Abstract
Background
This study assessed the contribution of organizational structures and processes identified from facility surveys to follow-up for positive Fecal Occult Blood Tests (FOBT+).
Methods
We identified 74,104 patients with FOBT+ results from 98 Veterans Health Administration (VHA) facilities between 8/16/09-3/20/11 and followed them until 9/30/11 for completion of colonoscopy. We identified patient characteristics from VHA administrative records, and organizational factors from facility surveys completed by Primary Care and Gastroenterology Chiefs. We estimated predictors of colonoscopy completion within 60 days and 6 months using hierarchical logistic regression models.
Results
30% of patients with FOBT+ results received colonoscopy within 60 days and 49% within 6 months. Having Gastroenterology or Laboratory staff notify Gastroenterology providers directly about FOBT+ cases was a significant predictor of 60-day (odds ratio (OR)=1.85, p=0.01) and 6-month follow-up (OR 1.25, p=0.008). Additional predictors of 60-day follow-up included adequacy of colonoscopy appointment availability (OR 1.43, p=0.01) and frequent individual feedback to Primary Care providers about FOBT+ referral timeliness (OR 1.79, p=0.04). Additional predictors of 6-month follow-up included using guideline-concordant surveillance intervals for low-risk adenomas (OR 1.57, p=0.01) and using group appointments and combined verbal-written methods for colonoscopy preparation instruction (OR 1.48, p=0.0001).
Conclusion
Directly notifying Gastroenterology providers about FOBT+ results, employing guideline-concordant adenoma surveillance intervals, and using colonoscopy preparations instruction methods that provide both verbal and written information may increase overall follow-up rates. Enhancing follow-up within 60-days may require increased colonoscopy capacity and feedback to Primary Care providers.
Impact
These findings may inform organizational-level interventions to improve FOBT+ follow-up.
Keywords: Early Detection of Cancer, Diagnostic Services, Mass Screening, Colorectal Neoplasms, Colonoscopy, Health Services Accessibility, Veterans Health
INTRODUCTION
Colorectal cancer is the third most common cancer and the third leading cause of cancer death among men and women in the United States.(1;2) The best known defense against colorectal cancer is early detection and prevention through routine screening. Current guidelines endorse multiple colorectal cancer screening methods,(3–5) but fecal occult blood testing (FOBT) and colonoscopy are the most widely used.(6) Two of the largest integrated health care systems in the United States (Kaiser Permanente and the Veterans Health Administration) have achieved high colorectal cancer screening rates using screening programs emphasizing FOBT.(7;8) Although randomized controlled trials have demonstrated that FOBT can be a highly efficacious screening method if FOBT positive (FOBT+) results are followed by diagnostic colonoscopy,(9–11) many FOBT-based screening programs document challenges assuring that FOBT+ results receive follow-up colonoscopy in a timely manner.(12–15) Proportions of FOBT+ cases failing to receive follow-up colonoscopy reported in prior studies range from 35–63%,(12–15) and the median waiting times from FOBT+ to colonoscopy range from 105–202 days.(12–14;16)
Both the Veterans Health Administration (VHA) and the Canadian Association of Gastroenterology Wait Time Consensus Group recommend performing a colonoscopy within 60 days of FOBT+ results.(17;18) However, recent data from the VHA documenting that 50% of FOBT+ cases fail to receive follow-up colonoscopy within this window,(19) and from a Canadian survey of Gastroenterologists documenting an average waiting time from FOBT+ results to colonoscopy of 105 days(16) suggest significant gaps remain in assuring timely follow-up. Closing these gaps will require identifying modifiable contributors to persistent FOBT+ follow-up delays.
Most prior studies examining contributors to FOBT+ follow-up have focused on non-modifiable individual-level factors,(20;21) identifying significant associations with patient age,(22–25) gender,(14;24;26) race,(25) comorbidity,(23) personal history of bowel disease,(27) family history of colorectal cancer,(28) and recent colonoscopy.(25) A few have identified modifiable individual-level contributors, including patient fears and worries about colorectal cancer(27;28) and provider awareness of guidelines(29;30) and intentions to order diagnostic testing for FOBT+ results.(26) However, very few prior studies have examined the contribution of modifiable organizational-level factors to FOBT+ follow-up patterns,(21) despite growing recognition that understanding the role that the care environment plays in assuring quality is essential to designing effective interventions and making further improvements in cancer care.(31;32)
We conducted a study to assess the contribution of modifiable organizational-level factors to FOBT+ follow-up rates. We hypothesized that higher follow-up rates would be associated with: (1) organizational structures designed to facilitate quality improvement (i.e., leadership support, resource alignment, feedback, and incentives), and (2) organizational processes that: control system-wide demand for colonoscopy (i.e., “demand efficiency” processes); minimize wasted appointments and the number of steps required to complete a colonoscopy (i.e., “supply efficiency” processes), and address patient barriers to colonoscopy completion (i.e., “patient-centered” processes). We assessed the contribution of these organizational-level factors while controlling for individual-level factors demonstrated to be associated with FOBT+ follow-up in prior studies.
MATERIALS AND METHODS
Setting and participants
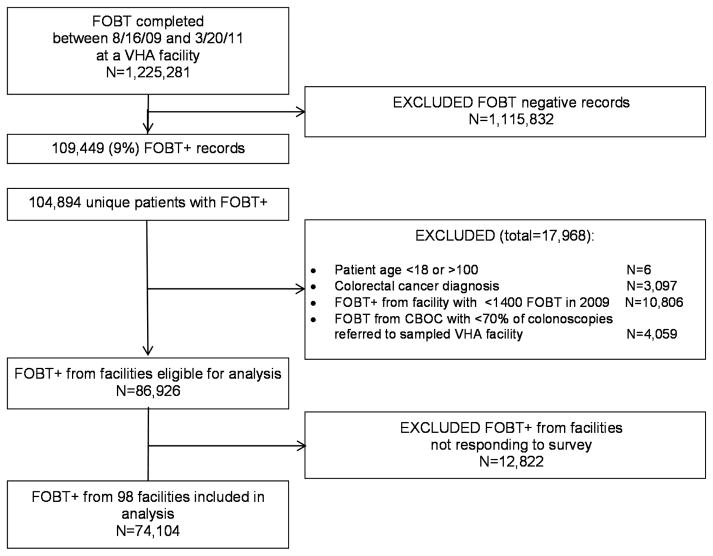
We identified a cohort of patients who had outpatient FOBT+ results from a Veterans Health Administration (VHA) facility between 8/2009-3/2011 (one year prior and six months after the start date for the organizational survey, described below) and followed them until 9/2011 (six months after the last FOBT date) for completion of follow-up colonoscopy. To identify patients with FOBT+ results, we identified from VHA laboratory records all outpatient FOBT procedures performed at VHA facilities during the sample accrual period, using the codes provided in Supplementary Material 1. We then defined FOBT+ cases as any individual card test with a positive result, or any multiple card series with one or more cards with positive results. If an eligible patient had more than one FOBT+ result in the sample selection window, the first FOBT+ result was selected for the sample. We then excluded patients if they: did not receive their FOBT+ results from one of 125 VHA facilities that conducted at least 1,400 FOBTs in 2009; were age <18 or >100 at the time the FOBT+ result was recorded; had a prior diagnosis of colorectal cancer in VHA medical records; or received their FOBT+ from a VHA community-based outpatient clinic that refers less than 70% of colonoscopies to one of the 125 VHA facilities included in the sampling frame, leaving 86,926 eligible FOBT+ patients available for analysis. We linked this patient sample to facility-level data on organizational structures and processes obtained from web-based surveys (described previously(33) and in Supplementary Material 2) administered to the Chiefs of Primary Care (73% response rate) and Gastroenterology (81% response rate) beginning in 8/2010, yielding 74,014 patients from 98 facilities responding to one or both surveys (Figure 1). We excluded 43 facilities completing <1,400 FOBT procedures in 2009 to ensure an adequate sample (≥ 100) of FOBT+ patients from each facility was available for estimating the association between organizational factors and follow-up rates.
