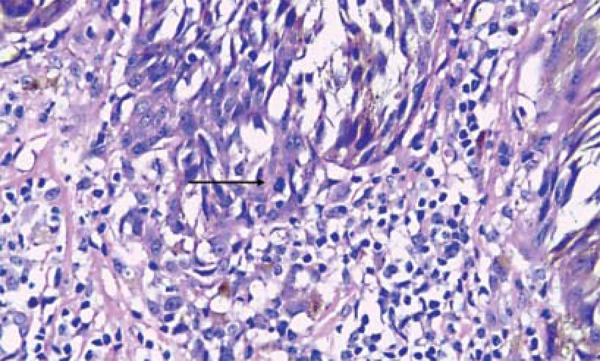
Atypical melanocytes with pleomorphism, hyperchromasia and mitotic figure at the base of an intraepidermal nest (arrow) (HE, 400x magnification)
Deposit of melanin in dermal keratinocytes and histiocytes (melanophages) was observed in 30 lesions (93.5%) . This pigment in the epidermis was located in all of the thickness of the epidermis or in the upper third of the epidermis and only in the superficial portion of the dermis (90.5%) with mild (40%) or moderate (46.5%) intensity.
A lymphocytic inflammatory infiltrate was observed in 75% of cases, distributed in the central part of the base of the lesion in six lesions (19%), in the periphery of the lesion in five lesions (15.5%) and diffuse in 13 lesions (40.5%). These were all in the superficial dermis and predominantly mild (47%) and moderate (18.5%) (Figure 6).
In 18 cases (56%), atypical melanocytes located in the epidermis were noted in 51% of lesions with epidermal component (31 cases) and were found in the dermis in 44% of lesions with dermal component (25 cases). Cariomegaly was observed in 12 cases (66%), hyperchromasia in 11 (61%), nuclear pleomorphism in 13 (72%), anisocoria and eosinophilic nucleoli in 8 (25%) (Figures 5 and 6).
The melanocytic proliferation extended to the epithelium of the skin appendages in 20 lesions (Figure 7).
FIGURE 7.
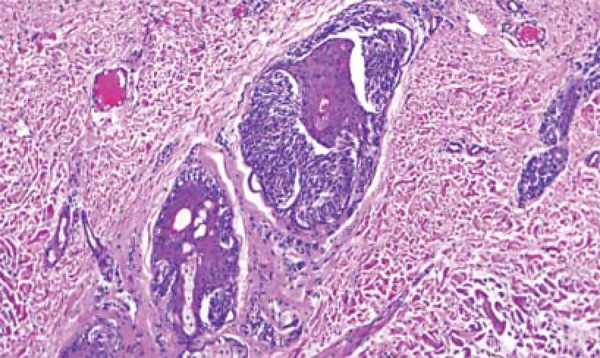
Spindle melanocytes forming nests in the epithelium of the skin appendages, located in a deeper position than the intradermal component (HE, original magnification - 100x)
Mitoses in the basal layer melanocytes were observed in 11 cases (34%). Only one case presented mitosis in the dermal melanocytes of the superior part of the lesion. A single atypical mitosis was seen in only one lesion (Figure 7).
DISCUSSION
There are few series of cases of Spitz nevi. Most of them take into account the various existing histopathological or more atypical variants that challenge the pathologist when making a diagnosis. However, with this study we intend to demonstrate that even Spitz nevi with classic histopathology have histopathologic features that can also be found in melanomas or atypical melanocytic lesions, making it difficult to differentiate among them.
Considering the variable 'age of the patient at diagnosis', the occurrence of lesions in adults has been reported in series of cases. This is corroborated by our study, with four patients in the fourth and one patient in the fifth decade of life. These findings confirm the current concept that age alone does not rule out the diagnosis of Spitz nevus.
We found a higher frequency of location in the lower limbs, which is supported by other studies, but deviates from the information in textbooks referring to the head and neck as the most common location.8,9
The clinical diagnosis of Spitz nevi is hampered by the variety of clinical presentations observed. In the series of Requena, clinical suspicion of Spitz nevi occurred in only 18.33% of cases, similar to the findings in our study (18.5%). In the latter, however, only cases displaying a classical histopathological pattern of the condition were selected, unlike the first. This increases diagnostic difficulty in all age groups, including the 42-year-old patient.5Conversely, clinical hypotheses encompassed only the most common differential diagnosis of pigmented lesions (brownish or blackened). The hypotheses of dermatofibroma and angioma - frequently observed by other authors were not found.
