Abstract
Background
Aspirin is an effective, safe, and inexpensive early treatment of acute myocardial infarction (AMI) with few barriers to administration, even in countries with limited healthcare resources. However, the rates and recent trends of aspirin use for the early treatment of AMI in China are unknown.
Methods and Results
Using data from the China Patient‐centered Evaluative Assessment of Cardiac Events Retrospective Study of Acute Myocardial Infarction (China PEACE‐Retrospective AMI Study), we identified a cohort of 14 041 patients with AMI eligible for early aspirin therapy. Early use of aspirin for AMI increased over time (78.4% in 2001, 86.5% in 2006, and 90.0% in 2011). However, about 15% of hospitals had a rate of use of <80% in 2011. Treatment was less likely in patients who were older, presented with cardiogenic shock at admission, presented without chest discomfort, had a final diagnosis of non‐ST‐segment elevation acute myocardial infarction, or did not receive reperfusion therapy. Hospitalization in rural regions was also associated with aspirin underuse.
Conclusions
Despite improvements in early use of aspirin for AMI in China, there remains marked variation in practice and opportunities for improvement that are concentrated in some hospitals and patient groups.
Clinical Trial Registration
URL: ClinicalTrials.gov Unique identifier: NCT01624883.
Keywords: acute myocardial infarction, aspirin, quality of care
Introduction
Practice guidelines recommend aspirin administered early in the course of acute myocardial infarction (AMI) for every patient without contraindications to treatment. The drug is safe, effective, inexpensive, widely available, and easy to administer.1–4 Because of these properties, even in care settings with limited resources and access to specialty care, there should be few barriers to the administration of aspirin.
In China, like many other low‐ and middle‐income countries, there is a particular need to optimize the use of cost‐effective medications such as aspirin. Prior studies have evaluated the early use of aspirin in selected Chinese hospitals,5–7 and recently a high‐level analysis of a nationally representative sample of Chinese hospitals demonstrated a significant increase in the utilization of aspirin therapy among eligible patients with ST‐segment elevation myocardial infarction over the past decade.8 However, it remains unknown whether the progress made in aspirin therapy has been experienced by all patients and in all treatment settings, including in urban and rural hospitals and across regions. A careful assessment of aspirin use over the past decade is important for learning about how best to position future interventions to ensure that each eligible patient with AMI receives aspirin.
Accordingly, to support efforts to improve the quality of care for AMI, we analyzed data from the China Patient‐centered Evaluative Assessment of Cardiac Events Retrospective Study of Acute Myocardial Infarction (China PEACE‐Retrospective AMI Study), a large, government‐sponsored, nationally representative study of patients with AMI admitted to 162 randomly selected hospitals throughout China in 2001, 2006, and 2011. Our objectives were to (1) describe current rates of early aspirin use (ie, within the first 24 hours of admission) among patients with AMI; (2) examine temporal trends in early aspirin use across regions and hospitals; and (3) identify the patient and hospital characteristics associated with a lower likelihood of receiving early aspirin. These findings are critical for China, a country with a population of 1.3 billion and estimated patients with AMI to reach 23 million by 2030,9 given the lifesaving potential of aspirin.
Methods
Design Overview of China PEACE‐Retrospective AMI Study
The design of the China PEACE‐Retrospective AMI Study has been published previously.10 In brief, we created a nationally representative sample of hospitalizations for AMI during 2001, 2006, and 2011 using 2‐stage random sampling. In the first stage, we identified hospitals using a simple random sampling procedure within each of the 5 study strata: Eastern‐rural, Central‐rural, Western‐rural, Eastern‐urban, and Central/Western‐urban regions, since hospital volumes and clinical capacities differ between urban and rural areas as well among the 3 official economic‐geographic regions (Eastern, Central, and Western) of Mainland China. We considered Central and Western urban regions together, given their similar per‐capita income and health services capacity. In the 3 rural strata, the sampling framework consisted of the central hospital in each of the predefined rural regions (2010 central hospitals in 2010 rural regions). In the 2 urban strata, the sampling framework consisted of the highest‐level hospitals in each of the predefined urban regions (833 hospitals in 287 urban regions) (Figure 1). Since the majority of hospitals in China are publicly owned and administered, hospital closure is rare. We selected representative hospitals from 2011 to reflect current practices and trace this cohort backward to 2006 and 2001 to describe temporal trends. In the second stage, we drew cases based on the local hospital database for patients with AMI in each year at each sampled hospital using systematic random sampling procedures. Patients with AMI were identified using International Classification of Diseases—Clinical Modification codes, including versions 9 (410.xx) and 10 (I21.xx), when available or through principal discharge diagnosis terms. Data were collected via standardized central medical chart abstraction using standardized data definitions. We adopted rigorous monitoring at each stage to ensure data quality.10 Data abstraction quality was monitored by randomly auditing 5% of the medical records, with overall variable accuracy exceeding 98%.
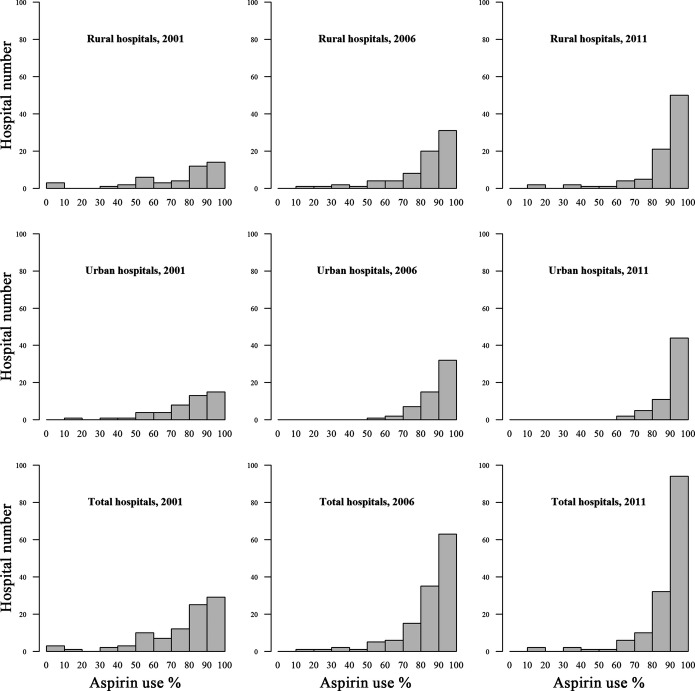
Figure 1.