Figure 1.
Subject Flowchart
Conceptual framework
Our conceptualization of key organizational-level contributors to FOBT+ follow-up is informed by Donabedian’s framework for understanding the quality of care,(34) and prior research documenting the association between specific organizational structures, organizational processes, individual-level factors, and quality outcomes. Organizational structures associated with quality outcomes in prior studies include: leadership support,(35;36) personal and frequent feedback, (37;38) incentives,(39) and resource alignment to improvement goals(35;36;40) (such as tracking systems,(41) and quality improvement training.(15)) Organizational processes refer to approaches used to complete each step required to assure FOBT+ follow-up (i.e., notification, referral, scheduling, patient education). For our analysis, we categorized organizational processes into three groups: (1) those that control system-wide demand for colonoscopy, which we refer to as “demand efficiency” processes; (2) those that minimize wasted appointments and the number of steps required to complete a colonoscopy, which we refer to as “supply efficiency” processes; and (3) those that address patient barriers to colonoscopy completion, which we refer to as “patient-centered” processes. Individual-level factors we control for in our hypothesis tests related to organizational-level factors include characteristics of patients and FOBT procedures found to be associated with FOBT+ follow-up rates in prior studies (i.e., age, race, residence, comorbidities, personal history of polyps, and ordering provider characteristics).
Data Sources and Measures
Our primary outcome was follow-up colonoscopy completion, identified from VHA administrative records using the codes in Supplementary Material 3. We separately examined correlates of colonoscopy completion within 60 days (the VHA recommended follow-up interval) and 6 months.
Predictors
Table 1 provides the survey question wording, response options, and coding for analysis for all organizational predictors we examined.
Table 1.
Question wording, response categories, and coding for analysis of Organizational Structure and Process measures.
| Measure | Source | Question Wording | Coding for analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Primary Care Leadership support | Primary Care Survey | Please rate each of the following potential barriers to providing timely follow-up for positive FOBTs, where 1 is not a barrier and 5 is a key barrier to providing timely follow-up for positive FOBTs. | 1=”key barrier” (category 5) 0=all other responses |
||||||
| Not a barrier | Key barrier | Don’t Know | |||||||
| 1 | 2 | 3 | 4 | 5 | |||||
| Not a priority to leadership | □ | □ | □ | □ | □ | □ | |||
|
| |||||||||
| Gastroenterology Leadership support | Gastroenterology Survey | Please rate each of the following potential barriers to providing timely follow-up for positive FOBTs, where 1 is not a barrier and 5 is a key barrier to providing timely follow-up for positive FOBTs. | 1=”key barrier” (category 5) 0=all other responses |
||||||
| Not a barrier | Key barrier | Don’t Know | |||||||
| 1 | 2 | 3 | 4 | 5 | |||||
| Not a priority to leadership | □ | □ | □ | □ | □ | □ | |||
|
| |||||||||
| Resource alignment: Tracking |
Primary Care Survey | Has your PRIMARY CARE PROGRAM assigned anyone the responsibility of tracking what happens to patients with positive FOBT results? (Select One) □ Yes Approximately how frequently does this person/s check these outcomes? (Select One) □ As needed on an ongoing basis □ Weekly □ Monthly □ Quarterly □ Don’t know □ No □ Don’t know |
1=someone is assigned to track “weekly or more frequently” 0=all other responses |
||||||
|
| |||||||||
| Resource alignment: Colonoscopy appointment availability |
Gastroenterology Survey | Please rate each of the following potential barriers to providing timely follow-up for positive FOBTs. | 1=”key barrier” (category 5) 0=all other responses |
||||||
| Not a barrier | Key barrier | Don’t Know | |||||||
| 1 | 2 | 3 | 4 | 5 | |||||
| Limited availability of colonoscopy appointments | □ | □ | □ | □ | □ | □ | |||
|
| |||||||||
| Primary Care Feedback | Primary Care Survey | Do primary care providers receive feedback about the amount of time it takes them to refer patients with positive FOBT results for colonoscopy? □ Yes □ No □ Don’t know How are primary care providers given this feedback? (Check all that apply) □ Individualized information at provider level □ Aggregate information at the team or clinic level □ Aggregate information at the facility level □ Other (specify): □ Don’t know How frequently are primary care providers given this feedback? (Select One) □ Weekly □ Monthly □ Quarterly □ Annually □ Other (specify): □ Don’t know |
0=no feedback 1=aggregate feedback at any frequency 2=individual infrequent feedback (less frequently than monthly) 3=individual frequent feedback (at least monthly) |
||||||
|
| |||||||||
| Gastroenterology Feedback | Gastroenterology survey | How is feedback on the timeliness of follow-up for patients with positive FOBT results given to GI/Endoscopy staff? (Check all that apply) □ Verbally in a staff meeting □ In writing in the form of an aggregate team, clinic or facility report □ Other (specify): □ No feedback provided to GI/Endoscopy staff on this aspect of care □ Don’t know Approximately how frequently are GI/Endoscopy staff given this feedback? (Select One) □ Weekly □ Monthly □ Quarterly □ Annually □ Don’t know |
0=written less than monthly 1=written feedback at least monthly 2=verbal feedback less than monthly 3=verbal feedback at least monthly (hypothesized as the optimal category, based on prior research)(43–44) |
||||||
|
| |||||||||
| Primary Care Incentives | Primary Care Survey | Which of the following do providers in your primary care program receive from leadership for their performance on assuring TIMELY FOLLOW-UP OF POSITIVE FOBT RESULTS? (Check all that apply) □ Recognition for good performance □ Monetary rewards for good performance □ Counseling or reprimands for poor performance □ None of the above □ Don’t know |
0=no rewards or reprimands 1=Recognition only 2=Monetary rewards (alone or in combination with other incentives) 3=Reprimands (alone or in combination with recognition) |
||||||
|
| |||||||||
| Gastroenterology Incentives | Gastroenterology Survey | Which of the following rewards or reprimands do staff in your GI/Endoscopy program receive for their performance on assuring timely follow-up of positive FOBT results? (Check all that apply) □ Recognition from leadership for good performance □ Monetary rewards for good performance □ Counseling or reprimands for poor performance □ Other (specify): □ None of the above □ Don’t know |
0=no rewards or reprimands 1=Recognition only 2=Monetary rewards (alone or in combination with other incentives) 3=Reprimands (alone or in combination with recognition) |
||||||
|
| |||||||||
| Demand Efficiency: Number of contraindications on screening reminder |
Primary Care Survey | Does your facility’s colorectal cancer screening clinical reminder ask about contraindications? □ Yes □ No □ Don’t know Which of the following contraindications are asked about in the reminder? (Check all that apply) □ Life limiting comorbidities/limited life expectancy □ Health issues that increase risk of complications of colonoscopy □ Recent colonoscopy □ Patient not willing to undergo colonoscopy if screen is positive □ Other (specify) |
0=none 1=1–2 2=3 3=4 or more |
||||||
|
| |||||||||
| Demand Efficiency: Does colonoscopy consult template include contraindications? |
Primary Care Survey | Does your Primary Care program use a consult template for referrals to Gastroenterology for follow-up of positive FOBT results? □ Yes □ No □ Don’t know Which of the following items are included in the template? (Check all that apply) □ Anticoagulant use □ Anti-platelet use □ Diabetic □ Anemia/Iron deficiency □ Life expectancy or comorbidities related to life expectancy □ Previous colonoscopy results □ Physical/cognitive impairments that would make difficult to follow prep instructions □ Lab values □ Other (specify): □ None □ Don’t know |
0=some contraindications 1=indications only 2=neither |
||||||
|
| |||||||||
| Demand Efficiency: Guideline-concordant surveillance |
Gastroenterology Survey | How soon is a repeat colonoscopy typically scheduled at your facility for the following types of patients: □ 1–2 small adenomas (<1cm) on last colonoscopy:________years |
0=not guideline-concordant (<5 years) 1=5 years 2=7–10 years |
||||||
|
| |||||||||
| Supply Efficiency: How Gastroenterology providers are notified of FOBT+ |
Gastroenterology Survey | How is the GI/Endoscopy clinic first notified of an FOBT positive result? (Check all that apply) □ Lab sends notification directly to GI/Endoscopy □ Primary care notifies using consult template/referral □ Other(specify):(n=5 said Gastroenterology identifies FOBT+) □ Don’t know |
0=Primary care notifies 1=Lab notifies 2=Gastroenterology notifies |
||||||
|
| |||||||||
| Supply Efficiency: Does prep instruction require a separate appointment? |