The occurrence of the intradermal type is associated with the more advanced age of the patient. It is in accordance with the concept of Abtropfung, which considers the genesis of the nevi from melanocytes in the epidermis. They then proliferate and reach the superficial dermis, and later the reticular dermis. In our study, however, we did not observe such a correlation.10,11
The predominant cell type in our series of cases was epithelioid, observed in all age groups, including the 42-year-old patient. In the series of Cesinaro, the lesions were mainly composed of epithelioid and spindle cells, whereas Requena described spindle cells as the most frequent cell type, except in patients over 45 years of age. They highlight that the older the patient, the greater the chance of finding epithelioid cells.5,7Pseudoinclusion, multinucleation and eosinophilic nucleoli were mainly present in cases with epithelioid cell component. A correlation between epithelioid cell type and the presence of multinucleation was observed by Requena.5However, we found no references on the relationship between pseudoinclusions and eosinophilic nucleoli and the predominant cell type, which makes this study, to our knowledge, the first report of this association. Symmetry and circumscription are also important criteria of benignity which help in the differential diagnosis with melanoma. According to some authors, it is found in 80-90% of the lesions, which is consistent with our findings (78 and 81%).12,13
Large series of cases do not describe the cytologic atypia of melanocytes in detail. However, according to our results, cytologic atypia can be so intense that the non-specialist pathologist may mistakenly interpret the lesions as melanoma. We observed its presence in 56% of our cases. They were represented by pleomorphism, cariomegaly, hyperchromasia, anisocoria and eosinophilic nucleoli.
Maturation of melanocytes is an important criterion in the diagnosis of melanocytic lesions and is usually present in Spitz nevi. Thus, it is used as a criterion of benignity. Some series of cases report maturation in 72-86.6%.5,7In this study, such feature was observed in 81%, which is consistent with the literature. However, in 50% of these cases, maturation was irregular, i.e., there were alternating immature and fully mature areas in the lower half of the lesion.
Pagetoid spread of melanocytes to the upper layers of the epidermis is a frequent finding in melanomas. It may also be present in Spitz nevi, being generally restricted to the central portion of the lesion, and ranging from 13-63% in different studies.5,7,13In the present study, we found a 65% frequency, similar to the variation shown in the literature. This draws attention to the correct interpretation of this phenomenon.
In melanomas it is common to find atrophy of the epidermis, while in Spitz nevi hyperplasia of the epidermis is frequent. In our series we could confirm this information. We observed orthokeratosis and acanthosis in 100% of cases.
Kamino bodies are frequently seen in Spitz nevi lesions with junctional component, especially if the cell density of the lesion is high.14They were initially described in Spitz nevi and considered pathognomonic. Its occurrence was later also reported in melanomas.15,16The presence of Kamino bodies in our cases agrees with the large variation found among different studies (11-34%). This difference is attributed by one of the authors to the amount of sections examined.5,7,13
Classic Spitz nevus is not considered a lesion rich in melanin, since in its classically described clinical presentation the lesion is erythematous and cupuliformic. Reed´s variant is clinically pigmented and blackened, has an increased concentration of melanin, can be histopathologically easily seen, even without the use of special stains such as Fontana-Masson.17,18However, we show that the classic histopathologic lesions exhibit variable hyperpigmentation in the histopathological examination and are often clinically pigmented.
The inflammatory infiltrate, present in 75% of cases, is consistent with the literature, with mild intensity and composed by lymphocytes.5,7,19Plasma cells may be present in melanomas, but are not commonly found in Spitz nevi. They were absent in all lesions of our series.
Spitz nevi may present mitotic figures, ranging from 10% to 58% in the different series.7,19,20We found mitoses in 30% of cases. They were all located in melanocytes of the basal layer, except for one case, in which mitosis was located in the dermis, in the top half of the lesion. The location of the mitoses is an important criterion for differentiating Spitz nevus from spitzoid melanoma. The latter is favored when mitoses are located in deeper portions (dermis) or grouped in a specific area of the lesion.
CONCLUSION
The following features of Spitz nevi are highlighted: a) it is not exclusive to children and young people, as it may occur in adults; b) symmetry and circumscription are important criteria of benignity; c) pagetoid spread and atypical cells are present in varying intensities; d) maturation of melanocytes may be absent or irregular; e) Kamino bodies are not essential; f) mitotic figures may be present in the melanocytes located near the basal layer of the epidermis and in the upper third of the lesion in the dermis. Detailed knowledge of the cytologic and architectural features of the classic histopathological picture of these peculiar lesions represented by Spitz nevi is essential for the differential diagnosis with melanomas, pointing out that no single criterion is definitive in this differentiation.
Footnotes
Conflict of interest: None
Financial funding: Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - CAPES.
How to cite this article: Verardino GC, Rochael MC. Spitz nevi in the classic histopathological pattern - lamb in wolf`s clothing. An Bras Dermatol. 2015;90(1):91-5.
Study conducted at the Hospital Universitário Antônio Pedro - Universidade Federal Fluminense (HUAP-UFF) – Niterói (RJ), Brazil.