Flow diagram of the study sample. AMI indicates acute myocardial infarction.
We sampled 175 hospitals; 7 did not have admissions for AMI and 6 declined participation. Examination of patient databases from the participating 162 hospitals yielded 31 601 hospitalizations for AMI in 2001, 2006, and 2011. We sampled 18 631 cases and finally acquired eligible medical records for 18 110 (97.2%). After excluding those that were uninterpretable medical chart, duplicate, non‐AMI, beyond the study periods, and developed AMI during hospitalization, we identified 16 100 cases with available medical charts (Figure 1).
The central ethics committee at the China National Center for Cardiovascular Diseases approved the China PEACE‐Retrospective AMI Study. All collaborating hospitals accepted the central ethics approval except for 5 hospitals, which obtained local approval by internal ethics committees. The study is registered at www.clinicalTrials.gov (NCT01624883).
Study Sample
Only those patients with a definite discharge diagnosis of AMI and eligible for aspirin therapy within 24 hours of admission were included in the study sample. The diagnosis of AMI was determined by the combination of clinical discharge diagnosis terms and ECG results. If the local diagnosis was not definitive, cardiologists at the coordinating centre reviewed the medical record and ECG to determine diagnosis. We excluded patients who were transferred from other hospitals because they might have received acute treatments at their presenting hospitals. We also excluded patients who died, were discharged, or transferred out within 24 hours of admission because we assumed that such patients might not have had an opportunity to receive aspirin. We also excluded patients with contraindications to aspirin (allergy to aspirin, active bleeding at admission, history of hemorrhagic stroke, or any physician‐documented contraindications to aspirin). All remaining patients were considered eligible for the study.
Variables
Patient‐level independent variables in this study included demographic information, medical history, clinical characteristics at admission, reperfusion therapy, and year of hospitalization. Hospital characteristics included teaching status, percutaneous coronary intervention capability, economic geographic region, and urban or rural location. Early aspirin use was defined as prescription of aspirin within 24 hours of admission for AMI. Details of these variables are shown in Table.
Table 1.
Bivariate Analysis of Characteristics Associated With Patients Receiving Early Aspirin
| Characteristics | Total (%) (N=14 041) | Early Aspirin User (%) (N=12 260) | Early Aspirin Non‐User (%) (N=1781) | P Value |
|---|---|---|---|---|
| Demographic | ||||
| Age, y | <0.001 | |||
| <55 | 22.1 | 23.0 | 16.3 | |
| 55 to 64 | 23.6 | 24.0 | 20.9 | |
| 65 to 74 | 30.1 | 29.9 | 31.0 | |
| ≥75 | 24.2 | 23.1 | 31.8 | |
| Gender | <0.001 | |||
| Male | 69.9 | 70.7 | 64.4 | |
| Female | 30.1 | 29.3 | 35.7 | |
| Cardiac risk factors | ||||
| Prior hypertension | 49.5 | 49.9 | 46.8 | 0.015 |
| Prior diabetes | 17.4 | 17.3 | 18.1 | 0.388 |
| Current smoker | 34.7 | 35.8 | 27.3 | <0.001 |
| Medical histories | ||||
| Ischemic stroke | 10.0 | 9.7 | 12.0 | 0.003 |
| Myocardial infarction | 10.8 | 10.9 | 10.3 | 0.460 |
| Primary PCI | 1.9 | 2.0 | 1.3 | 0.059 |
| Clinical characteristics at admission | ||||
| Chest discomfort | 91.9 | 93.5 | 81.5 | <0.001 |
| Cardiac arrest | 1.0 | 0.8 | 2.0 | <0.001 |
| Cardiogenic shock | 4.2 | 4.0 | 5.9 | <0.001 |
| Blood pressure mmHg | 0.080 | |||
| SBP<180 and DBP<110 | 91.6 | 91.8 | 90.6 | |
| SBP≥180 or DBP≥110 | 8.4 | 8.2 | 9.4 | |
| AMI type | <0.001 | |||
| STEMI | 85.4 | 86.1 | 80.6 | |
| NSTEMI | 14.6 | 13.9 | 19.4 | |
| Reperfusion therapy | 0.027 | |||
| No reperfusion | 69.3 | 67.4 | 82.5 | |
| Fibrinolytic therapy | 20.3 | 21.4 | 12.4 | |
| Primary PCI | 10.4 | 11.2 | 5.2 | |
| Hospital characteristics | ||||
| Teaching hospital | 80.8 | 80.7 | 75.5 | <0.001 |
| PCI‐capable hospital | 60.7 | 62.2 | 50.3 | <0.001 |
| Economic geographic region | 0.915 | |||
| Eastern | 59.2 | 58.6 | 62.7 | |
| Center | 21.3 | 21.5 | 19.4 | |
| Western | 19.6 | 19.8 | 17.9 | |
| Urban/Rural | <0.001 | |||
| Urban | 61.1 | 62.3 | 52.8 | |
| Rural | 38.9 | 37.7 | 47.2 | |
| Year | <0.001 | |||
| 2001 | 15.0 | 13.6 | 24.9 | |
| 2006 | 28.3 | 28.1 | 29.6 | |
| 2011 | 56.7 | 58.3 | 45.5 |
AMI indicates acute myocardial infarction; DBP, diastolic blood pressure; NSTEMI, non‐ST‐segment elevation myocardial infarction; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; STEMI, ST‐segment elevation myocardial infarction.