Gastroenterology Survey | What is the most typical way that patients receive their colonoscopy preparation instructions at your facility? (Select One) □ Written instructions provided with prep kit □ Written instructions mailed separate from prep kit □ Verbal instructions provided over the phone □ Individual appointment □ Group appointment □ Other (specify): □ Don’t know |
0=individual or group appointment (including those indicated in specified “other” responses) 1=all other categories |
||||||
|
| |||||||||
| Supply Efficiency: Pre-procedure appointment required? |
Gastroenterology Survey | Do you require a pre-procedure clinic appointment prior to the colonoscopy appointment? □ Yes □ No □ Don’t know |
0=Yes 1=No |
||||||
|
| |||||||||
| Supply Efficiency: Overbooking is used |
Gastroenterology Survey | In the past six months, did your GI program implement any of the following processes to keep up with colonoscopy demand? (Check all that apply) □ Added additional clinic hours □ Implemented make up clinics □ Added additional staff □ Increased use of contract providers □ Increased use of fee basis providers □ Overbooked appointments □ Other (specify): □ No change implemented □ Don’t know |
1=Overbooking appointments is used 0=all other responses |
||||||
|
| |||||||||
| Patient-Centered Process: Patient notification of FOBT+ includes phone contact |
Primary Care Survey | How are patients seen in your primary care program typically first notified of a positive FOBT result? (Select One) □ Letter from primary care clinic □ Letter from GI clinic □ Phone call from primary care or GI clerk □ Phone call from primary care or GI nurse □ Phone call from primary care or GI provider □ Email or secure messaging □ Other (specify): □ Don’t know |
0=notification does not include phone contact 1=notification includes some phone contact |
||||||
|
| |||||||||
| Patient-Centered Process: Are colonoscopy appointment times negotiated with patients? |
Gastroenterology Survey | Which of the following options best describes the most common way that patients are scheduled for the first appointment to follow-up on a positive FOBT at your facility? (Select One) □ Patient is sent a letter instructing them to come to the clinic at a specific date/time □ Patient is first sent a letter instructing them to call the clinic, and then an appointment date/time is negotiated over the phone □ A scheduler calls the patient to arrange an appointment date/time □ Other (specify): □ Don’t know |
1=Second and third response options, and other responses that include phone contact with patient 0=All other responses |
||||||
|
| |||||||||
| Patient-Centered Process: Do prep instruction methods include opportunities for questions? |
Gastroenterology Survey | What is the most typical way that patients receive their colonoscopy preparation instructions at your facility? (Select One) □ Written instructions provided with prep kit □ Written instructions mailed separate from prep kit □ Verbal instructions provided over the phone □ Individual appointment □ Group appointment □ Other (specify): □ Don’t know |
0=Written only 1=Verbal phone and individual appointment 2=Group appointment and “other” responses that included written and verbal combinations |
||||||
|
| |||||||||
| Patient-Centered Process: Do appointment reminders review prep instruction? |
Gastroenterology Survey | Are preparation procedures reviewed as part of the [colonoscopy appointment] reminder? □ Yes □ No □ Don’t know |
0=No reminders or reminders do not review prep 1=Reminders review prep |
||||||
Organizational structures
We measured leadership support using two items: (1) a question from the Primary Care survey asking the extent to which “not a priority to leadership” is a barrier to providing timely FOBT+ follow-up, and (2) an identical question from the Gastroenterology survey. We measured resource alignment with two items: (1) “tracking”, a question on the Primary Care Chief survey about how frequently their program tracks what happens to patients with FOBT+ results, and (2) a question on the Gastroenterology Chief survey asking the extent to which “colonoscopy appointment availability” is a barrier to providing timely FOBT+ follow-up. Feedback was assessed with two measures: (1) “Primary Care feedback”, which combined two measures on the type and frequency of feedback (see Table 1) into a single measure, and (2) “Gastroenterology feedback” which combined similar measures from the Gastroenterology survey. Incentives were assessed with two items: (1) “Primary Care Incentives”, and (2) “Gastroenterology Incentives”, both of which asked Chiefs “which of the following do [providers in your Primary Care program/staff in your Gastroenterology program] receive for their performance on assuring timely follow-up of positive FOBT results” (see Table 1 for response options and coding).
Organizational processes
Measures of demand efficiency processes included: (1) number of contraindications the facility’s colorectal cancer screening clinical reminder asks about; (2) information on the facility’s colonoscopy consult template includes contraindications; and (3) the typical surveillance interval for patients with 1–2 adenomas <1cm at the facility is guideline-consistent (i.e., 5–10 years).(42) Measures of supply efficiency processes included: (1) Gastroenterology providers are directly notified of FOBT+ cases (either by Lab or by Gastroenterology Staff who take responsibility for identifying FOBT+ cases); (2) patient colonoscopy prep instruction does not require a separate appointment; (3) a pre-op appointment is not required for colonoscopy; and (4) overbooking is used to minimize wasted appointments. Measures of patient-centered processes included: (1) patient notification of FOBT+ results includes phone contact; (2) colonoscopy appointment times are negotiated (using a scheduler or letter requesting the patient call the clinic to set up an appointment) rather than pre-assigned to patients in a mailed letter; (3) patient prep instruction procedures include opportunities for questions (i.e., some verbal instruction); and (4) patients receive colonoscopy appointment reminders that include prep instructions.
We used VHA administrative data to identify the following individual-level factors controlled for in our predictive models: age (<50, 50–64, 65–84, ≥85); race (Non-Hispanic White, Hispanic, African American, American Indian, Asian or Pacific Islander, Unknown); residence (urban, rural); drive time to the nearest VHA specialty care facility (≤60, >60 minutes); Charlson comorbidity score for the 1 year prior to the FOBT+ result; mental health diagnoses (psychiatric only, substance abuse only, or dual diagnosis, none); personal history of colorectal polyps or benign neoplasms (ICD-9 211.3-4, 569.0, v12.72); whether the FOBT was ordered by their primary care provider; what type of provider ordered their FOBT (physician, nurse practitioner or physician assistant, resident, nurse or other staff); and what type of facility ordered their FOBT (VHA specialty care facility or community-based outpatient clinic).
Analysis
Because the limited number of facilities in the sample precluded the simultaneous inclusion of a large number of facility-level predictors, we pursued the following steps to select predictors for inclusion in the final model. We initially fit separate bivariate hierarchical logistic regression models (with random effects for facility of care) for each organizational structure and process measure. We then included in a base multivariable model all measures with p-values < 0.10, or with more than a 5% difference between model estimated completion rates (among the levels of a categorical measure or between the mean and one standard deviation shift from the mean for a continuous measure). We also included in the base model month of FOBT+ result and any patient-level predictors associated with colonoscopy completion within the respective timeframe (see Supplementary Table 1 for bivariate estimates derived from this step). We then reduced the number of predictors in this model in a stepwise fashion, retaining explanatory measures with p-values <0.10. Using this final multivariable model, we constructed model-based odds ratios and least square mean completion rate estimates (using the observed marginal distributions of the other covariates) for each of the organizational structure and process measures included in the model. To explore the impact of potentially valid reasons for not completing a follow-up colonoscopy at a VHA facility on our estimates, we fit a final set of models excluding patients who may not have been appropriate for colorectal cancer screening (i.e., age <45 or >85, with documentation of limited life expectancy in the medical record, or a colonoscopy in the prior 10 years), and treating patients who refused colonoscopy or chose to pursue colonoscopy in the private sector as having adequate follow-up. Supplementary Material 4 provides details on how we estimated the prevalence of each of these reasons for not completing a colonoscopy.