REFERENCES
- 1.Mooi J, Krausz T. Spitz nevus versus spitzoid melanoma. Adv Anat Pathol. 2006;13:147–156. doi: 10.1097/00125480-200607000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Yoradjian A, Enokihara MM, Paschoal FM. Spitz nevus and Reed nevus. An Bras Dermatol. 2012;87:349–357. doi: 10.1590/s0365-05962012000300001. [DOI] [PubMed] [Google Scholar]
- 3.Ackerman AB, Mendonca AMN. Ackerman AB, Guo Y, Lazova R, Kaddu S. Differential Diagnosis in Dermatopathology. 2nd ed. New York: Ardor Scribendi; 2001. Spitz's Nevus, Compound Type vs. Malignant Melanoma; pp. 1:146–1:149. [Google Scholar]
- 4.Mooi J. Spitz nevus and its histologic simulators. Adv Anat Pathol. 2002;9:209–221. doi: 10.1097/00125480-200207000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Requena C, Requena L, Kutzner H, Sanchez Yus E. Spitz nevus: a clinicopathological study of 349 cases. Am J Dermatopathol. 2009;31:107–116. doi: 10.1097/DAD.0b013e3181934218. [DOI] [PubMed] [Google Scholar]
- 6.Berlingeri-Ramos AC, Morales-Burgos A, Sanchez JL, Nogales EM. Spitz Nevus in a Hispanic Population: A Clinicopathological Study of 130 Cases. Am J Dermatopathol. 2010;32:267–275. doi: 10.1097/DAD.0b013e3181c52b99. [DOI] [PubMed] [Google Scholar]
- 7.Cesinaro AM, Foroni M, Sighinolfi P, Migaldi M, Trentini GP. Spitz Nevus is relatively frequent in adults: a clinico-pathologic study of 247 cases related to patient´s age. Am J Dermatopathol. 2005;27:469–475. doi: 10.1097/01.dad.0000185249.21805.d3. [DOI] [PubMed] [Google Scholar]
- 8.Bolognia J, Jorizzo JL, Rapini RP. Dermatology. 2nd ed. Spain: Mosby; Elsevier; 2008. Chapter 112, Benign Melanocytic Neoplasms; pp. 1851–1879. [Google Scholar]
- 9.Burns T, Breathnatch S, Cox N, Griffiths C. Rook`s Textbook of Dermatology. 8th ed. Oxford: Wiley-Blackwell; 2010. Chapter 54, Lentigos, Melanocytic Naevi and Melanoma; pp. 54.1–54.57. [Google Scholar]
- 10.Unna PG. Naevi and naevocarcinome. Berl Klin Wochenschr. 1893;30:14–16. [Google Scholar]
- 11.Barnhill RL, Piepkorn M, Bussan KJ. Pathology of melanocytic nevi and malignant melanoma. Springer; New York: 2004. [Google Scholar]
- 12.Barnhill RL. The spitzoid lesion: the importance of atypical variants and risk assessment. Am J Dermatopathol. 2006;28:75–83. doi: 10.1097/01.dad.0000188868.19869.3b. [DOI] [PubMed] [Google Scholar]
- 13.Berlingeri-Ramos AC, Morales-Burgos A, Sanchez JL, Nogales EM. Spitz Nevus in a Hispanic Population: A Clinicopathological Study of 130 Cases. Am J Dermatopathol. 2010;32:267–275. doi: 10.1097/DAD.0b013e3181c52b99. [DOI] [PubMed] [Google Scholar]
- 14.Santa Cruz DJ, Walsh SN. Fletcher C. D. M. Diagnostic histopathology of tumors. Philadelphia: Elsevier; 2013. Tumors of the skin; pp. 1680–1795. [Google Scholar]
- 15.Kamino H, Flotte TJ, Misheloff E, Greco MA, Ackerman AB. Eosinophilic globules in Spitz's nevi. New findings and a diagnostic sign. Am J Dermatopathol. 1979;1:319–324. [PubMed] [Google Scholar]
- 16.LeBoit P. Kamino bodies: what they may mean. Am J Dermatopathol. 2001;23:374–377. doi: 10.1097/00000372-200108000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Choi JH, Sung KJ, Koh JK. Pigmented epithelioid cell nevus: a variant of Spitz nevus? J Am Acad Dermatol. 1993;28:497–498. doi: 10.1016/s0190-9622(08)81765-3. [DOI] [PubMed] [Google Scholar]
- 18.Requena C, Requena L, Sanchez-Yus E, Nagore E, Alfaro A, Llombart B. Pigmented epithelioid Spitz naevus: report of two cases. Histopathology. 2006;49:549–551. doi: 10.1111/j.1365-2559.2006.02485.x. [DOI] [PubMed] [Google Scholar]
- 19.Weedon D, Little JH. Spindle and epithelioid cell nevi in children and adults. A review of 211 cases of the Spitz nevus. Cancer. 1977;40:217–225. doi: 10.1002/1097-0142(197707)40:1<217::aid-cncr2820400134>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 20.Paniago-Pereira C, Maize JC, Ackerman AB. Nevus of large spindle and/or epithelioid cells (Spitz nevus) Arch Dermatol. 1978;114:1811–1823. [PubMed] [Google Scholar]