Statistical Analysis
Patient demographic information, clinical history, presenting clinical features, and treatment patterns were compared between eligible patients who received aspirin within 24 hours of admission and those who did not. We employed standard parametric and nonparametric techniques for observational data, including Wilcoxon rank sum tests for continuous variables and the χ2 test for categorical variables. For hospital rates of aspirin use, only those hospitals with at least 5 patients with AMI were included. To describe the rate of early aspirin therapy in China, we applied weights of each case to account for differences in the sampling fraction within each time period. Factors independently associated with early aspirin therapy were identified with logistic regression using the generalized estimating equation to account for the clustering of patients within hospitals. All selected variables, except those with frequencies <1%, were included in the multivariable model. Backward selection was used to identify the predictive factors of early aspirin use. Specifically, we evaluated all available variables for those that we thought might be associated with aspirin use based on prior reports, face validity, and clinical judgment. Eighteen candidate variables were identified, which we included in the initial model and then removed sequentially from least to most significant. Changes in the likelihood ratio and other parameter estimates were evaluated, and variables were retained if they were significant (P<0.05) in the model with likelihood ratio test. Odds ratios (OR) and 95% CI were reported. Interaction terms were tested between year of presentation and the other factors that were retained in the model. All comparisons were 2‐tailed, with a P<0.05 considered statistically significant. All statistical analyses were performed using SAS software (version 9.2; SAS Institute, Cary, NC).
Results
Study Sample
Of 16 100 patients with AMI, after excluding patients who transferred in (n=607), died (n=500), were discharged (n=326), transferred out (n=297) within 24 hours of admission, or had contraindications to aspirin (n=329), we identified a cohort of 14 041 patients with AMI eligible for early aspirin therapy (Figure 1). This cohort had a median age of 66 years (interquartile range 56 to 74) and 69.9% were men. Comorbidities were common: hypertension (49.5%), diabetes mellitus (17.4%), and previous myocardial infarction (10.8%) (Table).
Use of Early Aspirin Therapy
Overall, 87.3% of patients received early aspirin therapy. Weighted rates of use were 78.8%, 86.4%, and 90.0% in 2001, 2006, and 2011, respectively (P<0.0001 for trend). There were similar trends in use in all 5 regions over time (P<0.0001 for trend for all 5 regions); especially in Central and Western‐rural areas, aspirin early use increased from <70% in 2001 to almost 90% in 2011 (Figure 2). The rate of early aspirin use in 2011 was highest in the Central/Western‐urban region (92.7%) and lowest in the Eastern‐rural region (87.0%).
Figure 2.

Trends in early aspirin use for acute myocardial infarction in 2001, 2006, and 2011 by Chinese Geographic Regions. P<0.001 for trend for all 5 regions. CR indicates Central‐rural; C/WU, Central/Western‐urban; ER, Eastern‐rural; EU, Eastern‐urban; WR, Western‐rural.
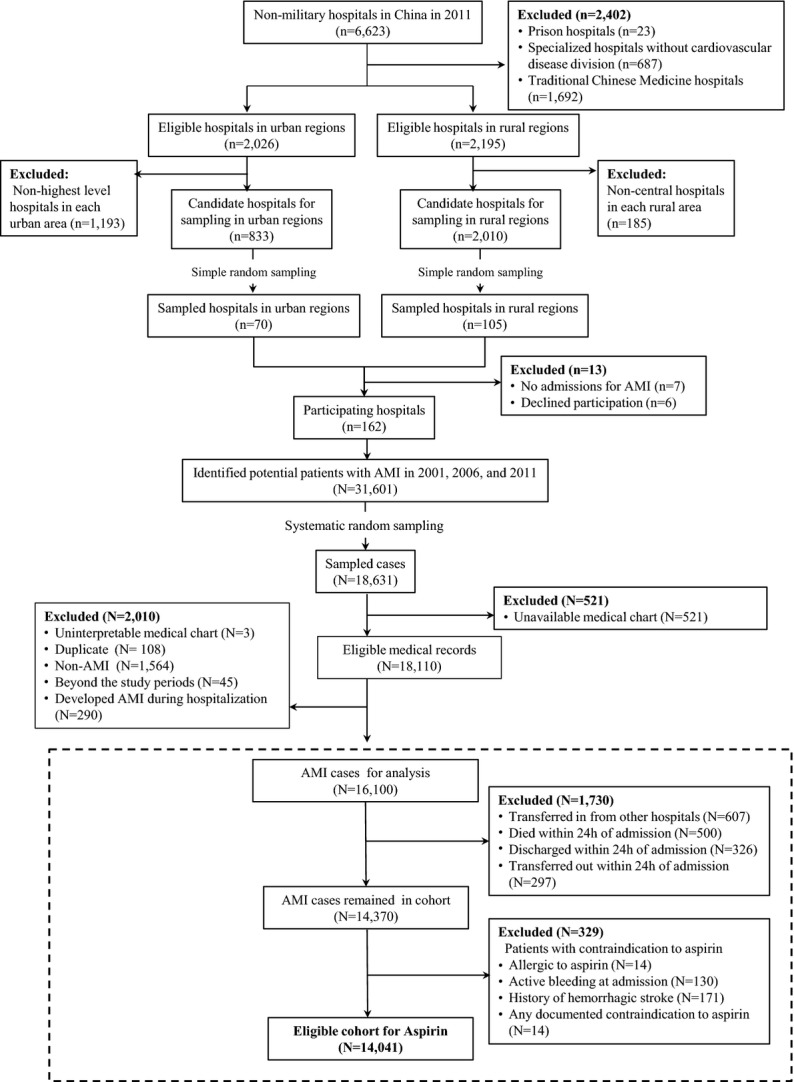
The proportion of best‐performing hospitals, defined as having at least 90% of eligible patients receiving early treatment, increased during the past decade, from 31.5% in 2001 to 48.8% in 2006 to 63.5% in 2011 (Figure 3). However, although the overall use of early aspirin therapy improved in rural hospitals, patients receiving care in these hospitals were less likely to receive early aspirin than in urban hospitals: in 2011, 17.4% of rural hospitals versus 11.3% of urban hospitals prescribed early aspirin for <80% of eligible patients.