Human subjects approval
The study was reviewed and approved by the Institutional Review Boards at the Minneapolis VA Medical Center (approval 9/15/2009), and the Boston VA Medical Center (approval 2/10/2010).
RESULTS
Patients included in the analysis were primarily non-Hispanic white (65%) married (53%) men (96%) over the age of 50 (95%) (Table 2). Roughly half (52%) lived in urban areas, and most (61%) lived less than 60 minutes from a VHA medical center providing specialty services. A total of 20% had a personal history of colorectal polyps or benign neoplasms, 68% had a mental health or substance abuse diagnosis, and the mean Charlson Comorbidity Score was 1.9. Most participants (58%) had their FOBT procedures ordered at a VHA hospital, by their Primary Care provider (70%), and most ordering providers were physicians (72%).
Table 2.
Characteristics of patients included in the analysis (N=74,104)
| Characteristic | N | % |
|---|---|---|
|
| ||
| Race/ethnicity | ||
| Native American | 638 | 1 |
| African American | 12,866 | 17 |
| Asian/Pacific Islander | 1,058 | 1 |
| White, Non-Hispanic | 48,018 | 65 |
| Hispanic | 4,453 | 6 |
| Unknown | 7,071 | 10 |
|
| ||
| Marital Status | ||
| Married | 38,887 | 53 |
| Widowed | 4,571 | 6 |
| All Others | 30,391 | 41 |
|
| ||
| Gender | ||
| Male | 71,067 | 96 |
| Female | 3,037 | 4 |
|
| ||
| Age | ||
| < 50 | 3,352 | 5 |
| 50 – 64 | 40,513 | 55 |
| 65 – 84 | 27,725 | 37 |
| ≥ 85 | 2,514 | 3 |
|
| ||
| Residence | ||
| Urban | 38,713 | 52 |
| Rural/Highly Rural | 35,118 | 48 |
|
| ||
| Drive time to VA Medical Center | ||
| > 60 minutes | 28,661 | 39 |
| 30–60 minutes | 17,694 | 24 |
| 6–29 minutes | 25,094 | 34 |
| <6 minutes | 2,387 | 3 |
|
| ||
| Polyps or benign neoplasms | 14,770 | 20 |
|
| ||
| Mental health diagnoses | ||
| no mental health diagnosis | 23,958 | 32 |
| psychiatric only | 19,383 | 26 |
| substance abuse only | 11,341 | 15 |
| both psychiatric and substance abuse | 19,422 | 26 |
|
| ||
| Charlson Comorbidity Score (mean and range) | 1.9 (0–19) | |
|
| ||
| FOBT ordering facility is a VHA hospital | 42,627 | 58 |
|
| ||
| FOBT was ordered by patient’s Primary Care Provider | 51,813 | 70 |
|
| ||
| FOBT ordering provider type | ||
| Physician | 53,661 | 72 |
| Nurse Practitioner, Physician Assistant | 16,203 | 22 |
| Resident | 2,686 | 4 |
| Other | 1,535 | 2 |
Few facilities cited lack of leadership support as a barrier to improving FOBT+ follow-up rates, but 38 (49%) considered colonoscopy appointment availability a barrier (Table 3). The majority (64%) reported tracking what happens to patients with FOBT+ results on a weekly or more frequent basis, but only 11% reported providing individual, frequent feedback to Primary Care Staff about their FOBT+ referral practices. A higher percentage (22%) reported providing verbal, frequent feedback to Gastroenterology Staff about colonoscopy follow-up rates. The majority reported no incentives for Primary Care (56%) or Gastroenterology Staff (63%) tied to FOBT+ follow-up performance. About half (48%) reported including some information on contraindications on their colorectal cancer screening clinical reminder, and 47% reported including information on contraindications on their colonoscopy consult template. The modal surveillance interval for patients with 1–2 adenomas <1cm was 5 years (84%). Most (70%) relied on Primary Care to notify Gastroenterology of FOBT+ cases, and most (70%) did not require a separate appointment for colonoscopy prep instruction. The majority (62%) did not require a pre-op appointment for colonoscopy, and 54% reported using overbooking to minimize wasted colonoscopy appointments. Most (67%) used patient notification procedures that included some phone contact, but scheduling procedures were highly variable. The approach used to instruct patients about colonoscopy preparation was highly variable, with 36% using written methods only, 23% using verbal methods delivered by phone or an individual appointment, and 32% using group appointments or some other method involving both written and verbal instruction. Finally, most (69%) did not review prep procedures in their colonoscopy appointment reminders.
Table 3.
Distribution of facilities and patients across organizational structures and processes examined
| Characteristic | Facilities (N=98)1 | Patients (N=74,104) | ||
|---|---|---|---|---|
| N | % | N | % | |
| ORGANIZATIONAL STRUCTURES | ||||
| Leadership support GI | ||||
| Primary Care leadership support b Is a key barrier | 0 | 0 | 0 | 0 |
| Is not a key barrier | 75 | 100 | 56,897 | 100 |
| Missing | 23 | 17,207 | ||
| Gastroenterology leadership support c - Is a key barrier | 2 | 2 | 671 | 1 |
| Is not a key barrier | 78 | 98 | 61,171 | 99 |
| Missing | 18 | 12,262 | ||
| Resources | ||||
| Colonoscopy appointment availability c - Is a key barrier | 38 | 49 | 37,658 | 63 |
| Is not a key barrier | 39 | 51 | 22,021 | 37 |
| Missing | 21 | 17,207 | ||
| Tracking b > weekly | 15 | 20 | 13,340 | 21 |
| At least weekly | 27 | 36 | 26,513 | 42 |
| No tracking | 33 | 44 | 23,429 | 37 |
| Missing | 23 | 10,822 | ||
| Feedback | ||||
| Primary Care feedback b – Aggregate | 5 | 6 | 2,655 | 4 |
| None | 47 | 62 | 34,001 | 59 |
| Individual, infrequent | 8 | 11 | 6,520 | 11 |
| Individual, frequent | 16 | 21 | 14,394 | 25 |
| Missing | 22 | 16,534 | ||
| Gastroenterology feedback c - None | 22 | 27 | 15,014 | 24 |
| Written, infrequent | 18 | 22 | 14,720 | 23 |
| Verbal, infrequent | 12 | 15 | 12,146 | 19 |
| Verbal, frequent | 18 | 22 | 13,432 | 21 |
| Written, frequent | 11 | 14 | 7,970 | 13 |
| Missing | 17 | 10,822 | ||
| Incentives | ||||
| Primary Care incentives b - None | 42 | 56 | 28,439 | 50 |
| Recognition only | 6 | 8 | 4,789 | 8 |
| Monetary reward (alone or in combination with other strategies) | 6 | 8 | 4,452 | 8 |
| Reprimand (alone or in combination with recognition) | 21 | 28 | 19,217 | 34 |
| Missing | 23 | 17,207 | ||
| Gastroenterology incentives c – None | 52 | 64 | 37,204 | 59 |
| Recognition only | 15 | 19 | 12,893 | 20 |
| Monetary reward (alone or in combination with other strategies) | 7 | 9 | 6,257 | 10 |
| Reprimand (alone or in combination with recognition) | 7 | 9 | 6,599 | 10 |
| Missing | 17 | 10,822 | ||
| ORGANIZATIONAL PROCESSES | ||||
| Demand Efficiency Processes | ||||
| Contraindications on colorectal Cancer Screening Reminder b – None | 39 | 52 | 29,996 | 53 |
| 1–2 | 21 | 28 | 14,327 | 25 |
| 3 | 7 | 9 | 4,669 | 8 |
| 4+ | 8 | 11 | 7,905 | 14 |
| Missing | 23 | 17,207 | ||
| Information on colonoscopy consult b - Contraindications | 35 | 47 | 29,167 | 51 |
| Indication | 22 | 29 | 16,781 | 29 |
| Neither | 18 | 24 | 10,949 | 19 |
| Missing | 23 | 17,207 | ||
| Surveillance for 1–2 Adenomas <1 cm c – <5 years | 6 | 8 | 2,519 | 4 |
| 5 years | 67 | 84 | 56,645 | 90 |
| 7–10 years | 7 | 9 | 3,693 | 6 |
| Missing | 18 | 11,247 | ||
| Supply Efficiency Processes | ||||
| Gastroenterology notification c - by primary care | 55 | 70 | 42,829 | 69 |