Figure 3.
Trends of early aspirin therapy in rural and urban regions in 2001, 2006, and 2011 (hospitals with sample size <5 patients were excluded).
Patient and Hospital Characteristics Associated With Early Aspirin Use
In the multivariable model, patients who were ≥75 years (OR 0.66; 95% CI 0.52 to 0.83 compared with younger patients), presented with cardiogenic shock (OR 0.67; 95% CI 0.52 to 0.85), had a final diagnosis of non‐ST segment elevation myocardial infarction (OR 0.73; 95% CI 0.63 to 0.85 versus ST‐segment elevation myocardial infarction) or were hospitalized in a rural region (OR 0.68; 95% CI 0.49 to 0.93) were significantly less likely to receive early aspirin. In contrast, patients presenting with chest discomfort (OR 2.76; 95% CI 2.32 to 3.28), were hospitalized in 2006 or 2011 (OR 1.92; 95% CI 1.44 to 2.56, and OR 2.74; 95% CI 2.08 to 3.62, respectively, versus 2001) or received reperfusion therapies during admission were more likely to receive early aspirin (OR 1.96; 95% CI 1.63 to 2.35 for fibrinolytic therapy versus no acute reperfusion, OR 1.76; 95% CI 1.05 to 2.94 for primary percutaneous coronary intervention versus no acute reperfusion) (Figure 4). There were no significant interactions between these factors and year.
Figure 4.
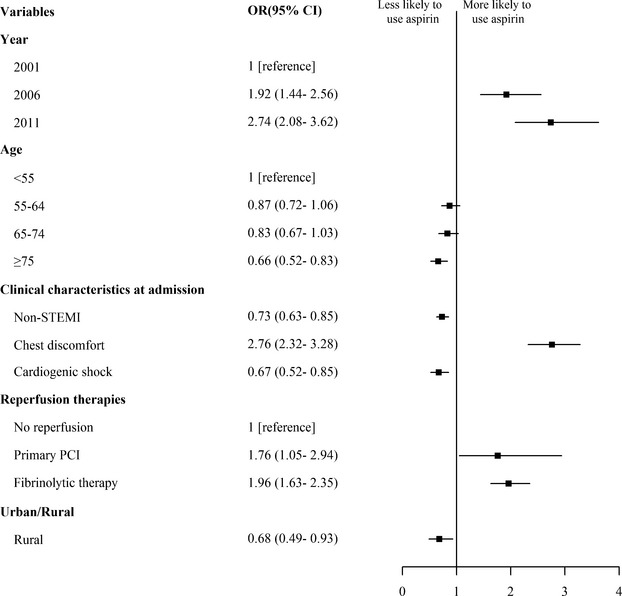
Factors associated with early use of aspirin in multivariable model (c‐statistic 0.683). Variables in the final multivariable model are shown along the vertical axis. The strength of effect is shown along the horizontal axis with the vertical line demarking an odds ratio (OR) of 1 (OR=1, no association); estimates to the left (OR<1) indicates that patients with the characteristic have a lower likelihood of receiving aspirin than those without the characteristic, while those to the right (OR>1) indicates that patients with the characteristic have a higher likelihood of receiving aspirin than those without the characteristic. Each square and line represents the point estimate of the effect of that variable in the model, while the line shows the 95% CI. CI indicates confidence interval; NSTEMI, non‐ST‐segment elevation myocardial infarction; OR, odds ratio; PCI, percutaneous coronary intervention.
Discussion
In this study of a nationally representative sample of hospitalizations in China, we found improvements between 2001 and 2011 in the use of aspirin therapy within 24 hours of admission for AMI and concomitant attenuation in regional variation in use. However, even in the final year of our study, there were still areas for improvement. In 2011, about 1 in 10 eligible patients still did not receive early aspirin therapy, with lower rates in rural hospitals or in certain patient groups. This is the first study, to our knowledge, that characterizes contemporary trends in the early use of a readily available and effective therapy in a nationally representative population of patients with AMI in China, a country that is experiencing a marked increase in mortality and morbidity due to AMI.
In the present study, the use of early aspirin therapy is somewhat lower than that among patients with acute coronary syndrome reported by previous studies. Some multicenter studies reported that 95% of patients with acute coronary syndrome received early or in‐hospital aspirin therapy in China.6–8 One possible explanation for the difference is that previous studies have been largely limited to tertiary care centers in urban regions and major metropolitan areas. The present study, with a nationally representative sample of hospitalizations for AMI in China, likely better reflects the actual practice patterns for AMI.
The increase in early aspirin use in China between 2001 and 2011 represents a substantial improvement in the use of a simple, inexpensive, and widely available evidence‐based therapy for AMI. In this study, we found that there has been marked improvement in early aspirin use over the past decade, with narrowing in the disparity in use between urban and rural regions. Moreover, the proportion of hospitals treating >90% of their eligible patients also significantly increased over time. Although we were not able to study the factors that may account for these dramatic improvements, they may be attributable to education on the utilization of evidence‐based therapies for AMI and increases in medical insurance coverage and in healthcare expenditure by government.11
Despite the overall improvement in early aspirin use, about 1 in 10 eligible patients did not receive early aspirin therapy in 2011. In developed countries, aspirin is more widely used. In the United States, rate of aspirin use within 24 hours after admission was >97% in 2009.12 There are few recent comparisons with the early use of aspirin in other countries but in Europe, 97% of patients with AMI from 47 countries received early aspirin management in 2009.13 The higher rates of use in the United States and Europe may reflect the impact of quality‐improvement efforts focused on this critical process of care that have not to this point been conducted in China.
Aspirin early in the course of AMI was particularly underused in specific patient groups. Consistent with previous studies, older patients were less likely to receive early aspirin.14–15 This may reflect concerns about the risk of bleeding. However, while elderly patients may be at high risk for adverse consequences of therapy, their risks for adverse consequences of no treatment are also likely substantially higher; a study reported that in elderly patients, the use of aspirin was associated with 22% lower odds of 30‐day mortality, which exceeded 20% in the older population.14 Therefore, the benefits of aspirin outweighed the risks for this subgroup in clinical trials. Patients who did not present with overt symptoms of AMI (such as chest discomfort) were less likely to be given aspirin, which may reflect diagnostic uncertainty. Patients with cardiogenic shock at admission were also less likely to be administered aspirin. This may have been because these patients were at a high risk for mortality and their physicians focused on emergency treatment to stabilize vital signs or interventions using advanced technology,16 while the simple use of aspirin was delayed. In addition, the early treatment of patients with aspirin was positively associated with the provision of reperfusion therapy. Thus, failure to use aspirin may be a marker for other deficits in the quality of care.
We also found that although use of aspirin improved in both urban and rural hospitals, gaps in care remained more pronounced in rural centers in 2011. China is a country with unbalanced economic development. Most of the rural hospitals, which are responsible for the care of more than 700 million people,17 have limited clinical capacity for advanced cardiac care and limited funding. However, because the cost of aspirin is minimal in China ($0.04 for acute treatment)18 and has a dramatic effect on mortality,1 this treatment is particularly relevant to rural hospitals. In our study, 17.4% of rural hospitals had treatment rates below 80% in 2011 compared with 11.3% of urban hospitals. Successful initiatives to improve aspirin use in China with a particular focus on rural hospitals could have an important impact on quality of care.
Certain factors should be considered in the interpretation of our results. First, the retrospective design restricted our analysis to information based on medical records. Some patients may have had contraindications to the therapy that were not documented in the records, which may have led to an underestimation of the utilization in eligible patients. However, the retrospective design and the standardized central abstraction ensured reliable data in accordance with the original medical records. Second, the missing data may vary across years, therefore biasing the analysis of trends. However, the number missing is small and therefore the effect should be minimal. Third, we excluded lower‐level urban hospitals and noncentral rural hospitals from our sample. This sampling strategy was employed to ensure sample sizes within each of the participating institutions to provide adequately precise hospital‐level estimates of care quality. It is possible that practice in the excluded hospitals differed from that of those in the study sample. Finally, we did not have long‐term follow‐up to determine whether the patterns of aspirin use were associated with health outcomes and we were underpowered to determine the early benefits and bleeding risk of aspirin therapy in the eligible cohort.
In conclusion, in China, we found a marked improvement in early aspirin therapy among patients with AMI over the past decade. However, use remained suboptimal in certain patient groups and care settings. Despite generally good performance, even this treatment could benefit from a quality improvement focus.
Appendix
Site Investigators by Hospital in China PEACE‐Retrospective AMI Study
Aba Tibetan and Qiang Autonomous Prefecture People's Hospital, Shiping Weng, Shuying Xie; Affiliated Hospital of Guiyang Medical College, Lirong Wu, Jiulin Chen; Affiliated Hospital of Hainan Medical College, Tianfa Li, Jun Wang; Affiliated Zhongshan Hospital of Dalian University, Qin Yu, Xiaofei Li; Alxa League Central Hospital, Zhong Li, Shiguo Hao, Yuzhen Zhang, Xuemei Wu; Baiquan County People's Hospital, Yachen Zhang, Zhifeng Liu; Biyang People's Hospital, Zhongxin Wang, Hao Jia; Bortala Mongol Autonomous Prefecture People's Hospital, Bayin Bate, Badeng Qiqige; Changda Hospital of Anshan, Xiang Jin, Ting Cai; Chengwu County People's Hospital, Fengqin Liu, Dayong Xu; Chenxi County People's Hospital, Xuejin He, Shui Yang; Chongren County People's Hospital, Chun Yuan, Jiping Wang; County People's Hospital of Jinning, Lihua Gu, Lin Li, Shijiao Chen; Dalian Municipal Central Hospital, Yongchao Zhi, Lili Sun; Dao County People's Hospital, Shengcheng Zhou, Lingjiao Jin; Daofu County People's Hospital, Yong Leng, Liangchuan Zhang, Tianyun Deng; Dingyuan County People's Hospital of Anhui Province, Yuanjin Wang, Wenhua Zhang, Xinmin Ma; Dongyang People's Hospital, Weimin Li, Liang Lu, Xuan Ge; Dulong