| by Lab | 19 | 24 | 14,005 | 22 |
| by Gastroenterology | 5 | 6 | 5,512 | 9 |
| Missing | 19 | 11,758 | ||
| Colonoscopy prep instruction c – separate appointment required | 24 | 30 | 21,079 | 33 |
| Separate appointment not required | 57 | 70 | 42,203 | 67 |
| Missing | 17 | 10,822 | ||
| Pre-op Appointment c – required | 31 | 38 | 28,060 | 44 |
| Not required | 50 | 62 | 35,222 | 56 |
| Missing | 17 | 10,822 | ||
| Overbooking c – is used to meet colonoscopy demand | 43 | 54 | 38,087 | 60 |
| Is not used | 24 | 30 | 17,427 | 28 |
| No changes to meet colonoscopy demand | 13 | 16 | 7,494 | 12 |
| Missing | 18 | 11,096 | ||
| Patient-centered Processes | ||||
| Patients notification b – Written contact only | 25 | 33 | 21,649 | 38 |
| Some phone contact | 50 | 67 | 35,248 | 62 |
| Missing | 23 | 17207 | ||
| Colonoscopy Scheduling c – call from scheduler | 25 | 31 | 19,560 | 31 |
| Letter requesting patient call for appointment | 11 | 14 | 7,887 | 12 |
| Letter with assigned appointment | 28 | 35 | 23,895 | 38 |
| Other | 17 | 21 | 11,940 | 19 |
| Missing | 17 | 10,822 | ||
| Colonoscopy prep instruction c – Verbal phone and individual appointment | 19 | 23 | 15,965 | 25 |
| Written only | 36 | 44 | 23,442 | 37 |
| Verbal Group or other combined verbal/written method | 16 | 32 | 23,875 | 38 |
| Missing | 17 | 10,822 | ||
| Appointment reminders c – do not review prep/no reminder | 25 | 31 | 24,385 | 39 |
| Do review prep | 56 | 69 | 38,897 | 61 |
| Missing | 17 | 10,822 | ||
Distribution from 81 facilities responding to Gastroenterology Survey, or 76 responding to Primary care survey, depending on measure (98 facilities responded to one or both of the surveys).
Primary Care survey item
Gastroenterology survey item
The cumulative proportion of patients with FOBT+ results receiving a colonoscopy at a VHA facility within 60 days was 30% (range 10–57% across facilities). Organizational structures significantly associated with 60-day follow-up rates in the multivariable model included: colonoscopy appointment availability is not a key barrier (OR 1.43, CI 1.09–1.90, p=0.01); and monthly or more frequent Primary Care feedback (OR 1.79, CI 1.02–3.16, p=0.04). Organizational processes significantly associated with 60-day follow-up rates in the multivariable model included: colonoscopy consult information does not ask about indication or contraindications for colonoscopy (OR 1.48, CI 1.07–2.05, p=0.02), or asks about indication only (OR 1.49, CI 1.10–2.02, p=0.01) (a finding counter to our demand efficiency hypothesis), and Gastroenterology notification directly of FOBT+ results by Gastroenterology Staff (OR 1.85, CI 1.17–2.91, p=0.01) (Table 4). No patient-centered process measures were significantly associated with the 60-day outcomes in the adjusted model. After excluding potentially inappropriate FOBTs, and treating refusals and private sector colonoscopies completed after the FOBT+ as adequately followed up, the estimated follow-up rates increase markedly, and the odds ratio estimates for colonoscopy appointment availability and Gastroenterology notification remain significant. However, the odds ratio estimates for Primary Care feedback, and colonoscopy consult information attenuate and are no longer statistically significant.
Table 4.
Odds ratios, 95% confidence intervals, and follow-up percentage estimates for organizational structures and processes derived from the original and sensitivity-adjusteda multivariable regression models for 60-day follow-up rate outcome measure.b,c
| Characteristic | Original Multivariable estimates | Sensitivity-adjusteda Multivariable estimates. | ||
|---|---|---|---|---|
| OR (95% CI) | Follow-up % (95% CI) | OR (95% CI) | Follow-up % (95% CI) | |
| ORGANIZATIONAL STRUCTURES | ||||
| Resources | ||||
| Colonoscopy appointment availability - Is a key barrier | 1.00 | 26 (23–30) | 1.00 | 48 (43–52) |
| Is not a key barrier | 1.43 (1.09–1.90) | 34 (30–38) | 1.48 (1.14–1.92) | 58 (53–62) |
| Feedback | ||||
| Primary Care feedback - Aggregate | 1.00 | 24 (16–34) | 1.00 | 48 (37–60) |
| None | 1.09 (0.65–1.82) | 26 (22–29) | 0.96 (0.59–1.58) | 47 (43–51) |
| Individual, infrequent | 1.52 (0.85–2.71) | 32 (25–40) | 1.32 (0.75–2.31) | 55 (47–63) |
| Individual, frequent | 1.79 (1.02–3.16) | 36 (30–43) | 1.71 (0.99–2.97) | 61 (54–68) |
| ORGANIZATIONAL PROCESSES | ||||
| Demand Efficiency Processes | ||||
| Information on colonoscopy consult - Contraindications | 1.00 | 25 (22–29) | 1.00 | 48 (44–53) |
| Indication | 1.49 (1.10–2.02) | 33 (28–40) | 1.30 (0.96–1.74) | 55 (49–61) |
| Neither | 1.48 (1.07–2.05) | 33 (27–40) | 1.19 (0.86–1.63) | 53 (46–60) |
| Supply Efficiency Processes | ||||
| Gastroenterology notification – by Primary Care | 1.00 | 26 (24–30) | 1.00 | 48 (45–52) |
| by lab | 1.36 (0.97–1.90) | 33 (26–40) | 1.24 (0.89–1.73) | 54 (46–61) |
| by Gastroenterology | 1.85 (1.17–2.91) | 40 (30–50) | 1.82 (1.17–2.83) | 63 (53–72) |
Excluding patients who may not have been appropriate for colorectal cancer screening (age <45 or >85, documentation of limited life expectancy in the medical record, or colonoscopy in the prior 10 years), and treating patients who refused colonoscopy or chose to pursue colonoscopy in the private sector as having adequate follow-up.
Bold odds ratios are significant at p <0.05
Odds ratios for the individual-level factors controlled for in the 60-day model (age, race, residence, drive time to the nearest VHA specialty care facility, personal history of colorectal polyps or benign neoplasms, Charlson comorbidity score for the 1 year prior to the FOBT+ result, mental health diagnoses, whether the FOBT was ordered by their primary care provider, and what type of facility ordered their FOBT) are provided in Supplementary Table 2.
The cumulative proportion of patients with FOBT+ results receiving a colonoscopy within 6 months was 49% (range 30–70% across facilities). No organizational structures were significantly associated with the 6-month outcome in the multivariable model. Organizational processes significantly associated with 6-month follow-up rates in the multivariable model included: using an adenoma surveillance interval of at least 5 years (5 years OR 1.32, CI 1.02–1.71, p=0.04; 7–10 years OR 1.57, CI 1.11–2.20, p=0.01); having Gastroenterology notification directly from lab about FOBT+ cases (OR 1.25, CI 1.06–1.47, p=0.008); and using group appointments or other combined verbal and written methods to provide patient colonoscopy prep instruction (OR 1.48, CI 1.22–1.79, p=0.05) (Table 5). After excluding potentially inappropriate FOBTs, and treating refusals and private sector colonoscopies completed after the FOBT+ as adequately followed up (last 2 columns of Table 5), the estimated follow-up rates increase to more than 67% in all subgroups, and only the estimate of group appointment for colonoscopy prep instructions remained significant (OR 1.50, CI 1.16–1.95, p=0.003).