and Nu Autonomous County People's Hospital of Gongshan, Xiaoping Wu, Yanming He; Dunhua City Hospital of Jilin Province, Fanju Meng, Jia Li; Fenghuang County People's Hospital, Dexi Liao, Guangyong Liu, Wen Qin; Fengshan County People's Hospital, Wen Long, Xiangwen Chen; Fourth Hospital of Baotou City, Baohong Zhang, Yonghou Yin, Bin Tian; Fourth People's Hospital of Zigong City, Yong Yi, Chaoyong Wu; Fugu County People's Hospital of Shaanxi Province, Baoqi Liu, Zhihui Zhao, Haiming Li; Fujian Provincial Hospital, Yansong Guo, Xinjing Chen; Fuling Center Hospital of Chongqing City, Liquan Xiang, Lin Ning; Gannan County People's Hospital, Mei Chen, Xin Jin, Guiling Li; General Hospital of the Yangtze River Shipping, Xiuqi Li, Xing'an Wu; Gongcheng Yao Autonomous County People's Hospital, Congjun Tan, Mingfang Feng, Meili Wang; Guangchang County People's Hospital, Liangfa Wen, Xiang Fu, Qunxing Xie; Guilin People's Hospital, Wei Zhang, Yanni Zhuang, Hua Lu;Guiping People's Hospital, Jiaqian Lu, Yu Huang; Haerbin 242 Hospital, Yin Zhou, Qiuling Hu; Haiyan People's Hospital, Chunhui Xiao, Xiaoli Hu; Heling Ge Er County People's Hospital, Yongshuan Wu, Qiuli Wang; Helong Municipal People's Hospital, Youlin Xu, Xuefei Yu; Henan Provincial People's Hospital, Chuanyu Gao, Jianhong Zhang, You Zhang; Heze Municipal Hospital, Wentang Niu, Xiaolei Ma, Yong Wang; HGKY Group Company General Hospital, Xiaowen Pan, Yanlong Liu; Hua Xin Hospital First Hospital of Tsinghua University, Lifu Miao, Yanping Yin, Zhiying Zhang; Huairen People's Hospital, Shutang Feng; Huayin People's Hospital, Aiping Wang, Jiangli Zhang, Feipeng Li; Huaying People's Hospital, Hong Wang; Hunchun Hospital, Lijun Yu, Xinxin Zhao; Huizhou Municipal Central Hospital, Yuansheng Shen, Zhiming Li, Lizhen He; Hunan Province Mawangdui Hospital, Zhiyi Rong, Wei Luo; Ji'an Municipal Central People's Hospital, Xueqiao Wang; Jianghua Yao Autonomous County People's Hospital, Rongjun Wan, Jianglin Tang, Guanghan Wu; Jiangsu Haimen People's Hospital, Jie Wu, Bin Xu; Jiangxi Provincial People's Hospital, Qing Huang, Xiaohe Wu; Jiangzi County People's Hospital, Sang Ge, Pian Pu, Pingcuo Duoji; Jilin Province People's Hospital, Hui Dai, Yuming Du, Wei Guo; Jilin Integrated Traditional Chinese & Western Medicine Hospital, Jilin Province, Jianping Shi; Jinghai County Hospital, Peihua Zhao, Jingsheng Sun; Jingxi County People's Hospital, Hongxiang Li, Wen Liang; Jingxing County Hospital, Zhiwen Dong, Zhenhai Zhao; Jingzhou Central Hospital, Xin Li, Qin Xu; Jiuquan City People's Hospital, Yaofeng Yuan, Zhirong Li; Jixi People's Hospital of The Jixi Municipal People's Hospital Medical Group, Jinbo Gao; Jize County Hospital, Qiu'e Guo; Kangbao County People's Hospital, Ruiqing Zhao, Guangjun Song; Keshiketengqi Hospital of Chifeng City, Lize Wang, Haiyun Song; Lanping Bai and Pumi Autonomous County People's Hospital, Jinwen He, Jinming He; Laoting County Hospital, Keyong Shang, Changjiang Liu, Kuituan Xi; Liaoyang Central Hospital, Rihui Liu, Peng Guo; Liaoyuan Central Hospital, Chaoyang Guo, Xiangjun Liu, Rujun Zhao, Zeyong Yu; Lindian County Hospital, Wenzhou Li, Xudong Jing, Huanling Wang; Linxiang People's Hospital, Xiyuan Zhao, Chao Zhang, Long Chen; Liujiang County People's Hospital, Meifa Wei, Yan Liu, Shengde Chen; Longyan First Hospital, Kaihong Chen, Yong Fang, Ying Liao; Luancheng County Hospital, Junli Wang, Tianyu Liu, Suzhe Cheng; Lucheng People's Hospital, Yunke Zhou, Xiaoxia Niu, Huifang Cao; Luchuan County People's Hospital, Zebin Feng, Min Feng; Luxi County People's Hospital, Feilong Duan, Haiming Yi; Luyi County People's Hospital, Yuanxun Xu, Anran Guo; Macheng People's Hospital, Xianshun Zhou, Hongzhuan Cai, Peng Zheng; Mengcheng First People's Hospital, Gaofeng Guo; Menglian Lahu dai wa autonomous counties People's Hospital, Xiang Li; Min County People's Hospital, Minwu Bao, Yuhong Liu; Nanjing First Hospital, Shaoliang Chen, Haibo Jia, Hongjuan Peng; Nan'an Hospital, Duanping Dai, Shaoxiong Hong; Nantong Third People's Hospital, Song Chen, Dongya Zhang, Ying Wang; Nanyang Central Hospital, Yudong Li, Jianbu Gao, Shouzhong Yang; Ningwu County People's Hospital, Junhu An; Peking University People's Hospital, Chenyang Shen, Yunfeng Liu; Peking University Shenzhen Hospital, Chun Wu, Huan Qu, Saiyong Chen; People's Hospital of Jingyu, Yuhui Lin, Dehai Jiao; People's Hospital of Yueqing City, Manhong Wang, Qiu Wang; Pianguan County People's Hospital, Yingliang Xue, Ruijun Zhang; Puding County People's Hospital, Cheng Yuan, Lei Wu; Qinghai Red Cross Hospital, Jianqing Zhang, Chunmei Wei, Yanmei Shen; Qinshui County People's Hospital, Hehua Zhang, Hongmei Pan, Yong Gao; Qinyang People's Hospital, Xiaowen Ma, Yanli Liang, Tianbiao Wang; Queshan County People's Hospital, Daguo Zhao; Quzhou People's Hospital, Xiaoming Tu, Zhenyan Gao; Rongjiang County People's Hospital, Fangning Wang, Qiang Yang; Rudong County People's Hospital, Xiaoping Kang, Jianbin Fang, Dongmei Liu; Ruyang County People's Hospital, Chengning Shen, Mengfei Li; Shangluo Central Hospital, Yingmin Guan, Wenfeng Wang, Ting