Table 5.
Odds ratios, follow-up percentage estimates, and 95% confidence intervals for organizational processes significantly associated with 6-month follow-up rates in original and sensitivity-adjusteda multivariable logistic regression models.b,c
| Characteristic | Original Multivariable estimates | Sensitivity-Adjusteda Multivariable estimates | ||
|---|---|---|---|---|
| OR (95% CI) | Follow-up % (95% CI) | OR (95% CI) | Follow-up % (95% CI) | |
| Demand Efficiency Processes | ||||
| Surveillance for 1–2 Adenomas <1 cm – <5 years | 1.00 | 42 (36–48) | 1.00 | 70 (63–76) |
| 5 years | 1.32 (1.02–1.71) | 49 (47–50) | 1.14 (0.80–1.62) | 73 (71–75) |
| 7–10 years | 1.57 (1.11–2.20) | 53 (47–58) | 1.33 (0.84–2.12) | 76 (70–82) |
| Supply Efficiency Processes | ||||
| Gastroenterology notification - by primary care | 1.00 | 47 (45–49) | 1.00 | 72 (69–74) |
| by lab | 1.25 (1.06–1.47) | 52 (49–56) | 1.18 (0.94–1.48) | 75 (71–78) |
| by Gastroenterology | 1.31 (0.99–1.73) | 53 (47–60) | 1.43 (0.98–2.10) | 78 (72–84) |
| Patient-Centered Processes | ||||
| Colonoscopy prep instruction – verbal phone or individual appointment | 1.00 | 43 (40–47) | 1.00 | 68 (64–72) |
| Written only | 1.18 (1.00–1.40) | 48 (45–50) | 1.22 (0.97–1.53) | 72 (69–75) |
| Verbal group appointment or other combined verbal/written method | 1.48 (1.22–1.79) | 53 (50–56) | 1.50 (1.16–1.95) | 76 (73–79) |
Excluding patients who may not have been appropriate for colorectal cancer screening (age <45 or >85, documentation of limited life expectancy in the medical record, or colonoscopy in the prior 10 years), and treating patients who refused colonoscopy or chose to pursue colonoscopy in the private sector as having adequate follow-up.
Bold odds ratios are significant at p <0.05
Odds ratios for the individual-level factors controlled for in the 6-month model (age, race, residence, drive time to the nearest VHA specialty care facility, personal history of colorectal polyps or benign neoplasms, Charlson comorbidity score for the 1 year prior to the FOBT+ result, mental health diagnoses, whether the FOBT was ordered by their primary care provider, what type of provider ordered their FOBT, and what type of facility ordered their FOBT) are provided in Supplementary Table 2.
DISCUSSION
Consistent with our hypothesis that organizational structures supporting quality improvement would be positively associated with follow-up rates, we found that adequacy of colonoscopy appointment availability, and providing primary care providers with individual, frequent feedback about the timeliness of FOBT+ referrals were positively associated with receiving follow-up colonoscopy within 60 days of an FOBT+. These findings are consistent with prior research documenting that limited colonoscopy capacity is the most common barrier to reducing FOBT+ follow-up delay,(41) and that individual, frequent feedback can improve adherence to clinical practice guidelines.(43;44) However, the fact that no organizational structures were significantly associated with 6 month follow-up rates suggests that these factors have more influence on how quickly, rather than whether, patients with FOBT+ results receive colonoscopy follow-up.
We found partial support for our hypotheses that higher follow-up rates would be associated with organizational processes enhancing demand efficiency, supply efficiency, and patient-centered processes. Specifically, our findings suggest that: using surveillance intervals for low-risk adenomas that are not more aggressive than recommended by guidelines(42) (a demand efficiency measure); assigning responsibility for identifying FOBT+ cases to Lab or Gastroenterology staff (a supply efficiency measure); and employing group and other combined verbal and written colonoscopy prep instruction processes (a patient-centered process) are positively associated with overall follow-up rates.
One organizational process measure (Gastroenterology providers are notified by lab or Gastroenterology Staff about FOBT+ results) was significantly associated with both 60-day and 6-month follow-up rates. These results are consistent with findings from a prior randomized trial conducted in four VHA facilities, which found 30-day, 90-day and 6-month follow-up rates improved significantly (by 9–31%, p<0.03) in facilities that implemented an electronic intervention to directly notify Gastroenterology staff of FOBT+ results, but did not significantly change in the usual care comparison facilities.(2)
Counter to our hypothesis that organizational processes designed to reduce unnecessary demand for colonoscopy would be positively associated with follow-up rates, we found facilities that asked about contraindications on colonoscopy consult templates had lower rather than higher 60-day follow-up rates. This finding might be explained by the fact that patients with documented limited life expectancy, recent colonoscopy, and refusal to complete follow-up colonoscopy were not initially excluded from our sample. Indeed, after excluding these cases from the analysis, the association of consult template characteristics with follow-up rates was no longer statistically significant. Thus, including information on contraindications on the colonoscopy consult template may identify individuals who should not have been screened, and some of these individuals appropriately do not have follow-up colonoscopy.
We hypothesized that colonoscopy prep instruction processes that involve some verbal instruction would be associated with higher follow-up rates than methods that involved only written instruction because verbal instruction processes would provide more opportunities to address patient questions. However, our findings suggest that some forms of verbal instruction (i.e., phone and individual appointments) were associated with lower 6-month follow-up rates than written only instruction methods. Because we did not collect information on the specific content of the prep instruction provided, we can only speculate about why group preparation instruction and other combined verbal and written methods were superior to verbal phone and individual appointment instruction. One possibility is that group prep appointments and other combined methods may employ a more structured approach than other verbal instruction methods, and so are more likely to encourage patients to identify and clarify aspects of the preparation they do not understand. Alternatively the group/peer setting and other combined approaches may prompt greater patient engagement. The resulting enhanced clarification and/or engagement may increase the proportion of patients that attend their scheduled colonoscopy appointment and present with adequate bowel preparation, thereby reducing delays associated with needing to reschedule colonoscopy appointments. A final possibility is that instruction approaches that require patients to complete a group class or other formal instruction before scheduling a colonoscopy lead to self-selection of individuals that are more likely to adhere to their colonoscopy appointment. All of these explanations are consistent with findings from one prior randomized trial, which found that patients participating in a nurse-led group colonoscopy prep education program had higher colonoscopy completion rates and lower cancellation rates due to poor bowel preparation than patients who received an educational brochure only.(45) Our finding that other measures of patient-centered processes (phone results notification, negotiated appointment scheduling, appointment reminders that review prep instructions) were not associated with follow-up rates contrasts with previous studies attributing high endoscopy attendance to patient-centered processes such as education(46) and reminder systems,(47;48) may be unique to this patient population trained in the hierarchical traditions of the military, and may not generalize to other health care settings.
This study has a number of strengths, including the large sample size of patients and medical facilities, the rigorous methodology used to adjust our estimates for reasons a colonoscopy was not completed, and the fact that it identifies several modifiable organizational predictors of FOBT+ follow-up rates. However, our findings should be qualified by several limitations. First, we may be underestimating actual follow-up rates because some patients with FOBT+ results may have pursued colonoscopy outside of the VHA. Indeed secondary analyses we conducted on this cohort suggest that up to 15% of patients with FOBT+ results who did not receive a colonoscopy in VHA within 6 months had documentation in their chart notes that they were pursuing colonoscopy in the private sector. However, sensitivity analyses treating patients with documentation of pursuing colonoscopy in the private sector as adequately followed up did not significantly alter the pattern of associations between organizational factors and follow-up rates reported here. A second possible limitation is that our measures of organizational structures and processes may include some measurement error. Structure and process reports from Chiefs were measured at one point in time, in most cases with single-item measures, and may therefore be inaccurate (given that facilities may make periodic adjustments to structures and processes) or insufficiently sensitive (from oversimplification of the underlying processes). Further, lack of variability in our sample forced us to collapse potentially distinct categories for several measures. Future studies should examine whether more detailed measures in more variable facility samples yield different results. Additionally, our analysis excluded 12,822 FOBT+ patients from 25 facilities with incomplete facility survey data, and 10,806 FOBT+ from 43 facilities conducting fewer than 1,400 FOBTs in 2009, which may raise concerns about whether our findings can be generalized to FOBT+ patients from other VHA facilities in the sampling frame. However, our previous analysis of the survey data found no significant variation in facility FOBT+ follow-up rates or characteristics by survey response status,(33) and facilities excluded based on FOBT volume represented not only smaller facilities with FOBT-based screening programs, but also larger facilities with colonoscopy-based screening programs. Finally, the VHA is a unique context, characterized by a predominantly male, low income population with higher than average comorbidity burden, including high rates of mental health and substance abuse diagnoses. Therefore, our findings may not generalize to other health care contexts. Given that VHA is the largest integrated health care system in the United States, however, our findings have important implications for a substantial population of health providers and consumers in this country.
Despite these limitations, the insights gleaned from this study regarding the role organizational structures and processes can play in assuring patients with FOBT+ results receive timely colonoscopy will be helpful in guiding future efforts to improve FOBT+ follow-up rates. Specifically, our most robust findings suggest that Gastroenterology clinics may be able to significantly increase the proportion of FOBT+ results that receive follow-up colonoscopy by assuming responsibility for identifying FOBT+ results, and employing prep education processes that include both written and verbal information, but in order to increase the proportion of FOBT+ patients that receive follow-up colonoscopy within 60 days, it may be necessary to increase colonoscopy appointment availability. Given that the significant organizational-level predictors of follow-up rates we identified all had modest effects (i.e., resulting in at most 5–14% differences in follow-up rates), multifaceted strategies designed not only to increase colonoscopy follow-up for FOBT+ results, but also to reduce FOBT use in patients who would not complete colonoscopy follow-up due to contraindications or personal preference, may be needed to close remaining gaps. A fruitful area for future research would be the evaluation of such multifaceted strategies.
Supplementary Material
Acknowledgments
Financial support: This research was funded by the Department of Veterans Affairs Health Services Research & Development (VA HSR&D) grant # IIR 08-334-2 (Partin), VA HSR&D Research Career Scientist award #RCS 10-185 (Partin), VA HSR&D Career Development Award (CDA) #CDA 07-016 (Haggstrom) VA HSR&D CDA #CDA 08-024 (Powell), VA Clinical Science Research & Development Career Development Award CDA-2 (Shaukat), and National Institute on Aging at the National Institutes of Health grant # K24AG041180 (Walter). The views expressed in this article are those of the authors and do not necessarily represent the position or policy of the Department of Veterans Affairs or the National Institutes of Health.
Footnotes
Potential competing interests: None
Reference List
- 1.American Cancer Society. Cancer Facts and Figures 2013. Atlanta: American Cancer Society; 2013. [Google Scholar]
- 2.Humphrey LL, Shannon J, Partin MR, O’Malley J, Chen Z, Helfand M. Improving the follow-up of positive hemoccult screening tests: an electronic intervention. J Gen Intern Med. 2011 Jul;26(7):691–7. doi: 10.1007/s11606-011-1639-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levin B, Lieberman DA, McFarland B, Andrews KS, Brooks D, Bond J, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. Gastroenterology. 2008 May;134(5):1570–95. doi: 10.1053/j.gastro.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 4.Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA, Inadomi JM. American College of Gastroenterology guidelines for colorectal cancer screening 2009 [corrected] Am J Gastroenterol. 2009 Mar;104(3):739–50. doi: 10.1038/ajg.2009.104. [DOI] [PubMed] [Google Scholar]
- 5.USPSTF. Screening for colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008 Nov 4;149(9):627–37. doi: 10.7326/0003-4819-149-9-200811040-00243. [DOI] [PubMed] [Google Scholar]
- 6.Yabroff KR, Klabunde CN, Yuan G, McNeel TS, Brown ML, Casciotti D, et al. Are Physicians’ Recommendations For Colorectal Cancer Screening Guideline-Consistent? Journal of General Internal Medicine. 2010 Oct 14;26(2):177–84. doi: 10.1007/s11606-010-1516-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levin TR, Jamieson L, Burley DA, Reyes J, Oehrli M, Caldwell C. Organized colorectal cancer screening in integrated health care systems. Epidemiol Rev. 2011 Jul;33(1):101–10. doi: 10.1093/epirev/mxr007. [DOI] [PubMed] [Google Scholar]
- 8.El Serag HB, Petersen L, Hampel H, Richardson P, Cooper G. The use of screening colonoscopy for patients cared for by the Department of Veterans Affairs. Arch Intern Med. 2006 Nov 13;166(20):2202–8. doi: 10.1001/archinte.166.20.2202. [DOI] [PubMed] [Google Scholar]
- 9.Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996 Nov 30;348(9040):1472–7. doi: 10.1016/S0140-6736(96)03386-7. [DOI] [PubMed] [Google Scholar]
- 10.Kronborg O, Fenger C, Olsen J, Jorgensen OD, Sondergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet. 1996 Nov 30;348(9040):1467–71. doi: 10.1016/S0140-6736(96)03430-7. [DOI] [PubMed] [Google Scholar]
- 11.Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993 May 13;328(19):1365–71. doi: 10.1056/NEJM199305133281901. [DOI] [PubMed] [Google Scholar]
- 12.Gellad ZF, Almirall D, Provenzale D, Fisher DA. Time from positive screening fecal occult blood test to colonoscopy and risk of neoplasia. Dig Dis Sci. 2009 Nov;54(11):2497–502. doi: 10.1007/s10620-008-0653-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Larson MF, Ko CW, Dominitz JA. Effectiveness of a provider reminder on fecal occult blood test follow-up. Dig Dis Sci. 2009 Sep;54(9):1991–6. doi: 10.1007/s10620-009-0751-2. [DOI] [PubMed] [Google Scholar]
- 14.Paszat L, Rabeneck L, Kiefer L, Mai V, Ritvo P, Sullivan T. Endoscopic follow-up of positive fecal occult blood testing in the Ontario FOBT Project. The Canadian Journal of Gastroenterology. 2007 Jun;21(6):379–82. doi: 10.1155/2007/569689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Powell AA, Nugent S, Ordin DL, Noorbaloochi S, Partin MR. Evaluation of a VHA Collaborative to Improve Follow-up After a Positive Colorectal Cancer Screening Test. Medical Care. 2011;49(41):897–903. doi: 10.1097/MLR.0b013e3182204944. [DOI] [PubMed] [Google Scholar]
- 16.Leddin D, Armstrong D, Borgaonkar M, Bridges RJ, Fallone CA, Telford JJ, et al. The 2012 SAGE wait times program: Survey of Access to GastroEnterology in Canada. Can J Gastroenterol. 2013 Feb;27(2):83–9. doi: 10.1155/2013/143018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Paterson WG, Depew WT, Pare P, Petrunia D, Switzer C, Veldhuyzen van Zanten SJ, et al. Canadian consensus on medically acceptable wait times for digestive health care. Canadian Journal of Gastroenterology. 2006 Jun;20(6):411–23. doi: 10.1155/2006/343686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Veterans Health Administration. VHA Directive 2007–004: Colorectal Cancer Screening. Washington DC: Department of Veterans Affairs; 2007. Jan 12, [Google Scholar]
- 19.Combined Assessment Program Summary Report: Evaluation of Colorectal Cancer Screening and Follow-Up in Veterans Health Administration Facilities. Department of Veterans Affairs Office of Inspector General; 2013. [Google Scholar]
- 20.Zapka J, Taplin SH, Price RA, Cranos C, Yabroff R. Factors in quality care--the case of follow-up to abnormal cancer screening tests--problems in the steps and interfaces of care. J Natl Cancer Inst Monogr. 2010;2010(40):58–71. doi: 10.1093/jncimonographs/lgq009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zapka JM, Edwards HM, Chollette V, Taplin SH. Follow-up to Abnormal Cancer Screening Tests: Considering the Multilevel Context of Care. Cancer Epidemiol Biomarkers Prev. 2014 Oct;23(10):1965–73. doi: 10.1158/1055-9965.EPI-14-0454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Choi KS, Lee HY, Jun JK, Shin A, Park EC. Adherence to follow-up after a positive fecal occult blood test in an organized colorectal cancer screening program in Korea, 2004–2008. J Gastroenterol Hepatol. 2012 Jun;27(6):1070–7. doi: 10.1111/j.1440-1746.2011.06944.x. [DOI] [PubMed] [Google Scholar]