Xiao; Shangqiu Changzheng People's Hospital, Qian Wang; Shaoyang County People's Hospital, Fengyun Jiang, Kaiyou Wu; Shengsi People's Hospital, Songguo Wang; Shenyang Weikang Hospital, Xujie Fu, Shu Zhang, Lifang Gao; Shougang Shuicheng Iron & Steel (Group) Co., Ltd. General Hospital, Min Zhang, Kai Fu, Xiaojing Duan; Shuangshan Hospital Of Anshan, Rui Xiao, Ruixia Wu, Bin Li; Siziwang County People's Hospital, Hongtu Zhang, Yuerong Ma, Zhonghui Cao; Sunan Yugur Autonomous County People's Hospital, Zhansheng Ba, Wanhai Fu; Taizhou Hospital of Zhejiang Province, Jianjun Jiang, Yafei Mi, Weiwei Zhou; The Affiliated Hospital of Beihua University, Feng Sun, Qi Zhang, Shiyu Zheng; The Fifth People's Hospital of Dalian, Jing Zhang, Yang Zhong; The First Affiliated Hospital of Hebei North University, Fangjiang Li, Xiaoyuan Wang; The First Affiliated Hospital of Henan University of Science & Technology, Pingshuan Dong, Laijing Du, Wei Liu; The First Affiliated Hospital of Jia Mu Si University, Zhaofa He, Meihua Jin; The First Hospital of Fuzhou City, Ting Jiang, Zhuoyan Chen; The First Hospital of Xi'an, Manli Cheng, Yuqiang Ji; The First People's Hospital of Danzhou, Youhua Zhou, Jvyuan Li; The First People's Hospital of Guangzhou, Yizhi Pan, Jian Liu; The First People's Hospital of Guangyuan, Tianxun Wang, Ping Yang; The Fourth People's Hospital of Shangqiu Shi, Guiyu Huang, Jianjun Pan, Qingliang Cai, Qianying Wang; The General Hospital of Yongzhou, Hunan Province, Mingli Lv; The People's Hospital of Wuchuan, Yuanming Yi, Xuelian Deng; The People's Hospital of Yuanling, Wenhua Chen, Rong Cai; The People's Hospital of Zhijiang City, Bing Zhang; The Second Affiliated Hospital of Harbin Medical University, Bo Yu, Yousheng Xu, Zhengqiu Wang; The Second Affiliated Hospital of Kunming Medical University, Jun Shu, Ge Zhang, Kai Li; The Second Central Hospital of Baoding City, Guang Ma, Puxia Suo; The Second People's Hospital of Liaoyuan City, Aimin Zhang, Yongfen Kang; Tianjin Medical University General Hospital, Zheng Wan, Yuemin Sun, Bo Bian; Tibet Autonomous Region People's Hospital, Xuejun Hu, Dawa Ciren; Tongchuan Mining Bureau Central Hospital, Guojiong Jia, Jieli Pan; Tongliang County People's Hospital, Guofu Li, Hongliang Zhang, Longliang Zhan; Tongliao City Horqin District First People's Hospital, Junping Fang, Xinli Yu; Ulanqab Central Hospital, Dacheng Wang, Dajun Liu, Xinhong Cao; Wencheng County People's Hospital, Yi Tian, Haisheng Zhu,Wanchuan Liu; Wuhai People's Hospital, Zhaohai Zhou, Lei Shi; Wuhu Second People's Hospital, Wuwang Fang, Manxin Chen; Wulate County People's Hospital, Fuqin Han, Jianye Fu, Yunmei Wang; Wuqiang County People's Hospital, Binglu Liu, Yanliang Zhang, Xiupin Yuan; Wuyishan Municipal Hospital, Qingfei Lin, Yun Chen; Xiangtan County People's Hospital, Yuliang Zhu, Zhiqiang Cai; Xing County People's Hospital, Xingping Li, Lirong Ao; Xingshan County People's Hospital, Shubing Wu, Hui Zhang; Xinmi First People's Hospital, Fusheng Zhao, Guangming Yang; Xinshao County People's Hospital, Renfei Liu, Wenwei Ai; Xiuwu County People's Hospital, Jianbao Chang, Haijie Zhao; Xuanhan County People's Hospital, Qijun Ran, Xuan Ma; Xupu County People's Hospital, Shijun Jiang, Xiaochun Shu; Yanggao County People's Hospital, Zhiru Peng, Yan Han; Yanqing County Hospital, Jianbin Wang, Li Yang; Ying County People's Hospital, Yu Shen, Xingcun Shang; Yitong Manchu Autonomous County First People's Hospital, Haifeng Wang; Yongxing County People's Hospital, Hongyan Li, Zhisong Liao, Yang Cao; Yuanzhou District People's Hospital of Guyuan City, Xiaoping Gao, Meiying Cai, Lining You; Yuncheng Central Hospital, Xuexin Li, Shuqin Li, Yingjia Li; Yunlong County People's Hospital, Jianxun Yang, Song Ai, Jianfei Ma; Yuyao People's Hospital, Lailin Deng; Zhangjiachuan Hui Autonomous County First People's Hospital, Keyu Wang, Shitang Gao, Jian Guan; Zhouning County Hospital, Banghua He, Youyi Lu; Zhuoni County People's Hospital, Weirong Yang, Hong Li; Zhuozi County People's Hospital, Zhizhong Zhang, Xiaohong Chi; Zuoyun County People's Hospital, Ru Duan, Guangli Wang.
Sources of Funding
This work was supported by the National Health and Family Planning Commission of the People's Republic of China (grant number 201202025) and the National Heart, Lung, and Blood Institute (HMK grant number U01 HL105270‐03 [Center for Cardiovascular Outcomes Research at Yale University]). The sponsors had no role in the conduct of the study; in the collection, management, analysis, and interpretation of the data; or in the preparation or approval of the manuscript.
Disclosures
Dr Krumholz reports that he is a recipient of research grants from Medtronic and Johnson & Johnson, through Yale University, to develop methods of clinical trial data sharing. In addition, he is the chair of a cardiac scientific advisory board for UnitedHealth. Dr Masoudi receives salary support from the American College of Cardiology for his role as the Senior Medical Officer of the National Cardiovascular Data Registries. The authors declare no other relevant conflicts of interest.