- 23.Fisher DA, Zullig LL, Grambow SC, Abbott DH, Sandler RS, Fletcher RH, et al. Determinants of medical system delay in the diagnosis of colorectal cancer within the Veteran Affairs Health System. Dig Dis Sci. 2010 May;55(5):1434–41. doi: 10.1007/s10620-010-1174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miglioretti DL, Rutter CM, Bradford SC, Zauber AG, Kessler LG, Feuer EJ, et al. Improvement in the diagnostic evaluation of a positive fecal occult blood test in an integrated health care organization. Med Care. 2008 Sep;46(9 Suppl 1):S91–S96. doi: 10.1097/MLR.0b013e31817946c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rao SK, Schilling TF, Sequist TD. Challenges in the management of positive fecal occult blood tests. J Gen Intern Med. 2009 Mar;24(3):356–60. doi: 10.1007/s11606-008-0893-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Turner B, Myers RE, Hyslop T, Hauck WW, Weinberg D, Brigham T, et al. Physician and patient factors associated with ordering a colon evaluation after a positive fecal occult blood test. J Gen Intern Med. 2003 May;18(5):357–63. doi: 10.1046/j.1525-1497.2003.20525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ishikawa Y, Zheng YF, Nishiuchi H, Suda T, Hasumi T, Saito H. Classification tree analysis to enhance targeting for follow-up exam of colorectal cancer screening. BMC Cancer. 2013;13:470. doi: 10.1186/1471-2407-13-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shields HM, Weiner MS, Henry DR, Lloyd JA, Ransil BJ, Lamphier DA, et al. Factors that influence the decision to do an adequate evaluation of a patient with a positive stool for occult blood. Am J Gastroenterol. 2001 Jan;96(1):196–203. doi: 10.1111/j.1572-0241.2001.03475.x. [DOI] [PubMed] [Google Scholar]
- 29.Lurie JD, Welch HG. Diagnostic testing following fecal occult blood screening in the elderly. J Natl Cancer Inst. 1999 Oct 6;91(19):1641–6. doi: 10.1093/jnci/91.19.1641. [DOI] [PubMed] [Google Scholar]
- 30.Nadel MR, Berkowitz Z, Klabunde CN, Smith RA, Coughlin SS, White MC. Fecal Occult Blood Testing Beliefs and Practices of U.S. Primary Care Physicians: Serious Deviations from Evidence-Based Recommendations. Journal of General Internal Medicine. 2010 Apr 10; doi: 10.1007/s11606-010-1328-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taplin SH, Clauser S, Rodgers AB, Breslau E, Rayson D. Interfaces across the cancer continuum offer opportunities to improve the process of care. J Natl Cancer Inst Monogr. 2010;2010(40):104–10. doi: 10.1093/jncimonographs/lgq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clauser SB, Taplin SH, Foster MK, Fagan P, Kaluzny AD. Multilevel intervention research: lessons learned and pathways forward. J Natl Cancer Inst Monogr. 2012 May;2012(44):127–33. doi: 10.1093/jncimonographs/lgs019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Partin MR, Powell AA, Burgess DJ, Haggstrom D, Gravely AA, Halek K, et al. Adding Postal Follow-Up to a Web-Based Survey of Primary Care and Gastroenterology Clinic Physician Chiefs Improved Response Rates but not Response Quality or Representativeness. Eval Health Prof. 2014 doi: 10.1177/0163278713513586. published online 5 December 2013. [DOI] [PubMed] [Google Scholar]
- 34.Donabedian A. Explorations in Quality Assessment and Monitoring. I. Ann Arbor, MI: Health Administration Press; 1980. [Google Scholar]
- 35.Lukas C, Holmes S, Cohen A, Restuccia J, Cramer I, Shwartz M, et al. Transformational change in health care systems: An organizational model. Health Care Management Review. 2007;32(4):309–20. doi: 10.1097/01.HMR.0000296785.29718.5d. [DOI] [PubMed] [Google Scholar]
- 36.Anhang PR, Zapka J, Edwards H, Taplin SH. Organizational factors and the cancer screening process. J Natl Cancer Inst Monogr. 2010;2010(40):38–57. doi: 10.1093/jncimonographs/lgq008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mandelblatt JS, Yabroff KR. Effectiveness of interventions designed to increase mammography use: a meta-analysis of provider-targeted strategies. Cancer Epidemiol Biomarkers Prev. 1999 Sep;8(9):759–67. [PubMed] [Google Scholar]
- 38.Myers RE, Turner B, Weinberg D, Hyslop T, Hauck WW, Brigham T, et al. Impact of a physician-oriented intervention on follow-up in colorectal cancer screening. Prev Med. 2004 Apr;38(4):375–81. doi: 10.1016/j.ypmed.2003.11.010. [DOI] [PubMed] [Google Scholar]
- 39.Engelstad LP, Stewart SL, Nguyen BH, Bedeian KL, Rubin MM, Pasick RJ, et al. Abnormal Pap smear follow-up in a high-risk population. Cancer Epidemiol Biomarkers Prev. 2001 Oct;10(10):1015–20. [PubMed] [Google Scholar]
- 40.Yano EM, Soban LM, Parkerton PH, Etzioni DA. Primary care practice organization influences colorectal cancer screening performance. Health Services Research. 2007 Jun;42(3 Pt 1):1130–49. doi: 10.1111/j.1475-6773.2006.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Powell AA, Gravely AA, Ordin DL, Schlosser JE, Partin MR. Timely follow-up of positive fecal occult blood tests strategies associated with improvement. Am J Prev Med. 2009 Aug;37(2):87–93. doi: 10.1016/j.amepre.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 42.Winawer SJ, Zauber AG, Fletcher RH, Stillman JS, O’Brien MJ, Levin B, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130:1872–85. doi: 10.1053/j.gastro.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 43.Hysong SJ. Meta-analysis: audit and feedback features impact effectiveness on care quality. Med Care. 2009 Mar;47(3):356–63. doi: 10.1097/MLR.0b013e3181893f6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;6:CD000259. doi: 10.1002/14651858.CD000259.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abuksis G, Mor M, Segal N, Shemesh I, Morad I, Plaut S, et al. A patient education program is cost-effective for preventing failure of endoscopic procedures in a gastroenterology department. Am J Gastroenterol. 2001 Jun;96(6):1786–90. doi: 10.1111/j.1572-0241.2001.03872.x. [DOI] [PubMed] [Google Scholar]
- 46.Denberg TD, Coombes JM, Byers TE, Marcus AC, Feinberg LE, Steiner JF, et al. Effect of a mailed brochure on appointment-keeping for screening colonoscopy: a randomized trial. Ann Intern Med. 2006 Dec 19;145(12):895–900. doi: 10.7326/0003-4819-145-12-200612190-00006. [DOI] [PubMed] [Google Scholar]
- 47.Gurudu SR, Fry LC, Fleischer DE, Jones BH, Trunkenbolz MR, Leighton JA. Factors contributing to patient nonattendance at open-access endoscopy. Dig Dis Sci. 2006 Nov;51(11):1942–5. doi: 10.1007/s10620-006-9215-0. [DOI] [PubMed] [Google Scholar]
- 48.Lee CS, McCormick PA. Telephone reminders to reduce non-attendance rate for endoscopy. J R Soc Med. 2003 Nov;96(11):547–8. doi: 10.1258/jrsm.96.11.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.