Acknowledgments
We appreciate the multiple contributions made by study teams at the China Oxford Centre for International Health Research and the Yale‐New Haven Hospital Center for Outcomes Research and Evaluation in the realms of study design and operations, particularly the data collection by Yi Pi, Jiamin Liu, Wuhanbilige Hundei, Haibo Zhang, Lihua Zhang, Xue Du, Wenchi Guan, Xin Zheng, and Yuanlin Guo. We appreciate the analysis advice by Yongfei Wang, Haiqun Lin, and Shuxia Li. We appreciate the editing by Sudhakar V. Nuti, Nicholas Downing, and Sisi Wang. We are grateful for the support provided by the Chinese government. We are particularly grateful for all the collaborators listed in the Appendix.
References
- 1.ISIS‐2 Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS‐2. Lancet. 1988; 2:349-360. [PubMed] [Google Scholar]
- 2.Gunnar RM, Passamani ER, Bourdillon PD, Pitt B, Dixon DW, Rapaport E, Fuster V, Reeves TJ, Karp RB, Russell RO., Jr Guidelines for the early management of patients with acute myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee to Develop Guidelines for the Early Management of Patients with Acute Myocardial Infarction). J Am Coll Cardiol. 1990; 16:249-292. [DOI] [PubMed] [Google Scholar]
- 3.Antithrombotic Trialists' Collaboration. Collaborative meta‐analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002; 324:71-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaspoz JM, Coxson PG, Goldman PA, Williams LW, Kuntz KM, Hunink MG, Goldman L. Cost effectiveness of aspirin, clopidogrel, or both for secondary prevention of coronary heart disease. N Engl J Med. 2002; 346:1800-1806. [DOI] [PubMed] [Google Scholar]
- 5.Gao R, Patel A, Gao W, Hu D, Huang D, Kong L, Qi W, Wu Y, Yang Y, Harris P, Algert C, Groenestein P, Turnbull F. Prospective observational study of acute coronary syndromes in China: practice patterns and outcomes. Heart. 2008; 94:554-560. [DOI] [PubMed] [Google Scholar]
- 6.Liu Q, Zhao D, Liu J, Wang W. Current clinical practice patterns and outcome for acute coronary syndromes in China: results of BRIG project. Zhonghua Xin Xue Guan Bing Za Zhi. 2009; 37:213-217. [PubMed] [Google Scholar]
- 7.Zhang LJ, Chen YD, Song XT, Zhao FH, Lu SZ. Antithrombotic and antiplatelet therapies in relation to risk stratification in patients with non‐ST elevation acute coronary syndrome: insights from the Sino‐Global Registry of Acute Coronary Events. Chin Med J (Engl). 2009; 122:502-508. [PubMed] [Google Scholar]
- 8.Li J, Li X, Wang Q, Hu S, Wang Y, Masoudi FA, Spertus JA, Krumholz HM, Jiang L. ST‐segment elevation myocardial infarction in China from, 2001 to 2011 (the China PEACE‐Retrospective Acute Myocardial Infarction Study): a retrospective analysis of hospital data. Lancet. 2014http://dx.doi.org/10.1016/S0140-6736(14)60921-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The World Bank. Toward a Healthy and Harmonious Life in China: Stemming the Rising Tide of Non‐Communicable Diseases Available at: http://www.worldbank.org/content/dam/Worldbank/document/NCD_report_en.pdf. Accessed February 8, 2014.
- 10.Dharmarajan K, Li J, Li X, Lin Z, Krumholz HM, Jiang L. The China Patient‐Centered Evaluative Assessment of Cardiac Events (China PEACE) retrospective study of acute myocardial infarction: study design. Circ Cardiovasc Qual Outcomes. 2013; 6:732-740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cao Q, Shi L, Wang H, Dong K. Report from China: health insurance in China—evolution, current status, and challenges. Int J Health Serv. 2012; 42:177-195. [DOI] [PubMed] [Google Scholar]
- 12.Roe MT, Messenger JC, Weintraub WS, Cannon CP, Fonarow GC, Dai D, Chen AY, Klein LW, Masoudi FA, McKay C, Hewitt K, Brindis RG, Peterson ED, Rumsfeld JS. Treatments, trends, and outcomes of acute myocardial infarction and percutaneous coronary intervention. J Am Coll Cardiol. 2010; 56:254-263. [DOI] [PubMed] [Google Scholar]
- 13.Puymirat E, Battler A, Birkhead J, Bueno H, Clemmensen P, Cottin Y, Fox KA, Gorenek B, Hamm C, Huber K, Lettino M, Lindahl B, Muller C, Parkhomenko A, Price S, Quinn T, Schiele F, Simoons M, Tatu‐Chitoiu G, Tubaro M, Vrints C, Zahger D, Zeymer U, Danchin N. Euro Heart Survey 2009 Snapshot: regional variations in presentation and management of patients with AMI in 47 countries. Eur Heart J Acute Cardiovasc Care. 2013; 2:359-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krumholz HM, Radford MJ, Ellerbeck EF, Hennen J, Meehan TP, Petrillo M, Wang Y, Kresowik TF, Jencks SF. Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries: patterns of use and outcomes. Circulation. 1995; 92:2841-2847. [DOI] [PubMed] [Google Scholar]
- 15.Becker RC, Burns M, Gore JM, Lambrew C, French W, Rogers WJ. Early and pre‐discharge aspirin administration among patients with acute myocardial infarction: current clinical practice and trends in the United States. J Thromb Thrombolysis. 2000; 9:207-215. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg RJ, Spencer FA, Gore JM, Lessard D, Yarzebski J. Thirty‐year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population‐based perspective. Circulation. 2009; 119:1211-1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Bureau of Statistics of China. China Statistical Yearbook 2011 Available at: http://www.stats.gov.cn/tjsj/ndsj/2011/indexch.htm. Accessed February 8, 2014.
- 18.Wang M, Moran AE, Liu J, Coxson PG, Heidenreich PA, Gu D, He J, Goldman L, Zhao D. Cost‐effectiveness of optimal use of acute myocardial infarction treatments and impact on coronary heart disease mortality in China. Circ Cardiovasc Qual Outcomes. 2014; 7:78-85. [DOI] [PMC free article] [PubMed] [Google Scholar]